Dietary Flavonoids: Mitigating Air Pollution’s Cardiovascular Risks
Abstract
1. Introduction
2. Methods
2.1. Study Selection
2.2. Data Extraction and Synthesis
3. Results
3.1. Literature Retrieval Process and Basic Study Characteristics
3.2. Studies on the Impact of Air Pollution on Cardiovascular Health
3.3. Studies on the Cardiovascular Benefits of Dietary Flavonoids
3.4. Impact of Air Pollution on Cardiovascular Health
- General cardiovascular outcomes
- Specific cardiovascular conditions
- Increased risk and mortality of CVD patients
3.5. Cardiovascular Effects of Flavonoids
- Reduction in cardiovascular disease risk and mortality
- Effects on specific cardiovascular conditions
3.6. Mechanisms of Action and Evidence
- Endothelial function and vascular health
- Antioxidant effects
- Anti-inflammatory effects
- Blood pressure regulation
- Antiplatelet and antithrombotic effects
- Cardioprotective effects
- Lipid metabolism
- Glucose and insulin metabolism
4. Discussion
4.1. Air Pollution and Cardiovascular Risks
4.2. Cardiovascular Benefits of Dietary Flavonoids
4.3. Potential Interactions between Flavonoid Intake and Air Pollution Exposure
4.3.1. Improvement in Endothelial Function Impaired by Pollutants
4.3.2. Antioxidant Effects
4.3.3. Anti-Inflammatory Actions
4.3.4. Blood Pressure Regulation to Offset the Hypertensive Effects of Pollution
4.3.5. Antiplatelet and Antithrombotic Effects Mitigating Pollution-Induced Thrombosis Risk
4.4. Public Health Implications
4.5. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Rajagopalan, S.; Landrigan, P.J. Pollution and the Heart. N. Engl. J. Med. 2021, 385, 1881–1892. [Google Scholar] [CrossRef] [PubMed]
- Shaddick, G.; Thomas, M.L.; Mudu, P.; Ruggeri, G.; Gumy, S. Half the World’s Population Are Exposed to Increasing Air Pollution. npj Clim. Atmos. Sci. 2020, 3, 23. [Google Scholar] [CrossRef]
- Hamanaka, R.B.; Mutlu, G.M. Particulate Matter Air Pollution: Effects on the Cardiovascular System. Front. Endocrinol. 2018, 9, 680. [Google Scholar] [CrossRef] [PubMed]
- Chin, M.T. Basic Mechanisms for Adverse Cardiovascular Events Associated with Air Pollution. Heart 2015, 101, 253–256. [Google Scholar] [CrossRef] [PubMed]
- Newby, D.E.; Mannucci, P.M.; Tell, G.S.; Baccarelli, A.A.; Brook, R.D.; Donaldson, K.; Forastiere, F.; Franchini, M.; Franco, O.H.; Graham, I.; et al. Expert Position Paper on Air Pollution and Cardiovascular Disease. Eur. Heart J. 2015, 36, 83–93. [Google Scholar] [CrossRef] [PubMed]
- Brook, R.D.; Rajagopalan, S.; Pope, C.A.; Brook, J.R.; Bhatnagar, A.; Diez-Roux, A.V.; Holguin, F.; Hong, Y.; Luepker, R.V.; Mittleman, M.A.; et al. Particulate Matter Air Pollution and Cardiovascular Disease. Circulation 2010, 121. [Google Scholar] [CrossRef]
- Lee, F.Y.; Chen, W.K.; Lin, C.L.; Kao, C.H. Carbon Monoxide Poisoning and Subsequent Cardiovascular Disease Risk: A Nationwide Population-Based Cohort Study. Medicine 2015, 94, e624. [Google Scholar] [CrossRef]
- Caldeira, D.; Franco, F.; Bravo Baptista, S.; Cabral, S.; do Carmo Cachulo, M.; Dores, H.; Peixeiro, A.; Rodrigues, R.; Santos, M.; Timóteo, A.T.; et al. Air Pollution and Cardiovascular Diseases: A Position Paper. Rev. Port. Cardiol. 2022, 41, 709–717. [Google Scholar] [CrossRef]
- Milojevic, A.; Wilkinson, P.; Armstrong, B.; Bhaskaran, K.; Smeeth, L.; Hajat, S. Short-Term Effects of Air Pollution on a Range of Cardiovascular Events in England and Wales: Case-Crossover Analysis of the MINAP Database, Hospital Admissions and Mortality. Heart 2014, 100, 1093–1098. [Google Scholar] [CrossRef]
- Palacio, L.C.; Pachajoa, D.C.; Echeverri-Londoño, C.A.; Saiz, J.; Tobón, C. Air Pollution and Cardiac Diseases: A Review of Experimental Studies. Dose Response 2023, 21. [Google Scholar] [CrossRef]
- Yang, B.Y.; Qian, Z.; Howard, S.W.; Vaughn, M.G.; Fan, S.J.; Liu, K.K.; Dong, G.H. Global Association between Ambient Air Pollution and Blood Pressure: A Systematic Review and Meta-Analysis. Environ. Pollut. 2018, 235, 576–588. [Google Scholar] [CrossRef] [PubMed]
- Liang, R.; Chen, R.; Yin, P.; van Donkelaar, A.; Martin, R.V.; Burnett, R.; Cohen, A.J.; Brauer, M.; Liu, C.; Wang, W.; et al. Associations of Long-Term Exposure to Fine Particulate Matter and Its Constituents with Cardiovascular Mortality: A Prospective Cohort Study in China. Environ. Int. 2022, 162, 107156. [Google Scholar] [CrossRef] [PubMed]
- Dominici, F.; Zanobetti, A.; Schwartz, J.; Braun, D.; Sabath, B.; Wu, X. Assessing Adverse Health Effects of Long-Term Exposure to Low Levels of Ambient Air Pollution: Implementation of Causal Inference Methods. Res. Rep. Health Eff. Inst. 2022, 2022, 1–56. [Google Scholar] [PubMed]
- Bhatnagar, A. Cardiovascular Effects of Particulate Air Pollution. Annu. Rev. Med. 2022, 73, 393–406. [Google Scholar] [CrossRef] [PubMed]
- Rao, X.; Zhong, J.; Brook, R.D.; Rajagopalan, S. Effect of Particulate Matter Air Pollution on Cardiovascular Oxidative Stress Pathways. Antioxid. Redox Signal. 2018, 28, 797–818. [Google Scholar] [CrossRef] [PubMed]
- Steven, S.; Frenis, K.; Oelze, M.; Kalinovic, S.; Kuntic, M.; Jimenez, M.T.B.; Vujacic-Mirski, K.; Helmstädter, J.; Kröller-Schön, S.; Münzel, T.; et al. Vascular Inflammation and Oxidative Stress: Major Triggers for Cardiovascular Disease. Oxid. Med. Cell Longev. 2019, 2019, 7092151. [Google Scholar] [CrossRef]
- Miller, M.R.; Shaw, C.A.; Langrish, J.P. From Particles to Patients: Oxidative Stress and the Cardiovascular Effects of Air Pollution. Future Cardiol. 2012, 8, 577–602. [Google Scholar] [CrossRef]
- Pope, C.A.; Bhatnagar, A.; McCracken, J.P.; Abplanalp, W.; Conklin, D.J.; O’Toole, T. Exposure to Fine Particulate Air Pollution Is Associated with Endothelial Injury and Systemic Inflammation. Circ. Res. 2016, 119, 1204. [Google Scholar] [CrossRef]
