Current Oncology Nutrition Care Practice in Southeast Asia: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Data Extraction
3. Results
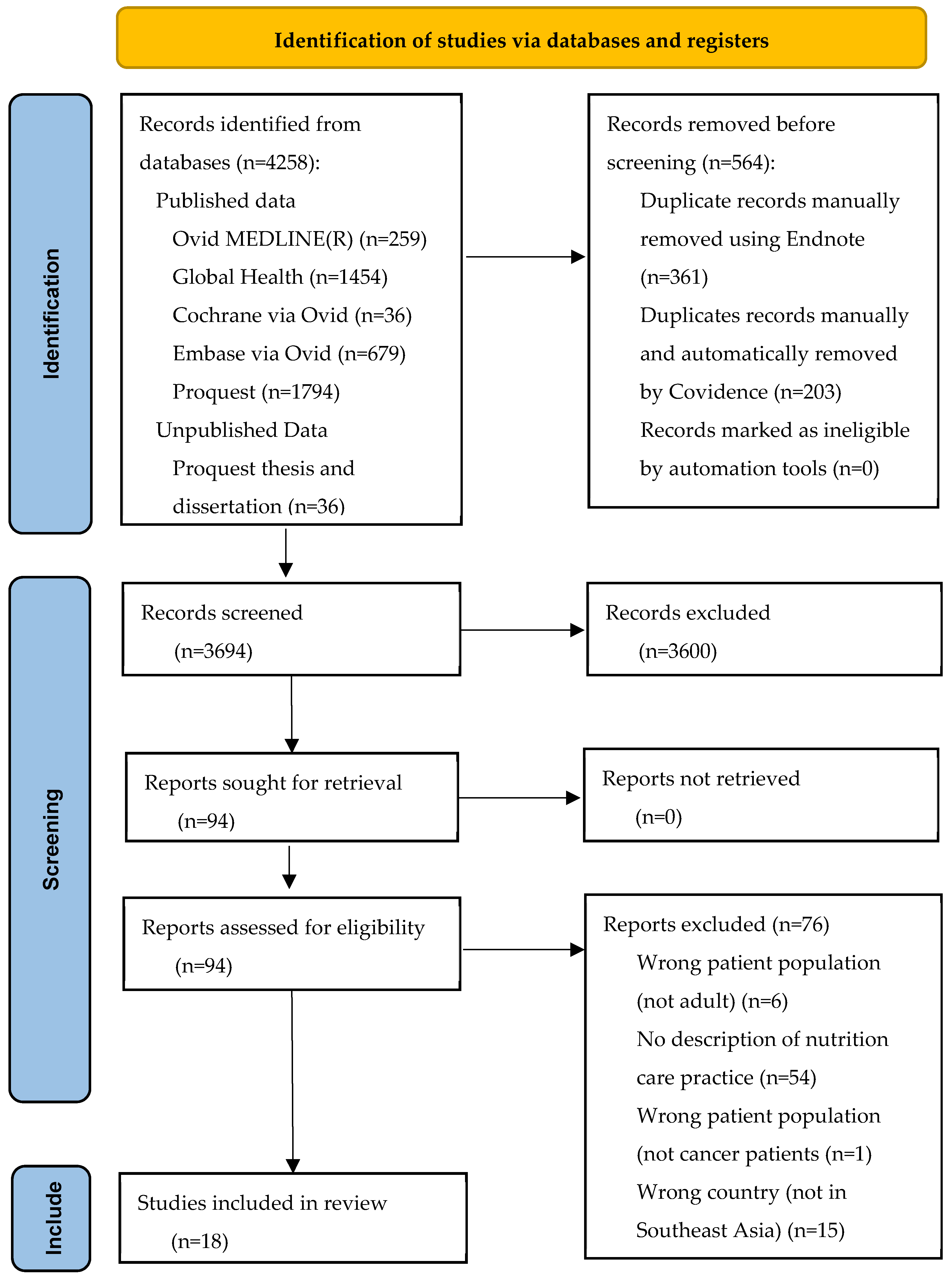
3.1. Search Result
3.2. Study Characteristics
3.3. Nutrition Screening
| Publication, Study Design, Sample Size | Cancer Treatment | Nutrition Care Provider | Nutrition Screening | Nutrition Assessment | Nutrition Intervention Current Practice | Nutrition Monitoring and Evaluation | Other Key Findings |
|---|---|---|---|---|---|---|---|
| A’zim et al. [32] Malaysia 2022 Study protocol for a pragmatic randomized control trial. | Gastrointestinal cancer. Major elective gastrointestinal and oncological surgery. No further details on treatment reported. | Dietitian | Malnutrition Screening Tool | Scored PG-SGA and triage based on score: 0–1: no intervention 2–3: health education 4–8: dietetic intervention ≥9: nutrition support. | Nutritional advice based on a guideline focused on the treatment of symptoms (nausea, vomiting, loss of appetite, diarrhea) provided by medical professionals or nurses. Patients with moderate and severe malnutrition referred to a dietitian for nutrition counseling. No routine pre/postoperative ONS. | Preoperative nutritional status monitored via phone. | - |
| Loan et al. [33] Vietnam 2018 Retrospective cohort study (n = 459) | Colorectal (n = 291), gastric (n = 149), esophageal (n = 19) cancer. Major curative surgery. Patients having chemo- or radiotherapy excluded. | Dietitian | - | Preoperative malnutrition defined as underweight classification or hypoalbuminemia within 30 days pre-surgery (via retrospective medical record review). | No preoperative hospital nutrition support due to routine overcrowding (even when clinically indicated). No details on post-operative nutritional support | - | Lack of license system for dietitians. Health insurance did not cover the cost of nutrition treatment. Poor people cannot afford enteral formula. |
| Chen et al. [34] Singapore 2012 Pre- and post-implementation audit (n = 24) | Oncological and hematological malignancy. Chemotherapy. No further details provided. | Dietitian | No nutritional screening within 24 h of admission. 3-MinNS was introduced to nurses by dietitians and incorporated into the nursing admission assessment form. Language barrier on nutritional screening solved with a colleague’s help. | 3-MinNS component (weight, food intake—meals, oral supplement, or tube feeding- and muscle wastage) assessed to determine its score. | - | - | No dietitian referral initiated on admission by medical professionals. Online system used during admission for referral to dietitians by medical professionals and nurses. |
| Cuong et al. [35] Vietnam 2018 Prospective observational Study (total n = 883, n = 44 cancer) | No cancer type or treatment type reported. | Nutrition and dietetics department staff. | Policies and guidelines to identify and manage hospital malnutrition were in the preliminary stage of development and implementation, | - | No hospital food provided as routine care. Food purchased from hospital canteen, outside hospital, or brought from home. | - | - |
| Hanna et al. [36] Vietnam 2016 Prospective observational study (total n = 372, n = 8 cancer) | No cancer type reported. Various treatments. | Dietitians | - | Subjective Global Assessment. Weight measured by calibrated body composition analyzer, (Thong Nat Hospital) or self-reported (Can Tho Hospital) | Thong Nhat Hospital: nutrition department and food service providing meals. Can Tho Hospital: No food service providing meals. | - | Lack of hospital food service infrastructure, less developed nutrition services, and a lack of health insurance funding for hospital food. |
