The ENDORSE Feasibility Study: Exploring the Use of M-Health, Artificial Intelligence and Serious Games for the Management of Childhood Obesity
Abstract
1. Introduction
2. Materials and Methods
2.1. The ENDORSE Platform as a Means for the Management of Childhood Obesity
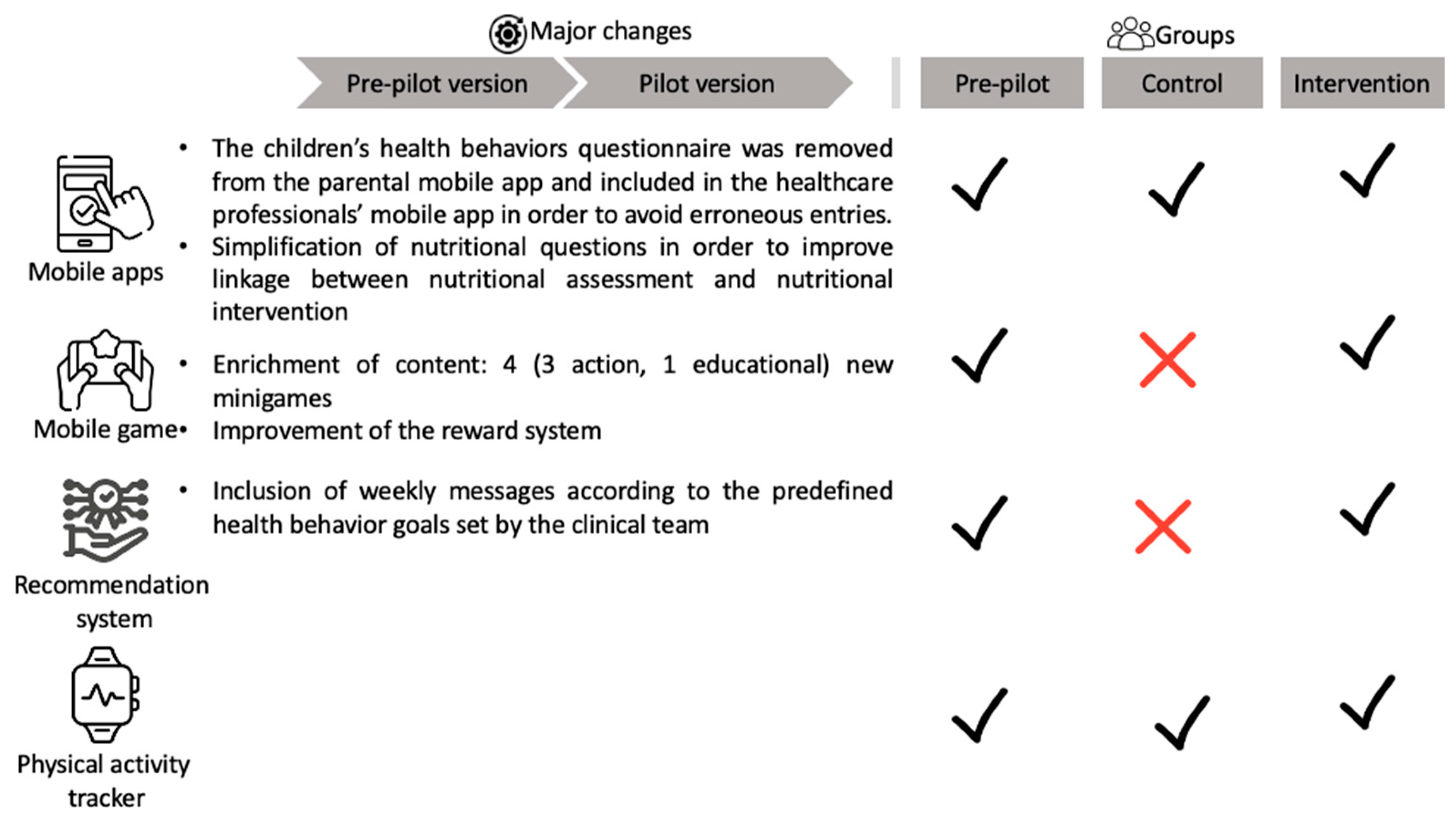
2.2. Study Design
2.3. Measures
2.3.1. Medical Assessment
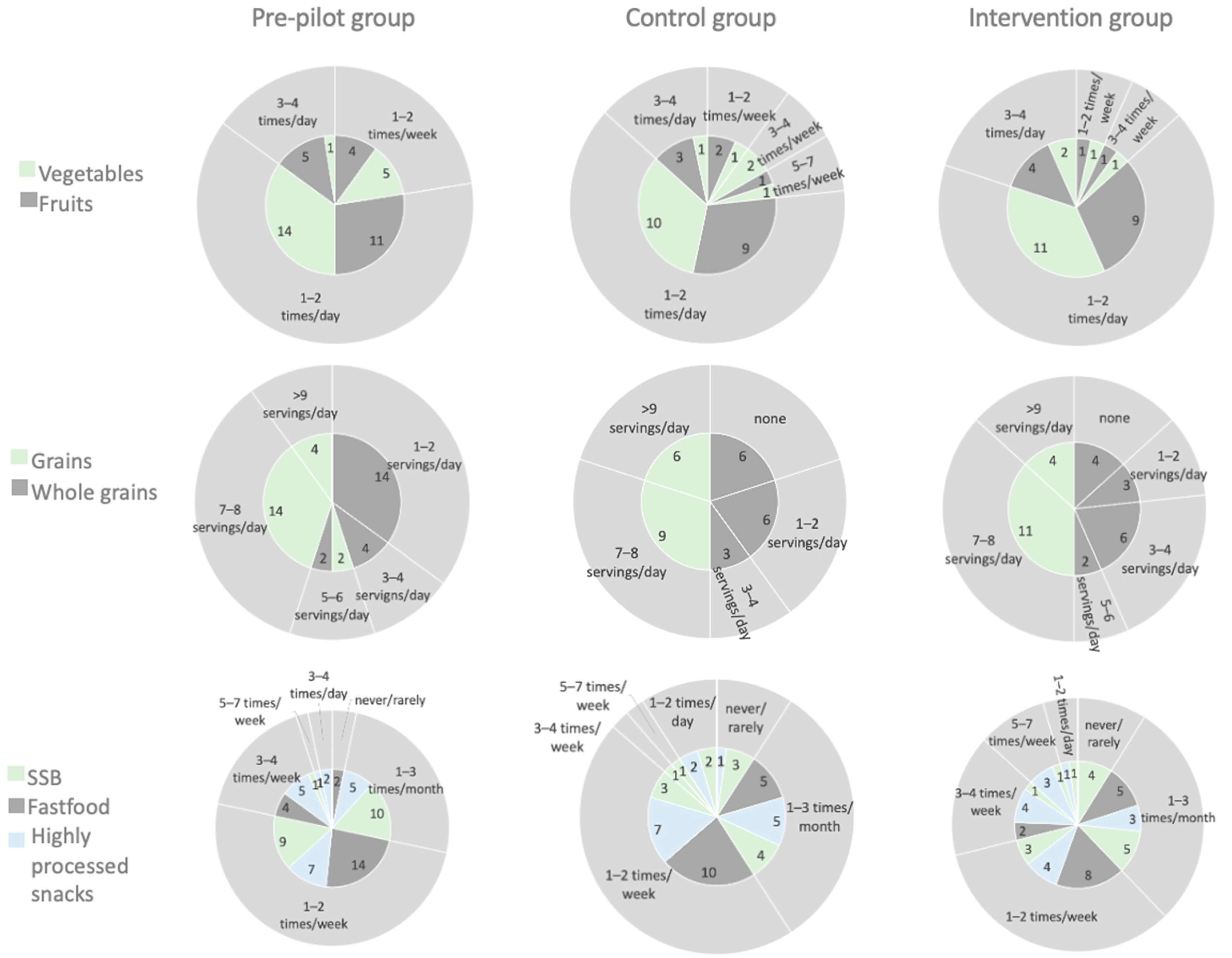
2.3.2. Nutritional Assessment and Dietary Intervention
2.3.3. Children’s Health Behaviors Questionnaire
2.3.4. Psychological Assessment
2.4. Study Implementation
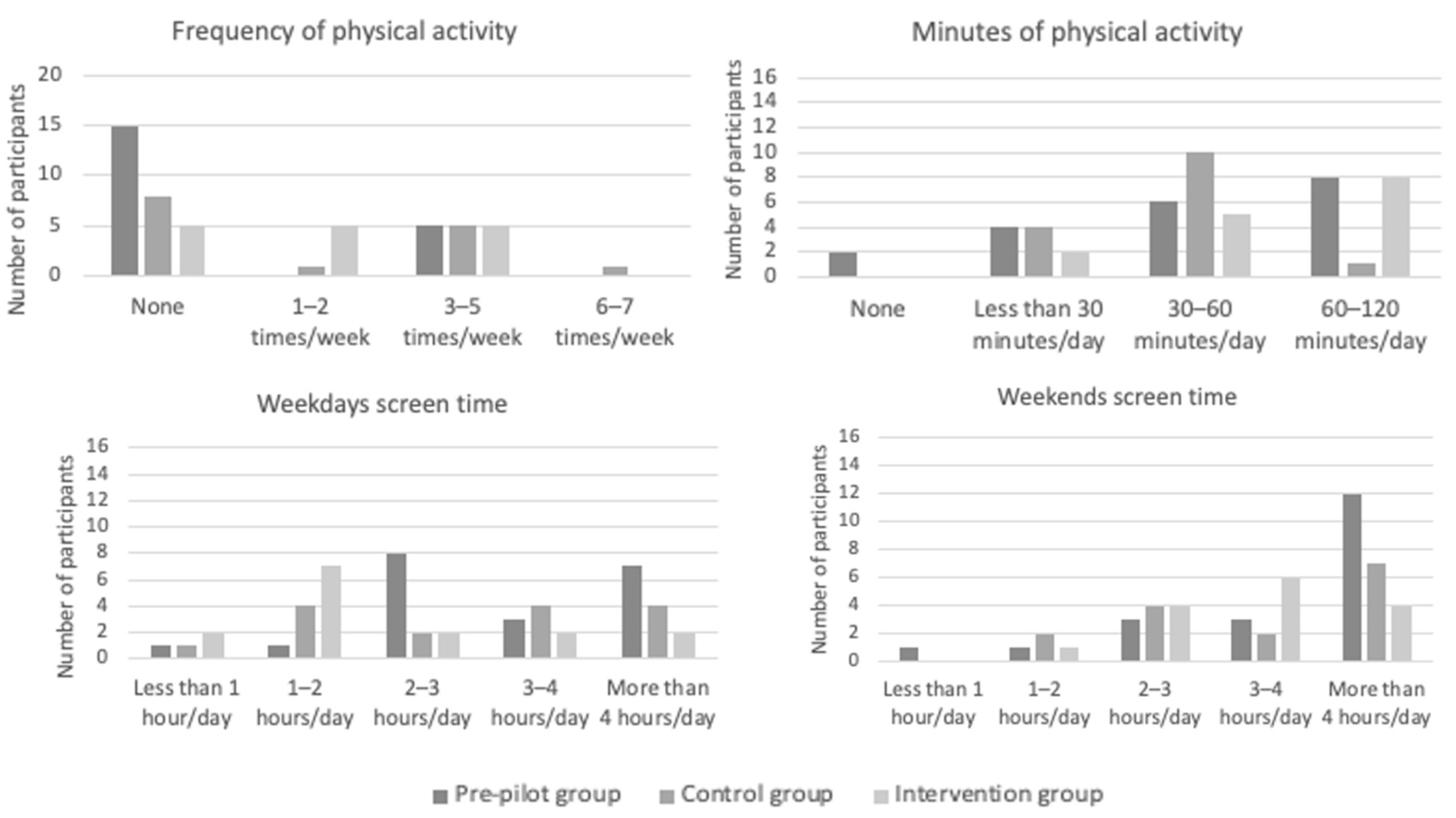
