Isotemporal Substitution Effects of Daily Time Use on Cardiorespiratory Fitness of Children in the OptiChild Study: A Mediation Analysis with Diet Quality
Abstract
:1. Introduction
2. Materials and Methods
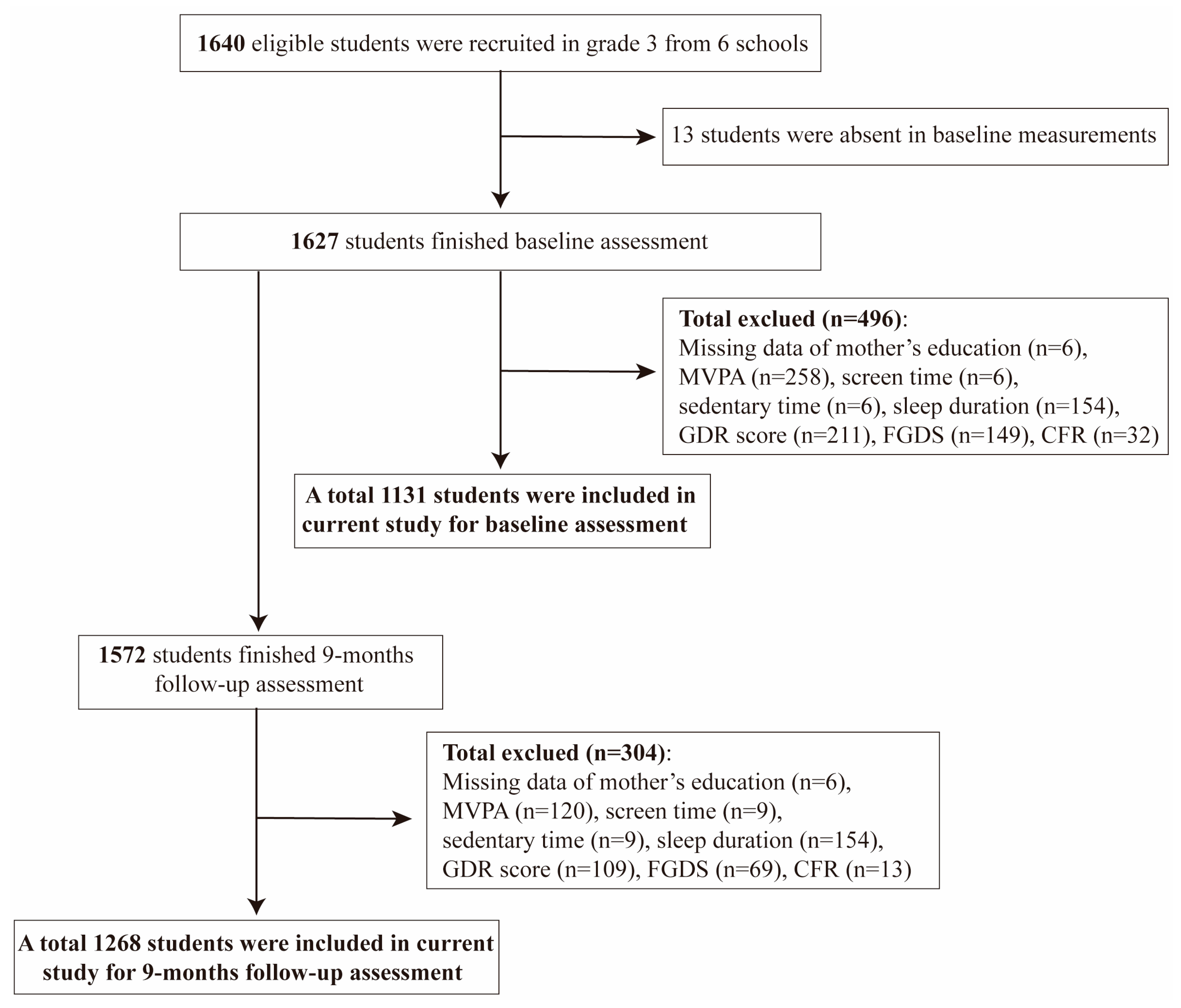
2.1. Study Design and Participants
2.2. Anthropometry and Daily Time Use Measurements
2.3. Physical Fitness and Diet Quality Measurements
2.4. Statistical Analysis
3. Results
3.1. Baseline and 9-Month Follow-Up Characteristics
3.2. Independent and Partition Model Analyses
3.3. Isotemporal Substitution Models
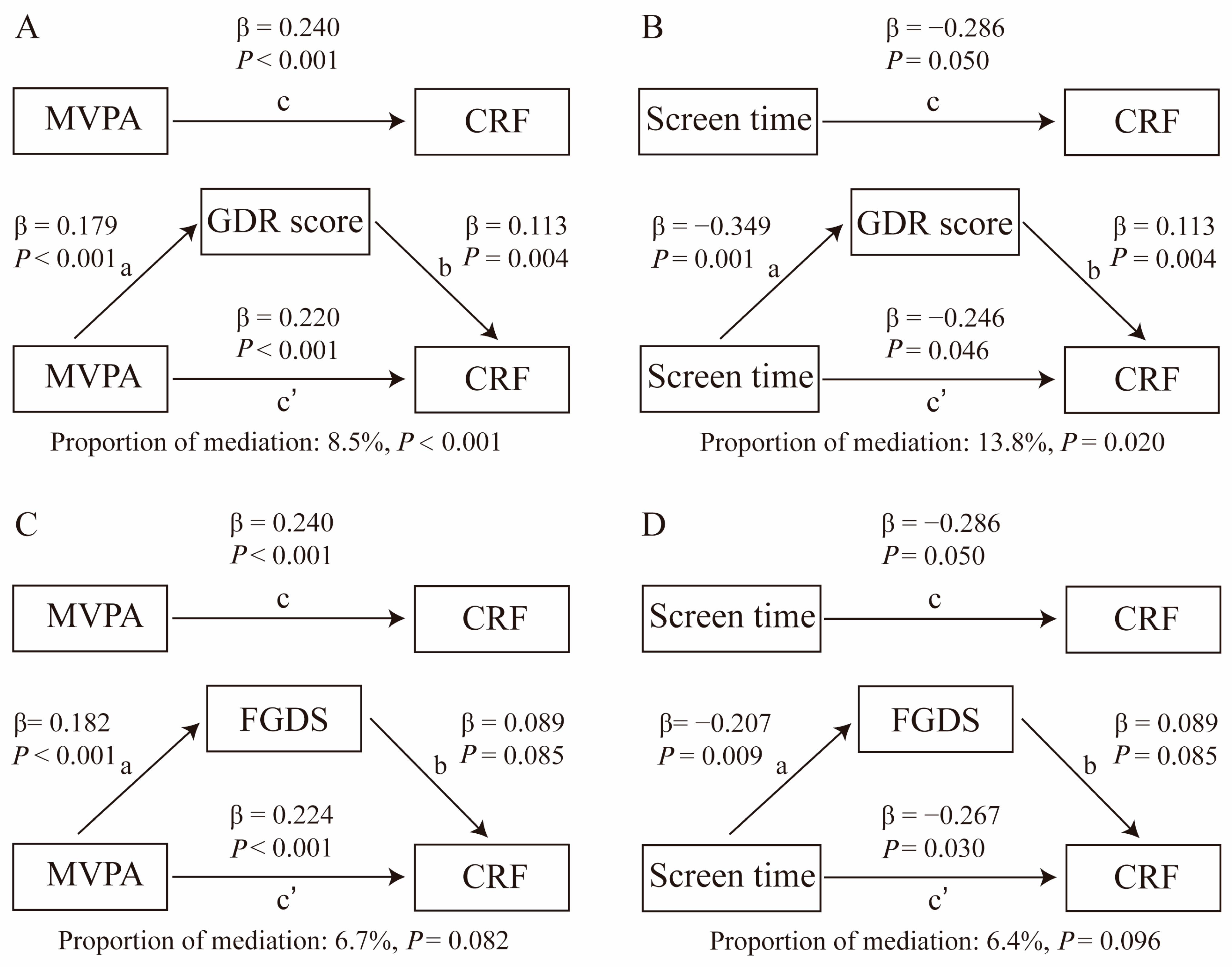
3.4. Mediation Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dumuid, D.; Olds, T.; Sawyer, S.M. Moving beyond more: Towards a healthy balance of daily behaviours. Lancet 2021, 398, 373–374. [Google Scholar] [CrossRef] [PubMed]
- Dumuid, D.; Olds, T.; Lange, K.; Edwards, B.; Lycett, K.; Burgner, D.P.; Simm, P.; Dwyer, T.; Le, H.; Wake, M. Goldilocks Days: Optimising children’s time use for health and well-being. J. Epidemiol. Community Health 2022, 76, 301–308. [Google Scholar] [CrossRef]
- Walmsley, R.; Chan, S.; Smith-Byrne, K.; Ramakrishnan, R.; Woodward, M.; Rahimi, K.; Dwyer, T.; Bennett, D.; Doherty, A. Reallocation of time between device-measured movement behaviours and risk of incident cardiovascular disease. Br. J. Sports Med. 2021, 56, 1008–1017. [Google Scholar] [CrossRef]
- van Sluijs, E.M.F.; Ekelund, U.; Crochemore-Silva, I.; Guthold, R.; Ha, A.; Lubans, D.; Oyeyemi, A.L.; Ding, D.; Katzmarzyk, P.T. Physical activity behaviours in adolescence: Current evidence and opportunities for intervention. Lancet 2021, 398, 429–442. [Google Scholar] [CrossRef] [PubMed]
- Aljahdali, A.A.; Peterson, K.E.; Cantoral, A.; Ruiz-Narvaez, E.; Tellez-Rojo, M.M.; Kim, H.M.; Hébert, J.R.; Wirth, M.D.; Torres-Olascoaga, L.A.; Shivappa, N.; et al. Diet Quality Scores and Cardiometabolic Risk Factors in Mexican Children and Adolescents: A Longitudinal Analysis. Nutrients 2022, 14, 896. [Google Scholar] [CrossRef]
- Marshall, S.; Burrows, T.; Collins, C.E. Systematic review of diet quality indices and their associations with health-related outcomes in children and adolescents. J. Hum. Nutr. Diet. Off. J. Br. Diet. Assoc. 2014, 27, 577–598. [Google Scholar] [CrossRef]
- Yang, W.; Li, S.; Guo, Y.; Bai, Y.; Liu, C. Association between Diet Quality and Health Outcomes among Children in Rural Areas of Northwest China. Int. J. Environ. Res. Public Health 2022, 19, 7803. [Google Scholar] [CrossRef] [PubMed]