| Han et al. [37] Malaysia 2018 Clinical audit (n = 739 (patients), n = 18 (nurses), n = 15 (medical professional)). | No cancer type or treatment type reported. | Dietitians | MST completed by nurse at outpatient appointment (new or follow up visit). Nurse completed a bilingual (English-Malay) electronic MST questionnaire. Nurse informed the attending medical professional to complete an EMR dietitian referral. | - | - | - | Dietitian referrals based on MST scores or on medical professionals’ clinical judgement. Referral policy changed from medical professionals to auto-referral, where nurses directly schedule dietitian appointments in an electronic system). |
| Kay et al. [38] Malaysia 2020 Prospective observational study (n = 50) | Head and neck cancer. Prior to radiotherapy and concurrent chemotherapy and radiotherapy. | Dietitians | - | Patients only referred to dietitians when having inadequate dietary intake during treatment. PG-SGA and one day 24 h recall used. No further information on routine practice. | Only 32.1% of malnourished patients referred to a dietitian on admission for nutrition management. No information on nutritional intervention provided. | - | A total of 67.9% of malnourished patients had no dietitian referral. No information on how dietitian referral conducted. |
| Kiew et al. [39] Malaysia 2022 Qualitative study (interviews) (n = 20) | Breast cancer. Post-primary treatment (surgery, chemotherapy, hormonal therapy, radiotherapy). | Dietitians and Nutritionists | - | - | Three of 20 patients met with the dietitian because of other medical conditions requiring dietary counseling (e.g., a healthy eating recommendation). One patient reported that different recommendations were provided by medical professionals and nutritionists. | - | - |
| Kiew et al. [40] Malaysia 2022 Prospective cohort study (n = 112) | Breast cancer. 9–15 months post-treatment (surgery, chemotherapy, hormonal therapy, radiotherapy). | Dietitians | - | - | Lack of dietary guidance from dietitians or clinicians post-active treatment. | - | - |
| Krishnasamy et al. [41] Malaysia 2017 Prospective observational study (n = 132) | Gastrointestinal (n = 44), breast (n = 20), sarcoma (n = 20), head and neck (n = 14), lung (n = 15), hematologic (n = 7), thyroid (n = 5), genitourinary (n = 4), and gynecologic (n = 3) cancers. No cancer treatment prior to study | Dietitians and nutritionists. | - | Subjective Global Assessment | - | - | Severely malnourished patients commonly referred to dietitians or nutritionists. No further information reported on how dietitian referral was conducted. |
| Huong et al. [42] Vietnam 2021 Quasi-experimental study (n = 120) | Stomach and colon cancer. Chemotherapy. | Dietitians and nutritionists | MST within 24 h of admission. | Nutritional status using anthropometric measurement (weight, BMI, % weight loss, MUAC, muscle mass, fat mass), PG-SGA, and laboratory measurement (albumin, prealbumin, total protein). | Nutrition counseling. No further details available. | - | Limited guidelines in nutritional support for patients with cancer in Vietnam. |
| Lohsiriwat V. [43] Thailand 2014 Prospective observational study (n = 149) | Colorectal adenocarcinoma. Elective surgical resection within the ERAS program. | Dietitians or nutritionists | - | Subjective Global Assessment on Admission. | No particular nutrition support protocol for malnourished patients within the modified ERAS program. No preoperative enteral fluid and carbohydrate loading as recommended in the ERAS pathway included in the modified ERAS program. ONS provided during early postoperative period for patients with inadequate food intake and no dietitian input. | - | - |