2.4.1. Self-Monitoring of Behavior and Outcome
2.4.2. Educational Material
2.5. Data Analysis
2.5.1. Descriptive Statistics and Pre-Post Intervention
2.5.2. Feasibility and Acceptability
3. Results
3.1. Baseline Characteristics
3.2. Adherence Results
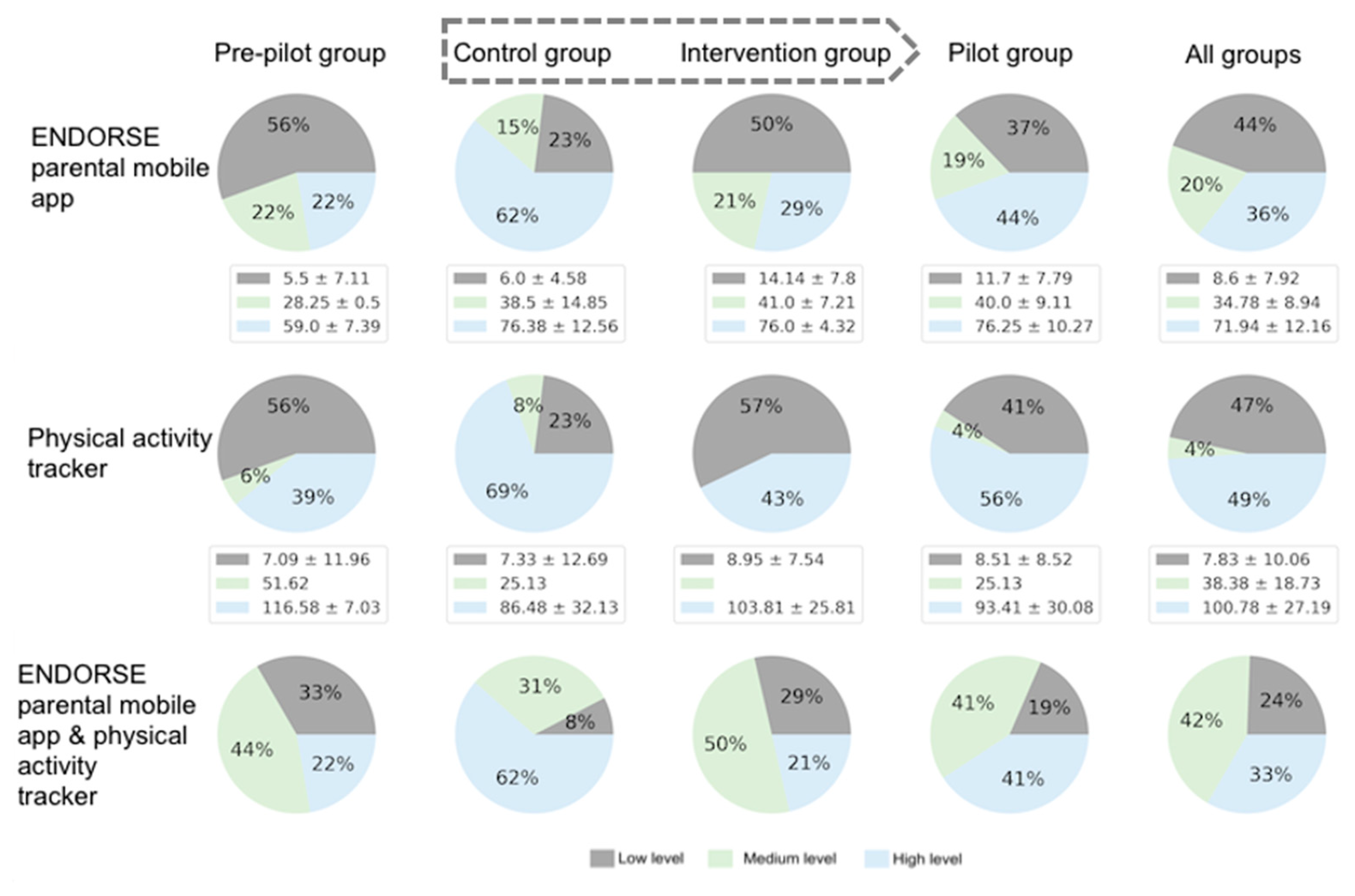
3.2.1. Usage Metrics
3.2.2. Level and Score of Adherence
3.2.3. Acceptability
3.3. Changes in Anthropometrics and Health Behaviors
3.3.1. Pre-Pilot Study
3.3.2. Pilot Study
3.3.3. Overall Changes
4. Discussion
4.1. Main Findings
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Styne, D.M.; Arslanian, S.A.; Connor, E.L.; Farooqi, I.S.; Murad, M.H.; Silverstein, J.H.; Yanovski, J.A. Pediatric Obesity—Assessment, Treatment, and Prevention: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2017, 102, 709–757. [Google Scholar] [CrossRef] [PubMed]
- Umer, A.; Kelley, G.A.; Cottrell, L.E.; Giacobbi, P.; Innes, K.E.; Lilly, C.L. Childhood obesity and adult cardiovascular disease risk factors: A systematic review with meta-analysis. BMC Public Health 2017, 17, 683. [Google Scholar] [CrossRef] [PubMed]
- Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 29 November 2022).
