Usefulness of the ECORE-BF Scale to Determine Atherogenic Risk in 386,924 Spanish Workers
Abstract
1. Introduction
2. Materials and Methods
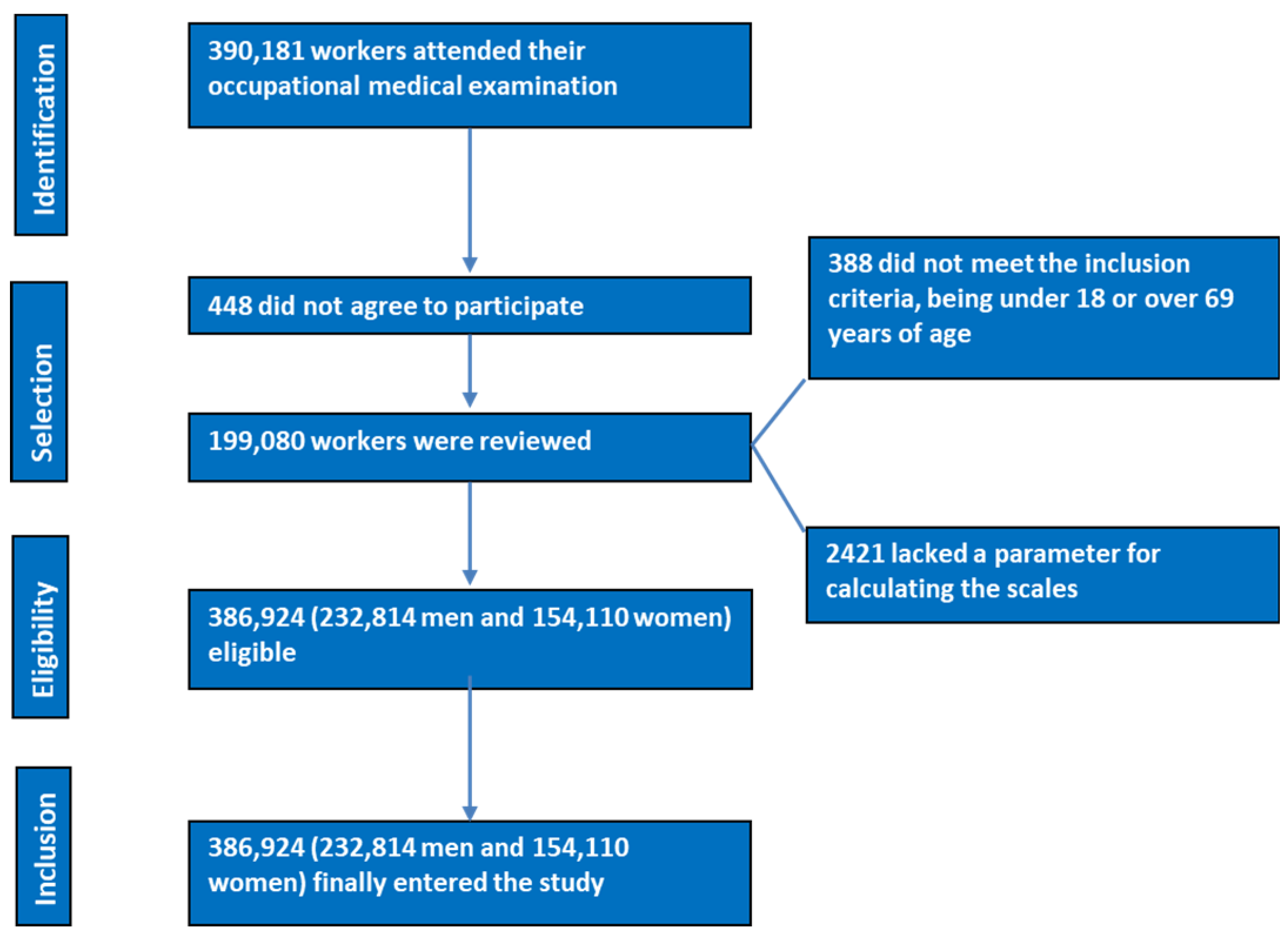
2.1. Participants
- -
- Being in the age range of 18 to 69.
- -
- Holding a job contract with one of the participating businesses.
- -
- Agreeing to participate in the research.
- -
- Agreeing to the transfer of data used for epidemiological research.
- -
- Age under 18 years or over 69 years.
- -
- Not being an employee of one of the participating companies.
- -
- Refusal to participate in the research study.
- -
- Refusal to consent to the use of data for epidemiological research.
2.2. Determination of Variables
- -
- Clinical and anthropometric computations included height, weight, waist circumference, and systolic and diastolic blood pressure.
- -
- Analytical conclusions, glycaemia, and lipid profiles were established.
2.2.1. Anthropometric Determinations
2.2.2. Clinical Determinations
2.2.3. Analytical Determinations
2.2.4. Risk Scales
- -
- Social class I: This comprises university-educated professionals, managers, professional athletes, and artists.
- -
- Social class II: This is made up of intermediate professions and qualified self-employed people.
- -
- Social class III: This group consists of workers with less qualification.
