Community Women’s Lifestyle and Eating Disorders in the Era of COVID-19 Pandemic: A 15-Year Follow-Up Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Assessment Instruments
2.3. Statistical Analysis
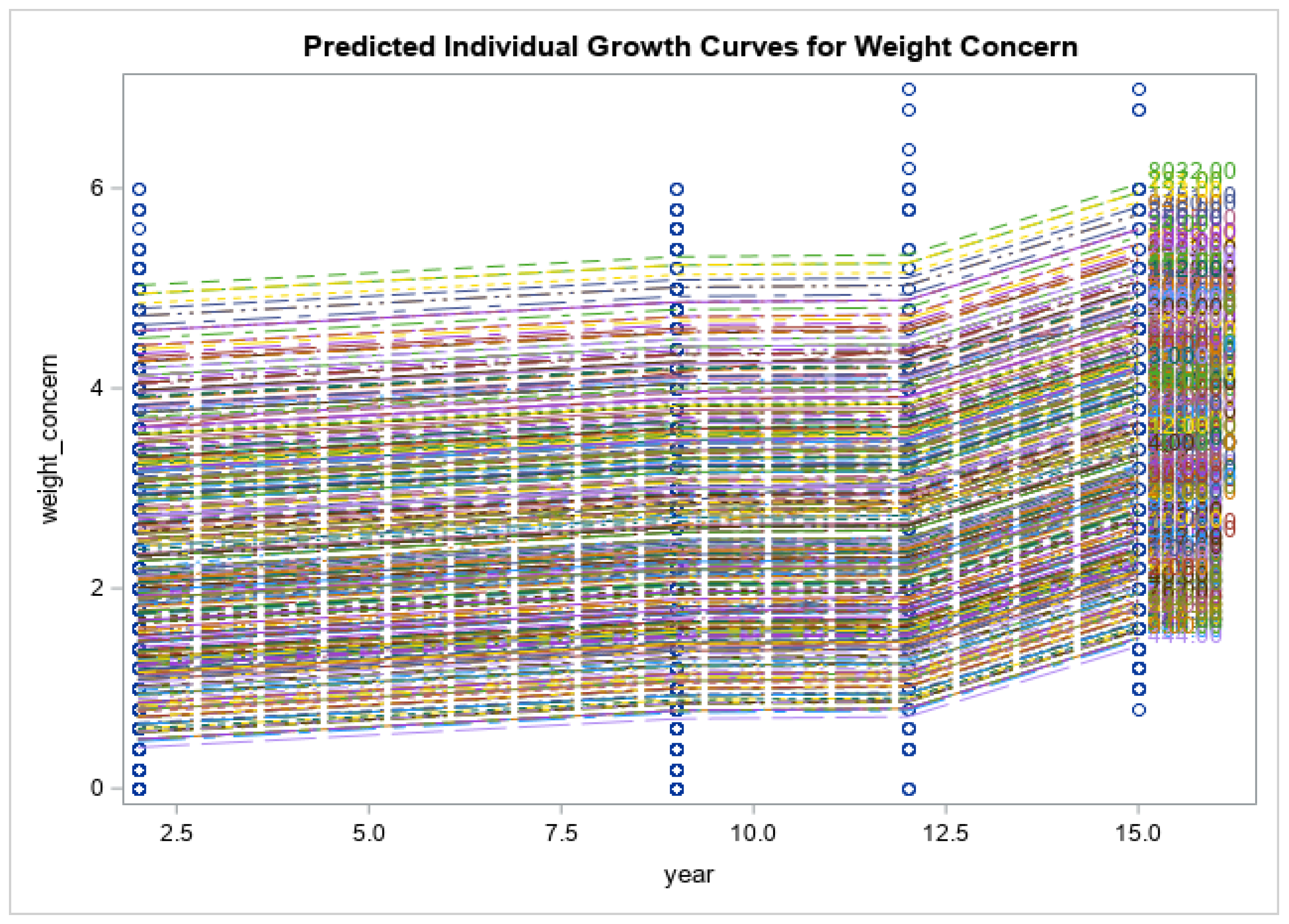
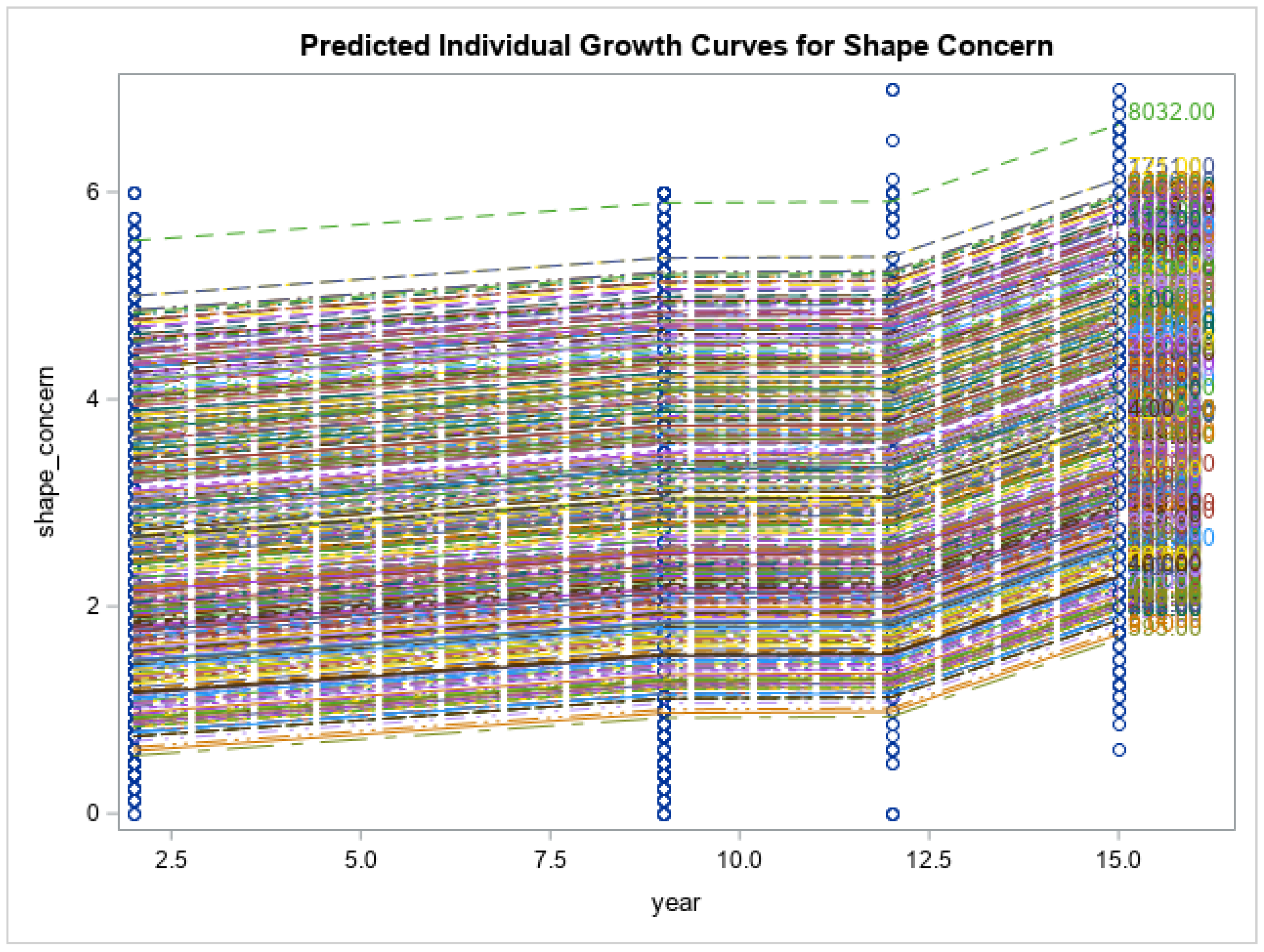
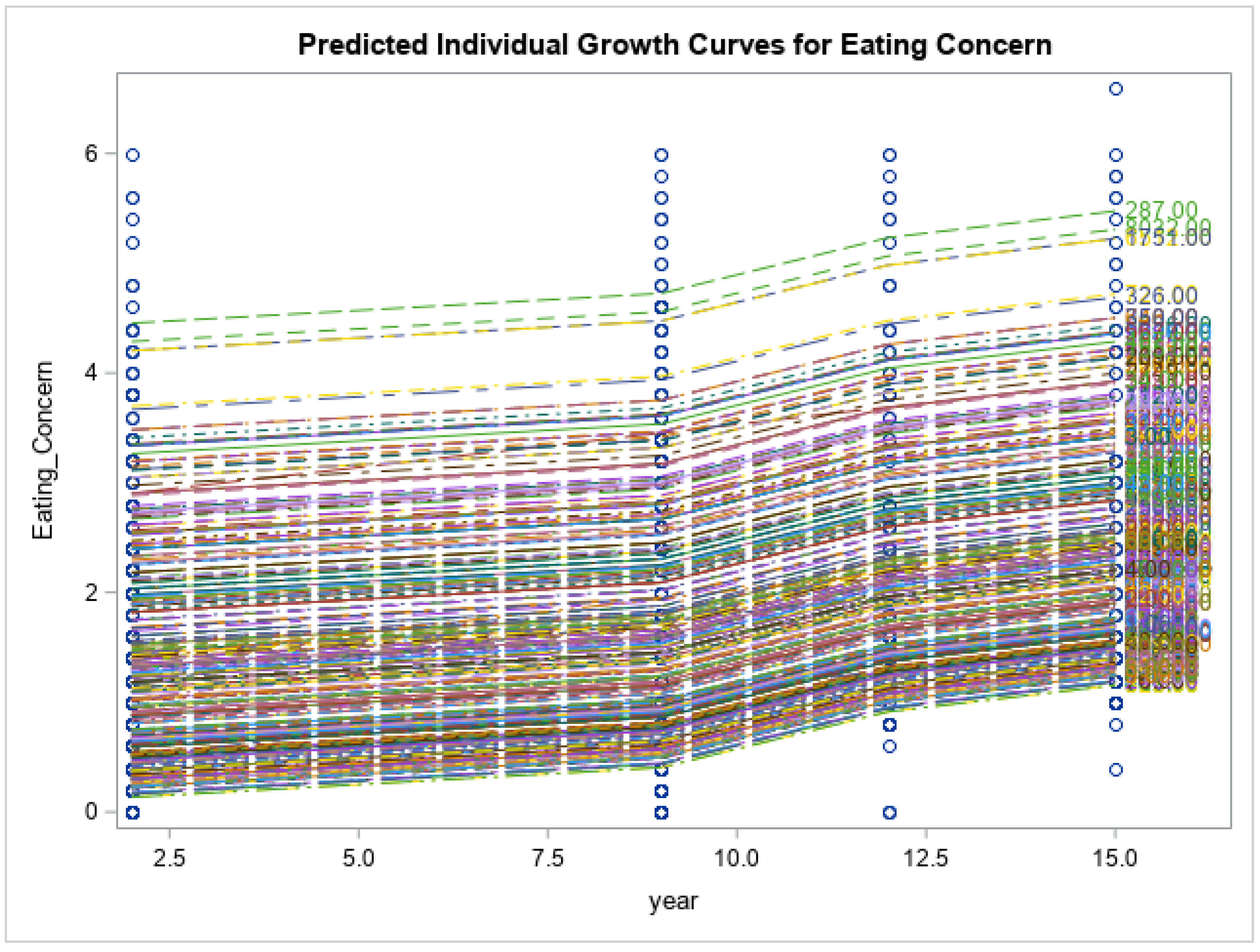
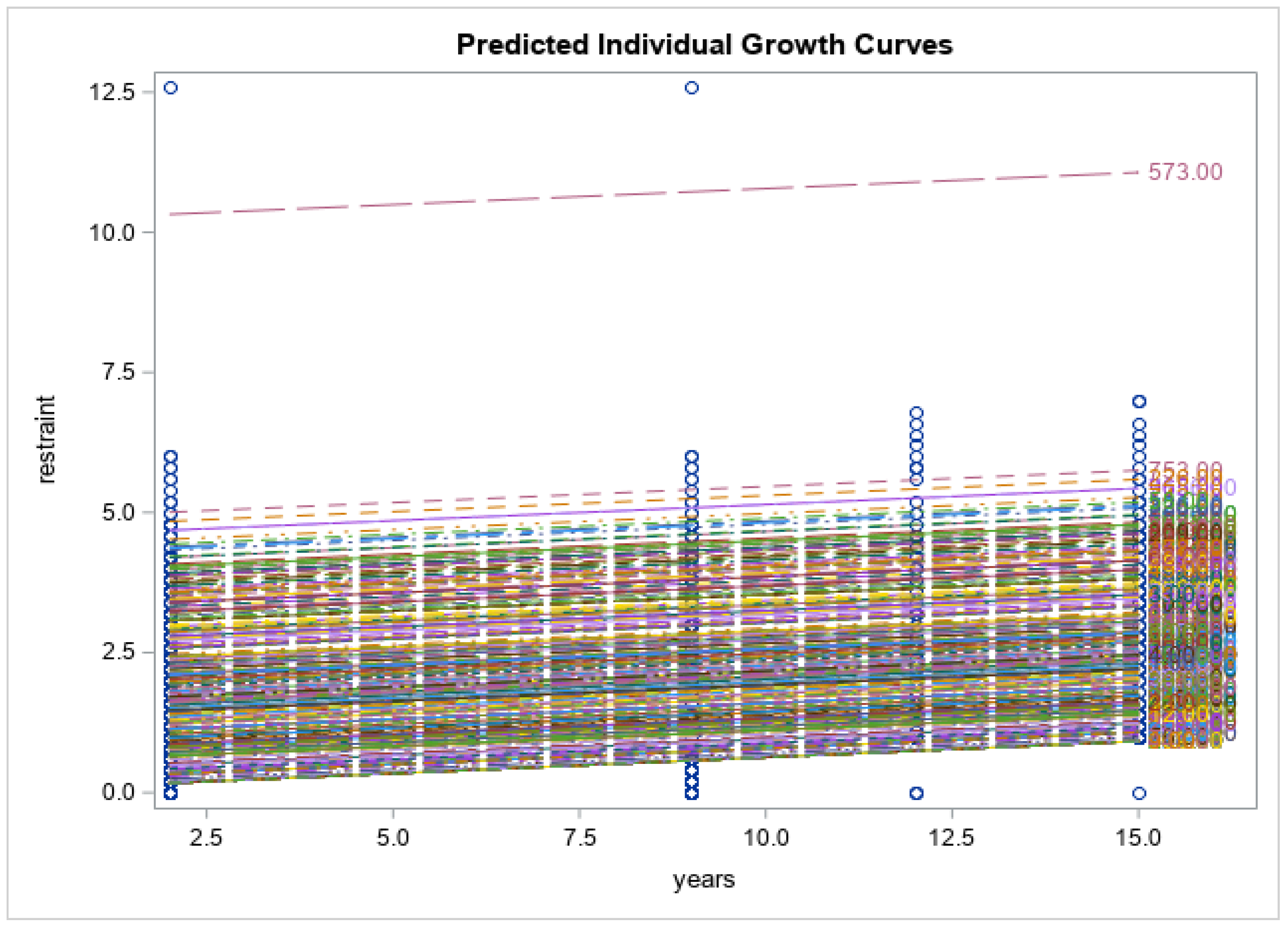
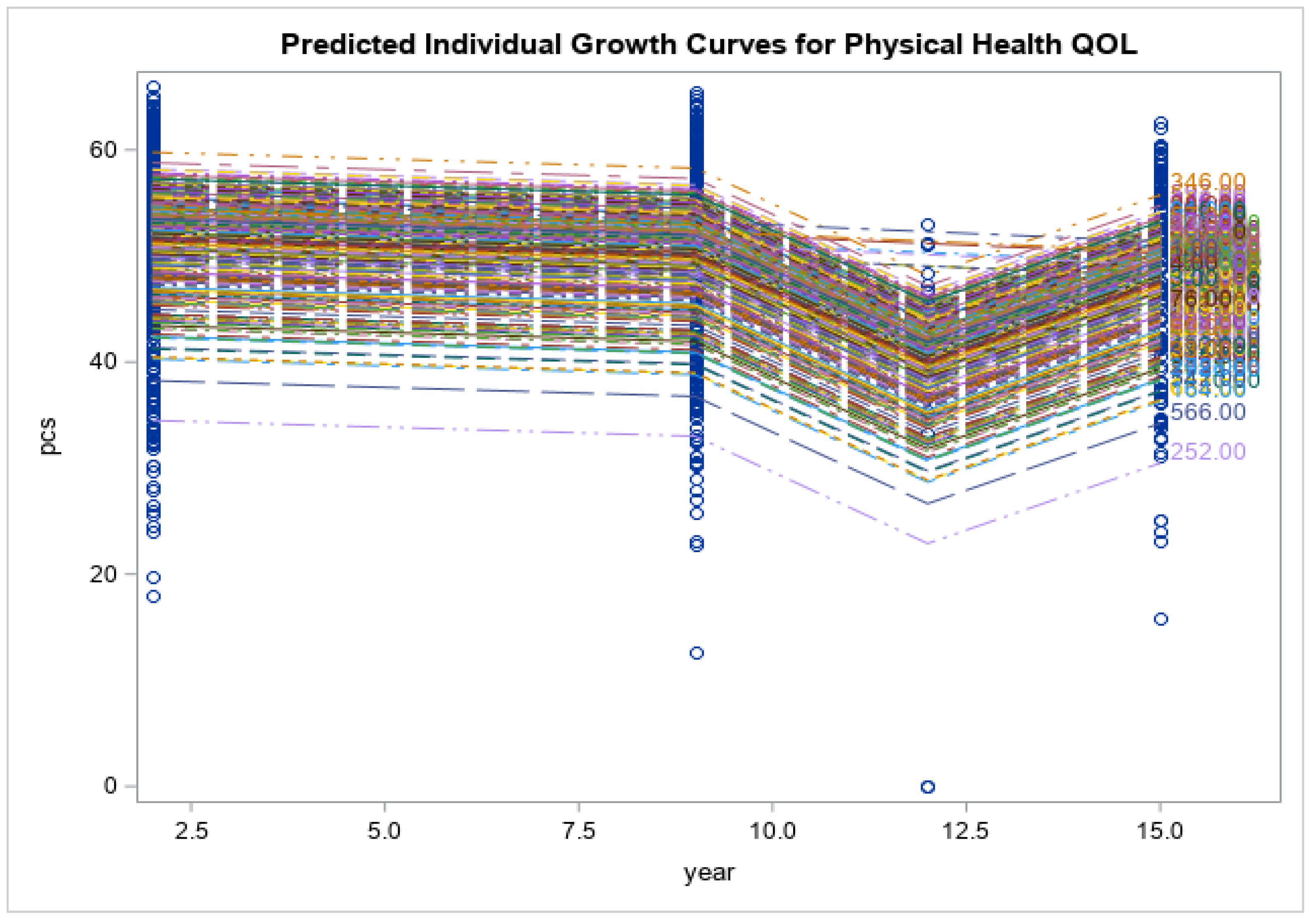
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dragovic, M.; Pascu, V.; Hall, T.; Ingram, J.; Waters, F. Emergency department mental health presentations before and during the COVID-19 outbreak in Western Australia. Australas. Psychiatry 2020, 28, 627–631. [Google Scholar] [CrossRef]