- Alotaibi, M.; Alnajjar, F.; Cappuccio, M.; Khalid, S.; Alhmiedat, T.; Mubin, O. Efficacy of Emerging Technologies to Manage Childhood Obesity. DMSO 2022, 15, 1227–1244. [Google Scholar] [CrossRef] [PubMed]
- Grossman, D.C.; Bibbins-Domingo, K.; Curry, S.J.; Barry, M.J.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W.; Kemper, A.R.; Krist, A.H.; US Preventive Services Task Force; et al. Screening for Obesity in Children and Adolescents: US Preventive Services Task Force Recommendation Statement. JAMA 2017, 317, 2417. [Google Scholar] [CrossRef]
- Clinical Practice Guideline for the Treatment of Obesity and Overweight in Children and Adolescents. Available online: https://www.apa.org/obesity-guideline (accessed on 13 December 2022).
- Fowler, L.A.; Grammer, A.C.; Staiano, A.E.; Fitzsimmons-Craft, E.E.; Chen, L.; Yaeger, L.H.; Wilfley, D.E. Harnessing technological solutions for childhood obesity prevention and treatment: A systematic review and meta-analysis of current applications. Int. J. Obes. 2021, 45, 957–981. [Google Scholar] [CrossRef]
- Hammersley, M.L.; Jones, R.A.; Okely, A.D. Parent-Focused Childhood and Adolescent Overweight and Obesity eHealth Interventions: A Systematic Review and Meta-Analysis. J. Med. Internet Res. 2016, 18, e203. [Google Scholar] [CrossRef]
- Park, J.; Park, M.-J.; Seo, Y.-G. Effectiveness of Information and Communication Technology on Obesity in Childhood and Adolescence: Systematic Review and Meta-analysis. J. Med. Internet Res. 2021, 23, e29003. [Google Scholar] [CrossRef]
- Patel, M.L.; Wakayama, L.N.; Bennett, G.G. Self-Monitoring via Digital Health in Weight Loss Interventions: A Systematic Review Among Adults with Overweight or Obesity. Obesity 2021, 29, 478–499. [Google Scholar] [CrossRef]
- Chai, L.K.; Farletti, R.; Fathi, L.; Littlewood, R. A Rapid Review of the Impact of Family-Based Digital Interventions for Obesity Prevention and Treatment on Obesity-Related Outcomes in Primary School-Aged Children. Nutrients 2022, 14, 4837. [Google Scholar] [CrossRef]
- Calcaterra, V.; Verduci, E.; Vandoni, M.; Rossi, V.; Di Profio, E.; Carnevale Pellino, V.; Tranfaglia, V.; Pascuzzi, M.C.; Borsani, B.; Bosetti, A.; et al. Telehealth: A Useful Tool for the Management of Nutrition and Exercise Programs in Pediatric Obesity in the COVID-19 Era. Nutrients 2021, 13, 3689. [Google Scholar] [CrossRef]
- Tully, L.; Burls, A.; Sorensen, J.; El-Moslemany, R.; O’Malley, G. Mobile Health for Pediatric Weight Management: Systematic Scoping Review. JMIR Mhealth Uhealth 2020, 8, e16214. [Google Scholar] [CrossRef] [PubMed]
- Kouvari, M.; Karipidou, M.; Tsiampalis, T.; Mamalaki, E.; Poulimeneas, D.; Bathrellou, E.; Panagiotakos, D.; Yannakoulia, M. Digital Health Interventions for Weight Management in Children and Adolescents: Systematic Review and Meta-analysis. J. Med. Internet Res. 2022, 24, e30675. [Google Scholar] [CrossRef]
- Comparative Assessment of Statistical and Machine Learning Techniques towards Estimating the Risk of Developing Type 2 Diabetes and Cardiovascular Complications—Dalakleidi—2017—Expert Systems—Wiley Online Library. Available online: https://onlinelibrary.wiley.com/doi/full/10.1111/exsy.12214 (accessed on 8 February 2023).
