Assessment of Vitamin D Status in the Drâa-Tafilalet Population (Morocco) Based on Sociodemographic, Health, and Nutritional Factors
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Subjects and Study Design
2.3. Pilot Sample
2.4. Data Collection
2.5. Laboratory Assessments
2.6. Statistics
3. Results
3.1. Features of Participants
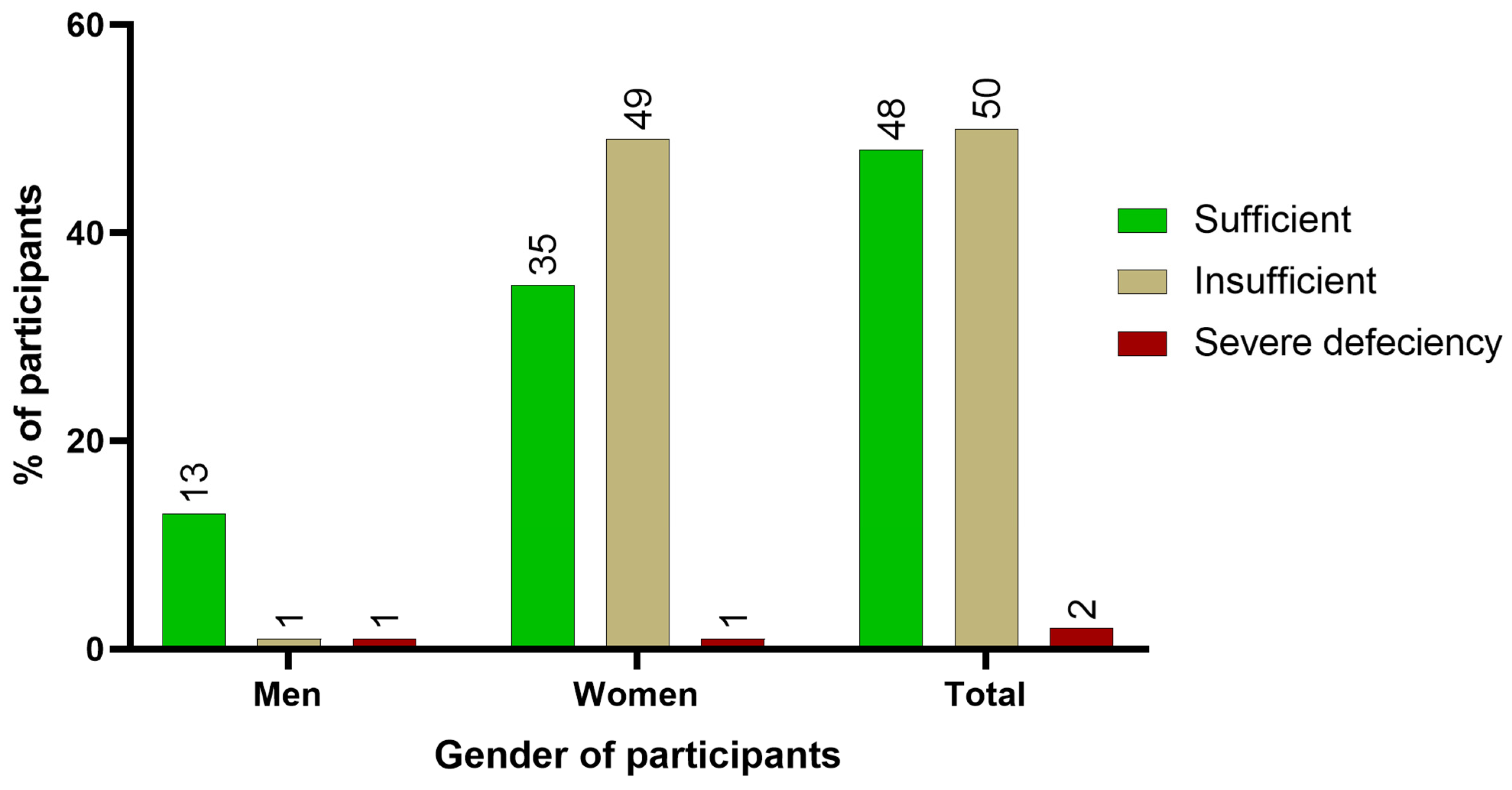
3.2. Status of Vitamin D
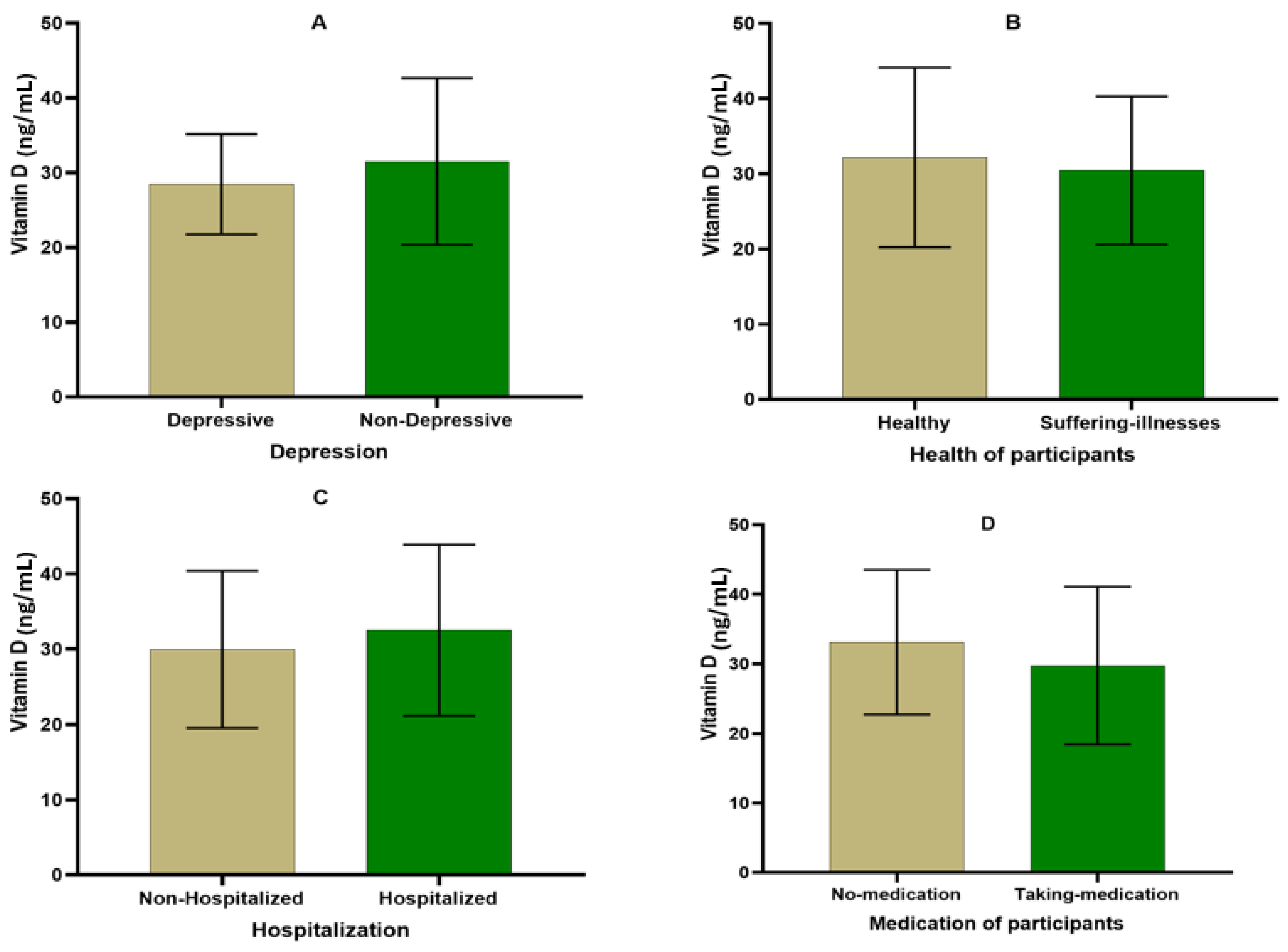
3.3. Health Status of Participants
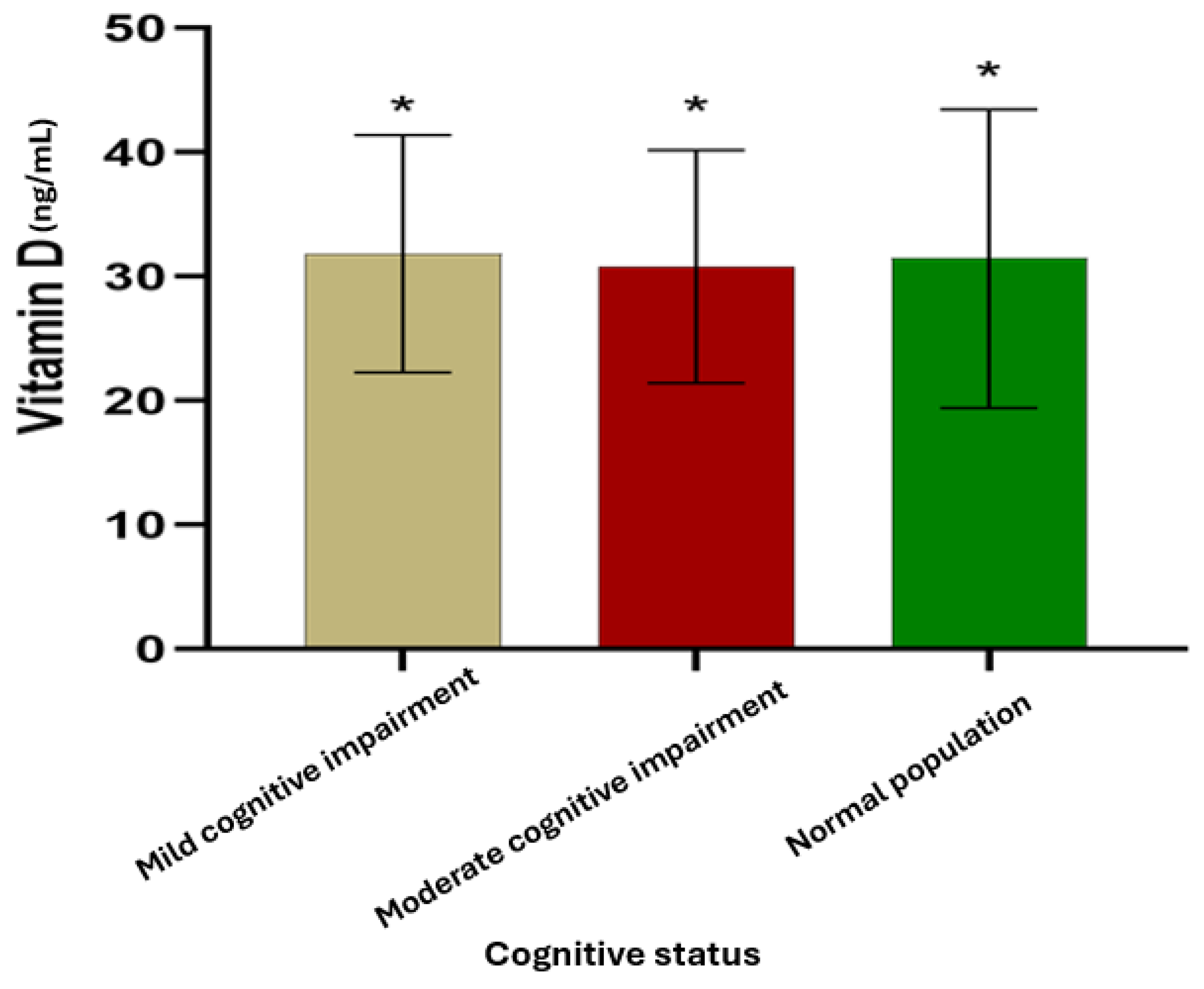
3.4. Cognitive Status
