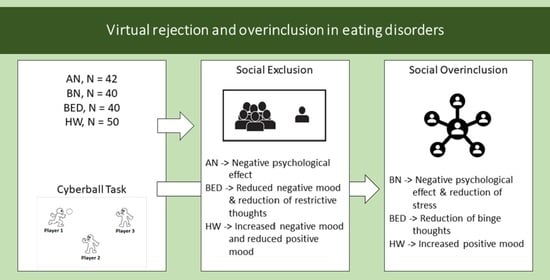
Virtual Rejection and Overinclusion in Eating Disorders: An Experimental Investigation of the Impact on Emotions, Stress Perception, and Food Attitudes
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Materials
2.2.1. Self-Reported Measures
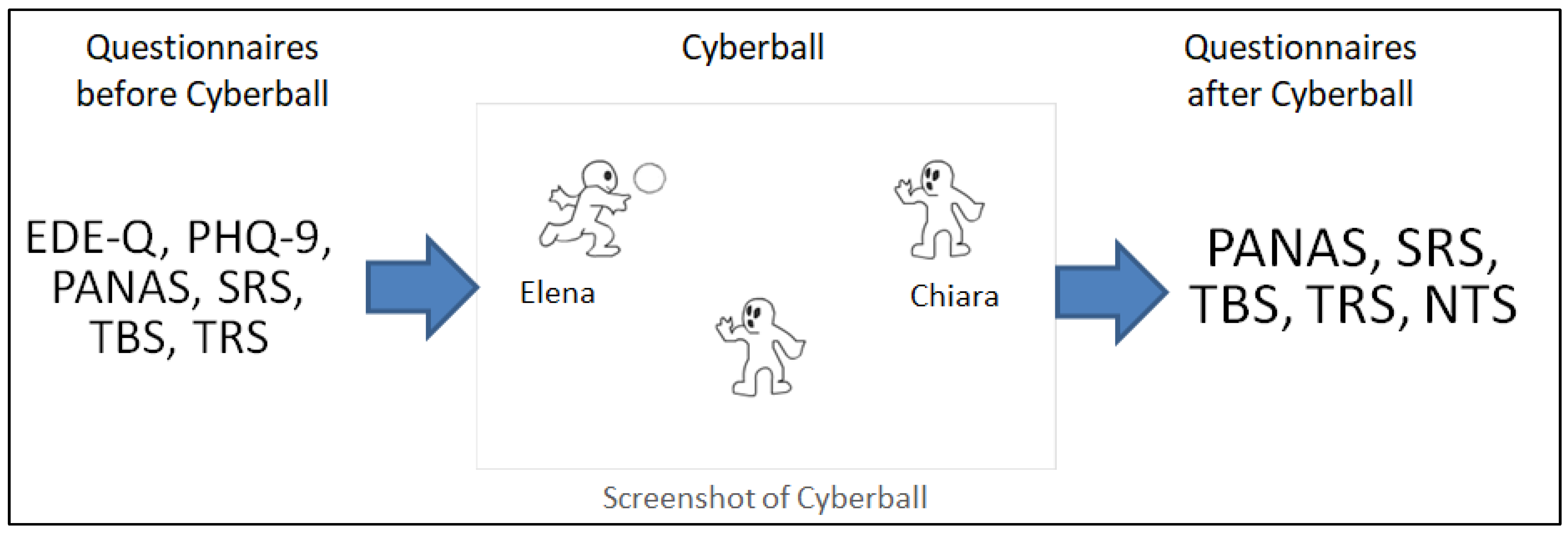
2.2.2. Cyberball Task
2.3. Procedure
2.4. Statistical Analyses
3. Results
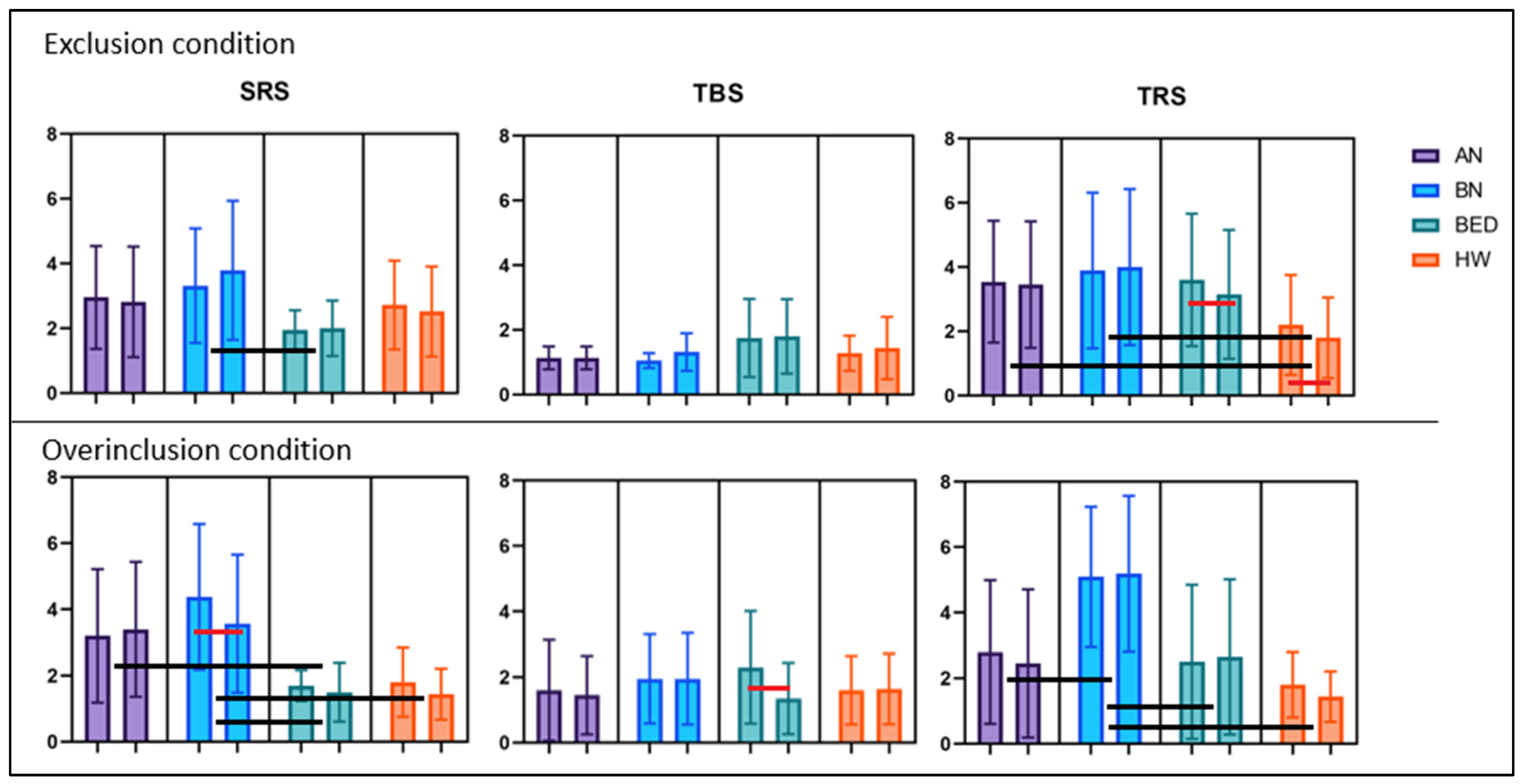
3.1. Exclusion Condition
3.2. Overinclusion Condition
3.3. Conditions Comparison
3.4. Correlations
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mason, T.B.; Lesser, E.L.; Dolgon-Krutolow, A.R.; Wonderlich, S.A.; Smith, K.E. An Updated Transdiagnostic Review of Social Cognition and Eating Disorder Psychopathology. J. Psychiatr. Res. 2021, 143, 602–627. [Google Scholar] [CrossRef]
- Meneguzzo, P.; Todisco, P.; Calonaci, S.; Mancini, C.; Dal Brun, D.; Collantoni, E.; Donini, L.M.; Tenconi, E.; Favaro, A. Health-Related Quality of Life Assessment in Eating Disorders: Adjustment and Validation of a Specific Scale with the Inclusion of an Interpersonal Domain. Eat. Weight. Disord. 2020, 26, 2251–2262. [Google Scholar] [CrossRef] [PubMed]
- Caglar-Nazali, H.P.; Corfield, F.; Cardi, V.; Ambwani, S.; Leppanen, J.; Olabintan, O.; Deriziotis, S.; Hadjimichalis, A.; Scognamiglio, P.; Eshkevari, E.; et al. A Systematic Review and Meta-Analysis of “Systems for Social Processes” in Eating Disorders. Neurosci. Biobehav. Rev. 2014, 42, 55–92. [Google Scholar] [CrossRef] [PubMed]
- Corsi, E.; Cardi, V.; Sowden, S.; Coll, M.P.; Cascino, G.; Ricca, V.; Treasure, J.; Bird, G.; Monteleone, A.M. Socio-Cognitive Processing in People with Eating Disorders: Computerized Tests of Mentalizing, Empathy and Imitation Skills. Int. J. Eat. Disord. 2021, 54, 1509–1518. [Google Scholar] [CrossRef] [PubMed]
- Marzola, E.; Porliod, A.; Panero, M.; De-Bacco, C.; Abbate-Daga, G. Affective Temperaments and Eating Psychopathology in Anorexia Nervosa: Which Role for Anxious and Depressive Traits? J. Affect. Disord. 2020, 266, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Monteleone, A.M.; Treasure, J.; Kan, C.; Cardi, V. Reactivity to Interpersonal Stress in Patients with Eating Disorders: A Systematic Review and Meta-Analysis of Studies Using an Experimental Paradigm. Neurosci. Biobehav. Rev. 2018, 87, 133–150. [Google Scholar] [CrossRef] [PubMed]
- McFillin, R.K.; Cahn, S.C.; Burks, V.S.; Levine, M.P.; Loney, S.L.; Levine, R.L. Social Information-Processing and Coping in Adolescent Females Diagnosed With an Eating Disorder: Toward a Greater Understanding of Control. Eat. Disord. 2012, 20, 42–59. [Google Scholar] [CrossRef] [PubMed]
- Bronstein, M.V.; Everaert, J.; Kummerfeld, E.; Haynos, A.F.; Vinogradov, S. Biased and Inflexible Interpretations of Ambiguous Social Situations: Associations with Eating Disorder Symptoms and Socioemotional Functioning. Int. J. Eat. Disord. 2022, 55, 518–529. [Google Scholar] [CrossRef]
- Levinson, C.A.; Rodebaugh, T.L. Social Anxiety and Eating Disorder Comorbidity: The Role of Negative Social Evaluation Fears. Eat. Behav. 2012, 13, 27–35. [Google Scholar] [CrossRef]