2.3. Statistical Analysis
3. Results
4. Discussion
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lovren, F.; Teoh, H.; Verma, S. Obesity and atherosclerosis: Mechanistic insights. Can. J. Cardiol. 2015, 31, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Riutord-Sbert, P.; Riutord-Fe, B.; Riutord-Fe, N.; Arroyo-Bote, S.; López González, A.A.; Ramírez-Manent, J.I. Influence of physical activity and mediterranean diet on the values of different scales of overweight and obesity. Acad. J. Health Sci. 2022, 37, 21–28. [Google Scholar]
- Bray, G.A. Beyond BMI. Nutrients 2023, 15, 2254. [Google Scholar] [CrossRef] [PubMed]
- Martin, S.S.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.M.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Barone Gibbs, B.; Beaton, A.Z.; Boehme, A.K.; et al. 2024 Heart Disease and Stroke Statistics: A Report of US and Global Data from the American Heart Association. Circulation 2024, 149, e347–e913. [Google Scholar]
- Jaakonmäki, N.; Zedde, M.; Sarkanen, T.; Martinez-Majander, N.; Tuohinen, S.; Sinisalo, J.; Ryödi, E.; Autere, J.; Hedman, M.; Junttola, U.; et al. Obesity and the Risk of Cryptogenic Ischemic Stroke in Young Adults. J. Stroke Cerebrovasc. Dis. 2022, 31, 106380. [Google Scholar] [CrossRef] [PubMed]
- Lopes, K.G.; Rodrigues, E.L.; da Silva Lopes, M.R.; do Nascimento, V.A.; Pott, A.; Guimarães, R.C.A.; Pegolo, G.E.; Freitas, K.C. Adiposity Metabolic Consequences for Adolescent Bone Health. Nutrients 2022, 14, 3260. [Google Scholar] [CrossRef]
- Durnin, J.V.; Womersley, J. Body fat assessed from total body density and its estimation from skinfold thickness: Measurements on 481 men and women aged from 16 to 72 years. Br. J. Nutr. 1974, 32, 77–97. [Google Scholar] [CrossRef] [PubMed]
- Lewandowski, Z.; Dychała, E.; Pisula-Lewandowska, A.; Danel, D.P. Comparison of Skinfold Thickness Measured by Caliper and Ultrasound Scanner in Normative Weight Women. Int. J. Environ. Res. Public Health 2022, 19, 16230. [Google Scholar] [CrossRef] [PubMed]
- Ward, L.C.; Brantlov, S. Bioimpedance basics and phase angle fundamentals. Rev. Endocr. Metab. Disord. 2023, 24, 381–391. [Google Scholar] [CrossRef]
- Rossi, L. Bioimpedance to Assess the Body Composition of High-performance Karate Athletes: Applications, Advantages and Perspectives. J. Electr. Bioimpedance 2021, 12, 69–72. [Google Scholar] [CrossRef]
- Maeda, S.S.; Peters, B.S.E.; Martini, L.A.; Antunes, H.K.M.; Gonzalez, M.C.; Arantes, H.P.; Prado, C.M.; Pinto, C.L.; de Araújo, I.M.; de Paula, F.J.A.; et al. Official position of the Brazilian Association of Bone Assessment and Metabolism (ABRASSO) on the evaluation of body composition by densitometry: Part I (technical aspects)-general concepts, indications, acquisition, and analysis. Adv. Rheumatol. 2022, 62, 7. [Google Scholar] [CrossRef]
- Frija-Masson, J.; Mullaert, J.; Vidal-Petiot, E.; Pons-Kerjean, N.; Flamant, M.; d’Ortho, M.P. Accuracy of Smart Scales on Weight and Body Composition: Observational Study. JMIR Mhealth Uhealth 2021, 9, e22487. [Google Scholar] [CrossRef] [PubMed]
- Hussain, Z.; Jafar, T.; Zaman, M.U.; Parveen, R.; Saeed, F. Correlations of skin fold thickness and validation of prediction equations using DEXA as the gold standard for estimation of body fat composition in Pakistani children. BMJ Open 2014, 4, e004194. [Google Scholar] [CrossRef] [PubMed]
- Holmes, C.J.; Racette, S.B. The Utility of Body Composition Assessment in Nutrition and Clinical Practice: An Overview of Current Methodology. Nutrients 2021, 13, 2493. [Google Scholar] [CrossRef]
- Dempster, P.; Aitkens, S. A new air displacement method for the determination of human body composition. Med. Sci. Sports Exerc. 1995, 27, 1692–1697. [Google Scholar] [CrossRef]
- Garrow, J.S.; Stalley, S.; Diethelm, R.; Pittet, P.; Hesp, R.; Halliday, D. A new method for measuring the body density of obese adults. Br. J. Nutr. 1979, 42, 173–183. [Google Scholar] [CrossRef]
- Goldman, R.; Buskirk, E. Body Volume Measurement by Underwater Weighing: Description of a Method; Brozek, J., Henschel, A., Eds.; National Academy of Sciences: Washington, DC, USA, 1961. [Google Scholar]
- Tesch, J.C.; Papadopoulos, P.; Dolgener, F.; Tinsley, G.M. New Equations for Hydrostatic Weighing without Head Submersion. J. Funct. Morphol. Kinesiol. 2022, 7, 70. [Google Scholar] [CrossRef]
- Demura, S.; Sato, S.; Kitabayashi, T. Estimation of body density based on hydrostatic weighing without head submersion in young Japanese adults. J. Sports Sci. 2006, 24, 589–596. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Ambrosi, J.; Silva, C.; Catalán, V.; Rodríguez, A.; Galofré, J.C.; Escalada, J.; Valentí, V.; Rotellar, F.; Romero, S.; Ramírez, B.; et al. Clinical usefulness of a new equation for estimating body fat. Diabetes Care 2012, 35, 383–388. [Google Scholar] [CrossRef]
- Molina-Luque, R.; Yañez, A.M.; Bennasar-Veny, M.; Romero-Saldaña, M.; Molina-Recio, G.; López-González, Á.A. A Comparison of Equation Córdoba for Estimation of Body Fat (ECORE-BF) with Other Prediction Equations. Int. J. Environ. Res. Public Health 2020, 17, 7940. [Google Scholar] [CrossRef]
- Libby, P.; Ridker, P.M.; Hansson, G.K. Progress and challenges in translating the biology of atherosclerosis. Nature 2011, 473, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Corti, A.; Khalil, D.; De Paolis, A.; Cardoso, L. Size and proximity of micro-scale hard-inclusions increase the risk of rupture in fibroatheroma-like laboratory models. J. Mech. Behav. Biomed. Mater. 2023, 141, 105749. [Google Scholar] [CrossRef] [PubMed]