- Zarkogianni, K.; Athanasiou, M.; Thanopoulou, A.C. Comparison of Machine Learning Approaches Toward Assessing the Risk of Developing Cardiovascular Disease as a Long-Term Diabetes Complication. IEEE J. Biomed. Health Inform. 2018, 22, 1637–1647. [Google Scholar] [CrossRef]
- Fico, G.; Hernanzez, L.; Cancela, J.; Dagliati, A.; Sacchi, L.; Martinez-Millana, A.; Posada, J.; Manero, L.; Verdú, J.; Facchinetti, A.; et al. What do healthcare professionals need to turn risk models for type 2 diabetes into usable computerized clinical decision support systems? Lessons learned from the MOSAIC project. BMC Med. Inform. Decis. Mak. 2019, 19, 163. [Google Scholar] [CrossRef]
- Triantafyllidis, A.; Polychronidou, E.; Alexiadis, A.; Rocha, C.L.; Oliveira, D.N.; da Silva, A.S.; Freire, A.L.; Macedo, C.; Sousa, I.F.; Werbet, E.; et al. Computerized decision support and machine learning applications for the prevention and treatment of childhood obesity: A systematic review of the literature. Artif. Intell. Med. 2020, 104, 101844. [Google Scholar] [CrossRef]
- Ryan, R.M.; Deci, E.L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 2000, 55, 68–78. [Google Scholar] [CrossRef]
- Kalafatis, E.; Mitsis, K.; Zarkogianni, K.; Athanasiou, M.; Voutetakis, A.; Nicolaides, N.; Chatzidaki, E.; Polychronaki, N.; Chioti, V.; Pervanidou, P.; et al. Artificial Intelligence based procedural content generation in serious games for health: The case of childhood obesity. EAI MobiHealth 2022, in press. [Google Scholar]
- Ntoumanis, N.; Ng, J.Y.Y.; Prestwich, A.; Quested, E.; Hancox, J.E.; Thøgersen-Ntoumani, C.; Deci, E.L.; Ryan, R.M.; Lonsdale, C.; Williams, G.C. A meta-analysis of self-determination theory-informed intervention studies in the health domain: Effects on motivation, health behavior, physical, and psychological health. Health Psychol. Rev. 2021, 15, 214–244. [Google Scholar] [CrossRef] [PubMed]
- Kohn, J.S. Michael Sample Size for Before-After Study (Paired T-Test)|Sample Size Calculators. Available online: https://sample-size.net/sample-size-study-paired-t-test/ (accessed on 9 March 2023).
- Cole, T.J.; Lobstein, T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr. Obes. 2012, 7, 284–294. [Google Scholar] [CrossRef]
- Tanner, J.M.; Whitehouse, R.H. Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch. Dis. Child. 1976, 51, 170–179. [Google Scholar] [CrossRef]
- Ogden, C.L.; Kuczmarski, R.J.; Flegal, K.M.; Mei, Z.; Guo, S.; Wei, R.; Grummer-Strawn, L.M.; Curtin, L.R.; Roche, A.F.; Johnson, C.L. Centers for Disease Control and Prevention 2000 Growth Charts for the United States: Improvements to the 1977 National Center for Health Statistics Version. Pediatrics 2002, 109, 45–60. [Google Scholar] [CrossRef] [PubMed]
- Freedman, D.S.; Berenson, G.S. Tracking of BMI z Scores for Severe Obesity. Pediatrics 2017, 140, e20171072. [Google Scholar] [CrossRef]
- Browning, L.M.; Hsieh, S.D.; Ashwell, M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0·5 could be a suitable global boundary value. Nutr. Res. Rev. 2010, 23, 247–269. [Google Scholar] [CrossRef] [PubMed]
- Kastorini, C.-M.; Critselis, E.; Zota, D.; Coritsidis, A.L.; Nagarajan, M.K.; Papadimitriou, E.; Belogianni, K.; Benetou, V.; Linos, A.; on behalf of the Greek National Dietary Guidelines Scientific Team. National Dietary Guidelines of Greece for children and adolescents: A tool for promoting healthy eating habits. Public Health Nutr. 2019, 22, 2688–2699. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine (U.S.) (Ed.) Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids; National Academies Press: Washington, DC, USA, 2005; ISBN 978-0-309-08525-0. [Google Scholar]
- Barlow, S.E.; Expert Committee. Expert Committee Recommendations Regarding the Prevention, Assessment, and Treatment of Child and Adolescent Overweight and Obesity: Summary Report. Pediatrics 2007, 120, S164–S192. [Google Scholar] [CrossRef]
- Di Pasquale, R.; Rivolta, A. A Conceptual Analysis of Food Parenting Practices in the Light of Self-Determination Theory: Relatedness-Enhancing, Competence-Enhancing and Autonomy-Enhancing Food Parenting Practices. Front. Psychol. 2018, 9, 2373. [Google Scholar] [CrossRef]
- Rollins, B.Y.; Savage, J.S.; Fisher, J.O.; Birch, L.L. Alternatives to restrictive feeding practices to promote self-regulation in childhood: A developmental perspective: Alternatives to restrictive feeding. Pediatr. Obes. 2016, 11, 326–332. [Google Scholar] [CrossRef]
- Hall, K.D.; Ayuketah, A.; Brychta, R.; Cai, H.; Cassimatis, T.; Chen, K.Y.; Chung, S.T.; Costa, E.; Courville, A.; Darcey, V.; et al. Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake. Cell Metab. 2019, 30, 67–77.e3. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Patient Health Questionnaire (PHQ) Screeners. Free Download. Available online: https://www.phqscreeners.com/select-screener/ (accessed on 3 December 2022).
