Comparative Effects of Gymnema sylvestre and Berberine on Adipokines, Body Composition, and Metabolic Parameters in Obese Patients: A Randomized Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Trial Oversight
2.2. Patients
2.3. Trial Procedures and Outcomes
2.4. Statistical Analysis
3. Results
3.1. Clinical and Demographic Data
3.2. Follow-Up and Outcomes
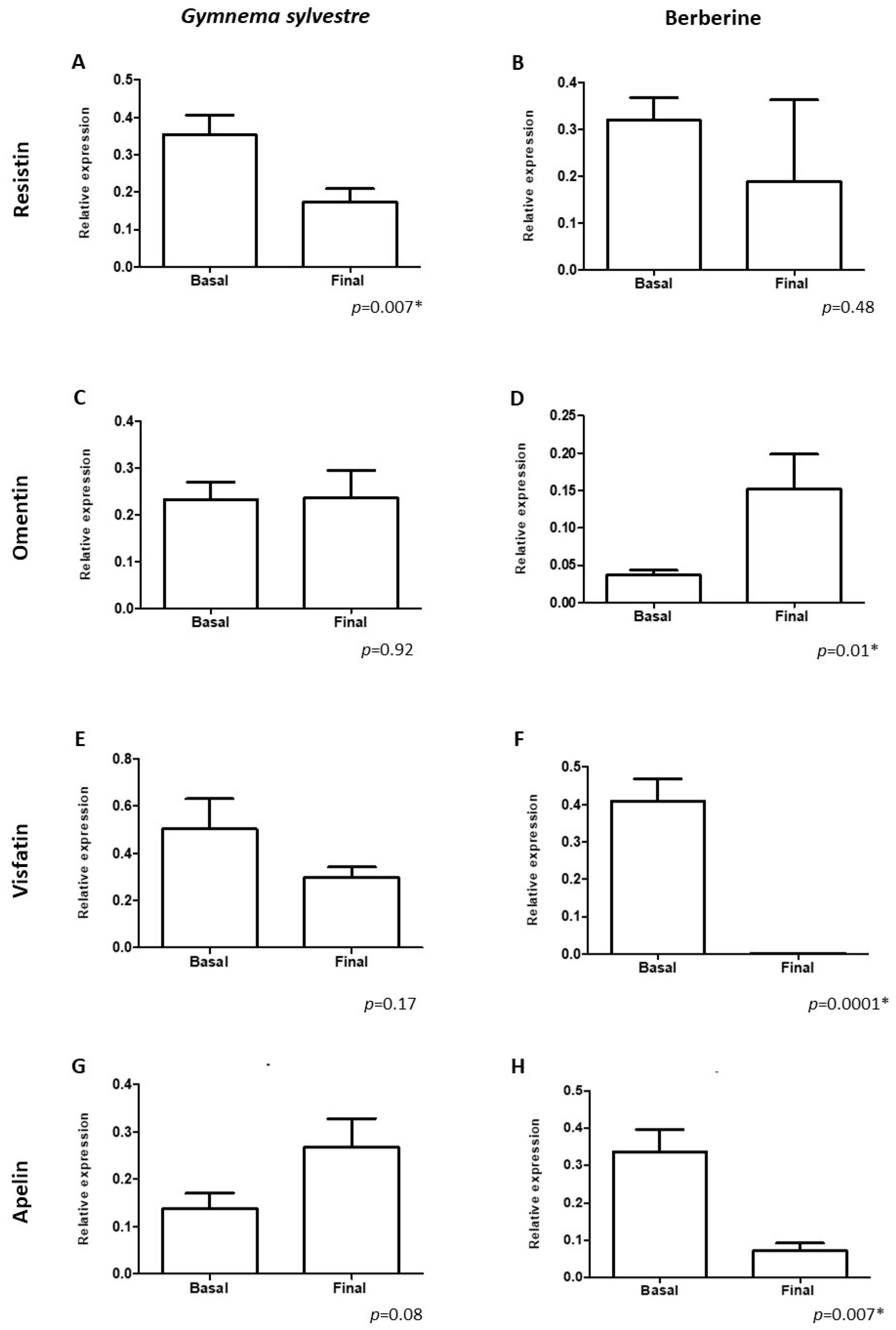
3.2.1. Principal Outcomes
3.2.2. Secondary Outcomes
3.2.3. Adverse Effects of Gymnema sylvestre and Berberine
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization: WHO. Obesity and Overweight. Available online: https://www.who.int/es/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 13 May 2024).