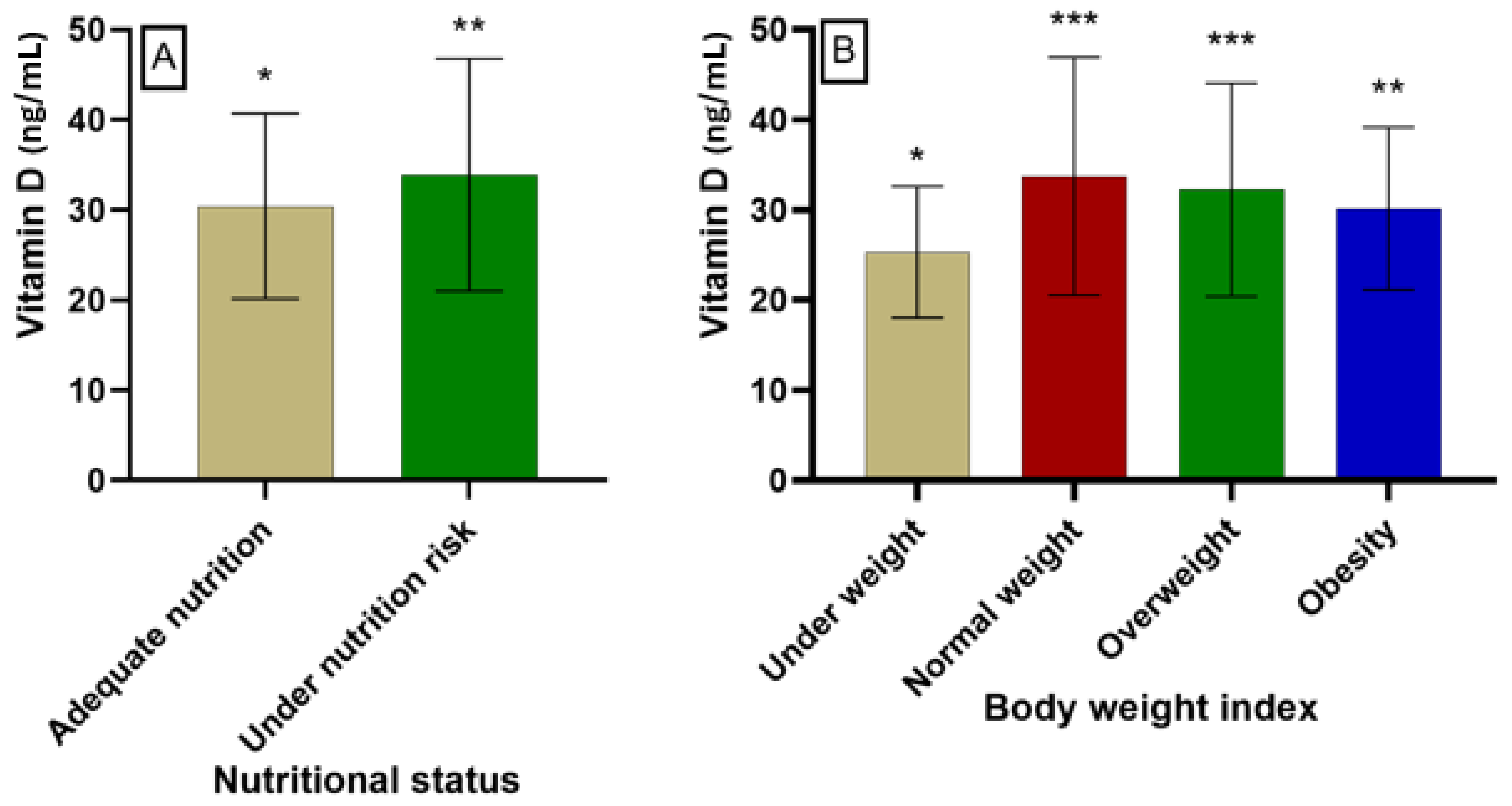
3.5. Nutritional Status and Body Weight Index
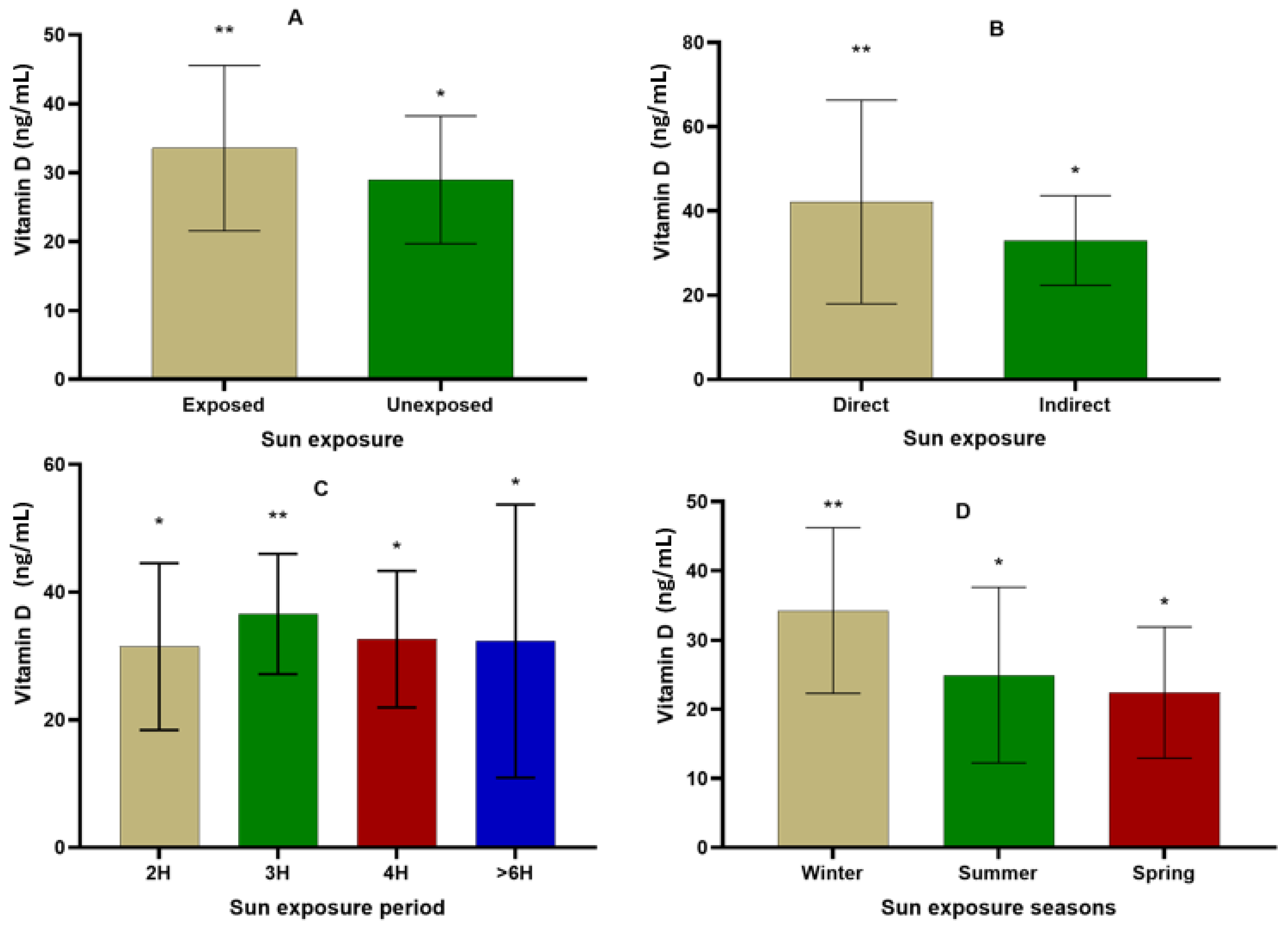
3.6. Effect of Sun Exposition on Vitamin D
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rathore, H.; Prasad, S.; Sharma, S. Mushroom Nutraceuticals for Improved Nutrition and Better Human Health: A Review. PharmaNutrition 2017, 5, 35–46. [Google Scholar] [CrossRef]
- Janoušek, J.; Pilařová, V.; Macáková, K.; Nomura, A.; Veiga-Matos, J.; da Silva, D.D.; Remião, F.; Saso, L.; Malá-Ládová, K.; Malý, J.; et