Abstract
Nutrition interventions to prevent pediatric obesity can help to establish healthy habits to improve current and future health. The objective of this umbrella review of systematic reviews (SRs) is to examine the impact of obesity prevention interventions with a nutrition component on body mass index measures, overweight/obesity prevalence, and cost-effectiveness in participants 2–17 years old. Grading of Recommendations Assessment, Development and Evaluation (GRADE) methods were used, and this umbrella review was registered on PROSPERO (CRD42023443033). Included SRs were required to search ≥2 databases and to assess the risk of bias (RoB) of primary studies, and they were published 2017–June 2023. Database searches identified 4776 articles, and 31 SRs were included. In all age groups combined, interventions with both nutrition and physical activity were effective and cost-effective in all settings combined, and in the community setting specifically. In children ≤5 years old, interventions in the home and family, community, and healthcare settings demonstrated some efficacy, whereas in children 6–12 years old, school interventions were most effective. Evidence with individuals 13–17 years was limited. The certainty of evidence was generally low due to RoB in included studies, inconsistency, and imprecision. Pediatric obesity prevention interventions with nutrition should be tailored to the developmental stage to ensure appropriateness and efficacy.
Keywords:
pediatrics; nutrition; obesity; dietitian; primary prevention; diet; exercise; systematic review; schools 1. Introduction
Pediatric obesity can impact physical and psychological health and can lead to several adverse health conditions, including type 2 diabetes mellitus (T2DM), cardiovascular problems, and gastroesophageal reflux [1]. Accordingly, a Healthy People 2030 goal is to reduce the proportion of children and adolescents with obesity from its current rate of 19.7% [2]. The United States Preventive Task Force recommends that children and adolescents be screened for obesity and referred for or offered comprehensive behavioral interventions, which may include parent involvement and instruction on nutrition and physical activity [3]. The nutrition component of interventions is ideally led or designed by dietitians, who may provide nutrition counseling in child-based settings, develop and deliver theory-based nutrition education programs, and implement environmental and policy changes to improve access to healthy foods [4].
Interventions to prevent pediatric obesity can help to establish healthy habits to improve current and future health. Childhood and adolescence are stages of dynamic growth in which developmental skills, interests, and emotional maturity vary between peers and within individuals over time. Whereas younger children rely more on caregivers to learn how to eat and prepare food, older children become increasingly autonomous in choosing foods [5]. Thus, for interventions to be effective, they must accommodate diverse contexts and changing needs, including level of involvement in home life, in school, and with peers.
A recent overview of systematic reviews (SRs), also called an umbrella review, found that interventions for pediatric obesity prevention for children 6–12 years old improved BMI measures [6]. Another overview of reviews from 2019 found no overall effect of prevention interventions on BMI measures in pediatric participants but did not discuss results by type of intervention or age [7]. These umbrella reviews included 3–5 SRs each, though a recent scoping review identified many current SRs addressing a wide range of nutrition interventions to prevent pediatric obesity [8]. A 2020 overview of reviews identified 13 SRs that generally demonstrated little to no effect of prevention interventions on BMI measures in adolescents [9]. In 2021, the Academy of Nutrition and Dietetics conducted an umbrella review on pediatric obesity prevention interventions with nutrition to inform a Position Paper for nutrition practitioners, funders, and policymakers working to prevent pediatric obesity [4]. However, the umbrella review was never published. To provide those working in the nutrition field with detailed evidence to assess and to inform practice, the current manuscript provides a comprehensive account of updated evidence on nutrition interventions to prevent pediatric obesity.
Given the importance of facilitating healthy behaviors in children and adolescents and the uncertainty about which types of interventions are effective at which developmental stages, a comprehensive umbrella review is needed to inform practitioners, program funders, and policymakers working in the nutrition field about effective methods to prevent obesity throughout childhood and adolescence. The objective of this umbrella review is to examine the research question: In presumably healthy children and adolescents in the general population, what is the impact of pediatric obesity prevention interventions with nutrition on BMI measures, overweight and obesity incidence, and cost-effectiveness?
2. Methods
This umbrella review of SRs was designed using a social-ecological model [10], used methods described by the Cochrane Collaboration [11] and the Academy of Nutrition and Dietetics [12], and was reported according to the PRIOR checklist for overviews of SRs [13]. This umbrella review was registered on PROSPERO (CRD42023443033) [14].