- Zhang, X.; Ha, S.; Lau, H.C.; Yu, J. Excess Body Weight: Novel Insights into its Roles in Obesity Comorbidities. Semin. Cancer Biol. 2023, 92, 16–27. [Google Scholar] [CrossRef]
- Zwick, R.K.; Guerrero-Juarez, C.F.; Horsley, V.; Plikus, M.V. Anatomical, Physiological, and Functional Diversity of Adipose Tissue. Cell Metab. 2018, 27, 68–83. [Google Scholar] [CrossRef] [PubMed]
- Recinella, L.; Orlando, G.; Ferrante, C.; Chiavaroli, A.; Brunetti, L.; Leone, S. Adipokines: New Potential Therapeutic Target for Obesity and Metabolic, Rheumatic, and Cardiovascular Diseases. Front. Physiol. 2020, 11, 578966. [Google Scholar] [CrossRef] [PubMed]
- Steppan, C.M.; Bailey, S.T.; Bhat, S.; Brown, E.J.; Banerjee, R.R.; Wright, C.M.; Patel, H.R.; Ahima, R.S.; Lazar, M.A. The hormone resistin links obesity to diabetes. Nature 2001, 409, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Ugur, K.; Erman, F.; Turkoglu, S.; Aydin, Y.; Aksoy, A.; Lale, A.; Karagöz, Z.K.; Ugur, I.; Akkoc, R.F.; Yalniz, M. Asprosin, visfatin and subfatin as new biomarkers of obesity and metabolic syndrome. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 2124–2133. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Kang, S.; Park, S.J.; Im, D.S. Apelin protects against liver X receptor-mediated steatosis through AMPK and PPARα in human and mouse hepatocytes. Cell. Signal. 2017, 39, 84–94. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Cheng, H.; Adhikari, B.K.; Wang, S.; Yang, N.; Liu, W.; Sun, J.; Wang, Y. The Role of Apelin-APJ System in Diabetes and Obesity. Front. Endocrinol. 2022, 13, 820002. [Google Scholar] [CrossRef] [PubMed]
- Sperling, M.; Grzelak, T.; Pelczyńska, M.; Bogdański, P.; Formanowicz, D.; Czyżewska, K. Association of Serum Omentin-1 Concentration with the Content of Adipose Tissue and Glucose Tolerance in Subjects with Central Obesity. Biomedicines 2023, 11, 331. [Google Scholar] [CrossRef] [PubMed]
- Derosa, G.; Catena, G.; Gaudio, G.; D’Angelo, A.; Maffioli, P. Adipose tissue dysfunction and metabolic disorders: Is it possible to predict who will develop type 2 diabetes mellitus? Role of markErs in the progreSsion of dIabeteS in obese paTIeNts (The RESISTIN trial). Cytokine 2020, 127, 154947. [Google Scholar] [CrossRef]
- Su, K.Z.; Li, Y.R.; Zhang, D.; Yuan, J.H.; Zhang, C.S.; Liu, Y.; Song, L.M.; Lin, Q.; Li, M.W.; Dong, J. Relation of Circulating Resistin to Insulin Resistance in Type 2 Diabetes and Obesity: A Systematic Review and Meta-Analysis. Front. Physiol. 2019, 10, 1399. [Google Scholar] [CrossRef]
- Yang, H.M.; Kim, J.; Shin, D.; Kim, J.Y.; You, J.; Lee, H.C.; Jang, H.D.; Kim, H.S. Resistin impairs mitochondrial homeostasis via cyclase-associated protein 1-mediated fission, leading to obesity-induced metabolic diseases. Metabolism 2023, 138, 155343. [Google Scholar] [CrossRef] [PubMed]
- Younus, I.; Iqbal, S.; Shahid, M.; Hassan, H. Serum visfatin levels in obese and non-obese individuals; A comparative cross-sectional study. Prof. Med, J. 2023, 30, 40–44. [Google Scholar] [CrossRef]
- Vliora, M.; Ravelli, C.; Grillo, E.; Corsini, M.; Flouris, A.D.; Mitola, S. The impact of adipokines on vascular networks in adipose tissue. Cytokine Growth Factor Rev. 2023, 69, 61–72. [Google Scholar] [CrossRef] [PubMed]
- Romacho, T.; Valencia, I.; Ramos-González, M.; Vallejo, S.; López-Esteban, M.; Lorenzo, O.; Cannata, P.; Romero, A.; San Hipólito-Luengo, A.; Gómez-Cerezo, J.F.; et al. Visfatin/eNampt induces endothelial dysfunction in vivo: A role for Toll-Like Receptor 4 and NLRP3 inflammasome. Sci. Rep. 2020, 10, 5386. [Google Scholar] [CrossRef] [PubMed]
- Heo, Y.J.; Choi, S.E.; Jeon, J.Y.; Han, S.J.; Kim, D.J.; Kang, Y.; Lee, K.W.; Kim, H.J. Visfatin Induces Inflammation and Insulin Resistance via the NF-κB and STAT3 Signaling Pathways in Hepatocytes. J. Diabetes Res. 2019, 2019, 4021623. [Google Scholar] [CrossRef]
- Zaki, M.; Kamal, S.; Ezzat, W.; Hassan, N.; Yousef, W.; Ryad, H.; Mohamed, R.; Youness, E.; Basha, W.; Elhosary, Y. Serum apelin levels and metabolic risk markers in obese women. J. Genet. Eng. Biotechnol. 2017, 15, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Sena, C.M. Omentin: A Key Player in Glucose Homeostasis, Atheroprotection, and Anti-Inflammatory Potential for Cardiovascular Health in Obesity and Diabetes. Biomedicines 2024, 12, 284. [Google Scholar] [CrossRef] [PubMed]
- Sperling, M.; Grzelak, T.; Pelczyńska, M.; Jasinska, P.; Bogdanski, P.; Pupek-Musialik, D.; Czyzewska, K. Concentrations of omentin and vaspin versus insulin resistance in obese individuals. Biomed. Pharmacother. 2016, 83, 542–547. [Google Scholar] [CrossRef] [PubMed]
