Comparison of Several Adiposity Indexes in Predicting Hypertension among Chinese Adults: Data from China Nutrition and Health Surveillance (2015–2017)
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Basic Information Collection
2.3. Anthropometric Measurement and Definition of Hypertension
2.4. Laboratory Test
2.5. Adiposity Indexes Calculations
2.6. Covariates
2.7. Statistical Analysis
3. Results
3.1. Basic Characteristics
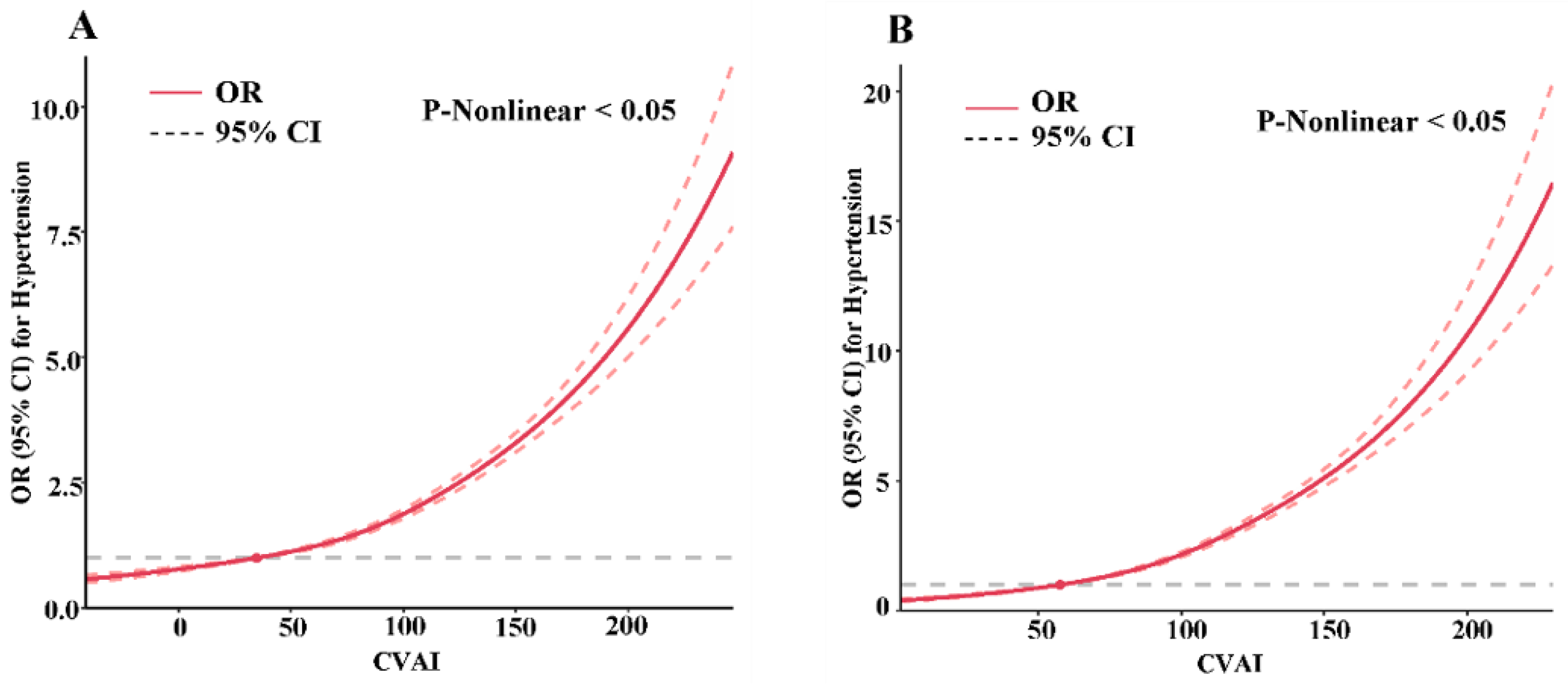
3.2. Association of Adiposity Indexes and Hypertension Risk
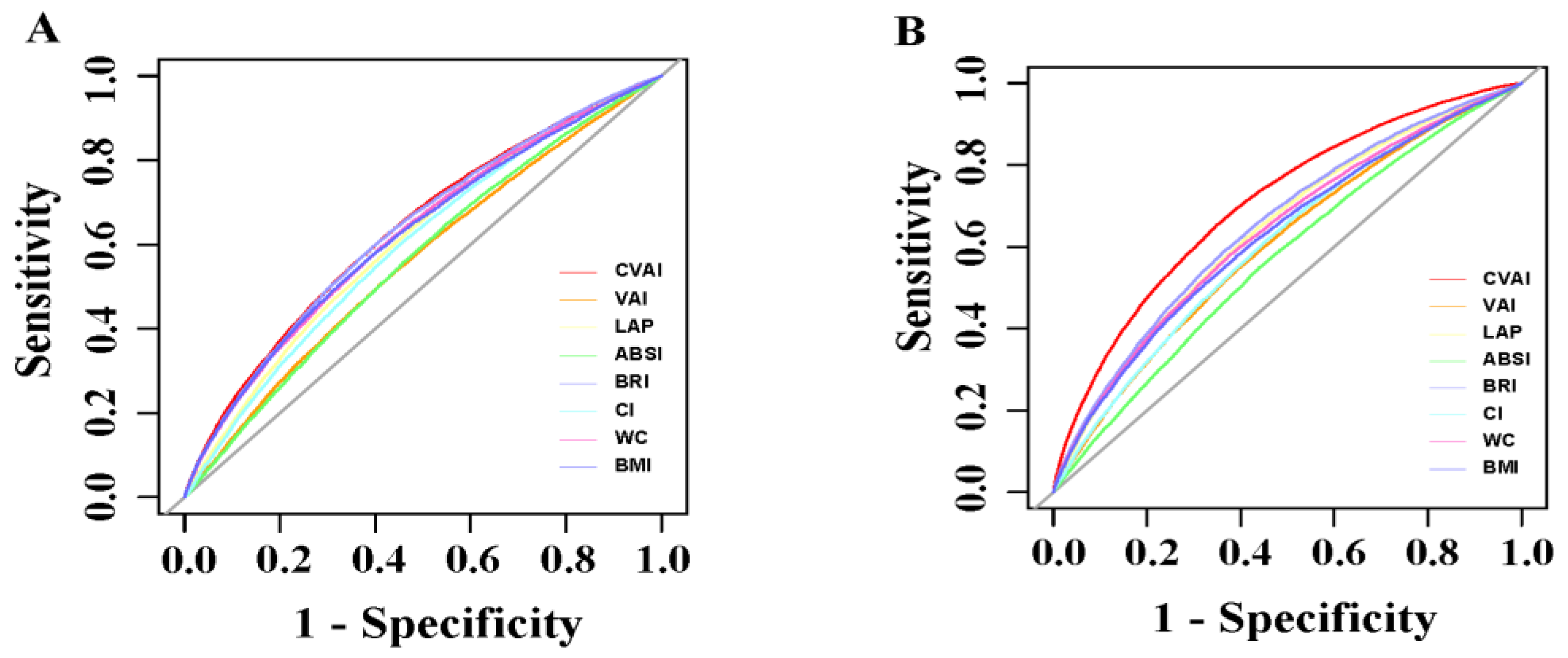
3.3. Comparison of the Association of CVAI, VAI, LAP, ABSI, BRI, CI, WC, and BMI with Hypertension Risk
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhou, B.; Carrillo-Larco, R.M.; Danaei, G.; Riley, L.M.; Paciorek, C.J.; Stevens, G.A.; Gregg, E.W.; Bennett, J.E.; Solomon, B.; Singleton, R.K.; et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Liu, Z.; Joseph, P.; Hu, B.; Yin, L.; Tse, L.A.; Rangarajan, S.; Wang, C.; Wang, Y.; Islam, S.; et al. Modifiable risk factors associated with cardiovascular disease and mortality in China: A PURE substudy. Eur. Heart J. 2022, 43, 2852–2863. [Google Scholar] [CrossRef] [PubMed]
- Stamler, R.; Stamler, J.; Riedlinger, W.F.; Algera, G.; Roberts, R.H. Weight and blood pressure. Findings in hypertension screening of 1 million Americans. JAMA 1978, 240, 1607–1610. [Google Scholar] [CrossRef]
- Hayashi, T.; Boyko, E.J.; Leonetti, D.L.; McNeely, M.J.; Newell-Morris, L.; Kahn, S.E.; Fujimoto, W.Y. Visceral adiposity is an independent predictor of incident hypertension in Japanese Americans. Ann. Intern. Med. 2004, 140, 992–1000. [Google Scholar] [CrossRef] [PubMed]
- Leite, N.N.; Cota, B.C.; Gotine, A.; Rocha, D.; Pereira, P.F.; Hermsdorff, H.H.M. Visceral adiposity index is positively associated with blood pressure: A systematic review. Obes. Res. Clin. Pract. 2021, 15, 546–556. [Google Scholar] [CrossRef]
- Amato, M.C.; Giordano, C.; Galia, M.; Criscimanna, A.; Vitabile, S.; Midiri, M.; Galluzzo, A.; for the AlkaMeSy Study Group. Visceral Adiposity Index: A reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care 2010, 33, 920–922. [Google Scholar] [CrossRef]
- Thomas, D.M.; Bredlau, C.; Bosy-Westphal, A.; Mueller, M.; Shen, W.; Gallagher, D.; Maeda, Y.; McDougall, A.; Peterson, C.M.; Ravussin, E.; et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity 2013, 21, 2264–2271. [Google Scholar] [CrossRef]
- Krakauer, N.Y.; Krakauer, J.C. A new body shape index predicts mortality hazard independently of body mass index. PLoS ONE 2012, 7, e39504. [Google Scholar] [CrossRef]
- Valdez, R. A simple model-based index of abdominal adiposity. J. Clin. Epidemiol. 1991, 44, 955–956. [Google Scholar] [CrossRef]
- Kahn, H.S. The “lipid accumulation product” performs better than the body mass index for recognizing cardiovascular risk: A population-based comparison. BMC Cardiovasc. Disord. 2005, 5, 26. [Google Scholar] [CrossRef]
- Adab, P.; Pallan, M.; Whincup, P.H. Is BMI the best measure of obesity? BMJ 2018, 360, k1274. [Google Scholar] [CrossRef]
- Hu, L.; Hu, G.; Huang, X.; Zhou, W.; You, C.; Li, J.; Li, P.; Wu, Y.; Wu, Q.; Wang, Z.; et al. Different adiposity indices and their associations with hypertension among Chinese population from Jiangxi province. BMC Cardiovasc. Disord. 2020, 20, 115. [Google Scholar] [CrossRef]
- Wang, C.; Fu, W.; Cao, S.; Xu, H.; Tian, Q.; Gan, Y.; Guo, Y.; Yan, S.; Yan, F.; Yue, W.; et al. Association of adiposity indicators with hypertension among Chinese adults. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 1391–1400. [Google Scholar] [CrossRef]