- Tragomalou, A.; Paltoglou, G.; Manou, M.; Kostopoulos, I.V.; Loukopoulou, S.; Binou, M.; Tsitsilonis, O.E.; Bacopoulou, F.; Kassari, P.; Papadopoulou, M.; et al. Non-Traditional Cardiovascular Risk Factors in Adolescents with Obesity and Metabolic Syndrome May Predict Future Cardiovascular Disease. Nutrients 2023, 15, 4342. [Google Scholar] [CrossRef] [PubMed]
- Csige, I.; Ujvárosy, D.; Szabó, Z.; Lőrincz, I.; Paragh, G.; Harangi, M.; Somodi, S. The Impact of Obesity on the Cardiovascular System. J. Diabetes Res. 2018, 2018, 3407306. [Google Scholar] [CrossRef] [PubMed]
- Safaei, M.; Sundararajan, E.A.; Driss, M.; Boulila, W.; Shapi’i, A. A systematic literature review on obesity: Understanding the causes & consequences of obesity and reviewing various machine learning approaches used to predict obesity. Comput. Biol. Med. 2021, 136, 104754. [Google Scholar]
- Obita, G.; Alkhatib, A. Effectiveness of Lifestyle Nutrition and Physical Activity Interventions for Childhood Obesity and Associated Comorbidities among Children from Minority Ethnic Groups: A Systematic Review and Meta-Analysis. Nutrients 2023, 15, 2524. [Google Scholar] [CrossRef] [PubMed]
- Melo, E.; Silva, F.V.; Almonfrey, F.B.; Freitas, C.M.N.; Fonte, F.K.; Sepulvida, M.B.C.; Almada-Filho, C.M.; Cendoroglo, M.S.; Quadrado, E.B.; Amodeo, C.; et al. Association of Body Composition with Arterial Stiffness in Long-lived People. Arq. Bras. Cardiol. 2021, 117, 457–462, (In English, Portuguese). [Google Scholar]
- Stewart, A.; Marfell-Jones, M.; Olds, T.; Ridder, H. International Standards for Anthropometric Assessment; International Society for the Advancement of Kinanthropometry—ISAK: Lower Hutt, New Zealand, 2011. [Google Scholar]
- WHO Expert Committee. Physical status: The use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech. Rep. Ser. 1995, 854, 312–344. [Google Scholar]
- NHLBI Obesity Education Initiative. The Practical Guide to the Identification, Evaluation and Treatment of Overweight and Obesity in Adults; NIH: Bethesda, MD, USA, 2000. [Google Scholar]
- Allain, C.C.; Poon, L.S.; Chan, C.S.; Richmond, W.; Fu, P.C. Enzymatic determination of total serum cholesterol. Clin. Chem. 1974, 20, 470–475. [Google Scholar] [CrossRef]
- Roeschlau, P.; Bernt, E.; Gruber, W. Enzymatic determination of total cholesterol in serum. Z. Klin. Chem. Klin. Biochem. 1974, 12, 226. [Google Scholar]
- Molina-Luque, R.; Romero-Saldaña, M.; Álvarez-Fernández, C.; Bennasar-Veny, M.; Álvarez-López, Á.; Molina-Recio, G. Equation Córdoba: A Simplified Method for Estimation of Body Fat (ECORE-BF). Int. J. Environ. Res. Public Health 2019, 16, 4529. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Manent, J.I.; Tomás-Gil, P.; Coll Villalonga, J.L.; Marti-Lliteras, P.; López-González, A.A.; Paublini, H. Association between atherogenic dyslipidemia and lipid triad with cardiovascular risk scales in 418.343 Spanish workers. Acad. J. Health Sci. 2024, 39, 9–15. [Google Scholar]
- Riutord-Sbert, P.; Riutord-Fe, B.; Riutord-Fe, N.; Arroyo-Bote, S.; López González, A.A.; Ramírez-Manent, J.I. Relationship between healthy habits and sociodemographic variables in the values of different atherogenic indices. Acad. J. Health Sci. 2022, 37, 22–27. [Google Scholar]
- Domingo-Salvany, A.; Bacigalupe, A.; Carrasco, J.M.; Espelt, A.; Ferrando, J.; Borrell, C. del Grupo de Determinantes Sociales de Sociedad Española de Epidemiología. Propuestas de clase social neoweberiana y neomarxista a partir de la Clasificación Nacional de Ocupaciones 2011. Gac. Sanit. 2013, 27, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Riutord-Sbert, P.; Riutord-Fe, B.; Riutord-Fe, N.; Arroyo-Bote, S.; López González, A.A.; Ramírez-Manent, J.I. Relationship between physical activity and adherence to the mediterranean diet with metabolic syndrome, hypertriglyceridemic waist phenotype and hypertensive waist. Acad. J. Health Sci. 2022, 37, 33–38. [Google Scholar]
- Vicente-Herrero, M.T.; Ramírez-Iñiguez, M.V.; Capdevila, L.; Partida-Hanon, A.; Reinoso-Barbero, L.; López González, A.A. Lifestyle, overweight and obesity in spanish workers: Related variables. Acad. J. Health Sci. 2022, 37, 135–143. [Google Scholar]
- Purnell, J.Q. What is Obesity?: Definition as a Disease, with Implications for Care. Gastroenterol. Clin. N. Am. 2023, 52, 261–275. [Google Scholar] [CrossRef]
- WHO. Available online: https://www.who.int/es/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 7 June 2024).
- Puljiz, Z.; Kumric, M.; Vrdoljak, J.; Martinovic, D.; Ticinovic Kurir, T.; Krnic, M.O.; Urlic, H.; Puljiz, Z.; Zucko, J.; Dumanic, P.; et al. Obesity, Gut Microbiota, and Metabolome: From Pathophysiology to Nutritional Interventions. Nutrients 2023, 15, 2236. [Google Scholar] [CrossRef]
- Guo, Y.; Yue, X.J.; Li, H.H.; Song, Z.X.; Yan, H.Q.; Zhang, P.; Gui, Y.K.; Chang, L.; Li, T. Overweight and Obesity in Young Adulthood and the Risk of Stroke: A Meta-analysis. J. Stroke Cerebrovasc. Dis. 2016, 25, 2995–3004. [Google Scholar] [CrossRef]
- Ye, J.; Hu, Y.; Chen, X.; Yin, Z.; Yuan, X.; Huang, L.; Li, K. Association between the weight-adjusted waist index and stroke: A cross-sectional study. BMC Public Health 2023, 23, 1689. [Google Scholar] [CrossRef]
- Katta, N.; Loethen, T.; Lavie, C.J.; Alpert, M.A. Obesity and Coronary Heart Disease: Epidemiology, Pathology, and Coronary Artery Imaging. Curr. Probl. Cardiol. 2021, 46, 100655. [Google Scholar] [CrossRef]
