Parkinson Symptom Severity and Use of Nutraceuticals
Abstract
1. Introduction
2. Materials and Methods
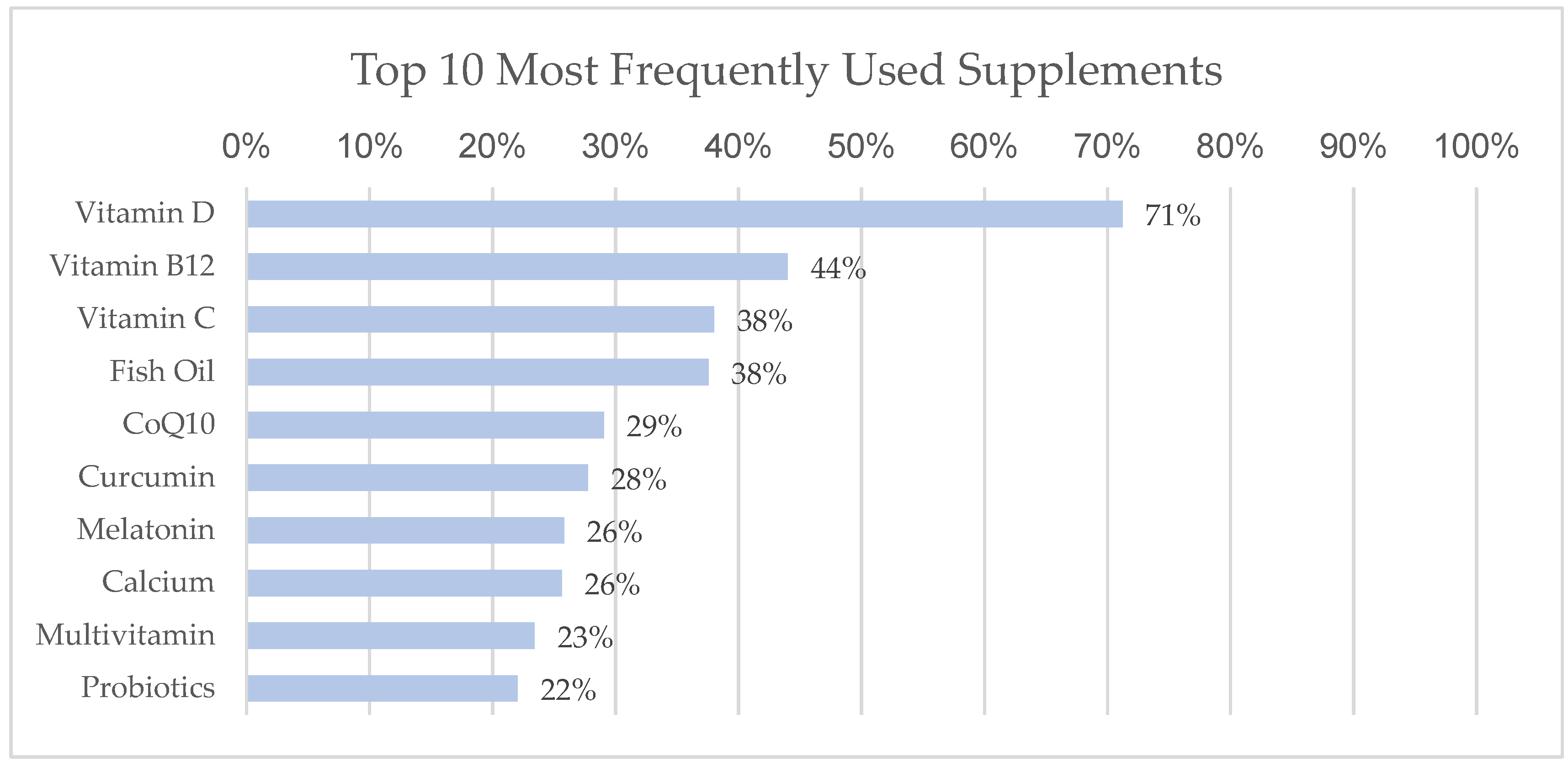
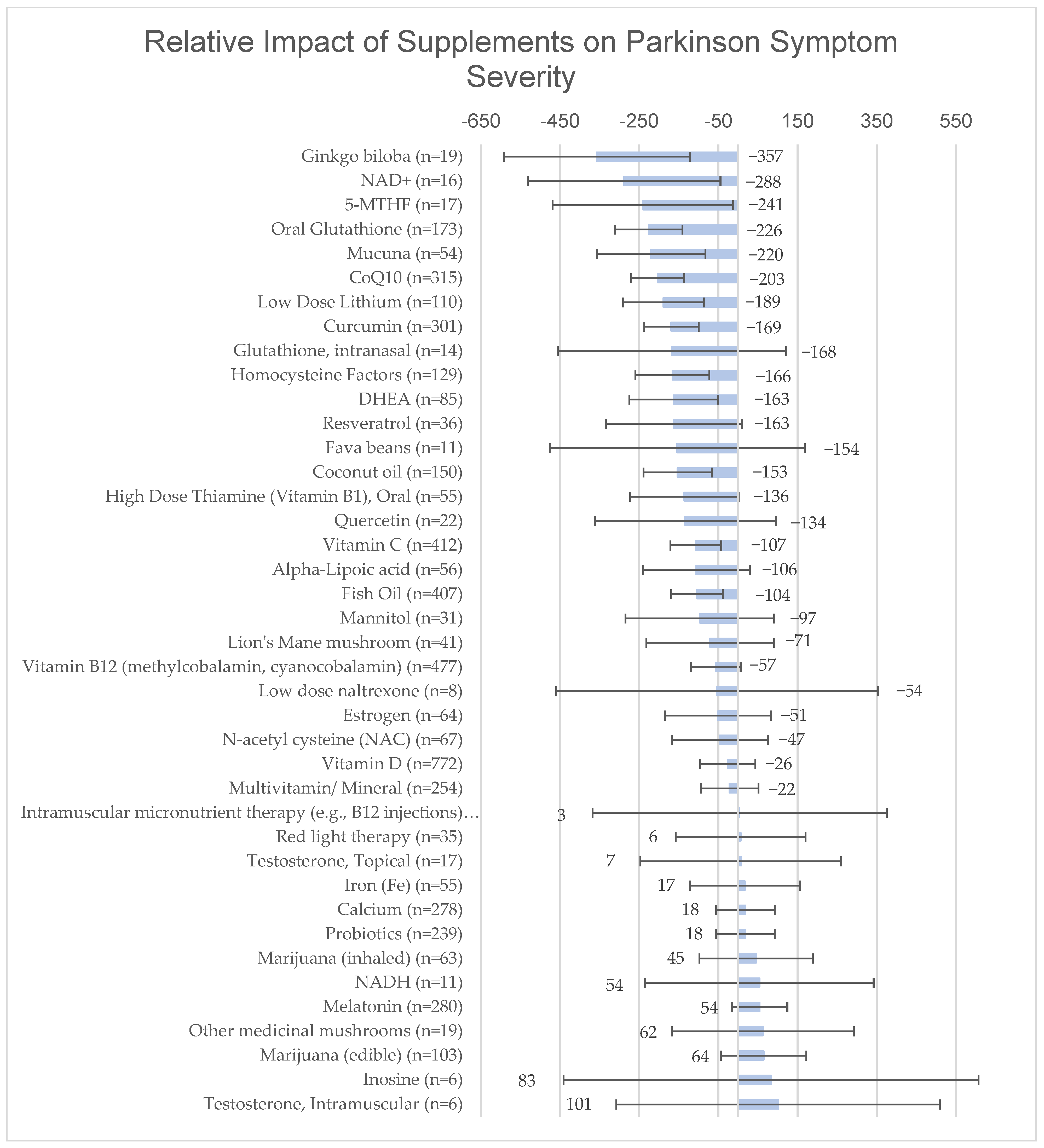
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Santini, A.; Novellino, E. To Nutraceuticals and Back: Rethinking a Concept. Foods 2017, 6, 74. [Google Scholar] [CrossRef] [PubMed]
- Dietary Supplement Health and Education Act of 1994. Available online: https://www.fda.gov/food/information-consumers-using-dietary-supplements/questions-and-answers-dietary-supplements#:~:text=A%20dietary%20supplement%20is%20a,intended%20to%20supplement%20the%20diet (accessed on 1 December 2022).
- DeFelice, S.L. The nutraceutical revolution: Its impact on food industry R&D. Trends Food Sci. Technol. 1995, 6, 59–61. [Google Scholar]
- Dietary Supplements Market Size, Share & Trends Analysis Report by Ingredient (Vitamins, Minerals), by Form, by Application, by End User, by Distribution Channel, by Region, and Segment Forecasts, 2022–2030; Market Analysis Report; Grand View Research, 2020; p. 200. Available online: https://www.researchandmarkets.com/reports/4479727/dietary-supplements-market-size-share-and-trends (accessed on 1 December 2022).