2.1. Eligibility Criteria
Eligibility criteria are described in Table 1. Included SRs addressed all aspects of the Population-Intervention-Comparison-Outcome (PICO) question: In presumably healthy children and adolescents (2–17 years) what is the impact of pediatric obesity prevention interventions that include nutrition, compared to no intervention, on BMI measures, prevalence of overweight and obesity and cost-effectiveness? SRs were excluded if they targeted individuals with diagnosed diseases, including those with overweight or obesity. SRs were eligible if they searched at ≥2 databases, assessed the risk of bias (RoB) of included primary studies, and were published after January 2017 to ensure the inclusion of recent primary research. SRs conducting meta-analysis or grading the certainty of evidence (CoE) for outcomes of interest were prioritized. When SRs using gold-standard methods were not available, SRs without these methods were included [8].

Table 1.
Eligibility Criteria for Umbrella Review of Systematic Reviews Examining the Effect of Nutrition Interventions to Prevent Pediatric Obesity.
2.2. Information Sources
Authors utilized search terms from a supporting scoping review [8], which was designed by an information specialist for Medline (Ebsco, Ipswich, MA, USA), CINAHL (Ebsco), Cochrane Database of Systematic Reviews (Ebsco), and Food Science Source (Ebsco) databases. This search was updated by M.R. The full search plan can be found in Supplementary Tables S1–S5.
2.3. Study Selection
A sample of titles and abstracts were independently screened by M.R. and D.H. using Rayyan screening software (https://rayyan.ai/cite), and >80% agreement was achieved [15]. Therefore, the remaining titles and abstracts were screened by M.R., consulting with D.H. as needed. SRs included from the title and abstract screening were reviewed independently and in full by M.R. and D.H. Any disagreements between reviewers were resolved by consensus.
2.4. Data Collection
Data were extracted from the SRs by M.R. and cross-checked by D.H. Data were extracted onto a study-characteristics table and included: bibliographic information; participant ages; number and study designs of articles included in the SR; description of the intervention of interest and comparison groups; setting (e.g., school, healthcare); reported outcomes of interest; if the SR conducted meta-analysis or graded CoE, and the tool used to assess the RoB in primary studies. Interventions were required to have a nutrition component. However, results from interventions that additionally included physical activity were prioritized when interpreting findings, as multi-component interventions may be more effective [16]. For each study, quantitative and narrative results were extracted for each outcome of interest in each age group and setting of interest. In addition, primary studies included for each SR were compared to primary studies included in other SRs examining interventions in the same settings and age groups.
2.5. Quality Assessment
Included SRs were required to assess the RoB of included primary studies (Table 1). Additionally, each included SR was assessed for quality using the AMSTAR2 tool [17]. SR quality was determined independently by two reviewers and discrepancies were resolved through consensus.
2.6. Synthesis of Results and Certainty Assessment
The inclusion process for this study was documented in a PRISMA flowchart [18]. Characteristics and results from each included SR were described in tables. If SRs included interventions from all settings or age groups, results were categorized as “all settings” or “all age groups combined” only unless sub-group analysis was provided for specific settings or age groups. SRs examining interventions in a specific setting (e.g., school) or age group (e.g., 6–12 years) were included in results for those categories only. The highest-quality SRs as determined by AMSTAR2 ratings and SRs that were the most comprehensive were used to inform conclusions. However, we were not able to conduct novel meta-analysis of included primary studies, as included SRs did not report sufficient data.
If SRs reported CoE using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) method, this grade was used to report CoE in this umbrella review. If the SRs used a different method or did not assess CoE, evidence was graded using the GRADE method [19], which was documented in summary of findings tables. CoE was graded as high, moderate, low, or very low [19]. Heterogeneity and sensitivity analyses conducted in the included SRs were used to inform conclusions.
3. Results
There were 4776 unique articles identified by the database searches, and authors reviewed the full text of 445 articles. A list of articles excluded during full-text review, including reasons for exclusion is available in Supplementary Table S6. Thirty-one SRs were included in this umbrella review [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50]. SRs examined nutrition interventions for pediatric obesity prevention in all settings combined [20,22,30,33,34,43,44,47] or in the home and family [20,22,35], healthcare [22,37,49,50], school [20,22,23,25,27,28,29,36,38,40,41,42,46], or community settings [21,22], or examined the efficacy of food assistance programs [24,26,27,31,32,39] or electronic interventions [45,48]. The study selection process is described in Figure 1. Study characteristics are described in Table 2, and SR quality, as measured by the AMSTAR2 tool, can be found in Supplementary Table S7. Some SRs reported findings for more than one age group or settings category (Table 2).