- Fisher, J.R.; Tran, T.D.; Hammarberg, K.; Sastry, J.; Nguyen, H.; Rowe, H.; Popplestone, S.; Stocker, R.; Stubber, C.; Kirkman, M. Mental health of people in Australia in the first month of COVID -19 restrictions: A national survey. Med. J. Aust. 2020, 213, 458–464. [Google Scholar] [CrossRef]
- Asmundson, G.; Taylor, S. Coronaphobia: Fear and the 2019-nCoV outbreak. J. Anxiety Disord. 2020, 70, 102–196. [Google Scholar] [CrossRef] [PubMed]
- Lima, C.; Carvalho, P.; Lima, I.; Nunes, J.; Saraiva, J.; de Souza, R.; da Silva, C.; Neto, M. The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease). Psychiatry Res. 2020, 287, 112–915. [Google Scholar] [CrossRef]
- Maunder, R. Was SARS a mental health catastrophe? Gen. Hosp. Psychiatry 2009, 31, 316–317. [Google Scholar] [CrossRef] [PubMed]
- Phillipou, A.; Meyer, D.; Neill, E.; Tan, E.; Toh, W.; Van Rheenen, T.; Rossell, S. Eating and exercise behaviors in eating disorders and the general population during the COVID -19 pandemic in Australia: Initial results from the COLLATE project. Int. J. Eat. Disord. 2020, 53, 1158–1165. [Google Scholar] [CrossRef]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Cinelli, G.; Bigioni, G.; Soldati, L.; Attinà, A.; Bianco, F.; Caparello, G.; Camodeca, V.; Carrano, E.; et al. Psychological Aspects and Eating Habits during COVID-19 Home Confinement: Results of EHLC-COVID-19 Italian Online Survey. Utrients 2020, 12, 2152. [Google Scholar] [CrossRef]
- Shahrokni, R.O.; Ferriday, D.; Miguel, S.; Laurent, A.L.; Brunstrom, J.M. Portion size reduction and food choice: The role of perceptual boundaries. Appetite 2021, 157, 104941. [Google Scholar] [CrossRef]
