Impacts of a Multi-Professional Family versus Isolated Intervention on Food Level Processing in Overweight Adolescents: A Randomized Trial
Abstract
1. Introduction
2. Materials and Methods
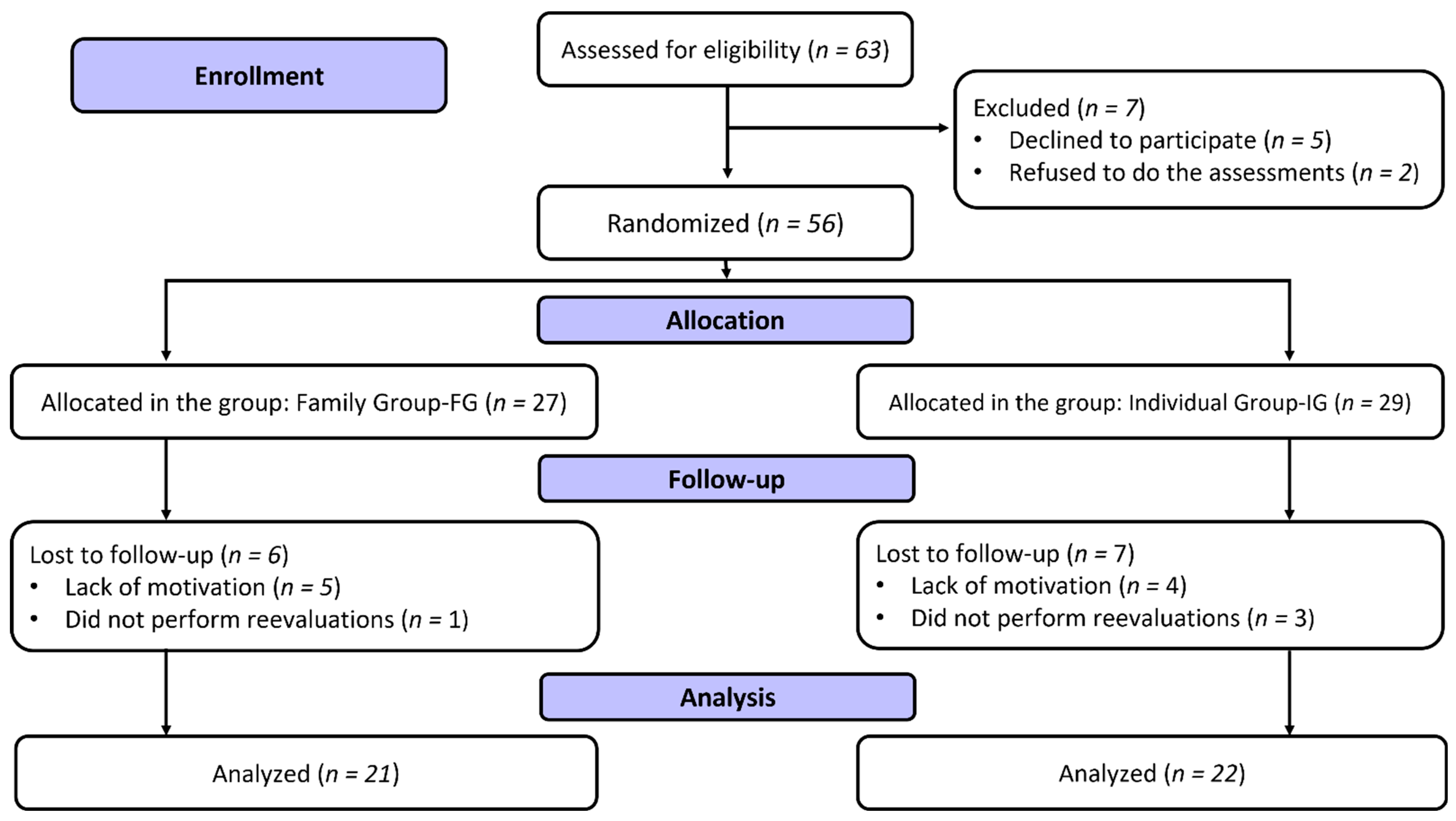
2.1. Study Design
2.2. Participants
2.3. Anthropometry
2.4. 24-Hour Food Record (24hR)
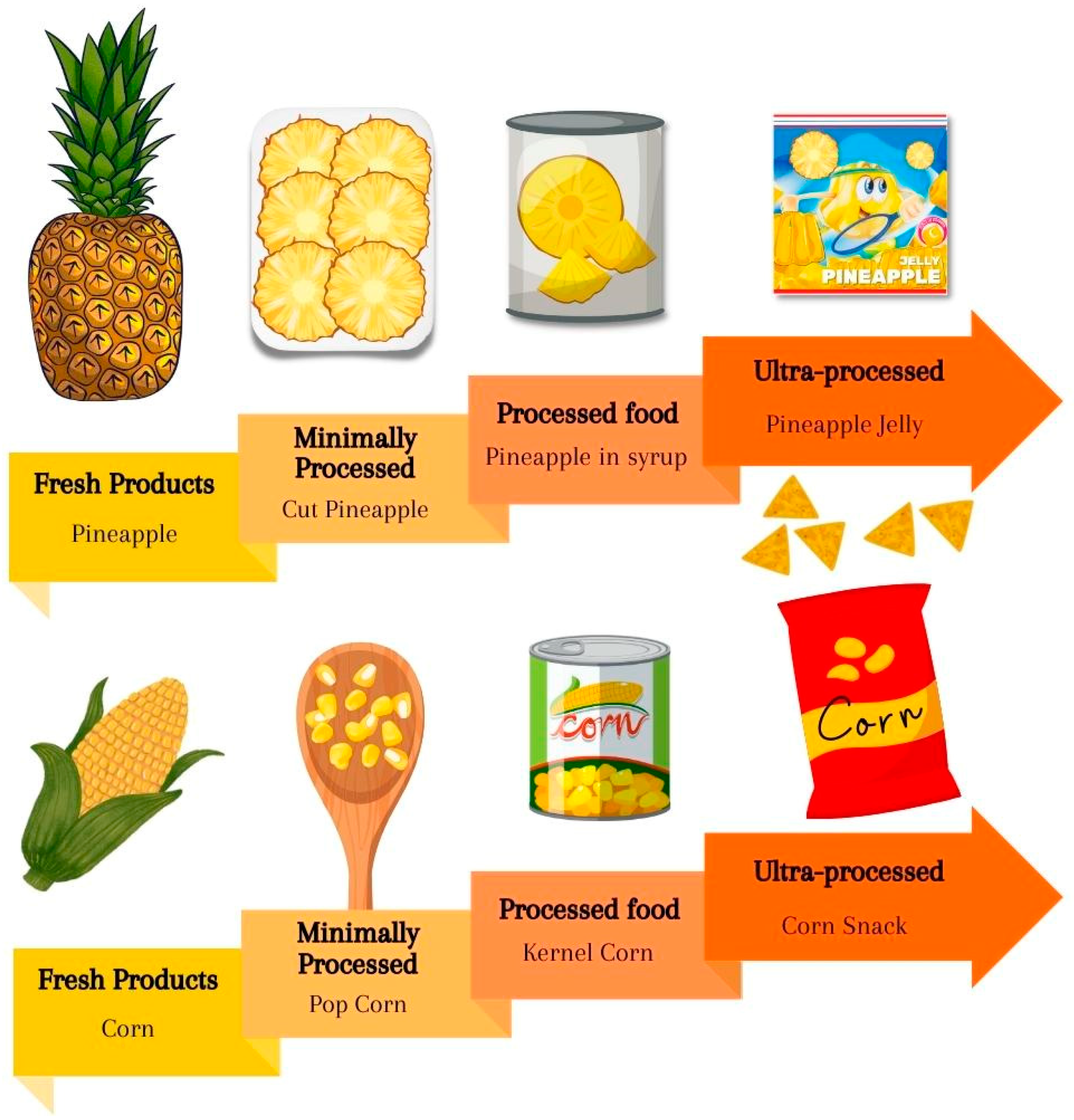
2.5. Food-Level Processing
2.6. Tanner Scale
2.7. Interventions
2.8. Data Analysis
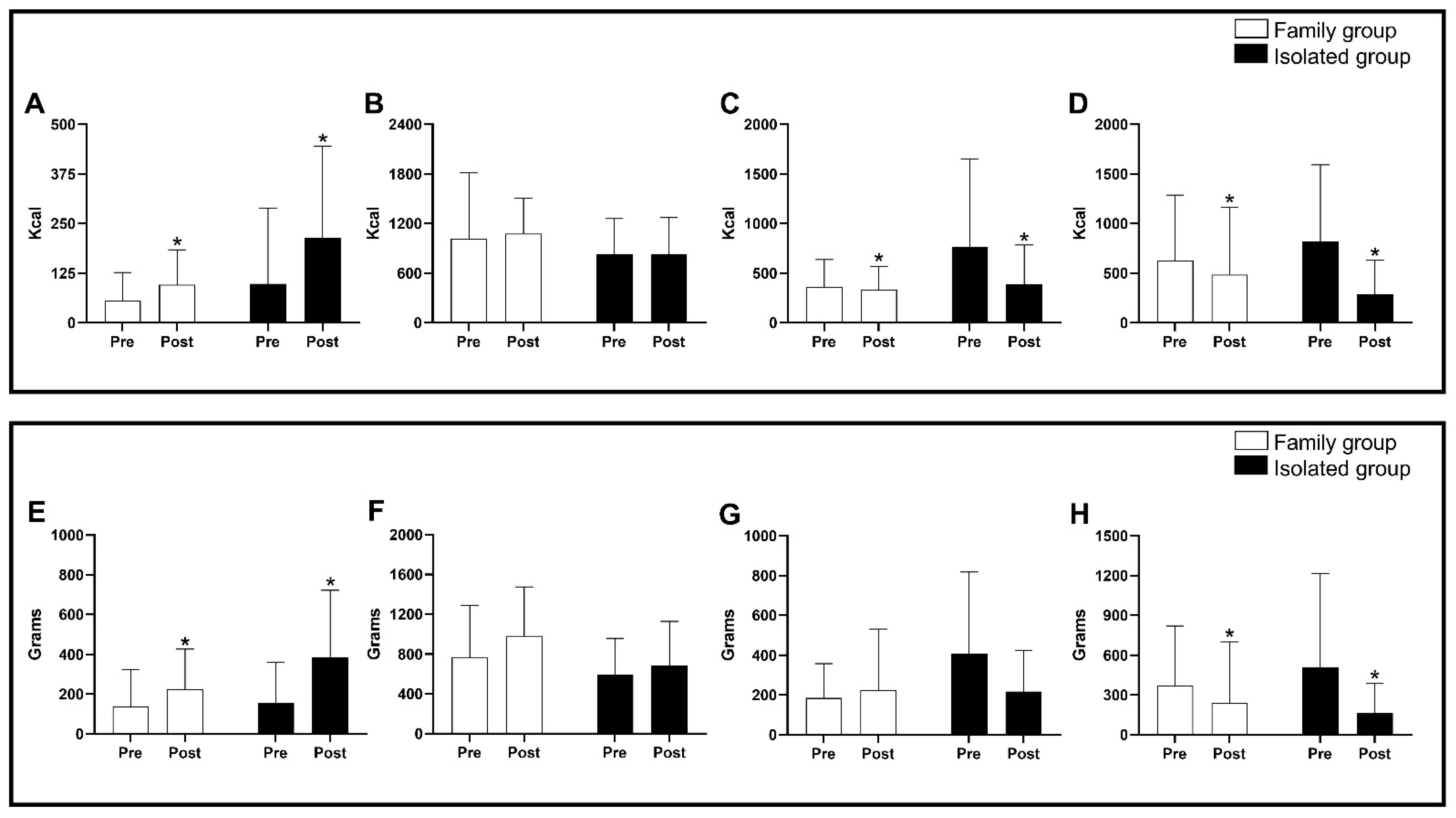
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Popkin, B.M. Global nutrition dynamics: The world is shifting rapidly toward a diet linked with non-communicable diseases. Am. J. Clin. Nutr. 2006, 84, 289–298. [Google Scholar] [CrossRef] [PubMed]
- Costa, L.; Rubio, K.L.; Munhoz, S.; Lopes, A.; De, A.T. Effects of 12 weeks of interdisciplinary interventions on behavioral and eating parameters of adolescents with overweight or obesity. J. Hum. Growth Dev. 2019, 29, 177–186. [Google Scholar] [CrossRef]
- Ruiter, E.L.M.; Molleman, G.R.M.; Fransen, G.A.J.; Wagenaar, M.; Velden, K.V.D.; Engels, R.C.M.E. A set of pedagogical recommendations for improving the integrated approach to childhood overweight and obesity: A Delphi study. PLoS ONE 2020, 15, e0231245. [Google Scholar] [CrossRef] [PubMed]
- Enes, C.C.; de Camargo, C.M.; Justino, M.I.C. Ultra-processed food consumption and obesity in adolescents. Rev. Nutr. 2019, 32, 1–11. [Google Scholar] [CrossRef]
- Ministério da Saúde. Guia Alimentar para a População Brasileira, 2nd ed.; Ministério da Saúde: Rio de Janeiro, Brazil, 2014. Available online: https://www.gov.br/saude/pt-br (accessed on 15 July 2022).