al. Vitamin D: Sources, Physiological Role, Biokinetics, Deficiency, Therapeutic Use, Toxicity, and Overview of Analytical Methods for Detection of Vitamin D and Its Metabolites. Crit. Rev. Clin. Lab. Sci. 2022, 59, 517–554. [Google Scholar] [CrossRef] [PubMed]
- Dodd, S.A.S.; Shoveller, A.K.; Fascetti, A.J.; Yu, Z.Z.; Ma, D.W.L.; Verbrugghe, A. A Comparison of Key Essential Nutrients in Commercial Plant-Based Pet Foods Sold in Canada to American and European Canine and Feline Dietary Recommendations. Animals 2021, 11, 2348. [Google Scholar] [CrossRef] [PubMed]
- Vadaga, B.S. To Increase the Efficacy of Vitamin D2 on Cell Lines by Using Cissus Quadrangularis. Master of Science in Biotechnology Thesis, Jaypee University of Information Technology Waknaghat Department of Biotechnology and Bioinformatics, Waknaghat, India, 2022. Available online: http://www.ir.juit.ac.in:8080/jspui/bitstream/123456789/5107/1/To%20Increase%20the%20Efficacy%20of%20Vitamin%20D2%20on%20Cell%20Lines%20by%20Using%20Cissus%20Quadrangularis.pdf (accessed on 30 April 2024).