- Ren, J.; Wu, N.N.; Wang, S.; Sowers, J.R.; Zhang, Y. Obesity cardiomyopathy: Evidence, mechanisms, and therapeutic implications. Physiol. Rev. 2021, 101, 1745–1807. [Google Scholar] [CrossRef]
- Landsberg, L.; Aronne, L.J.; Beilin, L.J.; Burke, V.; Igel, L.I.; Lloyd-Jones, D.; Sowers, J. Obesity-related hypertension: Pathogenesis, cardiovascular risk, and treatment: A position paper of The Obesity Society and the American Society of Hypertension. J. Clin. Hypertens. 2013, 15, 14–33. [Google Scholar] [CrossRef]
- Cunha, C.L.P.D. Obesity-Induced Hypertension. Arq. Bras. Cardiol. 2023, 120, e20230391, (In English, Portuguese). [Google Scholar] [CrossRef] [PubMed]
- Suárez, R.; Chapela, S.P.; Álvarez-Córdova, L.; Bautista-Valarezo, E.; Sarmiento-Andrade, Y.; Verde, L.; Frias-Toral, E.; Sarno, G. Epigenetics in Obesity and Diabetes Mellitus: New Insights. Nutrients 2023, 15, 811. [Google Scholar] [CrossRef]
- Ruze, R.; Liu, T.; Zou, X.; Song, J.; Chen, Y.; Xu, R.; Yin, X.; Xu, Q. Obesity and type 2 diabetes mellitus: Connections in epidemiology, pathogenesis, and treatments. Front. Endocrinol. 2023, 14, 1161521. [Google Scholar] [CrossRef] [PubMed]
- Zang, B.Y.; He, L.X.; Xue, L. Intermittent Fasting: Potential Bridge of Obesity and Diabetes to Health? Nutrients 2022, 14, 981. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, B.; Sultana, R.; Greene, M.W. Adipose tissue and insulin resistance in obese. Biomed. Pharmacother. 2021, 137, 111315. [Google Scholar] [CrossRef] [PubMed]
- Vekic, J.; Stefanovic, A.; Zeljkovic, A. Obesity and Dyslipidemia: A Review of Current Evidence. Curr. Obes. Rep. 2023, 12, 207–222. [Google Scholar] [CrossRef] [PubMed]
- Nussbaumerova, B.; Rosolova, H. Obesity and Dyslipidemia. Curr. Atheroscler. Rep. 2023, 25, 947–955. [Google Scholar] [CrossRef]
- Silswal, N.; Singh, A.K.; Aruna, B.; Mukhopadhyay, S.; Ghosh, S.; Ehtesham, N.Z. Human resistin stimulates the pro-inflammatory cytokines TNF-alpha and IL-12 in macrophages by NF-kappaB-dependent pathway. Biochem. Biophys. Res. Commun. 2005, 334, 1092–1101. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.Y.; Kim, S.; Yang, S.J.; Yoo, H.J.; Seo, J.A.; Kim, S.G.; Kim, N.H.; Baik, S.H.; Choi, D.S.; Choi, K.M. Association of adiponectin, resistin, and vascular inflammation: Analysis with 18F-fluorodeoxyglucose positron emission tomography. Arterioscler. Thromb. Vasc. Biol. 2011, 31, 944–949. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.; Li, S.H.; Wang, C.H.; Fedak, P.W.; Li, R.K.; Weisel, R.D.; Mickle, D.A. Resistin promotes endothelial cell activation: Further evidence of adipokine-endothelial interaction. Circulation 2003, 108, 736–740, Erratum in Circulation 2004, 109, 2254. [Google Scholar] [CrossRef]
- Lopez-Yañez Blanco, A.; Díaz-López, K.M.; Vilchis-Gil, J.; Diaz-Garcia, H.; Gomez-Lopez, J.; Medina-Bravo, P.; Granados-Riveron, J.T.; Gallardo, J.M.; Klünder-Klünder, M.; Sánchez-Urbina, R. Diet and Maternal Obesity Are Associated with Increased Oxidative Stress in Newborns: A Cross-Sectional Study. Nutrients 2022, 14, 746. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Torres, I.; Castrejón-Téllez, V.; Soto, M.E.; Rubio-Ruiz, M.E.; Manzano-Pech, L.; Guarner-Lans, V. Oxidative Stress, Plant Natural Antioxidants, and Obesity. Int. J. Mol. Sci. 2021, 22, 1786. [Google Scholar] [CrossRef]
- Bonomini, F.; Rodella, L.F.; Rezzani, R. Metabolic syndrome, aging and involvement of oxidative stress. Aging Dis. 2015, 6, 109–120. [Google Scholar] [CrossRef]
- Miao, C.Y.; Li, Z.Y. The role of perivascular adipose tissue in vascular smooth muscle cell growth. Br. J. Pharmacol. 2012, 165, 643–658. [Google Scholar] [CrossRef]
- Kawai, T.; Autieri, M.V.; Scalia, R. Adipose tissue inflammation and metabolic dysfunction in obesity. Am. J. Physiol. Cell Physiol. 2021, 320, C375–C391. [Google Scholar] [CrossRef]
- Mehta, P.K.; Huang, J.; Levit, R.D.; Malas, W.; Waheed, N.; Bairey Merz, C.N. Ischemia and no obstructive coronary arteries (INOCA): A narrative review. Atherosclerosis 2022, 363, 8–21. [Google Scholar] [CrossRef]
- Virdis, A.; Santini, F.; Colucci, R.; Duranti, E.; Salvetti, G.; Rugani, I.; Segnani, C.; Anselmino, M.; Bernardini, N.; Blandizzi, C.; et al. Vascular generation of tumor necrosis factor-alpha reduces nitric oxide availability in small arteries from visceral fat of obese patients. J. Am. Coll. Cardiol. 2011, 58, 238–247. [Google Scholar] [CrossRef]
- Peña-Jorquera, H.; Cid-Jofré, V.; Landaeta-Díaz, L.; Petermann-Rocha, F.; Martorell, M.; Zbinden-Foncea, H.; Ferrari, G.; Jorquera-Aguilera, C.; Cristi-Montero, C. Plant-Based Nutrition: Exploring Health Benefits for Atherosclerosis, Chronic Diseases, and Metabolic Syndrome—A Comprehensive Review. Nutrients 2023, 15, 3244. [Google Scholar] [CrossRef] [PubMed]
- Zafar, U.; Khaliq, S.; Ahmad, H.U.; Manzoor, S.; Lone, K.P. Metabolic syndrome: An update on diagnostic criteria, pathogenesis, and genetic links. Hormones 2018, 17, 299–313. [Google Scholar] [CrossRef] [PubMed]
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 12. [Google Scholar] [CrossRef] [PubMed]
- Santulli, G.; Pascale, V.; Finelli, R.; Visco, V.; Giannotti, R.; Massari, A.; Morisco, C.; Ciccarelli, M.; Illario, M.; Iaccarino, G.; et al. We are What We Eat: Impact of Food from Short Supply Chain on Metabolic Syndrome. J. Clin. Med. 2019, 8, 2061. [Google Scholar] [CrossRef] [PubMed]
- Kesse-Guyot, E.; Ahluwalia, N.; Lassale, C.; Hercberg, S.; Fezeu, L.; Lairon, D. Adherence to Mediterranean diet reduces the risk of metabolic syndrome: A 6-year prospective study. Nutr. Metab. Cardiovasc. Dis. 2013, 23, 677–683. [Google Scholar] [CrossRef]
