Sleep Patterns and Tryptophan Consumption among Students at Spanish Universities: The Unihcos Project
Abstract
1. Introduction
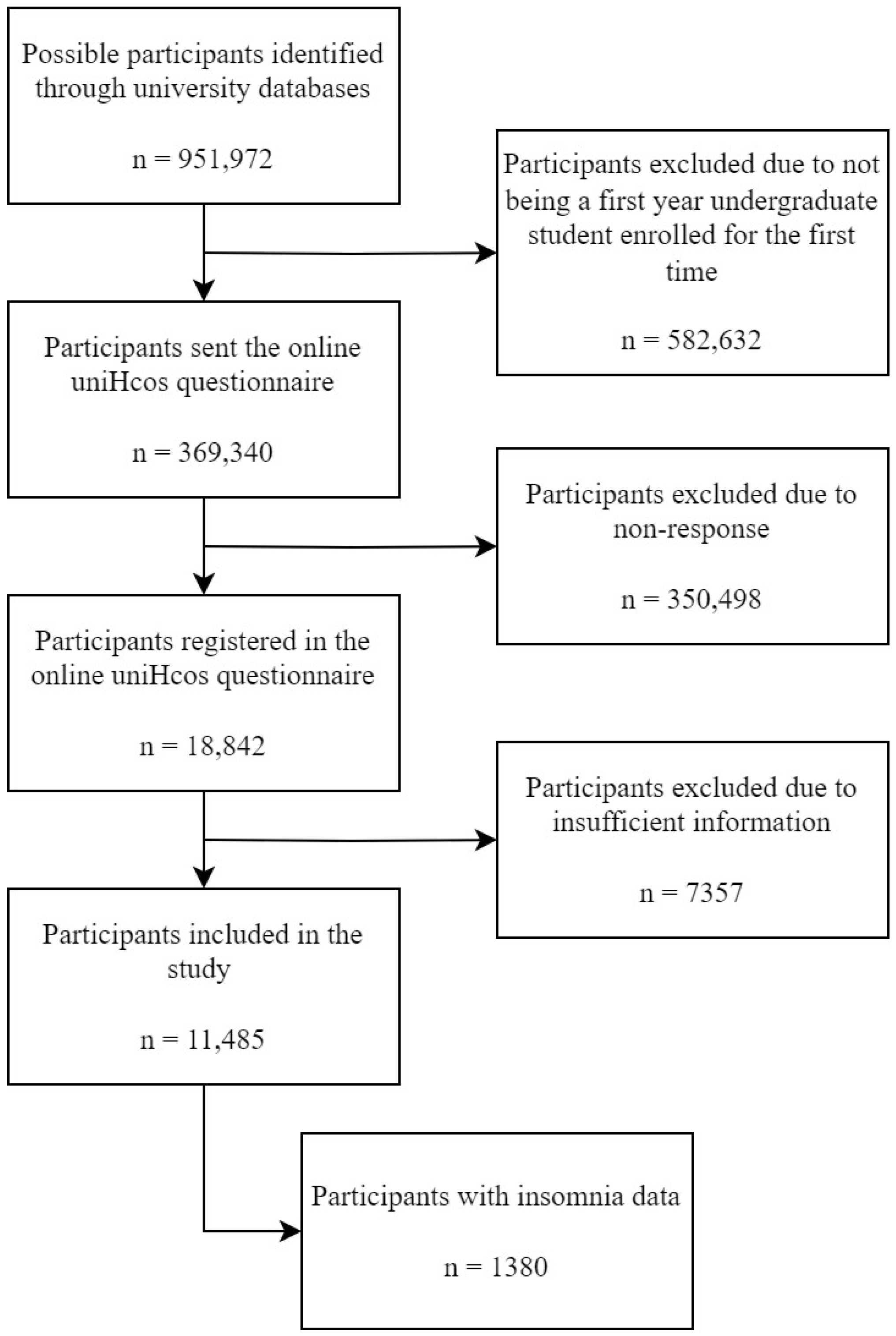
2. Material and Methods
2.1. Design and Ethical Considerations
2.2. Questionnaire
2.3. Data Collected
- Marital status: single (single, separated, divorced, widowed), married (married, domestic partner);
- Employment status: unemployed (only study and do not look for work, study and look for work), employed (study and work part time, study and work full time);
- Housing: family home, university residence (residence hall/university residence), rental (rental, home-own, others);
- Coexistence: parents, roommates (roommates/friends), partner (with my partner, with my children), alone.