- Souza, A.M.; Barufaldi, L.A.; Abreu, G.A.; Giannini, D.T.; Oliveira, C.L.; Santos, M.M.; Leal, V.S.; Vasconcelos, F.D. ERICA: Intake of macro and micronutrients of Brazilian adolescents. Rev. Saúde Pública 2016, 50, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Machado, P.P.; Claro, R.M.; Canella, D.S.; Sarti, F.M.; Levy, R.B. Price and convenience: The influence of supermarkets on consumption of ultra-processed foods and beverages in Brazil. Appetite 2017, 116, 381–388. [Google Scholar] [CrossRef]
- Yanovsky, J.A. Pediatric obesity. An introduction. J. Appet. 2016, 1, 3–12. [Google Scholar] [CrossRef]
- Wright, J.; Maher, J.; Tanner, C. Social class, anxieties and mothers’ foodwork. Sociol. Health Illn. 2015, 37, 422–436. [Google Scholar] [CrossRef]
- Grzymisławska, M.; Puch, E.A.; Zawada, A.; Grzymislawski, M. Do nutricional behaviors depend on biological sex and cultural gender? Adv. Clin. Exp. Med. 2020, 26, 165–172. [Google Scholar] [CrossRef]
- Alonso-Geta, P.M.P.; Moreno, M.C.B. Hygiene and eating healthy habits and practices in spanish families with children aged 6 to 14. Int. J. Environ. Res. Public Health 2020, 17, 8671. [Google Scholar] [CrossRef]
- Rodgers, R.; Chabrol, H. Parental attitudes, body image disturbance and disordered eating amongst adolescents and young adults: A review. Eur. Eat. Disord. Rev. 2009, 17, 137–151. [Google Scholar] [CrossRef] [PubMed]
- Michael, D.; Ryan, D.H.; Apovian, C.M.; Ard, J.D.; Comuzzie, A.G.; Donato, K.A.; Hu, F.B.; Hubbard, V.S.; Jakicic, J.M.; Kushner, R.F.; et al. 2013 AHA/ACC/TOS Guideline for the management of overweight and obesity in adults: A report of the american college of cardiology/american heart association task force on practice guidelines and the obesity society. J. Am. Coll. Cardiol. 2014, 63, 3029–3030. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. PLoS Med. 2010, 7, 17. [Google Scholar] [CrossRef]