- Xia, M.F.; Chen, Y.; Lin, H.D.; Ma, H.; Li, X.M.; Aleteng, Q.; Li, Q.; Wang, D.; Hu, Y.; Pan, B.S.; et al. A indicator of visceral adipose dysfunction to evaluate metabolic health in adult Chinese. Sci. Rep. 2016, 6, 38214. [Google Scholar] [CrossRef]
- Tang, M.; Wei, X.H.; Cao, H.; Zhen, Q.; Liu, F.; Wang, Y.F.; Fan, N.G.; Peng, Y.D. Association between Chinese visceral adiposity index and metabolic-associated fatty liver disease in Chinese adults with type 2 diabetes mellitus. Front. Endocrinol. 2022, 13, 935980. [Google Scholar] [CrossRef] [PubMed]
- Pan, L.; Xu, Q.; Liu, J.; Gao, Y.; Li, J.; Peng, H.; Chen, L.; Wang, M.; Mai, G.; Yang, S. Dose-response relationship between Chinese visceral adiposity index and type 2 diabetes mellitus among middle-aged and elderly Chinese. Front. Endocrinol. 2022, 13, 959860. [Google Scholar] [CrossRef] [PubMed]
- Wan, H.; Wang, Y.; Xiang, Q.; Fang, S.; Chen, Y.; Chen, C.; Zhang, W.; Zhang, H.; Xia, F.; Wang, N.; et al. Associations between abdominal obesity indices and diabetic complications: Chinese visceral adiposity index and neck circumference. Cardiovasc. Diabetol. 2020, 19, 118. [Google Scholar] [CrossRef]
- Bi, H.; Zhang, Y.; Qin, P.; Wang, C.; Peng, X.; Chen, H.; Zhao, D.; Xu, S.; Wang, L.; Zhao, P.; et al. Association of Chinese Visceral Adiposity Index and Its Dynamic Change with Risk of Carotid Plaque in a Large Cohort in China. J. Am. Heart Assoc. 2022, 11, e022633. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.; Li, N.; Heizhati, M.; Gan, L.; Zhu, Q.; Yao, L.; Li, M.; Yang, W. Chinese Visceral Adiposity Index Is Associated with Incident Renal Damage in Patients With Hypertension and Abnormal Glucose Metabolism: A Longitudinal Study. Front. Endocrinol. 2022, 13, 910329. [Google Scholar] [CrossRef] [PubMed]
- Han, M.; Qie, R.; Li, Q.; Liu, L.; Huang, S.; Wu, X.; Zhang, D.; Cheng, C.; Zhao, Y.; Liu, D.; et al. Chinese visceral adiposity index, a novel indicator of visceral obesity for assessing the risk of incident hypertension in a prospective cohort study. Br. J. Nutr. 2021, 126, 612–620. [Google Scholar] [CrossRef]
- Yu, D.; Zhao, L.; Zhang, J.; Yang, Z.; Yang, L.; Huang, J.; Fang, H.; Guo, Q.; Xu, X.; Ju, L.; et al. China Nutrition and Health Surveys (1982–2017). China CDC Wkly. 2021, 3, 193–195. [Google Scholar] [CrossRef]
- Yang, Y.; Yu, D.; Piao, W.; Huang, K.; Zhao, L. Nutrient-Derived Beneficial for Blood Pressure Dietary Pattern Associated with Hypertension Prevention and Control: Based on China Nutrition and Health Surveillance 2015–2017. Nutrients 2022, 14, 3108. [Google Scholar] [CrossRef] [PubMed]
- Force, C.M.-A.G.O.C.O.T. Predictive values of body mass index and waist circumference to risk factors of related diseases in Chinese adult population. Zhonghua Liu Xing Bing Xue Za Zhi 2002, 23, 5–10. [Google Scholar]
- Fan, M.; Lyu, J.; He, P. Chinese guidelines for data processing and analysis concerning the International Physical Activity Questionnaire. Zhonghua Liu Xing Bing Xue Za Zhi 2014, 35, 961–964. [Google Scholar]
- Nave, O. Modification of Semi-Analytical Method Applied System of ODE. Mod. Appl. Sci. 2020, 14, 75. [Google Scholar] [CrossRef]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef]
- Li, B.; Wang, J.; Zhou, X.; Liu, Y.; Wang, W.; Gao, Z.; Tang, X.; Yan, L.; Wan, Q.; Luo, Z.; et al. Chinese Visceral Adiposity Index Is More Closely Associated with Hypertension and Prehypertension Than Traditional Adiposity Indices in Chinese Population: Results From the REACTION Study. Front. Endocrinol. 2022, 13, 921997. [Google Scholar] [CrossRef]
- Wang, Y.; Zhao, X.; Chen, Y.; Yao, Y.; Zhang, Y.; Wang, N.; Liu, T.; Fu, C. Visceral adiposity measures are strongly associated with cardiovascular disease among female participants in Southwest China: A population-based prospective study. Front. Endocrinol. 2022, 13, 969753. [Google Scholar] [CrossRef]