- Engelsen, O. The Relationship between Ultraviolet Radiation Exposure and Vitamin D Status. Nutrients 2010, 2, 482–495. [Google Scholar] [CrossRef] [PubMed]
- Miyauchi, M.; Nakajima, H. Determining an Effective UV Radiation Exposure Time for Vitamin D Synthesis in the Skin Without Risk to Health: Simplified Estimations from UV Observations. Photochem. Photobiol. 2016, 92, 863–869. [Google Scholar] [CrossRef]
- Pignolo, A.; Mastrilli, S.; Davì, C.; Arnao, V.; Aridon, P.; dos Santos Mendes, F.A.; Gagliardo, C.; D’Amelio, M. Vitamin D and Parkinson’s Disease. Nutrients 2022, 14, 1220. [Google Scholar] [CrossRef] [PubMed]
- Pike, J.W.; Meyer, M.B. Fundamentals of Vitamin D Hormone-Regulated Gene Expression. J. Steroid Biochem. Mol. Biol. 2014, 144, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Caprio, M.; Infante, M.; Calanchini, M.; Mammi, C.; Fabbri, A. Vitamin D: Not Just the Bone. Evidence for Beneficial Pleiotropic Extraskeletal Effects. Eat. Weight Disord. 2017, 22, 27–41. [Google Scholar] [CrossRef] [PubMed]
- Jean, G.; Souberbielle, J.C.; Chazot, C. Vitamin D in Chronic Kidney Disease and Dialysis Patients. Nutrients 2017, 9, 328. [Google Scholar] [CrossRef]
- Wang, H.; Chen, W.; Li, D.; Yin, X.; Zhang, X.; Olsen, N.; Zheng, S.G. Vitamin D and Chronic Diseases. Aging Dis. 2017, 8, 346–353. [Google Scholar] [CrossRef]
- Wimalawansa, S.J. Non-Musculoskeletal Benefits of Vitamin D. J. Steroid Biochem. Mol. Biol. 2018, 175, 60–81. [Google Scholar] [CrossRef] [PubMed]
- Bivona, G.; Agnello, L.; Bellia, C.; Iacolino, G.; Scazzone, C.; Lo Sasso, B.; Ciaccio, M. Non-Skeletal Activities of Vitamin D: From Physiology to Brain Pathology. Medicina 2019, 55, 341. [Google Scholar] [CrossRef] [PubMed]
- Rai, V.; Agrawal, D.K. Role of Vitamin D in Cardiovascular Diseases. Endocrinol. Metab. Clin. 2017, 46, 1039–1059. [Google Scholar] [CrossRef]
- Scragg, R.; Holdaway, I.; Jackson, R.; Lim, T. Plasma 25-hydroxyvitamin D3 and its relation to physical activity and other heart disease risk factors in the general population. Ann. Epidemiol. 1992, 2, 697–703. [Google Scholar] [CrossRef] [PubMed]
- D’Cruz, L.G.; Husain, S.A.; Wells, T.; Morgan, C.; Stanczyk, P.J.; Satgunarajah, A.; Kashir, J.; Calver, B.L.; Blayney, L.M.; Lai, F.A. Long Sun-Exposures Influencing High Sub-Cutaneous Synthesis of Vitamin-D3 May Be Associated with Exacerbation of Symptoms in Allergic-Asthma. J. Aging Res. Clin. Pract. 2018, 7, 47–54. [Google Scholar] [CrossRef]
- Cardwell, G.; Bornman, J.F.; James, A.P.; Black, L.J. A Review of Mushrooms as a Potential Source of Dietary Vitamin D. Nutrients 2018, 10, 1498. [Google Scholar] [CrossRef]
- Martineau, A.R.; Thummel, K.E.; Wang, Z.; Jolliffe, D.A.; Boucher, B.J.; Griffin, S.J.; Forouhi, N.G.; Hitman, G.A. Differential Effects of Oral Boluses of Vitamin D2 vs Vitamin D3 on Vitamin D Metabolism: A Randomized Controlled Trial. J. Clin. Endocrinol. Metab. 2019, 104, 5831–5839. [Google Scholar] [CrossRef]
- Jones, G.; Prosser, D.E.; Kaufmann, M. Chapter 5—The Activating Enzymes of Vitamin D Metabolism (25- and 1α-Hydroxylases). In Vitamin D, 4th ed.; Feldman, D., Ed.; Academic Press: Cambridge, MA, USA, 2018; pp. 57–79. ISBN 978-0-12-809965-0. [Google Scholar]
- Rozmus, D.; Płomiński, J.; Augustyn, K.; Cieślińska, A. Rs7041 and Rs4588 Polymorphisms in Vitamin D Binding Protein Gene (VDBP) and the Risk of Diseases. Int. J. Mol. Sci. 2022, 23, 933. [Google Scholar] [CrossRef]