- Tomkinson, G.R.; Carver, K.D.; Atkinson, F.; Daniell, N.D.; Lewis, L.K.; Fitzgerald, J.S.; Lang, J.J.; Ortega, F.B. European normative values for physical fitness in children and adolescents aged 9-17 years: Results from 2 779 165 Eurofit performances representing 30 countries. Br. J. Sports Med. 2018, 52, 1445–14563. [Google Scholar] [CrossRef]
- Raghuveer, G.; Hartz, J.; Lubans, D.R.; Takken, T.; Wiltz, J.L.; Mietus-Snyder, M.; Perak, A.M.; Baker-Smith, C.; Pietris, N.; Edwards, N.M. Cardiorespiratory Fitness in Youth: An Important Marker of Health: A Scientific Statement From the American Heart Association. Circulation 2020, 142, e101–e118. [Google Scholar] [CrossRef]
- Alves Donato, A.N.; Waclawovsky, A.J.; Tonello, L.; Firth, J.; Smith, L.; Stubbs, B.; Schuch, F.B.; Boullosa, D. Association between cardiorespiratory fitness and depressive symptoms in children and adolescents: A systematic review and meta-analysis. J. Affect. Disord. 2021, 282, 1234–1240. [Google Scholar] [CrossRef]
- Bawaked, R.A.; Gomez, S.F.; Homs, C.; Casas Esteve, R.; Cardenas, G.; Fíto, M.; Schröder, H. Association of eating behaviors, lifestyle, and maternal education with adherence to the Mediterranean diet in Spanish children. Appetite 2018, 130, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Arriscado, D.; Muros, J.J.; Zabala, M.; Dalmau, J.M. Factors associated with low adherence to a Mediterranean diet in healthy children in northern Spain. Appetite 2014, 80, 28–34. [Google Scholar] [CrossRef]
- Ptomey, L.T.; Montgomery, R.N.; Gorczyca, A.M.; Szabo-Reed, A.N.; Sullivan, D.K.; Hastert, M.; Foster, R.N.S.; Washburn, R.A.; Donnelly, J.E. The impact of exercise and cumulative physical activity on energy intake and diet quality in adults enrolled in the Midwest Exercise Trial for the Prevention of Weight Regain. Br. J. Nutr. 2022, 128, 2498–2509. [Google Scholar] [CrossRef] [PubMed]
- Fang, H.; Quan, M.; Zhou, T.; Sun, S.; Zhang, J.; Zhang, H.; Cao, Z.; Zhao, G.; Wang, R.; Chen, P. Relationship between Physical Activity and Physical Fitness in Preschool Children: A Cross-Sectional Study. BioMed Res. Int. 2017, 2017, 9314026. [Google Scholar] [CrossRef]
- Li, M.; Yin, X.; Li, Y.; Sun, Y.; Zhang, T.; Zhang, F.; Liu, Y.; Guo, Y.; Sun, P. Associations between Sedentary Time and Sedentary Patterns and Cardiorespiratory Fitness in Chinese Children and Adolescents. Children 2022, 9, 1140. [Google Scholar] [CrossRef]
- Vissers, P.A.; Jones, A.P.; van Sluijs, E.M.; Jennings, A.; Welch, A.; Cassidy, A.; Griffin, S.J. Association between diet and physical activity and sedentary behaviours in 9-10-year-old British White children. Public Health 2013, 127, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Cristi-Montero, C.; Chillón, P.; Labayen, I.; Casajus, J.A.; Gonzalez-Gross, M.; Vanhelst, J.; Manios, Y.; Moreno, L.A.; Ortega, F.B.; Ruiz, J.R. Cardiometabolic risk through an integrative classification combining physical activity and sedentary behavior in European adolescents: HELENA study. J. Sport Health Sci. 2019, 8, 55–62. [Google Scholar] [CrossRef]
