Adherence to Mediterranean Diet: A Population-Based Longitudinal Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Biochemistry and Clinical Parameters
2.3. The MEDAS Score
2.4. Statistical Analysis
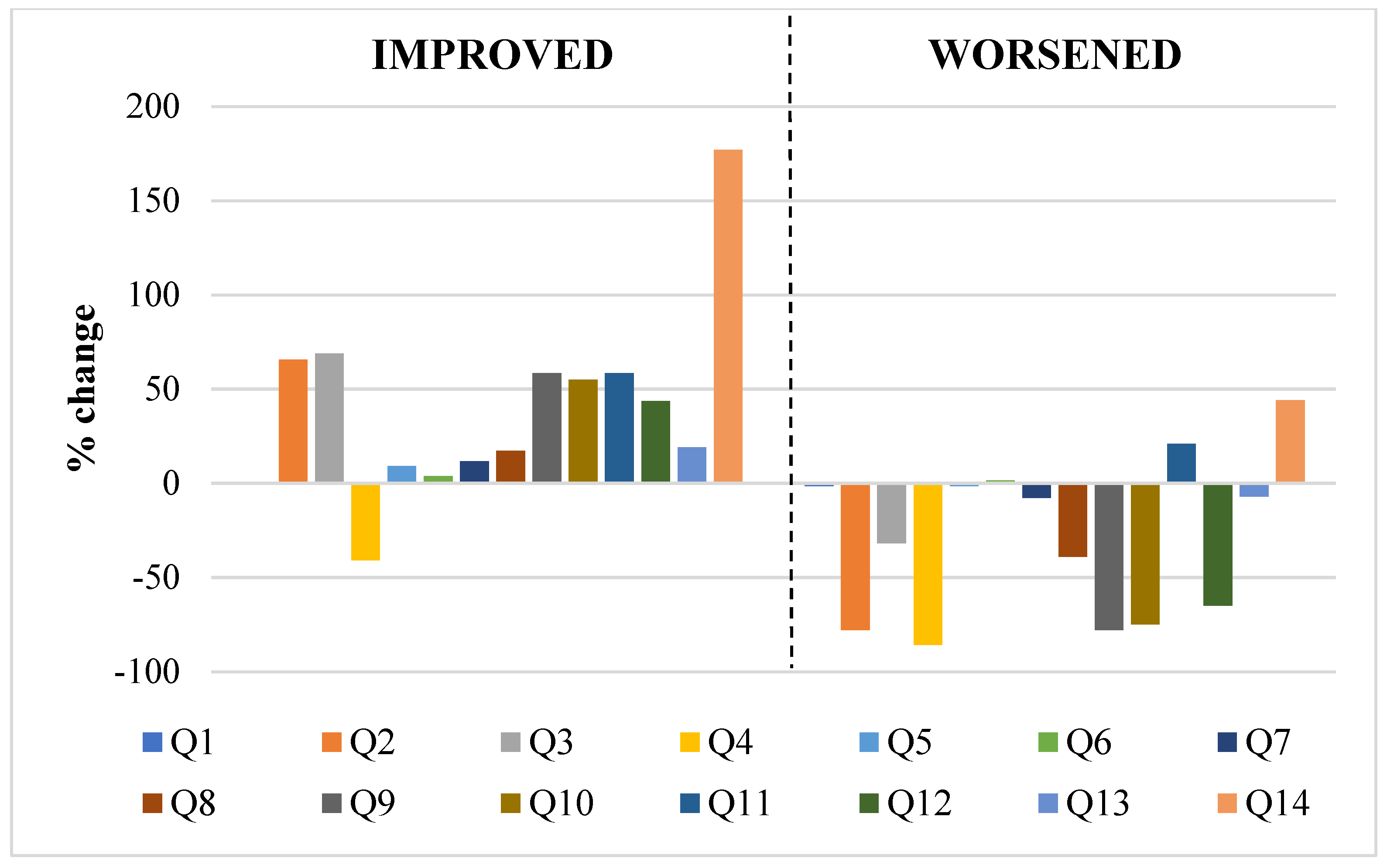
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Martínez-González, M.A.; Villegas, A.S. The emerging role of Mediterranean diets in cardiovascular epidemiology: Monounsaturated fats, olive oil, red wine or the whole pattern? Eur. J. Epidemiol. 2003, 19, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Guasch-Ferré, M.; Willett, W.C. The Mediterranean diet and health: A comprehensive overview. J. Intern. Med. 2021, 290, 549–566. [Google Scholar] [CrossRef] [PubMed]
- Bucciantini, M.; Leri, M.; Nardiello, P.; Casamenti, F.; Stefani, M. Olive Polyphenols: Antioxidant and Anti-Inflammatory Properties. Antioxidants 2021, 10, 1044. [Google Scholar] [CrossRef] [PubMed]
- Dominguez, L.; Di Bella, G.; Veronese, N.; Barbagallo, M. Impact of Mediterranean Diet on Chronic Non-Communicable Diseases and Longevity. Nutrients 2021, 13, 2028. [Google Scholar] [CrossRef]
- Trevisan, M.; Krogh, V.; Grioni, S.; Farinaro, E. Mediterranean diet and all-cause mortality: A cohort of Italian men. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1673–1678. [Google Scholar] [CrossRef]
- Hidalgo-Liberona, N.; Meroño, T.; Zamora-Ros, R.; Rabassa, M.; Semba, R.; Tanaka, T.; Bandinelli, S.; Ferrucci, L.; Andres-Lacueva, C.; Cherubini, A. Adherence to the Mediterranean diet assessed by a novel dietary biomarker score and mortality in older adults: The InCHIANTI cohort study. BMC Med. 2021, 19, 280. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Retraction and Republication: Primary Prevention of Cardiovascular Disease with a Mediterranean Diet. N. Engl. J. Med. 2018, 378, 2441–2442. [Google Scholar] [CrossRef]
- Eleftheriou, D.; Benetou, V.; Trichopoulou, A.; La Vecchia, C.; Bamia, C. Mediterranean diet and its components in relation to all-cause mortality: Meta-analysis. Br. J. Nutr. 2018, 120, 1081–1097. [Google Scholar] [CrossRef]
- Tang, C.; Wang, X.; Qin, L.-Q.; Dong, J.-Y. Mediterranean Diet and Mortality in People with Cardiovascular Disease: A Meta-Analysis of Prospective Cohort Studies. Nutrients 2021, 13, 2623. [Google Scholar] [CrossRef]
- Mattavelli, E.; Olmastroni, E.; Bonofiglio, D.; Catapano, A.L.; Baragetti, A.; Magni, P. Adherence to the Mediterranean Diet: Impact of Geographical Location of the Observations. Nutrients 2022, 14, 2040. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. J. Prev. Cardiol. 2022, 29, 5–115. [Google Scholar] [CrossRef] [PubMed]
- Quintana-Navarro, G.M.; Alcala-Diaz, J.F.; Lopez-Moreno, J.; Perez-Corral, I.; Leon-Acuña, A.; Torres-Peña, J.D.; Rangel-Zuñiga, O.A.; De Larriva, A.P.A.; Corina, A.; Camargo, A.; et al. Long-term dietary adherence and changes in dietary intake in coronary patients after intervention with a Mediterranean diet or a low-fat diet: The CORDIOPREV randomized trial. Eur. J. Nutr. 2020, 59, 2099–2110. [Google Scholar] [CrossRef] [PubMed]