- Faccioli, N.; Poitou, C.; Clément, K.; Dubern, B. Current Treatments for Patients with Genetic Obesity. J. Clin. Res. Pediatr. Endocrinol. 2023, 15, 108–119. [Google Scholar] [CrossRef]
- Sahebkar, A. Why it is necessary to translate curcumin into clinical practice for the prevention and treatment of metabolic syndrome? Biofactors 2013, 39, 197–208. [Google Scholar] [CrossRef]
- Pothuraju, R.; Sharma, R.K.; Rather, S.A.; Singh, S. Comparative evaluation of anti-obesity effect of Aloe vera and Gymnema sylvestre supplementation in high-fat diet fed C57BL/6J mice. J. Intercult. Ethnopharmacol. 2016, 5, 403–407. [Google Scholar] [CrossRef]
- Ilyas, Z.; Perna, S.; Al-Thawadi, S.; Alalwan, T.A.; Riva, A.; Petrangolini, G.; Gasparri, C.; Infantino, V.; Peroni, G.; Rondanelli, M. The effect of Berberine on weight loss in order to prevent obesity: A systematic review. Biomed. Pharmacother. 2020, 127, 110137. [Google Scholar] [CrossRef] [PubMed]
- Basciani, S.; Nordio, M.; Dinicola, S.; Unfer, V.; Gnessi, L. Diet Plus Inositols, A-Lactalbumin and Gymnema Sylvestre: The successful combo to restore body weight and metabolic profile in obese and dysmetabolic patients. Nutrients 2023, 15, 3142. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, P.; Mishra, B.N.; Sangwan, N.S. Phytochemical and pharmacological properties of Gymnema sylvestre: An important medicinal plant. BioMed Res. Int. 2014, 2014, 830285. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.; Kashiwagi, A.; Shibahara, T.; Yamada, K. Decreased bodyweight without reboundand regulated lipoprotein metabolism by gymnemate in genetic multifactor syndrome animal. Mol. Cell. Biochem. 2007, 299, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Vora, D.; Kapadia, H.; Dinesh, S.; Sharma, S.; Sosalagere, M.D. Gymnema sylvestre as a potential therapeutic agent for PCOS: Insights from mRNA differential gene expression and molecular docking analysis. Future J. Pharm. Sci. 2023, 9, 76. [Google Scholar] [CrossRef]
- Devangan, S.; Varghese, B.; Johny, E.; Gurram, S.; Adela, R. The effect of Gymnema sylvestre supplementation on glycemic control in type 2 diabetes patients: A systematic review and meta-analysis. Phytother. Res. 2021, 35, 6802–6812. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, P.; Ahmad, K.; Baig, M.H. Gymnema sylvestre for Diabetes: From Traditional Herb to Future’s Therapeutic. Curr. Pharm. Des. 2017, 23, 1667–1676. [Google Scholar] [CrossRef] [PubMed]
- Zuñiga, L.Y.; González-Ortiz, M.; Martínez-Abundis, E. Effect of Gymnema sylvestre Administration on Metabolic Syndrome, Insulin Sensitivity, and Insulin Secretion. J. Med. Food 2017, 20, 750–754. [Google Scholar] [CrossRef]
- Khan, F.; Sarker, M.M.R.; Ming, L.C.; Mohamed, I.N.; Zhao, C.; Sheikh, B.Y.; Tsong, H.F.; Rashid, M.A. Comprehensive Review on Phytochemicals, Pharmacological and Clinical Potentials of Gymnema sylvestre. Front. Pharmacol. 2019, 10, 1223. [Google Scholar] [CrossRef]
- Di Pierro, F.; Bellone, I.; Rapacioli, G.; Putignano, P. Clinical role of a fixed combination of standardized Berberis aristata and Silybum marianum extracts in diabetic and hypercholesterolemic patients intolerant to statins. Diabetes Metab. Syndr. Obes. 2015, 8, 89–96. [Google Scholar] [CrossRef]
- Chuang, T.Y.; Wu, H.L.; Min, J.; Diamond, M.; Azziz, R.; Chen, Y.H. Berberine regulates the protein expression of multiple tumorigenesis-related genes in hepatocellular carcinoma cell lines. Cancer Cell Int. 2017, 17, 59. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Zhang, Y.; Liu, Y.; Hou, L.; Li, S.; Tian, H.; Zhao, T. Berberine Modulates Gut Microbiota and Reduces Insulin Resistance via the TLR4 Signaling Pathway. Exp. Clin. Endocrinol. Diabetes 2018, 126, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Utami, A.R.; Maksum, I.P.; Deawati, Y. Berberine and Its Study as an Antidiabetic Compound. Biology 2023, 12, 973. [Google Scholar] [CrossRef] [PubMed]
- Ye, Y.; Liu, X.; Wu, N.; Han, Y.; Wang, J.; Yu, Y.; Chen, Q. Efficacy and Safety of Berberine Alone for Several Metabolic Disorders: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Front. Pharmacol. 2021, 12, 653887. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization: WHO. A Healthy Lifestyle—WHO Recommendations. Available online: https://www.who.int/europe/news-room/fact-sheets/item/a-healthy-lifestyle---who-recommendations (accessed on 5 July 2024).