- Ain, N.U.; Qamar, S.U.R. Particulate Matter-Induced Cardiovascular Dysfunction: A Mechanistic Insight. Cardiovasc. Toxicol. 2021, 21, 505–516. [Google Scholar] [CrossRef]
- Tian, M.; Zhao, J.; Mi, X.; Wang, K.; Kong, D.; Mao, H.; Wang, T. Progress in Research on Effect of PM2.5 on Occurrence and Development of Atherosclerosis. J. Appl. Toxicol. 2021, 41, 668–682. [Google Scholar] [CrossRef]
- Rajagopalan, S.; Al-Kindi, S.G.; Brook, R.D. Air Pollution and Cardiovascular Disease: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2018, 72, 2054–2070. [Google Scholar] [CrossRef] [PubMed]
- Blaustein, J.R.; Quisel, M.J.; Hamburg, N.M.; Wittkopp, S. Environmental Impacts on Cardiovascular Health and Biology: An Overview. Circ. Res. 2024, 134, 1048–1060. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Qian, Z.M.; Chen, L.; Zhao, X.; Cai, M.; Wang, C.; Zou, H.; Wu, Y.; Zhang, Z.; Li, H.; et al. Exposure to Air Pollution during Pre-Hypertension and Subsequent Hypertension, Cardiovascular Disease, and Death: A Trajectory Analysis of the UK Biobank Cohort. Environ. Health Perspect. 2023, 131, 17008. [Google Scholar] [CrossRef] [PubMed]
- Hayes, R.B.; Lim, C.; Zhang, Y.; Cromar, K.; Shao, Y.; Reynolds, H.R.; Silverman, D.T.; Jones, R.R.; Park, Y.; Jerrett, M.; et al. PM2.5 Air Pollution and Cause-Specific Cardiovascular Disease Mortality. Int. J. Epidemiol. 2020, 49, 25–35. [Google Scholar] [CrossRef] [PubMed]
- Leong, D.P.; Joseph, P.G.; McKee, M.; Anand, S.S.; Teo, K.K.; Schwalm, J.D.; Yusuf, S. Reducing the Global Burden of Cardiovascular Disease, Part 2: Prevention and Treatment of Cardiovascular Disease. Circ. Res. 2017, 121, 695–710. [Google Scholar] [CrossRef]
- Kim, J.B.; Prunicki, M.; Haddad, F.; Dant, C.; Sampath, V.; Patel, R.; Smith, E.; Akdis, C.; Balmes, J.; Snyder, M.P.; et al. Cumulative Lifetime Burden of Cardiovascular Disease from Early Exposure to Air Pollution. J. Am. Heart Assoc. 2020, 9, e014944. [Google Scholar] [CrossRef]
- Mead, M.N. Who’s at Risk? Gauging Susceptibility to Air Pollutants. Environ. Health Perspect. 2011, 119, A176. [Google Scholar] [CrossRef]
- Parmenter, B.H.; Croft, K.D.; Hodgson, J.M.; Dalgaard, F.; Bondonno, C.P.; Lewis, J.R.; Cassidy, A.; Scalbert, A.; Bondonno, N.P. An Overview and Update on the Epidemiology of Flavonoid Intake and Cardiovascular Disease Risk. Food Funct. 2020, 11, 6777–6806. [Google Scholar] [CrossRef]
- Hollman, P.C. Absorption, bioavailability, and metabolism of flavonoids. Pharm. Biol. 2004, 42, 74–83. [Google Scholar] [CrossRef]
- Manach, C.; Scalbert, A.; Morand, C.; Rémésy, C.; Jiménez, L. Polyphenols: Food sources and bioavailability. Am. J. Clin. Nutr. 2004, 79, 727–747. [Google Scholar] [CrossRef] [PubMed]
- Manach, C.; Williamson, G.; Morand, C.; Scalbert, A.; Rémésy, C. Bioavailability and bioefficacy of polyphenols in humans. I. Review of 97 bioavailability studies. Am. J. Clin. Nutr. 2005, 81, 230S–242S. [Google Scholar] [CrossRef] [PubMed]
- Williamson, G.; Manach, C. Bioavailability and bioefficacy of polyphenols in humans. II. Review of 93 intervention studies. Am. J. Clin. Nutr. 2005, 81, 243S–255S. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Zhao, Y.; Yuan, L.; Zhang, D.; Feng, Y.; Hu, H.; Hu, D.; Liu, J. Total dietary flavonoid intake and risk of cardiometabolic diseases: A dose-response meta-analysis of prospective cohort studies. Crit. Rev. Food Sci. Nutr. 2024, 64, 2760–2772. [Google Scholar] [CrossRef]
- Panche, A.N.; Diwan, A.D.; Chandra, S.R. Flavonoids: An Overview. J. Nutr. Sci. 2016, 5, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Kozłowska, A.; Szostak-Wegierek, D. Flavonoids--Food Sources and Health Benefits. Rocz. Panstw. Zakl. Hig. 2014, 65, 79–85. [Google Scholar]
- Escobar-Cévoli, R.; Castro-Espín, C.; Béraud, V.; Buckland, G.; Zamora-Ros, R.; Escobar-Cévoli, R.; Castro-Espín, C.; Béraud, V.; Buckland, G.; Zamora-Ros, R. An Overview of Global Flavonoid Intake and Its Food Sources. In Flavonoids—From Biosynthesis to Human Health; IntechOpen: London, UK, 2017. [Google Scholar] [CrossRef]
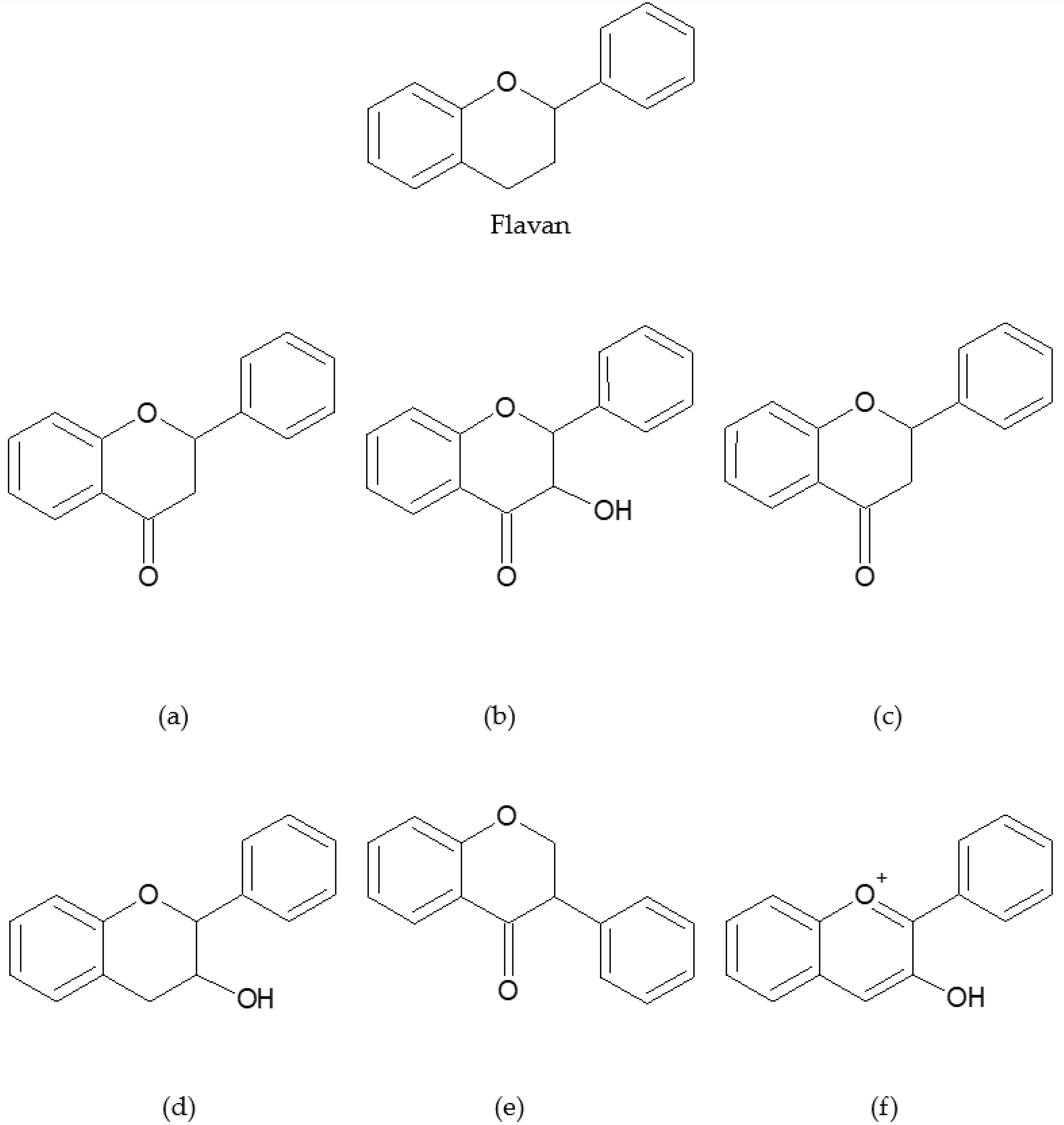
- de Souza Farias, S.A.; da Costa, K.S.; Martins, J.B. Analysis of conformational, structural, magnetic, and electronic properties related to antioxidant activity: Revisiting flavan, anthocyanidin, flavanone, flavonol, isoflavone, flavone, and flavan-3-ol. ACS Omega 2021, 6, 8908–8918. [Google Scholar] [CrossRef] [PubMed]
- Feliciano, R.P.; Pritzel, S.; Heiss, C.; Rodriguez-Mateos, A. Flavonoid Intake and Cardiovascular Disease Risk. Curr. Opin. Food Sci. 2015, 2, 92–99. [Google Scholar] [CrossRef]
- Sebastian, R.S.; Goldman, J.D.; Moshfegh, A.J. Dietary Intake and Sources of Flavonoids by Adults in the US; FSRG Dietary Data Briefs [Internet]; United States Department of Agriculture (USDA): Washington, DC, USA, 2023. [Google Scholar]
- Beecher, G.R. Overview of dietary flavonoids: Nomenclature, occurrence and intake. J. Nutr. 2003, 133, 3248S–3254S. [Google Scholar] [CrossRef]
- Maleki, S.J.; Crespo, J.F.; Cabanillas, B. Anti-Inflammatory Effects of Flavonoids. Food Chem. 2019, 299, 125124. [Google Scholar] [CrossRef]
- Grassi, D.; Desideri, G.; Ferri, C. Flavonoids: Antioxidants against Atherosclerosis. Nutrients 2010, 2, 890–902. [Google Scholar] [CrossRef]
- Ullah, A.; Munir, S.; Badshah, S.L.; Khan, N.; Ghani, L.; Poulson, B.G.; Emwas, A.H.; Jaremko, M. Important Flavonoids and Their Role as a Therapeutic Agent. Molecules 2020, 25, 5243. [Google Scholar] [CrossRef]
- Murphy, K.J.; Walker, K.M.; Dyer, K.A.; Bryan, J. Estimation of daily intake of flavonoids and major food sources in middle-aged Australian men and women. Nutr. Res. 2019, 61, 64–81. [Google Scholar] [CrossRef]