- Okorodudu, D.O.; Jumean, M.F.; Montori, V.M.; Romero-Corral, A.; Somers, V.K.; Erwin, P.J.; Lopez-Jimenez, F. Diagnostic performance of body mass index to identify obesity as defined by body adiposity: A systematic review and meta-analysis. Int. J. Obes. 2010, 34, 791–799. [Google Scholar] [CrossRef]
- Pou, K.M.; Massaro, J.M.; Hoffmann, U.; Lieb, K.; Vasan, R.S.; O’Donnell, C.J.; Fox, C.S. Patterns of Abdominal Fat Distribution: The Framingham Heart Study. Diabetes Care 2009, 32, 481–485. [Google Scholar] [CrossRef]
- Tee, J.Y.H.; Gan, W.Y.; Lim, P.Y. Comparisons of body mass index, waist circumference, waist-to-height ratio and a body shape index (ABSI) in predicting high blood pressure among Malaysian adolescents: A cross-sectional study. BMJ Open 2020, 10, e032874. [Google Scholar] [CrossRef]
- Fujita, M.; Sato, Y.; Nagashima, K.; Takahashi, S.; Hata, A. Predictive Power of a Body Shape Index for Development of Diabetes, Hypertension, and Dyslipidemia in Japanese Adults: A Retrospective Cohort Study. PLoS ONE 2015, 10, e0128972. [Google Scholar] [CrossRef]
- Andrade, M.D.; Freitas, M.C.; Sakumoto, A.M.; Pappiani, C.; Andrade, S.C.; Vieira, V.L.; Damasceno, N.R. Association of the conicity index with diabetes and hypertension in Brazilian women. Arch. Endocrinol. Metab. 2016, 60, 436–442. [Google Scholar] [CrossRef] [PubMed]
- Nkwana, M.R.; Monyeki, K.D.; Lebelo, S.L. Body Roundness Index, A Body Shape Index, Conicity Index, and Their Association with Nutritional Status and Cardiovascular Risk Factors in South African Rural Young Adults. Int. J. Environ. Res. Public Health 2021, 18, 281. [Google Scholar] [CrossRef]
- Li, Y.; He, Y.; Yang, L.; Liu, Q.; Li, C.; Wang, Y.; Yang, P.; Wang, J.; Chen, Z.; Huang, X. Body Roundness Index and Waist-Hip Ratio Result in Better Cardiovascular Disease Risk Stratification: Results From a Large Chinese Cross-Sectional Study. Front. Nutr. 2022, 9, 801582. [Google Scholar] [CrossRef]
- Calderón-García, J.F.; Roncero-Martín, R.; Rico-Martín, S.; De Nicolás-Jiménez, J.M.; López-Espuela, F.; Santano-Mogena, E.; Alfageme-García, P.; Sánchez Muñoz-Torrero, J.F. Effectiveness of Body Roundness Index (BRI) and a Body Shape Index (ABSI) in Predicting Hypertension: A Systematic Review and Meta-Analysis of Observational Studies. Int. J. Environ. Res. Public Health 2021, 18, 11607. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.R.; Ahn, S.V.; Kim, J.Y.; Koh, S.B.; Choi, E.H.; Lee, G.Y.; Jang, Y.E. Comparison of various anthropometric indices for the identification of a predictor of incident hypertension: The ARIRANG study. J. Hum. Hypertens. 2018, 32, 294–300. [Google Scholar] [CrossRef]
- Deurenberg, P.; Deurenberg-Yap, M.; Guricci, S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes. Rev. 2002, 3, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Nishida, C.; Ko, G.T.; Kumanyika, S. Body fat distribution and noncommunicable diseases in populations: Overview of the 2008 WHO Expert Consultation on Waist Circumference and Waist–Hip Ratio. Eur. J. Clin. Nutr. 2010, 64, 2–5. [Google Scholar] [CrossRef]
- Chen, Z.; Smith, M.; Du, H.; Guo, Y.; Clarke, R.; Bian, Z.; Collins, R.; Chen, J.; Qian, Y.; Wang, X.; et al. Blood pressure in relation to general and central adiposity among 500 000 adult Chinese men and women. Int. J. Epidemiol. 2015, 44, 1305–1319. [Google Scholar] [CrossRef]
- Lee, X.; Gao, Y.; Zhang, Y.; Feng, Y.; Gao, L.; Wang, A.; Jiang, Y.; Huang, H. Comparison of 10 obesity-related indices for predicting hypertension based on ROC analysis in Chinese adults. Front. Public Health 2022, 10, 1042236. [Google Scholar] [CrossRef]