- Sleep duration (“Could you tell me, approximately, how many hours you sleep?”);
- Short sleep duration (less than 7 h) [54];
- Sleep efficiency (“Do the hours you sleep allow you to get enough rest?” yes, no);
- Difficulty to sleep (never, some days, several days, most days, every day);
- Wake up several times while sleeping (never, some days, several days, most days, every day);
- Wake up early (never, some days, several days, most days, every day); insomnia (“Do you suffer from insomnia?” yes, no);
2.4. Tryptophan Intake
2.5. Statistical Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Spiegel, K.; Tasali, E.; Leproult, R.; Van Cauter, E. Effects of poor and short sleep on glucose metabolism and obesity risk. Nat. Rev. Endocrinol. 2009, 5, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Alafif, N. Association between consumption of tryptophan with sleep quality in King Saud University students. J. King Saud Univ.-Sci. 2024, 36, 103046. [Google Scholar] [CrossRef]
- Christensen, D.S.; Zachariae, R.; Amidi, A.; Wu, L.M. Sleep and allostatic load: A systematic review and meta-analysis. Sleep Med. Rev. 2022, 64, 101650. [Google Scholar] [CrossRef] [PubMed]
- Calhoun, D.A.; Harding, S.M. Sleep and hypertension. Chest 2010, 138, 434–443. [Google Scholar] [CrossRef] [PubMed]
- Ramar, K.; Malhotra, R.K.; Carden, K.A.; Martin, J.L.; Abbasi-Feinberg, F.; Aurora, R.N.; Kapur, V.K.; Olson, E.J.; Rosen, C.L.; Rowley, J.A. Sleep is essential to health: An American Academy of Sleep Medicine position statement. J. Clin. Sleep Med. 2021, 17, 2115–2119. [Google Scholar] [CrossRef] [PubMed]
- de Entrambasaguas, M.; Romero, O.; Guevara, J.A.C.; de Larrinaga, A.Á.R.; Cañellas, F.; Salud, J.P.; Díaz, H.P. The prevalence of insomnia in Spain: A stepwise addition of ICSD-3 diagnostic criteria and notes. Sleep Epidemiol. 2023, 3, 100053. [Google Scholar] [CrossRef]
- Carrión-Pantoja, S.; Prados, G.; Chouchou, F.; Holguín, M.; Mendoza-Vinces, Á.; Expósito-Ruiz, M.; Fernández-Puerta, L. Insomnia symptoms, sleep hygiene, mental health, and academic performance in Spanish university students: A cross-sectional study. J. Clin. Med. 2022, 11, 1989. [Google Scholar] [CrossRef] [PubMed]
- AlDabal, L.; BaHammam, A.S. Metabolic, endocrine, and immune consequences of sleep deprivation. Open Respir. Med. J. 2011, 5, 31. [Google Scholar] [CrossRef]
- Vélez, J.C.; Souza, A.; Traslaviña, S.; Barbosa, C.; Wosu, A.; Andrade, A.; Frye, M.; Fitzpatrick, A.L.; Gelaye, B.; Williams, M.A. The epidemiology of sleep quality and consumption of stimulant beverages among Patagonian Chilean college students. Sleep Disord. 2013, 2013, 910104. [Google Scholar] [CrossRef] [PubMed]
- Edwards, M.K.; Loprinzi, P.D. Experimentally increasing sedentary behavior results in decreased sleep quality among young adults. Ment. Health Phys. Act. 2017, 12, 132–140. [Google Scholar] [CrossRef]
- Gilbert, S.P.; Weaver, C.C. Sleep quality and academic performance in university students: A wake-up call for college psychologists. J. Coll. Stud. Psychother. 2010, 24, 295–306. [Google Scholar] [CrossRef]
- Hershner, S.D.; Chervin, R.D. Causes and consequences of sleepiness among college students. Nat. Sci. Sleep 2014, 6, 73–84. [Google Scholar] [CrossRef] [PubMed]
- Brown, F.C.; Buboltz, W.C., Jr.; Soper, B. Relationship of sleep hygiene awareness, sleep hygiene practices, and sleep quality in university students. Behav. Med. 2002, 28, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Kloss, J.D.; Nash, C.O.; Horsey, S.E.; Taylor, D.J. The delivery of behavioral sleep medicine to college students. J. Adolesc. Health 2011, 48, 553–561. [Google Scholar] [CrossRef] [PubMed]
- Forquer, L.M.; Camden, A.E.; Gabriau, K.M.; Johnson, C.M. Sleep patterns of college students at a public university. J. Am. Coll. Health 2008, 56, 563–565. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, S.K.; Francis-Jimenez, C.M.; Knibbs, M.D.; Umali, I.L.; Truglio-Londrigan, M. Effectiveness of sleep education programs to improve sleep hygiene and/or sleep quality in college students: A systematic review. JBI Evid. Synth. 2016, 14, 108–134. [Google Scholar] [CrossRef] [PubMed]
- Wolfson, A.R. Adolescents and emerging adults’ sleep patterns: New developments. J. Adolesc. Health 2010, 46, 97–99. [Google Scholar] [CrossRef] [PubMed]
- Altun, İ.; Cınar, N.; Dede, C. The contributing factors to poor sleep experiences in according to the university students: A cross-sectional study. J. Res. Med. Sci. Off. J. Isfahan Univ. Med. Sci. 2012, 17, 557. [Google Scholar]
- Friedrich, A.; Schlarb, A.A. Let’s talk about sleep: A systematic review of psychological interventions to improve sleep in college students. J. Sleep Res. 2018, 27, 4–22. [Google Scholar] [CrossRef] [PubMed]
- Vail-Smith, K.; Felts, W.M.; Becker, C. Relationship between sleep quality and health risk behaviors in undergraduate college students. Coll. Stud. J. 2009, 43, 924–930. [Google Scholar]
