The Associations between Healthy Eating Patterns and Risk of Metabolic Dysfunction-Associated Steatotic Liver Disease: A Case–Control Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Assessment of Dietary Intake
2.3. Assessment of Covariates
2.4. Statistical Analysis
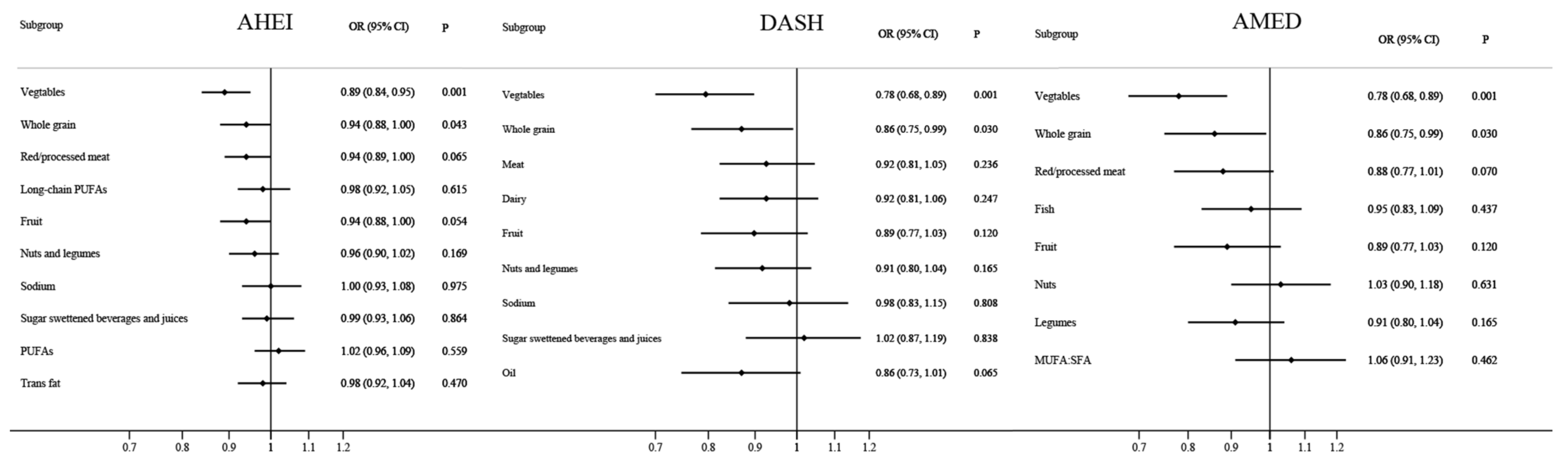
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rinella, M.E.; Lazarus, J.V.; Ratziu, V.; Francque, S.M.; Sanyal, A.J.; Kanwal, F.; Romero, D.; Abdelmalek, M.F.; Anstee, Q.M.; Arab, J.P.; et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. Ann. Hepatol. 2024, 29, 101133. [Google Scholar] [CrossRef]
- Riazi, K.; Azhari, H.; Charette, J.H.; Underwood, F.E.; King, J.A.; Afshar, E.E.; Swain, M.G.; Congly, S.E.; Kaplan, G.G.; Shaheen, A.A. The prevalence and incidence of NAFLD worldwide: A systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2022, 7, 851–861. [Google Scholar]
- Zhou, F.; Zhou, J.; Wang, W.; Zhang, X.-J.; Ji, Y.-X.; Zhang, P.; She, Z.-G.; Zhu, L.; Cai, J.; Li, H. Unexpected Rapid Increase in the Burden of NAFLD in China From 2008 to 2018: A Systematic Review and Meta-Analysis. Hepatology 2019, 70, 1119–1133. [Google Scholar]
- Estes, C.; Anstee, Q.M.; Arias-Loste, M.T.; Bantel, H.; Bellentani, S.; Caballeria, J.; Colombo, M.; Craxi, A.; Crespo, J.; Day, C.P.; et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016–2030. J. Hepatol. 2018, 69, 896–904. [Google Scholar]
- Ekstedt, M.; Hagström, H.; Nasr, P.; Fredrikson, M.; Stål, P.; Kechagias, S.; Hultcrantz, R. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology 2015, 61, 1547–1554. [Google Scholar] [CrossRef]
- Tapper, E.B.; Parikh, N.D. Mortality due to cirrhosis and liver cancer in the United States, 1999–2016: Observational study. BMJ 2018, 362, k2817. [Google Scholar] [CrossRef]
- Younossi, Z.M.; Zelber-Sagi, S.; Henry, L.; Gerber, L.H. Lifestyle interventions in nonalcoholic fatty liver disease. Nat. Rev. Gastroenterol. Hepatol. 2023, 20, 708–722. [Google Scholar]
- Romero-Gomez, M.; Zelber-Sagi, S.; Trenell, M. Treatment of NAFLD with diet, physical activity and exercise. J. Hepatol. 2017, 67, 829–846. [Google Scholar]
- Zelber-Sagi, S.; Ivancovsky-Wajcman, D.; Isakov, N.F.; Webb, M.; Orenstein, D.; Shibolet, O.; Kariv, R. High red and processed meat consumption is associated with non-alcoholic fatty liver disease and insulin resistance. J. Hepatol. 2018, 68, 1239–1246. [Google Scholar]
- Hu, F.B. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr. Opin. Lipidol. 2002, 13, 3–9. [Google Scholar]
- Cespedes, E.M.; Hu, F.B. Dietary patterns: From nutritional epidemiologic analysis to national guidelines. Am. J. Clin. Nutr. 2015, 101, 899–900. [Google Scholar] [CrossRef]
- Schulze, M.B.; Hu, F.B. Dietary patterns and risk of hypertension, type 2 diabetes mellitus, and coronary heart disease. Curr. Atheroscler. Rep. 2002, 4, 462–467. [Google Scholar]