- Garner, D.M.; Olmsted, M.P.; Bohr, Y.; Garfinkel, P.E. The Eating Attitudes Test: Psychometric features and clinical correlates. Psychol. Med. 1982, 12, 871–878. [Google Scholar] [CrossRef]
- Simos, G. Investigation of Psychogenic Eating Disorders and Prevention Possibilities; Aristotle University of Thessaloniki: Thessaloniki, Greece, 1996. [Google Scholar]
- Musher-Eizenman, D.; Holub, S. Comprehensive Feeding Practices Questionnaire: Validation of a New Measure of Parental Feeding Practices. J. Pediatr. Psychol. 2007, 32, 960–972. [Google Scholar] [CrossRef] [PubMed]
- Michou, M.; Panagiotakos, D.B.; Mamalaki, E.; Yannakoulia, M.; Costarelli, V. Development and validation of the Greek version of the comprehensive parental feeding questionnaire. Mediterr. J. Nutr. Metab. 2019, 12, 211–221. [Google Scholar] [CrossRef]
- Goodman, R. The Strengths and Difficulties Questionnaire: A research note. J. Child Psychol. Psychiatry 1997, 38, 581–586. [Google Scholar] [CrossRef]
- Bibou-Nakou, I.; Kiosseoglou, G.; Stogiannidou, A. Strengths and difficulties of school-aged children in the family and school context. Psychol. J. Hell. Psychol. Soc. 2001, 8, 506–525. [Google Scholar]
- Gibson, L.Y.; Allen, K.L.; Davis, E.; Blair, E.; Zubrick, S.R.; Byrne, S.M. The psychosocial burden of childhood overweight and obesity: Evidence for persisting difficulties in boys and girls. Eur. J. Pediatr. 2017, 176, 925–933. [Google Scholar] [CrossRef]
- Quek, Y.-H.; Tam, W.W.S.; Zhang, M.W.B.; Ho, R.C.M. Exploring the association between childhood and adolescent obesity and depression: A meta-analysis: Depression and obesity in childhood and adolescence. Obes. Rev. 2017, 18, 742–754. [Google Scholar] [CrossRef]
- Rankin, J.; Matthews, L.; Cobley, S.; Han, A.; Sanders, R.; Wiltshire, H.D.; Baker, J.S. Psychological consequences of childhood obesity: Psychiatric comorbidity and prevention. AHMT 2016, 7, 125–146. [Google Scholar] [CrossRef]
- Eichen, D.M.; Strong, D.R.; Rhee, K.E.; Rock, C.L.; Crow, S.J.; Epstein, L.H.; Wilfley, D.E.; Boutelle, K.N. Change in eating disorder symptoms following pediatric obesity treatment. Int. J. Eat. Disord. 2019, 52, 299–303. [Google Scholar] [CrossRef]
- Hayes, J.F.; Fitzsimmons-Craft, E.E.; Karam, A.M.; Jakubiak, J.; Brown, M.L.; Wilfley, D.E. Disordered Eating Attitudes and Behaviors in Youth with Overweight and Obesity: Implications for Treatment. Curr. Obes. Rep. 2018, 7, 235–246. [Google Scholar] [CrossRef]
- Spear, B.A.; Barlow, S.E.; Ervin, C.; Ludwig, D.S.; Saelens, B.E.; Schetzina, K.E.; Taveras, E.M. Recommendations for Treatment of Child and Adolescent Overweight and Obesity. Pediatrics 2007, 120, S254–S288. [Google Scholar] [CrossRef]
- Adams, M.A.; Johnson, W.D.; Tudor-Locke, C. Steps/day translation of the moderate-to-vigorous physical activity guideline for children and adolescents. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 49. [Google Scholar] [CrossRef] [PubMed]
- Llewellyn, C.H.; Fildes, A. Behavioural Susceptibility Theory: Professor Jane Wardle and the Role of Appetite in Genetic Risk of Obesity. Curr. Obes. Rep. 2017, 6, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Davis, F.D. Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Q. 1989, 13, 319. [Google Scholar] [CrossRef]
- Wang, W.; Cheng, J.; Song, W.; Shen, Y. The Effectiveness of Wearable Devices as Physical Activity Interventions for Preventing and Treating Obesity in Children and Adolescents: Systematic Review and Meta-analysis. JMIR Mhealth Uhealth 2022, 10, e32435. [Google Scholar] [CrossRef] [PubMed]
- Taveras, E.M.; Marshall, R.; Kleinman, K.P.; Gillman, M.W.; Hacker, K.; Horan, C.M.; Smith, R.L.; Price, S.; Sharifi, M.; Rifas-Shiman, S.L.; et al. Comparative Effectiveness of Childhood Obesity Interventions in Pediatric Primary Care: A Cluster-Randomized Clinical Trial. JAMA Pediatr. 2015, 169, 535. [Google Scholar] [CrossRef] [PubMed]
- Mitsis, K.; Zarkogianni, K.; Kalafatis, E.; Dalakleidi, K.; Jaafar, A.; Mourkousis, G.; Nikita, K.S. A Multimodal Approach for Real Time Recognition of Engagement towards Adaptive Serious Games for Health. Sensors 2022, 22, 2472. [Google Scholar] [CrossRef]
- Baranowski, T.; Ryan, C.; Hoyos-Cespedes, A.; Lu, A.S. Nutrition Education and Dietary Behavior Change Games: A Scoping Review. Games Health J. 2019, 8, 153–176. [Google Scholar] [CrossRef]
- Baranowski, T.; Baranowski, J.; Chen, T.-A.; Buday, R.; Beltran, A.; Dadabhoy, H.; Ryan, C.; Lu, A.S. Videogames That Encourage Healthy Behavior Did Not Alter Fasting Insulin or Other Diabetes Risks in Children: Randomized Clinical Trial. Games Health J. 2019, 8, 257–264. [Google Scholar] [CrossRef]