- Husain, M.M.; Black, K.J.; Doraiswamy, P.M.; Shah, S.A.; Rockwell, W.K.; Ellinwood, E.H., Jr.; Krishnan, K.R. Subcortical brain anatomy in anorexia and bulimia. Biol. Psychiatry 1992, 31, 735–738. [Google Scholar] [CrossRef]
- Touyz, S.; Lacey, H.; Hay, P. Eating disorders in the time of COVID-19. J. Eat. Disord. 2020, 8, 19. [Google Scholar] [CrossRef] [PubMed]
- Machado, P.P.P.; Pinto-Bastos, A.; Ramos, R.; Rodrigues, T.F.; Louro, E.; Gonçalves, S.; Brandão, I.; Vaz, A. Impact of COVID-19 lockdown measures on a cohort of eating disorders patients. J. Eat. Disord. 2020, 8, 57. [Google Scholar] [CrossRef]
- Ramalho, S.M.; Trovisqueira, A.; de Lourdes, M.; Gonçalves, S.; Ribeiro, I.; Vaz, A.R.; Machado, P.P.P.; Conceição, E. The impact of COVID-19 lockdown on disordered eating behaviors: The mediation role of psychological distress. Eat. Weight Disord. 2022, 27, 179–188. [Google Scholar] [CrossRef]
- Mihashi, M.; Otsubo, Y.; Yinjuan, X.; Nagatomi, K.; Hoshiko, M.; Ishitake, T. Predictive factors of psychological disorder development during recovery following SARS outbreak. Health Psychol. 2009, 28, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Foroughi, N.; Zhu, K.C.Y.; Smith, C.; Hay, P. The perceived therapeutic benefits of complementary medicine in eating disorders. Complement. Ther. Med. 2019, 4, 176–180. [Google Scholar] [CrossRef]
- Kessler, R.C.; Barker, P.R.; Colpe, L.J.; Epstein, J.F.; Gfroerer, J.C.; Hiripi, E. The Kessler Psychological Distress Scale (K10). Available online: https://www.worksafe.qld.gov.au/__data/assets/pdf_file/0010/22240/kessler-psychological-distress-scale-k101.pdf (accessed on 23 March 2023).
