Effects of Very Low-Calorie Diet versus Roux-en-Y Gastric Bypass Surgery on Body Composition in Patients with Obesity
Abstract
1. Introduction
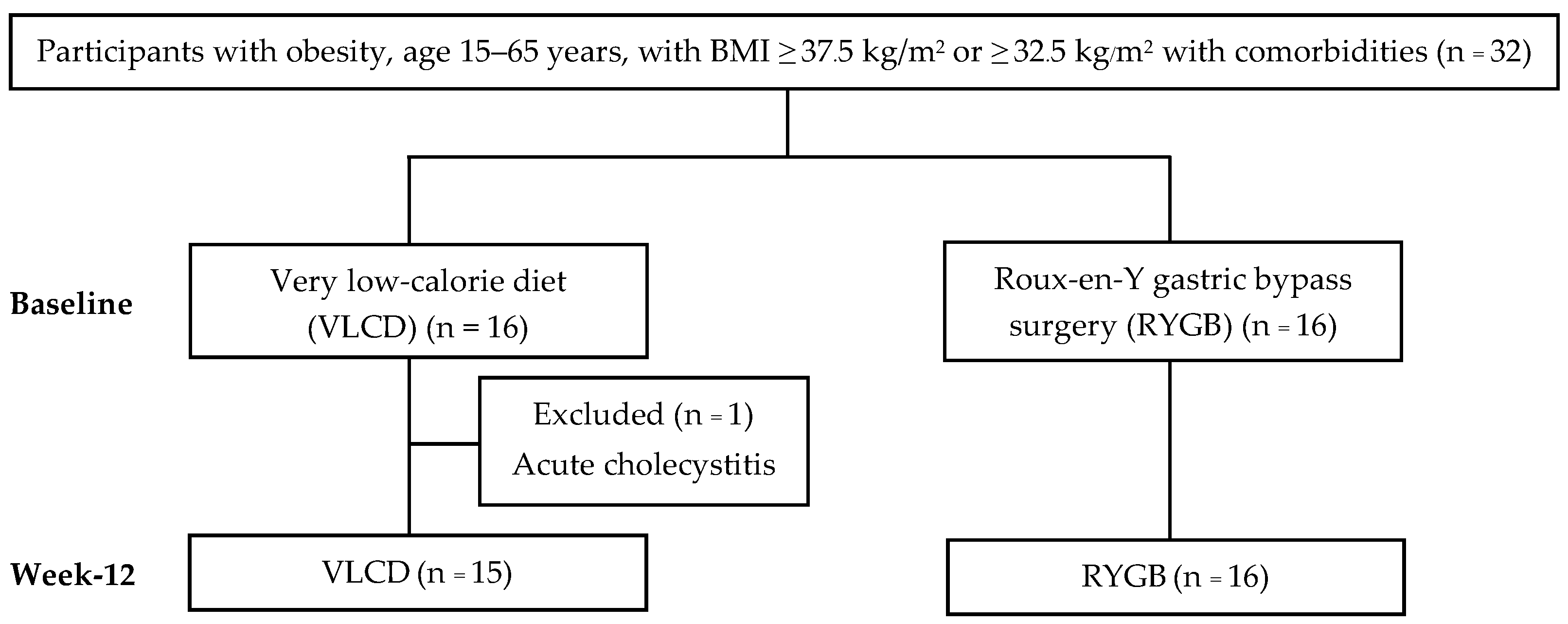
2. Materials and Methods
2.1. Participants
2.2. Intervention
2.2.1. Very Low-Calorie Diet Group
2.2.2. Roux-en-Y Gastric Bypass Group
2.3. Weight and Body Composition Measurements
2.4. Dietary Assessment and Blood Chemistry Measurement
2.5. Diabetes Remission
2.6. Statistical Analysis
3. Results
3.1. Characterization of the Participants
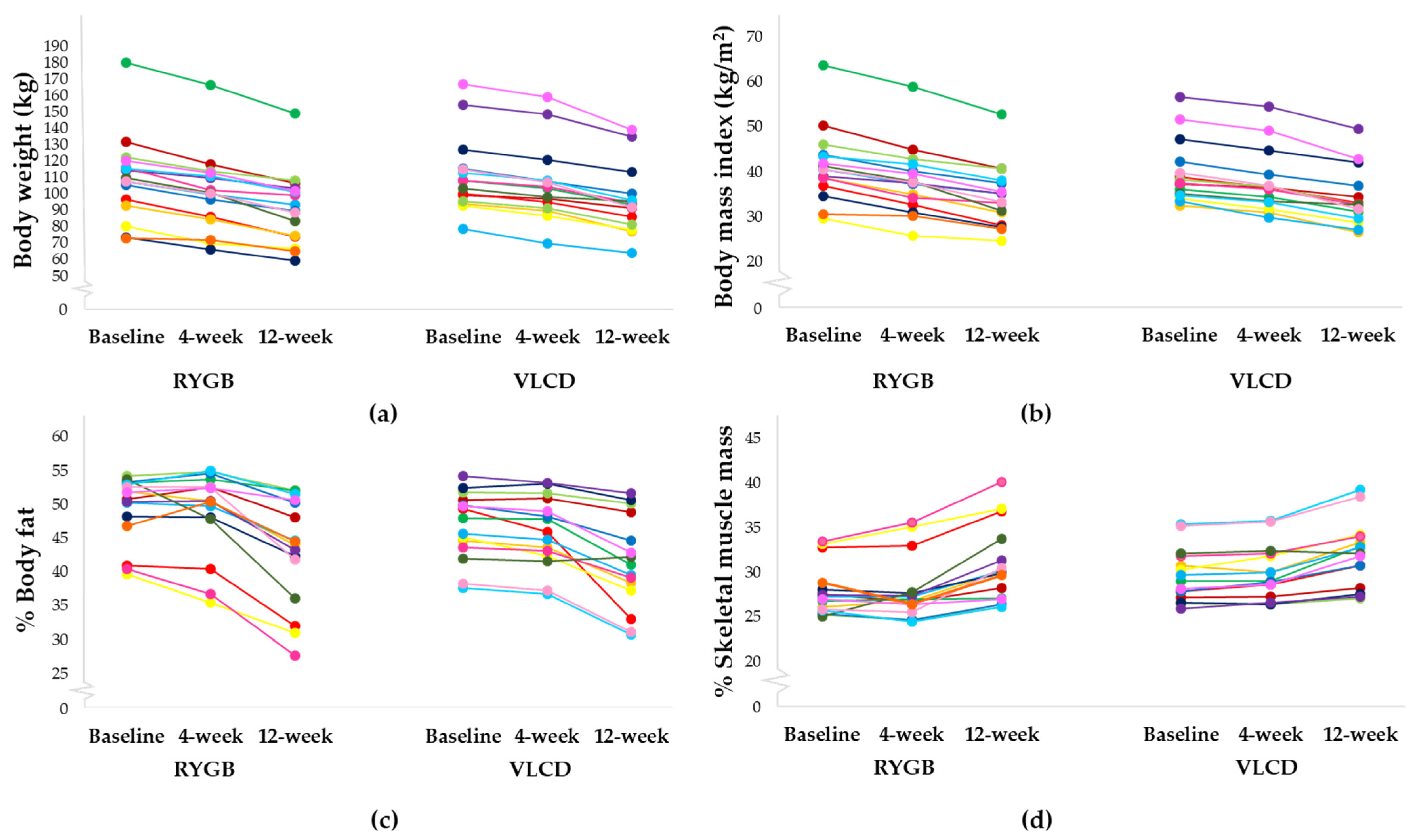
3.2. Study Endpoints
3.3. Adverse Events
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sbraccia, P.; Dicker, D. Obesity is a chronic progressive relapsing disease of particular interest for internal medicine. Intern. Emerg. Med. 2023, 18, 1–5. [Google Scholar] [CrossRef]
- Blüher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef] [PubMed]
- WHO. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 28 March 2024).
- Aekplakorn, W.; Puckcharern, H.; Satheannoppakao, W. Thai National Health Examination Survey VI (2019–2020); Faculty of Medicine Ramathibodi Hospital, Mahidol University: Bangkok, Thailand, 2021; p. 172. [Google Scholar]
- Magro, D.O.; Ueno, M.; de Souza Coelho-Neto, J.; Callejas-Neto, F.; Pareja, J.C.; Cazzo, E. Long-term weight loss outcomes after banded Roux-en-Y gastric bypass: A prospective 10-year follow-up study. Surg. Obes. Relat. Dis. 2018, 14, 910–917. [Google Scholar] [CrossRef] [PubMed]
- Eghbali, F.; Bahardoust, M.; Pazouki, A.; Barahman, G.; Tizmaghz, A.; Hajmohammadi, A.; Karami, R.; Hosseini-Baharanchi, F.S. Predictors for weight loss after Roux-en-Y gastric bypass: The trend and associated factors for weight loss. BMC Surg. 2022, 22, 310. [Google Scholar] [CrossRef] [PubMed]
- Madsen, L.R.; Baggesen, L.M.; Richelsen, B.; Thomsen, R.W. Effect of Roux-en-Y gastric bypass surgery on diabetes remission and complications in individuals with type 2 diabetes: A Danish population-based matched cohort study. Diabetologia 2019, 62, 611–620. [Google Scholar] [CrossRef] [PubMed]
- Balasubaramaniam, V.; Pouwels, S. Remission of type 2 diabetes mellitus (T2DM) after sleeve gastrectomy (SG), one-anastomosis gastric bypass (OAGB), and Roux-en-Y gastric bypass (RYGB): A systematic review. Medicina 2023, 59, 985. [Google Scholar] [CrossRef] [PubMed]
- Salem, V.; Demetriou, L.; Behary, P.; Alexiadou, K.; Scholtz, S.; Tharakan, G.; Miras, A.D.; Purkayastha, S.; Ahmed, A.R.; Bloom, S.R. Weight loss by low-calorie diet versus gastric bypass surgery in people with diabetes results in divergent brain activation patterns: A functional MRI study. Diabetes Care 2021, 44, 1842–1851. [Google Scholar] [CrossRef] [PubMed]
- Lips, M.A.; van Klinken, J.B.; Pijl, H.; Janssen, I.; van Dijk, K.W.; Koning, F.; van Harmelen, V. Weight loss induced by very low calorie diet is associated with a more beneficial systemic inflammatory profile than by Roux-en-Y gastric bypass. Metabolism 2016, 65, 1614–1620. [Google Scholar] [CrossRef]