| Menon et al. [44] Malaysia 2014 Prospective observational study (n = 70) | Digestive organs (n = 22), breast (n = 13), thyroid (n = 9), respiratory system (n = 8), genitourinary (n = 6), and others, i.e., bone, cervix, head and neck, blood, and bladder cancers (n = 12). Newly diagnosed, pre-treatment. | Dietitians | Nutrition screening rarely performed. | - | - | Recommendations for evaluation of nutritional status using standardized protocol existed but were neglected in routine practice. | Terminally ill patients with severe malnourished cancer often referred to dietitians. |
| Sowerbutts et al. [45] Philippines 2022 Qualitative semi-structured interviews and focus groups (n = 2 (nurses), 10 (dietitians or nutritionists), 3 (oncologists), 1 (study coordinator), 8 (surgeons), 10 (patients)). Not all health professionals came from the Philippines. | Healthcare professionals and patients on a surgical cancer ward. No information on cancer type and treatment provided. | Dietitians or Nutritionists | A junior resident or nurse conducted screening using a Nutrition Risk Assessment. Staff missed performing screening due to the old chart not being included in the EMR. Nurses trained by dietitians in the use of screening tools. | The initial assessment occurred with outpatients. Nutritional Risk Assessment combined subjective with objective methods. Patients routinely weighed. | Nutritional advice provided to outpatients by nutritionists. Parenteral nutrition occasionally used. Patients received meals daily, however, purchased additional food as a supplement. Supply of readymade supplements occasionally ran out. ONS inconsistently supplied to or consumed by outpatients. | Patients did not attend the healthcare facility for the sole purpose of nutritional assessment or monitoring. | Patients referred to a dietitian as an outpatient. |
| Velasco et al. [46] Philippine 2022 Prospective observational study (n = 292) | Colorectal cancer. Active treatment: chemotherapy, pre- or post-surgery, or radiotherapy) | Dietitians | - | Formal nutrition assessment not performed in the Philippine General Hospital-Cancer Institute. | - | - | Only 17% of patients referred by attending medical professionals to the dietary service for counseling. |
| Wong et al. [47] Malaysia 2021 Study Protocol for an open labeled randomized controlled trial. | Breast and colorectal cancer. Elective surgery. | Dietitians | - | Preoperative: Patients received nutrition counseling and a meal plan from a dietitian. Postoperative: the patients received ONS (milk powder drink) until discharged. | - | Milk-based ONS provided postoperatively: 4 leveled scoops of powder (55 g) into 210 mL of lukewarm water. Patients required to consume three servings of ONS per day (750 kcal and 33 g protein per day). | |
| Wong et al. [48] Malaysia 2022 Open-label, multi-arm, parallel-group randomized controlled trial (n = 91) | Breast and colorectal cancer. Elective surgery. | Not reported | - | - | Patients received usual diet preoperatively and provided with ONS postoperatively (three servings per day) until discharge. | - | - |
| Abu Zaid et al. [49] Malaysia 2016 Open-label randomized controlled trial (n = 42) | Colorectal cancer. Chemotherapy | Oncologist or nurse, and service dietitian | - | - | Oncologists or nurses gave guideline-based general nutritional advice verbally, visually, and written, focused on symptom treatment. Malnourished patients referred to a service dietitian for dietary counseling. | - | - |
3.4. Dietitian Referral
3.5. Assessment Practices
3.6. Intervention Practices
3.7. Nutrition Monitoring and Evaluation Practices
3.8. Barriers to Accessing and Providing Nutritional Care
3.9. Enablers in Accessing and Providing Nutritional Care