- Schaumberg, K.; Reilly, E.E.; Gorrell, S.; Levinson, C.A.; Farrell, N.R.; Brown, T.A.; Smith, K.M.; Schaefer, L.M.; Essayli, J.H.; Haynos, A.F.; et al. Conceptualizing Eating Disorder Psychopathology Using an Anxiety Disorders Framework: Evidence and Implications for Exposure-Based Clinical Research. Clin. Psychol. Rev. 2021, 83, 101952. [Google Scholar] [CrossRef]
- Menatti, A.R.; DeBoer, L.B.H.; Weeks, J.W.; Heimberg, R.G. Social Anxiety and Associations with Eating Psychopathology: Mediating Effects of Fears of Evaluation. Body Image 2015, 14, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Cook, S.I.; Moore, S.; Bryant, C.; Phillips, L.J. The Role of Fear of Positive Evaluation in Social Anxiety: A Systematic Review and Meta-Analysis. Clin. Psychol. Sci. Pract. 2022, 29, 352. [Google Scholar] [CrossRef]
- Levinson, C.A.; Sala, M.; Murray, S.; Ma, J.; Rodebaugh, T.L.; Lenze, E.J. Diagnostic, Clinical, and Personality Correlates of Food Anxiety during a Food Exposure in Patients Diagnosed with an Eating Disorder. Eat. Weight. Disord. 2019, 24, 1079–1088. [Google Scholar] [CrossRef] [PubMed]
- Robinson, K.; Wade, T.D. Perfectionism Interventions Targeting Disordered Eating: A Systematic Review and Meta-Analysis. Int. J. Eat. Disord. 2021, 54, 473–487. [Google Scholar] [CrossRef]
- Arcelus, J.; Haslam, M.; Farrow, C.; Meyer, C. The Role of Interpersonal Functioning in the Maintenance of Eating Psychopathology: A Systematic Review and Testable Model. Clin. Psychol. Rev. 2013, 33, 156–167. [Google Scholar] [CrossRef]
- Brockmeyer, T.; Walther, S.; Ingenerf, K.; Wild, B.; Hartmann, M.; Weisbrod, M.; Weber, M.A.; Eckhardt-Henn, A.; Herzog, W.; Friederich, H.C. Brain Effects of Computer-Assisted Cognitive Remediation Therapy in Anorexia Nervosa: A Pilot FMRI Study. Psychiatry Res. Neuroimaging 2016, 249, 52–56. [Google Scholar] [CrossRef]
- Carter, J.C.; Mercer-Lynn, K.B.; Norwood, S.J.; Bewell-Weiss, C.V.; Crosby, R.D.; Woodside, D.B.; Olmsted, M.P. A Prospective Study of Predictors of Relapse in Anorexia Nervosa: Implications for Relapse Prevention. Psychiatry Res. 2012, 200, 518–523. [Google Scholar] [CrossRef]
- Courty, A.; Godart, N.; Lalanne, C.; Berthoz, S. Alexithymia, a Compounding Factor for Eating and Social Avoidance Symptoms in Anorexia Nervosa. Compr. Psychiatry 2015, 56, 217–228. [Google Scholar] [CrossRef]
- Christensen, K.A.; Haynos, A.F. A Theoretical Review of Interpersonal Emotion Regulation in Eating Disorders: Enhancing Knowledge by Bridging Interpersonal and Affective Dysfunction. J. Eat. Disord. 2020, 8, 21. [Google Scholar] [CrossRef]
- Bora, E.; Köse, S. Meta-Analysis of Theory of Mind in Anorexia Nervosa and Bulimia Nervosa: A Specific İmpairment of Cognitive Perspective Taking in Anorexia Nervosa? Int. J. Eat. Disord. 2016, 49, 739–740. [Google Scholar] [CrossRef]
- Aloi, M.; Rania, M.; Caroleo, M.; De Fazio, P.; Segura-García, C. Social Cognition and Emotional Functioning in Patients with Binge Eating Disorder. Eur. Eat. Disord. Rev. 2017, 25, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Westwood, H.; Kerr-Gaffney, J.; Stahl, D.; Tchanturia, K. Alexithymia in Eating Disorders: Systematic Review and Meta-Analyses of Studies Using the Toronto Alexithymia Scale. J. Psychosom. Res. 2017, 99, 66–81. [Google Scholar] [CrossRef] [PubMed]