- Taylor, E.B. The complex role of adipokines in obesity, inflammation, and autoimmunity. Clin. Sci. 2021, 135, 731–752. [Google Scholar] [CrossRef]
- Dec, P.; Poniewierska-Baran, A.; Modrzejewski, A.; Pawlik, A. The Role of Omentin-1 in Cancers Development and Progression. Cancers 2023, 15, 3797. [Google Scholar] [CrossRef]
- Zhang, Q.; Zhu, L.; Zheng, M.; Fan, C.; Li, Y.; Zhang, D.; He, Y.; Yang, H. Changes of serum omentin-1 levels in normal subjects, type 2 diabetes and type 2 diabetes with overweight and obesity in Chinese adults. Ann. D’endocrinol. 2014, 75, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Leandro, A.; Queiroz, M.; Azul, L.; Seiça, R.; Sena, C.M. Omentin: A novel therapeutic approach for the treatment of endothelial dysfunction in type 2 diabetes. Free Radic. Biol. Med. 2021, 162, 233–242. [Google Scholar] [CrossRef]
- Zhou, Q.; Chen, L.; Tang, M.; Guo, Y.; Li, L. Apelin/APJ system: A novel promising target for anti-aging intervention. Clin. Chim. Acta 2018, 487, 233–240. [Google Scholar] [CrossRef]
- Mughal, A.; O’Rourke, S.T. Vascular effects of apelin: Mechanisms and therapeutic potential. Pharmacol. Ther. 2018, 190, 139–147. [Google Scholar] [CrossRef]
- Soriguer, F.; Garrido-Sanchez, L.; Garcia-Serrano, S.; Garcia-Almeida, J.M.; Garcia-Arnes, J.; Tinahones, F.J.; Garcia-Fuentes, E. Apelin levels are increased in morbidly obese subjects with type 2 diabetes mellitus. Obes. Surg. 2009, 19, 1574–1580. [Google Scholar] [CrossRef]
- Mohammad, M.; Karim, D.; Mehdi, M.; Marziyeh, S.; Hadi, S.; Shila, N. The Combinatory Effect of Spirulina Supplementation and Resistance Exercise on Plasma Contents of Adipolin, Apelin, Ghrelin, and Glucose in Overweight and Obese Men. Mediat. Inflamm. 2022, 2022, 9539286. [Google Scholar] [CrossRef]
- Jamaluddin, M.S.; Weakley, S.M.; Yao, Q.; Chen, C. Resistin: Functional roles and therapeutic considerations for cardiovascular disease. Br. J. Pharmacol. 2012, 165, 622–632. [Google Scholar] [CrossRef]
- Filková, M.; Haluzík, M.; Gay, S.; Senolt, L. The role of resistin as a regulator of inflammation: Implications for various human pathologies. Clin. Immunol. 2009, 133, 157–170. [Google Scholar] [CrossRef] [PubMed]
- Mu, H.; Ohashi, R.; Yan, S.; Chai, H.; Yang, H.; Lin, P.; Yao, Q.; Chen, C. Adipokine resistin promotes in vitro angiogenesis of human endothelial cells. Cardiovasc. Res. 2006, 70, 146–157. [Google Scholar] [CrossRef]
- Abdalla, M.M.I. Role of visfatin in obesity-induced insulin resistance. World J. Clin. Cases 2022, 10, 10840–10851. [Google Scholar] [CrossRef]
- Ognjanovic, S.; Ku, T.L.; Bryant-Greenwood, G.D. Pre-B-cell colony-enhancing factor is a secreted cytokine-like protein from the human amniotic epithelium. Am. J. Obstet. Gynecol. 2005, 193, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Lei, H.; Zhang, Z. Pre-B-cell colony enhancing factor (PBEF), a cytokine with multiple physiological functions. Cytokine Growth Factor. Rev. 2013, 24, 433–442. [Google Scholar] [CrossRef] [PubMed]
- Hetta, H.F.; Ez-Eldeen, M.E.; Mohamed, G.A.; Gaber, M.A.; ElBadre, H.M.; Ahmed, E.A.; Abdellatief, R.B.; Abd-ElBaky, R.M.; Elkady, A.; Nafee, A.M.; et al. Visfatin Serum Levels in Obese Type 2 Diabetic Patients: Relation to Proinflammatory Cytokines and Insulin Resistance. Egypt. J. Immunol. 2018, 25, 141–151. [Google Scholar]
