Prospective Association between Adherence to the Mediterranean Diet and Health-Related Quality of Life in Spanish Children
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Health-Related Quality of Life Assessment
2.3. Dietary Assessment
2.4. Physical Activity
2.5. Maternal Socioeconomic Status
2.6. Anthropometric Variables
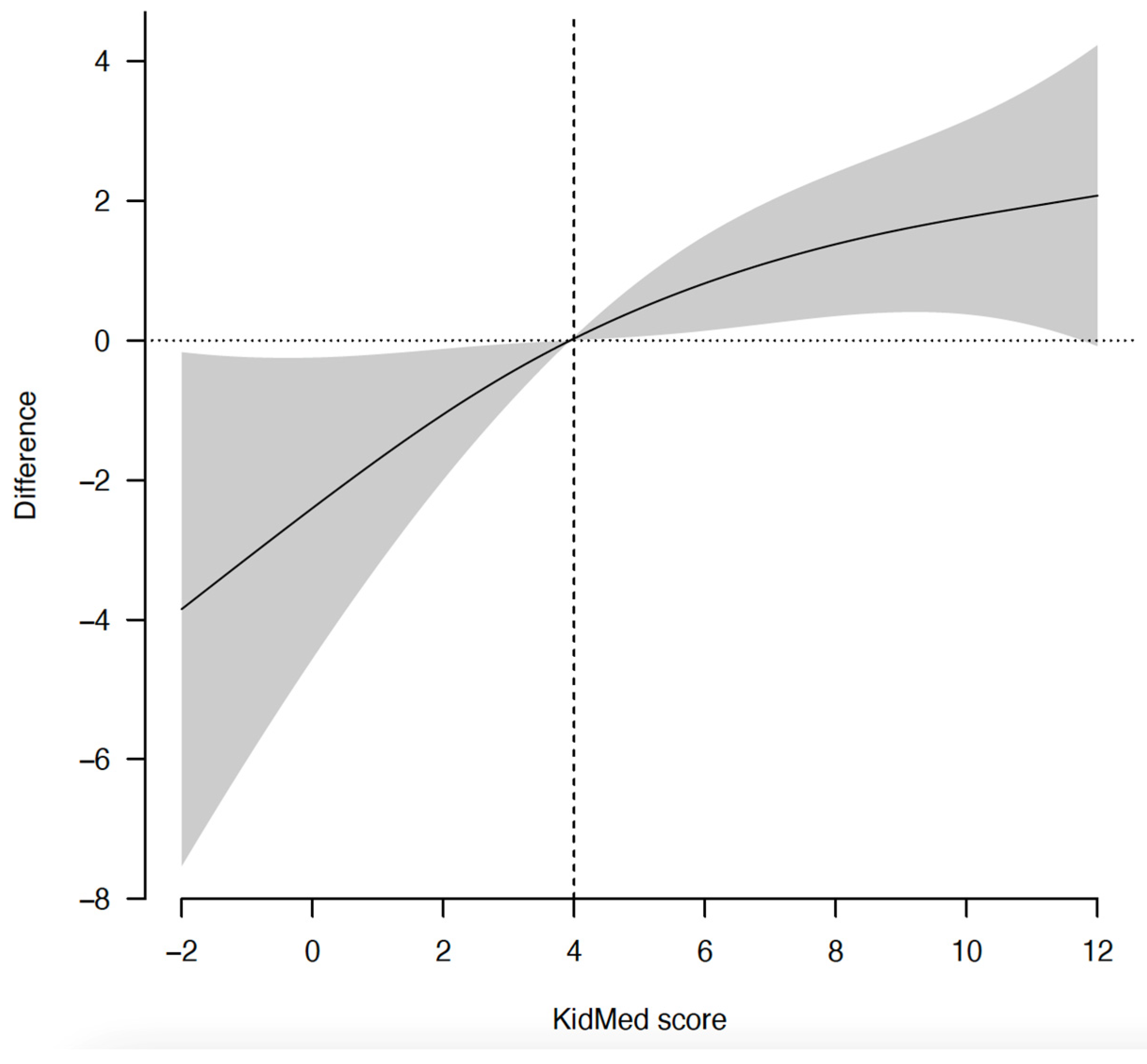
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Constitution of the World Health Organization. Available online: https://www.who.int/about/governance/constitution (accessed on 7 April 2022).
- HRQOL Concepts|CDC. Available online: https://www.cdc.gov/hrqol/concept.htm (accessed on 7 April 2022).