- Dal Grande, E.; Taylor, A.; Wilson, D. South Australian Health and Wellbeing Survey; South Australian Department of Human Services: Adelaide, Australia, 2022.
- Kessler, R.; Barker, P.; Colpe, L.; Epstein, J.; Gfroerer, J.; Hiripi, E.; Howes, M.J.; Normand, S.L.; Manderscheid, R.W.; Walters, E.E.; et al. Screening for serious mental illness in the general population. Arch. Gen. Psychiatry 2003, 60, 184–189. [Google Scholar] [CrossRef]
- Ware, J.E.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef]
- Salyers, M.P.; Bosworth, H.B.; Swanson, J.W.; Lamb-Pagone, J.; Osher, F.C. Reliability and validity of the SF-12 health survey among people with severe mental illness. Med. Care 2000, 38, 1141–1150. [Google Scholar] [CrossRef] [PubMed]
- Beglin, S.J.; Fairburn, C.G. disorders in community samples. Psychiatry Res. 1992, 44, 191–201. [Google Scholar] [CrossRef]
- Mond, J.M.; Hay, P.J.; Rodgers, B.; Owen, C. Eating Disorder examination questionnaire (EDE-Q): Norms for young adult women. Behav. Res. Ther. 2006, 44, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef]
- Fernández-Aranda, F.; Munguía, L.; Mestre-Bach, G.; Steward, T.; Etxandi, M.; Baenas, I.; Granero, R.; Sánchez, I.; Ortega, E.; Andreu, A.; et al. COVID Isolation Eating Scale (CIES): Analysis of the impact of confinement in eating disorders and obesity-A collaborative international study. Eur. Eat. Disord. Rev. 2020, 28, 871–883. [Google Scholar] [CrossRef]
- Kavoor, A.R. COVID-19 in people with mental illness: Challenges and vulnerabilities. Asian J. Psychiatry 2020, 51, 102051. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.C.; Nguyen, M.H.; Do, B.N.; Tran, C.Q.; Nguyen, T.T.; Pham, K.M.; Pham, L.V.; Tran, K.V.; Duong, T.T.; Tran, T.V.; et al. People with suspected COVID-19 symptoms were more likely depressed and had lower health-related quality of life: The potential benefit of health literacy. J. Clin. Med. 2020, 9, 965. [Google Scholar] [CrossRef] [PubMed]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020, 33, e100213. [Google Scholar] [CrossRef]
- Wang, Y.; Di, Y.; Ye, J.; Wei, W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Health Med. 2020, 30, 13–22. [Google Scholar] [CrossRef]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Richter, D.; Riedel-Heller, S.; Zürcher, S.J. Mental health problems in the general population during and after the first lockdown phase due to the SARS-cov-2 pandemic: Rapid review of multi-wave studies. Epidemiol. Psychiatr. Sci. 2021, 30, e27. [Google Scholar] [CrossRef] [PubMed]
- Castellini, G.; Cassioli, E.; Rossi, E.; Innocenti, M.; Gironi, V.; Sanfilippo, G.; Felciai, F.; Monteleone, A.M.; Ricca, V. The impact of COVID-19 epidemic on eating disorders: A longitudinal observation of pre versus post psychopathological features in a sample of patients with eating disorders and a group of healthy controls. Int. J. Eat. Disord. 2020, 53, 1855–1862. [Google Scholar] [CrossRef]
- Daly, M.; Robinson, R. Longitudinal changes in psychological distress in the UK from 2019 to September 2020 during the COVID-19 pandemic: Evidence from a large nationally representative study. Psychiatry Res. 2021, 300, 113920. [Google Scholar] [CrossRef]
- Levinson, C.A.; Brosof, L.C.; Vanzhula, I.; Christian, C.; Jones, P.; Rodebaugh, T.L.; Langer, J.K.; White, E.K.; Warren, C.; Weeks, J.W.; et al. Social anxiety and eating disorder comorbidity and underlying vulnerabilities: Using network analysis to conceptualize comorbidity. Int. J. Eat. Disord. 2018, 51, 693–709. [Google Scholar] [CrossRef]
