A Glimpse into Milestones of Insulin Resistance and an Updated Review of Its Management
Abstract
1. Introduction
2. Metabolic Syndrome
2.1. Type 2 Diabetes
2.2. Obesity
2.3. Gestational Diabetes
2.4. Human Insulin in Brief
2.5. Glucose Transporters
2.5.1. GLUT1
2.5.2. GLUT2
2.5.3. GLUT3
2.5.4. GLUT4
2.5.5. GLUT14
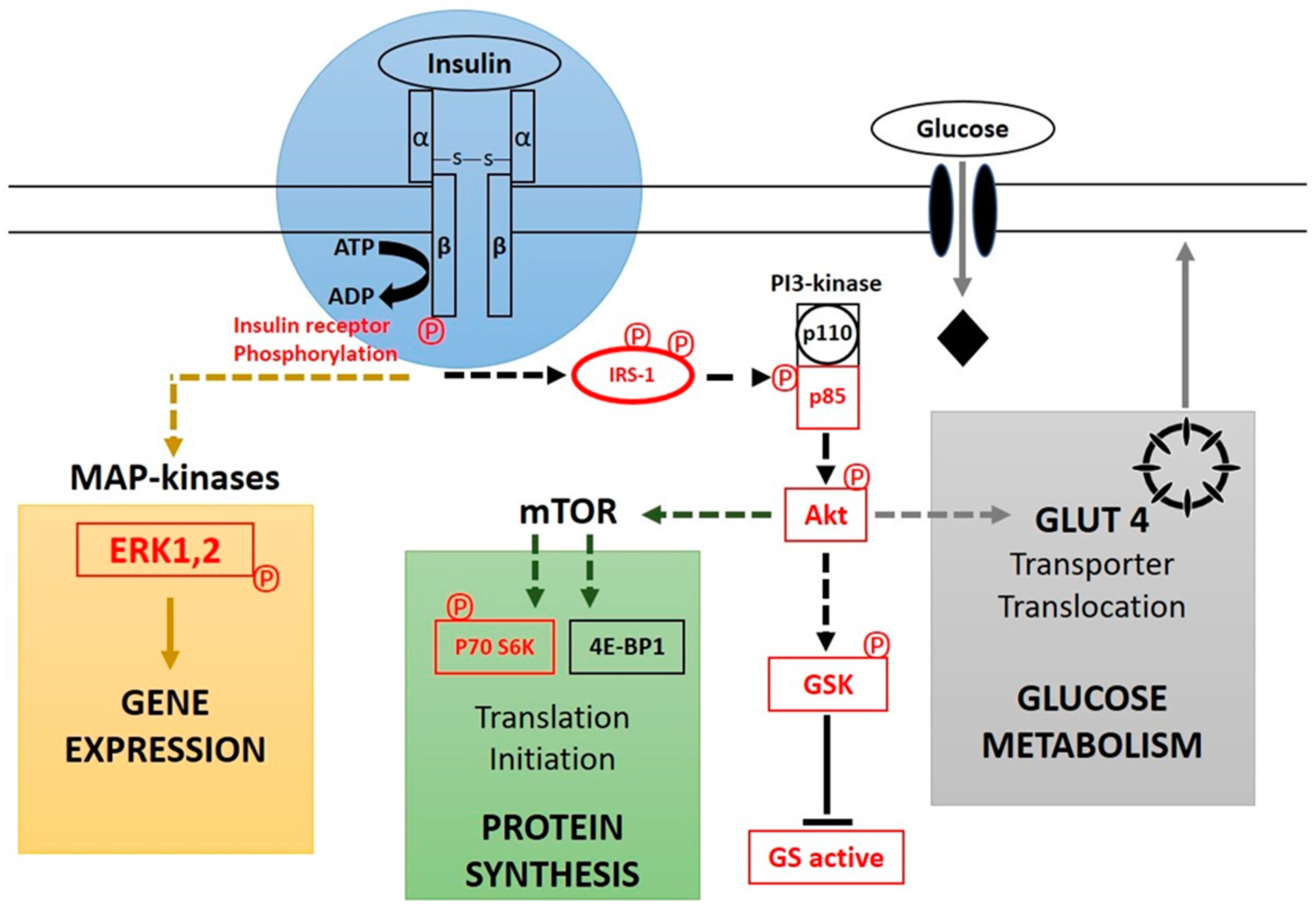
2.6. Insulin as a First Messenger in Signal Transduction Cascade
2.7. Physiological Effects of Insulin
2.8. Treatment
3. Discussion
3.1. Lipotoxicity and Effects of Ceramide
3.2. The Inflammatory and Autoimmunity Theory
3.3. Impact of Eosinophilia
3.4. Oxidative Stress
3.5. Mitochondrial Dysfunction
3.6. Impact of Platelets
3.7. Microbiota and Insulin Resistance
3.8. Drug-Induced Insulin Resistance
3.9. Membrane Function and Membrane Pacemaker Hypothesis
3.10. N-Glycosylation of Membrane Proteins
3.11. Vitamin D Deficiency and Insulin Resistance
3.12. Influence of COVID-19
3.13. How to Combat Insulin Resistance?
4. Conclusions
5. Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Rasooly, R.S.; Akolkar, B.; Spain, L.M.; Guill, M.H.; Del Vecchio, C.T.; Carroll, L.E. The National Institute of Diabetes and Digestive and Kidney Diseases Central Repositories. Clin. J. Am. Soc. Nephrol. 2015, 10, 710–715. [Google Scholar] [CrossRef]
- Amrita, A.A. Relevance of Lipoprotein (a) in predicting the diagnosis of type II diabetes mellitus. Medpulse Int. J. Biochem. 2019, 9, 23–27. [Google Scholar]
- WHO. Diabetes Fact sheet N°312; WHO: Geneva, Switzerland, 2013. [Google Scholar]
- Saedi, E.; Gheini, M.R.; Faiz, F.; Arami, M.A. Diabetes mellitus and cognitive impairments. World J. Diabetes 2016, 7, 412–422. [Google Scholar] [CrossRef] [PubMed]
- Long, B.; Lentz, S.; Koyfman, A.; Gottlieb, M. Euglycemic diabetic ketoacidosis: Etiologies, evaluation, and management. Am. J. Emerg. Med. 2021, 44, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Shoback, D.M.; Gardner, D.G. (Eds.) Chapter 17: Pancreatic hormones & diabetes mellitus. In Greenspan’s Basic & Clinical Endocrinology, 9th ed.; McGraw-Hill Medical: New York, NY, USA, 2011; ISBN 978-0-07-162243-1. [Google Scholar]
- Melmed, S.; Polonsky, K.S.; Larsen, P.R.; Kronenberg, H.M. (Eds.) Williams Textbook of Endocrinology, 12th ed.; Elsevier/Saunders: Philadelphia, PA, USA, 2011; pp. 1371–1435. ISBN 978-1-4377-0324-5. [Google Scholar]
- GBD 2013 Risk Factors Collaborators; Forouzanfar, M.H.; Alexander, L.; Anderson, H.R.; Bachman, V.F.; Biryukov, S.; Brauer, M.; Burnett, R.; Casey, D.; Coates, M.M.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990-2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 2287–2323. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Ley, S.H.; Hu, F.B. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol. 2018, 14, 88–98. [Google Scholar] [CrossRef] [PubMed]
- Vijan, S. Type 2 Diabetes. Ann. Intern. Med. 2010, 152, ITC3-1. [Google Scholar] [CrossRef] [PubMed]
- Abate, N.; Chandalia, M. Ethnicity and type 2 diabetes: Focus on Asian Indians. J. Diabetes Complicat. 2001, 15, 320–327. [Google Scholar] [CrossRef]
- Carulli, L.; Rondinella, S.; Lombardini, S.; Canedi, I.; Loria, P.; Carulli, N. Review article: Diabetes, genetics and ethnicity. Aliment Pharmacol. Ther. 2005, 22 (Suppl. 2), 16–19. [Google Scholar] [CrossRef]
- World Health Organization. Diabetes Fact sheet N°312; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- Smyth, S.; Heron, A. Diabetes and obesity: The twin epidemics. Nat. Med. 2006, 12, 75–80. [Google Scholar] [CrossRef]
- Beltran-Sanchez, H.; Harhay, M.O.; Harhay, M.M.; McElligott, S. Prevalence and trends of metabolic syndrome in the adult U.S. population, 1999–2010. J. Am. Coll Cardiol. 2013, 62, 697–703. [Google Scholar] [CrossRef] [PubMed]
- Hurrle, S.; Hsu, W.H. The etiology of oxidative stress in insulin resistance. Biomed. J. 2017, 40, 257–262. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. Classification and Diagnosis of Diabetes. Diabetes Care 2017, 40 (Suppl. 1), S11–S24. [Google Scholar] [CrossRef] [PubMed]