- Liang, Z.; Wu, Y.; Xu, J.; Fang, Q.; Chen, D. Correlations of serum visfatin and metabolisms of glucose and lipid in women with gestational diabetes mellitus. J. Diabetes Investig. 2016, 7, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Nourbakhsh, M.; Nourbakhsh, M.; Gholinejad, Z.; Razzaghy-Azar, M. Visfatin in obese children and adolescents and its association with insulin resistance and metabolic syndrome. Scand. J. Clin. Lab. Investig. 2015, 75, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, A.R.; Alsayari, A.; Habib, A.H.; Wahab, S.; Nadig, A.P.R.; Rafeeq, M.M.; Binothman, N.; Aljadani, M.; Al-Dhuayan, I.S.; Alaqeel, N.K.; et al. Anti-Tumor Potential of Gymnema sylvestre Saponin Rich Fraction on In Vitro Breast Cancer Cell Lines and In Vivo Tumor-Bearing Mouse Models. Antioxidants 2023, 12, 134. [Google Scholar] [CrossRef] [PubMed]
- Aleisa, A.M.; Al-Rejaie, S.S.; Abuohashish, H.M.; Ola, M.S.; Parmar, M.Y.; Ahmed, M.M. Pretreatment of Gymnema sylvestre revealed the protection against acetic acid-induced ulcerative colitis in rats. BMC Complement. Altern. Med. 2014, 14, 49. [Google Scholar] [CrossRef] [PubMed]
- Kanetkar, P.; Singhal, R.; Kamat, M. Gymnema sylvestre: A Memoir. J. Clin. Biochem. Nutr. 2007, 41, 77–81. [Google Scholar] [CrossRef]
- Wan, Q.; Liu, Z.; Yang, Y.; Cui, X. Suppressive effects of berberine on atherosclerosis via downregulating visfatin expression and attenuating visfatin-induced endothelial dysfunction. Int. J. Mol. Med. 2018, 41, 1939–1948. [Google Scholar] [CrossRef] [PubMed]
- Tu, J.; Luo, X.X.; Li, B.T.; Li, Y.; Xu, G.L. Effects of berberine on mRNA expression levels of PPARγ and adipocytokines in insulin-resistant adipocytes. Zhongguo Zhong Yao Za 2016, 41, 1983–1989. [Google Scholar] [CrossRef]
- Zhou, Z.; Qi, J.; Lim, C.W.; Kim, J.W.; Kim, B. Dual TBK1/IKKε inhibitor amlexanox mitigates palmitic acid-induced hepatotoxicity and lipoapoptosis in vitro. Toxicology 2020, 444, 152579. [Google Scholar] [CrossRef]
- Wang, M.; Xu, R.; Liu, X.; Zhang, L.; Qiu, S.; Lu, Y.; Zhang, P.; Yan, M.; Zhu, J. A cocrystal berberine-ibuprofen improves obesity by inhibiting the protein kinases TBK1 and IKKɛ. Commun. Biol. 2022, 5, 807. [Google Scholar] [CrossRef]
- Jangam, A.; Tirunavalli, S.K.; Adimoolam, B.M.; Kasireddy, B.; Patnaik, S.S.; Erukkambattu, J.; Thota, J.R.; Andugulapati, S.B.; Addlagatta, A. Anti-inflammatory and antioxidant activities of Gymnema Sylvestre extract rescue acute respiratory distress syndrome in rats via modulating the NF-κB/MAPK pathway. Inflammopharmacology 2023, 31, 823–844. [Google Scholar] [CrossRef]
- Yahia, S.; Salem, N.A.; El-Hawary, A.; Salem, M.; El-Farahaty, R.M.; El-Gilany, A.E.; Shoaib, R.M.S.; Noureldin, M.A. Serum apelin-12 and obesity-related markers in Egyptian children with Down syndrome. Eur. J. Pediatr. 2024, 183, 461–470. [Google Scholar] [CrossRef]
- Wang, J.; Gao, Y.; Lin, F.; Han, K.; Wang, X. Omentin-1 attenuates lipopolysaccharide (LPS)-induced U937 macrophages activation by inhibiting the TLR4/MyD88/NF-κB signaling. Arch. Biochem. Biophys. 2020, 679, 108187. [Google Scholar] [CrossRef]
- Al-Naimi, M.S.; Rasheed, H.A.; Al-Kuraishy, H.M.; Al-Gareeb, A.I. Berberine attenuates olanzapine induced-metabolic syndrome. J. Pak. Med. Assoc. 2019, 69, S88–S92. [Google Scholar]