- Linardon, J.; Messer, M.; Rodgers, R.F.; Fuller-Tyszkiewicz, M. A systematic scoping review of research on COVID-19 impacts on eating disorders: A critical appraisal of the evidence and recommendations for the field. Int. J. Eat. Disord. 2022, 55, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Eddy, K.T.; Tabri, N.; Thomas, J.J.; Murray, H.B.; Keshaviah, A.; Hastings, E.; Edkins, K.; Krishna, M.; Herzog, D.B.; Keel, P.K.; et al. Recovery from anorexia nervosa and bulimia nervosa at 22-year follow-up. J. Clin. Psychiatry 2017, 22, 17085. [Google Scholar] [CrossRef]
- Mond, J.M.; Hay, P.; Rodgers, B.; Owen, C.; Crosby, R.; Mitchell, J.E. Use of extreme weight control behaviors with and without binge eating in a community sample of women: Implications for the classification of bulimic-type eating disorders. Int. J. Eat. Disord. 2006, 39, 294–302. [Google Scholar] [CrossRef] [PubMed]
- Mond, J.; Hay, P.; Paxton, S.; Rodgers, B.; Darby, A.; Nillson, J.; Quirk, F.; Owen, C. Eating Disorders “Mental Health Literacy” in Low Risk, High Risk and Symptomatic Women: Implications for Health Promotion Programs. Eat. Disord. 2010, 18, 267–285. [Google Scholar] [CrossRef] [PubMed]
- Mond, J.M.; Hay, P.J.; Rodgers, B.; Owen, C. Health service utilization for eating disorders: Findings from a community-based study. Int. J. Eat. Disord. 2007, 40, 399–408. [Google Scholar] [CrossRef]
- Mitchison, D.; Morin, A.; Mond, J.; Slewa-Younan, S.; Hay, P. The bidirectional relationship between quality of life and eating disorder symptoms: A 9-year community-based study of Australian women. PLoS ONE 2015, 26, e0120591. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Australians Pursuing Higher Education in Record Numbers. 2017. Available online: https://www.abs.gov.au/AUSSTATS/abs@.nsf/mediareleasesbyReleaseDate/1533FE5A8541D66CCA2581BF00362D1D (accessed on 17 September 2021).

| Variables | N (%) |
|---|---|
| Marital status | |
| Single | 34 (14.7) |
| Married | 102 (44.0) |
| Living as married | 47 (20.3) |
| Separated or divorced | 33 (14.2) |
| Widowed | 2 (0.9) |
| Occupation | |
| Employed fulltime | 112 (48.3) |
| Employed Part time | 51 (22) |
| Home maker ^ | 9 (3.9) |
| Student | 6 (2.6) |
| Not employed, recovering, other | 25 (10.8) |
| Education | |
| Year 10 & 12 | 15 (6.5) |
| Trade certificate | 1 (0.4) |
| Undergraduate | 9 (3.9) |
| University degree | 193 (83.1) |
| Mean (SD), Median (Range), n | |
| BMI (kg/m2) | 28.2 (6.7), 26.7 (39.01), 211 |
| EDE-Q | |
| Restraint | 2.9 (1.7), 2.8 (7.0), 209 |
| Eating Concern | 2.2 (1.4), 1.6 (6.20), 205 |
| Weight concern | 3.3 (1.6), 3.0 (6.20), 210 |
| Shape concern | 3.8 (1.7), 3.9 (6.25), 208 |
| Global score | 3.0 (1.4), 2.7 (6.04), 194 |
| Psychological distress (Kessler 10) | 19.1 (7.7), 17.0 (40.0), 208 |
| Physical health related quality of life (SF-12) | 48.4 (9.5), 51.7 (46.7), 203 |
| Mental health related quality of life (SF-12) | 45.5 (12), 50.4 (48.2), 203 |
| Emotional Ormental Health Problems | Eating Disorders | Lose Weight | |
|---|---|---|---|
| N (%) | |||
| Used some type of treatment | 136 (58.6) | 39 (16.8) | 72 (31) |
| Talked about the problem | 110 (47.4) | 17 (7.3) | 11 (4.7) |
| Psychotherapy (focus on cause) | 42 (18.1) | 6 (2.6) | 4 (1.7) |
| Psychotherapy (Cognitive Behaviour Therapy) | 45 (19.4) | 9 (3.9) | 9 (3.9) |
| Psychotherapy (focus on current relationships) | 38 (16.4) | 3 (1.3) | 2 (.9) |
| Alternative therapy (naturopathy, homeopathy, aromatherapy) | 22 (9.5) | 2 (.9) | 5 (2.2) |
| Massage, spinal manipulation, or acupuncture | 62 (26.7) | 1 (.4) | 3 (1.3) |
| Relaxation therapy (meditation, stress management, yoga) | 72 (31) | 6 (2.6) | 7 (3.0) |
| Assertiveness or social skills training | 9 (3.9) | 1 (.4) | 1 (.4) |
| Drinking alcohol to relax | 60 (25.9) | 3 (1.3) | 3 (1.3) |
| Hypnosis | 5 (2.2) | 2 (.9) | 3 (1.3) |
| Following a self-help treatment manual | 25 (10.8) | 6 (2.6) | 9 (3.9) |
| Getting fit by increasing time spent on exercise | 80 (34.5) | 17 (7.3) | 57 (24.6) |