- Taylor, D.J.; Gardner, C.E.; Bramoweth, A.D.; Williams, J.M.; Roane, B.M.; Grieser, E.A.; Tatum, J.I. Insomnia and mental health in college students. Behav. Sleep Med. 2011, 9, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Schlarb, A.A.; Kulessa, D.; Gulewitsch, M.D. Sleep characteristics, sleep problems, and associations of self-efficacy among German university students. Nat. Sci. Sleep 2012, 4, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Nadorff, M.R.; Nazem, S.; Fiske, A. Insomnia symptoms, nightmares, and suicidal ideation in a college student sample. Sleep 2011, 34, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Medeiros, A.L.D.; Mendes, D.B.; Lima, P.F.; Araujo, J.F. The relationships between sleep-wake cycle and academic performance in medical students. Biol. Rhythm Res. 2001, 32, 263–270. [Google Scholar] [CrossRef]
- Trockel, M.T.; Barnes, M.D.; Egget, D.L. Health-related variables and academic performance among first-year college students: Implications for sleep and other behaviors. J. Am. Coll. Health 2000, 49, 125–131. [Google Scholar] [CrossRef]
- Lund, H.G.; Reider, B.D.; Whiting, A.B.; Prichard, J.R. Sleep patterns and predictors of disturbed sleep in a large population of college students. J. Adolesc. Health 2010, 46, 124–132. [Google Scholar] [CrossRef] [PubMed]
- Kelly, W.E.; Kelly, K.E.; Clanton, R.C. The relationship between sleep length and grade-point average among college students. Coll. Stud. J. 2001, 35, 84–86. [Google Scholar]
- Gaultney, J.F. The prevalence of sleep disorders in college students: Impact on academic performance. J. Am. Coll. Health 2010, 59, 91–97. [Google Scholar] [CrossRef]
- Spielman, A.J.; Caruso, L.S.; Glovinsky, P.B. A behavioral perspective on insomnia treatment. Psychiatr. Clin. N. Am. 1987, 10, 541–553. [Google Scholar] [CrossRef]
- Karna, B.; Sankari, A.; Tatikonda, G. Sleep Disorder; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- St-Onge, M.; Mikic, A.; Pietrolungo, C.E. Effects of diet on sleep quality. Adv. Nutr. 2016, 7, 938–949. [Google Scholar] [CrossRef]
- Godos, J.; Grosso, G.; Castellano, S.; Galvano, F.; Caraci, F.; Ferri, R. Association between diet and sleep quality: A systematic review. Sleep Med. Rev. 2021, 57, 101430. [Google Scholar] [CrossRef]
- Peuhkuri, K.; Sihvola, N.; Korpela, R. Diet promotes sleep duration and quality. Nutr. Res. 2012, 32, 309–319. [Google Scholar] [CrossRef] [PubMed]
- Knowlden, A.P.; Hackman, C.L.; Sharma, M. Systematic review of dietary interventions targeting sleep behavior. J. Altern. Complement. Med. 2016, 22, 349–362. [Google Scholar] [CrossRef] [PubMed]
- Sutanto, C.N.; Wang, M.X.; Tan, D.; Kim, J.E. Association of sleep quality and macronutrient distribution: A systematic review and meta-regression. Nutrients 2020, 12, 126. [Google Scholar] [CrossRef] [PubMed]
- Zuraikat, F.M.; Wood, R.A.; Barragán, R.; St-Onge, M. Sleep and diet: Mounting evidence of a cyclical relationship. Annu. Rev. Nutr. 2021, 41, 309–332. [Google Scholar] [CrossRef] [PubMed]
- Sutanto, C.N.; Loh, W.W.; Kim, J.E. The impact of tryptophan supplementation on sleep quality: A systematic review, meta-analysis, and meta-regression. Nutr. Rev. 2022, 80, 306–316. [Google Scholar] [CrossRef] [PubMed]
- Silber, B.Y.; Schmitt, J. Effects of tryptophan loading on human cognition, mood, and sleep. Neurosci. Biobehav. Rev. 2010, 34, 387–407. [Google Scholar] [CrossRef] [PubMed]
- EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA). Scientific opinion on dietary reference values for protein. EFSA J. 2012, 10, 2557. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids; The National Academies Press: Washington, DC, USA, 2005. [Google Scholar]
- Forbes, G.B. Joint FAO/WHO ad hoc Expert Committee, Energy and Protein Requirements; WHO Technical Report Series 522; Food and Agriculture Organization: Rome, Italy, 1974; Volume 127, pp. 296–297. [Google Scholar]
- World Health Organization. Energy and protein requirements: Report of a joint FAO/WHO/UNU expert consultation. In Energy and Protein Requirements: Report of a Joint FAO/WHO/UNU Expert Consultation; WHO: Rome, Italy, 1985; p. 206. [Google Scholar]
- Moore, P.; Landolt, H.; Seifritz, E.; Clark, C.; Bhatti, T.; Kelsoe, J.; Rapaport, M.; Gillin, J.C. Clinical and physiological consequences of rapid tryptophan depletion. Neuropsychopharmacology 2000, 23, 601–622. [Google Scholar] [CrossRef] [PubMed]
- Kitano, N.; Tsunoda, K.; Tsuji, T.; Osuka, Y.; Jindo, T.; Tanaka, K.; Okura, T. Association between difficulty initiating sleep in older adults and the combination of leisure-time physical activity and consumption of milk and milk products: A cross-sectional study. BMC Geriatr. 2014, 14, 1–7. [Google Scholar] [CrossRef]