- Carris, N.W.; Magness, R.R.; Labovitz, A.J. Prevention of Diabetes Mellitus in Patients With Prediabetes. Am. J. Cardiol. 2019, 123, 507–512. [Google Scholar] [CrossRef]
- Ling, C.; Ronn, T. Epigenetics in Human Obesity and Type 2 Diabetes. Cell Metab. 2019, 29, 1028–1044. [Google Scholar] [CrossRef]
- Laakso, M. Biomarkers for type 2 diabetes. Mol. Metab. 2019, 27S, S139–S146. [Google Scholar] [CrossRef]
- Malik, V.S.; Popkin, B.M.; Bray, G.A.; Despres, J.P.; Hu, F.B. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation 2010, 121, 1356–1364. [Google Scholar] [CrossRef]
- Malik, V.S.; Popkin, B.M.; Bray, G.A.; Despres, J.P.; Willett, W.C.; Hu, F.B. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: A meta-analysis. Diabetes Care 2010, 33, 2477–2483. [Google Scholar] [CrossRef]
- Riserus, U.; Willett, W.C.; Hu, F.B. Dietary fats and prevention of type 2 diabetes. Prog. Lipid Res. 2009, 48, 44–51. [Google Scholar] [CrossRef]
- Atkinson, F.S.; Foster-Powell, K.; Brand-Miller, J.C. International tables of glycemic index and glycemic load values: 2008. Diabetes Care 2008, 31, 2281–2283. [Google Scholar] [CrossRef]
- Di Ciaula, A.; Garruti, G.; Fruhbeck, G.; De Angelis, M.; de Bari, O.; Wang, D.Q.; Lammert, F.; Portincasa, P. The Role of Diet in the Pathogenesis of Cholesterol Gallstones. Curr. Med. Chem. 2019, 26, 3620–3638. [Google Scholar] [CrossRef] [PubMed]
- Hu, E.A.; Pan, A.; Malik, V.; Sun, Q. White rice consumption and risk of type 2 diabetes: Meta-analysis and systematic review. BMJ 2012, 344, e1454. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, D.J.; Wolever, T.M.; Taylor, R.H.; Barker, H.; Fielden, H.; Baldwin, J.M.; Bowling, A.C.; Newman, H.C.; Jenkins, A.L.; Goff, D.V. Glycemic index of foods: A physiological basis for carbohydrate exchange. Am. J. Clin. Nutr. 1981, 34, 362–366. [Google Scholar] [CrossRef]
- Morales, P.E.; Bucarey, J.L.; Espinosa, A. Muscle Lipid Metabolism: Role of Lipid Droplets and Perilipins. J. Diabetes Res. 2017, 2017, 1789395. [Google Scholar] [CrossRef] [PubMed]
- Meex, R.C.R.; Blaak, E.E.; van Loon, L.J.C. Lipotoxicity plays a key role in the development of both insulin resistance and muscle atrophy in patients with type 2 diabetes. Obes. Rev. 2019, 20, 1205–1217. [Google Scholar] [CrossRef]
- Glycemic Research Institute. Glycemic Load Defined; Glycemic Research Institute: Washington, DC, USA, 2013. [Google Scholar]
- U.S. Department of Health and Human Services. National Diabetes Clearinghouse (NDIC): National Diabetes Statistics; U.S. Department of Health and Human Services: Washington, DC, USA, 2011. [Google Scholar]
- Soldavini, J. Krause’s Food & The Nutrition Care Process. J. Nutr. Educ. Behav. 2019, 51, 1225. [Google Scholar] [CrossRef]
- Beilby, H.; Yang, F.; Gannon, B.; McIntyre, H.D. Cost-effectiveness of gestational diabetes screening including prevention of type 2 diabetes: Application of the GeDiForCE model in Australia. J. Matern. Fetal. Neonatal. Med. 2022, 35, 8286–8293. [Google Scholar] [CrossRef]
- Li, Z.; Cheng, Y.; Wang, D.; Chen, H.; Chen, H.; Ming, W.K.; Wang, Z. Incidence Rate of Type 2 Diabetes Mellitus after Gestational Diabetes Mellitus: A Systematic Review and Meta-Analysis of 170,139 Women. J. Diabetes Res. 2020, 2020, 3076463. [Google Scholar] [CrossRef]
- Amraei, M.; Mohamadpour, S.; Sayehmiri, K.; Mousavi, S.F.; Shirzadpour, E.; Moayeri, A. Effects of Vitamin D Deficiency on Incidence Risk of Gestational Diabetes Mellitus: A Systematic Review and Meta-analysis. Front. Endocrinol. 2018, 9, 7. [Google Scholar] [CrossRef]
- Zhang, Y.; Gong, Y.; Xue, H.; Xiong, J.; Cheng, G. Vitamin D and gestational diabetes mellitus: A systematic review based on data free of Hawthorne effect. BJOG 2018, 125, 784–793. [Google Scholar] [CrossRef]
- Managing & Treating Gestational Diabetes | NIDDK; National Institute of Diabetes and Digestive and Kidney Diseases: Bethesda, MD, USA, 2019.