- Vartanian, L.R.; Porter, A.M. Weight Stigma and Eating Behavior: A Review of the Literature. Appetite 2016, 102, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Cardi, V.; Turton, R.; Schifano, S.; Leppanen, J.; Hirsch, C.R.; Treasure, J. Biased Interpretation of Ambiguous Social Scenarios in Anorexia Nervosa. Eur. Eat. Disord. Rev. 2017, 25, 60–64. [Google Scholar] [CrossRef]
- Reinhard, M.A.; Dewald-Kaufmann, J.; Wüstenberg, T.; Musil, R.; Barton, B.B.; Jobst, A.; Padberg, F. The Vicious Circle of Social Exclusion and Psychopathology: A Systematic Review of Experimental Ostracism Research in Psychiatric Disorders. Eur. Arch. Psychiatry Clin. Neurosci. 2020, 270, 521–532. [Google Scholar] [CrossRef]
- Baumeister, R.F.; Brewer, L.E.; Tice, D.M.; Twenge, J.M. Thwarting the Need to Belong: Understanding the Interpersonal and Inner Effects of Social Exclusion. Soc. Pers. Psychol. Compass 2007, 1, 506–520. [Google Scholar] [CrossRef]
- Salvy, S.J.; de la Haye, K.; Bowker, J.C.; Hermans, R.C.J. Influence of Peers and Friends on Children’s and Adolescents’ Eating and Activity Behaviors. Physiol. Behav. 2012, 106, 369–378. [Google Scholar] [CrossRef]
- Tuschen-Caffier, B.; Vögele, C. Psychological and Physiological Reactivity to Stress: An Experimental Study on Bulimic Patients, Restrained Eaters and Controls. Psychother. Psychosom. 1999, 68, 333–340. [Google Scholar] [CrossRef]
- Dalgleish, T.; Walsh, N.D.; Mobbs, D.; Schweizer, S.; Van Harmelen, A.L.; Dunn, B.; Dunn, V.; Goodyer, I.; Stretton, J. Social Pain and Social Gain in the Adolescent Brain: A Common Neural Circuitry Underlying Both Positive and Negative Social Evaluation. Sci. Rep. 2017, 7, 42010. [Google Scholar] [CrossRef]
- Fredrick, J.W.; Luebbe, A.M. Fear of Positive Evaluation and Social Anxiety: A Systematic Review of Trait-Based Findings. J. Affect. Disord. 2020, 265, 157–168. [Google Scholar] [CrossRef]
- Williams, K.D.K.D.; Jarvis, B. Cyberball: A Program for Use in Research on Interpersonal Ostracism and Acceptance. J. Behav. Res. Methods 2006, 38, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Heeren, A.; Dricot, L.; Billieux, J.; Philippot, P.; Grynberg, D.; De Timary, P.; Maurage, P. Correlates of Social Exclusion in Social Anxiety Disorder: An FMRI Study. Sci. Rep. 2017, 7, 260. [Google Scholar] [CrossRef] [PubMed]
- Seidl, E.; Padberg, F.; Bauriedl-Schmidt, C.; Albert, A.; Daltrozzo, T.; Hall, J.; Renneberg, B.; Seidl, O.; Jobst, A. Response to Ostracism in Patients with Chronic Depression, Episodic Depression and Borderline Personality Disorder a Study Using Cyberball. J. Affect. Disord. 2020, 260, 254–262. [Google Scholar] [CrossRef] [PubMed]
- Sebastian, C.; Blakemore, S.J.; Charman, T. Reactions to Ostracism in Adolescents with Autism Spectrum Conditions. J. Autism. Dev. Disord. 2009, 39, 1122–1130. [Google Scholar] [CrossRef] [PubMed]
- Schell, S.E.; Banica, I.; Weinberg, A.; Racine, S.E. Hunger Games: Associations between Core Eating Disorder Symptoms and Responses to Rejection by Peers during Competition. Int. J. Eat. Disord. 2021, 54, 802–811. [Google Scholar] [CrossRef]