| Getting out and about more or finding some new hobbies | 60 (25.9) | 5 (2.2) | 8 (3.4) |
| Getting information about the problem and available services | 45 (19.4) | 5 (2.2) | 9 (3.9) |
| Medication (valium, serapax) | 25 (10.8) | 3 (1.3) | 3 (1.3) |
| Anti-depressant medication (Prozac or Zoloft) | 42 (18.1) | 4 (1.7) | 4 (1.7) |
| Vitamins and/or minerals (folate, B group vitamins, amino acids etc) | 55 (23.7) | 5 2.2 | 5 (2.2) |
| Herbal medicines (Valerian, St John’s Wort, ginseng) | 19 (8.2) | 4 1.7 | 6 (2.6) |
| Medicare Item Use | N (%) |
|---|---|
| Attempted using the items | 2 (0.9) |
| Accessed & used the items | 4 (1.7) |
| No attempt/not aware of it | 202 (87.1) |
| N (%) | |
|---|---|
| Had COVID-19 | 0 |
| Tested for COVID-19 | 107 (46.1) |
| Self isolated for 14 days | 15 (6.5) |
| CVID-19′s effect on Work and/or study | |
| Stopped attending work and/or study in person | 48 (20.7) |
| Continued work and/or study at home (online) | 76 (32.8) |
| Stopped work and/or study all together | 9 (3.9) |
| Continued work and/or study in person | 97 (41.8) |
| COVID-19’s effect on other activities such as sport, music, clubs, etc. | |
| Stopped attending activities in person | 71 (30.6) |
| Continued activities at home (online) | 63 (27.2) |
| Stopped activities all together | 17 (7.3) |
| Continued activities in person | 54 (23.3) |
| COVID-19’s effect on social life | |
| Stopped socializing in person | 31 (13.4) |
| Socializing via phone (online) | 45 (19.4) |
| Stopped socializing all together (even online) | 26 (11.2) |
| Continued socializing in person | 87 (37.5) |
| COVID-19’s effect on household such as family and housemates | |
| One or more persons had COVID-19 | 1 (0.4) |
| One or more persons were unable to work | 14 (6.0) |
| One or more persons are essential health worker | 15 (5.2) |
| I am an essential health worker | 62 (26.7) |
| None of the above | 129 (55.6) |
| COVID-19’s effect on eating | |
| Not at all | 119 (51.3) |
| More disordered eating (overeating, binge) | 59 (25.4) |
| More dieting and/or exercise for weight control/loss | 29 (12.5) |
| More weight/shape/eating concerns | 39 (16.8) |
| Weeks unbale to attend work | |
| Not applicable | 107 (46.1) |
| Unable to attend | 98 (42.2) |
| Worried about contracting COVID-19 | |
| Not at all | 56 (24.1) |
| A little worried | 81 (34.9) |
| Moderately worried | 49 (21.1) |
| Very worried | 11 (4.7) |
| Extremely worried | 13 (5.6) |
| Worried about a family member contracting COVID-19 | |
| Not at all | 27 (11.6) |
| A little worried | 79 (34.1) |
| Moderately worried | 48 (20.7) |
| Very worried | 39 (16.8) |
| Extremely worried | 17 (7.3) |
| Rate the information delivery about COVID-19 | |
| Very clear and understandable | 35 (15.1) |
| Quite clear and understandable | 90 (38.8) |
| Neutral | 37 (15.9) |
| Quiet confusing | 30 (12.9) |
| Very confusing | 16 (6.9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Foroughi, N.; Hay, P.; Mannan, H. Community Women’s Lifestyle and Eating Disorders in the Era of COVID-19 Pandemic: A 15-Year Follow-Up Study. Nutrients 2023, 15, 1676. https://doi.org/10.3390/nu15071676
Foroughi N, Hay P, Mannan H. Community Women’s Lifestyle and Eating Disorders in the Era of COVID-19 Pandemic: A 15-Year Follow-Up Study. Nutrients. 2023; 15(7):1676. https://doi.org/10.3390/nu15071676
Chicago/Turabian StyleForoughi, Nasim, Phillipa Hay, and Haider Mannan. 2023. "Community Women’s Lifestyle and Eating Disorders in the Era of COVID-19 Pandemic: A 15-Year Follow-Up Study" Nutrients 15, no. 7: 1676. https://doi.org/10.3390/nu15071676
APA StyleForoughi, N., Hay, P., & Mannan, H. (2023). Community Women’s Lifestyle and Eating Disorders in the Era of COVID-19 Pandemic: A 15-Year Follow-Up Study. Nutrients, 15(7), 1676. https://doi.org/10.3390/nu15071676