- Jassil, N.K.; Sharma, A.; Bikle, D.; Wang, X. Vitamin D Binding Protein and 25-Hydroxyvitamin D Levels: Emerging Clinical Applications. Endocr. Pract. 2017, 23, 605–613. [Google Scholar] [CrossRef]
- Petersen, H.H.; Hilpert, J.; Militz, D.; Zandler, V.; Jacobsen, C.; Roebroek, A.J.M.; Willnow, T.E. Functional Interaction of Megalin with the Megalinbinding Protein (MegBP), a Novel Tetratrico Peptide Repeat-Containing Adaptor Molecule. J. Cell Sci. 2003, 116, 453–461. [Google Scholar] [CrossRef]
- Chang, S.-W.; Lee, H.-C. Vitamin D and Health—The Missing Vitamin in Humans. Pediatr. Neonatol. 2019, 60, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Black, L.J.; Lucas, R.M.; Sherriff, J.L.; Björn, L.O.; Bornman, J.F. In Pursuit of Vitamin D in Plants. Nutrients 2017, 9, 136. [Google Scholar] [CrossRef] [PubMed]
- Mendes, M.M.; Charlton, K.; Thakur, S.; Ribeiro, H.; Lanham-New, S.A. Future Perspectives in Addressing the Global Issue of Vitamin D Deficiency. Proc. Nutr. Soc. 2020, 79, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Edis, Z.; Bloukh, S.H. Vitamin D Deficiency: Main Factors Affecting The Serum 25-Hydroxyvitamin D ([25 (Oh) D]) Status And Treatment Options. Oncology 2016, 8, 9. [Google Scholar]
- Riaz, H.; Finlayson, A.E.; Bashir, S.; Hussain, S.; Mahmood, S.; Malik, F.; Godman, B. Prevalence of Vitamin D Deficiency in Pakistan and Implications for the Future. Expert Rev. Clin. Pharmacol. 2016, 9, 329–338. [Google Scholar] [CrossRef] [PubMed]
- El Maataoui, A.; Biaz, A.; El Machtani, S.; Bouhsain, S.; Dami, A.; El Maghraoui, A.; Ouzzif, Z. Vitamin D Status in Healthy Moroccan Men and Women Aged 50 Years and Older: A Cross-Sectional Study. Arch. Osteoporos. 2016, 11, 24. [Google Scholar] [CrossRef] [PubMed]
- Skalli, A.; Ait Ben Haddou, E.H.; El Jaoudi, R.; Razine, R.; Mpandzou, G.A.; Tibar, H.; El Fahime, E.; Bouslam, N.; Alami, A.; Benomar, A.; et al. Association of Vitamin D Status with Multiple Sclerosis in a Case-Control Study from Morocco. Rev. Neurol. 2018, 174, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Benjeddou, K.; Qandoussi, L.; Mekkaoui, B.; Rabi, B.; El Hamdouchi, A.; Raji, F.; Saeid, N.; Belghiti, H.; Elkari, K.; Aguenaou, H. Effect of Multiple Micronutrient Fortified Milk Consumption on Vitamin D Status among School-Aged Children in Rural Region of Morocco. Appl. Physiol. Nutr. Metab. 2019, 44, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Sebbar, E.; Choukri, M. Vitamin D Status in the Population of Eastern Morocco: Study of Vitamin D2 and Vitamin D3 by High Performance Liquid Chromatography. Mater. Today Proc. 2023, 72, 3432–3434. [Google Scholar] [CrossRef]
- Ibn Yacoub, Y.; Amine, B.; Laatiris, A.; Wafki, F.; Znat, F.; Hajjaj-Hassouni, N. Bone Density in Moroccan Women with Systemic Scleroderma and Its Relationships with Disease-Related Parameters and Vitamin D Status. Rheumatol. Int. 2012, 32, 3143–3148. [Google Scholar] [CrossRef]
- Hmamouchi, I.; Allali, F.; Handaoui, B.E.; Amine, H.; Rostom, S.; Abouqal, R.; Hajjaj-Hassouni, N. The Relation between Disease Activity, Vitamin D Levels and Bone Mineral Density in Men Patients with Ankylosing Spondylitis. Rheumatol. Rep. 2013, 5, e3. [Google Scholar] [CrossRef]
- Torbahn, G.; Strauss, T.; Sieber, C.C.; Kiesswetter, E.; Volkert, D. Nutritional Status According to the Mini Nutritional Assessment (MNA)® as Potential Prognostic Factor for Health and Treatment Outcomes in Patients with Cancer—A Systematic Review. BMC Cancer 2020, 20, 594. [Google Scholar] [CrossRef] [PubMed]