- Senese, V.P.; Pezzella, M.; Pasquariello, L.; Ali, S.; Rohner, R.P. Effects of Social Exclusion and Maternal Rejection on Children’s High-Caloric Food Consumption. Appetite 2020, 145, 104494. [Google Scholar] [CrossRef]
- Salvy, S.J.; Bowker, J.C.; Nitecki, L.A.; Kluczynski, M.A.; Germeroth, L.J.; Roemmich, J.N. Impact of Simulated Ostracism on Overweight and Normal-Weight Youths’ Motivation to Eat and Food Intake. Appetite 2011, 56, 39–45. [Google Scholar] [CrossRef]
- Weiss, M.; Huppert, J.D. Shy, but Why? Vulnerable Narcissism and Avoidant Personality in Terms of Explicit and Implicit Interpretation Bias and Social Acceptance. Curr. Psychol. 2022, 2022, 1–13. [Google Scholar] [CrossRef]
- Karp, J.N.; Makol, B.A.; Keeley, L.M.; Qasmieh, N.; Deros, D.E.; Weeks, J.W.; Racz, S.J.; Lipton, M.F.; Augenstein, T.M.; De Los Reyes, A. Convergent, Incremental, and Criterion-Related Validity of Multi-Informant Assessments of Adolescents’ Fears of Negative and Positive Evaluation. Clin. Psychol. Psychother. 2018, 25, 217–230. [Google Scholar] [CrossRef]
- Tanaka, H.; Ikegami, T. Fear of Negative Evaluation Moderates Effects of Social Exclusion on Selective Attention to Social Signs. Cogn. Emot. 2015, 29, 1306–1313. [Google Scholar] [CrossRef]
- Meneguzzo, P.; Collantoni, E.; Bonello, E.; Busetto, P.; Tenconi, E.; Favaro, A. The Predictive Value of the Early Maladaptive Schemas in Social Situations in Anorexia Nervosa. Eur. Eat. Disord. Rev. 2020, 28, 318–331. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5); American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Fairburn, C.G.; Beglin, S.J. Assessment of Eating Disorder: Interview or Self-Report Questionnaire? Int. J. Eat. Disord. 1994, 16, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W.W. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Watson, D.; Clark, L.A.; Tellegen, A. Development and Validation of Brief Measures of Positive and Negative Affect: The PANAS Scales. J. Pers. Soc. Psychol. 1988, 54, 1063–1070. [Google Scholar] [CrossRef]
- Gerber, J.P.; Chang, S.-H.; Reimel, H. Construct Validity of Williams’ Ostracism Needs Threat Scale. Pers. Individ. Dif. 2017, 115, 50–53. [Google Scholar] [CrossRef]
- Zadro, L.; Williams, K.D.; Richardson, R. How Low Can You Go? Ostracism by a Computer Is Sufficient to Lower Self-Reported Levels of Belonging, Control, Self-Esteem, and Meaningful Existence. J. Exp. Soc. Psychol. 2004, 40, 560–567. [Google Scholar] [CrossRef]
- Hawes, D.J.; Zadro, L.; Fink, E.; Richardson, R.; O’Moore, K.; Griffiths, B.; Dadds, M.R.; Williams, K.D. The Effects of Peer Ostracism on Children’s Cognitive Processes. Eur. J. Dev. Psychol. 2012, 9, 599–613. [Google Scholar] [CrossRef]
- De Panfilis, C.; Riva, P.; Preti, E.; Cabrino, C.; Marchesi, C. When Social Inclusion Is Not Enough: Implicit Expectations of Extreme Inclusion in Borderline Personality Disorder. Personal. Disord. Theory Res. Treat. 2015, 6, 301. [Google Scholar] [CrossRef]
- Weinbrecht, A.; Niedeggen, M.; Roepke, S.; Renneberg, B. Feeling Excluded No Matter What? Bias in the Processing of Social Participation in Borderline Personality Disorder. Neuroimage Clin. 2018, 19, 343–350. [Google Scholar] [CrossRef]
- Wendler, D.; Miller, F.G. Deception in the Pursuit of Science. Arch. Intern. Med. 2004, 164, 597–600. [Google Scholar] [CrossRef]