- Masini, A.; Gori, D.; Marini, S.; Lanari, M.; Scrimaglia, S.; Esposito, F.; Campa, F.; Grigoletto, A.; Ceciliani, A.; Toselli, S.; et al. The Determinants of Health-Related Quality of Life in a Sample of Primary School Children: A Cross-Sectional Analysis. Int. J. Environ. Res. Public Health 2021, 18, 3251. [Google Scholar] [CrossRef] [PubMed]
- Becerra-Tomás, N.; Blanco Mejía, S.; Viguiliouk, E.; Khan, T.; Kendall, C.W.C.; Kahleova, H.; Rahelić, D.; Sievenpiper, J.L.; Salas-Salvadó, J. Mediterranean Diet, Cardiovascular Disease and Mortality in Diabetes: A Systematic Review and Meta-Analysis of Prospective Cohort Studies and Randomized Clinical Trials. Crit. Rev. Food Sci. Nutr. 2020, 60, 1207–1227. [Google Scholar] [CrossRef] [PubMed]
- Tosti, V.; Bertozzi, B.; Fontana, L. Health Benefits of the Mediterranean Diet: Metabolic and Molecular Mechanisms. J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Shafiei, F.; Salari-Moghaddam, A.; Larijani, B.; Esmaillzadeh, A. Adherence to the Mediterranean Diet and Risk of Depression: A Systematic Review and Updated Meta-Analysis of Observational Studies. Nutr. Rev. 2019, 77, 230–239. [Google Scholar] [CrossRef]
- Aridi, Y.S.; Walker, J.L.; Wright, O.R.L. The Association between the Mediterranean Dietary Pattern and Cognitive Health: A Systematic Review. Nutrients 2017, 9, 674. [Google Scholar] [CrossRef]
- Romero-Robles, M.A.; Ccami-Bernal, F.; Ortiz-Benique, Z.N.; Pinto-Ruiz, D.F.; Benites-Zapata, V.A.; Casas Patiño, D. Adherence to Mediterranean Diet Associated with Health-Related Quality of Life in Children and Adolescents: A Systematic Review. BMC Nutr. 2022, 8, 57. [Google Scholar] [CrossRef]
- Muros, J.J.; Salvador Pérez, F.; Zurita Ortega, F.; Gámez Sánchez, V.M.; Knox, E. The Association between Healthy Lifestyle Behaviors and Health-Related Quality of Life among Adolescents. J. Pediatr. (Rio. J.) 2017, 93, 406–412. [Google Scholar] [CrossRef]
- Evaristo, O.S.; Moreira, C.; Lopes, L.; Abreu, S.; Agostinis-Sobrinho, C.; Oliveira-Santos, J.; Póvoas, S.; Oliveira, A.; Santos, R.; Mota, J. Associations between Physical Fitness and Adherence to the Mediterranean Diet with Health-Related Quality of Life in Adolescents: Results from the LabMed Physical Activity Study. Eur. J. Public Health 2018, 28, 631–635. [Google Scholar] [CrossRef]
- Ferrer-Cascales, R.; Albaladejo-Blázquez, N.; Ruiz-Robledillo, N.; Clement-Carbonell, V.; Sánchez-SanSegundo, M.; Zaragoza-Martí, A. Higher Adherence to the Mediterranean Diet Is Related to More Subjective Happiness in Adolescents: The Role of Health-Related Quality of Life. Nutrients 2019, 11, 698. [Google Scholar] [CrossRef]
- Caamaño-Navarrete, F.; Ángel Latorre-Román, P.; Guzmán-Guzmán, I.P.; Párraga Montilla, J.; Jerez-Mayorga, D.; Delgado-Floody, P. Lifestyle Mediates the Relationship between Self-Esteem and Health-Related Quality of Life in Chilean Schoolchildren. Psychol. Health Med. 2022, 27, 638–648. [Google Scholar] [CrossRef]
- Costarelli, V.; Koretsi, E.; Georgitsogianni, E. Health-Related Quality of Life of Greek Adolescents: The Role of the Mediterranean Diet. Qual. Life Res. 2013, 22, 951–956. [Google Scholar] [CrossRef] [PubMed]
- Zervaki, K.; Yiannakouris, N.; Sdrali, D.; Costarelli, V. Diet Quality, Disordered Eating and Health-Related Quality of Life in Adolescents. Nutr. Food Sci. 2017, 47, 511–521. [Google Scholar] [CrossRef]
- Mitri, R.N.; Boulos, C.; Ziade, F. Mediterranean Diet Adherence amongst Adolescents in North Lebanon: The Role of Skipping Meals, Meals with the Family, Physical Activity and Physical Well-Being. Br. J. Nutr. 2021, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Esteban-Gonzalo, L.; Turner, A.I.; Torres, S.J.; Esteban-Cornejo, I.; Castro-Piñero, J.; Delgado-Alfonso, Á.; Marcos, A.; Gómez-Martínez, S.; Veiga, Ó.L. Diet Quality and Well-Being in Children and Adolescents: The UP&DOWN Longitudinal Study. Br. J. Nutr. 2019, 121, 221–231. [Google Scholar] [CrossRef]
- Gomez, S.F.; Casas, R.; Palomo, V.T.; Martin Pujol, A.; Fíto, M.; Schröder, H. Study Protocol: Effects of the THAO-Child Health Intervention Program on the Prevention of Childhood Obesity—The POIBC Study. BMC Pediatr. 2014, 14, 215. [Google Scholar] [CrossRef]
- The KIDSCREEN-10 Index. Available online: http://www.kidscreen.org/english/questionnaires/kidscreen-10-index/ (accessed on 1 July 2022).