- Voet, D.; Voet, J.G. Biochemistry, 4th ed.; Wiley: New York, NY, USA, 2011. [Google Scholar]
- Berg, J.M.; Tymoczko, J.L.; Stryer, L. Biochemistry, 5th ed.; W. H. Freeman and Company: New York, NY, USA, 2001; pp. 858–859. [Google Scholar]
- Koeslag, J.H.; Saunders, P.T.; Terblanche, E. A reappraisal of the blood glucose homeostat which comprehensively explains the type 2 diabetes mellitus-syndrome X complex. J. Physiol. 2003, 549, 333–346. [Google Scholar] [CrossRef] [PubMed]
- Rowlett, R. A Dictionary of Units of Measurement; The University of North Carolina at Chapel Hill: Chapel Hill, NC, USA, 2001. [Google Scholar]
- Iwase, H.; Kobayashi, M.; Nakajima, M.; Takatori, T. The ratio of insulin to C-peptide can be used to make a forensic diagnosis of exogenous insulin overdosage. Forensic Sci. Int. 2001, 115, 123–127. [Google Scholar] [CrossRef]
- Hellman, B.; Gylfe, E.; Grapengiesser, E.; Dansk, H.; Salehi, A. Insulin oscillations--clinically important rhythm. Antidiabetics should increase the pulsative component of the insulin release. Lakartidningen 2007, 104, 2236–2239. [Google Scholar] [PubMed]
- Thorens, B.; Mueckler, M. Glucose transporters in the 21st Century. Am. J. Physiol. Endocrinol. Metab. 2010, 298, E141–E145. [Google Scholar] [CrossRef] [PubMed]
- Bell, G.I.; Kayano, T.; Buse, J.B.; Burant, C.F.; Takeda, J.; Lin, D.; Fukumoto, H.; Seino, S. Molecular biology of mammalian glucose transporters. Diabetes Care 1990, 13, 198–208. [Google Scholar] [CrossRef]
- Berger, C.; Zdzieblo, D. Glucose transporters in pancreatic islets. Pflugers Arch. 2020, 472, 1249–1272. [Google Scholar] [CrossRef] [PubMed]
- Mueckler, M.; Caruso, C.; Baldwin, S.A.; Panico, M.; Blench, I.; Morris, H.R.; Allard, W.J.; Lienhard, G.E.; Lodish, H.F. Sequence and structure of a human glucose transporter. Science 1985, 229, 941–945. [Google Scholar] [CrossRef]
- Olson, A.L.; Pessin, J.E. Structure, function, and regulation of the mammalian facilitative glucose transporter gene family. Annu. Rev. Nutr. 1996, 16, 235–256. [Google Scholar] [CrossRef]
- Gould, G.W.; Thomas, H.M.; Jess, T.J.; Bell, G.I. Expression of human glucose transporters in Xenopus oocytes: Kinetic characterization and substrate specificities of the erythrocyte, liver, and brain isoforms. Biochemistry 1991, 30, 5139–5145. [Google Scholar] [CrossRef]
- Freitas, H.S.; Schaan, B.D.; Seraphim, P.M.; Nunes, M.T.; Machado, U.F. Acute and short-term insulin-induced molecular adaptations of GLUT2 gene expression in the renal cortex of diabetic rats. Mol. Cell Endocrinol. 2005, 237, 49–57. [Google Scholar] [CrossRef]
- Kellett, G.L.; Brot-Laroche, E. Apical GLUT2: A major pathway of intestinal sugar absorption. Diabetes 2005, 54, 3056–3062. [Google Scholar] [CrossRef] [PubMed]
- Vannucci, S.J.; Maher, F.; Simpson, I.A. Glucose transporter proteins in brain: Delivery of glucose to neurons and glia. Glia 1997, 21, 2–21. [Google Scholar] [CrossRef]
- Brown, K.; Heller, D.S.; Zamudio, S.; Illsley, N.P. Glucose transporter 3 (GLUT3) protein expression in human placenta across gestation. Placenta 2011, 32, 1041–1049. [Google Scholar] [CrossRef] [PubMed]
- Simpson, I.A.; Dwyer, D.; Malide, D.; Moley, K.H.; Travis, A.; Vannucci, S.J. The facilitative glucose transporter GLUT3: 20 years of distinction. Am. J. Physiol. Endocrinol. Metab. 2008, 295, E242–E253. [Google Scholar] [CrossRef] [PubMed]
- James, D.E.; Brown, R.; Navarro, J.; Pilch, P.F. Insulin-regulatable tissues express a unique insulin-sensitive glucose transport protein. Nature 1988, 333, 183–185. [Google Scholar] [CrossRef] [PubMed]
- Chadt, A.; Al-Hasani, H. Glucose transporters in adipose tissue, liver, and skeletal muscle in metabolic health and disease. Pflugers Arch. 2020, 472, 1273–1298. [Google Scholar] [CrossRef]
- Mueckler, M.; Thorens, B. The SLC2 (GLUT) family of membrane transporters. Mol. Asp. Med. 2013, 34, 121–138. [Google Scholar] [CrossRef]
- Buchberger, A.; Howard, M.J.; Proctor, M.; Bycroft, M. The UBX domain: A widespread ubiquitin-like module. J. Mol. Biol. 2001, 307, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Freeze, H.H. GLUT14, a duplicon of GLUT3, is specifically expressed in testis as alternative splice forms. Genomics 2002, 80, 553–557. [Google Scholar] [CrossRef]
- McManus, E.J.; Sakamoto, K.; Armit, L.J.; Ronaldson, L.; Shpiro, N.; Marquez, R.; Alessi, D.R. Role that phosphorylation of GSK3 plays in insulin and Wnt signalling defined by knockin analysis. EMBO J. 2005, 24, 1571–1583. [Google Scholar] [CrossRef] [PubMed]
- Cross, D.A.; Watt, P.W.; Shaw, M.; van der Kaay, J.; Downes, C.P.; Holder, J.C.; Cohen, P. Insulin activates protein kinase B, inhibits glycogen synthase kinase-3 and activates glycogen synthase by rapamycin-insensitive pathways in skeletal muscle and adipose tissue. FEBS Lett. 1997, 406, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Stryer, L. Biochemistry, 4th ed.; W. H. Freeman and Company: New York, NY, USA, 1995; pp. 351–356, 494–495, 505, 605–606, 773–775. ISBN 0-7167-2009-4. [Google Scholar]
- Hou, J.C.; Pessin, J.E. Ins (endocytosis) and outs (exocytosis) of GLUT4 trafficking. Curr. Opin Cell Biol. 2007, 19, 466–473. [Google Scholar] [CrossRef] [PubMed]
- Najjar, S. Insulin Action: Molecular Basis of Diabetes. In Encyclopedia of Life Sciences; John Wiley & Sons: Hoboken, NJ, USA, 2001; ISBN 978-0470016176. [Google Scholar] [CrossRef]
- Duckworth, W.C.; Bennett, R.G.; Hamel, F.G. Insulin degradation: Progress and potential. Endocr. Rev. 1998, 19, 608–624. [Google Scholar] [CrossRef] [PubMed]
- Physiologic Effects of Insulin. Available online: www.vivo.colostate.edu (accessed on 1 June 2017).