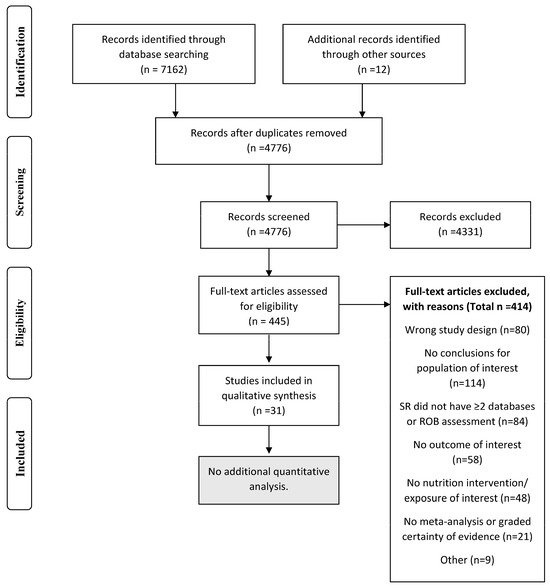
Figure 1.
PRISMA flow chart demonstrating the study inclusion process for the umbrella review of systematic reviews on nutrition interventions to prevent pediatric obesity.

Table 2.
Study characteristics of included systematic reviews examining the impact of nutrition interventions for pediatric obesity prevention.
3.1. All Settings
Eight included SRs examined the impact of nutrition interventions for pediatric obesity prevention in all settings, including in all ages combined [20,34,43,47], or in those ≤5 years [22], 6–12 years [20,22,44], or 13–17 years [22,30,33]. The eight SRs analyzed data from a total of 142 primary studies, and 33 of these studies were represented in more than one SR.
3.1.1. Age Groups Combined
Four SRs examined the effect of nutrition interventions for pediatric obesity prevention in combined age groups [20,34,43,47]. Results are described in Table 3 and CoE is described in Table 4. Salam et al., published in 2020, found that nutrition and physical activity interventions reduced BMI z-score [mean difference (MD) (95 % confidence interval (CI)):−0.12 (−0.18, −0.06)] and BMI [−0.41 kg/m2 (−0.06, −0.21)], and CoE was low due to high heterogeneity in results [43]. Long et al. 2021 agreed with these results but found smaller effect sizes [34]. In Abdel Rahman et al. 2018, there was no effect of the interventions to reduce sugar-sweetened beverage intake on BMI z-scores in three primary studies [20]. Specchia et al. 2018 reported that multi-component, multi-level, or multi-setting interventions reduced overweight and obesity prevalence [47]. In the supplementary materials, Salam et al. also reported effects on obesity prevalence, but there were errors in the analysis. Salam et al. 2020 [43] was the only SR to examine the cost-effectiveness of nutrition interventions to prevent obesity, and five out of six of the included primary studies demonstrated cost-effectiveness or cost savings. Salam et al. 2020 [43] and Specchia et al. 2018 [47] had a low quality score and the remaining SRs had critically low quality scores (Table S7).

Table 3.
Quantitative results of included systematic reviews examining the impact of pediatric obesity prevention interventions with nutrition.

Table 4.
Summary of findings table describing systematic reviews examining the effects of nutrition interventions for pediatric obesity prevention in all settings in individuals 2–17 years old.
3.1.2. Specific Age Groups
In SRs examining children ≤5 years, Brown et al. found moderate CoE that interventions including both diet and physical activity reduced BMI z-score [−0.07 (−0.14, −0.01)] and BMI [−0.11 kg/m2 (−0.21, 0.00)] compared to control groups [22]. Two SRs targeted children 6–12 years old [22,44]. Interventions with both diet and physical activity reduced BMI z-score [−0.05 (−0.10, −0.01)], but not BMI [−0.05 kg/m2 (−0.11, 0.01)] in 6–12-year-old children, and CoE was low (Table 3) [22]. Seral-Cortes et al. found that health programs targeting obesity prevention with nutrition and physical activity did not affect BMI z-score or BMI [44]. Brown had a high quality score and Seral-Cortes had a critically low quality score (Supplementary Table S7).