- Vieux, F.; Maillot, M.; Rehm, C.D.; Drewnowski, A. Flavonoid intakes in the US diet are linked to higher socioeconomic status and to tea consumption: Analyses of NHANES 2011–16 data. J. Nutr. 2020, 150, 2147–2155. [Google Scholar] [CrossRef] [PubMed]
- Zamora-Ros, R.; Andres-Lacueva, C.; Lamuela-Raventós, R.M.; Berenguer, T.; Jakszyn, P.; Barricarte, A.; Ardanaz, E.; Amiano, P.; Dorronsoro, M.; Larrañaga, N. Estimation of dietary sources and flavonoid intake in a Spanish adult population (EPIC-Spain). J. Am. Diet. Assoc. 2010, 110, 390–398. [Google Scholar] [CrossRef] [PubMed]
- Vogiatzoglou, A.; Mulligan, A.A.; Lentjes, M.A.; Luben, R.N.; Spencer, J.P.; Schroeter, H.; Khaw, K.; Kuhnle, G.G. Flavonoid intake in European adults (18 to 64 years). PLoS ONE 2015, 10, e0128132. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Haddaway, N.R.; Page, M.J.; Pritchard, C.C.; McGuinness, L.A. PRISMA2020: An R Package and Shiny App for Producing PRISMA 2020-Compliant Flow Diagrams, with Interactivity for Optimised Digital Transparency and Open Synthesis. Campbell Syst. Rev. 2022, 18, e1230. [Google Scholar] [CrossRef] [PubMed]
- Pun, V.C.; Kazemiparkouhi, F.; Manjourides, J.; Suh, H.H. Long-Term PM2.5 Exposure and Respiratory, Cancer, and Cardiovascular Mortality in Older US Adults. Am. J. Epidemiol. 2017, 186, 961–969. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.S.; Lin, Y.C.; Sung, L.C.; Chen, T.T.; Ma, H.P.; Hsu, Y.H.; Tsai, S.H.; Lin, Y.F.; Wu, M.Y. Increased Long-Term Risk of Major Adverse Cardiovascular Events in Patients with Carbon Monoxide Poisoning: A Population-Based Study in Taiwan. PLoS ONE 2017, 12, e0176465. [Google Scholar] [CrossRef]
- Sun, D.; Liu, C.; Ding, Y.; Yu, C.; Guo, Y.; Sun, D.; Pang, Y.; Pei, P.; Du, H.; Yang, L.; et al. Long-Term Exposure to Ambient PM2·5, Active Commuting, and Farming Activity and Cardiovascular Disease Risk in Adults in China: A Prospective Cohort Study. Lancet Planet. Health 2023, 7, e304–e312. [Google Scholar] [CrossRef]
- You, J.; Liu, Y.; Dong, J.; Wang, J.; Bao, H. Ambient Carbon Monoxide and the Risk of Cardiovascular Disease Emergency Room Visits: A Time-Series Study in Lanzhou, China. Environ. Geochem. Health 2023, 45, 7621–7636. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Zhao, J.; Zhuo, C.; Zheng, L. The Association Between Ambient Air Pollution and Atrial Fibrillation. Int. Heart J. 2021, 62, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Alexeeff, S.E.; Liao, N.S.; Liu, X.; Van Den Eeden, S.K.; Sidney, S. Long-Term PM2.5 Exposure and Risks of Ischemic Heart Disease and Stroke Events: Review and Meta-Analysis. J. Am. Heart Assoc. 2021, 10, e016890. [Google Scholar] [CrossRef]
- Cao, Y.; Feng, Y.; Xia, N.; Zhang, J. Causal Associations of Particulate Matter 2.5 and Cardiovascular Disease: A Two-Sample Mendelian Randomization Study. PLoS ONE 2024, 19, e0301823. [Google Scholar] [CrossRef] [PubMed]
- de Bont, J.; Jaganathan, S.; Dahlquist, M.; Persson, Å.; Stafoggia, M.; Ljungman, P. Ambient Air Pollution and Cardiovascular Diseases: An Umbrella Review of Systematic Reviews and Meta-Analyses. J. Intern. Med. 2022, 291, 779–800. [Google Scholar] [CrossRef] [PubMed]
- Jia, Y.; Lin, Z.; He, Z.; Li, C.; Zhang, Y.; Wang, J.; Liu, F.; Li, J.; Huang, K.; Cao, J.; et al. Effect of Air Pollution on Heart Failure: Systematic Review and Meta-Analysis. Environ. Health Perspect. 2023, 131, 76001. [Google Scholar] [CrossRef] [PubMed]
- Karim, N.; Hod, R.; Wahab, M.I.A.; Ahmad, N. Projecting Non-Communicable Diseases Attributable to Air Pollution in the Climate Change Era: A Systematic Review. BMJ Open 2024, 14, e079826. [Google Scholar] [CrossRef] [PubMed]
- Khoshakhlagh, A.H.; Mohammadzadeh, M.; Gruszecka-Kosowska, A.; Oikonomou, E. Burden of Cardiovascular Disease Attributed to Air Pollution: A Systematic Review. Glob. Health 2024, 20, 37. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Meijer, P.; Lam, T.M.; Timmermans, E.J.; Grobbee, D.E.; Beulens, J.W.J.; Vaartjes, I.; Lakerveld, J. The Built Environment and Cardiovascular Disease: An Umbrella Review and Meta-Meta-Analysis. Eur. J. Prev. Cardiol. 2023, 30, 1801–1827. [Google Scholar] [CrossRef]
- Serra, R.; Abramo, A.; Ielapi, N.; Procopio, S.; Marino, P. Environmental Pollution and Peripheral Artery Disease. Risk Manag. Healthc. Policy 2021, 14, 2181. [Google Scholar] [CrossRef]
- Yang, H.; Li, S.; Sun, L.; Zhang, X.; Cao, Z.; Xu, C.; Cao, X.; Cheng, Y.; Yan, T.; Liu, T.; et al. Smog and Risk of Overall and Type-Specific Cardiovascular Diseases: A Pooled Analysis of 53 Cohort Studies with 21.09 Million Participants. Environ. Res. 2019, 172, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Brook, R.D.; Li, Y.; Rajagopalan, S.; Kim, J.B. Air Pollution, Built Environment, and Early Cardiovascular Disease. Circ. Res. 2023, 132, 1707–1724. [Google Scholar] [CrossRef] [PubMed]
- Goetz, M.E.; Judd, S.E.; Safford, M.M.; Hartman, T.J.; McClellan, W.M.; Vaccarino, V. Dietary Flavonoid Intake and Incident Coronary Heart Disease: The REasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Am. J. Clin. Nutr. 2016, 104, 1236–1244. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.M.; Zhao, D.; Nie, Z.L.; Zhao, H.; Zhou, B.; Gao, W.; Wang, L.S.; Yang, Z.J. Flavonol Intake and Stroke Risk: A Meta-Analysis of Cohort Studies. Nutrition 2014, 30, 518–523. [Google Scholar] [CrossRef] [PubMed]