- Saeidi, A.; Saei, M.A.; Mohammadi, B.; Zarei, H.R.A.; Vafaei, M.; Mohammadi, A.S.; Barati, M.; Montazer, M.; Razi, O.; Kiyumi, M.H.A.; et al. Supplementation with spinach-derived thylakoid augments the benefits of high intensity training on adipokines, insulin resistance and lipid profiles in males with obesity. Front. Endocrinol. 2023, 14, 1141796. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.W.; Kim, J.H.; Lee, Y.J. The Role of Adipokines in Tumor Progression and Its Association with Obesity. Biomedicines 2024, 12, 97. [Google Scholar] [CrossRef] [PubMed]
- Prabhakar, P.K.; Doble, M. Mechanism of action of natural products used in the treatment of diabetes mellitus. Chin. J. Integr. Med. 2011, 17, 563–574. [Google Scholar] [CrossRef]
- Nahas, R.; Moher, M. Complementary and alternative medicine for the treatment of type 2 diabetes. Can. Fam. Physician 2009, 55, 591–596. [Google Scholar] [PubMed]
- Muzaffar, H.; Qamar, I.; Bashir, M.; Jabeen, F.; Irfan, S.; Anwar, H. Gymnema Sylvestre Supplementation Restores Normoglycemia, Corrects Dyslipidemia, and Transcriptionally Modulates Pancreatic and Hepatic Gene Expression in Alloxan-Induced Hyperglycemic Rats. Metabolites 2023, 13, 516. [Google Scholar] [CrossRef]
- Carretero, M.E. Especies vegetales con posible actividad hypoglucemiante (III). Panorama Actual. Med. 2005, 29, 343–347. [Google Scholar]
- Wang, Y.; Dawid, C.; Kottra, G.; Daniel, H.; Hofmann, T. Gymnemic acids inhibit sodium-dependent glucose transporter 1. J. Agric. Food Chem. 2014, 62, 5925–5931. [Google Scholar] [CrossRef]
- Ahrén, B.; Thorsson, O. Increased insulin sensitivity is associated with reduced insulin and glucagon secretion and increased insulin clearance in man. J. Clin. Endocrinol. Metab. 2003, 88, 1264–1270. [Google Scholar] [CrossRef][Green Version]
- Al-Romaiyan, A.; Liu, B.; Asare-Anane, H.; Maity, C.R.; Chatterjee, S.K.; Koley, N.; Biswas, T.; Chatterji, A.K.; Huang, G.C.; Amiel, S.A.; et al. A novel Gymnema sylvestre extract stimulates insulin secretion from human islets in vivo and in vitro. Phytother. Res. 2010, 24, 1370–1376. [Google Scholar] [CrossRef]
- Gaytán Martínez, L.A.; Sánchez-Ruiz, L.A.; Zuñiga, L.Y.; González-Ortiz, M.; Martínez-Abundis, E. Effect of Gymnema sylvestre Administration on Glycemic Control, Insulin Secretion, and Insulin Sensitivity in Patients with Impaired Glucose Tolerance. J. Med. Food 2021, 24, 28–32. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Bhandari, U.; Tripathi, C.D.; Khanna, G. Anti-obesity effect of Gymnema sylvestre extract on high fat diet-induced obesity in Wistar rats. Drug Res. 2013, 63, 625–632. [Google Scholar] [CrossRef]
- Kumar, V.; Bhandari, U.; Tripathi, C.D.; Khanna, G. Evaluation of antiobesity and cardioprotective effect of Gymnema sylvestre extract in murine model. Indian J. Pharmacol. 2012, 44, 607–613. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, J.A.; Flannery-Schroeder, E. Use of the Herb Gymnema sylvestre to Illustrate the Principles of Gustatory Sensation: An Undergraduate Neuroscience Laboratory Exercise. J. Undergrad. Neurosci. Educ. 2005, 3, A59–A62. [Google Scholar] [PubMed]
- Li, Y.; Zheng, M.; Zhai, X.; Huang, Y.; Khalid, A.; Malik, A.; Shah, P.; Karim, S.; Azhar, S.; Hou, X. Effect of-Gymnema Sylvestre, Citrullus Colocynthis and Artemisia Absinthium on blood glucose and lipid profile in Diabetic Human. Acta Pol. Pharm. 2015, 72, 981–985. [Google Scholar]