- Umphonsathien, M.; Prutanopajai, P.; Aiam-O-Ran, J.; Thararoop, T.; Karin, A.; Kanjanapha, C.; Jiamjarasrangsi, W.; Khovidhunkit, W. Immediate and long-term effects of a very-low-calorie diet on diabetes remission and glycemic control in obese Thai patients with type 2 diabetes mellitus. Food Sci. Nutr. 2019, 7, 1113–1122. [Google Scholar] [CrossRef]
- Gow, M.L.; Pham-Short, A.; Jebeile, H.; Varley, B.J.; Craig, M.E. Current perspectives on the role of very-low-energy diets in the treatment of obesity and type 2 diabetes in youth. Diabetes Metab. Syndr. Obes. 2021, 14, 215–225. [Google Scholar] [CrossRef]
- Faria, S.L.; Faria, O.P.; de Almeida Cardeal, M.; Ito, M.K. Effects of a very low calorie diet in the preoperative stage of bariatric surgery: A randomized trial. Surg. Obes. Relat. Dis. 2015, 11, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Van Nieuwenhove, Y.; Dambrauskas, Z.; Campillo-Soto, A.; Van Dielen, F.; Wiezer, R.; Janssen, I.; Kramer, M.; Thorell, A. Preoperative very low-calorie diet and operative outcome after laparoscopic gastric bypass: A randomized multicenter study. Arch. Surg. 2011, 146, 1300–1305. [Google Scholar] [CrossRef] [PubMed]
- Cassie, S.; Menezes, C.; Birch, D.W.; Shi, X.; Karmali, S. Effect of preoperative weight loss in bariatric surgical patients: A systematic review. Surg. Obes. Relat. Dis. 2011, 7, 760–767. [Google Scholar] [CrossRef]
- Hocking, S.L.; Markovic, T.P.; Lee, C.M.; Picone, T.J.; Gudorf, K.E.; Colagiuri, S. Intensive lifestyle intervention for remission of early type 2 diabetes in primary care in Australia: DiRECT-Aus. Diabetes Care 2024, 47, 66–70. [Google Scholar] [CrossRef] [PubMed]
- Ard, J.D.; Lewis, K.H.; Rothberg, A.; Auriemma, A.; Coburn, S.L.; Cohen, S.S.; Loper, J.; Matarese, L.; Pories, W.J.; Periman, S. Effectiveness of a total meal replacement program (OPTIFAST program) on weight loss: Results from the OPTIWIN study. Obesity 2019, 27, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Lean, M.E.; Leslie, W.S.; Barnes, A.C.; Brosnahan, N.; Thom, G.; McCombie, L.; Peters, C.; Zhyzhneuskaya, S.; Al-Mrabeh, A.; Hollingsworth, K.G. Primary care-led weight management for remission of type 2 diabetes (DiRECT): An open-label, cluster-randomised trial. Lancet 2018, 391, 541–551. [Google Scholar] [CrossRef]
- Taheri, S.; Zaghloul, H.; Chagoury, O.; Elhadad, S.; Ahmed, S.H.; El Khatib, N.; Abou Amona, R.; El Nahas, K.; Suleiman, N.; Alnaama, A. Effect of intensive lifestyle intervention on bodyweight and glycaemia in early type 2 diabetes (DIADEM-I): An open-label, parallel-group, randomised controlled trial. Lancet Diabetes Endocrinol. 2020, 8, 477–489. [Google Scholar] [CrossRef] [PubMed]
- Parrott, J.; Frank, L.; Rabena, R.; Craggs-Dino, L.; Isom, K.A.; Greiman, L. American Society for Metabolic and Bariatric Surgery integrated health nutritional guidelines for the surgical weight loss patient 2016 update: Micronutrients. Surg. Obes. Relat. Dis. 2017, 13, 727–741. [Google Scholar] [CrossRef]
- Mechanick, J.; Apovian, C.; Brethauer, S. AACE/TOS/ASMBS/OMA/ASA 2019 Guidelines; clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures–2019 update: Cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic & Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Endocr. Pract. 2019, 25, 1346–1359. [Google Scholar] [CrossRef]