- Lohman, T.G.; Roche, A.F.; Martorell, R. Anthropometric Standardization Reference Manual; Human Kinetics Books: Chicago, IL, USA, 1988; ISBN 0873221214. [Google Scholar]
- Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nichida, C.; Siekmann, J. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef]
- Oliveira, F.M.; Marques, D.C.S.; Coelho, A.A.; Marques, M.G.S.; Araújo, C.G.A.; Branco, B.H.M. Effects of a multiprofessional approach on anthropometric variables and food profile of overweight or obese adolescents. J. Hum. Growth Dev. 2021, 31, 257–266. [Google Scholar] [CrossRef]
- IBGE. Tabela de Composição de Alimentos (TACO), 4th ed.; IBGE: Rio de Janeiro, Brazil, 1996.
- Malta, M.B.; Papini, S.J.; Corrente, J.E. Avaliação da alimentação de idosos de município paulista: Aplicação do Índice de Alimentação Saudável. Ciênc. Saúde Coletiva 2013, 18, 377–384. [Google Scholar] [CrossRef]
- Tanner, J.M. Growth at Adolescence; Blackwell Scientific Publications: Oxford, UK, 1962. [Google Scholar] [CrossRef]
- Branco, B.H.M.; Carvalho, I.Z.; de Oliveira, H.G.; Fanhani, A.P.; dos Santos, M.C.M.; de Oliveira, L.P.; Boni, S.M.; Nelson Nardo, J. Effects of 2 Types of Resistance Training Models on Obese Adolescentsʼ Body Composition, Cardiometabolic Risk, and Physical Fitness. J. Strength Cond. Res. 2020, 34, 2672–2682. [Google Scholar] [CrossRef] [PubMed]
- Carbert, N.S.; Brussoni, M.; Geller, J.; Mâsse, L.C. Familial Environment and Overweight/Obese ‘Adolescents’ Physical Activity. Int. J. Environ. Res. Public Health 2019, 16, 2558. [Google Scholar] [CrossRef]
