The Role of Fresh Beef Intake and Mediterranean Diet Adherence during Pregnancy in Maternal and Infant Health Outcomes
Abstract
1. Introduction
2. Methods
2.1. Participants
2.2. Maternal and Infant Characteristics
2.3. Food Frequency Questionnaire
2.4. Supplement Intake
2.5. Beef Intake
2.6. Mediterranean Diet Adherence
2.7. Statistical Analysis
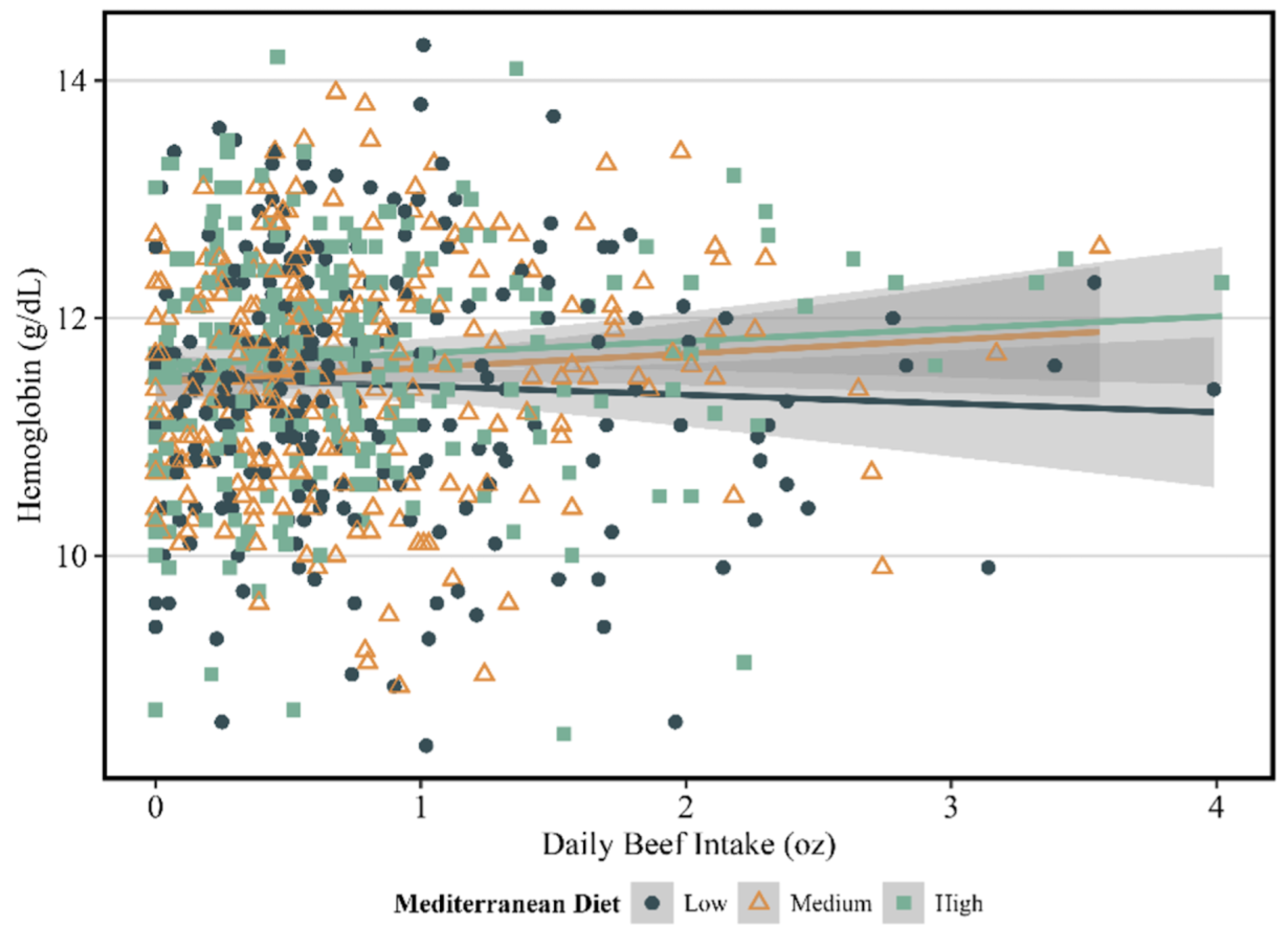
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bailey, R.L.; Pac, S.G.; Fulgoni, V.L., III; Reidy, K.C.; Catalano, P.M. Estimation of Total Usual Dietary Intakes of Pregnant Women in the United States. JAMA Netw. Open 2019, 2, e195967. [Google Scholar] [CrossRef] [PubMed]
- Geissler, C.; Singh, M. Iron, meat and health. Nutrients 2011, 3, 283–316. [Google Scholar] [CrossRef] [PubMed]
- McLean, E.; Cogswell, M.; Egli, I.; Wojdyla, D.; de Benoist, B. Worldwide prevalence of anaemia, WHO Vitamin and Mineral Nutrition Information System, 1993–2005. Public Health Nutr. 2009, 12, 444–454. [Google Scholar] [CrossRef]
- Force UPST. Iron Deficiency Anemia in Pregnant Women: Screening and Supplementation. 2015. Available online: https://www.uspreventiveservicestaskforce.org/uspstf/draft-recommendation/iron-deficiency-anemia-during-pregnancy-screening-supplementation (accessed on 29 February 2024).
- Dewey, K.G.; Oaks, B.M. U-shaped curve for risk associated with maternal hemoglobin, iron status, or iron supplementation. Am. J. Clin. Nutr. 2017, 106 (Suppl. 6), 1694s–1702s. [Google Scholar] [CrossRef] [PubMed]
- Georgieff, M.K. Iron deficiency in pregnancy. Am. J. Obstet. Gynecol. 2020, 223, 516–524. [Google Scholar] [CrossRef]
- Piskin, E.; Cianciosi, D.; Gulec, S.; Tomas, M.; Capanoglu, E. Iron Absorption: Factors, Limitations, and Improvement Methods. ACS Omega 2022, 7, 20441–20456. [Google Scholar] [CrossRef]
- Amati, F.; Hassounah, S.; Swaka, A. The Impact of Mediterranean Dietary Patterns During Pregnancy on Maternal and Offspring Health. Nutrients 2019, 11, 1098. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Wang, H.; Bian, J.; Xu, M.; Jiang, N.; Luo, W.; Zu, P.; Yin, W.; Zhu, P. Association between the Maternal Mediterranean Diet and Perinatal Outcomes: A Systematic Review and Meta-Analysis. Adv. Nutr. 2024, 15, 100159. [Google Scholar] [CrossRef]