- Hu, B.; Wang, Y.; Feng, J.; Hou, L. The Association between Flavonoids Intake and Hypertension in U.S. Adults: A Cross-Sectional Study from The National Health and Nutrition Examination Survey. J. Clin. Hypertens. 2024, 26, 573–583. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Li, D.; Huang, T. Associations of Dietary Flavonoids and Subclasses with Total and Cardiovascular Mortality among 369,827 Older People: The NIH-AARP Diet and Health Study. Atherosclerosis 2023, 365, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Zhu, X.; Xing, Y.; Guan, G.; Zhang, Y.; Hui, R.; Wang, X.; Liu, S.; Pang, H.; Zhu, L. Associations of Dietary Flavonoid Intake with the Risk of All-Cause and Cardiovascular Mortality in Adults. Clin. Nutr. ESPEN 2024, 62, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Zong, Z.; Cheng, X.; Yang, Y.; Qiao, J.; Hao, J.; Li, F. Association between Dietary Flavonol Intake and Mortality Risk in the U.S. Adults from NHANES Database. Sci. Rep. 2024, 14, 4572. [Google Scholar] [CrossRef] [PubMed]
- Bondonno, N.P.; Liu, Y.L.; Zheng, Y.; Ivey, K.; Willett, W.C.; Stampfer, M.J.; Rimm, E.B.; Cassidy, A. Change in Habitual Intakes of Flavonoid-Rich Foods and Mortality in US Males and Females. BMC Med. 2023, 21, 181. [Google Scholar] [CrossRef]
- Wan, Y.; Ma, D.; Shang, Q.; Xu, H. Association between Dietary Flavonoid Intake and Hypertension among U.S. Adults. Front. Immunol. 2024, 15, 1380493. [Google Scholar] [CrossRef] [PubMed]
- Bondonno, N.P.; Dalgaard, F.; Kyrø, C.; Murray, K.; Bondonno, C.P.; Lewis, J.R.; Croft, K.D.; Gislason, G.; Scalbert, A.; Cassidy, A.; et al. Flavonoid Intake Is Associated with Lower Mortality in the Danish Diet Cancer and Health Cohort. Nat. Commun. 2019, 10, 3651. [Google Scholar] [CrossRef] [PubMed]
- Bondonno, N.P.; Murray, K.; Cassidy, A.; Bondonno, C.P.; Lewis, J.R.; Croft, K.D.; Kyrø, C.; Gislason, G.; Torp-Pedersen, C.; Scalbert, A.; et al. Higher Habitual Flavonoid Intakes Are Associated with a Lower Risk of Peripheral Artery Disease Hospitalizations. Am. J. Clin. Nutr. 2021, 113, 187–199. [Google Scholar] [CrossRef] [PubMed]
- Adriouch, S.; Lampuré, A.; Nechba, A.; Baudry, J.; Assmann, K.; Kesse-Guyot, E.; Hercberg, S.; Scalbert, A.; Touvier, M.; Fezeu, L.K. Prospective Association between Total and Specific Dietary Polyphenol Intakes and Cardiovascular Disease Risk in the Nutrinet-Santé French Cohort. Nutrients 2018, 10, 1587. [Google Scholar] [CrossRef]
- Ponzo, V.; Goitre, I.; Fadda, M.; Gambino, R.; De Francesco, A.; Soldati, L.; Gentile, L.; Magistroni, P.; Cassader, M.; Bo, S. Dietary Flavonoid Intake and Cardiovascular Risk: A Population-Based Cohort Study. J. Transl. Med. 2015, 13, 218. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Micek, A.; Godos, J.; Pajak, A.; Sciacca, S.; Galvano, F.; Giovannucci, E.L. Dietary Flavonoid and Lignan Intake and Mortality in Prospective Cohort Studies: Systematic Review and Dose-Response Meta-Analysis. Am. J. Epidemiol. 2017, 185, 1304–1316. [Google Scholar] [CrossRef] [PubMed]
- Jiang, W.; Wei, H.; He, B. Dietary Flavonoids Intake and the Risk of Coronary Heart Disease: A Dose-Response Meta-Analysis of 15 Prospective Studies. Thromb. Res. 2015, 135, 459–463. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Je, Y. Flavonoid Intake and Mortality from Cardiovascular Disease and All Causes: A Meta-Analysis of Prospective Cohort Studies. Clin. Nutr. ESPEN 2017, 20, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.M.; Liu, Y.J.; Huang, Y.; Yu, H.J.; Yuan, S.; Tang, B.W.; Wang, P.G.; He, Q.Q. Dietary Total Flavonoids Intake and Risk of Mortality from All Causes and Cardiovascular Disease in the General Population: A Systematic Review and Meta-Analysis of Cohort Studies. Mol. Nutr. Food Res. 2017, 61, 1601003. [Google Scholar] [CrossRef] [PubMed]
- Micek, A.; Godos, J.; Del Rio, D.; Galvano, F.; Grosso, G. Dietary Flavonoids and Cardiovascular Disease: A Comprehensive Dose-Response Meta-Analysis. Mol. Nutr. Food Res. 2021, 65, 2001019. [Google Scholar] [CrossRef]
- Raman, G.; Avendano, E.E.; Chen, S.; Wang, J.; Matson, J.; Gayer, B.; Novotny, J.A.; Cassidy, A. Dietary Intakes of Flavan-3-Ols and Cardiometabolic Health: Systematic Review and Meta-Analysis of Randomized Trials and Prospective Cohort Studies. Am. J. Clin. Nutr. 2019, 110, 1067–1078. [Google Scholar] [CrossRef]
- Ciumărnean, L.; Milaciu, M.V.; Runcan, O.; Vesa, S.C.; Răchisan, A.L.; Negrean, V.; Perné, M.G.; Donca, V.I.; Alexescu, T.G.; Para, I.; et al. The Effects of Flavonoids in Cardiovascular Diseases. Molecules 2020, 25, 4320. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, I.; Pérez-Gregorio, R.; Soares, S.; Mateus, N.; De Freitas, V.; Santos-Buelga, C.; Feliciano, A.S. Wine Flavonoids in Health and Disease Prevention. Molecules 2017, 22, 292. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Luo, J.; Peng, L.; Zhang, Q.; Rong, X.; Luo, Y.; Li, J. Flavonoids: Potential Therapeutic Agents for Cardiovascular Disease. Heliyon 2024, 10, e32563. [Google Scholar] [CrossRef] [PubMed]
- Maaliki, D.; Shaito, A.A.; Pintus, G.; El-Yazbi, A.; Eid, A.H. Flavonoids in Hypertension: A Brief Review of the Underlying Mechanisms. Curr. Opin. Pharmacol. 2019, 45, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Macready, A.L.; George, T.W.; Chong, M.F.; Alimbetov, D.S.; Jin, Y.; Vidal, A.; Spencer, J.P.E.; Kennedy, O.B.; Tuohy, K.M.; Minihane, A.M.; et al. Flavonoid-Rich Fruit and Vegetables Improve Microvascular Reactivity and Inflammatory Status in Men at Risk of Cardiovascular Disease—FLAVURS: A Randomized Controlled Trial. Am. J. Clin. Nutr. 2014, 99, 479–489. [Google Scholar] [CrossRef] [PubMed]
- Rees, A.; Dodd, G.F.; Spencer, J.P.E. The Effects of Flavonoids on Cardiovascular Health: A Review of Human Intervention Trials and Implications for Cerebrovascular Function. Nutrients 2018, 10, 1852. [Google Scholar] [CrossRef] [PubMed]
- Vazhappilly, C.G.; Ansari, S.A.; Al-Jaleeli, R.; Al-Azawi, A.M.; Ramadan, W.S.; Menon, V.; Hodeify, R.; Siddiqui, S.S.; Merheb, M.; Matar, R.; et al. Role of Flavonoids in Thrombotic, Cardiovascular, and Inflammatory Diseases. Inflammopharmacology 2019, 27, 863–869. [Google Scholar] [CrossRef] [PubMed]