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Nishikawa, H.; Goto, M.; Fukunishi, S.; Asai, A.; Nishiguchi, S.; Higuchi, K. Cancer cachexia: Its mechanism and clinical significance. Int. J. Mol. Sci. 2021, 22, 8491. [Google Scholar] [CrossRef] [PubMed]
- Hanna, L.; Nguo, K.; Furness, K.; Porter, J.; Huggins, C.E. Association between skeletal muscle mass and quality of life in adults with cancer: A systematic review and meta-analysis. J. Cachexia Sarcopenia 2022, 13, 839–857. [Google Scholar] [CrossRef] [PubMed]
- Zacharias, C.; Zacharias, T. Outcome 1 year after digestive surgery in malnourished, elderly patients, with an emphasis on quality of life analysis. Can. J. Surg. 2013, 56, 128–134. [Google Scholar] [CrossRef]
- Arends, J. Malnutrition in cancer patients: Causes, consequences and treatment options. Eur. J. Surg. Oncol. 2023, 50, 107074. [Google Scholar] [CrossRef] [PubMed]
- Omlin, A.; Blum, D.; Wierecky, J.; Haile, S.R.; Ottery, F.D.; Strasser, F. Nutrition impact symptoms in advanced cancer patients: Frequency and specific interventions, a case-control study. J. Cachexia Sarcopenia 2013, 4, 55–61. [Google Scholar] [CrossRef]
- Crowder, S.L.; Douglas, K.G.; Pepino, M.Y.; Sarma, K.P.; Arthur, A.E. Nutrition impact symptoms and associated outcomes in post-chemoradiotherapy head and neck cancer survivors: A systematic review. J. Cancer Surviv. 2018, 12, 479–494. [Google Scholar] [CrossRef]
- de Pinho, N.B.; Martucci, R.B.; Rodrigues, V.D.; D’Almeida, C.A.; Thuler, L.C.S.; Saunders, C.; Jager-Wittenaar, H.; Peres, W.A.F. Malnutrition associated with nutrition impact symptoms and localization of the disease: Results of a multicentric research on oncological nutrition. Clin. Nutr. 2019, 38, 1274–1279. [Google Scholar] [CrossRef]
- Liposits, G.; Orrevall, Y.; Kaasa, S.; Österlund, P.; Cederholm, T. Nutrition in cancer care: A brief, practical guide with a focus on clinical practice. JCO Oncol. Pract. 2021, 17, e992–e998. [Google Scholar] [CrossRef]
- Viana, E.C.R.d.M.; Oliveira, I.d.S.; Rechinelli, A.B.; Marques, I.L.; Souza, V.F.d.; Spexoto, M.C.B.; Pereira, T.S.S.; Guandalini, V.R. Malnutrition and nutrition impact symptoms (NIS) in surgical patients with cancer. PLoS ONE 2020, 15, e0241305. [Google Scholar] [CrossRef]
- de Melo Silva, F.R.; de Oliveira, M.G.O.A.; Souza, A.S.R.; Figueroa, J.N.; Santos, C.S. Factors associated with malnutrition in hospitalized cancer patients: A croos-sectional study. Nutr. J. 2015, 14, 123. [Google Scholar] [CrossRef]
- Muscaritoli, M.; Arends, J.; Bachmann, P.; Baracos, V.; Barthelemy, N.; Bertz, H.; Bozzetti, F.; Hütterer, E.; Isenring, E.; Kaasa, S.; et al. ESPEN practical guideline: Clinical Nutrition in cancer. Clin. Nutr. 2021, 40, 2898–2913. [Google Scholar] [CrossRef] [PubMed]
- Arends, J.; Bachmann, P.; Baracos, V.; Barthelemy, N.; Bertz, H.; Bozzetti, F.; Fearon, K.; Hütterer, E.; Isenring, E.; Kaasa, S.; et al. ESPEN guidelines on nutrition in cancer patients. Clin. Nutr. 2017, 36, 11–48. [Google Scholar] [CrossRef]
- Cintakaweni, D.M.W.; Hariani, R.; Sutandyo, N.; Jayusman, A.M.; Ranuhardy, D.; Herawati, C.; Hanafi, W.L. The prevalence of malnutrition in 5 big cancer in Indonesia. Clin. Nutr. 2020, 40, 663. [Google Scholar] [CrossRef]
- Sing, L.S.; Vanoh, D. Malnutrition among cancer patients: Role of social support. Malays. J. Public Health Med. 2022, 22, 182–192. [Google Scholar] [CrossRef]
- Van Tap, N.; Bang, H.T.; Huong, D.T.; Chi, P.C.; Anh, L.T.N. Malnutrition in hospitalized cancer patients: A single-center, cross-sectional study in Southern Vietnam. SAGE Open Med. 2023, 11, 20503121231171491. [Google Scholar] [CrossRef] [PubMed]
