Added Sugar Consumption in Spanish Children (7–12 y) and Nutrient Density of Foods Contributing to Such Consumption: An Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Study Population
2.2. Data Collection Instrument and Study Variables
2.3. Estimation of the Intake of Added Sugars
2.4. Calculation of Nutritional Density Indexes
2.5. Statistical Analysis
3. Results
3.1. Description of the Study Population
3.2. Consumption of Added Sugars
3.3. Parents’ Quality Perception
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 10 January 2023).
- Caballero, B. Humans against Obesity: Who Will Win? Adv. Nutr. 2019, 10, S4–S9. [Google Scholar] [CrossRef] [PubMed]
- García-Solano, M.; Gutiérrez-González, E.; López-Sobaler, A.M.; Ruiz-Álvarez, M.; Bermejo López, L.M.; Aparicio, A.; Dal Re Saavedra, M.Á. Situación ponderal de la población escolar de 6 a 9 años en España: Resultados del estudio ALADINO 2019. Nutr. Hosp. 2021, 38, 943–953. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guideline: Sugars Intake for Adults and Children; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Blüher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef] [PubMed]
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development; United Nations: New York, NY, USA, 2016. [Google Scholar]
- FAO; WHO. Rome Declaration on Nutrition; FAO: Rome, Italy; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- World Health Organization. Report of the Commission on Ending Childhood Obesity; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- World Health Organization. Healthy Diet. Available online: https://www.who.int/es/news-room/fact-sheets/detail/healthy-diet (accessed on 10 January 2022).
- EFSA Panel on Nutrition, Novel Foods and Food Allergens (NDA); Turck, D.; Bohn, T.; Castenmiller, J.; de Henauw, S.; Hirsch-Ernst, K.I.; Knutsen, H.K.; Maciuk, A.; Mangelsdorf, I.; McArdle, H.J.; et al. Tolerable upper intake level for dietary sugars. EFSA J. 2022, 20, e07074. [Google Scholar]
- Gil, Á.U.R.; Varela-Moreiras, G. Posicionamiento sobre la deinición de azúcares añadidos y su declaración en el etiquetado de los productos alimenticios en España. Nutr. Hosp. 2021, 38, 645–660. [Google Scholar] [CrossRef]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef]