- Lacirignola, C.; Capone, R.; El Bilali, H.; Debs, P.; Cardone, G.L.; Driouech, N.; Dernini, S.B.B.; Gitz, V.M.A. Priority 5, Mediterranean food consumption patterns: Diet, environment, society, economy and health. Feed. Knowl. 2017, 139–184. [Google Scholar]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Adjibade, M.; Assmann, K.E.; Andreeva, V.A.; Lemogne, C.; Hercberg, S.; Galan, P.; Kesse-Guyot, E. Prospective association between adherence to the Mediterranean diet and risk of depressive symptoms in the French SU.VI.MAX cohort. Eur. J. Nutr. 2018, 57, 1225–1235. [Google Scholar] [CrossRef] [PubMed]
- Maraki, M.I.; Yannakoulia, M.; Stamelou, M.; Stefanis, L.; Xiromerisiou, G.; Kosmidis, M.H.; Dardiotis, E.; Hadjigeorgiou, G.M.; Sakka, P.; Anastasiou, C.A.; et al. Mediterranean diet adherence is related to reduced probability of prodromal Parkinson’s disease. Mov. Disord. 2019, 34, 48–57. [Google Scholar] [CrossRef]
- Pelucchi, C.; Galeone, C.; Negri, E.; La Vecchia, C. Trends in adherence to the Mediterranean diet in an Italian population between 1991 and 2006. Eur. J. Clin. Nutr. 2010, 64, 1052–1056. [Google Scholar] [CrossRef]
- Leone, A.; Battezzati, A.; Bertoli, S.; De Amicis, R.; De Carlo, G. Trends of Adherence to the Mediterranean Dietary Pattern in Northern Italy from 2010 to 2016. Nutrients 2017, 9, 734. [Google Scholar] [CrossRef]
- Quarta, S.; Massaro, M.; Chervenkov, M.; Ivanova, T.; Dimitrova, D.; Jorge, R.; Andrade, V.; Philippou, E.; Zisimou, C.; Maksimova, V.; et al. Persistent Moderate-to-Weak Mediterranean Diet Adherence and Low Scoring for Plant-Based Foods across Several Southern European Countries: Are We Overlooking the Mediterranean Diet Recommendations? Nutrients 2021, 13, 1432. [Google Scholar] [CrossRef]
- Gerić, M.; Matković, K.; Gajski, G.; Rumbak, I.; Štancl, P.; Karlić, R.; Bituh, M. Adherence to Mediterranean Diet in Croatia: Lessons Learned Today for a Brighter Tomorrow. Nutrients 2022, 14, 3725. [Google Scholar] [CrossRef]
- Grosso, G.; Marventano, S.; Giorgianni, G.; Raciti, T.; Galvano, F.; Mistretta, A. Mediterranean diet adherence rates in Sicily, southern Italy. Public Health Nutr. 2014, 17, 2001–2009. [Google Scholar] [CrossRef] [PubMed]
- Aljabri, M.K.; Al-Raddadi, R.; Bahijri, S.M.; Al Ahmadi, J.; Ajabnoor, G.; Jambi, H.A. Factors associated with adherence to Mediterranean diet among Saudi non-diabetic patients attending primary health care centers: A cross-sectional study. J. Taibah Univ. Med. Sci. 2019, 14, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Obeid, C.A.; Gubbels, J.S.; Jaalouk, D.; Kremers, S.P.J.; Oenema, A. Adherence to the Mediterranean diet among adults in Mediterranean countries: A systematic literature review. Eur. J. Nutr. 2022, 61, 3327–3344. [Google Scholar] [CrossRef] [PubMed]
- Olmastroni, E.; Baragetti, A.; Casula, M.; Grigore, L.; Pellegatta, F.; Pirillo, A.; Tragni, E.; Catapano, A.L. Multilevel Models to Estimate Carotid Intima-Media Thickness Curves for Individual Cardiovascular Risk Evaluation. Stroke 2019, 50, 1758–1765. [Google Scholar] [CrossRef]