- Yan, Q.; Liu, S.; Sun, Y.; Chen, C.; Yang, S.; Lin, M.; Long, J.; Yao, J.; Lin, Y.; Yi, F.; et al. Targeting Oxidative Stress as a Preventive and Therapeutic Approach for Cardiovascular Disease. J. Transl. Med. 2023, 21, 519. [Google Scholar] [CrossRef]
- Yang, Y.; Trevethan, M.; Wang, S.; Zhao, L. Beneficial Effects of Citrus Flavanones Naringin and Naringenin and Their Food Sources on Lipid Metabolism: An Update on Bioavailability, Pharmacokinetics, and Mechanisms. J. Nutr. Biochem. 2022, 104, 108967. [Google Scholar] [CrossRef]
- Zhou, D.; Bai, Z.; Guo, T.; Li, J.; Li, Y.; Hou, Y.; Chen, G.; Li, N. Dietary Flavonoids and Human Top-Ranked Diseases: The Perspective of in vivo Bioactivity and Bioavailability. Trends Food Sci. Technol. 2022, 120, 374–386. [Google Scholar] [CrossRef]
- Chen, Z.; Zhang, S.L. The Role of Flavonoids in the Prevention and Management of Cardiovascular Complications: A Narrative Review. Ann. Palliat. Med. 2021, 10, 8254–8263. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Lu, T.; Yang, R.; Zhou, S. Associations of Flavonoid Intakes with Mortality among Populations with Hypertension: A Prospective Cohort Study. Nutrients 2024, 16, 1534. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Ouyang, Y.Y.; Liu, J.; Zhao, G. Flavonoid Intake and Risk of CVD: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Br. J. Nutr. 2014, 111, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Zhong, J.; Colicino, E.; Lin, X.; Mehta, A.; Kloog, I.; Zanobetti, A.; Byun, H.M.; Bind, M.A.; Cantone, L.; Prada, D.; et al. Cardiac Autonomic Dysfunction: Particulate Air Pollution Effects Are Modulated by Epigenetic Immunoregulation of Toll-like Receptor 2 and Dietary Flavonoid Intake. J. Am. Heart Assoc. Cardiovasc. Cerebrovasc. Dis. 2015, 4. [Google Scholar] [CrossRef] [PubMed]
- Münzel, T.; Hahad, O.; Daiber, A.; Lelieveld, J. Air Pollution and Cardiovascular Diseases. Herz 2021, 46, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Montano, L.; Maugeri, A.; Volpe, M.G.; Micali, S.; Mirone, V.; Mantovani, A.; Navarra, M.; Piscopo, M. Mediterranean Diet as a Shield against Male Infertility and Cancer Risk Induced by Environmental Pollutants: A Focus on Flavonoids. Int. J. Mol. Sci. 2022, 23, 1568. [Google Scholar] [CrossRef] [PubMed]
- Hadley, M.B.; Baumgartner, J.; Vedanthan, R. Developing a Clinical Approach to Mitigating Risks of Air Pollution and Protecting Cardiovascular Health. Circulation 2018, 137, 725. [Google Scholar] [CrossRef] [PubMed]
- Barthelemy, J.; Sanchez, K.; Miller, M.R.; Khreis, H. New Opportunities to Mitigate the Burden of Disease Caused by Traffic Related Air Pollution: Antioxidant-Rich Diets and Supplements. Int. J. Environ. Res. Public Health 2020, 17, 630. [Google Scholar] [CrossRef]
- Halliwell, B.; Rafter, J.; Jenner, A. Health Promotion by Flavonoids, Tocopherols, Tocotrienols, and Other Phenols: Direct or Indirect Effects? Antioxidant or Not? Am. J. Clin. Nutr. 2005, 81, 268S–276S. [Google Scholar] [CrossRef]
- Neves, M.F.; Cunha, M.R.; de Paula, T. Effects of Nutrients and Exercises to Attenuate Oxidative Stress and Prevent Cardiovascular Disease. Curr. Pharm. Des. 2018, 24, 4800–4806. [Google Scholar] [CrossRef]
- Laumbach, R.; Meng, Q.; Kipen, H. What Can Individuals Do to Reduce Personal Health Risks from Air Pollution? J. Thorac. Dis. 2015, 7, 96. [Google Scholar] [CrossRef] [PubMed]
- Brauer, M.; Casadei, B.; Harrington, R.A.; Kovacs, R.; Sliwa, K.; Brauer, M.; Davaakhuu, N.; Hadley, M.; Kass, D.; Miller, M.; et al. Taking a Stand against Air Pollution—The Impact on Cardiovascular Disease. Circulation 2021, 143, E800–E804. [Google Scholar] [CrossRef] [PubMed]
- Péter, S.; Holguin, F.; Wood, L.G.; Clougherty, J.E.; Raederstorff, D.; Antal, M.; Weber, P.; Eggersdorfer, M. Nutritional Solutions to Reduce Risks of Negative Health Impacts of Air Pollution. Nutrients 2015, 7, 10398–10416. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.L.; Gong, Y.; Qi, Y.J.; Shao, Z.M.; Jiang, Y.Z. Effects of Dietary Intervention on Human Diseases: Molecular Mechanisms and Therapeutic Potential. Signal Transduct. Target. Ther. 2024, 9, 59. [Google Scholar] [CrossRef] [PubMed]
- Pueyo-Garrigues, M.; Whitehead, D.; Pardavila-Belio, M.I.; Canga-Armayor, A.; Pueyo-Garrigues, S.; Canga-Armayor, N. Health Education: A Rogerian Concept Analysis. Int. J. Nurs. Stud. 2019, 94, 131–138. [Google Scholar] [CrossRef]
- Nelson, M.E.; Hamm, M.W.; Hu, F.B.; Abrams, S.A.; Griffin, T.S. Alignment of Healthy Dietary Patterns and Environmental Sustainability: A Systematic Review. Adv. Nutr. 2016, 7, 1005–1025. [Google Scholar] [CrossRef]
- Wu, Q.; Gao, Z.J.; Yu, X.; Wang, P. Dietary Regulation in Health and Disease. Signal Transduct. Target. Ther. 2022, 7, 252. [Google Scholar] [CrossRef]
- Solnier, J.; Chang, C.; Pizzorno, J. Consideration for Flavonoid-Containing Dietary Supplements to Tackle Deficiency and Optimize Health. Int. J. Mol. Sci. 2023, 24, 8663. [Google Scholar] [CrossRef]
- Tilman, D.; Clark, M. Global Diets Link Environmental Sustainability and Human Health. Nature 2014, 515, 518–522. [Google Scholar] [CrossRef]
- Romanello, M.; McGushin, A.; Di Napoli, C.; Drummond, P.; Hughes, N.; Jamart, L.; Kennard, H.; Lampard, P.; Solano Rodriguez, B.; Arnell, N.; et al. The 2021 Report of the Lancet Countdown on Health and Climate Change: Code Red for a Healthy Future. Lancet 2021, 398, 1619–1662. [Google Scholar] [CrossRef]
- World Health Organization. New WHO Global Air Quality Guidelines Aim to Save Millions of Lives from Air Pollution. Available online: https://www.who.int/news/item/22-09-2021-new-who-global-air-quality-guidelines-aim-to-save-millions-of-lives-from-air-pollution (accessed on 4 July 2024).