- Nisar, M.; Mohammad, R.M.; Arshad, A.; Hashmi, I.; Yousuf, S.M.; Baig, S.; Hashmi, S.M.I. Influence of dietary intake on sleeping patterns of medical students. Cureus 2019, 11, e4106. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, J.; Yoshizaki, T.; Yamamoto, K.; Yoshino, M.; Ota, M.; Kawahara, T.; Kamei, A. Association of frequency of milk or dairy product consumption with subjective sleep quality during training periods in Japanese elite athletes: A cross-sectional study. J. Nutr. Sci. Vitaminol. 2019, 65, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Bravo, R.; Matito, S.; Cubero, J.; Paredes, S.D.; Franco, L.; Rivero, M.; Rodríguez, A.B.; Barriga, C. Tryptophan-enriched cereal intake improves nocturnal sleep, melatonin, serotonin, and total antioxidant capacity levels and mood in elderly humans. Age 2013, 35, 1277–1285. [Google Scholar] [CrossRef] [PubMed]
- Mohajeri, M.H.; Wittwer, J.; Vargas, K.; Hogan, E.; Holmes, A.; Rogers, P.J.; Goralczyk, R.; Gibson, E.L. Chronic treatment with a tryptophan-rich protein hydrolysate improves emotional processing, mental energy levels and reaction time in middle-aged women. Br. J. Nutr. 2015, 113, 350–365. [Google Scholar] [CrossRef] [PubMed]
- Alkhatatbeh, M.J.; Khwaileh, H.N.; Abdul-Razzak, K.K. High prevalence of low dairy calcium intake and association with insomnia, anxiety, depression and musculoskeletal pain in university students from Jordan. Public Health Nutr. 2021, 24, 1778–1786. [Google Scholar] [CrossRef] [PubMed]
- Meier, T.B.; Savitz, J. The kynurenine pathway in traumatic brain injury: Implications for psychiatric outcomes. Biol. Psychiatry 2022, 91, 449–458. [Google Scholar] [CrossRef] [PubMed]
- Platten, M.; Nollen, E.A.; Röhrig, U.F.; Fallarino, F.; Opitz, C.A. Tryptophan metabolism as a common therapeutic target in cancer, neurodegeneration and beyond. Nat. Rev. Drug Discov. 2019, 18, 379–401. [Google Scholar] [CrossRef] [PubMed]
- Clarke, G.; Grenham, S.; Scully, P.; Fitzgerald, P.; Moloney, R.D.; Shanahan, F.; Dinan, T.G.; Cryan, J. The microbiome-gut-brain axis during early life regulates the hippocampal serotonergic system in a sex-dependent manner. Mol. Psychiatry 2013, 18, 666–673. [Google Scholar] [CrossRef] [PubMed]
- Fernández Villa, T.; Alguacil Ojeda, J.; Ayán Pérez, C.; Bueno Cavanillas, A.; Cancela Carral, J.M.; Capelo Álvarez, R.; Delgado Rodríguez, M.; Jiménez Mejías, E.; Jiménez Moleón, J.J.; Llorca Díaz, J. Proyecto UNIHCOS: Cohorte dinámica de estudiantes universitarios para el estudio del consumo de drogas y otras adicciones. Rev. Española Salud Pública 2013, 87, 575–585. [Google Scholar] [CrossRef]
- Andréu, M.M.; de Larrinaga, A.Á.R.; Pérez, J.A.; Martínez, M.Á.M.; Cuesta, F.J.P.; Guerra, A.J.A.; Santo-Tomás, O.R.; Luque, M.J.J.; Isern, F.J.S.; Sanz, T.C. Sueño saludable: Evidencias y guías de actuación. Documento oficial de la Sociedad Española de Sueño. Rev. Neurol. 2016, 63, S1–S27. [Google Scholar]
- Gómez-Benito, J.; Ruiz, C.; Guilera, G. A Spanish version of the Athens Insomnia Scale. Qual. Life Res. 2011, 20, 931–937. [Google Scholar] [CrossRef]
- Soldatos, C.R.; Dikeos, D.G.; Paparrigopoulos, T.J. Athens Insomnia Scale: Validation of an instrument based on ICD-10 criteria. J. Psychosom. Res. 2000, 48, 555–560. [Google Scholar] [CrossRef] [PubMed]
- Chung, K.; Yeung, W.; Ho, F.Y.; Yung, K.; Yu, Y.; Kwok, C. Cross-cultural and comparative epidemiology of insomnia: The Diagnostic and statistical manual (DSM), International classification of diseases (ICD) and International classification of sleep disorders (ICSD). Sleep Med. 2015, 16, 477–482. [Google Scholar] [CrossRef]
- Cao, X.; Wang, S.; Zhong, B.; Zhang, L.; Ungvari, G.S.; Ng, C.H.; Li, L.; Chiu, H.F.; Lok, G.K.; Lu, J. The prevalence of insomnia in the general population in China: A meta-analysis. PLoS ONE 2017, 12, e0170772. [Google Scholar] [CrossRef] [PubMed]
- Riera-Sampol, A.; Rodas, L.; Martínez, S.; Moir, H.J.; Tauler, P. Caffeine intake among undergraduate students: Sex differences, sources, motivations, and associations with smoking status and self-reported sleep quality. Nutrients 2022, 14, 1661. [Google Scholar] [CrossRef]
- Gallego-Gómez, J.I.; González-Moro, M.T.R.; González-Moro, J.M.R.; Vera-Catalán, T.; Balanza, S.; Simonelli-Muñoz, A.J.; Rivera-Caravaca, J.M. Relationship between sleep habits and academic performance in university Nursing students. BMC Nurs. 2021, 20, 100. [Google Scholar] [CrossRef]
- Suardiaz-Muro, M.; Ortega-Moreno, M.; Morante-Ruiz, M.; Monroy, M.; Ruiz, M.A.; Martín-Plasencia, P.; Vela-Bueno, A. Sleep quality and sleep deprivation: Relationship with academic performance in university students during examination period. Sleep Biol. Rhythm. 2023, 21, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Navarro-Martínez, R.; Chover-Sierra, E.; Colomer-Pérez, N.; Vlachou, E.; Andriuseviciene, V.; Cauli, O. Sleep quality and its association with substance abuse among university students. Clin. Neurol. Neurosurg. 2020, 188, 105591. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, H.R.; Agarwal, S.; Fulgoni, V.L., III. Tryptophan intake in the US adult population is not related to liver or kidney function but is associated with depression and sleep outcomes. J. Nutr. 2016, 146, 2609S–2615S. [Google Scholar] [CrossRef]