- Benziane, B.; Chibalin, A.V. Frontiers: Skeletal muscle sodium pump regulation: A translocation paradigm. Am. J. Physiol. Endocrinol. Metab. 2008, 295, E553–E558. [Google Scholar] [CrossRef]
- Bergamini, E.; Cavallini, G.; Donati, A.; Gori, Z. The role of autophagy in aging: Its essential part in the anti-aging mechanism of caloric restriction. Ann. N. Y. Acad. Sci. 2007, 1114, 69–78. [Google Scholar] [CrossRef]
- Clausen, T. Regulatory role of translocation of Na+-K+ pumps in skeletal muscle: Hypothesis or reality? Am. J. Physiol. Endocrinol. Metab. 2008, 295, E727–E728. [Google Scholar] [CrossRef] [PubMed]
- Dimitriadis, G.; Mitrou, P.; Lambadiari, V.; Maratou, E.; Raptis, S.A. Insulin effects in muscle and adipose tissue. Diabetes Res. Clin. Pract 2011, 93 (Suppl. 1), S52–S59. [Google Scholar] [CrossRef]
- Gupta, A.K.; Clark, R.V.; Kirchner, K.A. Effects of insulin on renal sodium excretion. Hypertension 1992, 19, I78–I82. [Google Scholar] [CrossRef]
- Kreitzman, S.N.; Coxon, A.Y.; Szaz, K.F. Glycogen storage: Illusions of easy weight loss, excessive weight regain, and distortions in estimates of body composition. Am. J. Clin. Nutr. 1992, 56, 292S–293S. [Google Scholar] [CrossRef]
- Zheng, C.; Liu, Z. Vascular function, insulin action, and exercise: An intricate interplay. Trends Endocrinol. Metab. 2015, 26, 297–304. [Google Scholar] [CrossRef]
- Rhea, E.M.; Nirkhe, S.; Nguyen, S.; Pemberton, S.; Bammler, T.K.; Beyer, R.; Niehoff, M.L.; Morley, J.E.; Farr, S.A.; Banks, W.A. Molecular Mechanisms of Intranasal Insulin in SAMP8 Mice. J. Alzheimers Dis. 2019, 71, 1361–1373. [Google Scholar] [CrossRef]
- Benedict, C.; Brede, S.; Schioth, H.B.; Lehnert, H.; Schultes, B.; Born, J.; Hallschmid, M. Intranasal insulin enhances postprandial thermogenesis and lowers postprandial serum insulin levels in healthy men. Diabetes 2011, 60, 114–118. [Google Scholar] [CrossRef]
- Sliwowska, J.H.; Fergani, C.; Gawalek, M.; Skowronska, B.; Fichna, P.; Lehman, M.N. Insulin: Its role in the central control of reproduction. Physiol. Behav. 2014, 133, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Berg, J.M.; Tymoczko, J.L.; Stryer, L. Glycolysis Chapter 16. In Biochemistry, 5th ed.; W. H. Freeman and Company: New York, NY, USA, 2002; pp. 688–690. Available online: www.whfreeman.com/biochem5 (accessed on 1 June 2017).
- Eurich, D.T.; McAlister, F.A.; Blackburn, D.F.; Majumdar, S.R.; Tsuyuki, R.T.; Varney, J.; Johnson, J.A. Benefits and harms of antidiabetic agents in patients with diabetes and heart failure: Systematic review. BMJ. 2007, 335, 497. [Google Scholar] [CrossRef] [PubMed]
- Rena, G.; Hardie, D.G.; Pearson, E.R. The mechanisms of action of metformin. Diabetologia 2017, 60, 1577–1585. [Google Scholar] [CrossRef] [PubMed]
- Bloomgarden, Z.T. Developments in diabetes and insulin resistance. Diabetes Care 2006, 29, 161–167. [Google Scholar] [CrossRef]
- Landau, Z.; Raz, I.; Wainstein, J.; Bar-Dayan, Y.; Cahn, A. The role of insulin pump therapy for type 2 diabetes mellitus. Diabetes Metab. Res. Rev. 2017, 33, e2822. [Google Scholar] [CrossRef]
- Costanzo, P.; Cleland, J.G.; Pellicori, P.; Clark, A.L.; Hepburn, D.; Kilpatrick, E.S.; Perrone-Filardi, P.; Zhang, J.; Atkin, S.L. The obesity paradox in type 2 diabetes mellitus: Relationship of body mass index to prognosis: A cohort study. Ann. Intern. Med. 2015, 162, 610–618. [Google Scholar] [CrossRef]
- Mikstas, C. U.S. Department of Agriculture FoodData Central. 9 November 2020. Available online: https://fdc.nal.usda.gov/docs/Foundation_Foods_Documentation_Apr2021.pdf (accessed on 1 June 2017).
- Vaag, A.; Lund, S.S. Non-obese patients with type 2 diabetes and prediabetic subjects: Distinct phenotypes requiring special diabetes treatment and (or) prevention? Appl. Physiol. Nutr. Metab. 2007, 32, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Hirose, H.; Ohneda, M.; Johnson, J.H.; McGarry, J.D.; Unger, R.H. Beta-cell lipotoxicity in the pathogenesis of non-insulin-dependent diabetes mellitus of obese rats: Impairment in adipocyte-beta-cell relationships. Proc. Natl. Acad. Sci. USA 1994, 91, 10878–10882. [Google Scholar] [CrossRef]
- Oh, Y.S.; Bae, G.D.; Baek, D.J.; Park, E.Y.; Jun, H.S. Fatty Acid-Induced Lipotoxicity in Pancreatic Beta-Cells During Development of Type 2 Diabetes. Front. Endocrinol. 2018, 9, 384. [Google Scholar] [CrossRef] [PubMed]
- Xin, Y.; Wang, Y.; Chi, J.; Zhu, X.; Zhao, H.; Zhao, S.; Wang, Y. Elevated free fatty acid level is associated with insulin-resistant state in nondiabetic Chinese people. Diabetes Metab. Syndr. Obes. 2019, 12, 139–147. [Google Scholar] [CrossRef]
- DeFronzo, R.A. Insulin resistance, lipotoxicity, type 2 diabetes and atherosclerosis: The missing links. The Claude Bernard Lecture 2009. Diabetologia 2010, 53, 1270–1287. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, M.K.; De Nardo, W.; Watt, M.J. Impact of Lipotoxicity on Tissue “Cross Talk” and Metabolic Regulation. Physiology 2019, 34, 134–149. [Google Scholar] [CrossRef]
- Sokolowska, E.; Blachnio-Zabielska, A. The Role of Ceramides in Insulin Resistance. Front. Endocrinol. 2019, 10, 577. [Google Scholar] [CrossRef]
- Li, D.; Zhu, Y.; Wang, Y.; Zou, Q.; Duan, J.; Sun-Waterhouse, D.; Sun, B. Perspectives on diacylglycerol-induced improvement of insulin sensitivity in type 2 diabetes. Food Sci. Hum. Wellness 2022, 11, 230–237. [Google Scholar] [CrossRef]
- Brons, C.; Grunnet, L.G. MECHANISMS IN ENDOCRINOLOGY: Skeletal muscle lipotoxicity in insulin resistance and type 2 diabetes: A causal mechanism or an innocent bystander? Eur. J. Endocrinol. 2017, 176, R67–R78. [Google Scholar] [CrossRef]
- Virtue, S.; Vidal-Puig, A. Adipose tissue expandability, lipotoxicity and the Metabolic Syndrome—An allostatic perspective. Biochim. Biophys. Acta 2010, 1801, 338–349. [Google Scholar] [CrossRef]