- Mekary, R.A.; Willett, W.C.; Hu, F.B.; Ding, E.L. Isotem physical activity epidemiology and weight change. Am. J. Epidemiol. 2009, 170, 519–527. [Google Scholar] [CrossRef]
- Sun, Y.; Yin, X.; Li, Y.; Bi, C.; Li, M.; Yang, X.; Zhang, T.; Zhang, F.; Cao, J.; Guo, Y.; et al. Isotemporal substitution of sedentary behavior for physical activity on cardiorespiratory fitness in children and adolescents. Medicine 2020, 99, e21367. [Google Scholar] [CrossRef] [PubMed]
- Santos, D.A.; Marques, A.; Minderico, C.S.; Ekelund, U.; Sardinha, L.B. A cross-sectional and prospective analyse of reallocating sedentary time to physical activity on children’s cardiorespiratory fitness. J. Sports Sci. 2018, 36, 1720–1726. [Google Scholar] [CrossRef]
- Farrahi, V.; Rostami, M.; Nauha, L.; Korpisaari, M.; Niemelä, M.; Jämsä, T.; Korpelainen, R.; Oussalah, M. Replacing sedentary time with physical activity and sleep: Associations with cardiometabolic health markers in adults. Scand. J. Med. Sci. Sports 2023, 33, 907–920. [Google Scholar] [CrossRef]
- Antoniassi, S.G.; Machado, C.O.; Santos, D.S.D.; Santos, L.D.; Höfelmann, D.A. Screen time, quality of the adolescent diet, and profile of the school environment. Cienc. Saude Coletiva 2024, 29, e00022023. [Google Scholar] [CrossRef]
- Rivera-Ochoa, M.; López-Gil, J.F.; Brazo-Sayavera, J.; Pantoja-Arévalo, L.; González-Gross, M.; Vizmanos-Lamotte, B.; Guadalupe-Grau, A. Clustering Health Behaviors in Mexican Adolescents: The HELENA-MEX Study. Res. Q. Exerc. Sport 2024, 95, 281–288. [Google Scholar] [CrossRef] [PubMed]
- Seong, M.; Kim, Y.; Park, S.; Kim, H.; Kwon, O. Association Between Diet Quality and Cardiorespiratory Fitness in Korean Adults: The 2014-2015 National Fitness Award Project. Nutrients 2020, 12, 3226. [Google Scholar] [CrossRef]
- Payandeh, N.; Shahinfar, H.; Jafari, A.; Babaei, N.; Djafarian, K.; Shab-Bidar, S. Mediterranean diet quality index is associated with better cardiorespiratory fitness and reduced systolic blood pressure in adults: A cross-sectional study. Clin. Nutr. ESPEN 2021, 46, 200–205. [Google Scholar] [CrossRef]
- Martinez-Avila, W.D.; Sanchez-Delgado, G.; Acosta, F.M.; Jurado-Fasoli, L.; Oustric, P.; Labayen, I.; Blundell, J.E.; Ruiz, J.R. Eating Behavior, Physical Activity and Exercise Training: A Randomized Controlled Trial in Young Healthy Adults. Nutrients 2020, 12, 3685. [Google Scholar] [CrossRef]