- Clarys, P.; Deliens, T.; Huybrechts, I.; Deriemaeker, P.; Vanaelst, B.; De Keyzer, W.; Hebbelinck, M.; Mullie, P. Comparison of Nutritional Quality of the Vegan, Vegetarian, Semi-Vegetarian, Pesco-Vegetarian and Omnivorous Diet. Nutrients 2014, 6, 1318–1332. [Google Scholar] [CrossRef]
- Sprake, E.F.; Russell, J.M.; Cecil, J.E.; Cooper, R.J.; Grabowski, P.; Pourshahidi, L.K.; Barker, M.E. Dietary patterns of university students in the UK: A cross-sectional study. Nutr. J. 2018, 17, 90. [Google Scholar] [CrossRef]
- Bradbury, K.E.; Murphy, N.; Key, T.J. Diet and colorectal cancer in UK Biobank: A prospective study. Int. J. Epidemiol. 2019, 49, 246–258. [Google Scholar] [CrossRef]
- Robinson, E.; Boyland, E.; Chisholm, A.; Harrold, J.; Maloney, N.G.; Marty, L.; Mead, B.R.; Noonan, R.; Hardman, C.A. Obesity, eating behavior and physical activity during COVID-19 lockdown: A study of UK adults. Appetite 2021, 156, 104853. [Google Scholar] [CrossRef]
- Moser, C.; Kalton, G. Survey Methods in Social Investigation; Routledge: London, UK, 2017; Volume 9. [Google Scholar] [CrossRef]
- Ruiz-López, M.D.; de Martínez Victoria, E.; Gil, A. Guía Fotográfica de Porciones de Alimentos Consumidos en España; Fundación Iberoamericana de Nutrición: Granada, Spain, 2019. [Google Scholar]
- AESAN. Base de Datos Española de Composición de Alimentos, Version 1.0; AESAN: Madrid, Spain, 2010. [Google Scholar]
- EFSA. Dietary Reference Values for Nutrients Summary Report; EFSA: Parma, Italy, 2017. [Google Scholar] [CrossRef]
- Agnoli, C.; Baroni, L.; Bertini, I.; Ciappellano, S.; Fabbri, A.; Papa, M.; Pellegrini, N.; Sbarbati, R.; Scarino, M.L.; Siani, V.; et al. Position paper on vegetarian diets from the working group of the Italian Society of Human Nutrition. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 1037–1052. [Google Scholar] [CrossRef] [PubMed]
- Beal, T.; Ortenzi, F. Priority Micronutrient Density in Foods. Front. Nutr. 2022, 9, 379. [Google Scholar] [CrossRef] [PubMed]
- Rumbold, P.; McCullogh, N.; Boldon, R.; Haskell-Ramsay, C.; James, L.; Stevenson, E.; Green, B. The potential nutrition-, physical- and health-related benefits of cow’s milk for primary-school-aged children. Nutr. Res. Rev. 2022, 35, 50–69. [Google Scholar] [CrossRef] [PubMed]