- Yazici, D.; Sezer, H. Insulin Resistance, Obesity and Lipotoxicity. Adv. Exp. Med. Biol. 2017, 960, 277–304. [Google Scholar] [CrossRef]
- Lair, B.; Laurens, C.; Van Den Bosch, B.; Moro, C. Novel Insights and Mechanisms of Lipotoxicity-Driven Insulin Resistance. Int. J. Mol. Sci. 2020, 21, 6358. [Google Scholar] [CrossRef]
- Takaya, M.; Nagao, M.; Takemitsu, S.; Nakajima, Y.; Sugihara, H.; Uchigata, Y.; Oikawa, S. Severe Insulin-resistant Diabetes due to Insulin Antibodies Associated with Eosinophilia. Intern. Med. 2015, 54, 2367–2371. [Google Scholar] [CrossRef] [PubMed]
- Shoelson, S.E.; Lee, J.; Goldfine, A.B. Inflammation and insulin resistance. J. Clin. Investig. 2006, 116, 1793–1801. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.C.; Lee, J. Cellular and molecular players in adipose tissue inflammation in the development of obesity-induced insulin resistance. Biochim. Biophys. Acta 2014, 1842, 446–462. [Google Scholar] [CrossRef]
- Shimobayashi, M.; Albert, V.; Woelnerhanssen, B.; Frei, I.C.; Weissenberger, D.; Meyer-Gerspach, A.C.; Clement, N.; Moes, S.; Colombi, M.; Meier, J.A.; et al. Insulin resistance causes inflammation in adipose tissue. J. Clin. Investig. 2018, 128, 1538–1550. [Google Scholar] [CrossRef]
- Wu, H.; Ballantyne, C.M. Metabolic Inflammation and Insulin Resistance in Obesity. Circ. Res. 2020, 126, 1549–1564. [Google Scholar] [CrossRef]
- Bell, D.S. Protean manifestations of vitamin D deficiency, part 2: Deficiency and its association with autoimmune disease, cancer, infection, asthma, dermopathies, insulin resistance, and type 2 diabetes. South. Med. J. 2011, 104, 335–339. [Google Scholar] [CrossRef]
- Velloso, L.A.; Eizirik, D.L.; Cnop, M. Type 2 diabetes mellitus--an autoimmune disease? Nat. Rev. Endocrinol. 2013, 9, 750–755. [Google Scholar] [CrossRef]
- Lei, Y.; Yang, J.; Li, H.; Zhong, H.; Wan, Q. Changes in glucose-lipid metabolism, insulin resistance, and inflammatory factors in patients with autoimmune thyroid disease. J. Clin. Lab. Anal. 2019, 33, e22929. [Google Scholar] [CrossRef]
- Calco, G.N.; Fryer, A.D.; Nie, Z. Unraveling the connection between eosinophils and obesity. J. Leukoc. Biol. 2020, 108, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.; Jian, T.; Wu, Y.; Zuo, Y.; Li, J.; Lv, H.; Ma, L.; Ren, B.; Zhao, L.; Li, W.; et al. Ellagic acid ameliorates oxidative stress and insulin resistance in high glucose-treated HepG2 cells via miR-223/keap1-Nrf2 pathway. Biomed. Pharmacother. 2019, 110, 85–94. [Google Scholar] [CrossRef]
- Henriksen, E.J.; Diamond-Stanic, M.K.; Marchionne, E.M. Oxidative stress and the etiology of insulin resistance and type 2 diabetes. Free Radic. Biol. Med. 2011, 51, 993–999. [Google Scholar] [CrossRef]
- Oruch, R.; Pryme, I. The biological significance of vitamin A in humans: A review of nutritional aspects and clinical considerations. ScienceJet 2012, 1, 1–13. [Google Scholar]
- Oruch, R.; Pryme, I.; Holmsen, H. GLOBAL JOURNAL OF BIOCHEMISTRY 28 Global Journal of Biochemistry | Volume 2 | Issue 1 | March 2011 The fat soluble antioxidant vitamin E: Its metabolism, and biological and physiological significance. Glob. J. Biochem. 2011, 2, 28–48. [Google Scholar]
- Fazakerley, D.J.; Minard, A.Y.; Krycer, J.R.; Thomas, K.C.; Stockli, J.; Harney, D.J.; Burchfield, J.G.; Maghzal, G.J.; Caldwell, S.T.; Hartley, R.C.; et al. Mitochondrial oxidative stress causes insulin resistance without disrupting oxidative phosphorylation. J. Biol. Chem. 2018, 293, 7315–7328. [Google Scholar] [CrossRef] [PubMed]
- Krycer, J.R.; Elkington, S.D.; Diaz-Vegas, A.; Cooke, K.C.; Burchfield, J.G.; Fisher-Wellman, K.H.; Cooney, G.J.; Fazakerley, D.J.; James, D.E. Mitochondrial oxidants, but not respiration, are sensitive to glucose in adipocytes. J. Biol. Chem. 2020, 295, 99–110. [Google Scholar] [CrossRef]
- Maciejczyk, M.; Zebrowska, E.; Chabowski, A. Insulin Resistance and Oxidative Stress in the Brain: What’s New? Int. J. Mol. Sci. 2019, 20, 874. [Google Scholar] [CrossRef]
- Oruch, R.; Pryme, I.F. Biomedical Importance of Thiamin and Impact on Mitochondrial Machinery. EC Nutr. 2020, 15, 41–51. [Google Scholar]
- Nishikawa, H.; Asai, A.; Fukunishi, S.; Nishiguchi, S.; Higuchi, K. Metabolic Syndrome and Sarcopenia. Nutrients 2021, 13, 3519. [Google Scholar] [CrossRef]
- Sangwung, P.; Petersen, K.F.; Shulman, G.I.; Knowles, J.W. Mitochondrial Dysfunction, Insulin Resistance, and Potential Genetic Implications. Endocrinology 2020, 161, bqaa017. [Google Scholar] [CrossRef] [PubMed]
- Morino, K.; Petersen, K.F.; Shulman, G.I. Molecular mechanisms of insulin resistance in humans and their potential links with mitochondrial dysfunction. Diabetes 2006, 55 (Suppl. 2), S9–S15. [Google Scholar] [CrossRef]
- Gonzalez-Franquesa, A.; Patti, M.E. Insulin Resistance and Mitochondrial Dysfunction. In Mitochondrial Dynamics in Cardiovascular Medicine; Santulli, G., Ed.; Advances in Experimental Medicine and Biology; Springer: Cham, Switzerland, 2017; Volume 982. [Google Scholar] [CrossRef]
- Manucha, W.; Ritchie, B.; Ferder, L. Hypertension and insulin resistance: Implications of mitochondrial dysfunction. Curr. Hypertens. Rep. 2015, 17, 504. [Google Scholar] [CrossRef]
- Jheng, H.F.; Tsai, P.J.; Guo, S.M.; Kuo, L.H.; Chang, C.S.; Su, I.J.; Chang, C.R.; Tsai, Y.S. Mitochondrial fission contributes to mitochondrial dysfunction and insulin resistance in skeletal muscle. Mol. Cell Biol. 2012, 32, 309–319. [Google Scholar] [CrossRef]
- Zorzano, A.; Liesa, M.; Palacin, M. Mitochondrial dynamics as a bridge between mitochondrial dysfunction and insulin resistance. Arch. Physiol. Biochem. 2009, 115, 1–12. [Google Scholar] [CrossRef]