- Park, S.Y.; Noureddin, M.; Boushey, C.; Wilkens, L.R.; Setiawan, V.W. Diet Quality Association with Nonalcoholic Fatty Liver Disease by Cirrhosis Status: The Multiethnic Cohort. Curr. Dev. Nutr. 2020, 4, nzaa024. [Google Scholar] [CrossRef]
- Xiao, M.L.; Lin, J.S.; Li, Y.H.; Liu, M.; Deng, Y.Y.; Wang, C.Y.; Chen, Y.M. Adherence to the Dietary Approaches to Stop Hypertension (DASH) diet is associated with lower presence of non-alcoholic fatty liver disease in middle-aged and elderly adults. Public Health Nutr. 2020, 23, 674–682. [Google Scholar] [CrossRef]
- Sun, Y.; Chen, S.; Zhao, X.; Wang, Y.; Lan, Y.; Jiang, X.; Gao, X.; Wu, S.; Wang, L. Adherence to the dietary approaches to stop hypertension diet and non-alcoholic fatty liver disease. Liver Int. 2022, 42, 809–819. [Google Scholar]
- Wu, Y.; Zheng, Q.; Zou, B.; Yeo, Y.H.; Li, X.; Li, J.; Xie, X.; Feng, Y.; Stave, C.D.; Zhu, Q.; et al. The epidemiology of NAFLD in Mainland China with analysis by adjusted gross regional domestic product: A meta-analysis. Hepatol. Int. 2020, 14, 259–269. [Google Scholar]
- Xie, X.; Guo, B.; Xiao, X.; Yin, J.; Wang, Z.; Jiang, X.; Li, J.; Long, L.; Zhou, J.; Zhang, N.; et al. Healthy dietary patterns and metabolic dysfunction-associated fatty liver disease in less-developed ethnic minority regions: A large cross-sectional study. BMC Public. Health 2022, 22, 118. [Google Scholar]
- National Workshop on Fatty Liver and Alcoholic Liver Disease; Chinese Society of Hepatology; Chinese Medical Association; Fatty Liver Expert Committee; Chinese Medical Doctor Association. Guidelines of prevention and treatment for nonalcoholic fatty liver disease: A 2018 update. Zhonghua Gan Zang Bing Za Zhi 2018, 26, 195–203. [Google Scholar]
- The Chinese Society of Hepatology of Chinese Medical Association. Guidelines for the Prevention and Treatment of metabolically related (non-alcoholic) fatty Liver Disease (Version 2024). Zhonghua Gan Zang Bing Za Zhi 2024, 32, 418–434. [Google Scholar]
- Cheng, Y.; Yan, H.; Dibley, M.J.; Shen, Y.; Li, Q.; Zeng, L. Validity and reproducibility of a semi-quantitative food frequency questionnaire for use among pregnant women in rural China. Asia Pac. J. Clin. Nutr. 2008, 17, 166–177. [Google Scholar]
- McCullough, M.L.; Willett, W.C. Evaluating adherence to recommended diets in adults: The Alternate Healthy Eating Index. Public. Health Nutr. 2006, 9, 152–157. [Google Scholar] [CrossRef]
- Appel, L.J.; Moore, T.J.; Obarzanek, E.; Vollmer, W.M.; Svetkey, L.P.; Sacks, F.M.; Bray, G.A.; Vogt, T.M.; Cutler, J.A.; Windhauser, M.M.; et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N. Engl. J. Med. 1997, 336, 1117–1124. [Google Scholar]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef]