- Madalosso, M.; Schaan, B.; Cureau, F.V. Association between body weight perception and quality of diet in brazilian adolescents. Rev. Paul. Pediatr. 2020, 38, e2020057. [Google Scholar] [CrossRef] [PubMed]
- Nardo Junior, N.; Bianchini, J.A.A.; da Silva, D.F.; Ferraro, Z.M.; Lopera, C.A.; Antonini, V.D.S. Building a response criterion for pediatric multi-professional obesity intervention success based on combined benefits. Eur. J. Pediatr. 2018, 177, 1–12. [Google Scholar] [CrossRef]
- Kalantari, N.; Mohammadi, N.K.; Rafieifar, S.; Eini-Zinab, H.; Aminifard, A.; Malmir, H.; Ashoori, N.; Abdi, S.; Gholamalizadeh, M.; Doaei, S. Indicator for Success of Obesity Reduction Programs in Adolescents: Body Composition or Body Mass Index? Evaluating a School-based Health Promotion Project after 12 Weeks of Intervention. Int. J. Prev. Med. 2017, 8, 73. [Google Scholar] [CrossRef]
- Goldschmidt, A.B.; Wall, M.M.; Choo, T.J.; Evans, E.W.; Jelalian, E.; Larson, N.; Neumark-Sztainer, D. Fifteen-year Weight and Disordered Eating Patterns Among Community-based Adolescents. Am. J. Prev. Med. 2018, 54, e21–e29. [Google Scholar] [CrossRef]
- Costa, C.S.; Del-Ponte, B.; Assunção, M.C.F.; Santos, I.S. Consumption of ultra-processed foods and body fat during childhood and adolescence: A systematic review. Public Health Nutr. 2018, 21, 148–159. [Google Scholar] [CrossRef] [PubMed]
- Steele, E.M.; Baraldi, L.G.; Da Costa Louzada, M.L.; Moubarac, J.C.; Mozaffarian, D.; Monteiro, C.A. Ultra-processed foods and added sugars in the US diet: Evidence from a nationally representative cross-sectional study. BMJ Open 2016, 6, e009892. [Google Scholar] [CrossRef]