| Cardiovascular Outcome/Condition | Air Pollution Exposure and Association | Study Design | Author |
|---|---|---|---|
| General Cardiovascular Outcomes | |||
| Increased occurrence of CVDs | Increased exposure to PM2.5 and O3 (CHD, IHD, and stroke) | Systematic review | Karim, 2024 [59] |
| PM2.5, NO2, O3, and VOC associations: short-term outcomes, acute effects (myocardial infraction, coronary events, endothelial injury) and long-term exposure, chronic processes (atherosclerosis) | Review | Blaustein et al., 2024 [22] | |
| Early onset of CVDs | PM2.5, NO2, O3, and VOC, specifically HTN and atherosclerosis | Review | Zhang et al., 2023 [64] |
| Progression from pre-HTN to HTN, CVD, and death | Exposure to PM2.5 associated with progression from pre-HTN to HTN (HR: 1.105), pre-HTN to CVD (HR: 1.045), and pre-HTN to death (HR: 1.086). Air pollution could act directly on CVD progression | Cohort study | Zhang et al., 2023 [23] |
| Increased prevalence, hospitalization, disability, mortality, and costs of CVDs | Chronic exposure to NO2, O3, PM10, PM2.5, and SO2 | Review | Khoshakhlagh, 2024 [60] |
| Projected increase in NCD burden | Projected increase in CVD, stroke, IHD, and CHD under adverse scenarios | Systematic review | Karim et al., 2024 [59] |
| Specific cardiovascular conditions | |||
| Coronary artery disease | Causal effect observed with PM2.5 (IVW: OR 2.06, 95% CI 1.35, 3.14) | Mendelian randomization | Cao et al., 2024 [56] |
| Hypertension (HTN) | Causal effect observed with PM2.5 (IVW: OR 1.07, 95% CI 1.03, 1.12) | Mendelian randomization | Cao et al., 2024 [56] |
| Chronic exposure to NO2, O3, PM10, PM2.5, and SO2, with PM2.5 and NO2 being closely associated | Review | Khoshakhlagh, 2024 [60] | |
| Long-term exposure to PM2.5 (OR: 1.05); short-term exposure to PM10, PM2.5, SO2, and NO2 (ORs: 1.05 to 1.10) | Meta-analysis | Yang et al., 2018 [11] | |
| Short-term exposures to PM2.5, PM10, and NOx consistently associated with increased risks of HTN | Systematic review | de Bont et al., 2022 [57] | |
| Stroke | Long-term exposure to PM2.5 (per 10 µg/m3 increase) associated with a 13% increased risk | Cohort study | Alexeeff et al., 2021 [43] |
| Long-term exposure to PM2.5 (per 10 μg/m3 increase) associated with increased risk (RR: 1.12, 95% CI 1.05–1.19) | Meta-analysis | Yang et al., 2019 [63] | |
| Short-term exposures to PM2.5, PM10, and NOx consistently associated with increased risks of stroke (fatal and nonfatal) | Systematic review | de Bont et al., 2022 [57] | |
| Incident myocardial infarction (MI) | Long-term exposure to PM2.5 (per 10 µg/m3 increase) associated with an 8% increased risk | Cohort study | Alexeeff et al., 2021 [55] |
| Short-term exposure to PM2.5, PM10, and NOx (per 10 μg/m3 increase) is associated with increased MI risk: PM2.5 (1.20–2.40%, 95% CI 1.00–4.10%), PM10 (0.50–1.10%, 95% CI 0.10–1.60%), and NOx (1.10%, 95% CI 0.60–1.60%) | Systematic review | de Bont et al., 2022 [57] | |
| Atrial fibrillation (AF) | AF attack: Short-term exposure to PM2.5 (ER: 1.8%), SO2 (ER: 2.9%), and NO2 (ER: 3.2%) per 10 μg/m3 or 10 ppb increase AF incidence: Long-term exposure to PM2.5, PM10, SO2, NO2, and CO | Meta-analysis | Chen et al., 2021 [54] |
| Heart failure (HF) | Short-term exposure: PM2.5 (RR: 1.018), PM10 (RR: 1.016), and significantly associated with NO2, SO2, CO Long-term exposure: PM2.5 (RR: 1.748), PM10 (RR: 1.212), NO2 (RR: 1.204) | Meta-analysis | Jia et al., 2023 [58] |
| Cardiac arrhythmias and other cardiac diseases | PM, lead, CO, SO2, and NOx proarrhythmic effects associated with HF, ischemia, atrial and ventricular arrhythmias | Review | Palacio et al., 2023 [10] |
| Major adverse cardiovascular events (MACEs) | CO poisoning associated with higher risk of MACEs (HR: 2.00, 95% CI: 1.83–2.18) | Cohort study | Wong, 2017 [51] |
| Peripheral artery disease (PAD) | Long-term exposure to PM10 significantly associated with PAD (R2: 0.5) | Review | Serra et al., 2021 [62] |
| Atherosclerosis | Long-term exposure to PM2.5 associated with the development of atherosclerosis | Review | Tian et al., 2021 [20] |
| Long-term exposure to PM2.5 associated with increased risk of atherosclerosis | Systematic review | de Bont et al., 2022 [57] | |
| Increased Risk and Mortality of CVDs | |||
| Increased risk of mortality from CVDs (including IHD and stroke) | Long-term exposure to PM2.5 (per 10 μg/m3 increase), IHD mortality increased (HR: 1.16), stroke mortality increase (HR: 1.14) Different levels of PM2.5 exposure, 8–12 μg/m3, 12–20 μg/m3, and >20 μg/m3, are associated with increased mortality risk by 4%, 8%, and 19% | Cohort study | Hayes, 2020 [24] |
| Long-term exposure to PM2.5 (per 10 μg/m3 increase) associated with increased mortality risk (RR: 1.10 to 1.33) | Meta-analysis | Pun, 2017 [50] | |
| Long-term exposure to PM2.5 (per 10 μg/m3 increase) associated with increased risks of IHD mortality (RR: 1.23) and cerebrovascular mortality (RR: 1.24) | Cohort study | Alexeeff et al., 2021 [55] | |
| Long-term exposure to PM2.5, PM10, NO2, and O3 associated with increased risk of CVD mortality (RRs: 1.11, 1.09, 1.23, and 1.03, respectively) | Meta-analysis | Yang et al., 2019 [63] | |
| Increased risk of CVD | Long-term exposure to PM2.5 below the current US standards (12 µg/m3) | Cohort study | Hayes, 2020 [24] |
| Strong evidence of increased risk with PM2.5, SO2, NO2 exposure | Meta-analysis | Liu et al., 2023 [61] | |
| Long-term exposure to PM2.5 (≥54 µg/m3) increases CeVD risk | Cohort study | Sun et al., 2023 [52] | |
| CO poisoning associated with increased risk of arrhythmia (HR: 1.83). CO-poisoned patients with comorbidities have substantially increased risk of CVD | Cohort study | Lee et al., 2015 [7] | |
| Short-term exposure to ambient CO (per 1 mg/m3 increase) associated with increased ERVs for total CVD (RR: 1.041) | Time-series study | You et al., 2023 [53] | |
| Original articles | |||||||
|---|---|---|---|---|---|---|---|
| Author | Publication Date | Location | Population | Study Design | Flavonoid(s) Studied | Beneficial Effects Observed to Prevent CVDs | Limitations |
| Wan et al. [72] | 2024 | United States | 8010 adults | Cross-sectional analysis of NHANES (2007–2010 and 2017–2018) | 29 flavonoid compounds and main subgroups (anthocyanidins, flavan-3-ols, flavanones, flavones, flavonols, and isoflavones) | Reduced risk of hypertension with higher anthocyanin intake (>12.904 mg/day, from diet) (OR: 0.81; 95% CI: 0.66–0.99) and moderate flavan-3-ol intake (16.895–170.916 mg/day, from diet) (OR: 0.79; 95% CI: 0.63–0.99). | Study design limits causal inference. Dietary flavonoid intake recall bias. |
| Hu et al. [67] | 2024 | United States | 15,752 adults | Cross-sectional study (NHANES data from 2007–2010 and 2017–2018) | 29 flavonoid compounds and main subgroups (excluding isoflavones) | Higher total flavonoid intake (specific mg/day not detailed in the data, from diet) was significantly associated with a lower risk of hypertension (OR: 0.78; 95% CI: 0.70–0.88). Additionally, for each unit increase in flavonoid intake (specific mg/day not detailed in the data, from diet), the risk of hypertension decreased by 5% (OR: 0.95; 95% CI: 0.92–0.98). | Study design limits causal inference. HTN severities were not stratified. Potential biases from lifestyle changes postdiagnosis. Flavonoid intake was assessed only at baseline. |
| Wang Kan et al. [94] | 2024 | United States | 6110 adults with HTN | Prospective cohort study (NHANES data from 2007–2008, 2009–2010, and 2017–2018) | 29 flavonoid compounds and main subgroups (anthocyanidins, flavan-3-ols, flavanones, flavones, flavonols, and isoflavones) | Reduced risk of all-cause mortality with higher total flavonoid intake (~375 mg/day, from diet) was observed in hypertensive patients (HR: 0.74; 95% CI: 0.56–0.97). | Study design limits causal inference. Possible misclassification of dietary habits. |
| Bondonno et al. [71] | 2023 | United States | 55,786 females and 29,800 males | Cohort study (NHS and HPFS data from 1994–2018) | Flavonoid-rich foods and beverages (blueberry, apple, orange, tea, onion, pepper, raisin, red wine, orange and grapefruit juice) | Increased intake of flavonoid-rich foods for each 3.5 servings/week increase of blueberries (HR: 0.95; 95% CI: 0.91–0.99), red wine (HR: 0.96; 95% CI: 0.93–0.99), and peppers (HR: 0.91; 95% CI: 0.88–0.95) showed a 4–9% lower cardiovascular mortality risk. | Variability in the flavonoid composition between the seven foods and beverages in flavodiet score. Possible residual confounding despite adjustments. Study design limits causal inference. |