- 2018 Chinese Guidelines for Prevention and Treatment of Hypertension-A report of the Revision Committee of Chinese Guidelines for Prevention and Treatment of Hypertension. J. Geriatr. Cardiol. 2019, 16, 182–241. [CrossRef]
- Ge, Q.; Qi, Z.; Xu, Z.; Li, M.; Zheng, H.; Duan, X.; Chu, M.; Zhuang, X. Comparison of different obesity indices related with hypertension among different sex and age groups in China. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 793–801. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zhang, Z.; Wang, J.; Sun, H.; Zhao, X.; Cheng, X.; Zhao, Q. Sex differences in the association of abdominal adipose tissue and anthropometric data with untreated hypertension in a Chinese population. Biol. Sex Differ. 2020, 11, 38. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.K.; Dong, J.; Sun, Y.; Hu, L.K.; Liu, Y.H.; Chu, X.; Yan, Y.X. Gender-specific predictive ability for the risk of hypertension incidence related to baseline level or trajectories of adiposity indices: A cohort study of functional community. Int. J. Obes. 2022, 46, 1036–1043. [Google Scholar] [CrossRef]
- Deng, W.-W.; Wang, J.; Liu, M.-M.; Wang, D.; Zhao, Y.; Liu, Y.-Q.; Wang, H.; Dong, G.-H. Body Mass Index Compared with Abdominal Obesity Indicators in Relation to Prehypertension and Hypertension in Adults: The CHPSNE Study. Am. J. Hypertens. 2012, 26, 58–67. [Google Scholar] [CrossRef]
- Denton, K.M.; Hilliard, L.M.; Tare, M. Sex-related differences in hypertension: Seek and ye shall find. Hypertension 2013, 62, 674–677. [Google Scholar] [CrossRef]
| Characteristics | Overall | Male | Female | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total (n = 99,201) | Hypertension (n = 51,556) | No Hypertension (n = 47,645) | Total (n = 47,044) | Hypertension (n = 24,428) | No Hypertension (n = 22,616) | Total (n = 52,157) | Hypertension (n = 27,128) | No Hypertension (n = 25,029) | |
| Age (years) | 59.01 (14.27) | 61.62 (14.39) | 55.69 (12.84) | 59.67 (14.59) | 61.89 (14.68) | 56.91 (13.34) | 58.48 (13.89) | 61.39 (14.09) | 54.53 (12.33) |
| Geographic region (n, %) | |||||||||
| Urban | 41,848 (42.19) | 21,816 (42.32) | 20,032 (42.04) | 19,217 (40.85) | 10,282 (42.09) | 8935 (39.51) | 22,631 (43.39) | 11,534 (42.52) | 11,097 (44.34) |
| Rural | 57,353 (57.81) | 29,740 (57.68) | 27,613 (57.96) | 27,827 (59.15) | 14,146 (57.91) | 13,681 (60.49) | 29,526 (56.61) | 15,594 (57.48) | 13,932 (55.66) |
| Education level (n, %) | |||||||||
| Primary school or below | 55,688 (56.14) | 30,398 (58.96) | 25,290 (53.08) | 22,052 (46.88) | 11,711 (47.94) | 10,341 (45.72) | 33,636 (64.49) | 18,687 (68.88) | 14,949 (59.73) |
| Junior middle school | 27,458 (27.68) | 13,474 (26.13) | 13,984 (29.35) | 15,768 (33.52) | 8013 (32.8) | 7755 (34.29) | 11,690 (22.41) | 5461 (20.13) | 6229 (24.89) |
| Senior high school and above | 16,055 (16.18) | 7684 (14.90) | 8371 (17.57) | 9224 (19.61) | 4704 (19.26) | 4520 (19.99) | 6831 (13.1) | 2980 (10.98) | 3851 (15.39) |
| Marital status (n, %) | |||||||||
| Married | 91,793 (92.53) | 46,895 (90.96) | 44,898 (94.23) | 44,541 (94.68) | 22,923 (93.84) | 21,618 (95.59) | 47,252 (90.6) | 23,972 (88.37) | 23,280 (93.01) |
| Other status | 7408 (7.47) | 4661 (9.04) | 2747 (5.77) | 2503 (5.32) | 1505 (6.16) | 998 (4.41) | 4905 (9.4) | 3156 (11.63) | 1749 (6.99) |
| Income (CNY) | |||||||||
| low | 36,316(36.61) | 19,729(38.27) | 16,587(34.81) | 17,585(37.38) | 9322(38.16) | 8263(36.54) | 18,731(35.91) | 10,407 (38.36) | 8324 (33.26) |
| medium | 40,033(40.36) | 20,309(39.39) | 19,724(41.4) | 18,900(40.18) | 9533(39.02) | 9367(41.42) | 21,133(40.52) | 10,776 (39.72) | 10,357 (41.38) |
