Voluntary Hydration with Skimmed Lactose-Free Milk during Exercise in the Heat: Exploring Effectiveness and Tolerance
Abstract
1. Introduction
2. Materials and Methods
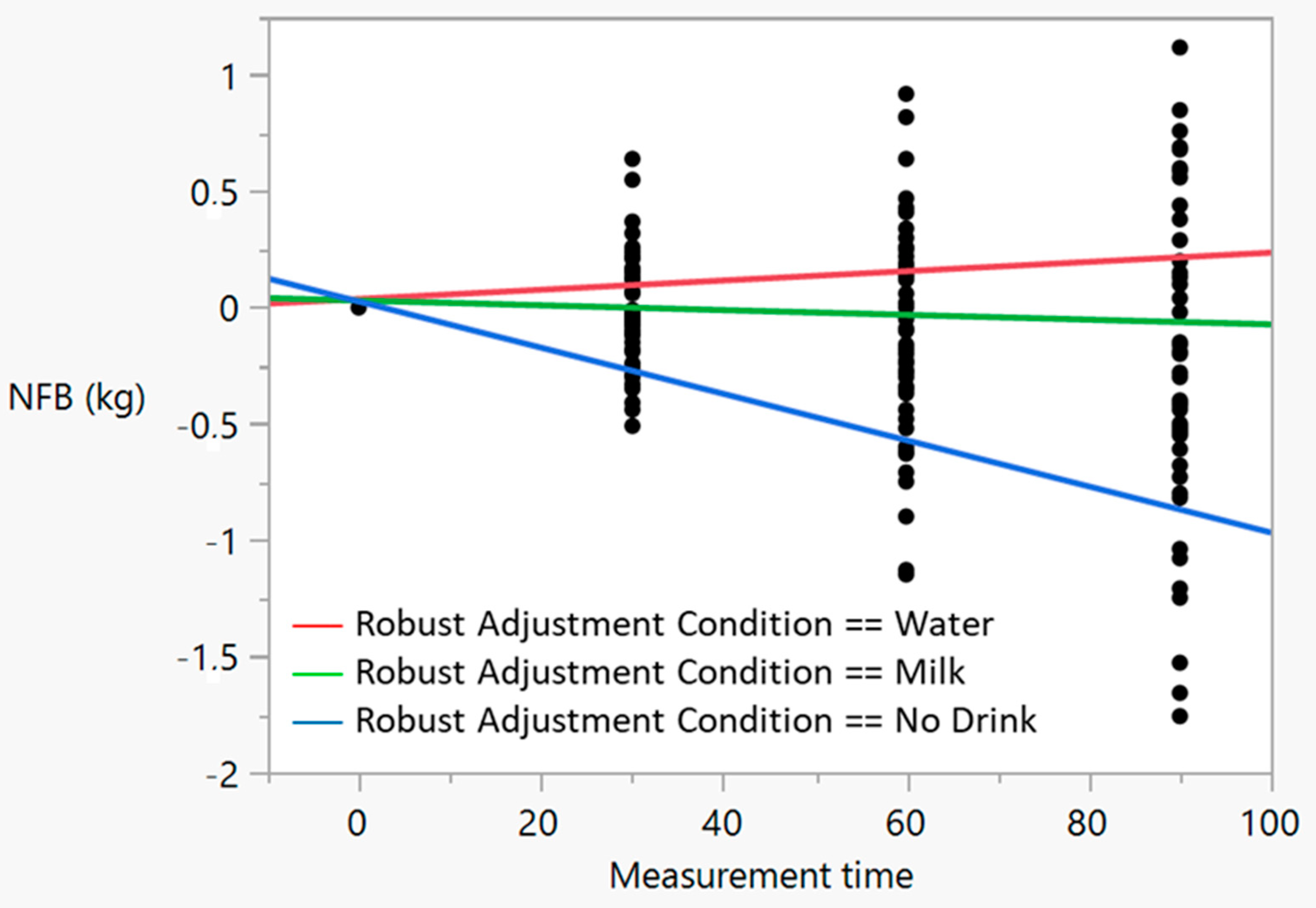
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Benelam, B.; Wyness, L. Hydration and Health: A Review. Nutr. Bull. 2010, 35, 3–25. [Google Scholar] [CrossRef]
- Willis, N.; Westfall, D.; Bottin, J.; Perrier, E.; Hillman, C.; Khan, N. Characterizing Dietary and Physical Activity Patterns in Relation to Hydration Among Pre-Adolescent Children. Curr. Dev. Nutr. 2020, 4 (Suppl. S2), 576. [Google Scholar] [CrossRef]
- Abu-Reidah, I.M. Carbonated Beverages. In Trends in Non-Alcoholic Beverages; Elsevier: Amsterdam, The Netherlands, 2020; pp. 1–36. [Google Scholar] [CrossRef]
- Kalman, D.S.; Feldman, S.; Krieger, D.R.; Bloomer, R.J. Comparison of Coconut Water and a Carbohydrate-Electrolyte Sport Drink on Measures of Hydration and Physical Performance in Exercise-Trained Men. J. Int. Soc. Sport. Nutr. 2012, 9, 1. [Google Scholar] [CrossRef]
- Orrù, S.; Imperlini, E.; Nigro, E.; Alfieri, A.; Cevenini, A.; Polito, R.; Daniele, A.; Buono, P.; Mancini, A. Role of Functional Beverages on Sport Performance and Recovery. Nutrients 2018, 10, 1470. [Google Scholar] [CrossRef]
- Pérez-Idárraga, A.; Aragón-Vargas, L.F. Postexercise Rehydration: Potassium-Rich Drinks versus Water and a Sports Drink. Appl. Physiol. Nutr. Metab. 2014, 39, 1167–1174. [Google Scholar] [CrossRef]
- James, L. Milk Ingestion in Athletes and Physically Active Individuals. Nutr. Bull. 2012, 37, 257–261. [Google Scholar] [CrossRef]
- Pegoretti, C.; Antunes, A.E.C.; Manchado-Gobatto, F.d.B.; Capitani, C.D. Milk: An Alternative Beverage for Hydration? FNS 2015, 6, 547–554. [Google Scholar] [CrossRef]
- Baguley, B.J.; Zilujko, J.; Leveritt, M.D.; Desbrow, B.; Irwin, C. The Effect of Ad Libitum Consumption of a Milk-Based Liquid Meal Supplement vs. a Traditional Sports Drink on Fluid Balance After Exercise. Int. J. Sport Nutr. Exerc. Metab. 2016, 26, 347–355. [Google Scholar] [CrossRef]
- Berry, C.W.; Wolf, S.T.; Murray, B.; Kenney, W.L. Hydration Efficacy of a Milk Permeate-Based Oral Hydration Solution. Nutrients 2020, 12, 1502. [Google Scholar] [CrossRef]
- Baker, L.B.; Jeukendrup, A.E. Optimal Composition of Fluid-replacement Beverages. Compr. Physiol. 2011, 4, 575–620. [Google Scholar] [CrossRef]
- Calbet, J.; MacLean, D. Role of Caloric Content on Gastric Emptying in Humans. J. Physiol. 1997, 498, 553–559. [Google Scholar] [CrossRef]
- Shirreffs, S.M.; Watson, P.; Maughan, R.J. Milk as an Effective Post-Exercise Rehydration Drink. Br. J. Nutr. 2007, 98, 173–180. [Google Scholar] [CrossRef]