- Sofi, F.; Macchi, C.; Abbate, R.; Gensini, G.F.; Casini, A. Mediterranean diet and health status: An updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr. 2014, 17, 2769–2782. [Google Scholar] [CrossRef]
- Kromhout, D.; Keys, A.; Aravanis, C.; Buzina, R.; Fidanza, F.; Giampaoli, S.; Jansen, A.; Menotti, A.; Nedeljkovic, S.; Pekkarinen, M. Food consumption patterns in the 1960s in seven countries. Am. J. Clin. Nutr. 1989, 49, 889–894. [Google Scholar] [CrossRef]
- Chen, X.; Zhao, D.; Mao, X.; Xia, Y.; Baker, P.N.; Zhang, H. Maternal Dietary Patterns and Pregnancy Outcome. Nutrients 2016, 8, 351. [Google Scholar] [CrossRef] [PubMed]
- Czerwonka, M.; Tokarz, A. Iron in red meat-friend or foe. Meat Sci. 2017, 123, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Givens, D.I. Review: Dairy foods, red meat and processed meat in the diet: Implications for health at key life stages. Animal 2018, 12, 1709–1721. [Google Scholar] [CrossRef] [PubMed]
- Gifford, C.L.; O’Connor, L.E.; Campbell, W.W.; Woerner, D.R.; Belk, K.E. Broad and Inconsistent Muscle Food Classification Is Problematic for Dietary Guidance in the U.S. Nutrients 2017, 9, 1027. [Google Scholar] [CrossRef]
- Carlson, S.E.; Gajewski, B.J.; Valentine, C.J.; Kerling, E.H.; Weiner, C.P.; Cackovic, M.; Buhimschi, C.S.; Rogers, L.K.; Sands, S.A.; Brown, A.R.; et al. Higher dose docosahexaenoic acid supplementation during pregnancy and early preterm birth: A randomised, double-blind, adaptive-design superiority trial. eClinicalMedicine 2021, 36, 100905. [Google Scholar] [CrossRef] [PubMed]
- Gustafson, K.M.; Christifano, D.N.; Hoyer, D.; Schmidt, A.; Carlson, S.E.; Colombo, J.; Mathis, N.B.; Sands, S.A.; Chollet-Hinton, L.; Brown, A.R.; et al. Prenatal docosahexaenoic acid effect on maternal-infant DHA-equilibrium and fetal neurodevelopment: A randomized clinical trial. Pediatr. Res. 2022, 92, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Meltzer, H.M.; Brantsaeter, A.L.; Ydersbond, T.A.; Alexander, J.; Haugen, M. Methodological challenges when monitoring the diet of pregnant women in a large study: Experiences from the Norwegian Mother and Child Cohort Study (MoBa). Matern. Child Nutr. 2008, 4, 14–27. [Google Scholar] [CrossRef] [PubMed]