- Susetyowati, S.; Sarasati, R.M.; Rizqi, F.; Sanubari, N.D.G.; Nuraini, A. Determining the valid tools to screen malnutrition in cancer patients: A comparison to Patient Generated-Subjective Global Assessment (PG-SGA). J. Gizi Indones. (Indones. J. Nutr.) 2022, 11, 8. [Google Scholar] [CrossRef]
- Prado, C.M.; Laviano, A.; Gillis, C.; Sung, A.D.; Gardner, M.; Yalcin, S.; Dixon, S.; Newman, S.M.; Bastasch, M.D.; Sauer, A.C.; et al. Examining guidelines and new evidence in oncology nutrition: A position paper on gaps and opportunities in multimodal approaches to improve patient care. Support Care Cancer 2022, 30, 3073–3083. [Google Scholar] [CrossRef] [PubMed]
- Indonesia Population (Live). Available online: https://www.worldometers.info/world-population/indonesia-population/#:~:text=The%20current%20population%20of%20Indonesia,of%20the%20total%20world%20population (accessed on 8 January 2024).
- Sebaran Tenaga Kesehatan Prioritas Teregistrasi di RS dan Puskesmas (Distribution of Prioritized Registered Health Professional in Hospital and Public Health Center). Available online: https://ditjen-nakes.kemkes.go.id/ (accessed on 8 January 2024).
- Rencana Pengembangan Tenaga Kesehatan Tahun 2011–2025 (Health Personal Development Plan 2011–2025). Keputusan Menteri Koordinator Bidang Kesejahteraan Rakyat Nomor 54 Tahun 2013 (Decision of the Coordinating Minister for People’s Welfare of The Republic of Indonesia. 2013; p. 32. Available online: https://www.academia.edu/44562691/KEPMENKOKESRA_54_TH (accessed on 21 September 2023).
- Siopis, G.; Jones, A.; Allman-Farinelli, M. The dietetic workforce distribution geographic atlas provides insight into the inequitable access for dietetic services for people with type 2 diabetes in Australia. Nutr. Diet. 2020, 77, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Lacey, K.; Pritchett, E. Nutrition care process and model: ADA adopts road map to quality care and outcomes management. J. Am. Diet. Assoc. 2003, 103, 1061–1072. [Google Scholar] [CrossRef]
- Thompson, K.L.; Davidson, P.; Swan, W.I.; Hand, R.K.; Rising, C.; Dunn, A.V.; Lewis, N.; Murphy, W.J. Nutrition care process chains: The “missing link” between research and evidence-based practice. J. Acad. Nutr. Diet. 2015, 115, 1491–1498. [Google Scholar] [CrossRef]
- Writing Group of the Nutrition Care Process/Standardized Language Committee. Nutrition care process part II: Using the International Dietetics and Nutrition Terminology to document the nutrition care process. J. Am. Diet. Assoc. 2008, 108, 1287–1293. [Google Scholar] [CrossRef] [PubMed]
- Swan, W.I.; Pertel, D.G.; Hotson, B.; Lloyd, L.; Orrevall, Y.; Trostler, N.; Vivanti, A.; Howarter, K.B.; Papoutsakis, C. Nutrition Care Process (NCP) Update Part 2: Developing and Using the NCP Terminology to Demonstrate Efficacy of Nutrition Care and Related Outcomes. J. Acad. Nutr. Diet. 2019, 119, 840–855. [Google Scholar] [CrossRef]
- Kemp, J.D.; Hamady, C.M.; Ludy, M.-J. Data Analysis Outside of Clinical Practice: An Innovative Application of the Nutrition Care Process and Model. J. Acad. Nutr. Diet. 2022, 122, 500–505. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.J.; Alexander, L.; Marnie, C.; Tricco, A.C.; McInerney, P.; Pollock, D.; Godfrey, C.M.; Munn, Z.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef]
- Godin, K.; Stapleton, J.; Kirkpatrick, S.I.; Hanning, R.M.; Leatherdale, S.T. Applying systematic review search methods to the grey literature: A case study examining guidelines for school-based breakfast programs in Canada. Syst. Rev. 2015, 4, 138. [Google Scholar] [CrossRef] [PubMed]
- The EndNote Team. EndNote. EndNote 21. Philadelphia, PA. 2013. Available online: https://support.clarivate.com/Endnote/s/article/Download-EndNote?language=en_US&language%C2%BCen_US.= (accessed on 22 March 2024).