- Shan, Z.; Li, Y.; Baden, M.Y.; Bhupathiraju, S.N.; Wang, D.D.; Sun, Q.; Rexrode, K.M.; Rimm, E.B.; Qi, L.; Willett, W.C.; et al. Association between Healthy Eating Patterns and Risk of Cardiovascular Disease. JAMA Intern. Med. 2020, 180, 1090–1100. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Alberti, K.G.; Zimmet, P.; Shaw, J.I.D.F. Epidemiology Task Force Consensus Group. The metabolic syndrome—A new worldwide definition. Lancet 2005, 366, 1059–1062. [Google Scholar]
- Baratta, F.; Pastori, D.; Polimeni, L.; Bucci, T.; Ceci, F.; Calabrese, C.; Ernesti, I.; Pannitteri, G.; Violi, F.; Angelico, F.; et al. Adherence to Mediterranean Diet and Non-Alcoholic Fatty Liver Disease: Effect on Insulin Resistance. Am. J. Gastroenterol. 2017, 112, 1832–1839. [Google Scholar] [CrossRef]
- Razavi Zade, M.; Telkabadi, M.H.; Bahmani, F.; Salehi, B.; Farshbaf, S.; Asemi, Z. The effects of DASH diet on weight loss and metabolic status in adults with non-alcoholic fatty liver disease: A randomized clinical trial. Liver Int. 2016, 36, 563–571. [Google Scholar]
- George, E.S.; Reddy, A.; Nicoll, A.J.; Ryan, M.C.; Itsiopoulos, C.; Abbott, G.; Johnson, N.A.; Sood, S.; Roberts, S.K.; Tierney, A.C. Impact of a Mediterranean diet on hepatic and metabolic outcomes in non-alcoholic fatty liver disease: The MEDINA randomised controlled trial. Liver Int. 2022, 42, 1308–1322. [Google Scholar] [CrossRef]
- Utzschneider, K.M.; Kahn, S.E. Review: The role of insulin resistance in nonalcoholic fatty liver disease. J. Clin. Endocrinol. Metab. 2006, 91, 4753–4761. [Google Scholar]
- Masarone, M.; Rosato, V.; Dallio, M.; Gravina, A.G.; Aglitti, A.; Loguercio, C.; Federico, A.; Persico, M. Role of Oxidative Stress in Pathophysiology of Nonalcoholic Fatty Liver Disease. Oxid. Med. Cell Longev. 2018, 2018, 9547613. [Google Scholar] [CrossRef]
- Peiseler, M.; Schwabe, R.; Hampe, J.; Kubes, P.; Heikenwalder, M.; Tacke, F. Immune mechanisms linking metabolic injury to inflammation and fibrosis in fatty liver disease—Novel insights into cellular communication circuits. J. Hepatol. 2022, 77, 1136–1160. [Google Scholar] [CrossRef]
- Polyzos, S.A.; Kountouras, J.; Mantzoros, C.S. Obesity and nonalcoholic fatty liver disease: From pathophysiology to therapeutics. Metabolism 2019, 92, 82–97. [Google Scholar]
- Tobias, D.K.; Hu, F.B.; Chavarro, J.; Rosner, B.; Mozaffarian, D.; Zhang, C. Healthful dietary patterns and type 2 diabetes mellitus risk among women with a history of gestational diabetes mellitus. Arch. Intern. Med. 2012, 172, 1566–1572. [Google Scholar]
- Luo, K.; Wang, X.; Zhang, G. Starch and beta-glucan in a whole-grain-like structural form improve hepatic insulin sensitivity in diet-induced obese mice. Food Funct. 2019, 10, 5091–5101. [Google Scholar] [CrossRef]
- Choudhury, P.; Samanta, S.K.; Bhattacharjee, S.; Sarma, H.; Devi, R. Chemical composite of indigenous whole grain scented joha rice varietal prevents type 2 diabetes in rats through ameliorating insulin sensitization by the IRS-1/AKT/PI3K signalling cascade. Food Funct. 2022, 13, 11879–11895. [Google Scholar]