- Ahluwalia, N.; Andreeva, V.A.; Kesse-Guyot, E.; Hercberg, S. Dietary patterns, inflammation and the metabolic syndrome. Diabetes Metab. 2013, 39, 99–110. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Mistretta, A.; Marventano, S.; Purrello, A.; Vitaglione, P.; Calabrese, G.; Drago, F.; Galvano, F. Beneficial effects of the Mediterranean diet on metabolic syndrome. Curr. Pharm. Des. 2014, 20, 5039–5044. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Manent, J.I.; Belmonte Lomas, S.; Tárraga Marcos, L.; López-González, A.A.; Gordito Soler, M.; Tárraga López, P.J. Analysis of the efficacy of the main dietary patterns in reducing cardiovascular risk. Acad. J. Health Sci. 2023, 38, 153–170. [Google Scholar]
- Willeit, P.; Raschenberger, J.; Heydon, E.E.; Tsimikas, S.; Haun, M.; Mayr, A.; Weger, S.; Witztum, J.L.; Butterworth, A.S.; Willeit, J.; et al. Leucocyte telomere length and risk of type 2 diabetes mellitus: New prospective cohort study and literature-based meta-analysis. PLoS ONE 2014, 9, e112483. [Google Scholar] [CrossRef] [PubMed]
- Ojeda-Rodriguez, A.; Alcala-Diaz, J.F.; Rangel-Zuñiga, O.A.; Arenas-de Larriva, A.P.; Gutierrez-Mariscal, F.M.; Gómez-Luna, P.; Torres-Peña, J.D.; Garcia-Rios, A.; Romero-Cabrera, J.L.; Malagon, M.M.; et al. Association between telomere length and intima-media thickness of both common carotid arteries in patients with coronary heart disease: From the CORDIOPREV randomized controlled trial. Atherosclerosis 2023, 380, 117193. [Google Scholar] [CrossRef]
- Schneider, C.V.; Schneider, K.M.; Teumer, A.; Rudolph, K.L.; Hartmann, D.; Rader, D.J.; Strnad, P. Association of Telomere Length With Risk of Disease and Mortality. JAMA Intern. Med. 2022, 182, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Ojeda-Rodriguez, A.; Rangel-Zuñiga, O.A.; Arenas-de Larriva, A.P.; Gutierrez-Mariscal, F.M.; Torres-Peña, J.D.; Romero-Cabrera, J.L.; Podadera-Herreros, A.; García-Fernandez, H.; Porras-Pérez, E.; Luque, R.M.; et al. Telomere length as biomarker of nutritional therapy for prevention of type 2 diabetes mellitus development in patients with coronary heart disease: CORDIOPREV randomised controlled trial. Cardiovasc. Diabetol. 2024, 23, 98. [Google Scholar] [CrossRef] [PubMed]
- Ditano-Vázquez, P.; Torres-Peña, J.D.; Galeano-Valle, F.; Pérez-Caballero, A.I.; Demelo-Rodríguez, P.; Lopez-Miranda, J.; Katsiki, N.; Delgado-Lista, J.; Alvarez-Sala-Walther, L.A. The Fluid Aspect of the Mediterranean Diet in the Prevention and Management of Cardiovascular Disease and Diabetes: The Role of Polyphenol Content in Moderate Consumption of Wine and Olive Oil. Nutrients 2019, 11, 2833. [Google Scholar] [CrossRef] [PubMed]
- Guasch-Ferré, M.; Willett, W.C. The Mediterranean diet and health: A comprehensive overview. J. Intern. Med. 2021, 290, 549–566. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.X.; Deng, X.R.; Zhang, C.H.; Yuan, H.J. Gut microbiota and metabolic syndrome. Chin. Med. J. 2020, 133, 808–816. [Google Scholar] [CrossRef] [PubMed]
- Campaniello, D.; Corbo, M.R.; Sinigaglia, M.; Speranza, B.; Racioppo, A.; Altieri, C.; Bevilacqua, A. How Diet and Physical Activity Modulate Gut Microbiota: Evidence, and Perspectives. Nutrients 2022, 14, 2456. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Li, Q.; Wang, L.; Ding, H.; Wang, Y.; Liu, Y.; Gong, T. The interaction between oral microbiota and gut microbiota in atherosclerosis. Front. Cardiovasc. Med. 2024, 11, 1406220. [Google Scholar] [CrossRef] [PubMed]
- Korakas, E.; Dimitriadis, G.; Raptis, A.; Lambadiari, V. Dietary Composition and Cardiovascular Risk: A Mediator or a Bystander? Nutrients 2018, 10, 1912. [Google Scholar] [CrossRef] [PubMed]
- Williams, K.J. Eradicating Atherosclerotic Events by Targeting Early Subclinical Disease: It Is Time to Retire the Therapeutic Paradigm of Too Much, Too Late. Arterioscler. Thromb. Vasc. Biol. 2024, 44, 48–64. [Google Scholar] [CrossRef]
- Laclaustra, M.; Casasnovas, J.A.; Fernández-Ortiz, A.; Fuster, V.; León-Latre, M.; Jiménez-Borreguero, L.J.; Pocovi, M.; Hurtado-Roca, Y.; Ordovas, J.M.; Jarauta, E.; et al. Femoral and Carotid Subclinical Atherosclerosis Association with Risk Factors and Coronary Calcium: The AWHS Study. J. Am. Coll. Cardiol. 2016, 67, 1263–1274. [Google Scholar] [CrossRef]
- Bergström, G.; Persson, M.; Adiels, M.; Björnson, E.; Bonander, C.; Ahlström, H.; Alfredsson, J.; Angerås, O.; Berglund, G.; Blomberg, A.; et al. Prevalence of Subclinical Coronary Artery Atherosclerosis in the General Population. Circulation 2021, 144, 916–929. [Google Scholar] [CrossRef]
- Bentzon, J.F.; Otsuka, F.; Virmani, R.; Falk, E. Mechanisms of plaque formation and rupture. Circ. Res. 2014, 114, 1852–1866. [Google Scholar] [CrossRef] [PubMed]
- Rojo-López, M.I.; Bermúdez-López, M.; Castro, E.; Farràs, C.; Torres, G.; Pamplona, R.; Lecube, A.; Valdivielso, J.M.; Fernández, E.; Julve, J.; et al. Low adherence to the Mediterranean diet is associated with increased prevalence and number of atherosclerotic plaques in the ILERVAS cohort. Atherosclerosis 2023, 380, 117191. [Google Scholar] [CrossRef] [PubMed]
- Determinantes de Salud (Consumo de Tabaco, Exposición Pasiva al Humo de Tabaco, Alcohol, Problemas Medioambientales en la Vivienda). Available online: https://www.ine.es/ss/Satellite?L=es_ES&c=INESeccion_C&cid=1259926698156&p=1254735110672&pagename=ProductosYServicios/PYSLayout (accessed on 12 June 2024).