| high | 22,852(23.04) | 11,518(22.34) | 11,334(23.79) | 10,559(22.44) | 5573(22.81) | 4986(22.05) | 12,293(23.57) | 5945 (21.91) | 6348 (25.36) |
| Family history | |||||||||
| No | 67,948(68.5) | 32,703(63.43) | 35,245(73.97) | 32,860(69.85) | 15,809(64.72) | 17,051(75.39) | 35,088(67.27) | 16,894 (62.28) | 18,194 (72.69) |
| Yes | 31,253(31.5) | 18,853(36.57) | 12,400(26.03) | 14,184(30.15) | 8619(35.28) | 5565(24.61) | 17,069(32.73) | 10,234 (37.72) | 6835 (27.31) |
| WC-based (n, %) | |||||||||
| Normal weight | 52,644 (53.07) | 23,085 (44.78) | 29,559 (62.04) | 32,373 (68.81) | 14,941 (61.16) | 17,432 (77.08) | 20,271 (38.87) | 8144 (30.02) | 12,127 (48.45) |
| Central obesity | 46,557 (46.93) | 28,471 (55.22) | 18,086 (37.96) | 14,671 (31.19) | 9487 (38.84) | 5184 (22.92) | 31,886 (61.13) | 18,984 (69.98) | 12,902 (51.55) |
| BMI-based (n, %) | |||||||||
| Underweight | 3177 (3.2) | 1203 (2.33) | 1974 (4.14) | 1544 (3.28) | 583 (2.39) | 961 (4.25) | 1633 (3.13) | 620 (2.29) | 1013 (4.05) |
| Normal weight | 44,134 (44.49) | 18,949 (36.75) | 25,18 (52.86) | 22,209 (47.21) | 9643 (39.48) | 12,566 (55.56) | 21,925 (42.04) | 9306 (34.3) | 12,619 (50.42) |
| Overweight | 37,074 (37.37) | 20,979 (40.69) | 16,095 (33.78) | 17,331 (36.84) | 9970 (40.81) | 7361 (32.55) | 19,743 (37.85) | 11,009 (40.58) | 8734 (34.9) |
| Obesity | 14,816 (14.94) | 10,425 (20.22) | 4391 (9.22) | 5960 (12.67) | 4232 (17.32) | 1728 (7.64) | 8856 (16.98) | 6193 (22.83) | 2663 (10.64) |
| Current smoker (n, %) | |||||||||
| No | 72,691 (73.28) | 38,666 (75.00) | 34,025 (71.41) | 22,479 (47.78) | 12,544 (51.35) | 9935 (43.93) | 50,212 (96.27) | 26,122 (96.29) | 24,090 (96.25) |
| Yes | 26,510 (26.72) | 12,890 (25.00) | 13,620 (28.59) | 24,565 (52.22) | 11,884 (48.65) | 12,681 (56.07) | 1945 (3.73) | 1006 (3.71) | 939 (3.75) |
| Alcohol drinking (n, %) | |||||||||
| NO | 72,146 (72.73) | 37,485 (72.71) | 34,661 (72.75) | 25,077 (53.31) | 12,763 (52.25) | 12,314 (54.45) | 47,069 (90.24) | 24,722 (91.13) | 22,347 (89.28) |
| YES | 27,055 (27.27) | 14,071 (27.29) | 12,984 (27.25) | 21,967 (46.69) | 11,665 (47.75) | 10,302 (45.55) | 5088 (9.76) | 2406 (8.87) | 2682 (10.72) |
| Sleep duration (n, %) | |||||||||
| <7 h | 25,727 (25.93) | 13,894 (26.95) | 11,833 (24.84) | 11,430 (24.3) | 6091 (24.93) | 5339 (23.61) | 14,297 (27.41) | 7803 (28.76) | 6494 (25.95) |
| 7~9 h | 52,905 (53.33) | 26,311 (51.03) | 26,594 (55.82) | 25,796 (54.83) | 12,940 (52.97) | 12,856 (56.84) | 27,109 (51.98) | 13,371 (49.29) | 13,738 (54.89) |
| >9 h | 20,569 (20.73) | 11,351 (22.02) | 9218 (19.35) | 9818 (20.87) | 5397 (22.09) | 4421 (19.55) | 10,751 (20.61) | 5954 (21.95) | 4797 (19.17) |
| Physical activity (n, %) | |||||||||
| Low | 22,033 (22.21) | 12,049 (23.37) | 9984 (20.95) | 11,852 (25.19) | 6345 (25.97) | 5507 (24.35) | 10,181 (19.52) | 5704 (21.03) | 4477 (17.89) |
| Moderate | 24,859 (25.06) | 13,414 (26.02) | 11,445 (24.02) | 11,436 (24.31) | 6299 (25.79) | 5137 (22.71) | 13,423 (25.74) | 7115 (26.23) | 6308 (25.2) |
| High | 52,309 (52.73) | 26,093 (50.61) | 26,216 (55.02) | 23,756 (50.5) | 11,784 (48.24) | 11,972 (52.94) | 28,553 (54.74) | 14,309 (52.75) | 14,244 (56.91) |
| Sedentary behavior | |||||||||
| 0 ~< 2 h | 13,295 (13.4) | 6716 (13.03) | 65,79 (13.81) | 5753 (12.23) | 2907 (11.9) | 2846 (12.58) | 7542 (14.46) | 3809 (14.04) | 3733 (14.91) |
| 2~3 h | 38,539 (38.85) | 19,519 (37.86) | 19,020 (39.92) | 18,312 (38.93) | 9238 (37.82) | 9074 (40.12) | 20,227 (38.78) | 10,281 (37.9) | 9946 (39.74) |
| ≥4 h | 47,367 (47.75) | 25,321 (49.11) | 22,046 (46.27) | 22,979 (48.85) | 12,283 (50.28) | 10,696 (47.29) | 24,388 (46.76) | 13,038 (48.06) | 11,350 (45.35) |