- Yan, H.; Zhang, R.; Oniffrey, T.M.; Chen, G.; Wang, Y.; Wu, Y.; Zhang, X.; Wang, Q.; Ma, L.; Li, R.; et al. Associations among Screen Time and Unhealthy Behaviors, Academic Performance, and Well-Being in Chinese Adolescents. Int. J. Environ. Res. Public Health 2017, 14, 596. [Google Scholar] [CrossRef]
- Zhang, P.P.; Wang, Y.X.; Shen, F.J.; Xing, Y.F.; Gu, J.Y.; Li, X.Y.; Jin, H.; Jin, S.F.; Xu, M.; Wang, H.J.; et al. Lifestyle intervention in children with obesity and nonalcoholic fatty liver disease (NAFLD): Study protocol for a randomized controlled trial in Ningbo city (the SCIENT study). Trials 2024, 25, 196. [Google Scholar] [CrossRef]
- Xing, Y.; Zhang, P.; Li, X.; Jin, S.; Xu, M.; Jia, J.; Wang, H.J.; Li, L.; Wang, H. New predictive models and indices for screening MAFLD in school-aged overweight/obese children. Eur. J. Pediatr. 2023, 182, 5025–5036. [Google Scholar] [CrossRef]
- Liu, Z.; Gao, P.; Gao, A.Y.; Lin, Y.; Feng, X.X.; Zhang, F.; Xu, L.Q.; Niu, W.Y.; Fang, H.; Zhou, S.; et al. Effectiveness of a Multifaceted Intervention for Prevention of Obesity in Primary School Children in China: A Cluster Randomized Clinical Trial. JAMA Pediatr. 2022, 176, e214375. [Google Scholar] [CrossRef]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.; Herforth, A.W.; Vogliano, C.; Zou, Z. Most Commonly-Consumed Food Items by Food Group, and by Province, in China: Implications for Diet Quality Monitoring. Nutrients 2022, 14, 1754. [Google Scholar] [CrossRef]
- Zhou, J.; Wang, H.; Zou, Z. Inverse Association between Dietary Diversity Score Calculated from the Diet Quality Questionnaire and Psychological Stress in Chinese Adults: A Prospective Study from China Health and Nutrition Survey. Nutrients 2022, 14, 3297. [Google Scholar] [CrossRef]
- Wang, H.; Herforth, A.W.; Xi, B.; Zou, Z. Validation of the Diet Quality Questionnaire in Chinese Children and Adolescents and Relationship with Pediatric Overweight and Obesity. Nutrients 2022, 14, 3551. [Google Scholar] [CrossRef] [PubMed]
- Gao, D.; Wang, H.; Wang, Y.; Ma, S.; Zou, Z. Association between Diet Quality and Stroke among Chinese Adults: Results from China Health and Nutrition Survey 2011. Nutrients 2023, 15, 3229. [Google Scholar] [CrossRef]
- Lang, J.J.; Belanger, K.; Poitras, V.; Janssen, I.; Tomkinson, G.R.; Tremblay, M.S. Systematic review of the relationship between 20m shuttle run performance and health indicators among children and youth. J. Sci. Med. Sport 2018, 21, 383–397. [Google Scholar] [CrossRef]
- Tomkinson, G.R.; Lang, J.J.; Blanchard, J.; Léger, L.A.; Tremblay, M.S. The 20-m Shuttle Run: Assessment and Interpretation of Data in Relation to Youth Aerobic Fitness and Health. Pediatr. Exerc. Sci. 2019, 31, 152–163. [Google Scholar] [CrossRef]