- Gommers, L.M.; Hoenderop, J.G.; Bindels, R.J.; de Baaij, J.H. Hypomagnesemia in Type 2 Diabetes: A Vicious Circle? Diabetes 2016, 65, 3–13. [Google Scholar] [CrossRef]
- Aleksandrova, K.; Koelman, L.; Rodrigues, C.E. Dietary patterns and biomarkers of oxidative stress and inflammation: A systematic review of observational and intervention studies. Redox Biol. 2021, 42, 101869. [Google Scholar]
- Fung, T.T.; McCullough, M.L.; Newby, P.K.; Manson, J.E.; Meigs, J.B.; Rifai, N.; Willett, W.C.; Hu, F.B. Diet-quality scores and plasma concentrations of markers of inflammation and endothelial dysfunction. Am. J. Clin. Nutr. 2005, 82, 163–173. [Google Scholar] [CrossRef]
- Linnewiel-Hermoni, K.; Motro, Y.; Miller, Y.; Levy, J.; Sharoni, Y. Carotenoid derivatives inhibit nuclear factor kappa B activity in bone and cancer cells by targeting key thiol groups. Free Radic. Biol. Med. 2014, 75, 105–120. [Google Scholar]
- Nidhi, B.; Sharavana, G.; Ramaprasad, T.R.; Vallikannan, B. Lutein derived fragments exhibit higher antioxidant and anti-inflammatory properties than lutein in lipopolysaccharide induced inflammation in rats. Food Funct. 2015, 6, 450–460. [Google Scholar]
- Smethers, A.D.; Rolls, B.J. Dietary Management of Obesity: Cornerstones of Healthy Eating Patterns. Med. Clin. N. Am. 2018, 102, 107–124. [Google Scholar] [CrossRef]
- Crosby, L.; Rembert, E.; Levin, S.; Green, A.; Ali, Z.; Jardine, M.; Nguyen, M.; Elliott, P.; Goldstein, D.; Freeman, A.; et al. Changes in Food and Nutrient Intake and Diet Quality on a Low-Fat Vegan Diet Are Associated with Changes in Body Weight, Body Composition, and Insulin Sensitivity in Overweight Adults: A Randomized Clinical Trial. J. Acad. Nutr. Diet. 2022, 122, 1922–1939. [Google Scholar] [CrossRef]
- Azadi-Yazdi, M.; Karimi-Zarchi, M.; Salehi-Abargouei, A.; Fallahzadeh, H.; Nadjarzadeh, A. Effects of Dietary Approach to Stop Hypertension diet on androgens, antioxidant status and body composition in overweight and obese women with polycystic ovary syndrome: A randomised controlled trial. J. Hum. Nutr. Diet. 2017, 30, 275–283. [Google Scholar] [CrossRef]
- Jaruvongvanich, V.; Sanguankeo, A.; Riangwiwat, T.; Upala, S. Testosterone, Sex Hormone-Binding Globulin and Nonalcoholic Fatty Liver Disease: A Systematic Review and Meta-Analysis. Ann. Hepatol. 2017, 16, 382–394. [Google Scholar] [CrossRef]
- Kim, C.; Lee, J.; Kim, M.B.; Hwang, J.K. Hypoglycemic effect of whole grain diet in C57BL/KsJ-db/db mice by activating PI3K/Akt and AMPK pathways. Food Sci. Biotechnol. 2019, 28, 895–905. [Google Scholar] [CrossRef]
- Adams, M.R.; Golden, D.L.; Chen, H.; Register, T.C.; Gugger, E.T. A diet rich in green and yellow vegetables inhibits atherosclerosis in mice. J. Nutr. 2006, 136, 1886–1889. [Google Scholar] [CrossRef]