| Zhao et al. [68] | 2023 | United States | 369,827 older adults | Prospective cohort study (NIH-AARP Diet and Health Study) | Total flavonoids and main subgroups (flavonols, flavanols, flavanones, flavones, anthocyanins) | Higher intake from diet of total flavonoids (660 mg/day), flavonols (37.8 mg/day), anthocyanidins (26.9 mg/day), and flavones (2.8 mg/day) is linked to lower risks of death from CVDs (HR: 0.90–0.93), IHD (HR: 0.89–0.94), CeVD (HR: 0.84–0.89), and PAD (HR: 0.79–0.81). | Self-reported dietary intake may lead to recall bias. Baseline flavonoid intake may not accurately reflect subsequent dietary changes. Possible residual confounding despite adjustments. Study design limits causal inference. |
| Bondonno et al. [73] | 2019 | Denmark | 56,048 adults | Prospective cohort study (Danish Diet, Cancer, and Health cohort) | Total flavonoids and main subgroups (flavonols, flavanols, flavanones, flavones, anthocyanins) | Moderate habitual flavonoid intake (~500 mg/day, from diet) inversely associated with cardiovascular mortality (P-nonlinearity < 0.001), particularly in smokers and heavy drinkers. | Study design limits causal inference. Dietary data may have changed over 23 years, affecting association detection. Limited generalizability due to homogeneity of population. |
| Bondonno et al. [74] | 2021 | Denmark | 55,647 adults | Prospective cohort study (Danish Diet, Cancer, and Health cohort) | Total flavonoids and main subgroups (isoflavones were excluded) | Higher total flavonoid intake (~750–1000 mg/d) vs. lowest median intake (174 mg/d) linked to significantly lower risks of any PAD hospitalization (HR: 0.68; 95% CI: 0.60–0.77), atherosclerosis (HR: 0.74; 95% CI: 0.62–0.88), aneurysm (HR: 0.72; 95% CI: 0.59–0.88), hospitalization for other PADs (HR: 0.53; 95% CI: 0.42–0.67). | Study design limits causal inference. Dietary data may have changed over 23 years, affecting association detection. Limited generalizability due to homogeneity of population. |
| Goetz et al. [65] | 2016 | United States | 16,678 adults | Prospective cohort study (REGARDS study, 2003–2007) | Total flavonoid, anthocyanidins, flavan-3-ols, flavanones, flavone, flavonols, and proanthocyanidins | Higher intake of anthocyanidin (≥18.6 mg/day, from diet) (HR: 0.71; 95% CI: 0.52–0.98) and proanthocyanidin (≥137 mg/day, form diet) (HR: 0.63; 95% CI: 0.47–0.84) linked to lower incidence of CHD. | Self-reported dietary intake may lead to recall bias. Limited by the accuracy of the USDA flavonoid database. |
| Macready et al. [87] | 2014 | United Kingdom | 174 adults at risk of CVD | Randomized controlled trial (FLAVURS study) | Flavonoid-rich fruits and vegetables (berries, citrus fruit, apples, grapes, peppers, onions, broccoli, herbs) | In men, the high-flavonoid fruit and vegetable diet (>15 mg/100 g of total flavonoids) increased endothelium-dependent microvascular reactivity (p = 0.017) with +2 portions/d (at 6 weeks) and reduced C-reactive protein (p = 0.001) and E-selectin (p = 0.0005), while +4 portions/d (at 12 weeks) reduced vascular cell adhesion molecule (p = 0.0468). Additionally, +14 portions/d (at 12 weeks) increased plasma NO (p = 0.0243) in the group as a whole. | Single-blind design. Limited to low fruit and vegetable consumers. Results may not be generalizable to other populations. |
| Zong et al. [70] | 2024 | United States | 11,679 adults | Prospective cohort study (NHANES data from 2007–2008, 2009–2010, and 2017–2018) | Total flavonol, isorhamnetin, kaempferol, myricetin, quercetin | Total flavonol intake (~24–288 mg/day, from diet) was associated with reduced CVD-specific mortality (HR: 0.67; 95% CI: 0.47–0.96). Similarly, quercetin intake (~15.07–196.51 mg/day, from diet) and myricetin intake (~1.6–79.76 mg/day, from diet) were linked to reduced CVD-specific mortality risk, with HRs of 0.61 (95% CI: 0.40–0.93) and 0.61 (95% CI: 0.47–0.80), respectively. | Database limitations (lack of dietary flavonol intake data for over half the sample). Potential residual confounding (unadjusted factors like total energy intake and/or supplementation). Study design limits causal inference. |
| Ponzo et al. [76] | 2015 | Italy | 1658 adults | Prospective cohort study (2001–2003) | Total flavonoids, flavan-3-ols, anthocyanidins, flavanones, flavones, isoflavones | Higher intake of flavonoids (251 mg/day), flavan-3-ols (50.4 mg/day), anthocyanidins (32.9 mg/day), and flavanones (24.2 mg/day) from diet is linked to lower CV risk and all-cause mortality (HR: 0.64, 0.68, 0.66, and 0.59, respectively). | Limited by self-reported dietary data, potential confounding factors, low consumption of certain flavonoid-rich foods. |
| Xu et al. [69] | 2024 | United States | 8758 adults | Prospective cohort study (NHANES data from 2007–2010) | 29 flavonoid compounds and main subgroups (anthocyanidins, flavan-3-ols, flavanones, flavones, flavonols, and isoflavones). | Higher intake of total flavonoids (>169.65 mg/day, from diet) associated with reduced risk of cardiovascular mortality (HR: 0.54, 95% CI: 0.36–0.80). Significant inverse associations for flavonols (>21.30 mg/day, from diet) (HR: 0.41, 95% CI: 0.22–0.78) and flavones (>0.97 mg/day, from diet) (HR: 0.68, 95% CI: 0.29–0.89). | Observational design limits causal inference. Potential misclassification of flavonoid intake due to 24 h recall method. Residual confounding possible. Study population limited to US adults. |
| Adriouch et al. [75] | 2018 | France | 84,158 adults | Prospective cohort study (2009–2017) | Anthocyanins, catechins, flavonols, dihydrochalcones, proanthocyanidins, dihydroflavonols, hydroxybenzoic acids, stilbenes | For each 10 mg/day intake of anthocyanins (HR: 0.98), catechins (HR: 0.98), and flavonols (HR: 0.94), there was a strong inverse association with cardiovascular disease risk. | Shorter follow-up period, reliance on self-reported dietary data, potential for residual confounding. |
| Review Articles | |||||||
| Author | Publication Date | Study Design | Flavonoid(s) Studied | Beneficial Effects Observed to Prevent CVDs | Limitations | ||
| Liu et al. [85] | 2024 | Literature review | Various flavonoids (such as quercetin, myricetin, catechin, anthocyanins, nobiletin, hesperidin, formononetin, baicalin, vitexin, silymarin) | Antioxidant, anti-inflammatory, and therapeutic effects through modulation of TLR4-NF-ĸB, PI3K-AKT, and Nrf2/HO-1 pathways. Sources include dietary flavonoids from green tea, soybeans, citrus fruits, red wine, purple grapes, etc.; specific doses are not consistently reported across human, in vitro, and animal studies. | Bioavailability and efficacy of flavonoids are not fully addressed due to variability in study designs and dosing. | ||
| Yan et al. [90] | 2023 | Literature review | Herbal monomers baicalin, quercetin, luteolin, naringin | Flavonoid compounds can prevent OS and reduce oxidative damage in cardiovascular diseases by scavenging ROS and enhancing endogenous antioxidant capacity. Sources include red wine, tea, fruits, and citrus fruits, and dietary supplementation. Specific doses are not reported. Effects observed across various studies including human, in vitro, and animal research. | Variability in bioavailability and efficacy of different flavonoids not fully addressed. | ||
| Yang et al. [91] | 2022 | Literature review | Citrus flavanones (naringin and naringenin) | Naringenin and naringin (450 mg/day, daily oral intake, in humans) can enhance lipid metabolism and cardiovascular health in in vitro, animal, and human studies. Effects were also observed from dietary sources and supplements. | Results across clinical trials are inconsistent. Further research is needed to determine optimal doses, intervention periods, and timing. High in vitro doses (e.g., 100 µM) may not directly translate to in vivo relevance. | ||
| Ciumărnean et al. [83] | 2020 | Literature review | Various flavonoids (such as: myricetin, quercetin, methyl-flavonol, kaempferol, naringenin, apigenin-7-O-neohesperidoside, tannins, luteolin, rutin, hesperidin, naringenin, pinocembrin, resveratrol, apigenin, cyanidins, phenolic acids, tallianine, diosmetin, catechin, epicatechin, epiafzelechin, gallocatechin) | Multiple cardiovascular benefits in in vivo and in vitro studies: antiplatelet, anti-inflammatory, antioxidant, antiatherogenic, antihypertensive. Doses were not specified. | Mechanisms not fully understood. Variability in bioavailability and efficacy of different flavonoids. | ||
| Fernandes et al. [84] | 2017 | Literature review | Wine flavonoids (flavanols and anthocyanins) | Wine flavonoids protect CV health by improving endothelial function, reducing LDL oxidation, lowering blood pressure, inhibiting platelet aggregation, and exerting anti-inflammatory and antioxidant effects. Effects shown in in vivo and in vitro studies. Dietary intake and supplementation, doses were not specified. | Insufficient epidemiological and in vivo evidence. Complex variables such as human age, metabolism, and complex wine chemistry complicate the assessment of bioavailability and health-promoting effects. | ||