- Goyal, R.K.; Guo, Y.; Mashimo, H. Advances in the Physiology of Gastric Emptying. Neurogastroenterol. Motil. 2019, 31, e13546. [Google Scholar] [CrossRef]
- Rosado, J.L. Intolerancia a La Lactosa. Gac. Med. Mex. 2016, 152, 67–73. [Google Scholar]
- Di Costanzo, M.; Canani, R.B. Lactose Intolerance: Common Misunderstandings. Ann. Nutr. Metab. 2018, 73, 30–37. [Google Scholar] [CrossRef]
- Vázquez, S.M.; de Rojas, J.N.; Troche, J.R.; Adame, E.C.; Ruíz, R.R.; Domínguez, L.U. The Importance of Lactose Intolerance in Individuals with Gastrointestinal Symptoms. Rev. Gastroenterol. México 2020, 85, 321–331. [Google Scholar] [CrossRef]
- Shirreffs, S.M.; Aragon-Vargas, L.F.; Keil, M.; Love, T.D.; Phillips, S. Rehydration after Exercise in the Heat: A Comparison of 4 Commonly Used Drinks. Int. J. Sport Nutr. Exerc. Metab. 2007, 17, 244–258. [Google Scholar] [CrossRef]
- Sudsa-ard, K.; Kijboonchoo, K.; Chavasit, V.; Chaunchaiyakul, R.; Nio, A.Q.X.; Lee, J.K.W. Lactose-Free Milk Prolonged Endurance Capacity in Lactose Intolerant Asian Males. J. Int. Soc. Sport. Nutr. 2014, 11, 49. [Google Scholar] [CrossRef]
- Mallari, M.F.T.; Nana, A.; Pinthong, M.; Kongkum, S.; Chaunchaiyakul, R. Post-Exercise Ingestion of Lactose-Free Skim Milk Affects Thirst but Not Subsequent Performance and Net Fluid Balance of Collegiate Badminton Athletes. Malays. J. Nutr. 2019, 25, 337–349. [Google Scholar] [CrossRef]
- Adams, R. Revised Physical Activity Readiness Questionnaire. Can. Fam. Physician 1999, 45, 992. [Google Scholar]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.-M.; Nieman, D.C.; Swain, D.P. American College of Sports Medicine Position Stand. Quantity and Quality of Exercise for Developing and Maintaining Cardiorespiratory, Musculoskeletal, and Neuromotor Fitness in Apparently Healthy Adults: Guidance for Prescribing Exercise. Med. Sci. Sport. Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef]
- Pfeiffer, B.; Cotterill, A.; Grathwohl, D.; Stellingwerff, T.; Jeukendrup, A.E. The Effect of Carbohydrate Gels on Gastrointestinal Tolerance during a 16-Km Run. Int. J. Sport Nutr. Exerc. Metab. 2009, 19, 485–503. [Google Scholar] [CrossRef]
- Tanaka, H.; Monahan, K.D.; Seals, D.R. Age-Predicted Maximal Heart Rate Revisited. J. Am. Coll. Cardiol. 2001, 37, 153–156. [Google Scholar] [CrossRef]
- Borg, G.A. Psychophysical Bases of Perceived Exertion. Med. Sci. Sport. Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef]
- Rolls, B.J. Palatability and Fluid Intake. In Fluid Replacement and Heat Stress; National Academies Press: Washington, DC, USA, 1994; pp. 161–168. [Google Scholar]
- Convertino, V.A.; Armstrong, L.E.; Coyle, E.F.; Mack, G.W.; Sawka, M.N.; Senay, L.C., Jr.; Sherman, W.M. American College of Sports Medicine Position Stand. Exercise and Fluid Replacement. Med. Sci. Sport. Exerc. 1996, 28, i–ix. [Google Scholar] [CrossRef]