- Ravens-Sieberer, U.; KIDSCREEN Group Europe. The KIDSCREEN Questionnaires Quality of Life Questionnaires for Children and Adolescents; PABST: Lengerich, Germany, 2006. [Google Scholar]
- Ellert, U.; Brettschneider, A.-K.; Ravens-Sieberer, U.; KiGGS Study Group. Gesundheitsbezogene Lebensqualität bei Kindern und Jugendlichen in Deutschland. Bundesgesundheitsblatt 2014, 57, 798–806. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, Youth and the Mediterranean Diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in Children and Adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef]
- Moore, J.B.; Hanes, J.C.; Barbeau, P.; Gutin, B.; Treviño, R.P.; Yin, Z. Validation of the Physical Activity Questionnaire for Older Children in Children of Different Races. Pediatric Exerc. Sci. 2007, 19, 6–19. [Google Scholar] [CrossRef]
- de Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO Growth Reference for School-Aged Children and Adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef]
- Jacka, F.N.; Kremer, P.J.; Berk, M.; de Silva-Sanigorski, A.M.; Moodie, M.; Leslie, E.R.; Pasco, J.A.; Swinburn, B.A. A Prospective Study of Diet Quality and Mental Health in Adolescents. PLoS ONE 2011, 6, e24805. [Google Scholar] [CrossRef]
- Boyle, S.E.; Jones, G.L.; Walters, S.J. Physical Activity, Quality of Life, Weight Status and Diet in Adolescents. Qual. Life Res. 2010, 19, 943–954. [Google Scholar] [CrossRef] [PubMed]
- Dalton III, W.T.; Schetzina, K.E.; Pfortmiller, D.T.; Slawson, D.L.; Frye, W.S. Health Behaviors and Health-Related Quality of Life among Middle School Children in Southern Appalachia: Data from the Winning with Wellness Project. J. Pediatric Psychol. 2011, 36, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Sekine, M.; Chen, X.; Yamagami, T.; Kagamimori, S. Lifestyle at 3 Years of Age and Quality of Life (QOL) in First-Year Junior High School Students in Japan: Results of the Toyama Birth Cohort Study. Qual. Life Res. 2008, 17, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Sekine, M.; Hamanishi, S.; Yamagami, T.; Kagamimori, S. Associations of Lifestyle Factors with Quality of Life (QOL) in Japanese Children: A 3-Year Follow-up of the Toyama Birth Cohort Study. Child Care Health Dev. 2005, 31, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Gopinath, B.; Flood, V.M.; Burlutsky, G.; Louie, J.C.Y.; Baur, L.A.; Mitchell, P. Dairy Food Consumption and Health-Related Quality of Life in Boys: Preliminary Findings from a 5-Year Cohort Study. J. Am. Coll. Nutr. 2016, 35, 522–558. [Google Scholar] [CrossRef]
- Chen, G.; Ratcliffe, J.; Olds, T.; Magarey, A.; Jones, M.; Leslie, E. BMI, Health Behaviors, and Quality of Life in Children and Adolescents: A School-Based Study. Pediatrics 2014, 133, e868–e874. [Google Scholar] [CrossRef]
- Mentella, M.C.; Scaldaferri, F.; Ricci, C.; Gasbarrini, A.; Miggiano, G.A.D. Cancer and Mediterranean Diet: A Review. Nutrients 2019, 11, 2059. [Google Scholar] [CrossRef]
- Bauer, M.E.; Teixeira, A.L. Inflammation in Psychiatric Disorders: What Comes First? Ann. N. Y. Acad. Sci. 2019, 1437, 57–67. [Google Scholar] [CrossRef]