- Olmastroni, E.; Shlyakhto, E.V.; Konradi, A.O.; Rotar, O.P.; Alieva, A.S.; Boyarinova, M.A.; Baragetti, A.; Grigore, L.; Pellegatta, F.; Tragni, E.; et al. Epidemiology of cardiovascular risk factors in two population-based studies. Atheroscler. Suppl. 2018, 35, e14–e20. [Google Scholar] [CrossRef] [PubMed]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497. [Google Scholar] [CrossRef]
- Schröder, H.; Fitó, M.; Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Lamuela-Raventós, R.; Ros, E.; Salaverría, I.; Fiol, M.; et al. A Short Screener Is Valid for Assessing Mediterranean Diet Adherence among Older Spanish Men and Women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Fernández-Jarne, E.; Serrano-Martínez, M.; Marti, A.; Martinez, J.A.; Martín-Moreno, J.M. Mediterranean diet and reduction in the risk of a first acute myocardial infarction: An operational healthy dietary score. Eur. J. Nutr. 2002, 41, 153–160. [Google Scholar] [CrossRef]
- Martinez-Gonzalez, M.A.; Fernández-Jarne, E.; Serrano-Martínez, M.; Wright, M.; Gomez-Gracia, E. Development of a short dietary intake questionnaire for the quantitative estimation of adherence to a cardioprotective Mediterranean diet. Eur. J. Clin. Nutr. 2004, 58, 1550–1552. [Google Scholar] [CrossRef]
- Sánchez-Taínta, A.; Estruch, R.; Bulló, M.; Corella, D.; Gómez-Gracia, E.; Fiol, M.; Algorta, J.; Covas, M.-I.; Lapetra, J.; Zazpe, I.; et al. Adherence to a Mediterranean-type diet and reduced prevalence of clustered cardiovascular risk factors in a cohort of 3204 high-risk patients. Eur. J. Cardiovasc. Prev. Rehabil. 2008, 15, 589–593. [Google Scholar] [CrossRef]
- León-Muñoz, L.M.; Guallar-Castillón, P.; Graciani, A.; López-García, E.; Mesas, A.E.; Aguilera, M.T.; Banegas, J.R.; Rodríguez-Artalejo, F. Adherence to the Mediterranean Diet Pattern Has Declined in Spanish Adults. J. Nutr. 2012, 142, 1843–1850. [Google Scholar] [CrossRef] [PubMed]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [PubMed]
- Mente, A.; De Koning, L.; Shannon, H.S.; Anand, S.S. A Systematic Review of the Evidence Supporting a Causal Link Between Dietary Factors and Coronary Heart Disease. Arch. Intern. Med. 2009, 169, 659. [Google Scholar] [CrossRef]
- Veronese, N.; Notarnicola, M.; Cisternino, A.M.; Inguaggiato, R.; Guerra, V.; Reddavide, R.; Donghia, R.; Rotolo, O.; Zinzi, I.; Leandro, G.; et al. Trends in adherence to the Mediterranean diet in South Italy: A cross sectional study. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Bonaccio, M.; Di Castelnuovo, A.; Bonanni, A.; Costanzo, S.; De Lucia, F.; Persichillo, M.; Zito, F.; Donati, M.B.; de Gaetano, G.; Iacoviello, L. Decline of the Mediterranean diet at a time of economic crisis. Results from the Moli-sani study. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 853–860. [Google Scholar] [CrossRef]