- Dill, D.; Yousef, M.; Nelson, J.D. Responses of Men and Women to Two-Hour Walks in Desert Heat. J. Appl. Physiol. 1973, 35, 231–235. [Google Scholar] [CrossRef]
- Lee, J.K.W.; Maughan, R.J.; Shirreffs, S.M.; Watson, P. Effects of Milk Ingestion on Prolonged Exercise Capacity in Young, Healthy Men. Nutrition 2008, 24, 340–347. [Google Scholar] [CrossRef]
- Aragón-Vargas, L.F. Need of Other Elements. In Fluid Balance, Hydration, and Athletic Performance; Taylor and Francis Group: London, UK, 2016; p. 397. [Google Scholar]
- Passe, D.; Horn, M.; Stofan, J.; Horswill, C.; Murray, R. Voluntary Dehydration in Runners despite Favorable Conditions for Fluid Intake. Int. J. Sport Nutr. Exerc. Metab. 2007, 17, 284–295. [Google Scholar] [CrossRef]
- Solera Herrera, A.; Aragón-Vargas, L.F. Deshidratación y sobrehidratación voluntarias durante el ejercicio en el calor: Posibles factores relacionados. Pensar Mov. Rev. Cienc. Del Ejerc. y Salud 2006, 4, 22–33. [Google Scholar] [CrossRef]
- Sieber, R.; Stransky, M.; De Vrese, M. Lactose Intolerance and Consumption of Milk and Milk Products. Z. Ernahr. 1997, 36, 375–393. [Google Scholar] [CrossRef]
- Grumezescu, A.; Holban, A.M. Sports and Energy Drinks; Volume 10: The Science of Beverages; Woodhead Publishing: Sawston, UK, 2019. [Google Scholar]
- Dini, E.; Abreu, D.; López, E. Osmolalidad de Bebidas de Consumo Frecuente. Investig. Clínica 2004, 45, 323–335. [Google Scholar]
- Rehrer, N.; Janssen, G.; Brouns, F.; Saris, W. Fluid Intake and Gastrointestinal Problems in Runners Competing in a 25-Km Race and a Marathon. Int. J. Sport. Med. 1989, 10, S22–S25. [Google Scholar] [CrossRef]
- Morton, D.P.; Aragón-Vargas, L.F.; Callister, R. Effect of Ingested Fluid Composition on Exercise-Related Transient Abdominal Pain. Int. J. Sport Nutr. Exerc. Metab. 2004, 14, 197–208. [Google Scholar] [CrossRef]
- Pfeiffer, B.; Stellingwerff, T.; Hodgson, A.B.; Randell, R.; Pöttgen, K.; Res, P.; Jeukendrup, A.E. Nutritional Intake and Gastrointestinal Problems during Competitive Endurance Events. Med. Sci. Sport. Exerc. 2012, 44, 344–351. [Google Scholar] [CrossRef]
- Peters, H.P.; van Schelven, F.W.; Verstappen, P.A.; de Boer, R.W.; Bol, E.; Erich, W.B.; van der Togt, C.R.; de Vries, W.R. Gastrointestinal Problems as a Function of Carbohydrate Supplements and Mode of Exercise. Med. Sci. Sport. Exerc. 1993, 25, 1211–1224. [Google Scholar] [CrossRef]
- Ligtenberg, A.J.; Liem, E.H.; Brand, H.S.; Veerman, E.C. The Effect of Exercise on Salivary Viscosity. Diagnostics 2016, 6, 40. [Google Scholar] [CrossRef]
- Pinnock, C.; Arney, W. The Milk-Mucus Belief: Sensory Analysis Comparing Cow’s Milk and a Soy Placebo. Appetite 1993, 20, 61–70. [Google Scholar] [CrossRef]