- Razeghi Jahromi, S.; Togha, M.; Ghorbani, Z.; Hekmatdoost, A.; Khorsha, F.; Rafiee, P.; Shirani, P.; Nourmohammadi, M.; Ansari, H. The association between dietary tryptophan intake and migraine. Neurol. Sci. 2019, 40, 2349–2355. [Google Scholar] [CrossRef]
- Suga, H.; Asakura, K.; Kobayashi, S.; Nojima, M.; Sasaki, S. Association between habitual tryptophan intake and depressive symptoms in young and middle-aged women. J. Affect. Disord. 2018, 231, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Sutanto, C.; Xia, X.; Heng, C.W.; Tan, Y.S.; Gan, A.X.; Wang, X.F.; Fam, J.; Kim, J.E. Impact of 5-Hydroxytryptophan Supplementation on Gut Microbiota Composition of Older Adults with Different Sleep Status in Singapore: A Randomized Controlled Trial. Curr. Dev. Nutr. 2022, 6, 337. [Google Scholar] [CrossRef]
- Sutanto, C.N.; Xia, X.; Heng, C.W.; Tan, Y.S.; Lee, D.P.S.; Fam, J.; Kim, J.E. The impact of 5-hydroxytryptophan supplementation on sleep quality and gut microbiota composition in older adults: A randomized controlled trial. Clin. Nutr. 2024, 43, 593–602. [Google Scholar] [CrossRef] [PubMed]
- da Silva, I.T.S.A.; da Silva Fidelis, D.E.; de Souza, R.F.; de Sousa Fernandes, M.S. Comment on “The impact of 5-hydroxytryptophan supplementation on sleep quality and gut microbiota composition in older adults: A randomized controlled trial” clinical nutrition 2024. Clin. Nutr. 2024, 43, 1597–1598. [Google Scholar] [CrossRef] [PubMed]
- van Egmond, L.; Tan, X.; Sjögren, P.; Cederholm, T.; Benedict, C. Association between healthy dietary patterns and self-reported sleep disturbances in older men: The ULSAM study. Nutrients 2019, 11, 1029. [Google Scholar] [CrossRef] [PubMed]
- Min, C.; Kim, H.-J.; Park, I.-S.; Park, B.; Kim, J.-H.; Sim, S.; Hyo, G.C. The association between sleep duration, sleep quality, and food consumption in adolescents: A cross-sectional study using the Korea Youth Risk Behavior Web-based Survey. BMJ Open 2018, 8, e022848. [Google Scholar] [CrossRef] [PubMed]
- Sato-Mito, N.; Sasaki, S.; Murakami, K.; Okubo, H.; Takahashi, Y.; Shibata, S.; Yamada, K.; Sato, K.; Freshmen in Dietetic Courses Study II group. The midpoint of sleep is associated with dietary intake and dietary behavior among young Japanese women. Sleep Med. 2011, 12, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Thompson, R.S.; Roller, R.; Mika, A.; Greenwood, B.N.; Knight, R.; Chichlowski, M.; Berg, B.M.; Fleshner, M. Dietary prebiotics and bioactive milk fractions improve NREM sleep, enhance REM sleep rebound and attenuate the stress-induced decrease in diurnal temperature and gut microbial alpha diversity. Front. Behav. Neurosci. 2017, 10, 240. [Google Scholar] [CrossRef] [PubMed]
- Komada, Y.; Okajima, I.; Kuwata, T. The Effects of Milk and Dairy Products on Sleep: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 9440. [Google Scholar] [CrossRef]
- Cavero-Redondo, I.; Alvarez-Bueno, C.; Sotos-Prieto, M.; Gil, A.; Martinez-Vizcaino, V.; Ruiz, J.R. Milk and Dairy Product Consumption and Risk of Mortality: An Overview of Systematic Reviews and Meta-Analyses. Adv. Nutr. 2019, 10, S97–S104. [Google Scholar] [CrossRef]
- Heine, W.; Radke, M.; Wutzke, K.-D. The significance of tryptophan in human nutrition. Amino Acids 1995, 9, 91–205. [Google Scholar] [CrossRef] [PubMed]
- Peters, J.C. Tryptophan nutrition and metabolism: An overview. In Kynurenine and Serotonin Pathways: Progress in Tryptophan Research; Springer Science & Business Media: New York, NY, USA, 1991; pp. 345–358. [Google Scholar]
- Ardiansyah, S.; Shirakawa, H.; Inagawa, Y.; Koseki, T.; Komai, M. Regulation of blood pressure and glucose metabolism induced by L-tryptophan in stroke-prone spontaneously hypertensive rats. Nutr. Metab. 2011, 8, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Fernstrom, J.D. A perspective on the safety of supplemental tryptophan based on its metabolic fates. J. Nutr. 2016, 146, 2601S–2608S. [Google Scholar] [CrossRef] [PubMed]
- Fernstrom, J.D. Role of precursor availability in control of monoamine biosynthesis in brain. Physiol. Rev. 1983, 63, 484–546. [Google Scholar] [CrossRef] [PubMed]
- Muldoon, M.F.; Mackey, R.H.; Williams, K.V.; Korytkowski, M.T.; Flory, J.D.; Manuck, S.B. Low central nervous system serotonergic responsivity is associated with the metabolic syndrome and physical inactivity. J. Clin. Endocrinol. Metab. 2004, 89, 266–271. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, R.C.; McDougle, C.J.; Schumacher, M.; Olcese, J.; Mason, J.W.; Heninger, G.R.; Price, L.H. Effects of acute tryptophan depletion on nocturnal melatonin secretion in humans. J. Clin. Endocrinol. Metab. 1993, 76, 1160–1164. [Google Scholar]
- Dawson, D.; Encel, N. Melatonin and sleep in humans. J. Pineal Res. 1993, 15, 1–12. [Google Scholar] [CrossRef]
- Smith, W.G. Does Gender Influence Online Survey Participation? A Record-Linkage Analysis of University Faculty Online Survey Response Behavior; Online Submission. Available online: https://eric.ed.gov/?id=ED501717 (accessed on 9 July 2024).