- Ong, J.X.; Ullah, S.; Magarey, A.; Miller, J.; Leslie, E. Relationship between the home environment and fruit and vegetable consumption in children aged 6–12 years: A systematic review. Public Health Nutr. 2017, 20, 464–480. [Google Scholar] [CrossRef]
- Carroll, N.; Sadowski, A.; Laila, A.; Hruska, V.; Nixon, M.; Ma, D.W.L.; Haines, J. The impact of COVID-19 on health behavior, stress, financial and food security among middle to high income canadian families with young children. Nutrients 2020, 12, 2352. [Google Scholar] [CrossRef] [PubMed]
- Henrique, C.R.P.; Ferreira, W.C.; Henriques, V.F.; Marques, D.C.S.; Silva, M.P.P.; Valdes-badilla, P.; Mota, J.; Branco, B.H.M. Deleterious effects of COVID-2019 lockdown on health responses in adolescents with obesity: Longitudinal study. Rev. Saúde Pesqui. 2022, 15, 1–4. [Google Scholar] [CrossRef]
- Hennessy, E.; Hughes, S.O.; Goldberg, J.P.; Hyatt, R.R.; Economos, C.D. Permissive parental feeding behavior is associated with an increase in intake of low-nutrient-dense foods among american children living in rural communities. J. Acad. Nutr. Diet. 2012, 112, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Sena, R.P.; Santos, I.C.; Cerqueira, B.S.; Oliveira, F.M.; Acencio, F.R.; Franco, C.B.; Branco, B.H.M. Establishing a normative table for classifying body fat percentage in adolescents. J. Hum. Growth Dev. 2022, 32, 129–135. [Google Scholar] [CrossRef]
- Branco, B.H.M.; Mariano, I.R.; Oliveira, L.P.; Bertolini, S.M.M.G.; Oliveira, F.M.; Araújo, C.J.A.; Adamo, K. Sports and functional training improve a subset of obesity-related health parameters in adolescents: A randomized controlled trial. Front. Psychol. 2021, 11, 589554. [Google Scholar] [CrossRef] [PubMed]