- Peters, H.; Bos, M.; Seebregts, L.; Akkermans, L.; van Berge Henegouwen, G.; Bol, E.; Mosterd, W.; De Vries, W. Gastrointestinal Symptoms in Long-Distance Runners, Cyclists, and Triathletes: Prevalence, Medication, and Etiology. Am. J. Gastroenterol. 1999, 94, 1570–1581. [Google Scholar] [CrossRef]
- Stuempfle, K.J.; Hoffman, M.D. Gastrointestinal Distress Is Common during a 161-Km Ultramarathon. J. Sport. Sci. 2015, 33, 1814–1821. [Google Scholar] [CrossRef]
- Gurton, W.H.; Faulkner, S.H.; James, R.M. Effect of Warm-up and Sodium Bicarbonate Ingestion on 4-Km Cycling Time-Trial Performance. Int. J. Sport. Physiol. Perform. 2021, 16, 1573–1579. [Google Scholar] [CrossRef]
- Bredenoord, A.J.; Smout, A.J. Physiologic and Pathologic Belching. Clin. Gastroenterol. Hepatol. 2007, 5, 772–775. [Google Scholar] [CrossRef] [PubMed]
- Pearce, J.; Hunter, J.O. Nutrition and the Gastrointestinal Tract for Athletes. In Sport and Exercise Nutrition; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2011; pp. 264–280. [Google Scholar] [CrossRef]
- Capitán-Jiménez, C.; Aragón-Vargas, L.F. Awareness of Fluid Losses Does Not Impact Thirst during Exercise in the Heat: A Double-Blind, Cross-Over Study. Nutrients 2021, 13, 4357. [Google Scholar] [CrossRef] [PubMed]
| Variable | Meaningful Mean Difference | Statistical Power |
|---|---|---|
| Final urine specific gravity | 0.003 | 0.9345 |
| Voluntary fluid intake | 220 mL | 0.9036 |
| Urine volume | 60 mL | 0.9302 |
| Percent dehydration | 0.5% BM | 0.9964 |
| Sweat rate | 75 mL/h | 0.8606 |
| GI symptoms | 0.2 a.u. | >0.85 * |
| Variable | Water (Mean) | Milk (Mean) | No Drink (Mean) |
|---|---|---|---|
| Room temperature (°C) | 32.0 | 32.1 | 31.7 |
| Room relative humidity (%) | 69.3 | 69.0 | 70.1 |
| Average heart rate (bpm) | 134.9 | 136.3 | 135.9 |
| Average rating of perceived exertion | 11.8 | 11.8 | 11.7 |
| Baseline body mass (kg) | 67.41 | 67.36 | 67.43 |
| Initial Urine Specific Gravity | 1.018 | 1.018 | 1.019 |
| Final Urine Specific Gravity | 1.016 a | 1.022 | 1.021 |
| Voluntary fluid intake (mL) | 1206.2 b | 918.8 | 0 d |
| Urine output (mL) | 220.4 a | 81.3 | 86.1 |
| Dehydration (% BM) | 0.28 | −0.07 | 1.38 c |
| Sweat rate (mL/h) | 538.5 | 599.6 | 567.2 |
| Effects Tests | Sum of Squares | F-Value | Probability > F |
|---|---|---|---|
| Condition | 0.004 | 0.029 | 0.971 |
| Measuring time | 1.907 | 25.725 | <0.0001 |
| Condition × measurement time | 6.294 | 42.437 | <0.0001 |
| Subject of measurement | 3.507 | 2.956 | 0.0002 |
| Symptom | 0 min | 30 min | 60 min | 90 min | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| W | SM | ND | W | SM | ND | W | SM | ND | W | SM | ND | p-Value (Cond.) | |
| Reflux | 0 | 0 | 0.25 | 0 | 0.44 | 0.25 | 0 | 0.44 | 0.25 | 0 | 0.44 | 0.25 | 0.0685 |