| Medical examination within one year (n, %) | |||||||||
| NO | 70,492 (71.06) | 34,900 (67.69) | 35,592 (74.70) | 19,217 (40.85) | 16,719 (68.44) | 17,229 (76.18) | 36,544 (70.07) | 18,181 (67.02) | 18,363 (73.37) |
| YES | 28,709 (28.94) | 16,656 (32.31) | 12,053 (25.30) | 27,827(59.15) | 7709 (31.56) | 5387 (23.82) | 15,613 (29.93) | 8947 (32.98) | 6666 (26.63) |
| Diabetes (n, %) | |||||||||
| NO | 87,241 (87.94) | 43,370 (84.12) | 43,871 (92.08) | 41,494 (88.2) | 20,739 (84.9) | 20,755 (91.77) | 45,747 (87.71) | 22,631 (83.42) | 23,116 (92.36) |
| YES | 11,960 (12.06) | 8186 (15.88) | 3774 (7.92) | 5550 (11.8) | 3689 (15.1) | 1861 (8.23) | 6410 (12.29) | 4497 (16.58) | 1913 (7.64) |
| Dyslipidemia (n, %) | |||||||||
| NO | 57,637 (58.10) | 27,322 (52.99) | 30,315 (63.63) | 26,906 (57.19) | 13,018 (53.29) | 13,888 (61.41) | 30,731 (58.92) | 14,304 (52.73) | 16,427 (65.63) |
| YES | 41,564 (41.90) | 24,234 (47.01) | 17,330 (36.37) | 20,138 (42.81) | 11,410 (46.71) | 8728 (38.59) | 21,426 (41.08) | 12,824 (47.27) | 8602 (34.37) |
| Characteristics | Overall | Male | Female | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Hypertension | No Hypertension | p-Value | Total | Hypertension | No Hypertension | p-Value | Total | Hypertension | No Hypertension | p-Value | |
| Height (cm) | 159.00 (12.00) | 158.90 (12.00) | 159.50 (11.60) | <0.0001 | 165.00 (9.00) | 165.00 (9.00) | 165.20 (9.00) | <0.0001 | 154.20 (8.30) | 154.00 (8.10) | 155.00 (8.30) | <0.0001 |
| Weight (kg) | 61.30 (15.10) | 63.00 (15.90) | 59.70 (14.00) | <0.0001 | 65.10 (15.30) | 67.10 (16.00) | 63.30 (14.20) | <0.0001 | 58.10 (13.30) | 59.80 (14.00) | 56.70 (12.30) | <0.0001 |
| SBP (mmHg) | 137.33 (27.67) | 152.00 (21.34) | 125.33 (14.33) | <0.0001 | 137.00 (26.34) | 151.00 (20.00) | 125.67 (14.00) | <0.0001 | 137.33 (29.00) | 153.00 (22.33) | 125.00 (15.00) | <0.0001 |
| DBP (mmHg) | 80.00 (14.67) | 86.33 (14.66) | 75.00 (11.00) | <0.0001 | 81.67 (14.66) | 88.33 (14.33) | 76.67 (10.67) | <0.0001 | 78.67 (14.67) | 84.33 (14.34) | 73.67 (11.66) | <0.0001 |
| FPG (mmol/L) | 5.29 (0.92) | 5.40 (1.02) | 5.18 (0.82) | <0.0001 | 5.30 (0.95) | 5.42 (1.03) | 5.20 (0.85) | <0.0001 | 5.28 (0.90) | 5.39 (1.01) | 5.17 (0.78) | <0.0001 |
| TC (mmol/L) | 4.85 (1.23) | 4.93 (1.26) | 4.78 (1.19) | <0.0001 | 4.72 (1.20) | 4.78 (1.23) | 4.66 (1.17) | <0.0001 | 4.97 (1.24) | 5.06 (1.26) | 4.89 (1.21) | <0.0001 |
| TG (mmol/L) | 1.26 (1.00) | 1.37 (1.09) | 1.15 (0.88) | <0.0001 | 1.21 (1.01) | 1.29 (1.10) | 1.12 (0.91) | <0.0001 | 1.31 (0.98) | 1.44 (1.07) | 1.18 (0.85) | <0.0001 |
| LDL-C (mmol/L) | 3.02 (1.09) | 3.09 (1.12) | 2.94 (1.06) | <0.0001 | 2.92 (1.07) | 2.97 (1.08) | 2.87 (1.04) | <0.0001 | 3.11 (1.10) | 3.20 (1.13) | 3.01 (1.06) | <0.0001 |
| HDL-C (mmol/L) | 1.26 (0.44) | 1.25 (0.44) | 1.28 (0.44) | <0.0001 | 1.22 (0.45) | 1.22 (0.45) | 1.23 (0.45) | <0.0001 | 1.3 (0.43) | 1.27 (0.42) | 1.33 (0.44) | <0.0001 |
| HbA1c (%) | 5.10 (0.90) | 5.10 (0.80) | 5.00 (0.80) | <0.0001 | 5.00 (0.80) | 5.10 (0.90) | 5.00 (0.90) | <0.0001 | 5.10 (0.90) | 5.20 (0.90) | 5.00 (0.80) | <0.0001 |
| Characteristics | Overall | Male | Female | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Hypertension | No Hypertension | p-Value | Total | Hypertension | No Hypertension | p-Value | Total | Hypertension | No Hypertension | p-Value | |
| CVAI | 98.68 (55.56) | 110.64 (52.93) | 85.78 (51.20) | <0.0001 | 93.84 (65.39) | 105.41 (63.21) | 81.51 (61.74) | <0.0001 | 101.80 (48.65) | 113.90 (45.29) | 88.51 (43.76) | <0.0001 |
| VAI | 1.56 (1.73) | 1.74 (1.94) | 1.39 (1.48) | <0.0001 | 1.25 (1.42) | 1.36 (1.57) | 1.13 (1.25) | <0.0001 | 1.86 (1.90) | 2.13 (2.15) | 1.62 (1.60) | <0.0001 |