- Shanmugasundaram, E.R.; Rajeswari, G.; Baskaran, K.; Rajesh Kumar, B.R.; Radha Shanmugasundaram, K.; Kizar Ahmath, B. Use of Gymnema sylvestre leaf extract in the control of blood glucose in insulin-dependent diabetes mellitus. J. Ethnopharmacol. 1990, 30, 281–294. [Google Scholar] [CrossRef]
- Preuss, H.G.; Bagchi, D.; Bagchi, M.; Rao, C.V.S.; Dey, D.K.; Satyanarayana, S. Effects of a natural extract of (-)-hydroxycitric acid (HCA-SX) and a combination of HCA-SX plus niacin-bound chromium and Gymnema sylvestre extract on weight loss. Diabetes Obes. Metab. 2004, 6, 171–180. [Google Scholar] [CrossRef]
- Martínez-Abundis, E.; Méndez-Del Villar, M.; Pérez-Rubio, K.G.; Zuñiga, L.Y.; Cortez-Navarrete, M.; Ramírez-Rodriguez, A.; González-Ortiz, M. Novel nutraceutic therapies for the treatment of metabolic syndrome. World J. Diabetes 2016, 7, 142–152. [Google Scholar] [CrossRef]
- Yin, J.; Xing, H.; Ye, J. Efficacy of berberine in patients with type 2 diabetes mellitus. Metabolism 2008, 57, 712–717. [Google Scholar] [CrossRef] [PubMed]
- Kong, W.; Wei, J.; Abidi, P.; Lin, M.; Inaba, S.; Li, C.; Wang, Y.; Wang, Z.; Si, S.; Pan, H.; et al. Berberine is a novel cholesterol-lowering drug working through a unique mechanism distinct from statins. Nat. Med. 2004, 10, 1344–1351. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Ehli, E.A.; Kittelsrud, J.; Ronan, P.J.; Munger, K.; Downey, T.; Bohlen, K.; Callahan, L.; Munson, V.; Jahnke, M.; et al. Lipid-lowering effect of berberine in human subjects and rats. Phytomedicine 2012, 19, 861–867. [Google Scholar] [CrossRef] [PubMed]
- Yin, J.; Hu, R.; Chen, M.; Tang, J.; Li, F.; Yang, Y.; Chen, J. Effects of berberine on glucose metabolism in vitro. Metabolism 2002, 51, 1439–1443. [Google Scholar] [CrossRef] [PubMed]
- Yin, J.; Ye, J.; Jia, W. Effects and mechanisms of berberine in diabetes treatment. Acta Pharm. Sin. B 2012, 2, 327–334. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, X.; Zou, D.; Liu, W.; Yang, J.; Zhu, N.; Huo, L.; Wang, M.; Hong, J.; Wu, P.; et al. Treatment of type 2 diabetes and dyslipidemia with the natural plant alkaloid berberine. J. Clin. Endocrinol. Metab. 2008, 93, 2559–2565. [Google Scholar] [CrossRef] [PubMed]
- Guarino, G.; Strollo, F.; Carbone, L.; Della Corte, T.; Letizia, M.; Marino, G.; Gentile, S. Bioimpedance analysis, metabolic effects and safety of the association Berberis aristata/Bilybum marianum: A 52-week double-blind, placebo-controlled study in obese patients with type 2 diabetes. J. Biol. Regul. Homeost. Agents 2017, 31, 495–502. [Google Scholar] [PubMed]
- Jia, R.; Hou, Y.; Zhang, L.; Li, B.; Zhu, J. Effects of Berberine on Lipid Metabolism, Antioxidant Status, and Immune Response in Liver of Tilapia (Oreochromis niloticus) under a High-Fat Diet Feeding. Antioxidants 2024, 13, 548. [Google Scholar] [CrossRef] [PubMed]
- Tian, H.; Kang, Y.M.; Gao, H.L.; Shi, X.L.; Fu, L.Y.; Li, Y.; Jia, X.Y.; Liu, K.L.; Qi, J.; Li, H.B.; et al. Chronic infusion of berberine into the hypothalamic paraventricular nucleus attenuates hypertension and sympathoexcitation via the ROS/Erk1/2/iNOS pathway. Phytomedicine 2019, 52, 216–224. [Google Scholar] [CrossRef]
- Peretti, N.; Mas, E. Congenital disorders of intestinal digestion and absorption (sugars, proteins, lipids, ions). Best Pract. Res. Clin. Gastroenterol. 2022, 56, 101785. [Google Scholar] [CrossRef]