- Dietary Supplements Market Size, Share & COVID-19 Impact Analysis, by Type (Vitamins, Minerals, Enzymes, Fatty Acids, Proteins, and Others), Form (Tablets, Capsules, Liquids, and Powders), and REgional Forecasts, 2021–2028; Market Research Report; 2022; p. 130. Available online: https://www.fortunebusinessinsights.com/dietary-supplements-market-102082 (accessed on 1 December 2022).
- Davis, D.R.; Epp, M.D.; Riordan, H.D. Changes in USDA food composition data for 43 garden crops, 1950 to 1999. J. Am. Coll. Nutr. 2004, 23, 669–682. [Google Scholar] [CrossRef]
- Darmon, N.; Darmon, M.; Maillot, M.; Drewnowski, A. A nutrient density standard for vegetables and fruits: Nutrients per calorie and nutrients per unit cost. J. Am. Diet. Assoc. 2005, 105, 1881–1887. [Google Scholar] [CrossRef] [PubMed]
- Kantor, E.D.; Rehm, C.D.; Du, M.; White, E.; Giovannucci, E.L. Trends in Dietary Supplement Use among US Adults from 1999–2012. JAMA 2016, 316, 1464–1474. [Google Scholar] [CrossRef] [PubMed]
- Rajendran, P.R.; Thompson, R.E.; Reich, S.G. The use of alternative therapies by patients with Parkinson’s disease. Neurology 2001, 57, 790–794. [Google Scholar] [CrossRef]
- Calfio, C.; Gonzalez, A.; Singh, S.K.; Rojo, L.E.; Maccioni, R.B. The Emerging Role of Nutraceuticals and Phytochemicals in the Prevention and Treatment of Alzheimer’s Disease. J. Alzheimers Dis. 2020, 77, 33–51. [Google Scholar] [CrossRef] [PubMed]
- Poti, F.; Santi, D.; Spaggiari, G.; Zimetti, F.; Zanotti, I. Polyphenol Health Effects on Cardiovascular and Neurodegenerative Disorders: A Review and Meta-Analysis. Int. J. Mol. Sci. 2019, 20, 351. [Google Scholar] [CrossRef] [PubMed]
- Karunaratne, T.B.; Okereke, C.; Seamon, M.; Purohit, S.; Wakade, C.; Sharma, A. Niacin and Butyrate: Nutraceuticals Targeting Dysbiosis and Intestinal Permeability in Parkinson’s Disease. Nutrients 2020, 13, 28. [Google Scholar] [CrossRef]
- The Parkinson Study Group QE3 Investigators; Beal, M.F.; Oakes, D.; Shoulson, I.; Henchcliffe, C.; Galpern, W.R.; Haas, R.; Juncos, J.L.; Nutt, J.G.; Voss, T.S.; et al. A randomized clinical trial of high-dosage coenzyme Q10 in early Parkinson disease: No evidence of benefit. JAMA Neurol. 2014, 71, 543–552. [Google Scholar] [CrossRef]
- Investigators, N.N.-P. A randomized clinical trial of coenzyme Q10 and GPI-1485 in early Parkinson disease. Neurology 2007, 68, 20–28. [Google Scholar] [CrossRef]
- Shults, C.W.; Flint Beal, M.; Song, D.; Fontaine, D. Pilot trial of high dosages of coenzyme Q10 in patients with Parkinson’s disease. Exp. Neurol. 2004, 188, 491–494. [Google Scholar] [CrossRef] [PubMed]
- Bender, A.; Koch, W.; Elstner, M.; Schombacher, Y.; Bender, J.; Moeschl, M.; Gekeler, F.; Muller-Myhsok, B.; Gasser, T.; Tatsch, K.; et al. Creatine supplementation in Parkinson disease: A placebo-controlled randomized pilot trial. Neurology 2006, 67, 1262–1264. [Google Scholar] [CrossRef] [PubMed]
- Investigators, N.N.-P. A randomized, double-blind, futility clinical trial of creatine and minocycline in early Parkinson disease. Neurology 2006, 66, 664–671. [Google Scholar] [CrossRef] [PubMed]
- Hauser, R.A.; Lyons, K.E.; McClain, T.; Carter, S.; Perlmutter, D. Randomized, double-blind, pilot evaluation of intravenous glutathione in Parkinson’s disease. Mov. Disord. 2009, 24, 979–983. [Google Scholar] [CrossRef]