- Koc Okudur, S.; Soysal, P. Excessive Daytime Sleepiness Is Associated With Malnutrition, Dysphagia, and Vitamin D Deficiency in Older Adults. J. Am. Med. Dir. Assoc. 2021, 22, 2134–2139. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.-K.; Hung, K.-C.; Lin, Y.-T.; Chang, Y.-J.; Wu, Z.-F.; Ho, C.-H.; Chen, J.-Y. Age, Gender and Season Are Good Predictors of Vitamin D Status Independent of Body Mass Index in Office Workers in a Subtropical Region. Nutrients 2020, 12, 2719. [Google Scholar] [CrossRef] [PubMed]
- NejresHilal, N.; Ibraheem, N.M.; Suleiman, S.A.; Assim, H.S.; Ahmed, F.Y. Case Control Study: Estimation of Vitamin D Deficiency in Relation to Urinary Stones Formation among Tikritmale Population. Indian J. Forensic Med. Toxicol. 2019, 13, 1499–1504. [Google Scholar] [CrossRef]
- Van Schoor, N.; Lips, P. Chapter 59—Worldwide Vitamin D Status. In Vitamin D, 4th ed.; Feldman, D., Ed.; Academic Press: Cambridge, MA, USA, 2018; pp. 15–40. ISBN 978-0-12-809963-6. [Google Scholar]
- Amrein, K.; Scherkl, M.; Hoffmann, M.; Neuwersch-Sommeregger, S.; Köstenberger, M.; Tmava Berisha, A.; Martucci, G.; Pilz, S.; Malle, O. Vitamin D Deficiency 2.0: An Update on the Current Status Worldwide. Eur. J. Clin. Nutr. 2020, 74, 1498–1513. [Google Scholar] [CrossRef]
- Aguiar, M.; Andronis, L.; Pallan, M.; Högler, W.; Frew, E. The Economic Case for Prevention of Population Vitamin D Deficiency: A Modelling Study Using Data from England and Wales. Eur. J. Clin. Nutr. 2020, 74, 825–833. [Google Scholar] [CrossRef] [PubMed]
- Grant, W.B.; Bhattoa, H.P.; Boucher, B.J. Seasonal Variations of U.S. Mortality Rates: Roles of Solar Ultraviolet-B Doses, Vitamin D, Gene Exp Ression, and Infections. J. Steroid Biochem. Mol. Biol. 2017, 173, 5–12. [Google Scholar] [CrossRef]
- Huang, C.-H.; Huang, Y.-T.A.; Lai, Y.-C.; Sun, C.-K. Prevalence and Predictors of Hypovitaminosis D among the Elderly in Subtropical Region. PLoS ONE 2017, 12, e0181063. [Google Scholar] [CrossRef][Green Version]
- Van der Meer, I.M.; Middelkoop, B.J.C.; Boeke, A.J.P.; Lips, P. Prevalence of Vitamin D Deficiency among Turkish, Moroccan, Indian and Sub-Sahara African Populations in Europe and Their Countries of Origin: An Overview. Osteoporos. Int. 2011, 22, 1009–1021. [Google Scholar] [CrossRef]
- Allali, F.; El Aichaoui, S.; Khazani, H.; Benyahia, B.; Saoud, B.; El Kabbaj, S.; Bahiri, R.; Abouqal, R.; Hajjaj-Hassouni, N. High Prevalence of Hypovitaminosis D in Morocco: Relationship to Lifestyle, Physical Performance, Bone Markers, and Bone Mineral Density. Semin. Arthritis Rheum. 2009, 38, 444–451. [Google Scholar] [CrossRef] [PubMed]
- Lhilali, I.; Zouine, N.; Menouni, A.; Godderis, L.; Kestemont, M.-P.; El Midaoui, A.; El Jaafari, S.; Filali-Zegzouti, Y. Sun Exposure Score and Vitamin D Levels in Moroccan Women of Childbearing Age. Nutrients 2023, 15, 688. [Google Scholar] [CrossRef] [PubMed]
- Bour, A.; Nejjar, B. Knowledge about Vitamin D: An Overview of the Prevalence of Hypovitaminosis D among Moroccan Population. Ann. Sci. St 2017, 1, 24–31. [Google Scholar]
- Dadda, S.; Azekour, K.; Sebbari, F.; Houate, B.E.; Bouhali, B.E. Sun Exposure, Dressing Habits, and Vitamin D Status in Morocco. E3S Web Conf. 2021, 319, 01097. [Google Scholar] [CrossRef]
- Bouaddi, I.; Rostom, S.; El Badri, D.; Hassani, A.; Chkirate, B.; Abouqal, R.; Amine, B.; Hajjaj-Hassouni, N. Vitamin D Concentrations and Disease Activity in Moroccan Children with Juvenile Idiopathic Arthritis. BMC Musculoskelet. Disord. 2014, 15, 115. [Google Scholar] [CrossRef][Green Version]