- Sikorski, C.; Yang, S.; Stennett, R.; Miller, V.; Teo, K.; Anand, S.S.; Paré, G.; Yusuf, S.; Dehghan, M.; Mente, A. Changes in energy, macronutrient, and food consumption in 47 countries over the last 70 years (1950–2019): A systematic review and meta-analysis. Nutrition 2022, 108, 111941. [Google Scholar] [CrossRef]
- Bonaccio, M.; Bes-Rastrollo, M.; de Gaetano, G.; Iacoviello, L. Challenges to the Mediterranean diet at a time of economic crisis. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 1057–1063. [Google Scholar] [CrossRef]
- O’Connell, M.; Smith, K.; Stroud, R. The dietary impact of the COVID-19 pandemic. J. Health Econ. 2022, 84, 102641. [Google Scholar] [CrossRef]
- Celorio-Sardà, R.; Comas-Basté, O.; Latorre-Moratalla, M.L.; Zerón-Rugerio, M.F.; Urpi-Sarda, M.; Illán-Villanueva, M.; Farran-Codina, A.; Izquierdo-Pulido, M.; Vidal-Carou, M.D.C. Effect of COVID-19 Lockdown on Dietary Habits and Lifestyle of Food Science Students and Professionals from Spain. Nutrients 2021, 13, 1494. [Google Scholar] [CrossRef]
| Questions | Criteria for 1 Point |
|---|---|
| 1. Do you use olive oil as main culinary fat? | Yes |
| 2. How much olive oil do you consume in a given day (including oil used for frying, salads, out-of-house meals, etc.)? | ≥4 tablespoons |
| 3. How many vegetable servings do you consume per day? (1 serving: 200 g [consider side dishes as half a serving]) | ≥2 (≥1 portion raw or as a salad) |
| 4. How many fruit units (including natural fruit juices) do you consume per day? | ≥3 |
| 5. How many servings of red meat, hamburger, or meat products (ham, sausage, etc.) do you consume per day? (1 serving: 100–150 g) | <1 |
| 6. How many servings of butter, margarine, or cream do you consume per day? (1 serving: 12 g) | <1 |
| 7. How many sweet or carbonated beverages do you drink per day? | <1 |
| 8. How much wine do you drink per week? | ≥7 glasses |
| 9. How many servings of legumes do you consume per week? (1 serving: 150 g) | ≥3 |
| 10. How many servings of fish or shellfish do you consume per week? (1 serving 100–150 g of fish or 4–5 units or 200 g of shellfish) | ≥3 |
| 11. How many times per week do you consume commercial sweets or pastries (not homemade), such as cakes, cookies, biscuits, or custard? | <3 |
| 12. How many servings of nuts (including peanuts) do you consume per week? (1 serving 30 g) | ≥3 |
| 13. Do you preferentially consume chicken, turkey, or rabbit meat instead of veal, pork, hamburger, or sausage? | Yes |
| 14. How many times per week do you consume vegetables, pasta, rice, or other dishes seasoned with sofrito (sauce made with tomato and onion, leek, or garlic and simmered with olive oil)? | ≥2 |
| Baseline Visit | Follow-Up Visit | p-Value | |
|---|---|---|---|
| MEDAS score; mean (SD) | 8.72 (1.82) | 8.38 (1.45) | <0.0001 |
| Optimal adherence to Mediterranean diet; % | 74.82 | 72.86 | <0.0001 |
| MEDAS score by sex; mean (SD) | |||
| Females (N = 414) | 8.72 (1.75) | 8.25 (1.42) | <0.0001 |
| Males (N = 297) | 8.73 (1.91) | 8.56 (1.47) | 0.17 |