| Total N = 11,485 (100%) | Male n = 3138 (27.3%) | Female n = 8347 (72.7%) | p | |
|---|---|---|---|---|
| Age (Median ± SD) | 20.11 ± 4.62 | 20.47 ± 5.17 | 19.97 ± 4.38 | <0.001 |
| Housing | <0.001 | |||
| Family home | 5213 (45.4%) | 1537 (49.0%) | 3676 (44.0%) | <0.001 |
| University residence | 1303 (11.3%) | 327(10.4%) | 976 (11.7%) | 0.050 |
| Own home | 307(2.7%) | 112 (3.6%) | 195 (2.3%) | <0.001 |
| Other | 152(1.3%) | 31 (1.0%) | 121 (1.4%) | 0.091 |
| Rental | 4510 (39.3%) | 1131 (36.0%) | 3379 (40.5%) | <0.001 |
| Coexistence | <0.001 | |||
| Parents | 5253 (45.7%) | 1515 (48.3%) | 3738 (44.8%) | <0.001 |
| Roommates | 4627 (40.3%) | 1166 (37.2%) | 3461 (41.5%) | <0.001 |
| Partner | 60.4 (5.3%) | 146 (4.7%) | 458 (5.5%) | 0.088 |
| Alone | 1001 (8.7%) | 311 (9.9%) | 690 (8.3%) | 0.007 |
| Marital status | 0.140 | |||
| Single | 10,461 (91.1%) | 2843 (90.6%) | 7618 (91.3%) | 0.240 |
| Married | 1024 (8.9%) | 295 (9.4%) | 729 (8.7%) | 0.240 |
| Employment status | 0.007 | |||
| Unemployed | 10,261 (89.3%) | 2764 (88.1%) | 7487 (89.7%) | 0.014 |
| Employed | 1234 (10.7%) | 374 (11.9%) | 860 (10.3%) | 0.014 |
| Specialization | <0.001 | |||
| Humanity | 1387 (12.1%) | 297 (9.5%) | 1090 (13.1%) | <0.001 |
| Science College | 1741 (15.2%) | 571 (18.2%) | 1170 (14.0%) | <0.001 |
| Medical College | 2537 (22.1%) | 564 (18.0%) | 1973 (23.7%) | <0.001 |
| Management | 4656 (40.6%) | 1005 (32.1%) | 3651 (43.8%) | <0.001 |
| Engineering and architecture | 1155 (10.1%) | 698 (22.3%) | 457 (5.5%) | <0.001 |
| (a) | ||||
|---|---|---|---|---|
| Total N = 11,485 (100%) | Male n = 3138 (27.3%) | Female n = 8347 (72.7%) | p | |
| Sleep duration (Median ± SD) (h/day) | 7.49 ± 1.24 | 7.44 ± 1.19 | 7.51 ± 1.25 | 0.007 |
| Short sleep duration (<7 h/day) | 5860 (51.0%) | 1643 (52.4%) | 4217 (50.5%) | 0.041 |
| Sleep Efficiency (Inadequate) | 6315 (55.0%) | 1967 (62.7%) | 4348 (52.1%) | <0.001 |
| Difficulty to sleep | <0.001 | |||
| Never | 2333 (20.3%) | 754 (24.0%) | 1579 (18.9%) | <0.001 |
| Some days | 4633 (40.3%) | 1362 (43.4%) | 3271 (39.2%) | <0.001 |
| Several days | 2556 (22.3%) | 591(18.8%) | 1965 (23.5%) | <0.001 |
| Most days | 1383 (12.0%) | 297 (9.5%) | 1086 (13.0%) | <0.001 |
| Every day | 580 (5.1%) | 134 (4.3%) | 446 (5.3%) | 0.029 |
| Wake up several times while sleeping | <0.001 | |||
| Never | 2636 (23.0%) | 955 (30.4%) | 1681 (20.1%) | <0.001 |
| Some days | 4600 (40.1%) | 1308 (41.7%) | 3292 (39.4%) | 0.025 |
| Several days | 2345 (20.4%) | 514 (16.4%) | 1831 (21.9%) | <0.001 |
| Most days | 1360 (11.8%) | 247 (7.9%) | 1113 (13.3%) | <0.001 |
| Every day | 544 (4.7%) | 114 (3.6%) | 430 (5.2%) | <0.001 |
| Wake up early | <0.001 | |||
| Never | 3784 (32.9%) | 1106 (35.2%) | 2678 (32.1%) | 0.002 |
| Some days | 4407 (38.4%) | 1281 (40.8%) | 3126 (37.5%) | 0.001 |
| Several days | 1735 (15.1%) | 442 (14.1%) | 1293 (15.5%) | 0.062 |
| Most days | 1090 (9.5%) | 220 (7.0%) | 870 (10.4%) | <0.001 |
| Every day | 469 (4.1%) | 89 (2.8%) | 380 (4.6%) | <0.001 |
| (b) | ||||
| Total N = 1380 (100%) | Male n = 334 (24.2%) | Female n = 1046 (75.8%) | ||
| Insomnia | 777 (56.3%) | 154 (46.1%) | 623 (59.6%) | <0.001 |
| Athens Insomnia Scale | ||||
| Sleep induction | 0.079 | |||
| No problem | 441 (32.0%) | 102 (30.5%) | 339 (32.4%) | 0.517 |
| Slightly delayed | 517 (37.5%) | 144 (43.1%) | 373 (35.7%) | 0.015 |
| Markedly delayed | 348 (25.2%) | 74 (22.2%) | 274 (26.2%) | 0.143 |
| Very delayed or did not sleep at all | 74 (5.4%) | 14 (4.2%) | 60 (5.7%) | 0.289 |
| Wake up in the night | 0.323 | |||
| No problem | 568 (41.2%) | 146 (43.7%) | 422 (40.3%) | 0.272 |
| Slightly delayed | 537 (38.9%) | 133 (39.8%) | 404 (39.6%) | 0.948 |
| Markedly delayed | 223 (16.2%) | 44 (13.2%) | 179 (17.1%) | 0.092 |
| Very delayed or did not sleep at all | 52 (3.8%) | 11 (3.3%) | 41 (3.9%) | 0.616 |