- Mischley, L.K.; Lau, R.C.; Shankland, E.G.; Wilbur, T.K.; Padowski, J.M. Phase IIb Study of Intranasal Glutathione in Parkinson’s Disease. J. Park. Dis. 2017, 7, 289–299. [Google Scholar] [CrossRef] [PubMed]
- Mischley, L.K.; Leverenz, J.B.; Lau, R.C.; Polissar, N.L.; Neradilek, M.B.; Samii, A.; Standish, L.J. A randomized, double-blind phase I/IIa study of intranasal glutathione in Parkinson’s disease. Mov. Disord. 2015, 30, 1696–1701. [Google Scholar] [CrossRef]
- Monti, D.A.; Zabrecky, G.; Kremens, D.; Liang, T.W.; Wintering, N.A.; Bazzan, A.J.; Zhong, L.; Bowens, B.K.; Chervoneva, I.; Intenzo, C.; et al. N-Acetyl Cysteine Is Associated With Dopaminergic Improvement in Parkinson’s Disease. Clin. Pharmacol. Ther. 2019, 106, 884–890. [Google Scholar] [CrossRef]
- Brakedal, B.; Dölle, C.; Riemer, F.; Ma, Y.; Nido, G.S.; Skeie, G.O.; Craven, A.R.; Schwarzlmüller, T.; Brekke, N.; Diab, J.; et al. The NADPARK study: A randomized phase I trial of nicotinamide riboside supplementation in Parkinson’s disease. Cell Metab. 2022, 34, 396–407.e6. [Google Scholar] [CrossRef]
- Mischley, L.K.; Lau, R.C.; Bennett, R.D. Role of Diet and Nutritional Supplements in Parkinson’s Disease Progression. Oxid. Med. Cell. Longev. 2017, 2017, 6405278. [Google Scholar] [CrossRef]
- Mischley, L.K.; Lau, R.C.; Weiss, N.S. Use of a self-rating scale of the nature and severity of symptoms in Parkinson’s Disease (PRO-PD): Correlation with quality of life and existing scales of disease severity. NPJ Park. Dis. 2017, 3, 20. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef] [PubMed]
- Giardini, M.; Nardone, A.; Godi, M.; Guglielmetti, S.; Arcolin, I.; Pisano, F.; Schieppati, M. Instrumental or Physical-Exercise Rehabilitation of Balance Improves Both Balance and Gait in Parkinson’s Disease. Neural Plast. 2018, 2018, 5614242. [Google Scholar] [CrossRef] [PubMed]
- Ambrosio, L.; Portillo, M.C.; Rodriguez-Blazquez, C.; Rojo, J.M.; Martinez-Martin, P.; EC-PC Validation Group; Violante, M.R.; Castrillo, J.C.M.; Arillo, V.C.; Garretto, N.S.; et al. Influencing factors when living with Parkinson’s disease: A cross-sectional study. J. Clin. Nurs. 2019, 28, 3168–3176. [Google Scholar] [CrossRef]
- Avallone, R.; Vitale, G.; Bertolotti, M. Omega-3 Fatty Acids and Neurodegenerative Diseases: New Evidence in Clinical Trials. Int. J. Mol. Sci. 2019, 20, 4256. [Google Scholar] [CrossRef]
- Kocot, J.; Luchowska-Kocot, D.; Kiełczykowska, M.; Musik, I.; Kurzepa, J. Does Vitamin C Influence Neurodegenerative Diseases and Psychiatric Disorders? Nutrients 2017, 9, 659. [Google Scholar] [CrossRef]
- Deepika, N.P.; Kondengadan, M.S.; Sweilam, S.H.; Rahman, M.H.; Muhasina, K.M.; Ghosh, P.; Bhargavi, D.; Palati, D.J.; Maiz, F.; Duraiswamy, B. Neuroprotective role of coconut oil for the prevention and treatment of Parkinson’s disease: Potential mechanisms of action. Biotechnol. Genet. Eng. Rev. 2022, 1–33. [Google Scholar] [CrossRef]
- Choe, M.A.; An, G.J.; Koo, B.S.; Jeon, S. Effect of DHEA on recovery of muscle atrophy induced by Parkinson’s disease. J. Korean Acad. Nurs. 2011, 41, 834–842. [Google Scholar] [CrossRef]
- Shen, L. Associations between B Vitamins and Parkinson’s Disease. Nutrients 2015, 7, 7197–7208. [Google Scholar] [CrossRef]