| LAP | 27.65 (34.39) | 33.44 (39.31) | 22.35 (27.84) | <0.0001 | 23.12 (32.41) | 27.90 (36.60) | 18.68 (26.52) | <0.0001 | 31.55 (35.13) | 38.18 (40.03) | 25.50 (27.91) | <0.0001 |
| ABSI (m11/6/kg2/3) | 0.0788 (0.0065) | 0.0793 (0.0064) | 0.0781 (0.0065) | <0.0001 | 0.0790 (0.0062) | 0.0795 (0.0061) | 0.0784 (0.0062) | <0.0001 | 0.0786 (0.0068) | 0.0792 (0.0068) | 0.0779 (0.0067) | <0.0001 |
| BRI | 3.83 (1.64) | 4.13 (1.67) | 3.51 (1.50) | <0.0001 | 3.60 (1.55) | 3.89 (1.56) | 3.32 (1.43) | <0.0001 | 4.03 (1.70) | 4.36 (1.73) | 3.69 (1.54) | <0.0001 |
| CI (m2/3/kg1/2) | 1.23 (0.12) | 1.25 (0.11) | 1.21 (0.11) | <0.0001 | 1.23 (0.11) | 1.25 (0.11) | 1.22 (0.11) | <0.0001 | 1.23 (0.12) | 1.25 (0.11) | 1.21 (0.11) | <0.0001 |
| WC (cm) | 83.4 (13.55) | 85.70 (13.50) | 81.00 (13.00) | <0.0001 | 84.65 (14.15) | 87.00 (13.92) | 82.20 (13.55) | <0.0001 | 82.4 (13.15) | 84.85 (13.00) | 80.05 (12.25) | <0.0001 |
| BMI (kg/m2) | 24.2 (4.68) | 24.97 (4.80) | 23.43 (4.31) | <0.0001 | 23.95 (4.61) | 24.71 (4.67) | 23.21 (4.26) | <0.0001 | 24.41 (4.76) | 25.21 (4.88) | 23.63 (4.35) | <0.0001 |
| Indicators | Group of Quartile | N | No. of Cases | Hypertension OR (95% CI) | ||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||||
| CVAI | Q1 | 24,800 | 8179 | reference | reference | reference |
| Q2 | 24,800 | 11,338 | 1.71 (1.65, 1.78) | 1.60 (1.54, 1.66) | 1.55 (1.50, 1.61) | |
| Q3 | 24,801 | 14,268 | 2.75 (2.65, 2.86) | 2.43 (2.34, 2.52) | 2.30 (2.21, 2.39) | |
| Q4 | 24,800 | 17,771 | 5.14 (4.95, 5.34) | 4.12 (3.96, 4.29) | 3.70 (3.54, 3.86) | |
| p-trend | - | - | <0.0001 | <0.0001 | <0.0001 | |
| Per 1SD | - | - | 1.87 (1.84, 1.9) | 1.74 (1.72, 1.77) | 1.68 (1.66, 1.71) | |
| VAI | Q1 | 24,800 | 10,630 | reference | reference | reference |
| Q2 | 24,800 | 12,115 | 1.27 (1.23, 1.32) | 1.27 (1.23, 1.32) | 1.24 (1.19, 1.28) | |
| Q3 | 24,801 | 13,561 | 1.61 (1.55, 1.67) | 1.65 (1.59, 1.72) | 1.53 (1.47, 1.59) | |
| Q4 | 24,800 | 15,250 | 2.13 (2.05, 2.21) | 2.31 (2.22, 2.39) | 1.95 (1.87, 2.05) | |
| p-trend | - | - | <0.0001 | <0.0001 | <0.0001 | |
| Per 1SD | - | - | 1.27 (1.25, 1.29) | 1.31 (1.29, 1.33) | 1.18 (1.16, 1.2) | |
| LAP | Q1 | 24,798 | 9354 | reference | reference | reference |
| Q2 | 24,802 | 11,827 | 1.51 (1.45, 1.56) | 1.59 (1.53, 1.65) | 1.56 (1.50, 1.62) | |
| Q3 | 24,801 | 13,971 | 2.13 (2.06, 2.21) | 2.27 (2.19, 2.35) | 2.18 (2.09, 2.27) | |
| Q4 | 24,800 | 16,404 | 3.23 (3.11, 3.35) | 3.67 (3.53, 3.81) | 3.42 (3.27, 3.58) | |
| p-trend | - | - | <0.0001 | <0.0001 | <0.0001 | |
| Per 1SD | - | - | 1.53 (1.51, 1.56) | 1.62 (1.59, 1.64) | 1.54 (1.51, 1.57) | |
| ABSI | Q1 | 24,799 | 10,875 | reference | reference | reference |
| Q2 | 24,801 | 12,358 | 1.27 (1.23, 1.32) | 1.22 (1.18, 1.27) | 1.17 (1.13, 1.21) | |
| Q3 | 24,801 | 13,765 | 1.60 (1.54, 1.66) | 1.47 (1.42, 1.53) | 1.36 (1.31, 1.41) | |
| Q4 | 24,800 | 14,558 | 1.82 (1.76, 1.89) | 1.47 (1.42, 1.53) | 1.35 (1.3, 1.4) | |
| p-trend | - | - | <0.0001 | <0.0001 | <0.0001 | |
| Per 1SD | - | - | 1.25 (1.23, 1.26) | 1.14 (1.13, 1.16) | 1.11 (1.1, 1.13) | |
| BRI | Q1 | 24,800 | 9045 | reference | reference | reference |
| Q2 | 24,805 | 11,496 | 1.51 (1.45, 1.56) | 1.57 (1.52, 1.63) | 1.49 (1.44, 1.55) | |
| Q3 | 24,801 | 14,130 | 2.31 (2.23, 2.39) | 2.38 (2.29, 2.47) | 2.16 (2.08, 2.25) | |
| Q4 | 24,795 | 16,885 | 3.72 (3.58, 3.86) | 3.68 (3.54, 3.83) | 3.18 (3.06, 3.31) | |
| p-trend | - | - | <0.0001 | <0.0001 | <0.0001 | |
| Per 1SD | - | - | 1.68 (1.66, 1.71) | 1.70 (1.68, 1.73) | 1.61 (1.59, 1.63) | |
| CI | Q1 | 24,800 | 9877 | reference | reference | reference |
| Q2 | 24,800 | 12,134 | 1.45 (1.40, 1.5) | 1.45 (1.40, 1.51) | 1.36 (1.31, 1.41) | |