- O’Kane, M.; Parretti, H.M.; Pinkney, J.; Welbourn, R.; Hughes, C.A.; Mok, J.; Walker, N.; Thomas, D.; Devin, J.; Coulman, K.D. British Obesity and Metabolic Surgery Society Guidelines on perioperative and postoperative biochemical monitoring and micronutrient replacement for patients undergoing bariatric surgery—2020 update. Obes. Rev. 2020, 21, e13087. [Google Scholar] [CrossRef]
- Riddle, M.C.; Cefalu, W.T.; Evans, P.H.; Gerstein, H.C.; Nauck, M.A.; Oh, W.K.; Rothberg, A.E.; le Roux, C.W.; Rubino, F.; Schauer, P. Consensus report: Definition and interpretation of remission in type 2 diabetes. J. Clin. Endocrinol. Metab. 2022, 107, 1–9. [Google Scholar] [CrossRef]
- Herrington, G.J.; Peterson, J.J.; Cheng, L.; Allington, B.M.; Jensen, R.D.; Healy, H.S.; Correia, M.L. The use of very low-calorie diets in subjects with obesity complicated with nonalcoholic fatty liver disease: A scoping review. Obes. Sci. Pract. 2022, 8, 510–524. [Google Scholar] [CrossRef]
- Holderbaum, M.; Casagrande, D.S.; Sussenbach, S.; Buss, C. Effects of very low calorie diets on liver size and weight loss in the preoperative period of bariatric surgery: A systematic review. Surg. Obes. Relat. Dis. 2018, 14, 237–244. [Google Scholar] [CrossRef]
- Edholm, D.; Kullberg, J.; Karlsson, F.A.; Haenni, A.; Ahlström, H.; Sundbom, M. Changes in liver volume and body composition during 4 weeks of low calorie diet before laparoscopic gastric bypass. Surg. Obes. Relat. Dis. 2015, 11, 602–606. [Google Scholar] [CrossRef]
- Wing, R.R.; Marcus, M.D.; Salata, R.; Epstein, L.H.; Miaskiewicz, S.; Blair, E.H. Effects of a very-low-calorie diet on long-term glycemic control in obese type 2 diabetic subjects. Arch. Intern. Med. 1991, 151, 1334–1340. [Google Scholar] [CrossRef]
- Deshpande, N.; Mamata, A.; Parmaj, R.; Agarwal, S.; Sarda, A.; Bhatt, A.; Joshi, S.; Kapoor, N. The immediate impact of a balanced, very low-calorie diet on the metabolic health of Indian subjects-A prospective longitudinal study. Clin. Epidemiol. Glob. Health 2023, 24, 101397. [Google Scholar] [CrossRef]
- Lean, M.E.; Leslie, W.S.; Barnes, A.C.; Brosnahan, N.; Thom, G.; McCombie, L.; Peters, C.; Zhyzhneuskaya, S.; Al-Mrabeh, A.; Hollingsworth, K.G. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol. 2019, 7, 344–355. [Google Scholar] [CrossRef]
- Khemtong, A.; Shantavasinkul, P.C.; Boonchaya-Anant, P.; Rattanasiri, S.; Treeprasertsuk, S.; Udomsawaengsup, S. Effect of Preoperative Very Low-Calorie Diets on Hepatic Steatosis, Fibrosis, and Perioperative Outcomes of Bariatric Surgery. J. Laparoendosc. Adv. Surg. Tech. 2024, 34, 219–226. [Google Scholar] [CrossRef]
- Janssen, T.A.H.; Van Every, D.W.; Phillips, S.M. The impact and utility of very low-calorie diets: The role of exercise and protein in preserving skeletal muscle mass. Curr. Opin. Clin. Nutr. Metab. Care 2023, 26, 521–527. [Google Scholar] [CrossRef]
- Pekkarinen, T.; Mustaioki, P. Use of very low-calorie diet in preoperative weight loss: Efficacy and safety. Obes. Res. 1997, 5, 595–602. [Google Scholar] [CrossRef]
- le Roux, C.W.; Welbourn, R.; Werling, M.; Osborne, A.; Kokkinos, A.; Laurenius, A.; Lönroth, H.; Fändriks, L.; Ghatei, M.A.; Bloom, S.R. Gut hormones as mediators of appetite and weight loss after Roux-en-Y gastric bypass. Ann. Surg. 2007, 246, 780–785. [Google Scholar] [CrossRef]