- Léger, L.A.; Mercier, D.; Gadoury, C.; Lambert, J. The multistage 20 metre shuttle run test for aerobic fitness. J. Sports Sci. 1988, 6, 93–101. [Google Scholar] [CrossRef]
- Han, M.; Fang, J.; Zhang, Y.; Song, X.; Jin, L.; Ma, Y. Associations of sleeping, sedentary and physical activity with phenotypic age acceleration: A cross-sectional isotemporal substitution model. BMC Geriatr. 2023, 23, 165. [Google Scholar] [CrossRef]
- Baron, R.M.; Kenny, D.A. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Personal. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Volpato, L.A.; Costa, J.C.; Lopes, W.A.; Sasaki, J.E.; Romanzini, C.L.P.; Ronque, E.R.V.; Romanzini, M. Time Reallocations From Sedentary Behavior to Physical Activity and Cardiovascular Risk Factors in Children and Adolescents: A Systematic Review. J. Phys. Act. Health 2023, 20, 1084–1091. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Trautwein, E.A.; McKay, S. The Role of Specific Components of a Plant-Based Diet in Management of Dyslipidemia and the Impact on Cardiovascular Risk. Nutrients 2020, 12, 2671. [Google Scholar] [CrossRef]
- Mutalifu, M.; Zhao, Q.; Wang, Y.; Hamulati, X.; Wang, Y.S.; Deng, L.; Adili, N.; Liu, F.; Yang, Y.N.; Li, X.M. Joint association of physical activity and diet quality with dyslipidemia: A cross-sectional study in Western China. Lipids Health Dis. 2024, 23, 46. [Google Scholar] [CrossRef] [PubMed]
- Stiglic, N.; Viner, R.M. Effects of screentime on the health and well-being of children and adolescents: A systematic review of reviews. BMJ Open 2019, 9, e023191. [Google Scholar] [CrossRef]
- Sina, E.; Boakye, D.; Christianson, L.; Ahrens, W.; Hebestreit, A. Social Media and Children’s and Adolescents’ Diets: A Systematic Review of the Underlying Social and Physiological Mechanisms. Adv. Nutr. 2022, 13, 913–937. [Google Scholar] [CrossRef]
- Börnhorst, C.; Pigeot, I.; De Henauw, S.; Formisano, A.; Lissner, L.; Molnár, D.; Moreno, L.A.; Tornaritis, M.; Veidebaum, T.; Vrijkotte, T.; et al. The effects of hypothetical behavioral interventions on the 13-year incidence of overweight/obesity in children and adolescents. Int. J. Behav. Nutr. Phys. Act. 2023, 20, 100. [Google Scholar] [CrossRef] [PubMed]
- Petersen, K.S.; Kris-Etherton, P.M. Diet Quality Assessment and the Relationship between Diet Quality and Cardiovascular Disease Risk. Nutrients 2021, 13, 4305. [Google Scholar] [CrossRef]
- Satija, A.; Hu, F.B. Plant-based diets and cardiovascular health. Trends Cardiovasc. Med. 2018, 28, 437–441. [Google Scholar] [CrossRef]
- Mul, J.D.; Stanford, K.I.; Hirshman, M.F.; Goodyear, L.J. Exercise and Regulation of Carbohydrate Metabolism. Prog. Mol. Biol. Transl. Sci. 2015, 135, 17–37. [Google Scholar] [CrossRef] [PubMed]