- Branco, B.H.M.; Valladares, D.; de Oliveira, F.M.; Carvalho, I.Z.; Marques, D.C.; Coelho, A.A.; Oliveira, L.P.; Bertolini, S.M.M.G. Effects of the Order of Physical Exercises on Body Composition, Physical Fitness, and Cardiometabolic Risk in Adolescents Participating in an Interdisciplinary Program Focusing on the Treatment of Obesity. Front. Physiol. 2019, 10, 1013. [Google Scholar] [CrossRef] [PubMed]
| Variables | FG | Delta | Cohen’s d | IG | Delta | Cohen’s d | ||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | |||||
| Age (years old) * | 14.24 ± 2.61 | 14.52 ± 2.62 | 0.29 ± 0.46 | 0.11 | 13.23 ± 2.27 | 13.45 ± 2.39 | 0.23 ± 0.43 | 0.10 |
| Body Mass (kg) | 76.95 ± 22.30 | 77.47 ± 21.79 | 0.52 ± 2.12 | 0.02 | 83.52 ± 28.76 | 83.22 ± 26.60 | −0.30 ± 3.01 | −0.01 |
| Height (m2) * | 1.62 ± 0.13 | 1.63 ± 0.13 | 0.01 ± 0.01 | 0.07 | 1.64 ± 0.10 | 1.65 ± 0.10 | 0.01 ± 0.01 | 0.06 |
| BMI (kg/m2) | 28.89 ± 6.11 | 28.77 ± 5.78 | −0.12 ± 0.98 | −0.02 | 30.77 ± 9.47 | 30.52 ± 8.84 | −0.25 ± 1.11 | −0.03 |
| BMI Z-score | 2.17 ± 1.36 | 2.12 ± 1.23 | −0.05 ± 0.26 | −0.04 | 2.52 ± 1.63 | 2.45 ± 1.53 | −0.07 ± 0.20 | −0.05 |
| Kilocalories | Kilograms | |||||||
|---|---|---|---|---|---|---|---|---|
| Processing Level | Δ Absolute FG (Mean ± SD) | Δ Absolute IG (Mean ± SD) | p-Value | Cohen’s d | Δ Absolute FG (Mean ± SD) | Δ Absolute IG (Mean ± SD) | p-Value | Cohen’s d |
| Fresh Products | 40.2 ± 103.1 | 116.0 ± 224.0 | p = 0.16 | 0.43 | 86.5 ± 274.4 | 231.1 ± 285.8 | p = 0.09 | 0.51 |
| Minimally Processed | 58.9 ± 784.6 | 4.37 ± 574.5 | p = 0.79 | 0.02 | 210.4 ± 639.8 | 87.5 ± 515.8 | p = 0.49 | 0.21 |
| Processed | −28.9 ± 327.7 | −382.2 ± 833.5 | p = 0.07 | 0.55 | 39.9 ± 347.0 | −192.2 ± 465.2 | p = 0.07 | 0.56 |