- Ayoub, H.M.; McDonald, M.R.; Sullivan, J.A.; Tsao, R.; Platt, M.; Simpson, J.; Meckling, K.A. The Effect of Anthocyanin-Rich Purple Vegetable Diets on Metabolic Syndrome in Obese Zucker Rats. J. Med. Food. 2017, 20, 1240–1249. [Google Scholar] [CrossRef]
- Hernaez, R.; Lazo, M.; Bonekamp, S.; Kamel, I.; Brancati, F.L.; Guallar, E.; Clark, J.M. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: A meta-analysis. Hepatology 2011, 54, 1082–1090. [Google Scholar]
- Ampuero, J.; Gallego-Duran, R.; Romero-Gomez, M. Association of NAFLD with subclinical atherosclerosis and coronary-artery disease: Meta-analysis. Rev. Esp. Enferm. Dig. 2015, 107, 10–16. [Google Scholar]


| Characteristics | No MASLD | MASLD | p Value |
|---|---|---|---|
| No. of participants | 228 | 228 | |
| Age, year | 48.3 (14.2) | 48.4 (13.9) | 0.950 |
| Men, n (%) | 122 (53.5) | 122 (53.5) | >0.999 |
| College and above, n (%) | 132 (57.9) | 129 (56.6) | 0.780 |
| Monthly household income (≥7000 yuan/capita) | 80 (35.1) | 87 (38.2) | 0.500 |
| Married/living together, n (%) | 201 (88.2) | 205 (89.9) | 0.550 |
| Smokers, n (%) | 30 (13.2) | 35 (15.4) | 0.500 |
| Physical activity, MET hours/week | 20.5 (4.6–49.5) | 22.4 (6.6–44.8) | 0.481 |
| BMI, kg/m2 | 22.5 (3.1) | 26.0 (3.2) | <0.001 |
| Triglyceride, (mmol/L) | 1.2 (0.9–1.5) | 2.0 (1.5–2.8) | <0.001 |
| Low-density lipoprotein cholesterol, (mmol/L) | 2.6 (2.2–3.1) | 2.9 (2.4–3.4) | <0.001 |
| High-density lipoprotein cholesterol, (mmol/L) | 1.3 (1.1–1.5) | 1.1 (0.9–1.2) | <0.001 |
| Total cholesterol, (mmol/L) | 4.7 (4.2–5.4) | 5.0 (4.5–5.8) | 0.002 |
| Fasting plasma glucose, (mmol/L) | 4.8 (4.5–5.1) | 5.0 (4.6–5.5) | <0.001 |
| Alanine aminotransferase, (U/L) | 16.4 (13.0–21.5) | 26.9 (18.6–40.0) | <0.001 |
| Aspartate aminotransferase, (U/L) | 19.8 (17.4–23.0) | 21.6 (18.0–27.0) | <0.001 |
| Hypertension, n (%) | 15 (6.6%) | 37 (16.2%) | 0.001 |
| Type 2 diabetes, n (%) | 6 (2.6%) | 12 (5.3%) | 0.150 |
| Total energy intake, (kcal/day) | 1723.0 (406.9) | 1817.9 (480.6) | 0.023 |
| Alternate Healthy Eating Index score | 51.9 (11.1) | 48.0 (11.9) | <0.001 |
| Dietary Approaches to Stop Hypertension score | 27.7 (4.8) | 26.3 (5.2) | 0.004 |
| Alternate Mediterranean Diet score | 24.7 (4.9) | 23.2 (5.1) | <0.001 |
| Variables | Tertiles of Dietary Score | Per 20-Percentile Increase in the Dietary Score | p-Values for Trend | ||
|---|---|---|---|---|---|
| 1 | 2 | 3 | |||
| Alternate Healthy Eating Index score | |||||
| Median score | 39 | 50 | 62 | ||
| No. of MASLD/No. of Non-MASLD | 96/61 | 77/76 | 55/91 | ||
| Age-adjusted OR (95% CI) | 1 | 0.60 (0.37 to 0.96) | 0.39 (0.24 to 0.63) | 0.55 (0.39 to 0.77) | <0.001 |
| Multivariable-adjusted OR (95% CI) * | 1 | 0.60 (0.37 to 0.97) | 0.38 (0.23 to 0.62) | 0.54 (0.38 to 0.76) | <0.001 |