- Morínigo, R.; Moizé, V.; Musri, M.; Lacy, A.M.; Navarro, S.; Marín, J.L.; Delgado, S.; Casamitjana, R.; Vidal, J. Glucagon-like peptide-1, peptide YY, hunger, and satiety after gastric bypass surgery in morbidly obese subjects. J. Clin. Endocrinol. Metab. 2006, 91, 1735–1740. [Google Scholar] [CrossRef]
- Batterham, R.L.; Cummings, D.E. Mechanisms of diabetes improvement following bariatric/metabolic surgery. Diabetes Care 2016, 39, 893–901. [Google Scholar] [CrossRef]
- Giusti, V.; Theytaz, F.; Di Vetta, V.; Clarisse, M.; Suter, M.; Tappy, L. Energy and macronutrient intake after gastric bypass for morbid obesity: A 3-y observational study focused on protein consumption. Am. J. Clin. Nutr. 2016, 103, 18–24. [Google Scholar] [CrossRef]
- Shantavasinkul, P.C.; Omotosho, P.; Muehlbauer, M.J.; Natoli, M.; Corsino, L.; Tong, J.; Portenier, D.; Torquati, A. Metabolic profiles, energy expenditures, and body compositions of the weight regain versus sustained weight loss patients who underwent Roux-en-Y gastric bypass. Surg. Obes. Relat. Dis. 2021, 17, 2015–2025. [Google Scholar] [CrossRef]
- Shantavasinkul, P.C.; Omotosho, P.; Corsino, L.; Portenier, D.; Torquati, A. Predictors of weight regain in patients who underwent Roux-en-Y gastric bypass surgery. Surg. Obes. Relat. Dis. 2016, 12, 1640–1645. [Google Scholar] [CrossRef]
- Abdulsalam, F.; Ali, H.I.; Altinoz, A.; Nimeri, A. The effect of protein consumption on fat-free mass, fat mass, and weight loss 1 year after sleeve gastrectomy and Roux-en-Y gastric bypass. Obes. Surg. 2021, 31, 4741–4748. [Google Scholar] [CrossRef]
- Bertoni, L.; Valentini, R.; Zattarin, A.; Belligoli, A.; Bettini, S.; Vettor, R.; Foletto, M.; Spinella, P.; Busetto, L. Assessment of protein intake in the first three months after sleeve gastrectomy in patients with severe obesity. Nutrients 2021, 13, 771. [Google Scholar] [CrossRef]
- Carels, R.A.; Selensky, J.C.; Rossi, J.; Solar, C.; Hlavka, R. A novel stepped-care approach to weight loss: The role of self-monitoring and health literacy in treatment outcomes. Eat. Behav. 2017, 26, 76–82. [Google Scholar] [CrossRef]
- Erdogdu, U.E.; Cayci, H.M.; Tardu, A.; Demirci, H.; Kisakol, G.; Guclu, M. Health literacy and weight loss after bariatric surgery. Obes. Surg. 2019, 29, 3948–3953. [Google Scholar] [CrossRef]
- Martinez, M.; Salazar-Collier, C.L.; Pena, J.; Wilkinson, A.V.; Chavarria, E.A.; Reininger, B.M. Motivation for weight loss among completers of a free community-based weight loss program in a US-Mexico border region: A self-determination theory perspective. Front. Public Health 2022, 10, 652271. [Google Scholar] [CrossRef]
- Batsis, J.A.; Clark, M.M.; Grothe, K.; Lopez-Jimenez, F.; Collazo-Clavell, M.L.; Somers, V.K.; Sarr, M.G. Self-efficacy after bariatric surgery for obesity. A population-based cohort study. Appetite 2009, 52, 637–645. [Google Scholar] [CrossRef]
- Ugarte, C.; Quiñones, Á.; Saúl, L.A. Relationship among self-efficacy expectations, locus of control, and attributions in bariatric patients. Int. J. Environ. Res. Public Health 2022, 19, 7107. [Google Scholar] [CrossRef] [PubMed]