- Osimo, E.F.; Cardinal, R.N.; Jones, P.B.; Khandaker, G.M. Prevalence and Correlates of Low-Grade Systemic Inflammation in Adult Psychiatric Inpatients: An Electronic Health Record-Based Study. Psychoneuroendocrinology 2018, 91, 226–234. [Google Scholar] [CrossRef]
- Belliveau, R.; Horton, S.; Hereford, C.; Ridpath, L.; Foster, R.; Boothe, E. Pro-Inflammatory Diet and Depressive Symptoms in the Healthcare Setting. BMC Psychiatry 2022, 22, 125. [Google Scholar] [CrossRef]
- Firth, J.; Stubbs, B.; Teasdale, S.B.; Ward, P.B.; Veronese, N.; Shivappa, N.; Hebert, J.R.; Berk, M.; Yung, A.R.; Sarris, J. Diet as a Hot Topic in Psychiatry: A Population-scale Study of Nutritional Intake and Inflammatory Potential in Severe Mental Illness. World Psychiatry 2018, 17, 365–367. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.H.; Raison, C.L. The Role of Inflammation in Depression: From Evolutionary Imperative to Modern Treatment Target. Nat. Rev. Immunol. 2016, 16, 22–34. [Google Scholar] [CrossRef] [PubMed]
- Morrison, C.D.; Pistell, P.J.; Ingram, D.K.; Johnson, W.D.; Liu, Y.; Fernandez-Kim, S.O.; White, C.L.; Purpera, M.N.; Uranga, R.M.; Bruce-Keller, A.J.; et al. High Fat Diet Increases Hippocampal Oxidative Stress and Cognitive Impairment in Aged Mice: Implications for Decreased Nrf2 Signaling. J. Neurochem. 2010, 114, 1581–1589. [Google Scholar] [CrossRef] [PubMed]
- Fitó, M.; Guxens, M.; Corella, D.; Sáez, G.; Estruch, R.; de la Torre, R.; Francés, F.; Cabezas, C.; López-Sabater, M.D.C.; Marrugat, J.; et al. Effect of a Traditional Mediterranean Diet on Lipoprotein Oxidation: A Randomized Controlled Trial. Arch. Intern. Med. 2007, 167, 1195–1203. [Google Scholar] [CrossRef] [PubMed]
- Calder, P.C.; Ahluwalia, N.; Brouns, F.; Buetler, T.; Clement, K.; Cunningham, K.; Esposito, K.; Jönsson, L.S.; Kolb, H.; Lansink, M.; et al. Dietary Factors and Low-Grade Inflammation in Relation to Overweight and Obesity. Br. J. Nutr. 2011, 106, S5–S78. [Google Scholar] [CrossRef]
- Magnusson, K.R.; Hauck, L.; Jeffrey, B.M.; Elias, V.; Humphrey, A.; Nath, R.; Perrone, A.; Bermudez, L.E. Relationships between Diet-Related Changes in the Gut Microbiome and Cognitive Flexibility. Neuroscience 2015, 300, 128–140. [Google Scholar] [CrossRef] [PubMed]
- Ohland, C.L.; Kish, L.; Bell, H.; Thiesen, A.; Hotte, N.; Pankiv, E.; Madsen, K.L. Effects of Lactobacillus Helveticus on Murine Behavior Are Dependent on Diet and Genotype and Correlate with Alterations in the Gut Microbiome. Psychoneuroendocrinology 2013, 38, 1738–1747. [Google Scholar] [CrossRef]
- Ghosh, T.S.; Rampelli, S.; Jeffery, I.B.; Santoro, A.; Neto, M.; Capri, M.; Giampieri, E.; Jennings, A.; Candela, M.; Turroni, S.; et al. Mediterranean Diet Intervention Alters the Gut Microbiome in Older People Reducing Frailty and Improving Health Status: The NU-AGE 1-Year Dietary Intervention across Five European Countries. Gut 2020, 69, 1218–1228. [Google Scholar] [CrossRef]