- Covidence Systematic Review Software. Veritas Health Innovation, Melbourne, Australia. Available online: www.covidence.org (accessed on 24 January 2024).
- A’zim, A.I.Z.A.; Zaid, Z.A.; Yusof, B.N.M.; Jabar, M.F.; Shahar, A.S.M. Effectiveness of intensive perioperative nutrition therapy among adults undergoing gastrointestinal and oncological surgery in a public hospital: Study protocol for a pragmatic randomized control trial. Trials 2022, 23, 961. [Google Scholar] [CrossRef]
- Loan, B.T.H.; Nakahara, S.; Tho, B.A.; Dang, T.N.; Anh, L.N.; Huy, N.D.; Ichikawa, M. Nutritional status and postoperative outcomes in patients with gastrointestinal cancer in Vietnam: A retrospective cohort study. Nutrition 2018, 48, 117–121. [Google Scholar] [CrossRef]
- Chen, X.; Ang, E.; Bte Nasir, N. Nutritional screening among patients with cancer in an acute care hospital: A best practice implementation project. Int. J. Evid. Based Healthc. 2012, 10, 4. [Google Scholar] [CrossRef]
- Cuong, T.Q.; Banks, M.; Hannan-Jones, M.; Ngoc Diep, D.T.; Gallegos, D. Prevalence and associated risk factors of malnutrition among hospitalized adults in a multisite study in Ho Chi Minh city Viet Nam. Asia Pac. J. Clin. Nutr. 2018, 27, 986–995. [Google Scholar] [CrossRef]
- Hanna, K.L.; Glen, K.D.; Lau, B.T.; Tran, C.Q.; Truong, N.T.; Gallegos, D. Relationship between malnutrition and selected risk factors in two hospitals in Vietnam. Nutr. Diet. 2016, 73, 59–66. [Google Scholar] [CrossRef]
- Han, N.W.; Jamhuri, N.; Rahman, Z.A.; Sharina, B.; Lai, M.H.; Samwil, S.N.M. Clinical audit on adherence to using Malnutrition Screening Tool and dietitian referral in the Oncology Outpatient Clinic, National Cancer Institute, Malaysia. Malays. J. Nutr. 2018, 24, 4. [Google Scholar]
- Kay, N.M.; Zaid, Z.A.; Rahman, Z.A.; Jamhuri, N.; Kahairudin, Z.; Samwil, S.N.A.; Abdullah, A.; Yi, H.C.; Lai, B.S.H.; Han, N.W.; et al. Factors associated with malnutrition among head and neck cancer in-patients before radiotherapy in National Cancer Institute, Putrajaya. Malays. J. Nutr. 2020, 26, 257–271. [Google Scholar] [CrossRef]
- Kiew, S.J.; Majid, H.A.; Mohd Taib, N.A. A qualitative exploration: Dietary behaviour of Malaysian breast cancer survivors. Eur. J. Cancer Care 2022, 31, e13530. [Google Scholar] [CrossRef]
- Kiew, S.J.; Mohd Taib, N.A.; Islam, T.; Abdul Majid, H. Changes in dietary intake of breast cancer survivors: Early findings of a Malaysian breast cancer prospective cohort study. Nutr. Cancer 2022, 74, 2470–2478. [Google Scholar] [CrossRef] [PubMed]
- Krishnasamy, K.; Yoong, T.L.; Chan, C.M.; Choong, L.P.; Chinna, K. Identifying malnutrition: Nutritional status in newly diagnosed patients with cancer. Clin. J. Oncol. Nurs. 2017, 21, E23–E29. [Google Scholar] [CrossRef] [PubMed]
- Huong, L.T.; Phuong, D.T.; Anh, D.K.; Toi, P.L.; Anh, N.L.T.; Huy, T.L.; Linh, N.T. Nutritional intervention improves nutrition outcomes in stomach and colon cancer patients receiving chemotherapy: Finding from a quasi-experiment in Vietnam. Healthcare 2021, 9, 843. [Google Scholar] [CrossRef] [PubMed]
- Lohsiriwat, V. The influence of preoperative nutritional status on the outcomes of an enhanced recovery after surgery (ERAS) programme for colorectal cancer surgery. Tech. Coloproctol. 2014, 18, 1075–1080. [Google Scholar] [CrossRef]
- Menon, K.; Razak, S.A.; Ismail, K.A.; Krishna, B.V.M. Nutrient intake and nutritional status of newly diagnosed patients with cancer from the East Coast of Peninsular Malaysia. BMC Res. Notes 2014, 7, 680. [Google Scholar] [CrossRef]
- Sowerbutts, A.M.; Knight, S.R.; Lapitan, M.C.M.; Qureshi, A.U.; Maimbo, M.; Yenli, E.M.T.-A.; Tabiri, S.; Ghosh, D.; Kingsley, P.A.; Sundar, S.; et al. A Qualitative Exploration of Nutrition Screening, Assessment and Oral Support Used in Patients Undergoing Cancer Surgery in Low- and Middle-Income Countries. Nutrients 2022, 14, 863. [Google Scholar] [CrossRef]