| MEDAS score by yrs age groups; mean (SD) | |||
| ≤50 (N = 47) | 8.09 (2.09) | 7.91 (1.41) | 0.55 |
| 50–65 (N = 177) | 8.49 (1.85) | 8.06 (1.56) | 0.31 |
| 65–80 (N = 451) | 8.89 (1.78) | 8.51 (1.40) | <0.0001 |
| >80 (N = 36) | 8.58 (1.42) | 8.36 (1.46) | 0.30 |
| Classes of adherence to Mediterranean diet; % | |||
| Improved (N = 243) | 34.18 | ||
| Unchanged (N = 122) | 17.16 | ||
| Worsened (N = 346) | 48.66 |
| Covariates | Improved Score N = 243 (34%) | Worsened Score N = 346 (48%) | p-Value |
|---|---|---|---|
| Age, years; mean (±SD) | 67.6 (9.74) | 68.53 (9.71) | 0.25 |
| Women, % | 53.91 | 60.4 | 0.12 |
| Educational level, % | |||
| Primary schools | 18.93 | 18.50 | 0.93 |
| Secondary schools | 34.16 | 34.97 | |
| High schools | 38.68 | 38.44 | |
| University degree | 7.41 | 7.80 | |
| Weight, kg; mean (SD) | 73.55 (14.83) | 71.15 (13.68) | 0.04 |
| BMI, kg/m2; mean (SD) | 27.97 (4.85) | 27.17 (4.25) | 0.04 |
| WH ratio; mean (SD) | 0.91 (0.08) | 0.9 (0.09) | 0.13 |
| SBP, mm Hg; mean (SD) | 109.64 (32.24) | 116.81 (50.42) | 0.04 |
| DBP, mm Hg; mean (SD) | 66.88 (19.21) | 69.64 (18.06) | 0.08 |
| Total Chol, mg/dL; mean (SD) | 197.61 (34.18) | 194.72 (35.97) | 0.33 |
| HDL-C, mg/dL; mean (SD) | 56.93 (13.81) | 57.73 (13.76) | 0.49 |
| LDL-C, mg/dL; mean (SD) | 118.36 (29.39) | 114.54 (30.4) | 0.13 |
| TG, mg/dL; median (IQR) | 98 (76–131) | 94 (76–136) | 0.89 |
| Fasting glucose, mg/dL; mean (SD) | 107.39 (60.76) | 103.9 (19.25) | 0.40 |
| Dietary Therapy, % | 8.64 | 8.38 | 0.91 |
| Smoker, % | 10.46 | 12.14 | 0.48 |
| Physical activity, % | 29.58 | 30.72 | 0.17 |
| Antihypertensive treatment, % | 16.46 | 21.68 | 0.12 |
| Antidiabetic treatment, % | 3.7 | 1.45 | 0.08 |
| Lipid-lowering treatment, % | 34.16 | 35.55 | 0.73 |
| MetS, % | 67.6 (9.74) | 68.53 (9.71) | 0.25 |
| cIMT, mm; mean (SD) | 0.79 (0.16) | 0.80 (0.16) | 0.75 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mattavelli, E.; Olmastroni, E.; Casula, M.; Grigore, L.; Pellegatta, F.; Baragetti, A.; Magni, P.; Catapano, A.L. Adherence to Mediterranean Diet: A Population-Based Longitudinal Cohort Study. Nutrients 2023, 15, 1844. https://doi.org/10.3390/nu15081844
Mattavelli E, Olmastroni E, Casula M, Grigore L, Pellegatta F, Baragetti A, Magni P, Catapano AL. Adherence to Mediterranean Diet: A Population-Based Longitudinal Cohort Study. Nutrients. 2023; 15(8):1844. https://doi.org/10.3390/nu15081844
Chicago/Turabian StyleMattavelli, Elisa, Elena Olmastroni, Manuela Casula, Liliana Grigore, Fabio Pellegatta, Andrea Baragetti, Paolo Magni, and Alberico L. Catapano. 2023. "Adherence to Mediterranean Diet: A Population-Based Longitudinal Cohort Study" Nutrients 15, no. 8: 1844. https://doi.org/10.3390/nu15081844
APA StyleMattavelli, E., Olmastroni, E., Casula, M., Grigore, L., Pellegatta, F., Baragetti, A., Magni, P., & Catapano, A. L. (2023). Adherence to Mediterranean Diet: A Population-Based Longitudinal Cohort Study. Nutrients, 15(8), 1844. https://doi.org/10.3390/nu15081844