- Palma-Morales, M.; Mateos, A.; Rodríguez, J.; Casuso, R.A.; Huertas, J.R. Food made us human: Recent genetic variability and its relevance to the current distribution of macronutrients. Nutrition 2022, 101, 111702. [Google Scholar] [CrossRef] [PubMed]
- Babio, N.; Mena-Sánchez, G.; Salas-Salvadó, J. Más allá del valor nutricional del yogur: ¿un indicador de la calidad de la dieta? Nutr. Hosp. 2017, 34, 26–30. [Google Scholar] [CrossRef]
- Redruello-Requejo, M.; Samaniego-Vaesken, M.d.L.; Partearroyo, T.; Rodríguez-Alonso, P.; Soto-Méndez, M.J.; Hernández-Ruiz, Á.; Villoslada, F.L.; Leis, R.; Martínez de Victoria, E.; Moreno, J.M.; et al. Dietary Intake of Individual (Intrinsic and Added) Sugars and Food Sources from Spanish Children Aged One to <10 Years—Results from the EsNuPI Study. Nutrients 2022, 14, 1667. [Google Scholar] [CrossRef]
- Fundación Española de la Nutrición (FEN). Hábitos de Consumo de Bebidas y su Asociación con la Ingesta Total de Agua y de Energía en la Población Española: Resultados del Estudio Científico; ANIBES: 2015; FEN: Madrid, Spain, 2015. [Google Scholar]
- Lien, D.T.K.; Nhung, B.T.; Khan, N.C.; Hop, L.T.; Nga, N.T.Q.; Hung, N.T.; Kiers, J.; Shigeru, Y.; te Biesebeke, R. Impact of Milk Consumption on Performance and Health of Primary School Children in Rural Vietnam. Asia Pac. J. Clin. Nutr. 2009, 18, 326–334. [Google Scholar] [CrossRef]
- Kavezade, S.; Mozaffari-Khosravi, H.; Aflatoonian, M.; Asemi, M.; Mehrabani, S.; Salehi-Abargouei, A. The effects of whole milk compared to skim milk and apple juice consumption in breakfast on appetite and energy intake in obese children: A three-way randomized crossover clinical trial. BMC Nutr. 2018, 4, 44. [Google Scholar] [CrossRef]
- Mehrabani, S.; Safavi, S.M.; Mehrabani, S.; Asemi, M.; Feizi, A.; Bellissimo, N.; Salehi-Abargouei, A. Effects of low-fat milk consumption at breakfast on satiety and short-term energy intake in 10- to 12-year-old obese boys. Eur. J. Nutr. 2016, 55, 1389–1396. [Google Scholar] [CrossRef]
- Mehrabani, S.; Salehi-Abargouei, A.; Asemi, M.; Mehrabani, S.; Feizi, A.; Safavi, S.M. Effect of Low-fat Milk Consumption Compared to Apple Juice and Water on the Energy Intake Among 10-12-Year-Old Obese Boys: A Three-way Cross-over Clinical Trial. Int. J. Prev. Med. 2014, 5, 1405–1411. [Google Scholar]