- Bjerkan, K.K.; Sandvik, J.; Nymo, S.; Græslie, H.; Johnsen, G.; Mårvik, R.; Hyldmo, Å.A.; Kulseng, B.E.; Høydal, K.L.; Hoff, D.A.L. The long-term impact of postoperative educational programs on weight loss after Roux-en-Y gastric bypass. Obes. Surg. 2022, 32, 3005–3012. [Google Scholar] [CrossRef] [PubMed]
- Sacks, F.M.; Bray, G.A.; Carey, V.J.; Smith, S.R.; Ryan, D.H.; Anton, S.D.; McManus, K.; Champagne, C.M.; Bishop, L.M.; Laranjo, N. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N. Engl. J. Med. 2009, 360, 859–873. [Google Scholar] [CrossRef] [PubMed]
- Park, J.Y. Prediction of type 2 diabetes remission after bariatric or metabolic surgery. J. Obes. Metab. Syndr. 2018, 27, 213. [Google Scholar] [CrossRef] [PubMed]
- Juray, S.; Axen, K.V.; Trasino, S.E. Remission of type 2 diabetes with very low-calorie diets—A narrative review. Nutrients 2021, 13, 2086. [Google Scholar] [CrossRef] [PubMed]
- Nagaratnam, S.; Rajoo, S.; Bidin, M.B.L.; Rahim, N.S.C.; Tharmathurai, S.; Arip, M.; Ching, Y.M.; Foo, S.H. A Cross-sectional Study to Assess Beta-Cell Function in Individuals with Recently Diagnosed Young-Onset Type 2 Diabetes Mellitus and Its’ Complications. J. ASEAN Fed. Endocr. Soc. 2023, 38, 20. [Google Scholar] [CrossRef] [PubMed]
- Malandrucco, I.; Pasqualetti, P.; Giordani, I.; Manfellotto, D.; De Marco, F.; Alegiani, F.; Sidoti, A.M.; Picconi, F.; Di Flaviani, A.; Frajese, G. Very-low-calorie diet: A quick therapeutic tool to improve β cell function in morbidly obese patients with type 2 diabetes. Am. J. Clin. Nutr. 2012, 95, 609–613. [Google Scholar] [CrossRef]
- Kelley, D.E.; Wing, R.; Buonocore, C.; Sturis, J.; Polonsky, K.; Fitzsimmons, M. Relative effects of calorie restriction and weight loss in noninsulin-dependent diabetes mellitus. J. Clin. Endocrinol. Metab. 1993, 77, 1287–1293. [Google Scholar] [CrossRef]
- Lara-Castro, C.; Newcomer, B.R.; Rowell, J.; Wallace, P.; Shaughnessy, S.M.; Munoz, A.J.; Shiflett, A.M.; Rigsby, D.Y.; Lawrence, J.C.; Bohning, D.E. Effects of short-term very low-calorie diet on intramyocellular lipid and insulin sensitivity in nondiabetic and type 2 diabetic subjects. Metabolism 2008, 57, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.; Ramachandran, A.; Yancy, W.S.; Forouhi, N.G. Nutritional basis of type 2 diabetes remission. BMJ 2021, 374, n1449. [Google Scholar] [CrossRef] [PubMed]
- Isbell, J.M.; Tamboli, R.A.; Hansen, E.N.; Saliba, J.; Dunn, J.P.; Phillips, S.E.; Marks-Shulman, P.A.; Abumrad, N.N. The importance of caloric restriction in the early improvements in insulin sensitivity after Roux-en-Y gastric bypass surgery. Diabetes Care 2010, 33, 1438–1442. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Petersen, G.M.; Roth, M.-P.; Schoenfield, L.J.; Marks, J.W. Risk factors for gallstone formation during rapid loss of weight. Dig. Dis. Sci. 1992, 37, 912–918. [Google Scholar] [CrossRef] [PubMed]
- Liddle, R.A.; Goldstein, R.B.; Saxton, J. Gallstone formation during weight-reduction dieting. Arch. Intern. Med. 1989, 149, 1750–1753. [Google Scholar] [CrossRef] [PubMed]