- Treasure, J.; Corfield, F.; Cardi, V. A Three-Phase Model of the Social Emotional Functioning in Eating Disorders. Eur. Eat. Disord. Rev. 2012, 20, 431–438. [Google Scholar] [CrossRef] [PubMed]
- Björck, C.; Clinton, D.; Sohlberg, S.; Hällström, T.; Norring, C. Interpersonal Profiles in Eating Disorders: Ratings of SASB Self-Image. Psychol. Psychother. Theory Res. Pract. 2003, 76, 337–349. [Google Scholar] [CrossRef] [PubMed]
- Treasure, J. Treatment Resistance in Eating Disorders: A Question of Uncertain Targets or Insufficient Personalization? Int. Rev. Psychiatry 2019, 31, 305–307. [Google Scholar] [CrossRef] [PubMed]
- Anderson, L.K.; Claudat, K.; Cusack, A.; Brown, T.A.; Trim, J.; Rockwell, R.; Nakamura, T.; Gomez, L.; Kaye, W.H. Differences in Emotion Regulation Difficulties among Adults and Adolescents across Eating Disorder Diagnoses. J. Clin. Psychol. 2018, 74, 1867–1873. [Google Scholar] [CrossRef]
- De Paoli, T.; Fuller-Tyszkiewicz, M.; Krug, I. Insecure Attachment and Maladaptive Schema in Disordered Eating: The Mediating Role of Rejection Sensitivity. Clin. Psychol. Psychother. 2017, 24, 1273–1284. [Google Scholar] [CrossRef]
- De Sampaio, F.T.P.; Soneira, S.; Aulicino, A.; Harris, P.; Allegri, R.F. Emotional Reactivity to Social Stimuli in Patients with Eating Disorders. Psychiatry Res. 2015, 229, 887–894. [Google Scholar] [CrossRef]
- Mallorquí-Bagué, N.; Vintró-Alcaraz, C.; Sánchez, I.; Riesco, N.; Agüera, Z.; Granero, R.; Jiménez-Múrcia, S.; Menchón, J.M.; Treasure, J.; Fernández-Aranda, F. Emotion Regulation as a Transdiagnostic Feature Among Eating Disorders: Cross-Sectional and Longitudinal Approach. Eur. Eat. Disord. Rev. 2018, 26, 53–61. [Google Scholar] [CrossRef]
- Danner, U.N.; Sternheim, L.; Evers, C. The Importance of Distinguishing between the Different Eating Disorders (Sub) Types When Assessing Emotion Regulation Strategies. Psychiatry Res. 2014, 215, 727–732. [Google Scholar] [CrossRef]
- Meneguzzo, P.; Garolla, A.; Bonello, E.; Todisco, P. Alexithymia, Dissociation, and Emotional Regulation in Eating Disorders: Evidence of Improvement through Specialized Inpatient Treatment. Clin. Psychol. Psychother. 2021, 29, 718–724. [Google Scholar] [CrossRef]
- Longo, P.; Panero, M.; Amodeo, L.; Demarchi, M.; Abbate-Daga, G.; Marzola, E. Psychoform and Somatoform Dissociation in Anorexia Nervosa: A Systematic Review. Clin. Psychol. Psychother. 2021, 28, 295–312. [Google Scholar] [CrossRef]
- Meneguzzo, P.; Tenconi, E.; Collantoni, E.; Longobardi, G.; Zappalà, A.; Vindigni, V.; Favaro, A.; Pavan, C. The Cyberball Task in People after Obesity Surgery: Preliminary Evaluation of Cognitive Effects of Social Inclusion and Exclusion with a Laboratory Task. Eat. Weight. Disord. 2021, 27, 1523–1533. [Google Scholar] [CrossRef] [PubMed]
- Duchesne, M.; De Oliveira Falcone, E.M.; De Freitas, S.R.; D’Augustin, J.F.; Marinho, V.; Appolinario, J.C. Assessment of Interpersonal Skills in Obese Women with Binge Eating Disorder. J. Health Psychol. 2012, 17, 1065–1075. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.E.; Mason, T.B.; Schaefer, L.M.; Juarascio, A.; Dvorak, R.; Weinbach, N.; Crosby, R.D.; Wonderlich, S.A. Examining Intra-Individual Variability in Food-Related Inhibitory Control and Negative Affect as Predictors of Binge Eating Using Ecological Momentary Assessment. J. Psychiatr. Res. 2020, 120, 137–143. [Google Scholar] [CrossRef] [PubMed]