- Rumbold, P.; Reynolds, C.; Stevenson, E. Informing Primary School Nutritional Policy: Effects of Mid-Morning Snacks on Appetite and Energy Control. Food Nutr. Sci. 2013, 4, 529–537. [Google Scholar] [CrossRef]
- Vien, S.; Patel, B.; Panahi, S.; El Khoury, D.; Luhovyy, B.; Hamilton, J.; Anderson, G. The effect of fluid dairy products on food intake, glycemic and appetite hormone responses in children (120.3). FASEB J. 2014, 28, 120–123. [Google Scholar] [CrossRef]
- Cuadrado-Soto, E.; López-Sobaler, A.M.; Jiménez-Ortega, A.I.; Aparicio, A.; Bermejo, L.M.; Hernández-Ruiz, Á.; Lara Villoslada, F.; Leis, R.; Martínez de Victoria, E.; Moreno, J.M.; et al. Usual Dietary Intake, Nutritional Adequacy and Food Sources of Calcium, Phosphorus, Magnesium and Vitamin D of Spanish Children Aged One to <10 Years. Findings from the EsNuPI Study. Nutrients 2020, 12, 1787. [Google Scholar] [CrossRef] [PubMed]
- Cifelli, C.J.; Agarwal, S.; Fulgoni, V.L. Association of Yogurt Consumption with Nutrient Intakes, Nutrient Adequacy, and Diet Quality in American Children and Adults. Nutrients 2020, 12, 3435. [Google Scholar] [CrossRef] [PubMed]
- Investigators, P. Consumption of Yogurt, Low-Fat Milk, and Other Low-Fat Dairy Products Is Associated with Lower Risk of Metabolic Syndrome Incidence in an Elderly Mediterranean Population. J. Nutr. 2015, 145, 2308–2316. [Google Scholar] [CrossRef] [PubMed]
- Walther, B.; Guggisberg, D.; Badertscher, R.; Egger, L.; Portmann, R.; Dubois, S.; Haldimann, M.; Kopf-Bolanz, K.; Rhyn, P.; Zoller, O.; et al. Comparison of nutritional composition between plant-based drinks and cow’s milk. Front. Nutr. 2022, 9, 2645. [Google Scholar] [CrossRef]
- Vitoria, I. The nutritional limitations of plant-based beverages in infancy and childhood. Nutr. Hosp. 2017, 34, 1205–1214. [Google Scholar] [CrossRef]
- Pearson, D.; Barreto-Chang, O.; Shepard, W.E.; Greene, A.; Longhurst, C. Vitamin D–Deficient Rickets in a Child with Cow’s Milk Allergy. Nutr. Clin. Pract. 2010, 25, 394–398. [Google Scholar] [CrossRef]
- Fourreau, D.; Peretti, N.; Hengy, B.; Gillet, Y.; Courtil-Teyssedre, S.; Hess, L.; Loras-Duclaux, I.; Caron, N.; Didier, C.; Cour-Andlauer, F.; et al. Complications carentielles suite à l’utilisation de «laits» végétaux, chez des nourrissons de deux mois et demi à 14 mois (quatre cas). La Presse Médicale 2013, 42, e37–e43. [Google Scholar] [CrossRef]