- Zhou, Z.; Zhou, R.; Zhang, Z.; Li, K. The Association Between Vitamin D Status, Vitamin D Supplementation, Sunlight Exposure, and Parkinson’s Disease: A Systematic Review and Meta-Analysis. Med. Sci. Monit. 2019, 25, 666–674. [Google Scholar] [CrossRef]
- Aydın, C.G.; Dinçel, Y.M.; Arıkan, Y.; Taş, S.K.; Deniz, S. The Effects of Indoor and Outdoor Sports Participation and Seasonal Changes on Vitamin D Levels in Athletes. SAGE Open Med. 2019, 7, 2050312119837480. [Google Scholar] [CrossRef]
- Krzywanski, J.; Mikulski, T.; Krysztofiak, H.; Mlynczak, M.; Gaczynska, E.; Ziemba, A. Seasonal Vitamin D Status in Polish Elite Athletes in Relation to Sun Exposure and Oral Supplementation. PLoS ONE 2016, 11, e0164395. [Google Scholar] [CrossRef] [PubMed]

| Percentage or Mean | Parameters | |
|---|---|---|
| 69.65 ± 7.832 | Age (years) | |
| 85 (85%) | Women | Gender |
| 15 (15%) | Men | |
| 90 (90%) | Arab | Ancestor origin |
| 10 (10%) | Amazigh | |
| 1 (1%) | Single | Marital situation |
| 48 (48%) | Married | |
| 49 (49%) | Widow | |
| 2 (2%) | Divorced | |
| 40 (40%) | Illiterate | Scholar level |
| 35 (35%) | Autodidact | |
| 19 (19%) | Primary | |
| 3 (3%) | Secondary | |
| 3 (3%) | University | |
| 15 (15%) | With | Profession |
| 82 (82%) | Without | |
| 3 (3%) | Retired | |
| 26 (26%) | ≤2000 | Monthly income (MAD) |
| 61 (61%) | 2000–5000 | |
| 10 (10%) | 5000–8000 | |
| 3 (3%) | >8000 | |
| Percentages | Parameters | |
|---|---|---|
| 5 (5%) | Depressive | Depression |
| 95 (95%) | Non-depressive | |
| 48 (48%) | Yes | Sufferance of diseases |
| 52 (52%) | No | |
| 54 (54%) | Yes | Hospitalization |
| 46 (46%) | No | |
| 53 (53%) | Yes | Medication |
| 47 (47%) | No | |
| Percentages | Parameters | |
|---|---|---|
| 59 (59%) | Normal | Cognitive status |
| 26 (26%) | Mild cognitive impairment | |
| 15 (15%) | Moderate cognitive impairment | |
| 0 (0%) | Severe cognitive impairment | |
| Percentages | Parameters | |
|---|---|---|
| 72 (72%) | Adequate nutritional status | Nutritional status |
| 28 (28%) | Risk of malnutrition | |
| 0 (0%) | Severe malnutrition | |
| 9 (9%) | Underweight (<21) | Body mass index (kg/m2) |
| 20 (20%) | Normal weight (21 to 24.99) | |
| 35 (35%) | Overweight (≥25) | |
| 36 (36%) | Obesity (30–40) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sebbari, F.; Khallouki, F.; Salamatullah, A.M.; Bourhia, M.; Metouekel, A.; El Bouhali, B. Assessment of Vitamin D Status in the Drâa-Tafilalet Population (Morocco) Based on Sociodemographic, Health, and Nutritional Factors. Nutrients 2024, 16, 2118. https://doi.org/10.3390/nu16132118
Sebbari F, Khallouki F, Salamatullah AM, Bourhia M, Metouekel A, El Bouhali B. Assessment of Vitamin D Status in the Drâa-Tafilalet Population (Morocco) Based on Sociodemographic, Health, and Nutritional Factors. Nutrients. 2024; 16(13):2118. https://doi.org/10.3390/nu16132118
Chicago/Turabian StyleSebbari, Fouzia, Farid Khallouki, Ahmad Mohammad Salamatullah, Mohammed Bourhia, Amira Metouekel, and Bachir El Bouhali. 2024. "Assessment of Vitamin D Status in the Drâa-Tafilalet Population (Morocco) Based on Sociodemographic, Health, and Nutritional Factors" Nutrients 16, no. 13: 2118. https://doi.org/10.3390/nu16132118
APA StyleSebbari, F., Khallouki, F., Salamatullah, A. M., Bourhia, M., Metouekel, A., & El Bouhali, B. (2024). Assessment of Vitamin D Status in the Drâa-Tafilalet Population (Morocco) Based on Sociodemographic, Health, and Nutritional Factors. Nutrients, 16(13), 2118. https://doi.org/10.3390/nu16132118