- DeWall, C.N.; Twenge, J.M.; Koole, S.L.; Baumeister, R.F.; Marquez, A.; Reid, M.W. Automatic Emotion Regulation After Social Exclusion: Tuning to Positivity. Emotion 2011, 11, 623–636. [Google Scholar] [CrossRef] [PubMed]
- Almeida, L.; Savoy, S.; Boxer, P. The Role of Weight Stigmatization in Cumulative Risk for Binge Eating. J. Clin. Psychol. 2011, 67, 278–292. [Google Scholar] [CrossRef] [PubMed]
- Sawaoka, T.; Barnes, R.D.; Blomquist, K.K.; Masheb, R.M.; Grilo, C.M. Social Anxiety and Self-Consciousness in Binge Eating Disorder: Associations with Eating Disorder Psychopathology. Compr. Psychiatry 2012, 53, 740–745. [Google Scholar] [CrossRef]
- Dingemans, A.; Danner, U.; Parks, M. Emotion Regulation in Binge Eating Disorder: A Review. Nutrients 2017, 9, 1274. [Google Scholar] [CrossRef]
- Schag, K.; Leehr, E.J.; Meneguzzo, P.; Martus, P.; Zipfel, S.; Giel, K.E. Food-Related Impulsivity Assessed by Longitudinal Laboratory Tasks Is Reduced in Patients with Binge Eating Disorder in a Randomized Controlled Trial. Sci. Rep. 2021, 11, 8225. [Google Scholar] [CrossRef]
- Clyne, C.; Latner, J.D.; Gleaves, D.H.; Blampied, N.M. Treatment of Emotional Dysregulation in Full Syndrome and Subthreshold Binge Eating Disorder. Eat. Disord. 2010, 18, 408–424. [Google Scholar] [CrossRef]
- Barkus, E.; Badcock, J.C. A Transdiagnostic Perspective on Social Anhedonia. Front. Psychiatry 2019, 10, 216. [Google Scholar] [CrossRef]
- Alcalá-Herrera, V.; Marván, M.L. Early Menarche, Depressive Symptoms, and Coping Strategies. J. Adolesc. 2014, 37, 905–913. [Google Scholar] [CrossRef] [PubMed]
- Barrau-Sastre, P.; Birulés, I.; Verdaguer-Rodríguez, M.; López-Carrilero, R.; Ferrer-Quintero, M.; García-Mieres, H.; Díaz-Cutraro, L.; Grasa, E.; Pousa, E.; Lorente, E.; et al. Influence of Menstrual Cycle Length and Age at Menarche on Symptoms, Cognition, Social Cognition, and Metacognition in Patients with First-Episode Psychosis. Women 2022, 2, 135–146. [Google Scholar] [CrossRef]
- Shen, Y.; Varma, D.S.; Zheng, Y.; Boc, J.; Hu, H. Age at Menarche and Depression: Results from the NHANES 2005-2016. PeerJ 2019, 7, e7150. [Google Scholar] [CrossRef] [PubMed]
- Abraham, S.; Boyd, C.; Lal, M.; Luscombe, G.; Taylor, A. Time since Menarche, Weight Gain and Body Image Awareness among Adolescent Girls: Onset of Eating Disorders? J. Psychosom. Obstet. Gynecol. 2009, 30, 89–94. [Google Scholar] [CrossRef]
- Steiner, M.; Dunn, E.; Born, L. Hormones and Mood: From Menarche to Menopause and Beyond. J. Affect. Disord. 2003, 74, 67–83. [Google Scholar] [CrossRef]
- Chung, Y.S.; Poppe, A.; Novotny, S.; Epperson, C.N.; Kober, H.; Granger, D.A.; Blumberg, H.P.; Ochsner, K.; Gross, J.J.; Pearlson, G.; et al. A Preliminary Study of Association between Adolescent Estradiol Level and Dorsolateral Prefrontal Cortex Activity during Emotion Regulation. Psychoneuroendocrinology 2019, 109, 104398. [Google Scholar] [CrossRef]