- He, L.; Wang, J.; Ping, F.; Yang, N.; Huang, J.; Li, Y.; Xu, L.; Li, W.; Zhang, H. Association of glucagon-like peptide-1 receptor agonist use with risk of gallbladder and biliary diseases: A systematic review and meta-analysis of randomized clinical trials. JAMA Intern. Med. 2022, 182, 513–519. [Google Scholar] [CrossRef]
- Mahase, E. GLP-1 agonists linked to adverse gastrointestinal events in weight loss patients. BMJ 2023, 383, 2330. [Google Scholar] [CrossRef]
- Elgohary, H.; El Azawy, M.; Omar, W. The incidence of gall stones after bariatric surgery and its association with weight loss. Int. J. Surg. Open 2021, 33, 100340. [Google Scholar] [CrossRef]
- Nogueiro, J.; Santos-Sousa, H.; Ribeiro, M.; Cruz, F.; Pereira, A.; Resende, F.; Costa-Pinho, A.; Preto, J.; Sousa-Pinto, B.; Lima-da-Costa, E. Incidence of symptomatic gallstones after bariatric surgery: The impact of expectant management. Langenbeck’s Arch. Surg. 2023, 408, 160. [Google Scholar] [CrossRef]
- Shiffman, M.L.; Sugerman, H.J.; Kellum, J.M.; Moore, E.W. Changes in gallbladder bile composition following gallstone formation and weight reduction. Gastroenterology 1992, 103, 214–221. [Google Scholar] [CrossRef]
- Portincasa, P.; Moschetta, A.; Palasciano, G. Cholesterol gallstone disease. Lancet 2006, 368, 230–239. [Google Scholar] [CrossRef] [PubMed]
- Di Ciaula, A.; Wang, D.Q.H.; Portincasa, P. Gallbladder and gastric motility in obese newborns, pre-adolescents and adults. J. Gastroenterol. Hepatol. 2012, 27, 1298–1305. [Google Scholar] [CrossRef] [PubMed]
- Weinsier, R.L.; Ullmann, D.O. Gallstone formation and weight loss. Obes. Res. 1993, 1, 51–56. [Google Scholar] [CrossRef] [PubMed]
| Variables | RYGB (n = 16) | VLCD (n = 15) | p-Value |
|---|---|---|---|
| Sex, n (%) | 0.252 | ||
| Male | 3 (18.8) | 6 (40.0) | |
| Female | 13 (81.3) | 9 (60.0) | |
| Age, years | 38.4 ± 9.3 | 31.8 ± 5.4 | 0.023 |
| Weight, kg | 109.2 ± 25.6 | 111.5 ± 23.3 | 0.795 |
| Body mass index, kg/m2 | 41.3 ± 8.0 | 39.7 ± 7.0 | 0.576 |
| Body fat mass, kg | 54.5 ± 15.8 | 52.6 ± 14.5 | 0.736 |
| % Body fat | 49.4 ± 4.9 | 46.9 ± 5.0 | 0.163 |
| Skeletal muscle mass, kg | 30.2 ± 6.8 | 32.9 ± 6.6 | 0.280 |
| % Skeletal muscle mass | 27.9 ± 2.8 | 29.6 ± 3.0 | 0.102 |
| Waist circumference, cm | 115.2 ± 16.8 | 106.8 ± 9.5 | 0.311 |
| Systolic blood pressure, mmHg | 127.9 ± 16.4 | 127.0 ± 12.1 | 0.868 |
| Diastolic blood pressure, mmHg | 77.3 ± 7.6 | 83.7 ± 8.3 | 0.032 |
| Pulse rate, bpm | 87.4 ± 11.6 | 91.7 ± 11.4 | 0.302 |
| Comorbidities | |||
| Hypertension, n (%) | 9 (56.3) | 4 (26.7) | 0.095 |
| Dyslipidemia, n (%) | 9 (56.3) | 10 (66.7) | 0.552 |
| T2D, n (%) | 7 (43.8) | 5 (33.3) | 0.552 |
| Duration of T2D, year, median (IQR) | 1 (0.5, 5.8) | 0 (0, 0) | 0.043 |
| Medications | |||
| Antidiabetic drug | |||
| Insulin, n (%) | 2 (12.5) | 0 (0.0) | 0.484 |
| Oral hypoglycemic agent, n (%) | 6 (37.5) | 0 (0.0) | 0.018 |
| GLP-1 RA, n (%) | 3 (18.8) | 0 (0.0) | 0.226 |
| Antihypertensive drug | |||
| ACEI, n (%) | 3 (18.8) | 0 (0.0) | 0.226 |
| Angiotensin receptor blocker, n (%) | 2 (12.5) | 1 (6.7) | 1.000 |
| Calcium channel blocker, n (%) | 6 (37.5) | 1 (6.7) | 0.083 |
| Beta blocker, n (%) | 3 (18.8) | 1 (6.7) | 0.600 |
| Diuretic, n (%) | 1 (6.3) | 0 (0.0) | 1.000 |
| Antihyperlipidemic drug | |||