- INEbase/Indicadores de Calidad de Vida. Available online: https://www.ine.es/jaxi/Datos.htm?path=/t00/ICV/dim3/l0/&file=33201.px (accessed on 12 June 2024).
- INEbase/Indicadores de Calidad de Vida. Available online: https://www.ine.es/jaxi/Datos.htm?path=/t00/ICV/dim3/&file=33303.px (accessed on 12 June 2024).
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086, Erratum in Lancet Glob. Health 2019, 7, e36. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Yan, J.; Zhao, Y. A Trend Analysis of Adherence to the Muscle Strengthening Exercise Guidelines in US Adolescents. Int. J. Public Health 2022, 67, 1605022. [Google Scholar] [CrossRef] [PubMed]
- Ji, H.; Gulati, M.; Huang, T.Y.; Kwan, A.C.; Ouyang, D.; Ebinger, J.E.; Casaletto, K.; Moreau, K.L.; Skali, H.; Cheng, S. Sex Differences in Association of Physical Activity with All-Cause and Cardiovascular Mortality. J. Am. Coll. Cardiol. 2024, 83, 783–793. [Google Scholar] [CrossRef] [PubMed]
- Candás-Estébanez, B.; Fernández-Cidón, B.; Corbella, E.; Tebé, C.; Fanlo-Maresma, M.; Esteve-Luque, V.; Salas-Salvadó, J.; Fitó, M.; Riera-Mestre, A.; Ros, E.; et al. The Impact of the Mediterranean Diet and Lifestyle Intervention on Lipoprotein Subclass Profiles among Metabolic Syndrome Patients: Findings of a Randomized Controlled Trial. Int. J. Mol. Sci. 2024, 25, 1338. [Google Scholar] [CrossRef] [PubMed]
- Sayón-Orea, C.; Razquin, C.; Bulló, M.; Corella, D.; Fitó, M.; Romaguera, D.; Vioque, J.; Alonso-Gómez, Á.M.; Wärnberg, J.; Martínez, J.A.; et al. Effect of a Nutritional and Behavioral Intervention on Energy-Reduced Mediterranean Diet Adherence Among Patients with Metabolic Syndrome: Interim Analysis of the PREDIMED-Plus Randomized Clinical Trial. JAMA 2019, 322, 1486–1499. [Google Scholar] [CrossRef]
- Zhang, J.S.; Yeh, W.C.; Tsai, Y.W.; Chen, J.Y. The Relationship between Atherogenic Index of Plasma and Obesity among Adults in Taiwan. Int. J. Environ. Res. Public Health 2022, 19, 14864. [Google Scholar] [CrossRef]
- Zhu, X.; Yu, L.; Zhou, H.; Ma, Q.; Zhou, X.; Lei, T.; Hu, J.; Xu, W.; Yi, N.; Lei, S. Atherogenic index of plasma is a novel and better biomarker associated with obesity: A population-based cross-sectional study in China. Lipids Health Dis. 2018, 17, 37. [Google Scholar] [CrossRef]
- Göğebakan, H.; Kaşali, K. The correlation of plasma atherogenic index and obesity in patients with familial Mediterranean fever. Clin. Rheumatol. 2022, 41, 3471–3477. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.R.; Song, S.; Cho, J.A.; Ly, S.Y. Atherogenic Index of Plasma and Its Association with Risk Factors of Coronary Artery Disease and Nutrient Intake in Korean Adult Men: The 2013-2014 KNHANES. Nutrients 2022, 14, 1071. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.J.; Yoon, J.; Lee, Y.J.; Park, B.; Jung, D.H. Predictive Value of the Atherogenic Index of Plasma (AIP) for the Risk of Incident Ischemic Heart Disease among Non-Diabetic Koreans. Nutrients 2021, 13, 3231. [Google Scholar] [CrossRef] [PubMed]