- Jornayvaz, F.R.; Shulman, G.I. Regulation of mitochondrial biogenesis. Essays Biochem. 2010, 47, 69–84. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Rhodes, E.C. Oxygen uptake kinetics during exercise. Sports Med. 1999, 27, 313–327. [Google Scholar] [CrossRef]
- Belanger, M.J.; Rao, P.; Robbins, J.M. Exercise, Physical Activity, and Cardiometabolic Health: Pathophysiologic Insights. Cardiol. Rev. 2022, 30, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Iddir, M.; Brito, A.; Dingeo, G.; Fernandez Del Campo, S.S.; Samouda, H.; La Frano, M.R.; Bohn, T. Strengthening the Immune System and Reducing Inflammation and Oxidative Stress through Diet and Nutrition: Considerations during the COVID-19 Crisis. Nutrients 2020, 12, 1562. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, A.; Meir, A.Y.; Hagemann, T.; Czechowski, P.; Müller, L.; Engelmann, B.; Haange, S.B.; Rolle-Kampczyk, U.; Tsaban, G.; Zelicha, H.; et al. A polyphenol-rich green Mediterranean diet enhances epigenetic regulatory potential: The direct plus randomized controlled trial. Metab. Clin. Exp. 2023, 145, 155594. [Google Scholar] [CrossRef] [PubMed]
- Mason, S.A.; Trewin, A.J.; Parker, L.; Wadley, G.D. Antioxidant supplements and endurance exercise: Current evidence and mechanistic insights. Redox Biol. 2020, 35, 101471. [Google Scholar] [CrossRef]
- Hearon, C.M., Jr.; Dias, K.A.; MacNamara, J.P.; Hieda, M.; Mantha, Y.; Harada, R.; Samels, M.; Morris, M.; Szczepaniak, L.S.; Levine, B.D.; et al. 1 Year HIIT and Omega-3 Fatty Acids to Improve Cardiometabolic Risk in Stage-A Heart Failure. JACC. Heart Fail. 2022, 10, 238–249. [Google Scholar] [CrossRef]

| Variable | Baseline Sample (n = 1131) | Follow-Up Sample (n = 1268) |
|---|---|---|
| Sex, n (%) | ||
| Boys | 600 (53.1%) | 638 (50.3%) |
| Girls | 531 (46.9%) | 630 (49.7%) |
| Mother’s education, n (%) | ||
| Under high school | 325 (28.7%) | 356 (27.9%) |
| High school or above | 806 (71.3%) | 923 (72.1%) |
| Weight, kg | 28.0 (24.8, 31.8) | 29.9 (26.7, 34.5) |
| Height, cm | 132.0 (128.3, 136.0) | 136.5 (132.5, 140.4) |
| BMI, kg/m2 | 15.8 (14.7, 17.7) | 15.9 (14.8, 18.0) |
| Age, years | 8.5 (8.3, 8.8) | 9.3 (9.0, 9.5) |
| Daily behavior time | ||
| MVPA time, h/day | 1.04 (0.46, 1.83) | 1.31 (0.71, 2.18) |
| Sedentary time, h/day | 2.83 (2.00, 3.71) | 3.07 (2.19, 3.93) |
| Screen time, h/day | 0.43 (0.17, 0.86) | 0.48 (0.21, 0.79) |
| Sleep time, h/day | 9.93 (9.47, 10.33) | 10.04 (9.57, 10.48) |
| GDR score | 11.0 (9.0, 13.0) | 11.0 (9.0, 13.0) |
| FGDS | 6.0 (4.0, 7.0) | 6.0 (5.0, 7.0) |
| CRF, mL/kg/min | 47.5 (46.0, 50.8) | 48.3 (46.0, 51.8) |