| Statin, n (%) | 9 (56.3) | 1 (6.7) | 0.006 |
| Ezetimibe, n (%) | 1 (6.3) | 0 (0.0) | 1.000 |
| Dietary intake | |||
| Total energy intake, kcal/d | 1693.8 ± 505.2 | 1789.8 ± 621.1 | 0.639 |
| Protein intake, g/d | 52.7 ± 19.9 | 90.3 ± 36.4 | 0.002 |
| Fat intake, g/d | 71.7 ± 24.8 | 71.2 ± 27.4 | 0.961 |
| Carbohydrate intake, g/d | 206.6 ± 75.3 | 195.2 ± 71.8 | 0.669 |
| Variables | RYGB (n = 16) | VLCD (n = 15) | p-Value |
|---|---|---|---|
| FPG, mg/dL | |||
| All patients | 123.7 ± 45.0 | 123.5 ± 59.0 | 0.994 |
| Patients with T2D | 142.3 ± 75.2 | 180.2 ± 75.2 | 0.362 |
| Patients without T2D | 109.2 ± 18.7 | 95.2 ± 14.9 | 0.086 |
| HbA1c, % | |||
| All patients | 6.9 ± 1.8 | 7.0 ± 2.5 | 0.894 |
| Patients with T2D | 8.1 ± 2.3 | 9.5 ± 3.1 | 0.367 |
| Patients without T2D | 5.9 ± 0.4 | 5.7 ± 0.4 | 0.205 |
| Total cholesterol, mg/dL | 178.3 ± 33.1 | 216.8 ± 38.9 | 0.006 |
| Triglyceride, mg/dL | 144.2 ± 66.2 | 133.5 ± 68.7 | 0.661 |
| HDL cholesterol, mg/dL | 46.4 ± 7.8 | 46.7 ± 10.5 | 0.930 |
| LDL cholesterol, mg/dL | 131.9 ± 38.4 | 158.6 ± 38.5 | 0.063 |
| Uric acid, mg/dL | 6.5 ± 1.9 | 7.2 ± 1.8 | 0.257 |
| Serum creatinine, mg/dL | 0.7 ± 0.3 | 0.7 ± 0.1 | 0.476 |
| eGFR, mL/min/1.73 m2 | 107.7 ± 25.4 | 118.7 ± 14.3 | 0.148 |
| AST, U/L | 33.8 ± 19.9 | 50.9 ± 62.0 | 0.319 |
| ALT, U/L | 36.9 ± 23.3 | 77.9 ± 113.5 | 0.182 |
| Variables | RYGB (n = 16) | VLCD (n = 15) | Mean Difference (95% CI) | p-Value |
|---|---|---|---|---|
| Weight, kg | ||||
| 4 weeks | 100.8 ± 0.8 | 105.5 ± 0.8 | −4.7 (−6.8, −2.7) | <0.001 |
| 12 weeks | 91.4 ± 0.8 | 96.1 ± 0.8 | −4.7 (−6.8, −2.7) | <0.001 |
| Body mass index, kg/m2 | ||||
| 4 weeks | 38.0 ± 0.3 | 37.6 ± 0.3 | 0.4 (−0.4, 1.1) | 0.345 |
| 12 weeks | 34.6 ± 0.3 | 34.2 ± 0.3 | 0.4 (−0.4, 1.1) | 0.345 |
| Body fat mass, kg | ||||
| 4 weeks | 49.8 ± 0.9 | 49.2 ± 1 | 0.6 (−1.8, 3) | 0.619 |
| 12 weeks | 40.6 ± 0.9 | 40.0 ± 1 | 0.6 (−1.8, 3) | 0.619 |
| % Body fat | ||||
| 4 weeks | 48.8 ± 0.8 | 46.3 ± 0.8 | 2.5 (0.5, 4.5) | 0.014 |
| 12 weeks | 43.6 ± 0.8 | 41.1 ± 0.8 | 2.5 (0.5, 4.5) | 0.014 |
| Skeletal muscle mass, kg | ||||
| 4 weeks | 28.1 ± 0.3 | 31.3 ± 0.3 | −3.3 (−4.1, −2.4) | <0.001 |
| 12 weeks | 27.5 ± 0.3 | 30.8 ± 0.3 | −3.3 (−4.1, −2.4) | <0.001 |
| % Skeletal muscle mass | ||||
| 4 weeks | 28.1 ± 0.4 | 29.8 ± 0.4 | −1.7 (−2.7, −0.8) | <0.001 |
| 12 weeks | 30.5 ± 0.4 | 32.2 ± 0.4 | −1.7 (−2.7, −0.8) | <0.001 |
| Waist circumference, cm | ||||
| 4 weeks | 111.3 ± 1.8 | 101.1 ± 1.8 | 10.3 (5.2, 15.3) | <0.001 |
| 12 weeks | 97.0 ± 1.8 | 94.7 ± 1.8 | 2.3 (−2.8, 7.4) | 0.369 |
| Dietary intake | ||||
| Total energy intake, kcal/d | ||||
| 4 weeks | 304.7 ± 38.1 | 824.8 ± 39.4 | −520.1 (−627.6, −412.6) | <0.001 |
| 12 weeks | 679.3 ± 38.1 | 875 ± 39.4 | −195.7 (−303.2, −88.3) | <0.001 |
| Protein intake, g/d | ||||
| 4 weeks | 20.6 ± 4.6 | 96.3 ± 4.7 | −75.8 (−86.4, −65.2) | <0.001 |
| 12 weeks | 43.8 ± 4.6 | 119.6 ± 4.7 | −75.8 (−86.4, −65.2) | <0.001 |
| Fat intake, g/d | ||||
| 4 weeks | 14.6 ± 2.7 | 23.1 ± 2.8 | −8.5 (−16.1, −1.0) | 0.027 |
| 12 weeks | 31.7 ± 2.7 | 28.7 ± 2.8 | 3.0 (−4.6, 10.6) | 0.438 |
| Carbohydrate intake, g/d | ||||
| 4 weeks | 23.7 ± 4.7 | 48.8 ± 4.8 | −25.2 (−38.3, −12) | <0.001 |