- Montgomery, M.K.; Turner, N. Mitochondrial dysfunction and insulin resistance: An update. Endocr. Connect 2015, 4, R1–R15. [Google Scholar] [CrossRef]
- Park, J.M.; Lee, J.W.; Shim, J.Y.; Lee, Y.J. Relationship Between Platelet Count and Insulin Resistance in Korean Adolescents: A Nationwide Population-Based Study. Metab. Syndr. Relat Disord. 2018, 16, 470–476. [Google Scholar] [CrossRef] [PubMed]
- Basili, S.; Pacini, G.; Guagnano, M.T.; Manigrasso, M.R.; Santilli, F.; Pettinella, C.; Ciabattoni, G.; Patrono, C.; Davi, G. Insulin resistance as a determinant of platelet activation in obese women. J. Am. Coll. Cardiol. 2006, 48, 2531–2538. [Google Scholar] [CrossRef] [PubMed]
- Davi, G.; Guagnano, M.T.; Ciabattoni, G.; Basili, S.; Falco, A.; Marinopiccoli, M.; Nutini, M.; Sensi, S.; Patrono, C. Platelet activation in obese women: Role of inflammation and oxidant stress. JAMA 2002, 288, 2008–2014. [Google Scholar] [CrossRef]
- Taniguchi, A.; Fukushima, M.; Seino, Y.; Sakai, M.; Yoshii, S.; Nagasaka, S.; Yamauchi, I.; Okumura, T.; Nin, K.; Tokuyama, K.; et al. Platelet count is independently associated with insulin resistance in non-obese Japanese type 2 diabetic patients. Metabolism 2003, 52, 1246–1249. [Google Scholar] [CrossRef] [PubMed]
- Schneider, D.J. Factors contributing to increased platelet reactivity in people with diabetes. Diabetes Care 2009, 32, 525–527. [Google Scholar] [CrossRef]
- Sharma, S.; Tripathi, P. Gut microbiome and type 2 diabetes: Where we are and where to go? J. Nutr. Biochem. 2019, 63, 101–108. [Google Scholar] [CrossRef]
- Caricilli, A.M.; Saad, M.J. The role of gut microbiota on insulin resistance. Nutrients 2013, 5, 829–851. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Radjabzadeh, D.; Chen, L.; Kurilshikov, A.; Kavousi, M.; Ahmadizar, F.; Ikram, M.A.; Uitterlinden, A.G.; Zhernakova, A.; Fu, J.; et al. Association of Insulin Resistance and Type 2 Diabetes with Gut Microbial Diversity: A Microbiome-Wide Analysis From Population Studies. JAMA Netw. Open 2021, 4, e2118811. [Google Scholar] [CrossRef] [PubMed]
- Scheithauer, T.P.M.; Rampanelli, E.; Nieuwdorp, M.; Vallance, B.A.; Verchere, C.B.; van Raalte, D.H.; Herrema, H. Gut Microbiota as a Trigger for Metabolic Inflammation in Obesity and Type 2 Diabetes. Front. Immunol. 2020, 11, 571731. [Google Scholar] [CrossRef]
- Shen, J.; Obin, M.S.; Zhao, L. The gut microbiota, obesity and insulin resistance. Mol. Asp. Med. 2013, 34, 39–58. [Google Scholar] [CrossRef] [PubMed]
- La Preze, J.; Robinson, A. Detecting and Managing Drug-Induced Diabetes. US Pharm. 2021, 46, 18–30. [Google Scholar]
- Guest, P.C. Insulin Resistance in Schizophrenia. In Reviews on Biomarker Studies of Metabolic and Metabolism-Related Disorders; Advances in Experimental Medicine and Biology; Guest, P., Ed.; Springer: Cham, Switzerland, 2019; Volume 1134. [Google Scholar] [CrossRef]
- Rajasekaran, A.; Venkatasubramanian, G.; Berk, M.; Debnath, M. Mitochondrial dysfunction in schizophrenia: Pathways, mechanisms and implications. Neurosci. Biobehav. Rev. 2015, 48, 10–21. [Google Scholar] [CrossRef] [PubMed]
- Scaglia, F. The role of mitochondrial dysfunction in psychiatric disease. Dev. Disabil. Res. Rev. 2010, 16, 136–143. [Google Scholar] [CrossRef]
- Oruch, R.; Pryme, I.F.; Lund, A. The Ideal Antipsychotic: Hybrid between Typical “Haloperidol” And the Atypical “Clozapine” Antipsychotic. J. Bioanal. Biomed. 2015, 7, 124–135. [Google Scholar] [CrossRef]
- Li, H.; Peng, S.; Li, S.; Liu, S.; Lv, Y.; Yang, N.; Yu, L.; Deng, Y.H.; Zhang, Z.; Fang, M.; et al. Chronic olanzapine administration causes metabolic syndrome through inflammatory cytokines in rodent models of insulin resistance. Sci. Rep. 2019, 9, 1582. [Google Scholar] [CrossRef] [PubMed]
- Oruch, R.; Pryme, I.; Fasmer, O.; Lund, A. Quetiapine: An Objective Evaluation of Pharmacology, Clinical Uses and Intoxication. EC Pharmacol. Toxicol. 2020, 8, 1–26. [Google Scholar]
- Oruch, R. Psychosis and Antipsychotics: A Short Résumé. Austin J. Pharmacol. Ther. 2014, 2, 3. [Google Scholar]
- Teff, K.L.; Rickels, M.R.; Grudziak, J.; Fuller, C.; Nguyen, H.L.; Rickels, K. Antipsychotic-induced insulin resistance and postprandial hormonal dysregulation independent of weight gain or psychiatric disease. Diabetes 2013, 62, 3232–3240. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Huang, X.F.; Shao, R.; Chen, C.; Deng, C. Molecular Mechanisms of Antipsychotic Drug-Induced Diabetes. Front. Neurosci. 2017, 11, 643. [Google Scholar] [CrossRef]
- Hulbert, A.J.; Else, P.L. Membranes as possible pacemakers of metabolism. J. Theor. Biol. 1999, 199, 257–274. [Google Scholar] [CrossRef]
- Hulbert, A.J.; Turner, N.; Storlien, L.H.; Else, P.L. Dietary fats and membrane function: Implications for metabolism and disease. Biol. Rev. Camb. Philos. Soc. 2005, 80, 155–169. [Google Scholar] [CrossRef] [PubMed]
- Price, E.R.; Sirsat, T.S.; Sirsat, S.K.G.; Curran, T.; Venables, B.J.; Dzialowski, E.M. The membrane pacemaker hypothesis: Novel tests during the ontogeny of endothermy. J. Exp. Biol. 2018, 221, 174466. [Google Scholar] [CrossRef] [PubMed]
- Oruch, R.; Hodneland, E.; Pryme, I.F.; Holmsen, H. In thrombin stimulated human platelets Citalopram, Promethazine, Risperidone, and Ziprasidone, but not Diazepam, may exert their pharmacological effects also through intercalation in membrane phospholipids in a receptor-independent manner. J. Chem. Biol. 2009, 2, 89–103. [Google Scholar] [CrossRef]
- Schirmer, M.A.; Phinney, S.D. Gamma-linolenate reduces weight regain in formerly obese humans. J. Nutr. 2007, 137, 1430–1435. [Google Scholar] [CrossRef] [PubMed]