- Rabiei, Z.; Solati, K.; Amini-Khoei, H. Phytotherapy in treatment of Parkinson’s disease: A review. Pharm. Biol. 2019, 57, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Lazzara, C.A.; Kim, Y.H. Potential application of lithium in Parkinson’s and other neurodegenerative diseases. Front. Neurosci. 2015, 9, 403. [Google Scholar] [CrossRef] [PubMed]
- Pradhan, N.; Singh, C.; Singh, A. Coenzyme Q10 a mitochondrial restorer for various brain disorders. Naunyn Schmiedebergs Arch. Pharmacol. 2021, 394, 2197–2222. [Google Scholar] [CrossRef]
- Fong, C.S.; Shyu, H.Y.; Shieh, J.C.; Fu, Y.P.; Chin, T.Y.; Wang, H.W.; Cheng, C.W. Association of MTHFR, MTR, and MTRR polymorphisms with Parkinson’s disease among ethnic Chinese in Taiwan. Clin. Chim. Acta 2011, 412, 332–338. [Google Scholar] [CrossRef]
- Rennie, G.; Chen, A.C.; Dhillon, H.; Vardy, J.; Damian, D.L. Nicotinamide and neurocognitive function. Nutr. Neurosci. 2015, 18, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Patro-Gołąb, B.; Szajewska, H. Strengths and weaknesses of observational nutritional studies. World Rev. Nutr. Diet. 2013, 108, 11–17. [Google Scholar] [CrossRef]
| Idiopathic PD n = 1084 | |
|---|---|
| Mean age (SD) | 66.6 (8.62) |
| Years since diagnosis (SD) | 7.8 (5.41) |
| Gender | |
| Male | 400 (36.9%) |
| Female | 593 (54.7%) |
| Other/Not answered | 91 (8.4%) |
| Hoen & Yahr Stage | |
| 1: unilateral only | 441 (40.7%) |
| 2: bilateral, good balance | 252 (23.2%) |
| 3: postural instability | 275 (25.4%) |
| 4: severe disability, independent | 56 (5.2%) |
| 5: wheelchair/bed, dependent | 7 (0.6%) |
| Don’t know/unspecified | 53 (4.9%) |
| Income | |
| <$20K | 46 (4.2%) |
| $20–40K | 80 (7.4%) |
| $40–60K | 140 (12.9%) |
| $60–80K | 161 (14.9%) |
| $80–100K | 126 (11.6%) |
| $100–150K | 167 (15.4%) |
| >$150K | 208 (19.2%) |
| Not answered | 156 (14.4%) |
| Education | |
| Less than 8th grade | 1 (0.1%) |
| Grades 9–11 | 6 (0.6%) |
| Completed high school/GED | 88 (8.1%) |
| Technical school | 49 (4.5%) |
| Associate degree | 67 (6.2%) |
| Bachelor’s degree | 272 (25.1%) |
| Graduate/Professional degree | 507 (46.8%) |
| Not answered | 94 (8.7%) |
| Race/Ethnicity | |
| Caucasian | 306 (91.6%) |
| Black | 3 (0.9%) |
| Hispanic | 5 (1.5%) |
| Native American | 1 (0.3%) |
| Asian/Pacific Islander | 11 (3.3%) |
| Other | 3 (0.9%) |
| N/A | 5 (1.5%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mischley, L.K.; Farahnik, J.; Mantay, L.; Punzi, J.; Szampruch, K.; Ferguson, T.; Fox, D.J. Parkinson Symptom Severity and Use of Nutraceuticals. Nutrients 2023, 15, 802. https://doi.org/10.3390/nu15040802
Mischley LK, Farahnik J, Mantay L, Punzi J, Szampruch K, Ferguson T, Fox DJ. Parkinson Symptom Severity and Use of Nutraceuticals. Nutrients. 2023; 15(4):802. https://doi.org/10.3390/nu15040802
Chicago/Turabian StyleMischley, Laurie K., Joshua Farahnik, Ludwig Mantay, Jamie Punzi, Kayla Szampruch, Tyrice Ferguson, and Devon J. Fox. 2023. "Parkinson Symptom Severity and Use of Nutraceuticals" Nutrients 15, no. 4: 802. https://doi.org/10.3390/nu15040802
APA StyleMischley, L. K., Farahnik, J., Mantay, L., Punzi, J., Szampruch, K., Ferguson, T., & Fox, D. J. (2023). Parkinson Symptom Severity and Use of Nutraceuticals. Nutrients, 15(4), 802. https://doi.org/10.3390/nu15040802