| Ultra-processed | −139.5 ± 854.1 | −537.1 ± 828.0 | p = 0.12 | 0.47 | −130.2 ± 510.1 | −341.5 ± 742.5 | p = 0.28 | 0.33 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marques, D.C.S.; Ferreira, W.C.; Santos, I.C.; Ryal, J.J.; Marques, M.G.S.; Oliveira, F.M.; Milani, R.G.; Mota, J.; Valdés-Badilla, P.; Branco, B.H.M. Impacts of a Multi-Professional Family versus Isolated Intervention on Food Level Processing in Overweight Adolescents: A Randomized Trial. Nutrients 2023, 15, 935. https://doi.org/10.3390/nu15040935
Marques DCS, Ferreira WC, Santos IC, Ryal JJ, Marques MGS, Oliveira FM, Milani RG, Mota J, Valdés-Badilla P, Branco BHM. Impacts of a Multi-Professional Family versus Isolated Intervention on Food Level Processing in Overweight Adolescents: A Randomized Trial. Nutrients. 2023; 15(4):935. https://doi.org/10.3390/nu15040935
Chicago/Turabian StyleMarques, Déborah C. S., Willian C. Ferreira, Isabella C. Santos, Joed J. Ryal, Marilene G. S. Marques, Fabiano M. Oliveira, Rute G. Milani, Jorge Mota, Pablo Valdés-Badilla, and Braulio H. M. Branco. 2023. "Impacts of a Multi-Professional Family versus Isolated Intervention on Food Level Processing in Overweight Adolescents: A Randomized Trial" Nutrients 15, no. 4: 935. https://doi.org/10.3390/nu15040935
APA StyleMarques, D. C. S., Ferreira, W. C., Santos, I. C., Ryal, J. J., Marques, M. G. S., Oliveira, F. M., Milani, R. G., Mota, J., Valdés-Badilla, P., & Branco, B. H. M. (2023). Impacts of a Multi-Professional Family versus Isolated Intervention on Food Level Processing in Overweight Adolescents: A Randomized Trial. Nutrients, 15(4), 935. https://doi.org/10.3390/nu15040935