| 12 weeks | 44.7 ± 4.7 | 48.9 ± 4.8 | −4.2 (−17.4, 8.9) | 0.528 |
| Variables | RYGB (n = 16) | VLCD (n = 15) | Median Difference (95% CI) | p-Value |
|---|---|---|---|---|
| FPG, mg/dL | ||||
| All patients | −16.5 (−30.0, −6.0) | −10.0 (−29.0, −3.0) | −12.0 (−53.3, 29.3) | 0.557 |
| Patients with T2D | −22.0 (−46.0, 5.0) | −118.0 (−136.0, −11.0) | 96 (−58.2, 250.2) | 0.195 |
| Patients without T2D | −9.0 (−28.0, −6.0) | −5.5 (−11.0, −2.0) | −2 (−18.6, 14.6) | 0.802 |
| HbA1c, % | ||||
| All patients | −0.5 (−0.9, −0.3) | −0.4 (−1.0, −0.0) | −0.2 (−1.6, 1.2) | 0.766 |
| Patients with T2D | −0.6 (−3.4, 0.0) | −4.1 (−6.0, −1.0) | 3.6 (−0.8, 7.9) | 0.100 |
| Patients without T2D | −0.5 (−0.7, −0.3) | −0.2 (−0.4, 0.0) | −0.2 (−0.6, 0.1) | 0.160 |
| Total cholesterol, mg/dL | −16.5 (−35.0, 5.5) | −24.0 (−44.0, 2.0) | 5 (−24.1, 34.1) | 0.727 |
| Triglyceride, mg/dL | −38.0 (−69.5, −12.0) | −22.0 (−54.0, −3.0) | −28 (−64.5, 8.5) | 0.128 |
| HDL cholesterol, mg/dL | −3.0 (−10.0, 7.5) | −5.0 (−13.0, 1.0) | 3 (−7.1, 13.1) | 0.550 |
| LDL cholesterol, mg/dL | −25.0 (−34.0, −9.0) | −28.0 (−35.0, 8.0) | −1 (−29.5, 27.5) | 0.943 |
| Uric acid, mg/dL | −0.7 (−1.5, 0.3) | 0.2 (−1.4, 0.9) | −0.9 (−2.5, 0.7) | 0.255 |
| Serum creatinine, mg/dL | 0.0 (−0.1, 0.1) | 0.0 (−0.1, 0.0) | 0 (−0.1, 0.1) | 0.776 |
| eGFR, mL/min/1.73 m2 | −0.2 (−4.6, 2.6) | 0.0 (−2.6, 3.0) | −0.3 (−5.6, 5) | 0.908 |
| AST, U/L | 4.0 (−2.0, 14.0) | −5.0 (−21.0, 0.0) | 9 (−6.3, 24.3) | 0.237 |
| ALT, U/L | 2.0 (−12.0, 9.0) | −17.0 (−31.0, −2.0) | 19 (1.1, 36.9) | 0.039 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saiyalam, C.; Shantavasinkul, P.C.; Chirnaksorn, S.; Rattanakaemakorn, P.; Taonam, N.; Rodphech, V.; Putadechakum, S.; Rattanasiri, S.; Sirivarasai, J.; Ongphiphadhanakul, B.; et al. Effects of Very Low-Calorie Diet versus Roux-en-Y Gastric Bypass Surgery on Body Composition in Patients with Obesity. Nutrients 2024, 16, 2407. https://doi.org/10.3390/nu16152407
Saiyalam C, Shantavasinkul PC, Chirnaksorn S, Rattanakaemakorn P, Taonam N, Rodphech V, Putadechakum S, Rattanasiri S, Sirivarasai J, Ongphiphadhanakul B, et al. Effects of Very Low-Calorie Diet versus Roux-en-Y Gastric Bypass Surgery on Body Composition in Patients with Obesity. Nutrients. 2024; 16(15):2407. https://doi.org/10.3390/nu16152407
Chicago/Turabian StyleSaiyalam, Chanawit, Prapimporn Chattranukulchai Shantavasinkul, Supphamat Chirnaksorn, Ploysyne Rattanakaemakorn, Naphat Taonam, Vorachat Rodphech, Supanee Putadechakum, Sasivimol Rattanasiri, Jintana Sirivarasai, Boonsong Ongphiphadhanakul, and et al. 2024. "Effects of Very Low-Calorie Diet versus Roux-en-Y Gastric Bypass Surgery on Body Composition in Patients with Obesity" Nutrients 16, no. 15: 2407. https://doi.org/10.3390/nu16152407
APA StyleSaiyalam, C., Shantavasinkul, P. C., Chirnaksorn, S., Rattanakaemakorn, P., Taonam, N., Rodphech, V., Putadechakum, S., Rattanasiri, S., Sirivarasai, J., Ongphiphadhanakul, B., & Sumritpradit, P. (2024). Effects of Very Low-Calorie Diet versus Roux-en-Y Gastric Bypass Surgery on Body Composition in Patients with Obesity. Nutrients, 16(15), 2407. https://doi.org/10.3390/nu16152407