- Cao, C.; O’Brien, K.O. Pregnancy and iron homeostasis: An update. Nutr. Rev. 2013, 71, 35–51. [Google Scholar] [CrossRef] [PubMed]
- de Onis, M.; Garza, C.; Onyango, A.W.; Rolland-Cachera, M.F. Les standards de croissance de l’Organisation mondiale de la santé pour les nourrissons et les jeunes enfants—[WHO growth standards for infants and young children]. Arch. Pediatr. 2009, 16, 47–53. [Google Scholar] [CrossRef]
- Diet History Questionnaire, Version 2.0; National Institutes of Health, Epidemiology and Genomics Research Program, National Cancer Institute: Bethesda, MD, USA, 2010.
- Diet*Calc Analysis Program, Version 1.5.0; National Cancer Institute, Epidemiology and Genomics Research Program: Bethesda, MD, USA, 2012.
- Taylor, M.K.; Mahnken, J.D.; Sullivan, D.K. NHANES 2011–2014 Reveals Cognition of US Older Adults may Benefit from Better Adaptation to the Mediterranean Diet. Nutrients 2020, 12, 1929. [Google Scholar] [CrossRef] [PubMed]
- Cheng, F.W.; Ford, N.A.; Taylor, M.K. US Older Adults That Consume Avocado or Guacamole Have Better Cognition Than Non-consumers: National Health and Nutrition Examination Survey 2011–2014. Original Research. Front. Nutr. 2021, 8, 746453. [Google Scholar] [CrossRef] [PubMed]
- Biesalski, H.K. Meat as a component of a healthy diet—Are there any risks or benefits if meat is avoided in the diet? Meat Sci. 2005, 70, 509–524. [Google Scholar] [CrossRef] [PubMed]
- Tong, T.Y.; Key, T.J.; Gaitskell, K.; Green, T.J.; Guo, W.; Sanders, T.A.; Bradbury, K.E. Hematological parameters and prevalence of anemia in white and British Indian vegetarians and nonvegetarians in the UK Biobank. Am. J. Clin. Nutr. 2019, 110, 461–472. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, L.E.; Paddon-Jones, D.; Wright, A.J.; Campbell, W.W. A Mediterranean-style eating pattern with lean, unprocessed red meat has cardiometabolic benefits for adults who are overweight or obese in a randomized, crossover, controlled feeding trial. Am. J. Clin. Nutr. 2018, 108, 33–40. [Google Scholar] [CrossRef]
- Galloway, R.; McGuire, J. Determinants of compliance with iron supplementation: Supplies, side effects, or psychology? Soc. Sci. Med. 1994, 39, 381–390. [Google Scholar] [CrossRef]