| Outcomes | Daily Behavior Time | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|---|
| β (95% CI) | p | β (95% CI) | p | β (95% CI) | p | ||
| GDR score | Baseline | ||||||
| MVPA time | 0.11 (−0.01~0.23) | 0.080 | 0.13 (0.01~0.25) | 0.041 | 0.13 (0.01~0.25) | 0.037 | |
| Screen time | −0.09 (−0.22~0.05) | 0.220 | −0.06 (−0.20~0.08) | 0.363 | −0.09 (−0.24~0.06) | 0.257 | |
| Sedentary time | −0.001 (−0.06~0.06) | 0.966 | 0.002 (−0.06~0.06) | 0.938 | 0.02 (−0.05~0.08) | 0.675 | |
| Sleep time | −0.04 (−0.20~0.13) | 0.668 | −0.04 (−0.20~0.12) | 0.656 | −0.04 (−0.20~0.12) | 0.599 | |
| Follow-up | |||||||
| MVPA time | 0.15 (0.05~0.23) | 0.002 | 0.18 (0.09~0.26) | <0.001 | 0.18 (0.09~0.27) | <0.001 | |
| Screen time | −0.41 (−0.60~−0.22) | <0.001 | −0.32 (−0.51~−0.12) | 0.002 | −0.35 (−0.55~−0.15) | 0.001 | |
| Sedentary time | 0.00 (−0.07~0.08) | 0.908 | 0.01 (−0.07~0.08) | 0.945 | 0.04 (−0.03~0.12) | 0.268 | |
| Sleep time | −0.04 (−0.18~0.10) | 0.603 | −0.07 (−0.21~0.07) | 0.311 | −0.07 (−0.21~0.07) | 0.343 | |
| FGDS | Baseline | ||||||
| MVPA time | 0.15 (0.06~0.25) | 0.002 | 0.18 (0.08~0.27) | <0.001 | 0.18 (0.08~0.28) | <0.001 | |
| Screen time | −0.07 (−0.18~0.04) | 0.196 | −0.01 (−0.12~0.10) | 0.803 | −0.004 (−0.13~0.12) | 0.946 | |
| Sedentary time | −0.03 (−0.08~0.02) | 0.191 | −0.02 (−0.07~0.03) | 0.438 | −0.02 (−0.08~0.03) | 0.383 | |
| Sleep time | −0.02 (−0.15~0.11) | 0.782 | 0.01 (−0.12~0.14) | 0.882 | 0.01 (−0.11~0.14) | 0.856 | |
| Follow-up | |||||||
| MVPA time | 0.16 (0.09~0.23) | <0.001 | 0.18 (0.12~0.25) | <0.001 | 0.18 (0.12~0.25) | <0.001 | |
| Screen time | −0.33 (−0.48~−0.18) | <0.001 | −0.19 (−0.35~−0.04) | 0.017 | −0.21 (−0.36~−0.05) | 0.013 | |
| Sedentary time | −0.02 (−0.08~0.03) | 0.421 | −0.01 (−0.06~0.05) | 0.788 | 0.01 (−0.04~0.07) | 0.637 | |
| Sleep time | 0.01 (−0.10~0.11) | 0.927 | −0.05 (−0.16~0.06) | 0.359 | −0.05 (−0.15~0.06) | 0.384 | |
| CRF | Baseline | ||||||
| MVPA time | 0.40 (0.23~0.58) | <0.001 | 0.45 (0.28~0.61) | <0.001 | 0.45 (0.28~0.62) | <0.001 | |
| Screen time | −0.24 (−0.43~−0.04) | 0.018 | −0.14 (−0.33~0.05) | 0.157 | −0.30 (−0.50~−0.09) | 0.006 | |
| Sedentary time | 0.09 (0.00~0.18) | 0.047 | 0.09 (0.00~0.18) | 0.040 | 0.14 (0.04~0.23) | 0.006 | |
| Sleep time | −0.09 (−0.32~0.14) | 0.424 | −0.03 (−0.25~0.19) | 0.784 | −0.04 (−0.25~0.18) | 0.745 | |
| Follow-up | |||||||
| MVPA time | 0.21 (0.08~0.34) | 0.002 | 0.24 (0.12~0.36) | <0.001 | 0.24 (0.12~0.36) | <0.001 | |
| Screen time | −0.41 (−0.69~−0.12) | 0.005 | −0.20 (−0.48~0.08) | 0.153 | −0.29 (−0.57~0.00) | 0.050 | |
| Sedentary time | 0.05 (−0.06~0.16) | 0.357 | 0.08 (−0.02~0.18) | 0.129 | 0.11 (0.01~0.22) | 0.042 | |