| Men n = 232,814 | Women n = 154,110 | ||
|---|---|---|---|
| Mean (SD) | Mean (SD) | p-Value (t-Student) | |
| Age (years) | 39.8 (10.3) | 39.2 (10.2) | <0.001 |
| Height (cm) | 173.9 (7.0) | 161.2 (6.6) | <0.001 |
| Weight (kg) | 81.1 (13.9) | 65.3 (13.2) | <0.001 |
| Waist circumference (cm) | 87.7 (9.1) | 73.9 (7.9) | <0.001 |
| Hip circumference (cm) | 100.0 (8.4) | 97.2 (8.9) | <0.001 |
| Systolic blood pressure (mmHg) | 124.4 (15.1) | 114.4 (14.8) | <0.001 |
| Diastolic blood pressure (mmHg) | 75.4 (10.6) | 69.7 (10.3) | <0.001 |
| Total cholesterol (mg/dL) | 195.9 (38.9) | 193.6 (36.4) | <0.001 |
| HDL-c (mg/dL) | 51.0 (7.0) | 53.7 (7.6) | <0.001 |
| LDL-c (mg/dL) | 120.5 (37.6) | 122.3 (37.0) | <0.001 |
| Triglycerides (mg/dL) | 123.8 (88.0) | 88.1 (46.2) | <0.001 |
| Glycaemia (mg/dL) | 88.1 (12.9) | 84.1 (11.5) | <0.001 |
| % | % | p-Value (Chi-Square) | |
| 20–29 years | 17.9 | 19.5 | <0.001 |
| 30–39 years | 33.1 | 33.3 | |
| 40–49 years | 29.7 | 29.4 | |
| 50–59 years | 16.3 | 15.3 | |
| 60–69 years | 3.0 | 2.5 | |
| Primary school | 61.2 | 51.8 | <0.001 |
| Secondary school | 34.0 | 40.7 | |
| University | 4.8 | 7.5 | |
| Social class I | 5.3 | 7.2 | <0.001 |
| Social class II | 17.4 | 33.2 | |
| Social class III | 77.3 | 59.8 | |
| No physical activity | 54.5 | 47.8 | <0.001 |
| Yes physical activity | 45.5 | 52.2 | |
| Non Mediterranean diet | 59.0 | 48.6 | <0.001 |
| Yes Mediterranean diet | 41.0 | 51.4 | |
| Non-smokers | 62.9 | 67.0 | <0.001 |
| Smokers | 37.1 | 33.0 |
| Men | Women | |||||
|---|---|---|---|---|---|---|
| n | Mean (SD) | p-Value (t-Student) | n | Mean (SD) | p-Value (t-Student) | |
| Non AD | 221,582 | 25.4 (5.9) | <0.001 | 150,406 | 34.8 (6.9) | <0.001 |
| AD | 11,232 | 29.5 (5.4) | 3704 | 41.1 (6.6) | ||
| Non LT | 228,166 | 25.5 (5.9) | <0.001 | 152,030 | 34.9 (7.0) | <0.001 |
| LT | 4648 | 28.7 (5.2) | 2080 | 40.7 (6.6) | ||
| Low TC/HDL-c | 199,038 | 25.1 (5.9) | <0.001 | 122,908 | 34.3 (6.9) | <0.001 |
| Moderate TC/HDL-c | 33,182 | 28.5 (5.3) | 301,54 | 37.7 (6.7) | ||
| High TC/HDL-c | 594 | 29.4 (4.5) | 1048 | 38.8 (6.2) | ||
| Low LDL-c/HL-c | 176,954 | 24.9 (5.9) | <0.001 | 119,746 | 34.3 (7.0) | <0.001 |
| High LDL-c/HL-c | 55,860 | 27.7 (5.3) | 34,364 | 37.3 (6.6) | ||
| Low triglycerides/HDL-c | 175,926 | 24.6 (5.7) | <0.001 | 141,372 | 34.5 (6.8) | <0.001 |
| High triglycerides/HDL-c | 56,888 | 28.6 (5.4) | 12,738 | 40.2 (6.9) |
| Men | Women | |||||
|---|---|---|---|---|---|---|
| n | % | p-Value (Chi-Square) | n | % | p-Value (Chi-Square) | |
| Non AD | 221,582 | 51.4 | <0.001 | 150,406 | 44.2 | <0.001 |
| AD | 11,232 | 79.6 | 3704 | 81.4 | ||
| Non LT | 228,166 | 52.3 | <0.001 | 152,030 | 44.6 | <0.001 |
| LT | 4648 | 75.0 | 2080 | 79.6 | ||
| Low TC/HDL-c | 199,038 | 48.9 | <0.001 | 122,908 | 40.6 | <0.001 |
| Moderate TC/HDL-c | 33,182 | 75.3 | 30,154 | 62.4 | ||