- Darling, K.E.; Sato, A.F. Systematic Review and Meta-Analysis Examining the Effectiveness of Mobile Health Technologies in Using Self-Monitoring for Pediatric Weight Management. Child. Obes. 2017, 13, 347–355. [Google Scholar] [CrossRef]
- Perdew, M.; Liu, S.; Rhodes, R.; Ball, G.D.C.; Mâsse, L.C.; Hartrick, T.; Strange, K.; Naylor, P.-J. The Effectiveness of a Blended In-Person and Online Family-Based Childhood Obesity Management Program. Child. Obes. 2021, 17, 58–67. [Google Scholar] [CrossRef]
- Trost, S.G.; Sundal, D.; Foster, G.D.; Lent, M.R.; Vojta, D. Effects of a Pediatric Weight Management Program With and Without Active Video Games: A Randomized Trial. JAMA Pediatr. 2014, 168, 407. [Google Scholar] [CrossRef] [PubMed]
- Chai, L.K.; Collins, C.E.; May, C.; Ashman, A.; Holder, C.; Brown, L.J.; Burrows, T.L. Feasibility and efficacy of a web-based family telehealth nutrition intervention to improve child weight status and dietary intake: A pilot randomised controlled trial. J. Telemed. Telecare 2021, 27, 146–158. [Google Scholar] [CrossRef]
- Maddison, R.; Marsh, S.; Foley, L.; Epstein, L.H.; Olds, T.; Dewes, O.; Heke, I.; Carter, K.; Jiang, Y.; Mhurchu, C.N. Screen-Time Weight-loss Intervention Targeting Children at Home (SWITCH): A randomized controlled trial. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 111. [Google Scholar] [CrossRef] [PubMed]
- Duncanson, K.; Shrewsbury, V.; Burrows, T.; Chai, L.K.; Ashton, L.; Taylor, R.; Gow, M.; Ho, M.; Ells, L.; Stewart, L.; et al. Impact of weight management nutrition interventions on dietary outcomes in children and adolescents with overweight or obesity: A systematic review with meta-analysis. J. Hum. Nutr. Diet. 2021, 34, 147–177. [Google Scholar] [CrossRef] [PubMed]

| Health Behavior Goal | Brief Description of Goals |
|---|---|
| Physical activity | Children were advised to engage in medium to high intensity physical activities at least 60 min per day (or to approach the 10,000 steps/day goal) [1,48]. |
| Screen time | Mothers and children were advised to limit screen time for recreational reasons to less than 1–2 h daily) [1]. |
| Breakfast | Children were advised to make daily healthy breakfast choices according to their personalized dietary plan. Mothers were advised not to pressure children who did not want to consume breakfast, but to provide these children with a healthy, nutrient- and energy-dense mid-morning snack. |
| Mid-morning snack | Children were advised to make healthy snack choices and mothers were encouraged to give children homemade snacks to take with them to school according to their personalized dietary plan. |
| Lunch | Mothers were advised to provide homemade mediterranean-based meals to their children according to their personalized dietary plan and children were advised to eat until full. |
| Afternoon snack | Mothers were advised to limit access to energy-dense, nutrient-poor packaged snacks, set clear rules about snacking, but at the same time take into consideration the child’s likes and dislikes and offer them choices according to their personalized dietary plans. Children were advised to avoid excessive snacking. |
| Dinner | Mothers were advised to prepare healthy, homemade meals for dinner according to the child’s personalized dietary plan. Children were advised to participate as often as possible in the preparation of homemade easy-to-prepare meals and to avoid systematic consumption of fast foods. |
| Characteristics | Pre-Pilot Study (n = 20) | Pilot Study Control Group (n = 15) | Pilot Study Intervention Group (n = 15) | * p Value (Between Pilot Groups) |
|---|---|---|---|---|
| Mean Follow-up Duration (Baseline to the last visit, months) | 5.19 (0.66) | 4.74 (1.41) | 4.04 (0.71) | 0.402 |
| Age (years) | 10.94 (1.85) | 11.11 (1.98) | 9.27 (1.73) | 0.012 |
| Sex (Female) | 8 (40.0) | 8 (53.3) | 10 (66.7) | 0.709 |
| Pubertal Stage (Prepubertal) | 8 (40.0) | 4 (26.7) | 9 (60.0) | 0.141 |
| Weight (kg) | 76.94 (22.48) | 72.19 (23.11) | 57.97 (18.11) | 0.074 |
| Height (m) | 1.51 (0.13) | 1.53 (0.14) | 1.42 (0.12) | 0.029 |
| BMI (kg/m2) | 33.02 (6.51) | 30.11 (5.77) | 28.02 (5.37) | 0.325 |
| BMI z-score | 2.85 (2.57, 4.38) | 2.71 (1.97, 3.23) | 2.89 (1.91, 4.18) | 0.806 |
| Weight Status | 0.597 | |||
| Overweight | - | 2 (13.3) | 2 (13.3) | |
| Simple Obesity | 11 (55.0) | 8 (53.3) | 6 (40.0) | |
| Severe Obesity | 9 (45.0) | 5 (33.3) | 7 (46.7) | |
| Waist-to-Height Ratio | 0.64 (0.08) | 0.64 (0.09) | 0.60 (0.07) | 0.250 |