- Smith, K.E.; Mason, T.B.; Anderson, N.L.; Lavender, J.M. Unpacking Cognitive Emotion Regulation in Eating Disorder Psychopathology: The Differential Relationships between Rumination, Thought Suppression, and Eating Disorder Symptoms among Men and Women. Eat. Behav. 2019, 32, 95–100. [Google Scholar] [CrossRef]
- Mikhail, M.E.; Kring, A.M. Emotion Regulation Strategy Use and Eating Disorder Symptoms in Daily Life. Eat. Behav. 2019, 34, 101315. [Google Scholar] [CrossRef]
- Monteleone, A.M.; Cascino, G.; Marciello, F.; Abbate-Daga, G.; Baiano, M.; Balestrieri, M.; Barone, E.; Bertelli, S.; Carpiniello, B.; Castellini, G.; et al. Risk and Resilience Factors for Specific and General Psychopathology Worsening in People with Eating Disorders during COVID-19 Pandemic: A Retrospective Italian Multicentre Study. Eat. Weight. Disord. 2021, 26, 2443–2452. [Google Scholar] [CrossRef]
- Meneguzzo, P.; Sala, A.; Merlino, L.; Ceccato, E.; Santonastaso, P. One Year of COVID-19 Pandemic on Patients with Eating Disorders, Healthy Sisters, and Community Women: Evidence of Psychological Vulnerabilities. Eat. Weight. Disord. Stud. Anorex. Bulim. Obes. 2022, 27, 3429–3438. [Google Scholar] [CrossRef]
- Meneguzzo, P.; de Mico, A.; Gori, P.; Ajello, A.; Ceccato, E.; Consolati, M.D.; Vita, A.; Sala, A.; Santonastaso, P. A Multicenter Network Analysis Examining the Psychological Effects of the COVID-19 Pandemic on Patients with Eating Disorders versus Their Healthy Siblings. J. Clin. Med. 2022, 11, 7187. [Google Scholar] [CrossRef] [PubMed]
- Masiero, M.; Mazzocco, K.; Harnois, C.; Cropley, M.; Pravettoni, G. From Individual To Social Trauma: Sources Of Everyday Trauma In Italy, The US And UK During The COVID-19 Pandemic. J. Trauma Dissociation 2020, 21, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Paslakis, G.; Scholz-Hehn, A.D.; Sommer, L.M.; Kühn, S. Implicit Bias to Food and Body Cues in Eating Disorders: A Systematic Review. Eat. Weight. Disord. 2021, 26, 1303–1321. [Google Scholar] [CrossRef] [PubMed]
- Turgon, R.; Ruffault, A.; Juneau, C.; Blatier, C.; Shankland, R. Eating Disorder Treatment: A Systematic Review and Meta-Analysis of the Efficacy of Mindfulness-Based Programs. Mindfulness 2019, 10, 2225–2244. [Google Scholar] [CrossRef]

| AN n = 42 | BN n = 40 | BED n = 40 | HW n = 50 | F | p ηp2 | Post Hoc | |
|---|---|---|---|---|---|---|---|
| Age, years | 24.62 (8.26) | 23.60 (6.86) | 30.28 (9.67) | 24.16 (3.41) | 7.454 | <0.001 0.117 | AN < BED (p = 0.003) BN < BED (p < 0.001) HW < BED (p = 0.001) |
| BMI, kg/m2 | 16.68 (0.87) | 20.05 (2.06) | 33.13 (10.05) | 21.45 (2.96) | 75.419 | <0.001 0.574 | AN < BN (p = 0.007) AN < BED (p < 0.001) AN < HW (p < 0.001) BN < BED (p < 0.001) HW < BED (p < 0.001) |
| Menarche, years | 12.71 (1.29) | 11.98 (1.19) | 11.79 (1.27) | 12.38 (1.58) | 3.887 | 0.010 0.065 | BED < AN (p = 0.014) |
| Education, years | 13.98 (2.79) | 15.21 (2.95) | 14.83 (3.09) | 16.06 (2.74) | 4.106 | 0.008 0.069 | AN < HW (p = 0.004) |
| Illness duration, months | 5.83 (5.99) | 5.76 (6.72) | 12.14 (9.53) | - | 22.638 | <0.001 0.307 | AN < BED (p < 0.001) BN < BED (p < 0.001) |
| PHQ-9 | 10.02 (4.57) | 12.70 (5.75) | 10.65 (4.29) | 6.14 (3.94) | 15.975 | <0.001 0.222 | HW < AN (p = 0.001) HW < BN (p < 0.001) HW < BED (p < 0.001) |