| High TC/HDL-c | 594 | 83.8 | 1048 | 71.8 | ||
| Low LDL-c/HL-c | 176,954 | 47.6 | <0.001 | 119,746 | 40.8 | <0.001 |
| High LDL-c/HL-c | 55,860 | 69.1 | 34,364 | 60.1 | ||
| Low triglycerides/HDL-c | 175,926 | 45.6 | <0.001 | 141,372 | 42.3 | <0.001 |
| High triglycerides/HDL-c | 56,888 | 74.9 | 12,738 | 76.8 |
| Women | AUC (95% CI) | Cut-off-Sensitivity-Specificity-Youden |
|---|---|---|
| Atherogenic dyslipidemia | 0.803 (0.798–0.808) | 39.0-73.8-73.8-0.476 |
| Lipid triad | 0.797 (0.787–0.806) | 39.1-73.3-73.3-0.466 |
| High total cholesterol/HDL-c | 0.733 (0.723–0.743) | 39.0-70.3-70.6-0.414 |
| High triglycerides/HDL-c | 0.760 (0.755–0.764) | 38.0-70.2-70.2-0.404 |
| High LDL-c/HDL-c | 0.706 (0.702–0.710) | 38.0-69.2-69.1-0.383 |
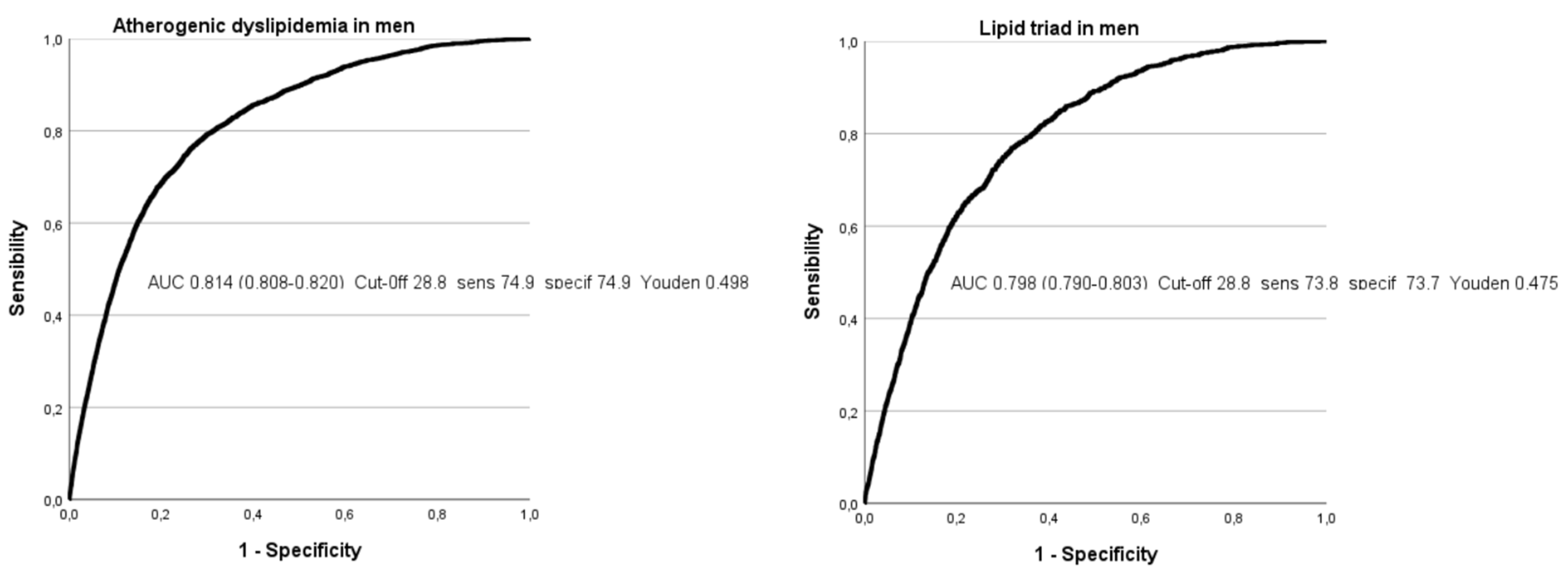
| Men | AUC (95% CI) | Cut-off-Sensitivity-Specificity-Youden |
| Atherogenic dyslipidemia | 0.812 (0.809–0.815) | 28.7-74.8-74.8-0.496 |
| Lipid triad | 0.798 (0.792–0.803) | 28.8-73.8-73.7-0.475 |
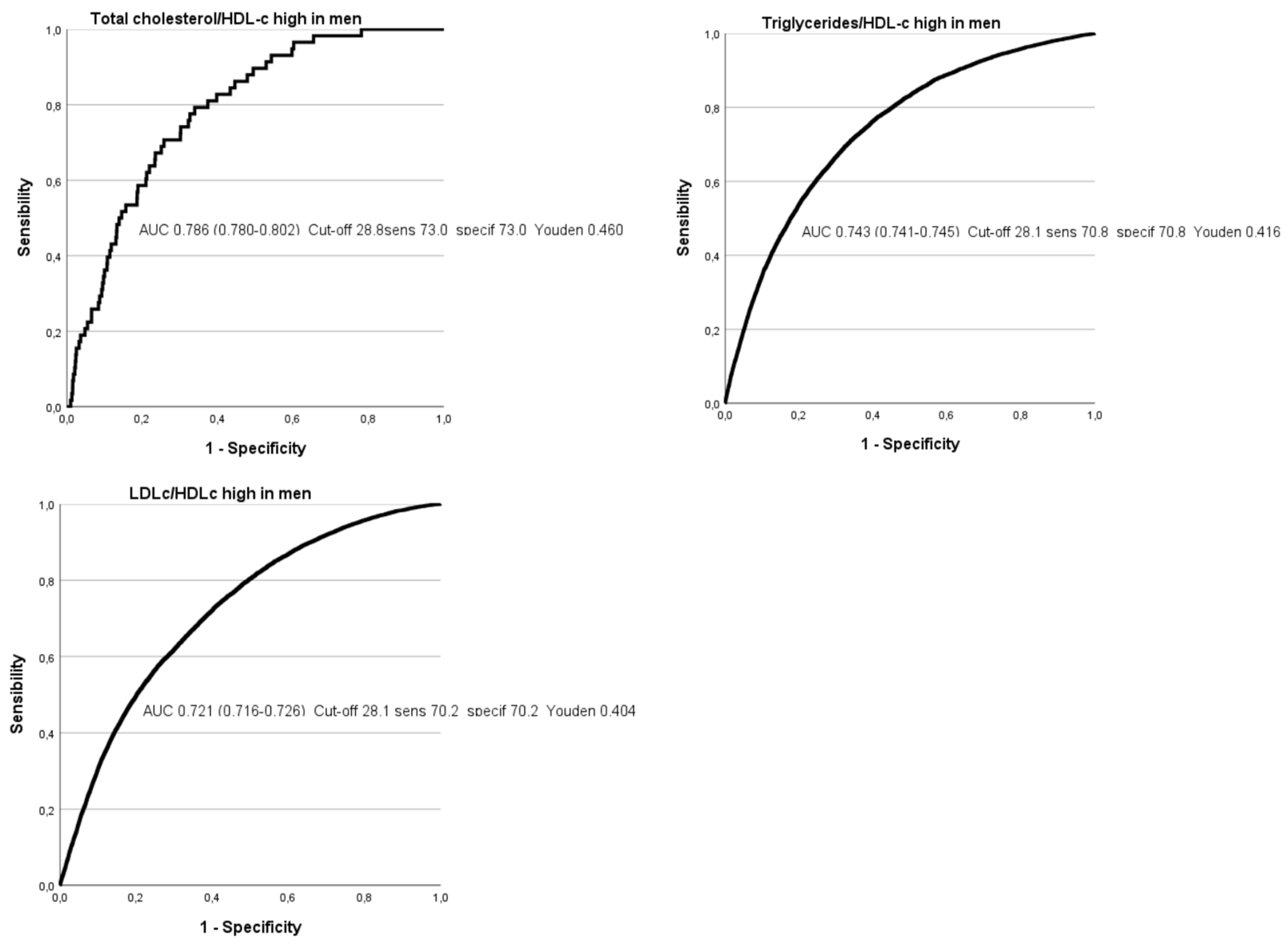
| High total cholesterol/HDL-c | 0.744 (0.720–0.769) | 28.1-70.9-70.9-0.418 |
| High triglycerides/HDL-c | 0.743 (0.741–0.745) | 28.1-70.8-70.8-0.416 |
| High LDL-c/HDL-c | 0.716 (0.714–0.719) | 28.0-69.9-69.8-0.397 |
| Atherogenic Dyslipidemia | Lipid Triad | High Total Cholesterol/HDL-c | High LDL-c/HDL-c | High Triglycerides/HDL-c | |
|---|---|---|---|---|---|
| Atherogenic dyslipidemia | 1 | 0.612 | 0.102 | 0.183 | 0.309 |
| Lipid triad | 1 | 0.182 | 0.110 | 0.149 | |
| High total cholesterol/HDL-c | 1 | 0.026 | 0.035 | ||
| High LDL-c/HDL-c | 1 | 0.204 | |||
| High triglycerides/HDL-c | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marina Arroyo, M.; Ramírez Gallegos, I.; López-González, Á.A.; Vicente-Herrero, M.T.; Vallejos, D.; Sastre-Alzamora, T.; Ramírez Manent, J.I. Usefulness of the ECORE-BF Scale to Determine Atherogenic Risk in 386,924 Spanish Workers. Nutrients 2024, 16, 2434. https://doi.org/10.3390/nu16152434
Marina Arroyo M, Ramírez Gallegos I, López-González ÁA, Vicente-Herrero MT, Vallejos D, Sastre-Alzamora T, Ramírez Manent JI. Usefulness of the ECORE-BF Scale to Determine Atherogenic Risk in 386,924 Spanish Workers. Nutrients. 2024; 16(15):2434. https://doi.org/10.3390/nu16152434
Chicago/Turabian StyleMarina Arroyo, Marta, Ignacio Ramírez Gallegos, Ángel Arturo López-González, María Teófila Vicente-Herrero, Daniela Vallejos, Tomás Sastre-Alzamora, and José Ignacio Ramírez Manent. 2024. "Usefulness of the ECORE-BF Scale to Determine Atherogenic Risk in 386,924 Spanish Workers" Nutrients 16, no. 15: 2434. https://doi.org/10.3390/nu16152434
APA StyleMarina Arroyo, M., Ramírez Gallegos, I., López-González, Á. A., Vicente-Herrero, M. T., Vallejos, D., Sastre-Alzamora, T., & Ramírez Manent, J. I. (2024). Usefulness of the ECORE-BF Scale to Determine Atherogenic Risk in 386,924 Spanish Workers. Nutrients, 16(15), 2434. https://doi.org/10.3390/nu16152434