| Systolic BP (mm Hg) | 111.40 (12.75) | 116.93 (5.48) | 113.33 (10.60) | 0.253 |
| Diastolic BP (mm Hg) | 73.25 (8.45) | 75.10 (8.20) | 73.40 (7.68) | 0.570 |
| Maternal Age (years) | 44.35 (5.08) | 44.80 (6.84) | 42.40 (3.81) | 0.245 |
| Maternal BMI (kg/m2) | 30.71 (6.35) | 29.45 (5.87) | 29.65 (6.11) | 0.838 |
| Greek Mothers | 19 (95.0) | 14 (93.3) | 15 (100.0) | 1.000 |
| Married Mothers | 13 (65.0) | 13 (86.7) | 13 (86.7) | 1.000 |
| Maternal Education | 0.335 | |||
| Primary | 3 (15.0) | 1 (6.7) | - | |
| Secondary | 12 (60.0) | 8 (53.3) | 7 (46.7) | |
| Tertiary | 5 (25.0) | 6 (40.0) | 8 (53.3) | |
| Tertiary | ||||
| Employed Mothers | 14 (70.0) | 12 (80) | 13 (86.7) | 1.000 |
| Metric | Pre-Pilot Group (n = 18) | Control Group (n = 13) | Intervention Group (n = 14) |
|---|---|---|---|
| Number of participants with zero usage | 3 (16.66%) | 0 (0.00%) | 0 (0.00%) |
| Days of usage | 19.13 ± 20.66 | 41.08 ± 36.12 | 27.64 ± 30.11 |
| Days of weight monitoring | 3.47 ± 3.36 | 7.31 ± 4.53 | 4.64 ± 3.67 |
| Days of monitoring of goals | 20.4 ± 20.42 | 41.54 ± 35.84 | 28.64 ± 29.8 |
| Number of communication messages with the clinical team | 1.4 ± 2.03 | 4.23 ± 5.64 | 0.79 ± 1.42 |
| Metric | Pre-Pilot Group (n = 18) | Control Group (n = 13) | Intervention Group (n = 14) |
|---|---|---|---|
| Number of participants with zero usage during sleep | 5 (27.77%) | 2 (14.28%) | 4 (30.76%) |
| Number of nights with sleep recordings | 29.31 ± 30.43 | 33.09 ± 28.52 | 23.00 ± 22.34 |
| Average time of sleep per day (min) | 465.02 ± 68.03 | 477.48 ± 49.22 | 482.62 ± 67.33 |
| Number of participants with zero usage during day | 4 (22.22%) | 2 (15.38%) | 3 (21.42%) |
| Average time of usage per day (h) | 13.64 ± 5.37 | 17.86 ± 3.45 | 14.25 ± 4.37 |
| Number of days with steps recordings | 55.64 ± 44.59 | 51.45 ± 30.73 | 46.64 ± 33.28 |
| Average steps per day | 7446.45 ± 3939.25 | 9090.63 ± 1197.41 | 7102.24 ± 2960.17 |
| Metric | Pre-Pilot Group n = 18 | Intervention Group n = 14 |
|---|---|---|
| Number of participants with zero usage | 4 (22.22%) | 0 (0.00%) |
| Days of usage | 3.86 ± 3.96 | 14.57 ± 8.93 |
| Number of action mini-games | 4.71 ± 6.65 | 16.43 ± 9.87 |
| Number of educational mini-games | 8.21 ± 7.35 | 9.79 ± 7.09 |
| Module | Pre-Pilot Group n = 15 | Intervention Group n = 14 | p-Value | |
|---|---|---|---|---|
| ENDORSE parental mobile app | Helpfulness | 3.60 ± 1.02 | 3.96 ± 0.82 | 0.039 |
| Usefulness | 4.01 ± 1.10 | 4.11 ± 0.85 | 0.470 | |
| Ease of Use | 3.98 ± 1.16 | 4.45 ± 0.80 | 0.015 | |
| Physical activity tracker | Helpfulness | 2.51 ± 1.25 | 3.73 ± 0.81 | 0.000 |
| Usefulness | 3.09 ± 1.26 | 3.87 ± 0.99 | 0.000 | |
| Ease of Use | 2.85 ± 1.37 | 3.99 ± 0.92 | 0.000 | |
| ENDORSE mobile game | Helpfulness | 4.13 ± 0.81 | 4.29 ± 0.96 | 0.658 |
| Usefulness | 4.13 ± 0.81 | 4.14 ± 0.91 | 0.977 | |
| Ease of Use | 4.20 ± 0.83 | 4.29 ± 0.70 | 0.775 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zarkogianni, K.; Chatzidaki, E.; Polychronaki, N.; Kalafatis, E.; Nicolaides, N.C.; Voutetakis, A.; Chioti, V.; Kitani, R.-A.; Mitsis, K.; Perakis, Κ.; et al. The ENDORSE Feasibility Study: Exploring the Use of M-Health, Artificial Intelligence and Serious Games for the Management of Childhood Obesity. Nutrients 2023, 15, 1451. https://doi.org/10.3390/nu15061451
Zarkogianni K, Chatzidaki E, Polychronaki N, Kalafatis E, Nicolaides NC, Voutetakis A, Chioti V, Kitani R-A, Mitsis K, Perakis Κ, et al. The ENDORSE Feasibility Study: Exploring the Use of M-Health, Artificial Intelligence and Serious Games for the Management of Childhood Obesity. Nutrients. 2023; 15(6):1451. https://doi.org/10.3390/nu15061451
Chicago/Turabian StyleZarkogianni, Konstantia, Evi Chatzidaki, Nektaria Polychronaki, Eleftherios Kalafatis, Nicolas C. Nicolaides, Antonis Voutetakis, Vassiliki Chioti, Rosa-Anna Kitani, Kostas Mitsis, Κonstantinos Perakis, and et al. 2023. "The ENDORSE Feasibility Study: Exploring the Use of M-Health, Artificial Intelligence and Serious Games for the Management of Childhood Obesity" Nutrients 15, no. 6: 1451. https://doi.org/10.3390/nu15061451
APA StyleZarkogianni, K., Chatzidaki, E., Polychronaki, N., Kalafatis, E., Nicolaides, N. C., Voutetakis, A., Chioti, V., Kitani, R.-A., Mitsis, K., Perakis, Κ., Athanasiou, M., Antonopoulou, D., Pervanidou, P., Kanaka-Gantenbein, C., & Nikita, K. (2023). The ENDORSE Feasibility Study: Exploring the Use of M-Health, Artificial Intelligence and Serious Games for the Management of Childhood Obesity. Nutrients, 15(6), 1451. https://doi.org/10.3390/nu15061451