| Wake up early end | 0.339 | |||
| No problem | 587 (43.5%) | 151 (45.2%) | 436 (41.7%) | 0.260 |
| Slightly delayed | 580 (42.0%) | 140 (41.9%) | 440 (42.1%) | 0.949 |
| Markedly delayed | 189 (13.7%) | 37 (11.1%) | 152 (14.5%) | 0.116 |
| Very delayed or did not sleep at all | 24 (1.7%) | 6 (1.8%) | 18 (1.7%) | 0.903 |
| Total sleep duration | 0.218 | |||
| No problem | 509 (36.9%) | 139 (41.6%) | 370 (35.4%) | 0.041 |
| Slightly delayed | 590 (428%) | 133 (39.8%) | 457 (43.7%) | 0.210 |
| Markedly delayed | 249 (18.0%) | 54 (16.2%) | 195 (18.6%) | 0.321 |
| Very delayed or did not sleep at all | 32 (2.3%) | 8 (2.4%) | 24 (2.3%) | 0.916 |
| Sleep quality | 0.055 | |||
| No problem | 532 (38.6%) | 148 (44.3%) | 384 (36.7%) | 0.013 |
| Slightly delayed | 555 (40.2%) | 128 (38.3%) | 427 (40.8%) | 0.417 |
| Markedly delayed | 245 (17.8%) | 47 (14.1%) | 198 (18.9%) | 0.046 |
| Very delayed or did not sleep at all | 48 (3.5%) | 11 (3.3%) | 37 (3.5%) | 0.862 |
| Wellbeing in the day | <0.001 | |||
| No problem | 575 (41.7%) | 175 (52.4%) | 400 (38.2%) | <0.001 |
| Slightly delayed | 560 (40.6%) | 119 (35.6%) | 441 (42.2%) | 0.033 |
| Markedly delayed | 187 (13.6%) | 35 (10.5%) | 152 (14.5%) | 0.063 |
| Very delayed or did not sleep at all | 58 (4.2%) | 5 (1.5%) | 53 (5.1%) | 0.004 |
| Daytime operation | <0.001 | |||
| No problem | 663 (48.0%) | 202 (60.5%) | 461 (44.1%) | <0.001 |
| Slightly delayed | 488 (35.4%) | 101 (30.2%) | 387 (37.0%) | 0.024 |
| Markedly delayed | 182 (13.2%) | 26 (7.8%) | 156 (14.9%) | <0.001 |
| Very delayed or did not sleep at all | 47 (3.4%) | 5 (1.5%) | 42 (4.0%) | 0.028 |
| Daytime sleepiness | <0.001 | |||
| No problem | 394 (28.6%) | 135 (40.4%) | 259 (24.8%) | <0.001 |
| Slightly delayed | 723 (52.4%) | 161 (48.2%) | 562 (53.7%) | 0.078 |
| Markedly delayed | 213 (15.4%) | 33 (9.9%) | 180 (17.2%) | 0.001 |
| Very delayed or did not sleep at all | 50 (3.6%) | 5 (1.5%) | 45 (4.3%) | 0.017 |
| Total sleep | ||||
| Total score (Median ± SD) | 6.79 ± 4.48 | 5.85 ± 4.10 | 7.10 ± 4.55 | <0.001 |
| 0–3: No insomnia | 366 (28.5%) | 257 (24.6%) | 109 (32.6%) | 0.006 |
| 4–7: Subclinical insomnia | 492 (35.7%) | 361 (34.5%) | 131 (39.2%) | 0.124 |
| 8–14: Clinically significant insomnia | 427 (30.9%) | 348 (33.3%) | 79 (23.7%) | <0.001 |
| 15–24: Severe insomnia | 95 (6.9%) | 80 (7.6%) | 15 (4.5%) | 0.027 |
| 0–7 No insomnia | 858 (62.2%) | 240 (71.9%) | 618 (59.1%) | <0.001 |
| 8–24 Insomnia | 522 (37.8%) | 94 (28.1%) | 428 (40.9%) | <0.001 |
| Total N = 11,485 (100%) | Male n = 3138 (27.3%) | Female n = 8347 (72.7%) | p | |
|---|---|---|---|---|
| Tryptophan requirement a (Median ± SD) (mg/day) | 285.11 ± 57.58 | 332.57 ± 57.03 | 268.03 ± 47.66 | <0.001 |
| Tryptophan intake | ||||
| Median ± SD (mg/day) | 692.16 ± 246.61 | 731.84 ± 246.86 | 677.24 ± 244.87 | <0.001 |
| Q1(<526.43 mg/day) | 2866 (25.0%) | 595 (19.0%) | 2271 (27.2%) | <0.001 |
| Q2 (526.43–663.65 mg/day) | 2860 (24.9%) | 782 (24.9%) | 2078 (24.9%) | 1 |
| Q3 (663.65–841.60 mg/day) | 2884 (25.1%) | 847 (27.0%) | 2037 (24.4%) | 0.004 |
| Q4 (>841.60 mg/day) | 2875 (25.0%) | 914 (29.1%) | 1961 (23.5%) | <0.001 |
| Intake/Requirement ratio | 2.51 ± 1.01 | 2.27 ± 0.85 | 2.60 ± 1.05 | <0.001 |
| Sleep Duration (<7 h/day) | Sleep Efficiency (Adequate) | Insomnia (Yes) | Athens Insomnia Scale (Insomnia) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ORc | 95% CI | ORc | 95% CI | ORc | 95% CI | ORc | 95% CI | |||||
| Male | ||||||||||||
| Q1 | 1.26 | 1.02 | 1.55 | 0.88 | 0.72 | 1.10 | 1.48 | 0.84 | 2.61 | 2.56 | 1.36 | 4.82 |
| Q2 | 1.00 | 0.83 | 1.21 | 0.83 | 0.68 | 1.04 | 1.35 | 0.74 | 2.47 | 1.39 | 0.68 | 2.79 |
| Q3 | 1.05 | 0.87 | 1.27 | 0.92 | 0.76 | 1.12 | 1.00 | 0.54 | 1.86 | 1.23 | 0.60 | 2.54 |
| Q4 | 1 Reference | 1 Reference | 1 Reference | 1 Reference | ||||||||
| Female | ||||||||||||