- Naughton, M.; Dinan, T.G.; Scott, L.V. Corticotropin-Releasing Hormone and the Hypothalamic-Pituitary-Adrenal Axis in Psychiatric Disease. Handb. Clin. Neurol. 2014, 124, 69–91. [Google Scholar] [CrossRef]
- Brody, S.; Preut, R.; Schommer, K.; Schürmeyer, T.H. A Randomized Controlled Trial of High Dose Ascorbic Acid for Reduction of Blood Pressure, Cortisol, and Subjective Responses to Psychological Stress. Psychopharmacology 2002, 159, 319–324. [Google Scholar] [CrossRef]
- Barbadoro, P.; Annino, I.; Ponzio, E.; Romanelli, R.M.L.; D’Errico, M.M.; Prospero, E.; Minelli, A. Fish Oil Supplementation Reduces Cortisol Basal Levels and Perceived Stress: A Randomized, Placebo-Controlled Trial in Abstinent Alcoholics. Mol. Nutr. Food Res. 2013, 57, 1110–1114. [Google Scholar] [CrossRef]
- Delarue, J.; Matzinger, O.; Binnert, C.; Schneiter, P.; Chioléro, R.; Tappy, L. Fish Oil Prevents the Adrenal Activation Elicited by Mental Stress in Healthy Men. Diabetes Metab. 2003, 29, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Tsang, C.; Hodgson, L.; Bussu, A.; Farhat, G.; Al-Dujaili, E. Effect of Polyphenol-Rich Dark Chocolate on Salivary Cortisol and Mood in Adults. Antioxidants 2019, 8, 149. [Google Scholar] [CrossRef] [PubMed]
- Shively, C.A.; Appt, S.E.; Chen, H.; Day, S.M.; Frye, B.M.; Shaltout, H.A.; Silverstein-Metzler, M.G.; Snyder-Mackler, N.; Uberseder, B.; Vitolins, M.Z.; et al. Mediterranean Diet, Stress Resilience, and Aging in Nonhuman Primates. Neurobiol. Stress 2020, 13, 100254. [Google Scholar] [CrossRef] [PubMed]
- Karege, F.; Perret, G.; Bondolfi, G.; Schwald, M.; Bertschy, G.; Aubry, J.-M. Decreased Serum Brain-Derived Neurotrophic Factor Levels in Major Depressed Patients. Psychiatry Res. 2002, 109, 143–148. [Google Scholar] [CrossRef]
- Sánchez-Villegas, A.; Galbete, C.; Martinez-González, M.A.; Martinez, J.A.; Razquin, C.; Salas-Salvadó, J.; Estruch, R.; Buil-Cosiales, P.; Martí, A. The Effect of the Mediterranean Diet on Plasma Brain-Derived Neurotrophic Factor (BDNF) Levels: The PREDIMED-NAVARRA Randomized Trial. Nutr. Neurosci. 2011, 14, 195–201. [Google Scholar] [CrossRef]
- Russo, S.; Kema, I.P.; Bosker, F.; Haavik, J.; Korf, J. Tryptophan as an Evolutionarily Conserved Signal to Brain Serotonin: Molecular Evidence and Psychiatric Implications. World J. Biol. Psychiatry 2009, 10, 258–268. [Google Scholar] [CrossRef]
| Total | 1st Tertile | 2nd Tertile | 3rd Tertile | p for Linear | |
|---|---|---|---|---|---|
| n = 1371 | n = 471 | n = 492 | n = 408 | Trend | |
| KIDSCREEN-10 2 | 50.4 (25.4; 83.8) | 41.4 (25.4; 45.7) | 49.9 (46.9; 53.1) | 61.6 (55.1; 83.8) | |
| Girls | 681 (49.7) | 237 (50.3) | 240 (48.8) | 204 (50.0) | 0.908 |
| Age (years) | 10.1 (10.0; 10.2) | 10.1 (10.0; 10.2) | 10.1 (10.0; 10.1) | 10.1 (10.0; 10.2) | 0.506 |
| Maternal education 3 | 468 (34.1) | 143 (30.4) | 171 (34.8) | 154 (37.7) | 0.021 |
| zBMI | 0.70 (0.64; 0.76) | 0.76 (0.65; 0.86) | 0.66 (0.55; 0.76) | 0.68 (0.57; 0.79) | 0.341 |
| KidMed score 4 | 6.9 (6.7; 7.0) | 6.1 (5.9; 6.3) | 7.1 (6.8; 7.3) | 7.5 (7.3; 7.7) | <0.001 |