| EDE-Q Global | 13.65 (8.23) | 20.21 (8.59) | 20.01 (5.36) | 7.36 (6.44) | 32.269 | <0.001 0.366 | HW < AN (p < 0.001) AN < BN (p < 0.001) AN < BED (p = 0.001) HW < BN (p < 0.001) HW < BED (p < 0.001) |
| Exclusion Condition | |||||||
| AN n = 22 | BN n = 19 | BED n = 20 | HW n = 25 | F | p ηp2 | Post Hoc | |
| % passes | 16.70 (8.30) | 15.30 (8.30) | 17.10 (8.90) | 21.20 (7.80) | 2.181 | 0.096 0.074 | |
| Belonging | 9.95 (3.61) | 12.53 (4.51) | 13.30 (2.03) | 12.48 (3.11) | 3.934 | 0.011 0.126 | AN < BED (p = 0.012) |
| Self-esteem | 10.50 (3.79) | 11.95 (5.17) | 14.20 (2.14) | 14.00 (3.33) | 4.922 | 0.003 0.153 | AN < BED (p = 0.011) AN < HW (p = 0.011) |
| Meaningful existence | 10.00 (4.27) | 13.42 (4.68) | 13.00 (2.43) | 14.32 (3.20) | 5.728 | 0.001 0.173 | AN < BN (p = 0.026) AN < HW (p = 0.001) |
| Control | 7.68 (1.81) | 8.84 (3.53) | 8.85 (2.39) | 9.52 (2.43) | 2.024 | 0.117 0.069 | |
| Manipulation check | 7.41 (2.13) | 6.37 (2.29) | 6.90 (2.38) | 6.52 (2.31) | 0.890 | 0.450 0.032 | |
| Overinclusion Condition | |||||||
| AN n = 20 | BN n = 21 | BED n = 20 | HW n = 25 | F | p ηp2 | Post Hoc | |
| % passes | 67.50 (15.80) | 53.90 (13.50) | 72.00 (5.20) | 55.80 (12.20) | 10.828 | <0.001 0.284 | BN < AN (p = 0.004) HW < AN (p = 0.013) BN < BED (p < 0.001) HW< BED (p < 0.001) |
| Belonging | 20.25 (3.31) | 17.81 (3.12) | 21.95 (2.74) | 21.16 (3.05) | 7.221 | <0.001 0.209 | BN < BED (p < 0.001) BN < HW (p = 0.002) |
| Self-esteem | 16.70 (4.85) | 12.71 (3.86) | 19.05 (2.52) | 17.60 (3.49) | 10.909 | <0.001 0.285 | BN < AN (p = 0.006) BN < BED (p < 0.001) BN < HW (p < 0.001) |
| Meaningful existence | 18.80 (4.25) | 17.05 (2.04) | 20.90 (2.10) | 20.32 (2.75) | 7.462 | <0.001 0.214 | BN < BED (p < 0.001) BN < HW (p = 0.002) |
| Control | 15.95 (5.96) | 13.05 (3.37) | 13.45 (4.12) | 16.32 (3.08) | 3.483 | 0.019 0.113 | BN < HW (p = 0.050) |
| Manipulation check | 2.60 (1.31) | 2.29 (0.72) | 2.00 (0.00) | 2.12 (0.60) | 2.191 | 0.095 0.074 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meneguzzo, P.; Meregalli, V.; Collantoni, E.; Cardi, V.; Tenconi, E.; Favaro, A. Virtual Rejection and Overinclusion in Eating Disorders: An Experimental Investigation of the Impact on Emotions, Stress Perception, and Food Attitudes. Nutrients 2023, 15, 1021. https://doi.org/10.3390/nu15041021
Meneguzzo P, Meregalli V, Collantoni E, Cardi V, Tenconi E, Favaro A. Virtual Rejection and Overinclusion in Eating Disorders: An Experimental Investigation of the Impact on Emotions, Stress Perception, and Food Attitudes. Nutrients. 2023; 15(4):1021. https://doi.org/10.3390/nu15041021
Chicago/Turabian StyleMeneguzzo, Paolo, Valentina Meregalli, Enrico Collantoni, Valentina Cardi, Elena Tenconi, and Angela Favaro. 2023. "Virtual Rejection and Overinclusion in Eating Disorders: An Experimental Investigation of the Impact on Emotions, Stress Perception, and Food Attitudes" Nutrients 15, no. 4: 1021. https://doi.org/10.3390/nu15041021
APA StyleMeneguzzo, P., Meregalli, V., Collantoni, E., Cardi, V., Tenconi, E., & Favaro, A. (2023). Virtual Rejection and Overinclusion in Eating Disorders: An Experimental Investigation of the Impact on Emotions, Stress Perception, and Food Attitudes. Nutrients, 15(4), 1021. https://doi.org/10.3390/nu15041021