| Fully adjusted OR (95% CI) † | 1 | 0.63 (0.39 to 1.03) | 0.40 (0.25 to 0.66) | 0.57 (0.40 to 0.80) | <0.001 |
| Dietary Approaches to Stop Hypertension score | |||||
| Median score | 22 | 27 | 33 | ||
| No. of MASLD/No. of Non-MASLD | 91/63 | 75/87 | 62/78 | ||
| Age-adjusted OR (95% CI) | 1 | 0.58 (0.36 to 0.94) | 0.54 (0.33 to 0.87) | 0.62 (0.45 to 0.87) | 0.012 |
| Multivariable-adjusted OR (95% CI) * | 1 | 0.57 (0.35 to 0.93) | 0.52 (0.32 to 0.86) | 0.60 (0.42 to 0.86) | 0.011 |
| Fully adjusted OR (95% CI) † | 1 | 0.50 (0.30 to 0.83) | 0.38 (0.22 to 0.66) | 0.48 (0.33 to 0.71) | 0.001 |
| Alternate Mediterranean Diet score | |||||
| Median score | 19 | 23 | 29 | ||
| No. of MASLD/No. of Non-MASLD | 91/60 | 74/68 | 63/100 | ||
| Age-adjusted OR (95% CI) | 1 | 0.71 (0.43 to 1.15) | 0.44 (0.28 to 0.70) | 0.63 (0.47 to 0.85) | <0.001 |
| Multivariable-adjusted OR (95% CI) * | 1 | 0.71 (0.44 to 1.16) | 0.43 (0.27 to 0.69) | 0.63 (0.46 to 0.84) | <0.001 |
| Fully adjusted OR (95% CI) † | 1 | 0.75 (0.46 to 1.24) | 0.46 (0.28 to 0.73) | 0.65 (0.48 to 0.88) | 0.001 |
| Variables | No. of Participants with Fibrosis/Participants with Fatty Liver/Participants without MASLD | Odds Ratio (95% CI) Based on Tertiles of Dietary Score | p-Values for Trend | ||
|---|---|---|---|---|---|
| 1 | 2 | 3 | |||
| Alternate Healthy Eating Index score | 35/193/228 | 1 | 0.71 (0.44 to 1.14) | 0.44 (0.27 to 0.73) | <0.001 |
| Dietary Approaches to Stop Hypertension score | 35/193/228 | 1 | 0.59 (0.36 to 0.95) | 0.49 (0.29 to 0.83) | 0.001 |
| Alternate Mediterranean Diet score | 35/193/228 | 1 | 0.91 (0.56 to 1.47) | 0.50 (0.31 to 0.82) | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, X.; Gan, D.; Fan, Y.; Fu, Q.; He, C.; Liu, W.; Li, F.; Ma, L.; Wang, M.; Zhang, W. The Associations between Healthy Eating Patterns and Risk of Metabolic Dysfunction-Associated Steatotic Liver Disease: A Case–Control Study. Nutrients 2024, 16, 1956. https://doi.org/10.3390/nu16121956
Huang X, Gan D, Fan Y, Fu Q, He C, Liu W, Li F, Ma L, Wang M, Zhang W. The Associations between Healthy Eating Patterns and Risk of Metabolic Dysfunction-Associated Steatotic Liver Disease: A Case–Control Study. Nutrients. 2024; 16(12):1956. https://doi.org/10.3390/nu16121956
Chicago/Turabian StyleHuang, Xia, Da Gan, Yahui Fan, Qihui Fu, Cong He, Wenjian Liu, Feng Li, Le Ma, Mingxu Wang, and Wei Zhang. 2024. "The Associations between Healthy Eating Patterns and Risk of Metabolic Dysfunction-Associated Steatotic Liver Disease: A Case–Control Study" Nutrients 16, no. 12: 1956. https://doi.org/10.3390/nu16121956
APA StyleHuang, X., Gan, D., Fan, Y., Fu, Q., He, C., Liu, W., Li, F., Ma, L., Wang, M., & Zhang, W. (2024). The Associations between Healthy Eating Patterns and Risk of Metabolic Dysfunction-Associated Steatotic Liver Disease: A Case–Control Study. Nutrients, 16(12), 1956. https://doi.org/10.3390/nu16121956