| Heartburn | 0 | 0.38 | 0 | 0 | 0.13 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.1873 |
| Ab. distension | 0 | 0 | 0.25 | 0 | 0.20 | 0.56 | 0.06 | 0.13 | 0.19 | 0.06 | 0.06 | 0 | 0.0492 a |
| Cramping | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.19 | 0 | 0 | 0 | 0 | 0.3701 |
| Vomiting | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ------ |
| Nausea | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ------ |
| Intestinal cramps | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.25 | 0 | 0.3701 |
| Urge to defecate | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.19 | 0 | 0 | 0 | 0 | 0.3701 |
| Flatulence | 0 | 0.19 | 0 | 0.31 | 0.31 | 0.06 | 0.25 | 0.56 | 0.06 | 0.25 | 0.25 | 0 | 0.0635 |
| Abdominal pain | 0 | 0 | 0 | 0 | 0.63 | 0.13 | 0 | 0.63 | 0 | 0 | 0.50 | 0 | 0.0008 b |
| Loose stools/diarrhea | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ------ |
| Dizziness | 0 | 0 | 0 | 0 | 0 | 0.13 | 0.13 | 0 | 0.06 | 0.19 | 0.13 | 0.13 | 0.1439 |
| Headache | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | ------ |
| Muscle cramping | 0 | 0 | 0 | 0.19 | 0.25 | 0.44 | 0.06 | 0.13 | 0.38 | 0 | 0.06 | 0.38 | 0.0972 |
| Urge to urinate | 0 | 0 | 0 | 0.88 | 0.13 | 0.88 | 1.38 | 0.75 | 1.19 | 1.19 | 0.38 | 0.63 | 0.2464 |
| Thick Saliva | 0 | 0 | 0 | 0 | 0.31 | 0 | 0 | 0.69 | 0.31 | 0 | 0.94 | 0.38 | 0.0007 b |
| Belching | 0 | 0 | 0 | 0.19 | 1.19 | 0 | 0.31 | 1.00 | 0.19 | 0.25 | 1.00 | 0.31 | 0.0001 b |
| Fullness | 0.31 | 0.31 | 0.31 | 0.31 | 0.69 | 0.31 | 0.63 | 1.19 | 0.63 | 0.56 | 0.94 | 0.50 | 0.0861 |
| Thirst | 0 | 0 | 0 | 0 | 0 | 0.38 | 0 | 0 | 0.44 | 0 | 0 | 0.44 | 0.0283 a |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aragón-Vargas, L.F.; Garzón-Mosquera, J.C.; Montoya-Arroyo, J.A. Voluntary Hydration with Skimmed Lactose-Free Milk during Exercise in the Heat: Exploring Effectiveness and Tolerance. Nutrients 2023, 15, 2069. https://doi.org/10.3390/nu15092069
Aragón-Vargas LF, Garzón-Mosquera JC, Montoya-Arroyo JA. Voluntary Hydration with Skimmed Lactose-Free Milk during Exercise in the Heat: Exploring Effectiveness and Tolerance. Nutrients. 2023; 15(9):2069. https://doi.org/10.3390/nu15092069
Chicago/Turabian StyleAragón-Vargas, Luis F., Julián Camilo Garzón-Mosquera, and Johnny A. Montoya-Arroyo. 2023. "Voluntary Hydration with Skimmed Lactose-Free Milk during Exercise in the Heat: Exploring Effectiveness and Tolerance" Nutrients 15, no. 9: 2069. https://doi.org/10.3390/nu15092069
APA StyleAragón-Vargas, L. F., Garzón-Mosquera, J. C., & Montoya-Arroyo, J. A. (2023). Voluntary Hydration with Skimmed Lactose-Free Milk during Exercise in the Heat: Exploring Effectiveness and Tolerance. Nutrients, 15(9), 2069. https://doi.org/10.3390/nu15092069