| Maaliki et al. [86] | 2019 | Literature review | Main subgroups: flavanones, flavan-3-ols, flavonols, flavones, anthocyanins, and isoflavones | Flavanols from apples, pears, tea, grapes, and particularly from cocoa show blood pressure-lowering effects, reduce OS (notably in green tea), improve endothelial function, increase eNOS activity, and induce vasodilation by modulating ion channels. Anthocyanins from vegetables and herbs also lower blood pressure. Flavanones from citrus foods exhibit antioxidant properties and protect endothelial function. These effects are observed in both animal and human studies, though specific doses are not specified. | Variability in bioavailability and efficacy of different flavonoids. Need for more human RCTs to confirm findings. | ||
| Grosso et al. [77] | 2017 | Systematic review and dose-response meta-analysis (22 prospective cohort studies) | Total flavonoids, flavonols, flavones, flavanones, anthocyanidins, proanthocyanidins, lignans | A 100 mg/day increment in total flavonoid intake from diet associated with 4% decreased risk of CVD mortality (P-linearity < 0.001). Dietary flavonoids are associated with decreased risk of CVD mortality. | Limited evidence on specific flavonoid classes and lignans. Potential for residual confounding. Variability in dietary assessment methods across studies. | ||
| Wang Xia et al. [95] | 2014 | Systematic review and meta-analysis (14 prospective cohort studies) | Anthocyanidins, proanthocyanidins, flavones, flavanones, flavan-3-ols, flavonols | An increase of 10 mg/day in dietary flavonol intake is associated with a 5% decreased risk of CVD (RR: 0.95; 95% CI: 0.91–0.99). Diversified intake of flavonoid subclasses through diet is inversely associated with CVD risk. | Potential for residual confounding. Variability in dietary assessment methods across studies. | ||
| Rees et al. [88] | 2018 | Literature review | Various flavonoids (such as: flavanols, epicatechin, procyanidins, quercetin, naringenin, hesperidin) | Flavanol-rich cocoa and green tea exhibit cardioprotective effects, improving FMD response and reducing blood pressure, especially in hypertensive individuals. Blood pressure reductions were noted with cocoa flavanol intake between 450 mg/day and 900 mg/day over one week to one month. | Conflicting results from studies. Need for further research to understand flavonoid effects. | ||
| Micek et al. [81] | 2021 | Dose–response meta-analysis (39 prospective cohort studies) | Total flavonoids, anthocyanins, flavan-3-ols, flavonols, flavones, flavanones, catechins, quercetin, kaempferol | Higher intake of total flavonoids (500 mg/day) is linked to lower CVD risk. Specific doses like 400 mg/day are associated with reduced risks of CHD and stroke. Anthocyanins and flavan-3-ols lower CVD risk; flavonols and flavones reduce CHD risk; flavanones lower stroke risk. Catechins benefit all cardiovascular outcomes. Quercetin and kaempferol are linked to lower CHD and CVD risk, respectively. Doses of other effects are not specified. | Potential for residual confounding. Variability in dietary assessment methods across studies. | ||
| Kim and Je [79] | 2017 | Meta-analysis (15 prospective cohort studies) | Various flavonoid subclasses (excluding flavonols and isoflavones) | High flavonoid intake from diet, specifically around 167.5 mg/day, is associated with a reduced risk of CVD mortality, with a pooled relative risk (RR: 0.86; 95% CI: 0.75, 0.98). | Potential for residual confounding. Variability in dietary assessment methods across studies. | ||
| Wang et al. [66] | 2014 | Meta-analysis of prospective cohort studies (8 studies) | Flavonol | An increase in flavonol intake of 20 mg/day from diet associated with a 14% decrease in stroke risk (summary RR: 0.86, 95% CI: 0.75–0.99). | Meta-analysis, not primary research. Potential for residual confounding. Variability in dietary assessment methods across studies. Inconsistent findings between men and women. | ||
| Liu et al. [80] | 2017 | Systematic review and meta-analysis (10 cohort studies) | Total flavonoids | Marginally significant association between total flavonoid intake (200 mg/day, from diet) and reduced risk of CVD mortality (summary RR: 0.85, 95% CI: 0.70–1.03) and CHD risk (summary RR: 0.74; 95% CI: 0.54–1.02; p = 0.069). | Potential for residual confounding. Variability in dietary assessment methods across studies. Marginal significance in results. Significant heterogeneity across studies. Dietary flavonoid intake collected via FFQs (possible recall and measurement bias). | ||
| Raman et al. [82] | 2019 | Systematic review and meta-analysis (157 randomized trials and 15 prospective cohort studies) | Flavan-3-ols | Higher habitual flavan-3-ol intake (e.g., >800 mg/day, from foods and beverages rich in flavan-3-ols) associated with a 13% reduction in CVD mortality and 19% reduction in CHD incidence. Significant improvements in vascular function, blood pressure regulation. Lipid profile improvement and glucose and insulin metabolism, aiding in cardiovascular health. | Considerable heterogeneity in meta-analysis. Many RCTs of poor quality. Reliance on self-reported intake in cohort studies. Need for integrated intake/biomarker approach in future research. | ||
| Zhou et al. [92] | 2022 | Literature review | Various flavonoids (such as: anthocyanins, citrus flavonoids, quercetin, kaempferol, luteolin, hesperidin) | Anthocyanins (320 mg/day, from an anthocyanin mixture) reduce inflammatory response in hypercholesterolemic patients. Citrus flavonoids (270 mg/day) improve cardiovascular parameters, including reducing cholesterol and LDL. Quercetin (500 mg/day) attenuates atherosclerosis. Kaempferol (50 or 100 mg/kg/day, in mice) decreases atherosclerotic lesion area and improves vasorelaxation. Luteolin (50–100 mg/kg, in rats) protects against cardiotoxicity and improves cardiac function. Hesperidin (500 mg/day in humans; 20–40 mg/kg in rats) improves endothelial function and reduces blood pressure. | Bioavailability and dose-responsive effects remain limitations. More studies needed to confirm findings. | ||
| Vazhappilly et al. [89] | 2019 | Literature review | Plant flavonoids (such as: quercetin, pycnogenol, kaempferol, galangin, nobiletin) | Flavonoids reduce the risk of atherosclerosis and atherothrombotic disease by inhibiting excessive tissue factor availability in the endothelium. They also mitigate endothelial dysfunction, reduce oxidative stress, and inhibit platelet aggregation, which are beneficial for cardiovascular health. Doses were not specified, with studies conducted on humans, rats, and in vitro. | Dose-responsive effects and bioavailability of flavonoids remain limitations. More studies needed to prove effectiveness as antithrombotic agents. | ||
| Chen and Zhang [93] | 2021 | Narrative review | Various flavonoids (rutin, quercetin, catechin, hesperidin, genistein, apigenin) | Hesperidin improves endothelial function and reduces blood pressure (10–50 mg/kg of glucosyl hesperidin in animals; 500 mg/day for 6 days of hesperidin capsules in humans). Rutin and quercetin regulate and restore elevated blood pressure, promote antioxidant defense, and reduce lipid peroxidation in rats. Catechin-rich green tea decreases systolic and diastolic blood pressure and LDL cholesterol in humans. Doses and sources for rutin, quercetin, and catechin were not specified. | More studies needed to confirm findings. | ||
| Jiang et al. [78] | 2015 | Meta-analysis (15 prospective cohort studies) | Various flavonoids (such as: quercetin, kaempferol, myricetin, nobiletin, hesperidin, sylmarin) | Highest flavonoid intake from diet (doses were not specified) associated with reduced risk of CHD (summary RR: 0.85, 95% CI: 0.79–0.91). Flavonoids improve endothelial function, reduce cardiomyocyte death, minimize postischemic infarct size, and lower inflammation, benefiting cardiovascular health. | Potential for residual confounding. Variability in dietary assessment methods across studies. | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rocha-Velasco, O.A.; Morales-Suárez-Varela, M.; Llopis-González, A. Dietary Flavonoids: Mitigating Air Pollution’s Cardiovascular Risks. Nutrients 2024, 16, 2647. https://doi.org/10.3390/nu16162647
Rocha-Velasco OA, Morales-Suárez-Varela M, Llopis-González A. Dietary Flavonoids: Mitigating Air Pollution’s Cardiovascular Risks. Nutrients. 2024; 16(16):2647. https://doi.org/10.3390/nu16162647
Chicago/Turabian StyleRocha-Velasco, Oscar Andrés, María Morales-Suárez-Varela, and Agustín Llopis-González. 2024. "Dietary Flavonoids: Mitigating Air Pollution’s Cardiovascular Risks" Nutrients 16, no. 16: 2647. https://doi.org/10.3390/nu16162647
APA StyleRocha-Velasco, O. A., Morales-Suárez-Varela, M., & Llopis-González, A. (2024). Dietary Flavonoids: Mitigating Air Pollution’s Cardiovascular Risks. Nutrients, 16(16), 2647. https://doi.org/10.3390/nu16162647