| Q1 | 1.19 | 1.05 | 1.34 | 0.93 | 0.82 | 1.05 | 1.48 | 1.06 | 2.06 | 1.47 | 1.10 | 2.05 |
| Q2 | 0.95 | 0.84 | 1.08 | 1.00 | 0.87 | 1.12 | 1.04 | 0.73 | 1.49 | 1.22 | 0.85 | 1.77 |
| Q3 | 1.12 | 1.00 | 1.27 | 0.98 | 0.87 | 1.11 | 1.22 | 0.83 | 1.80 | 1.23 | 0.83 | 1.83 |
| Q4 | 1 Reference | 1 Reference | 1 Reference | 1 Reference | ||||||||
| Total | ||||||||||||
| Q1 | 1.19 | 1.07 | 1.34 | 0.87 | 0.78 | 0.97 | 1.57 | 1.18 | 2.08 | 1.74 | 1.30 | 2.33 |
| Q2 | 0.96 | 0.87 | 1.08 | 0.93 | 0.83 | 1.03 | 1.15 | 0.49 | 1.56 | 1.32 | 0.95 | 1.82 |
| Q3 | 1.10 | 1.00 | 1.27 | 0.96 | 0.86 | 1.06 | 1.18 | 0.85 | 1.63 | 1.26 | 0.89 | 1.77 |
| Q4 | 1 Reference | 1 Reference | 1 Reference | 1 Reference | ||||||||
| Humanity n = 1387 (12.1%) | Science College n = 1741 (15.2%) | Medical College n = 2537 (22.1%) | Management n = 4656 (40.6%) | Engineering and Architecture n = 1155 (10.1%) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ORc | 95% CI | ORc | 95% CI | ORc | 95% CI | ORc | 95% CI | ORc | 95% CI | ||||||
| Male | |||||||||||||||
| Q1 | 3.00 | 0.39 | 23.07 | 2.10 | 0.56 | 7.81 | - | - | - | 1.48 | 0.49 | 4.55 | 2.78 | 0.70 | 11.10 |
| Q2 | 4.80 | 0.65 | 35.19 | 0.67 | 0.11 | 4.19 | - | - | - | 1.25 | 0.37 | 4.32 | 0.30 | 0.04 | 1.68 |
| Q3 | 0.86 | 0.06 | 11.25 | 0.67 | 0.08 | 2.80 | - | - | - | 1.00 | 0.31 | 3.18 | 1.73 | 0.34 | 8.87 |
| Q4 | 1 Reference | 1 Reference | 1 Reference | 1 Reference | 1 Reference | ||||||||||
| Female | |||||||||||||||
| Q1 | 3.15 | 1.04 | 9.55 | 1.46 | 0.62 | 3.49 | 1.35 | 0.63 | 2.89 | 1.49 | 0.95 | 2.42 | 0.53 | 0.13 | 2.20 |
| Q2 | 3.41 | 1.01 | 11.5 | 1.13 | 0.41 | 30.9 | 1.00 | 0.44 | 2.12 | 1.21 | 072 | 2.05 | 1.50 | 0.20 | 11.08 |
| Q3 | 3.30 | 0.96 | 11.57 | 0.92 | 0.32 | 2.63 | 1.01 | 0.42 | 2.43 | 1.27 | 0.72 | 2.26 | 1.00 | 0.19 | 6.25 |
| Q4 | 1 Reference | 1 Reference | 1 Reference | 1 Reference | 1 Reference | ||||||||||
| Total | |||||||||||||||
| Q1 | 3.50 | 1.29 | 8.68 | 1.64 | 0.97 | 3.39 | 2.04 | 1.02 | 4.11 | 1.57 | 1.02 | 2.44 | 1.28 | 0.49 | 3.37 |
| Q2 | 3.81 | 1.35 | 10.75 | 1.04 | 0.437 | 2.47 | 1.53 | 0.74 | 3.15 | 1.27 | 0.79 | 2.06 | 0.50 | 0.15 | 1.53 |
| Q3 | 2.69 | 1.35 | 10.75 | 0.79 | 0.33 | 1.91 | 1.50 | 0.67 | 3.34 | 1.19 | 0.72 | 1.98 | 1.36 | 0.40 | 4.50 |
| Q4 | 1 Reference | 1 Reference | 1 Reference | 1 Reference | 1 Reference | ||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morales-Suárez-Varela, M.; Amezcua-Prieto, C.; Peraita-Costa, I.; Mateos-Campos, R.; Ayán, C.; Ortiz-Moncada, R.; Fernández-Villa, T., on behalf of the Grupo de Investigación UniHcos. Sleep Patterns and Tryptophan Consumption among Students at Spanish Universities: The Unihcos Project. Nutrients 2024, 16, 2376. https://doi.org/10.3390/nu16142376
Morales-Suárez-Varela M, Amezcua-Prieto C, Peraita-Costa I, Mateos-Campos R, Ayán C, Ortiz-Moncada R, Fernández-Villa T on behalf of the Grupo de Investigación UniHcos. Sleep Patterns and Tryptophan Consumption among Students at Spanish Universities: The Unihcos Project. Nutrients. 2024; 16(14):2376. https://doi.org/10.3390/nu16142376
Chicago/Turabian StyleMorales-Suárez-Varela, María, Carmen Amezcua-Prieto, Isabel Peraita-Costa, Ramona Mateos-Campos, Carlos Ayán, Rocío Ortiz-Moncada, and Tania Fernández-Villa on behalf of the Grupo de Investigación UniHcos. 2024. "Sleep Patterns and Tryptophan Consumption among Students at Spanish Universities: The Unihcos Project" Nutrients 16, no. 14: 2376. https://doi.org/10.3390/nu16142376
APA StyleMorales-Suárez-Varela, M., Amezcua-Prieto, C., Peraita-Costa, I., Mateos-Campos, R., Ayán, C., Ortiz-Moncada, R., & Fernández-Villa, T., on behalf of the Grupo de Investigación UniHcos. (2024). Sleep Patterns and Tryptophan Consumption among Students at Spanish Universities: The Unihcos Project. Nutrients, 16(14), 2376. https://doi.org/10.3390/nu16142376