| Q3 | 24,801 | 13,867 | 1.92 (1.85, 1.99) | 1.87 (1.80, 1.94) | 1.68 (1.62, 1.75) | |
| Q4 | 24,800 | 15,678 | 2.60 (2.50, 2.69) | 2.28 (2.2, 2.37) | 1.99 (1.91, 2.06) | |
| p-trend | - | - | <0.0001 | <0.0001 | <0.0001 | |
| Per 1SD | - | - | 1.43 (1.41, 1.45) | 1.36 (1.34, 1.38) | 1.29 (1.27, 1.31) | |
| WC | Q1 | 24,868 | 9518 | reference | reference | reference |
| Q2 | 24,793 | 11,549 | 1.41 (1.36, 1.46) | 1.55 (1.49, 1.61) | 1.48 (1.42, 1.54) | |
| Q3 | 24,785 | 13,819 | 2.03 (1.96, 2.11) | 2.26 (2.18, 2.35) | 2.07 (1.99, 2.15) | |
| Q4 | 24,755 | 16,670 | 3.33 (3.20, 3.45) | 3.73 (3.59, 3.88) | 3.25 (3.12, 3.38) | |
| p-trend | - | - | <0.0001 | <0.0001 | <0.0001 | |
| Per 1SD | - | - | 1.59 (1.57, 1.61) | 1.68 (1.66, 1.7) | 1.60 (1.57, 1.62) | |
| BMI | Q1 | 24,800 | 9815 | reference | reference | reference |
| Q2 | 24,802 | 11,475 | 1.32 (1.27, 1.36) | 1.51 (1.45, 1.57) | 1.45 (1.39, 1.5) | |
| Q3 | 24,799 | 13,636 | 1.87 (1.80, 1.93) | 2.27 (2.19, 2.36) | 2.10 (2.02, 2.18) | |
| Q4 | 24,800 | 16,630 | 3.11 (3.00, 3.22) | 4.02 (3.87, 4.18) | 3.55 (3.41, 3.70) | |
| p-trend | - | - | <0.0001 | <0.0001 | <0.0001 | |
| Per 1SD | - | - | 1.57 (1.55, 1.59) | 1.75 (1.72, 1.77) | 1.51 (1.49, 1.54) | |
| Male | Female | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AUC | 95%CI | Cut-Off Point | Sensitivity | Specificity | Youden | AUC | 95%CI | Cut-Off Point | Sensitivity | Specificity | Youden | |
| CVAI | 0.636 | 0.631–0.641 | 98.268 | 0.562 | 0.638 | 0.199 | 0.706 | 0.702–0.710 | 101.165 | 0.653 | 0.651 | 0.304 |
| VAI | 0.561 * | 0.556–0.566 | 1.358 | 0.503 | 0.592 | 0.095 | 0.602 * | 0.597–0.607 | 1.937 | 0.552 | 0.599 | 0.152 |
| LAP | 0.610 * | 0.605–0.615 | 21.599 | 0.604 | 0.558 | 0.162 | 0.641 * | 0.637–0.646 | 30.272 | 0.621 | 0.588 | 0.209 |
| ABSI | 0.564 * | 0.559–0.569 | 0.078 | 0.644 | 0.455 | 0.099 | 0.570 * | 0.565–0.575 | 0.079 | 0.551 | 0.558 | 0.109 |
| BRI | 0.633 * | 0.628–0.638 | 3.608 | 0.595 | 0.605 | 0.200 | 0.651 * | 0.647–0.656 | 4.099 | 0.586 | 0.638 | 0.224 |
| CI | 0.598 * | 0.593–0.604 | 1.225 | 0.610 | 0.539 | 0.149 | 0.608 * | 0.603–0.61 | 1.223 | 0.608 | 0.552 | 0.160 |
| WC | 0.622 * | 0.617–0.627 | 84.450 | 0.595 | 0.587 | 0.181 | 0.634 * | 0.630–0.639 | 82.875 | 0.582 | 0.621 | 0.203 |
| BMI | 0.620 * | 0.615–0.625 | 24.096 | 0.571 | 0.610 | 0.181 | 0.625 * | 0.620–0.630 | 24.516 | 0.577 | 0.608 | 0.186 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.; Yu, D.; Yang, Y.; Cheng, X.; Piao, W.; Guo, Q.; Xu, X.; Zhao, L.; Wang, Y. Comparison of Several Adiposity Indexes in Predicting Hypertension among Chinese Adults: Data from China Nutrition and Health Surveillance (2015–2017). Nutrients 2023, 15, 2146. https://doi.org/10.3390/nu15092146
Li Y, Yu D, Yang Y, Cheng X, Piao W, Guo Q, Xu X, Zhao L, Wang Y. Comparison of Several Adiposity Indexes in Predicting Hypertension among Chinese Adults: Data from China Nutrition and Health Surveillance (2015–2017). Nutrients. 2023; 15(9):2146. https://doi.org/10.3390/nu15092146
Chicago/Turabian StyleLi, Yuge, Dongmei Yu, Yuxiang Yang, Xue Cheng, Wei Piao, Qiya Guo, Xiaoli Xu, Liyun Zhao, and Yuying Wang. 2023. "Comparison of Several Adiposity Indexes in Predicting Hypertension among Chinese Adults: Data from China Nutrition and Health Surveillance (2015–2017)" Nutrients 15, no. 9: 2146. https://doi.org/10.3390/nu15092146
APA StyleLi, Y., Yu, D., Yang, Y., Cheng, X., Piao, W., Guo, Q., Xu, X., Zhao, L., & Wang, Y. (2023). Comparison of Several Adiposity Indexes in Predicting Hypertension among Chinese Adults: Data from China Nutrition and Health Surveillance (2015–2017). Nutrients, 15(9), 2146. https://doi.org/10.3390/nu15092146