- Velasco Jr, R.N.; Catedral, L.I.G.; Chua, A.V., Jr.; Hernandez, A.R.B.; King, R.E.C.; Leones, L.M.B.; Mondragon, K.A.M.; Ting, F.I.L.; Callueng, J.M.C.; Tampo, M.M.T.; et al. The impact of malnutrition on the quality of life of colorectal cancer patients in a tertiary hospital. Nutr. Cancer 2022, 74, 2937–2945. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.X.; Chen, S.T.; Ong, S.H.; Shyam, S.; Kandasami, P.; Chee, W.S.S. Study protocol for an open labelled randomised controlled trial of perioperative oral nutrition supplement in breast and colorectal cancer patients undergoing elective surgery. Trials 2021, 22, 767. [Google Scholar] [CrossRef] [PubMed]
- Wong, T.X.; Wong, W.X.; Chen, S.T.; Ong, S.H.; Shyam, S.; Ahmed, N.; Hamdan, K.H.; Awang, R.R.; Ibrahim, M.R.; Palayan, K.; et al. Effects of perioperative oral nutrition supplementation in Malaysian patients undergoing elective surgery for breast and colorectal cancers-a randomised controlled trial. Nutrients 2022, 14, 615. [Google Scholar] [CrossRef]
- Abu Zaid, Z.; Jackson, K.; Kandiah, M.; Cobiac, L. Improving the nutritional status of patients with colorectal cancer undergoing chemotherapy through intensive individualised diet and lifestyle counselling. Malays. J. Nutr. 2016, 22, 65–79. [Google Scholar]
- Ferguson, M.; Capra, S.; Bauer, J.; Banks, M. Development of a valid and reliable malnutrition screening tool for adult acute hospital patients. Nutrition 1999, 15, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.-L.; Tong, C.-Y.; Ang, E.; Lee, E.J.-C.; Loke, W.-C.; Chen, Y.; Ferguson, M.; Daniels, L. Development and validation of 3-Minute Nutrition Screening (3-MinNS) tool for acute hospital patients in Singapore. Asia Pac. J. Clin. Nutr. 2009, 18, 395–403. Available online: https://apjcn.nhri.org.tw/server/APJCN/18/3/395.pdf (accessed on 16 January 2024).
- Kondrup, J.; Rasmussen, H.H.; Hamberg, O.; Stanga, Z. Nutritional risk screening (NRS 2002): A new method based on an analysis of controlled clinical trials. Clin. Nutr. 2003, 22, 321–336. [Google Scholar] [CrossRef] [PubMed]
- Melnyk, M.; Casey, R.G.; Black, P.; Koupparis, A.J. Enhanced recovery after surgery (ERAS) protocols: Time to change practice? Can. Urol. Assoc. J. 2011, 5, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Ottery, F.D. Definition of standardized nutritional assessment and interventional pathways in oncology. Nutrition 1996, 12, S15–S19. [Google Scholar] [CrossRef] [PubMed]
- Detsky, A.S.; McLaughlin, J.R.; Baker, J.P.; Johnston, N.; Whittaker, S.; Mendelson, R.A.; Jeejeebhoy, K.N. What is subjective global assessment of nutritional status? J. Parenter. Enter. Nutr. 1987, 11, 8–13. [Google Scholar] [CrossRef]
- Body Mass Index. Available online: https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/body-mass-index (accessed on 31 January 2024).
- Martínez-Ortega, A.J.; Piñar-Gutiérrez, A.; Serrano-Aguayo, P.; González-Navarro, I.; Remón-Ruíz, P.J.; Pereira-Cunill, J.L.; García-Luna, P.P. Perioperative nutritional support: A review of current literature. Nutrients 2022, 14, 1601. [Google Scholar] [CrossRef]
- Weimann, A.; Braga, M.; Carli, F.; Higashiguchi, T.; Hübner, M.; Klek, S.; Laviano, A.; Ljungqvist, O.; Lobo, D.N.; Martindale, R.G.; et al. ESPEN practical guideline: Clinical nutrition in surgery. Clin. Nutr. 2021, 40, 4745–4761. [Google Scholar] [CrossRef] [PubMed]
- Leh-Chii, C. History of Asian Federation of Dietetic Associations: Celebrating the 30th anniversary, 1991–2021. Asian J. Diet. 2021, 3, 67–77. [Google Scholar]
- Dietitians: Who Is a Dietitian? Available online: https://www.dietitians.org.my/dietitians/who-is-a-dietitian (accessed on 24 January 2024).