- Tessema, J.; Jefferds, M.E.; Cogswell, M.; Carlton, E. Motivators and barriers to prenatal supplement use among minority women in the United States. J. Am. Diet. Assoc. 2009, 109, 102–108. [Google Scholar] [CrossRef]
- Fonseca-Nunes, A.; Jakszyn, P.; Agudo, A. Iron and cancer risk—A systematic review and meta-analysis of the epidemiological evidence. Cancer Epidemiol. Biomark. Prev. 2014, 23, 12–31. [Google Scholar] [CrossRef]
- Hammerling, U.; Bergman Laurila, J.; Grafström, R.; Ilbäck, N.G. Consumption of Red/Processed Meat and Colorectal Carcinoma: Possible Mechanisms Underlying the Significant Association. Crit. Rev. Food Sci. Nutr. 2016, 56, 614–634. [Google Scholar] [CrossRef]
| Maternal Characteristics | Mean ± SD |
|---|---|
| Age | 30.1 ± 5.4 |
| Pre-Pregnancy BMI | 27.7 ± 7.1 |
| Race and Ethnicity | |
| White | 573 (68.4%) |
| Black or African American | 156 (18.6%) |
| Hispanic | 46 (5.5%) |
| Asian | 30 (3.6%) |
| Biracial: Black, White | 10 (1.2%) |
| Biracial: Asian, White | 7 (0.8%) |
| American Indian or Alaskan Native | 5 (0.5%) |
| Multiracial: Black, Native American, White | 3 (0.4%) |
| Other | 3 (0.4%) |
| Native Hawaiian or Other Pacific Islander | 2 (0.2%) |
| Biracial: Native American, White | 1 (0.1%) |
| Biracial: Black, Asian | 1 (0.1%) |
| Multiracial: Black, Asian, White | 1 (0.1%) |
| Anemia Diagnosis | 298 (35.6%) |
| Hemoglobin at ~20 Weeks | 11.6 ± 1.0 |
| Infant Characteristics | |
| Sex, Female | 395 (49.2%) |
| Gestational Age at Birth, Weeks | 38.4 ± 1.9 |
| Acceptable Gestational Age | 647 (81.2%) |
| Birth Weight, g | 3309.6 ± 560.7 |
| Birth Length, cm | 50.1 ± 3.9 |
| Head Circumference, cm | 34.1 ± 2.0 |
| All | Tertile 1: Beef Intake | Tertile 2: Beef Intake | Tertile 3: Beef Intake | p-Value | |
|---|---|---|---|---|---|
| n = 838 | (n = 280) | (n = 279) | (n = 279) | ||
| Energy (kcal/d) | 1996.2 ± 753.3 | 1803.6 ± 712.5 | 1842.3 ± 653.9 | 2343.4 ± 767.6 | <0.001 |
| Total fat (g/d) | 79.1 ± 31.9 | 66.9 ± 28.7 | 76.3 ± 27.4 | 94.2 ± 33.2 | <0.001 |
| Carbohydrates (g/d) | 251.6 ± 132.2 | 243.9 ± 143.5 | 222.1 ± 110.3 | 288.9 ± 132.2 | <0.001 |
| Protein (g/d) | 71.6 ± 28.6 | 59.5 ± 25.3 | 67.9 ± 23.7 | 87.5 ± 29.0 | <0.001 |
| Saturated fat (g/day) | 26.4 ± 11.8 | 21.8 ± 10.2 | 25.2 ± 9.8 | 32.4 ± 12.7 | <0.001 |
| Monounsaturated fat (g/d) | 30.3 ± 12.5 | 25.5 ± 11.4 | 29.5 ± 11.0 | 35.8 ± 12.8 | <0.001 |