- Kim, H.J.; Hong, S.H.; Chang, S.H.; Kim, S.; Lee, A.Y.; Jang, Y.; Davaadamdin, O.; Yu, K.N.; Kim, J.E.; Cho, M.H. Effects of feeding a diet containing Gymnema sylvestre extract: Attenuating progression of obesity in C57BL/6J mice. Asian Pac. J. Trop. Med. 2016, 9, 437–444. [Google Scholar] [CrossRef] [PubMed]
| Gymnema silvestre (n = 25) | Berberine (n = 25) | p Value | |
|---|---|---|---|
| Gender | |||
| Women | 84% (21) | 84% (21) | 0.64 |
| Age (Mean ± SE) | 39 ± 2.22 | 41 ± 2.24 | 0.58 |
| Obesity classification & | |||
| Class I | 52% (13) | 60% (15) | 0.30 |
| Class II | 32% (8) | 40% (10) | |
| Class III | 16% (4) | - |
| Gymnema silvestre Mean ± SE | Berberine Mean ± SE | p Value | |
|---|---|---|---|
| Body Weight (kg) | 93.18 ± 19.31 | 86 ± 11.06 | 0.11 |
| BMI (kg/m2) | 36.18 ± 6.22 | 31.53 ± 7.12 | 0.002 *a |
| WHR (cm) | 0.98 ± 0.08 | 0.90 ± 0.06 | 0.001 * |
| Body fat (BF%) | 46.93 ± 4.56 | 44.07 ± 4.80 | 0.54 b |
| Visceral fat (VF%) | 20.56 ± 3.91 | 44.07 ± 4.80 | 0.72 c |
| SBP (mmHg) | 119.20 ± 12.22 | 112.72 ± 7.67 | 0.02 * |
| DBP (mmHg) | 83.20 ± 11.53 | 72.80 ± 7.91 | 0.003 *d |
| Gymnema silvestre Mean ± SE | Berberine Mean ± SE | p Value | |
|---|---|---|---|
| Fasting glucose (mg/dL) | 86.43 ± 7.85 | 116.44 ± 7.37 | 0.0001 *a |
| Insulin (μU/mL) | 19.43 ± 13.80 | 15.76 ± 13.50 | 0.34 |
| Glycosylated hemoglobin (%) | 5.50 ± 0.28 | 5.68 ± 0.25 | 0.40 |
| Cholesterol (mg/dL) | 190.97 ± 39.09 | 185.46 ± 47.23 | 0.65 |
| Triglycerides (mg/dL) | 127.99 ± 57.17 | 141 ± 45.33 | 0.37 |
| LDL (mg/dL) | 101.64 ± 25.19 | 98.96 ± 34.39 | 0.75 |
| HDL (mg/dL) | 40.95 ± 11.10 | 35.10 ± 7.34 | 0.57 b |
| VLDL (mg/dL) | 48.37 ± 20.69 | 51.39 ± 26.65 | 0.65 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bandala, C.; Carro-Rodríguez, J.; Cárdenas-Rodríguez, N.; Peña-Montero, I.; Gómez-López, M.; Hernández-Roldán, A.P.; Huerta-Cruz, J.C.; Muñoz-González, F.; Ignacio-Mejía, I.; Domínguez, B.; et al. Comparative Effects of Gymnema sylvestre and Berberine on Adipokines, Body Composition, and Metabolic Parameters in Obese Patients: A Randomized Study. Nutrients 2024, 16, 2284. https://doi.org/10.3390/nu16142284
Bandala C, Carro-Rodríguez J, Cárdenas-Rodríguez N, Peña-Montero I, Gómez-López M, Hernández-Roldán AP, Huerta-Cruz JC, Muñoz-González F, Ignacio-Mejía I, Domínguez B, et al. Comparative Effects of Gymnema sylvestre and Berberine on Adipokines, Body Composition, and Metabolic Parameters in Obese Patients: A Randomized Study. Nutrients. 2024; 16(14):2284. https://doi.org/10.3390/nu16142284
Chicago/Turabian StyleBandala, Cindy, Jazmín Carro-Rodríguez, Noemí Cárdenas-Rodríguez, Itzel Peña-Montero, Modesto Gómez-López, Ana Paola Hernández-Roldán, Juan Carlos Huerta-Cruz, Felipe Muñoz-González, Iván Ignacio-Mejía, Brayan Domínguez, and et al. 2024. "Comparative Effects of Gymnema sylvestre and Berberine on Adipokines, Body Composition, and Metabolic Parameters in Obese Patients: A Randomized Study" Nutrients 16, no. 14: 2284. https://doi.org/10.3390/nu16142284
APA StyleBandala, C., Carro-Rodríguez, J., Cárdenas-Rodríguez, N., Peña-Montero, I., Gómez-López, M., Hernández-Roldán, A. P., Huerta-Cruz, J. C., Muñoz-González, F., Ignacio-Mejía, I., Domínguez, B., & Lara-Padilla, E. (2024). Comparative Effects of Gymnema sylvestre and Berberine on Adipokines, Body Composition, and Metabolic Parameters in Obese Patients: A Randomized Study. Nutrients, 16(14), 2284. https://doi.org/10.3390/nu16142284