- Hessvik, N.P.; Bakke, S.S.; Fredriksson, K.; Boekschoten, M.V.; Fjorkenstad, A.; Koster, G.; Hesselink, M.K.; Kersten, S.; Kase, E.T.; Rustan, A.C.; et al. Metabolic switching of human myotubes is improved by n-3 fatty acids. J. Lipid. Res. 2010, 51, 2090–2104. [Google Scholar] [CrossRef]
- Kelley, D.E.; Mandarino, L.J. Fuel selection in human skeletal muscle in insulin resistance: A reexamination. Diabetes 2000, 49, 677–683. [Google Scholar] [CrossRef]
- Aas, V.; Hessvik, N.P.; Wettergreen, M.; Hvammen, A.W.; Hallen, S.; Thoresen, G.H.; Rustan, A.C. Chronic hyperglycemia reduces substrate oxidation and impairs metabolic switching of human myotubes. Biochim. Biophys. Acta 2011, 1812, 94–105. [Google Scholar] [CrossRef]
- Corpeleijn, E.; Mensink, M.; Kooi, M.E.; Roekaerts, P.M.; Saris, W.H.; Blaak, E.E. Impaired skeletal muscle substrate oxidation in glucose-intolerant men improves after weight loss. Obesity 2008, 16, 1025–1032. [Google Scholar] [CrossRef] [PubMed]
- Valkovicova, T.; Skopkova, M.; Stanik, J.; Gasperikova, D. Novel insights into genetics and clinics of the HNF1A-MODY. Endocr. Regul. 2019, 53, 110–134. [Google Scholar] [CrossRef] [PubMed]
- Rudman, N.; Gornik, O.; Lauc, G. Altered N-glycosylation profiles as potential biomarkers and drug targets in diabetes. FEBS Lett. 2019, 593, 1598–1615. [Google Scholar] [CrossRef]
- Haga, Y.; Ishii, K.; Suzuki, T. N-glycosylation is critical for the stability and intracellular trafficking of glucose transporter GLUT4. J. Biol. Chem. 2011, 286, 31320–31327. [Google Scholar] [CrossRef] [PubMed]
- Blot, V.; McGraw, T.E. Molecular mechanisms controlling GLUT4 intracellular retention. Mol. Biol. Cell 2008, 19, 3477–3487. [Google Scholar] [CrossRef]
- Deng, D.; Xu, C.; Sun, P.; Wu, J.; Yan, C.; Hu, M.; Yan, N. Crystal structure of the human glucose transporter GLUT1. Nature 2014, 510, 121–125. [Google Scholar] [CrossRef]
- Wandel, S.; Schurmann, A.; Becker, W.; Summers, S.A.; Shanahan, M.F.; Joost, H.G. Mutation of two conserved arginine residues in the glucose transporter GLUT4 supresses transport activity, but not glucose-inhibitable binding of inhibitory ligands. Naunyn Schmiedebergs Arch. Pharmacol. 1995, 353, 36–41. [Google Scholar] [CrossRef]
- Inzucchi, S.E.; Maggs, D.G.; Spollett, G.R.; Page, S.L.; Rife, F.S.; Walton, V.; Shulman, G.I. Efficacy and metabolic effects of metformin and troglitazone in type II diabetes mellitus. N. Engl. J. Med. 1998, 338, 867–872. [Google Scholar] [CrossRef]
- Contreras-Bolivar, V.; Garcia-Fontana, B.; Garcia-Fontana, C.; Munoz-Torres, M. Mechanisms Involved in the Relationship between Vitamin D and Insulin Resistance: Impact on Clinical Practice. Nutrients 2021, 13, 3491. [Google Scholar] [CrossRef]
- Talaei, A.; Mohamadi, M.; Adgi, Z. The effect of vitamin D on insulin resistance in patients with type 2 diabetes. Diabetol. Metab. Syndr. 2013, 5, 8. [Google Scholar] [CrossRef]
- Lemieux, P.; Weisnagel, S.J.; Caron, A.Z.; Julien, A.S.; Morisset, A.S.; Carreau, A.M.; Poirier, J.; Tchernof, A.; Robitaille, J.; Bergeron, J.; et al. Effects of 6-month vitamin D supplementation on insulin sensitivity and secretion: A randomised, placebo-controlled trial. Eur. J. Endocrinol. 2019, 181, 287–299. [Google Scholar] [CrossRef]
- Hart, P.A.; Bradley, D.; Conwell, D.L.; Dungan, K.; Krishna, S.G.; Wyne, K.; Bellin, M.D.; Yadav, D.; Andersen, D.K.; Serrano, J.; et al. Diabetes following acute pancreatitis. Lancet Gastroenterol. Hepatol. 2021, 6, 668–675. [Google Scholar] [CrossRef] [PubMed]
- Li, D. Diabetes and pancreatic cancer. Mol. Carcinog. 2012, 51, 64–74. [Google Scholar] [CrossRef]
- Govender, N.; Khaliq, O.P.; Moodley, J.; Naicker, T. Insulin resistance in COVID-19 and diabetes. Prim. Care Diabetes 2021, 15, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Drucker, D.J. Coronavirus Infections and Type 2 Diabetes-Shared Pathways with Therapeutic Implications. Endocr. Rev. 2020, 41, 457–470. [Google Scholar] [CrossRef]
- Yang, L.; Han, Y.; Nilsson-Payant, B.E.; Gupta, V.; Wang, P.; Duan, X.; Tang, X.; Zhu, J.; Zhao, Z.; Jaffre, F.; et al. A Human Pluripotent Stem Cell-Based Platform to Study SARS-CoV-2 Tropism and Model Virus Infection in Human Cells and Organoids. Cell Stem. Cell 2020, 27, 125–136.e7. [Google Scholar] [CrossRef] [PubMed]
- Borghouts, L.B.; Keizer, H.A. Exercise and insulin sensitivity: A review. Int. J. Sports Med. 2000, 21, 1–12. [Google Scholar] [CrossRef]
- Shepherd, P.R.; Kahn, B.B. Glucose transporters and insulin action--implications for insulin resistance and diabetes mellitus. N. Engl. J. Med. 1999, 341, 248–257. [Google Scholar] [CrossRef]
- Janbozorgi, N.; Allipour, R.; Djafarian, K.; Shab-Bidar, S.; Badeli, M.; Safabakhsh, M. Water intake and risk of type 2 diabetes: A systematic review and meta-analysis of observational studies. Diabetes Metab. Syndr. 2021, 15, 102156. [Google Scholar] [CrossRef]
- Emanuele, N.V.; Swade, T.F.; Emanuele, M.A. Consequences of alcohol use in diabetics. Alcohol Health Res. World 1998, 22, 211–219. [Google Scholar] [PubMed]
- Sedaghat, G.; Montazerifar, F.; Keykhaie, M.A.; Karajibani, M.; Shourestani, S.; Dashipour, A. Effect of pre-meal water intake on the serum levels of Copeptin, glycemic control, lipid profile and anthropometric indices in patients with type 2 diabetes mellitus: A randomized, controlled trial. J. Diabetes Metab. Disord 2021, 20, 171–177. [Google Scholar] [CrossRef]
- Vanhaecke, T.; Perrier, E.T.; Melander, O. A Journey through the Early Evidence Linking Hydration to Metabolic Health. Ann. Nutr. Metab. 2020, 76 (Suppl. 1), 4–9. [Google Scholar] [CrossRef] [PubMed]
- Enhorning, S.; Brunkwall, L.; Tasevska, I.; Ericson, U.; Persson Tholin, J.; Persson, M.; Lemetais, G.; Vanhaecke, T.; Dolci, A.; Perrier, E.T.; et al. Water Supplementation Reduces Copeptin and Plasma Glucose in Adults with High Copeptin: The H2O Metabolism Pilot Study. J. Clin. Endocrinol. Metab. 2019, 104, 1917–1925. [Google Scholar] [CrossRef]