| Sleep time | 0.18 (−0.03~0.38) | 0.097 | 0.12 (−0.08~0.31) | 0.241 | 0.12 (−0.07~0.32) | 0.217 |
| Add 30 min/day | Remove 30 min/day | Baseline | Follow-Up | ||
|---|---|---|---|---|---|
| β (95% CI) | p | β (95% CI) | p | ||
| GDR score | |||||
| MVPA time | Screen time | 0.11 (0.02~0.21) | 0.024 | 0.26 (0.15~0.38) | <0.001 |
| Sedentary time | Screen time | 0.06 (−0.04~0.15) | 0.227 | 0.20 (0.08~0.31) | 0.001 |
| Sleep time | Screen time | 0.03 (−0.08~0.14) | 0.631 | 0.14 (0.02~0.26) | 0.026 |
| MVPA time | Sedentary time | 0.06 (−0.01~0.13) | 0.117 | 0.07 (0.01~0.12) | 0.020 |
| FGDS | |||||
| MVPA time | Screen time | 0.11 (0.03~0.19) | 0.006 | 0.19 (0.11~0.28) | <0.001 |
| Sedentary time | Screen time | 0.01 (−0.06~0.09) | 0.756 | 0.11 (0.02~0.20) | 0.017 |
| Sleep time | Screen time | 0.02 (−0.06~0.11) | 0.626 | 0.08 (−0.01~0.17) | 0.099 |
| MVPA time | Sedentary time | 0.10 (0.05~0.16) | <0.001 | 0.08 (0.04~0.13) | <0.001 |
| CRF | |||||
| MVPA time | Screen time | 0.40 (0.26~0.53) | <0.001 | 0.26 (0.11~0.42) | 0.001 |
| Sedentary time | Screen time | 0.24 (0.12~0.37) | <0.001 | 0.20 (0.03~0.36) | 0.019 |
| Sleep time | Screen time | 0.15 (0.00~0.30) | 0.052 | 0.20 (0.03~0.38) | 0.021 |
| MVPA time | Sedentary time | 0.16 (0.06~0.25) | 0.002 | 0.07 (−0.02~0.15) | 0.114 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Zhang, P.; Wang, M.; Gong, Q.; Yu, C.; Wang, H.; Hebestreit, A.; Lau, P.W.C.; Wang, H.; Li, L. Isotemporal Substitution Effects of Daily Time Use on Cardiorespiratory Fitness of Children in the OptiChild Study: A Mediation Analysis with Diet Quality. Nutrients 2024, 16, 2788. https://doi.org/10.3390/nu16162788
Wang Y, Zhang P, Wang M, Gong Q, Yu C, Wang H, Hebestreit A, Lau PWC, Wang H, Li L. Isotemporal Substitution Effects of Daily Time Use on Cardiorespiratory Fitness of Children in the OptiChild Study: A Mediation Analysis with Diet Quality. Nutrients. 2024; 16(16):2788. https://doi.org/10.3390/nu16162788
Chicago/Turabian StyleWang, Youxin, Pingping Zhang, Mingyue Wang, Qinghai Gong, Canqing Yu, Haijun Wang, Antje Hebestreit, Patrick W. C. Lau, Hui Wang, and Li Li. 2024. "Isotemporal Substitution Effects of Daily Time Use on Cardiorespiratory Fitness of Children in the OptiChild Study: A Mediation Analysis with Diet Quality" Nutrients 16, no. 16: 2788. https://doi.org/10.3390/nu16162788
APA StyleWang, Y., Zhang, P., Wang, M., Gong, Q., Yu, C., Wang, H., Hebestreit, A., Lau, P. W. C., Wang, H., & Li, L. (2024). Isotemporal Substitution Effects of Daily Time Use on Cardiorespiratory Fitness of Children in the OptiChild Study: A Mediation Analysis with Diet Quality. Nutrients, 16(16), 2788. https://doi.org/10.3390/nu16162788