| Physical activity | 2.98 (2.94; 3.01) | 2.68 (2.22; 2.74) | 3.04 (2.97; 3.10) | 3.25 (3.18; 3.31) | <0.001 |
| OR | 95% CI | p Value | |
|---|---|---|---|
| Takes a fruit or fruit juice every day | 1.31 | 1.02; 1.69 | 0.038 |
| Has a second fruit every day | 1.19 | 0.94; 1.50 | 0.150 |
| Has fresh or cooked vegetables regularly once a day | 1.29 | 1.02; 1.63 | 0.037 |
| Has fresh or cooked vegetables more than once a day | 1.03 | 0.79; 1.34 | 0.849 |
| Consumes fish regularly (at least 2–3 times/week) | 1.21 | 0.95; 1.55 | 0.127 |
| Eats > 1 meal/week in fast food restaurants | 0.59 | 0.43; 0.81 | 0.001 |
| Likes pulses and eats them more than once a week | 1.29 | 1.01; 1.65 | 0.039 |
| Consumes pasta or rice at least 5 days per week | 0.78 | 0.62; 0.98 | 0.035 |
| Has cereals or grains (bread, etc.) for breakfast | 1.12 | 0.87; 1.45 | 0.365 |
| Consumes nuts regularly (at least 2–3 times/week) | 1.15 | 0.92; 1.45 | 0.230 |
| Uses olive oil at home | 1.04 | 0.72; 1.50 | 0.850 |
| Skips breakfast | 0.85 | 0.47; 1.52 | 0.572 |
| Has a dairy product for breakfast (yoghurt, milk, etc.) | 1.36 | 0.98; 1.89 | 0.068 |
| Has commercially baked goods or pastries for breakfast | 0.56 | 0.42; 0.79 | <0.001 |
| Takes 2 cups of yoghurts and/or some cheese (40 g) daily | 1.19 | 0.91; 1.55 | 0.208 |
| Takes sweets and candy several times every day | 0.65 | 0.46; 0.91 | 0.012 |
| Adherence to the Mediterranean diet | |||
| Low | 1 | Reference | |
| Medium | 1.53 | 0.98; 2.39 | 0.063 |
| High | 2.13 | 1.35; 3.36 | 0.001 |
| p for linear trend <0.001 | |||
| HRQoL (KIDSCREEN-10) 2 | |||
|---|---|---|---|
| Beta Coefficient | 95% CI | p Value | |
| KidMed score 3 (unit) | |||
| Model 1 4 | 0.678 | 0.459; 0.896 | <0.001 |
| Model 2 5 | 0.550 | 0.323; 0.778 | <0.001 |
| Model 3 6 | 0.320 | 0.101; 0.540 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Juton, C.; Berruezo, P.; Rajmil, L.; Lerin, C.; Fíto, M.; Homs, C.; Según, G.; Gómez, S.F.; Schröder, H. Prospective Association between Adherence to the Mediterranean Diet and Health-Related Quality of Life in Spanish Children. Nutrients 2022, 14, 5304. https://doi.org/10.3390/nu14245304
Juton C, Berruezo P, Rajmil L, Lerin C, Fíto M, Homs C, Según G, Gómez SF, Schröder H. Prospective Association between Adherence to the Mediterranean Diet and Health-Related Quality of Life in Spanish Children. Nutrients. 2022; 14(24):5304. https://doi.org/10.3390/nu14245304
Chicago/Turabian StyleJuton, Charlotte, Paula Berruezo, Luis Rajmil, Carles Lerin, Montserrat Fíto, Clara Homs, Genís Según, Santiago F. Gómez, and Helmut Schröder. 2022. "Prospective Association between Adherence to the Mediterranean Diet and Health-Related Quality of Life in Spanish Children" Nutrients 14, no. 24: 5304. https://doi.org/10.3390/nu14245304
APA StyleJuton, C., Berruezo, P., Rajmil, L., Lerin, C., Fíto, M., Homs, C., Según, G., Gómez, S. F., & Schröder, H. (2022). Prospective Association between Adherence to the Mediterranean Diet and Health-Related Quality of Life in Spanish Children. Nutrients, 14(24), 5304. https://doi.org/10.3390/nu14245304