| Polyunsaturated fat (g/d) | 15.4 ± 7.0 | 13.7 ± 6.9 | 14.9 ± 6.6 | 17.7 ± 7.0 | <0.001 |
| Dietary fiber (g/d) | 17.7 ± 8.4 | 16.7 ± 8.3 | 17.3 ± 8.2 | 19.2 ± 8.5 | 0.001 |
| Retinol (mcg/d) | 468.1 ± 262.4 | 436.3 ± 288.0 | 441.7 ± 235.3 | 526.5 ± 252.0 | <0.001 |
| Vitamin E (mg/d) | 9.2 ± 4.2 | 8.7 ± 4.2 | 9.1 ± 4.3 | 9.9 ± 3.9 | 0.003 |
| Vitamin K (mcg/d) | 200.4 ± 216.6 | 208.3 ± 224.6 | 194.8 ± 202.1 | 198.2 ± 222.9 | 0.75 |
| Vitamin C (mg/d) | 141.2 ± 132.7 | 152.3 ± 171.4 | 123.4 ± 108.0 | 147.9 ± 106.8 | 0.02 |
| Thiamin (B1) (mg/d) | 1.5 ± 0.6 | 1.4 ± 0.6 | 1.4 ± 0.6 | 1.7 ± 0.6 | <0.001 |
| Riboflavin (B2) (mg/d) | 2.3 ± 1.1 | 2.2 ± 1.1 | 2.2 ± 0.9 | 2.6 ± 1.2 | <0.001 |
| Niacin (mg/d) | 22.7 ± 12.4 | 19.9 ± 12.0 | 21.0 ± 9.1 | 27.1 ± 14.4 | <0.001 |
| Vitamin B6 (mg/d) | 2.2 ± 1.3 | 2.1 ± 1.3 | 2.0 ± 1.0 | 2.6 ± 1.5 | <0.001 |
| Folate (mcg/d) | 425.6 ± 187.8 | 410.6 ± 197.7 | 407.8 ± 180.6 | 458.6 ± 180.8 | 0.002 |
| Vitamin B12 (mg/d) | 5.1 ± 3.1 | 4.4 ± 2.9 | 4.6 ± 2.3 | 6.4 ± 3.4 | <0.001 |
| Calcium (mg/d) | 1153.3 ± 571.9 | 1112.9 ± 613.2 | 1079.3 ± 536.8 | 1267.6 ± 546.9 | <0.001 |
| Phosphorous (mg/d) | 1271.4 ± 510.2 | 1127.3 ± 477.3 | 1205.5 ± 471.3 | 1482.0 ± 513.1 | <0.001 |
| Magnesium (mg/d) | 329.7 ± 126.1 | 311.3 ± 120.3 | 321.2 ± 128.5 | 356.8 ± 125.2 | <0.001 |
| Iron (mg/d) | 14.3 ± 6.0 | 13.0 ± 5.9 | 13.4 ± 5.6 | 16.4 ± 5.8 | <0.001 |
| Zinc (mg/d) | 11.4 ± 4.6 | 9.7 ± 4.2 | 10.8 ± 4.1 | 13.9 ± 4.4 | <0.001 |
| Copper (mg/d) | 1.5 ± 0.6 | 1.4 ± 0.6 | 1.5 ± 0.6 | 1.7 ± 0.6 | <0.001 |
| Selenium (mcg/d) | 93.7 ± 38.8 | 78.9 ± 36.4 | 89.9 ± 33.1 | 112.3 ± 39.2 | <0.001 |
| Sodium (mg/d) | 3010.3 ± 1158.3 | 2569.4 ± 1061.7 | 2841.7 ± 966.4 | 3621.5 ± 1172.6 | <0.001 |
| Potassium (mg/d) | 2933.4 ± 1190.3 | 2740.3 ± 1162.6 | 2768.8 ± 1095.4 | 3291.9 ± 1231.2 | <0.001 |
| Choline (mg/d) | 317.2 ± 129.5 | 274.8 ± 125.0 | 299.4 ± 106.8 | 377.7 ± 132.7 | <0.001 |
| Total Fresh Beef (oz/day) | 0.8 ± 0.7 | 0.2 ± 0.1 | 0.6 ± 0.1 | 1.5 ± 0.7 | <0.001 |
| Unstandardized-Beta | Standard Error | p-Value | |
|---|---|---|---|
| Maternal Outcomes | |||
| Anemia a | −0.22 | 0.14 | 0.11 |
| Hemoglobin (~20 wks) | 0.09 | 0.06 | 0.12 |
| Infant Outcomes | |||
| Gestational age at birth | −0.13 | 0.10 | 0.20 |