- Mudenuti, N.V.d.R.; de Camargo, A.C.; de Alencar, S.M.; Danielski, R.; Shahidi, F.; Madeira, T.B.; Hirooka, E.Y.; Spinosa, W.A.; Grossmann, M.V.E. Phenolics and alkaloids of raw cocoa nibs and husk: The role of soluble and insoluble-bound antioxidants. Food Biosci. 2021, 42, 101085. [Google Scholar] [CrossRef]
- Mayorga-Gross, A.L.; Esquivel, P. Impact of Cocoa Products Intake on Plasma and Urine Metabolites: A Review of Targeted and Non-Targeted Studies in Humans. Nutrients 2019, 11, 1163. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Escudero, F.; Casimiro-Gonzales, S.; Fernández-Prior, Á.; Cancino Chávez, K.; Gómez-Mendoza, J.; Fuente-Carmelino, L.d.l.; Muñoz, A.M. Colour, fatty acids, bioactive compounds, and total antioxidant capacity in commercial cocoa beans (Theobroma cacao L.). LWT 2021, 147, 111629. [Google Scholar] [CrossRef]
- Tahmassebi, J.F.; BaniHani, A. Impact of soft drinks to health and economy: A critical review. Eur. Arch. Paediatr. Dent. 2020, 21, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-M.; Lee, E. Association between Soft-Drink Intake and Obesity, Depression, and Subjective Health Status of Male and Female Adults. Int. J. Environ. Res. Public Health 2021, 18, 10415. [Google Scholar] [CrossRef]
- European Union. Council Directive 2001/112/EC of 20 December Relatin to Fruit Juices and Certain Similar Products Intended for Human Consumption; European Union: Brussels, Belgium, 2002; pp. 58–66. [Google Scholar]
- Gill, J.M.R.; Sattar, N. Fruit juice: Just another sugary drink? Lancet Diabetes Endocrinol. 2014, 2, 444–446. [Google Scholar] [CrossRef]
- Kypridemos, C.; O’Flaherty, M.; Capewell, S. Fruit and vegetable consumption and non-communicable disease: Time to update the ‘5 a day’ message? J. Epidemiol. Community Health 2014, 68, 799–800. [Google Scholar] [CrossRef]
- Boulton, J.; Hashem, K.M.; Jenner, K.H.; Lloyd-Williams, F.; Bromley, H.; Capewell, S. How much sugar is hidden in drinks marketed to children? A survey of fruit juices, juice drinks and smoothies. BMJ Open 2016, 6, e010330. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez Delgado, J.; Hoyos Vázquez, M. Los zumos de frutas y su papel en la alimentación infantil. ¿Debemos considerarlos como una bebida azucarada más? Posicionamiento del Grupo de Gastroenterología y Nutrición de la AEPap. Pediatría Atención Primaria 2017, 19, 103–116. [Google Scholar]