- Guidelines of Allied Health Professions Act for Nutritionists. Available online: https://nutriweb.org.my/pdf/Guidelines-for-Nutritionist-Under-AHP-Act-774.pdf (accessed on 24 January 2024).
- Agreement on Scope of Practice of Nutritionists and Dietitians in Preparation for the Implementation of the Allied Health Professions Act (Act 774). Available online: https://nutriweb.org.my/pdf/Agreement%20on%20scope%20of%20practice%20-%20final%20for%20web.pdf (accessed on 24 January 2024).
- Hewko, S.; Oyesegun, A.; Clow, S.; VanLeeuwen, C. High turnover in clinical dietetics: A qualitative analysis. BMC Health Serv. Res. 2021, 21, 25. [Google Scholar] [CrossRef]
- Hughes, R.; Odgers-Jewell, K.; Vivanti, A.; Ferguson, M.; Leveritt, M. A study of clinical dietetic workforce recruitment and retention in Queensland. Nutr. Diet. 2011, 68, 70–76. [Google Scholar] [CrossRef]
- Hammond, M.I.; Myers, E.F.; Trostler, N. Nutrition care process and model: An academic and practice odyssey. J. Acad. Nutr. Diet. 2014, 114, 1879–1891. [Google Scholar] [CrossRef]
- Joseph, R.; Hart, N.H.; Bradford, N.; Agbejule, O.A.; Koczwara, B.; Chan, A.; Wallen, M.P.; Chan, R.J. Diet and exercise advice and referrals for cancer survivors: An integrative review of medical and nursing perspectives. Support Care Cancer 2022, 30, 8429–8439. [Google Scholar] [CrossRef]
- Yinusa, G.; Scammell, J.; Murphy, J.; Ford, G.; Baron, S. Multidisciplinary provision of food and nutritional care to hospitalized adult in-patients: A scoping review. J. Multidiscip. Healthc. 2021, 14, 459–491. [Google Scholar] [CrossRef]
| Concept #1: Dietitian/Nutritionist | Concept #2: Southeast Asia | Concept #3: Cancer Treatment/Oncology |
|---|---|---|
| nutritionists/OR dietetics/OR dietary services/OR nutrition*.mp. OR (dietitian* or dietician* or dietetic*).mp. | exp Asia, Southeastern/OR Asia, southeastern/OR Borneo/OR Brunei/OR Cambodia/OR Indochina/OR Indonesia/OR Laos/OR Malaysia/OR Mekong Valley/OR Myanmar/OR Philippines/OR Singapore/OR Thailand/OR Timor-leste/OR Vietnam/OR (Southeast* Asia OR South-east* Asia* OR Borneo* OR Brunei OR Cambodia* OR Indochina* OR Indo-chin* OR Indonesia* OR Lao* OR Malaysia* OR Mekong Valley OR Myanmar OR Philippine* OR Singapore* OR Thai* Timor-Leste OR Vietnam*).mp OR (Southeast* Asia OR South-east* Asia* OR Borneo* OR Brunei OR Cambodia* OR Indochin* OR Indo-chin* or Indonesia* or Lao* or Malaysia* or Mekong Valley or Myanmar or Philippin* or Singapor* or Thai* Timor-Leste or Vietnam*).cp. | medical oncology/OR radiation oncology/OR surgical oncology/OR cancer care facilities/OR oncology service, hospital/OR exp neoplasms/OR cancer*.mp. OR oncolog*.mp. OR neoplasm*.mp. OR kanker.mp |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nissa, C.; Hanna, L.; Bauer, J. Current Oncology Nutrition Care Practice in Southeast Asia: A Scoping Review. Nutrients 2024, 16, 1427. https://doi.org/10.3390/nu16101427
Nissa C, Hanna L, Bauer J. Current Oncology Nutrition Care Practice in Southeast Asia: A Scoping Review. Nutrients. 2024; 16(10):1427. https://doi.org/10.3390/nu16101427
Chicago/Turabian StyleNissa, Choirun, Lauren Hanna, and Judy Bauer. 2024. "Current Oncology Nutrition Care Practice in Southeast Asia: A Scoping Review" Nutrients 16, no. 10: 1427. https://doi.org/10.3390/nu16101427
APA StyleNissa, C., Hanna, L., & Bauer, J. (2024). Current Oncology Nutrition Care Practice in Southeast Asia: A Scoping Review. Nutrients, 16(10), 1427. https://doi.org/10.3390/nu16101427