| Length | 0.21 | 0.23 | 0.36 |
| Head circumference | −0.06 | 0.12 | 0.63 |
| AGA a | 0.20 | 0.17 | 0.25 |
| Total Beef with LowMedD | Total Beef with Medium MedD | Total Beef with High MedD | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Beta | SE | p-Value | Beta | SE | p-Value | Beta | SE | p-Value | |
| Maternal Outcomes | |||||||||
| Hemoglobin (~20 wks) | −0.09 | 0.08 | 0.30 | 0.13 | 0.08 | 0.10 | 0.19 | 0.08 | 0.01 |
| Infant Outcomes | |||||||||
| Gestational age at birth | −0.20 | 0.13 | 0.13 | −0.19 | 0.14 | 0.18 | −0.01 | 0.13 | 0.91 |
| Length | 0.06 | 0.20 | 0.76 | −0.05 | 0.22 | 0.83 | 0.28 | 0.20 | 0.17 |
| Head circumference | −0.08 | 0.15 | 0.59 | −0.07 | 0.16 | 0.67 | −0.01 | 0.15 | 0.92 |
| AGA a | 0.13 | 0.22 | 0.56 | 0.22 | 0.24 | 0.35 | 0.26 | 0.24 | 0.28 |
| Predictor | Odds Ratio | 95% CI | p-Value |
|---|---|---|---|
| Total Beef (oz): Low MedD | 1.15 | 0.81–1.64 | 0.44 |
| Total Beef (oz): Medium MedD | 0.69 | 0.46–0.99 | 0.05 |
| Total Beef (oz): High MedD | 0.62 | 0.41–0.89 | 0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Christifano, D.N.; Gustafson, K.M.; Carlson, S.E.; Mathis, N.B.; Brown, A.; Onuoha, O.; Taylor, M.K. The Role of Fresh Beef Intake and Mediterranean Diet Adherence during Pregnancy in Maternal and Infant Health Outcomes. Nutrients 2024, 16, 1436. https://doi.org/10.3390/nu16101436
Christifano DN, Gustafson KM, Carlson SE, Mathis NB, Brown A, Onuoha O, Taylor MK. The Role of Fresh Beef Intake and Mediterranean Diet Adherence during Pregnancy in Maternal and Infant Health Outcomes. Nutrients. 2024; 16(10):1436. https://doi.org/10.3390/nu16101436
Chicago/Turabian StyleChristifano, Danielle Nicole, Kathleen M. Gustafson, Susan E. Carlson, Nicole B. Mathis, Alexandra Brown, Obianuju Onuoha, and Matthew K. Taylor. 2024. "The Role of Fresh Beef Intake and Mediterranean Diet Adherence during Pregnancy in Maternal and Infant Health Outcomes" Nutrients 16, no. 10: 1436. https://doi.org/10.3390/nu16101436
APA StyleChristifano, D. N., Gustafson, K. M., Carlson, S. E., Mathis, N. B., Brown, A., Onuoha, O., & Taylor, M. K. (2024). The Role of Fresh Beef Intake and Mediterranean Diet Adherence during Pregnancy in Maternal and Infant Health Outcomes. Nutrients, 16(10), 1436. https://doi.org/10.3390/nu16101436