- Fernández, R. Población de España en 2022, por Comunidad Autónoma. Available online: https://es.statista.com/estadisticas/472413/poblacion-de-espana-por-comunidad-autonoma/ (accessed on 10 January 2023).
| Age (years) | % Population (n) |
| 7 | 31.0 (550) |
| 8 | 15.7 (279) |
| 9 | 14.9 (264) |
| 10 | 13.4 (238) |
| 11 | 10.7 (190) |
| 12 | 14.3 (254) |
| Parent’s level of education | % Population (n) |
| Primary education | 6 (107) |
| Secondary education | 20.3 (360) |
| Vocational training in other areas | 21.8 (387) |
| Vocational training in health/food sciences | 6.3 (111) |
| Graduates other areas of knowledge | 37.9 (672) |
| Graduates in health/food sciences | 7.7 (136) |
| Others | 0.1 (2) |
| Autonomous Community | % Population (n) |
| Andalucía | 27.1 (481) |
| Madrid | 15.6 (277) |
| Comunidad Valenciana | 12.7 (225) |
| Cataluña | 11.6 (206) |
| Castilla y León | 6.1 (108) |
| Castilla la Mancha | 5.3 (94) |
| Aragón | 3.8 (68) |
| Galicia | 3.7 (66) |
| País Vasco | 3.3 (59) |
| Murcia | 2.7 (48) |
| Extremadura | 2.2 (39) |
| Canarias | 1.7 (31) |
| Asturias | 1.2 (21) |
| Cantabria | 0.9 (16) |
| Baleares | 0.7 (13) |
| Navarra | 0.7 (13) |
| La Rioja | 0.6 (10) |
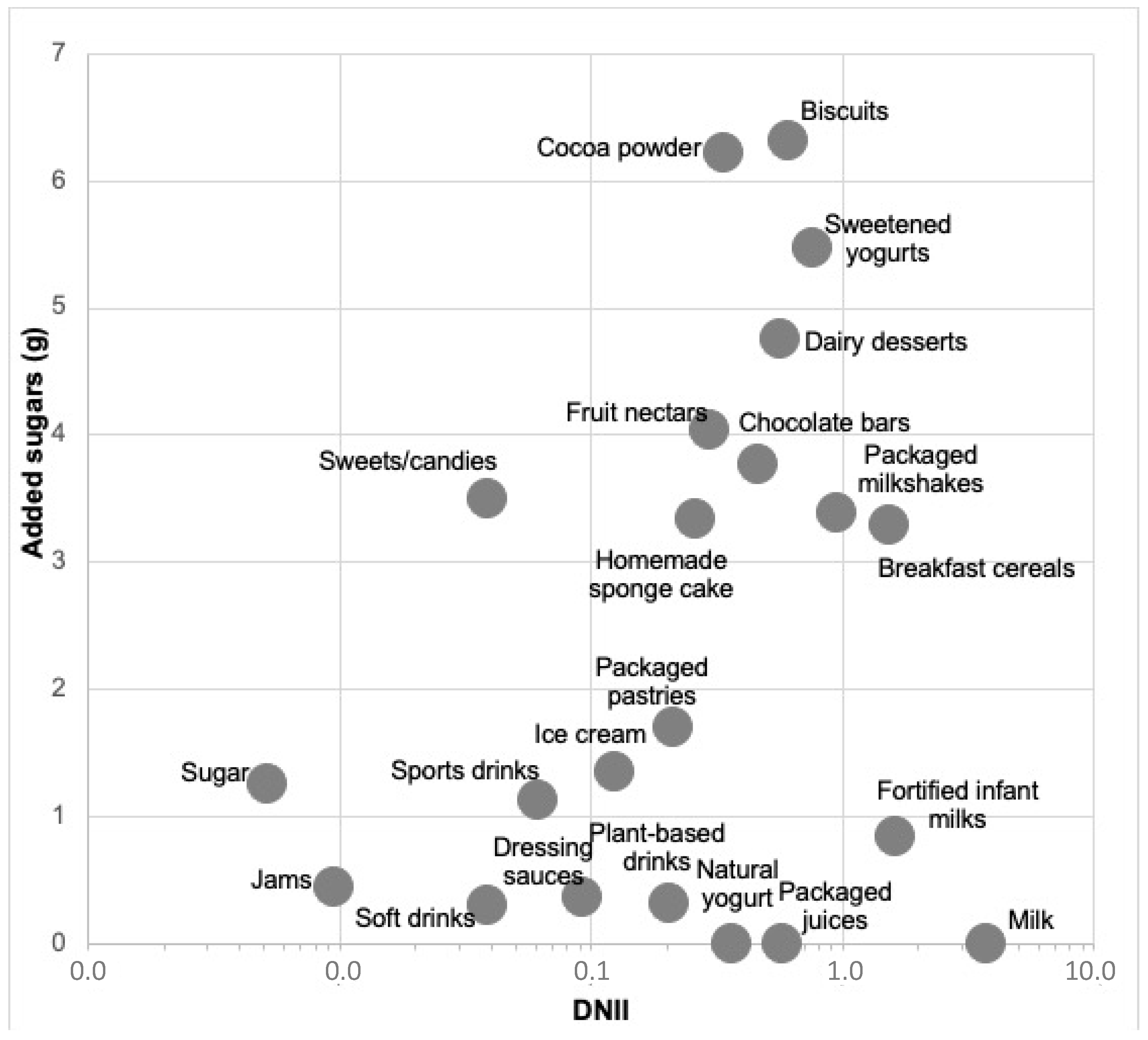
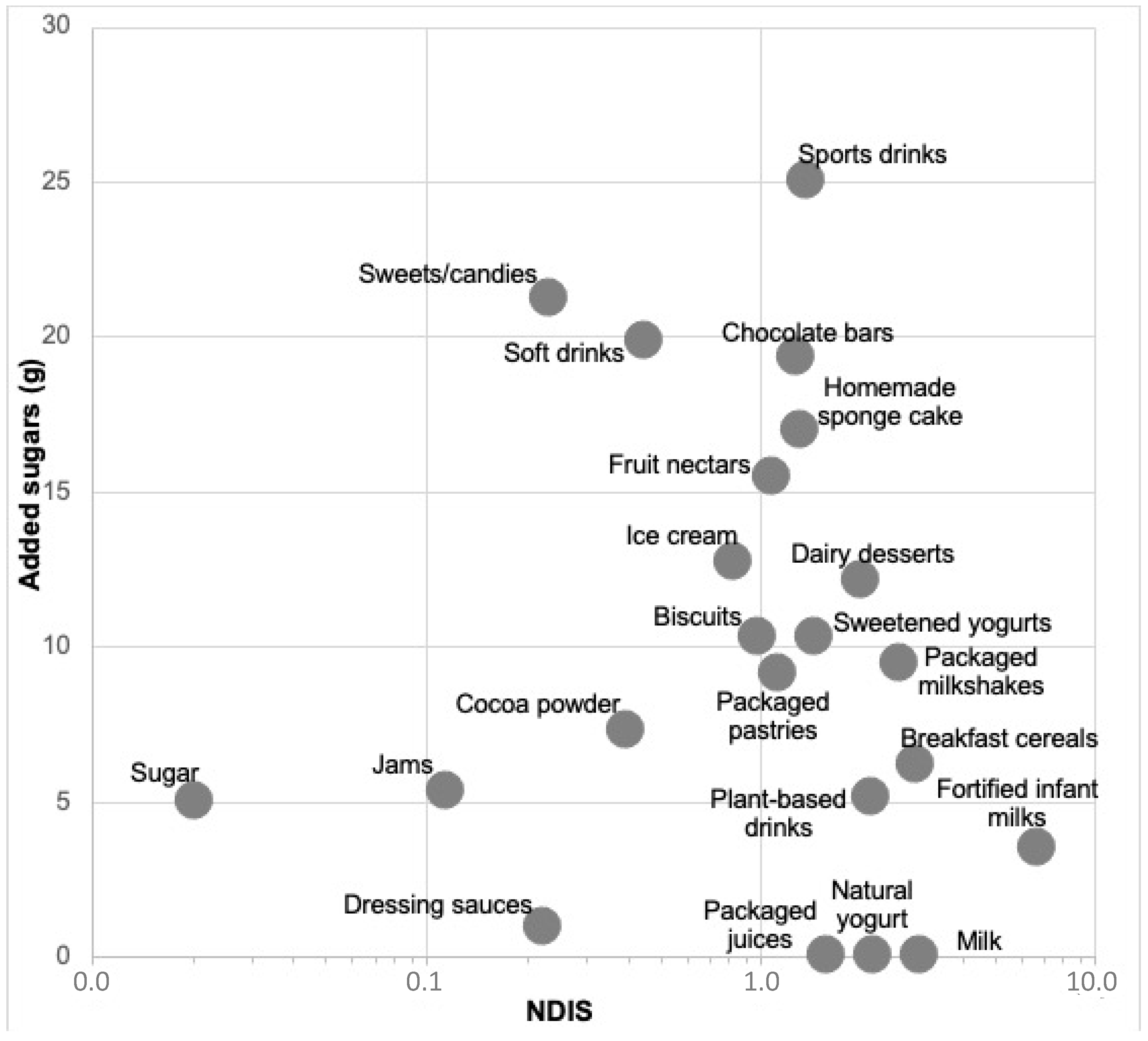
| Food | Added Sugars Daily Contribution | DNII | Servings/Week | Added Sugars (g)/Serving | NDIS | SAIN | LIM | Parent’s Perception of Quality | n-NC |
|---|---|---|---|---|---|---|---|---|---|
| Biscuits | 6.3 | 0.61 | 4.3 ± 0.1 | 10.3 | 1.0 | 3.11 | 41.08 | Normal | 158 |
| Cocoa powder | 6.2 | 0.34 | 6.0 ± 0.1 | 7.3 | 0.4 | 3.21 | 158.30 | Normal | 332 |
| Sweetened yogurts | 5.5 | 0.76 | 3.6 ± 0.1 | 10.3 | 1.5 | 4.95 | 12.06 | Normal | 381 |
| Dairy desserts | 4.8 | 0.57 | 2.0 ± 0.1 | 12.1 | 2.0 | 4.15 | 14.57 | Normal | 493 |
| Fruit nectars | 4.0 | 0.3 | 1.8 ± 0.1 | 15.5 | 1.1 | 22.43 | 15.56 | Normal | 798 |
| Chocolate bars | 3.8 | 0.47 | 2.6 ± 0.1 | 19.3 | 1.3 | 2.80 | 65.58 | Normal | 291 |
| Sweets/candies | 3.5 | 0.04 | 1.2 ± 0.0 | 21.2 | 0.2 | 4.02 | 142.84 | Bad | 482 |
| Packaged milkshakes | 3.4 | 0.94 | 2.5 ± 0.1 | 9.4 | 2.6 | 6.52 | 7.47 | Normal | 540 |