- Roussel, R.; Fezeu, L.; Bouby, N.; Balkau, B.; Lantieri, O.; Alhenc-Gelas, F.; Marre, M.; Bankir, L.; Group, D.E.S.I.R.S. Low water intake and risk for new-onset hyperglycemia. Diabetes Care 2011, 34, 2551–2554. [Google Scholar] [CrossRef]
- Ni, Y.; Nagashimada, M.; Zhan, L.; Nagata, N.; Kobori, M.; Sugiura, M.; Ogawa, K.; Kaneko, S.; Ota, T. Prevention and reversal of lipotoxicity-induced hepatic insulin resistance and steatohepatitis in mice by an antioxidant carotenoid, beta-cryptoxanthin. Endocrinology 2015, 156, 987–999. [Google Scholar] [CrossRef] [PubMed]
- Salvatore, T.; Pafundi, P.C.; Morgillo, F.; Di Liello, R.; Galiero, R.; Nevola, R.; Marfella, R.; Monaco, L.; Rinaldi, L.; Adinolfi, L.E.; et al. Metformin: An old drug against old age and associated morbidities. Diabetes Res. Clin. Pract. 2020, 160, 108025. [Google Scholar] [CrossRef]
- Salvatore, T.; Pafundi, P.C.; Galiero, R.; Rinaldi, L.; Caturano, A.; Vetrano, E.; Aprea, C.; Albanese, G.; Di Martino, A.; Ricozzi, C.; et al. Can Metformin Exert as an Active Drug on Endothelial Dysfunction in Diabetic Subjects? Biomedicines 2020, 9, 3. [Google Scholar] [CrossRef]
- Sasso, F.C.; Carbonara, O.; Cozzolino, D.; Rambaldi, P.; Mansi, L.; Torella, D.; Gentile, S.; Turco, S.; Torella, R.; Salvatore, T. Effects of insulin-glucose infusion on left ventricular function at rest and during dynamic exercise in healthy subjects and noninsulin dependent diabetic patients: A radionuclide ventriculographic study. J. Am. Coll. Cardiol. 2000, 36, 219–226. [Google Scholar] [CrossRef]
| Foodstuff and GI | Examples of Food |
|---|---|
| Food with a low GI range (55 or less) | Monosaccharides: fructose; tagatose. Pulses (beans): black; kidney; lentil; chickpea; pinto. Seeds (small): sesame; flax; sunflower; poppy; pumpkin; hemp. Nuts: walnuts; cashew; peanuts. Grains: wheat (durum, spelt, kamut); millet; oat; rye; rice; barley. Sweet fruits: peaches; strawberries; mangos. Vegetables: most vegetables; unpeeled sweet potatoes and mushrooms. |
| Food with medium GI ranges (56–69) | Table sugar; regular ice cream; cranberry juice; grape juice. Enriched whole wheat; basmati rice; unpeeled potatoes; peeled sweet potatoes; pita bread. Raisins; prunes; pumpernickel bread. |
| Food with high GI ranges (70 and above) | Sugars: glucose: dextrose; grape sugar; high fructose corn syrup; maltose; maltodextrins. White bread (from endosperm). Most white rice (from endosperm). Peeled potatoes Extruded breakfast cereals; corn flakes. |
| Parameter | Physiological Function | Improper Function/Decrease in Insulin |
|---|---|---|
| Glucose | Stimulates glucose uptake via insertion of GLUT4 in the membranes of myocytes and lipocytes. | Increase in blood glucose concentration. |
| Triglycerols (fat) | Increases lipogenesis by forcing lipocytes to take in glucose. | Decrease in lipogenesis and hyperglycemia. |
| Fatty acids | Increased esterification to triglycerides (neutral lipids). | Lipolysis of triglycerides to fatty acids and glycerol. |
| Lipolysis | Decreases lipolysis and decreases free fatty acid and glycerol in the circulation. | Hyperlipidemia |
| Glycogen | Induces glycogen synthesis, by activation of the hexokinase that activates glucose by adding a phosphate, a process that traps glucose inside the cell. | Inhibits glycogen synthesis by reverse steps that induce glycogen synthesis. |
| Inhibits glucose-6-phosphatase, which dephosphorylates glucose. | ||
| Activates both phosphofructokinase and glycogen synthase, which are responsible for glycogen synthesis. | ||
| Gluconeogenesis and glycogenolysis | Decreases these two processes by decreasing glucose synthesis from noncarbohydrate biomolecules mainly in the liver. | Gluconeogenesis in the liver from diverse substrate biomolecules. |
| Protein | Decreases protein breakdown | Proteolysis is eased, as is the case in advanced cases of diabetes. |
| Autophagy | Deceleration of degradation of damaged organelles. | Autophagy is accelerated. |
| Arterial muscle tone | Increases this, especially arterioles and micro-arteries, and thus increases blood flow. | Reduces blood flow in these by allowing muscles to contract. |
| Gastric chlorhydria | Increases hydrochloric acid secretion by the gastric parietal cells. | T he occurrence of the reverse process is expected. |
| Potassium uptake | Forces glycogen-synthesizing cells to absorb potassium with water from the extracellular fluids via translocation of the Na+/K+-ATPase to the membranes of skeletal myocytes. | Inhibits potassium absorption. |
| Renal sodium excretion | Decreases excretion of renal sodium. | The reverse process occurs. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aedh, A.I.; Alshahrani, M.S.; Huneif, M.A.; Pryme, I.F.; Oruch, R. A Glimpse into Milestones of Insulin Resistance and an Updated Review of Its Management. Nutrients 2023, 15, 921. https://doi.org/10.3390/nu15040921
Aedh AI, Alshahrani MS, Huneif MA, Pryme IF, Oruch R. A Glimpse into Milestones of Insulin Resistance and an Updated Review of Its Management. Nutrients. 2023; 15(4):921. https://doi.org/10.3390/nu15040921
Chicago/Turabian StyleAedh, Abdullah I., Majed S. Alshahrani, Mohammed A. Huneif, Ian F. Pryme, and Ramadhan Oruch. 2023. "A Glimpse into Milestones of Insulin Resistance and an Updated Review of Its Management" Nutrients 15, no. 4: 921. https://doi.org/10.3390/nu15040921
APA StyleAedh, A. I., Alshahrani, M. S., Huneif, M. A., Pryme, I. F., & Oruch, R. (2023). A Glimpse into Milestones of Insulin Resistance and an Updated Review of Its Management. Nutrients, 15(4), 921. https://doi.org/10.3390/nu15040921