| Homemade sponge cake | 3.3 | 0.26 | 1.4 ± 0.0 | 17.0 | 1.3 | 2.43 | 35.05 | Good | 420 |
| Breakfast cereals | 3.3 | 1.55 | 3.7 ± 0.1 | 6.2 | 2.9 | 9.74 | 32.08 | Normal | 516 |
| Packaged pastries | 1.7 | 0.21 | 1.3 ± 0.1 | 9.1 | 1.1 | 21.78 | 36.85 | Bad | 570 |
| Ice cream | 1.4 | 0.12 | 1.0 ± 0.0 | 12.7 | 0.8 | 3.62 | 35.96 | Normal | 506 |
| Table sugar | 1.3 | 0.01 | 1.8 ± 0.1 | 5.0 | 0.0 | 0.24 | 400 | Normal | 1023 |
| Sports drinks | 1.1 | 0.06 | 0.3 ± 0.0 | 25.0 | 1.4 | 0.26 | 10.60 | Normal | 1408 |
| Infant milks | 0.8 | 1.63 | 1.7 ± 0.1 | 3.5 | 6.7 | 21.78 | 5.60 | Good | 1354 |
| Jams | 0.4 | 0.01 | 0.6 ± 0.0 | 5.3 | 0.1 | 3.75 | 107.03 | Normal | 1145 |
| Dressing sauces | 0.4 | 0.09 | 2.9 ± 0.1 | 0.9 | 0.2 | 10.49 | 31.31 | Normal | 187 |
| Plant-based drinks | 0.3 | 0.20 | 0.4 ± 0.0 | 5.1 | 2.2 | 4.75 | 5.19 | Good | 1532 |
| Soft drinks | 0.3 | 0.04 | 0.6 ± 0.0 | 19.8 | 0.5 | 4.74 | 24.26 | Bad | 1076 |
| Packaged juices | 0.0 | 0.57 | 1.8 ± 0.1 | 0.0 | 2.2 | 30.08 | 0.16 | Normal | 798 |
| Milk | 0.0 | 3.71 | 8.6 ± 0.1 | 0.0 | 3.0 | 9.07 | 1.78 | 177 | |
| Natural yogurt | 0.0 | 0.36 | 1.6 ± 0.1 | 0.0 | 1.6 | 9.46 | 1.63 | 1041 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palma-Morales, M.; Mesa-García, M.D.; Huertas, J.R. Added Sugar Consumption in Spanish Children (7–12 y) and Nutrient Density of Foods Contributing to Such Consumption: An Observational Study. Nutrients 2023, 15, 560. https://doi.org/10.3390/nu15030560
Palma-Morales M, Mesa-García MD, Huertas JR. Added Sugar Consumption in Spanish Children (7–12 y) and Nutrient Density of Foods Contributing to Such Consumption: An Observational Study. Nutrients. 2023; 15(3):560. https://doi.org/10.3390/nu15030560
Chicago/Turabian StylePalma-Morales, Marta, María Dolores Mesa-García, and Jesús R. Huertas. 2023. "Added Sugar Consumption in Spanish Children (7–12 y) and Nutrient Density of Foods Contributing to Such Consumption: An Observational Study" Nutrients 15, no. 3: 560. https://doi.org/10.3390/nu15030560
APA StylePalma-Morales, M., Mesa-García, M. D., & Huertas, J. R. (2023). Added Sugar Consumption in Spanish Children (7–12 y) and Nutrient Density of Foods Contributing to Such Consumption: An Observational Study. Nutrients, 15(3), 560. https://doi.org/10.3390/nu15030560