Three SRs examined the effect of nutrition interventions in all settings for adolescents 13–17 years old [22,30,33]. Brown et al. and Hayba et al. were high quality SRs and Kornet van der Aa was of moderate quality. Hayba et al. and Kornet van der Aa targeted adolescents from under-represented groups. Nutrition and physical activity interventions did not affect BMI z-score or BMI, and CoE was low [22,30]. Overweight and obesity prevalence decreased in the intervention group compared to the control group in one study [33] and CoE was very low (Table 3 and Table 4).
Based on the current evidence, nutrition and physical activity interventions to prevent pediatric obesity may reduce BMI z-score and may be cost-effective for participants <18 years old. Interventions in all settings were most effective for individuals ≤12 years old. Obesity prevention programs that were multi-component, multi-level and/or within multiple settings may reduce overweight/obesity prevalence.
3.2. Home and Family Setting
Three SRs examined the impact of interventions of interest in the home and family setting [20,22,35] in all ages combined [35] and for children ≤5 years old [22], 6–12 years old [20,22], and 13–18 years old [22]. In the three SRs, 12 primary studies were represented, and there was no overlap in primary studies between SRs.
3.2.1. Age Groups Combined
Morgan et al. 2020 reported no pooled effect of interventions with children as active participants and caregivers involved in at least one aspect of the intervention compared to interventions in which a caregiver was not involved on BMI [standardized mean difference (95%CI): 0.05 (−0.04, 0.15) I2 = 0%] or overweight/obesity prevalence [relative risk (95% CI): 1.02 (0.89, 1.17)] (Table 3) [35]. CoE was low (Supplementary Table S8).
3.2.2. Specific Age Groups
Brown et al. reported that interventions in the home and family setting improved BMI [MD (95% CI): −0.33 kg/m2 (−0.55, −0.10)] but not BMI z-score [−0.13 (−0.35, 0.09)] in children ≤5 years old [22]. In 6–12-year-old children, there was no effect on BMI z-score compared to the control group in one RCT [0.03 (−0.04, 0.10)] [22], and CoE was low. Brown et al. found no effect of nutrition and physical activity intervention in the home setting on BMI z-score in 13–18 years olds [0.06 (−0.13, 0.26)] [22], and CoE was very low (Table 3 and Table S8).
Based on the current evidence, nutrition and physical activity interventions in the home setting or with a caregiver may be most effective for improving BMI measures in children ≤5 years old but may have little or no effect in individuals 6–18 years old compared to no intervention.
3.3. Healthcare Setting
Four SRs examined pediatric obesity prevention interventions with nutrition in healthcare settings [22,37,49,50], and included SRs with all age groups combined [49] and for children ≤5 years old [22,37,50]. The four SRs included 12 total primary studies, and there was no overlap in primary studies between SRs.
3.3.1. Age Groups Combined
In an SR by Tissot et al. reported in 2021, primary care-led interventions in individuals 10–19 years old reduced BMI percentile or z-scores in four studies, there was no effect in four studies, and findings were unclear in the remaining study. No meta-analysis was conducted and CoE was very low due to RoB, inconsistency in findings between studies, and small sample sizes (Supplementary Table S9) [49].
3.3.2. Specific Age Groups
Three SRs identified interventions provided for children ≤5 years old. BMI z-score improved in the intervention groups compared to control groups in 2–4-year-old Latino children [MD (95%CI): −0.24 (−0.46, −0.02)] [22]. BMI z-score improved in children when nurses trained childcare staff in obesity prevention compared to controls −0.14 (−0.26 to −0.02) [50]. In the final SR, there was no significant difference in children’s prevalence of overweight according to group assignment in children ≤5 years old [37].
Based on the current evidence, nutrition and physical activity interventions delivered in the healthcare setting may reduce BMI z-scores in children ≤5 years old, but the effect on overweight or obesity prevalence and effect in older children and adolescents is uncertain.
3.4. School Setting
Thirteen SRs examined the impact of obesity prevention interventions with nutrition in the school setting in all age groups combined [20,23,27,28,29,38,40], children ≤5 years old [22], children 6–12 years old [22,25,36,41,42,46] and adolescents 13–18 years old [22]. No studies reported the cost-effectiveness of these interventions. There were 139 unique primary studies analyzed in the 13 SRs combined, and 36 primary studies were represented in more than one SR.
3.4.1. Age Groups Combined
Of the seven SRs that examined the impact of nutrition interventions in age groups combined [20,23,27,28,29,38,40], Nury et al. 2021 [38] had a high quality score, Gonclaves et al. 2021 and Durão et al. 2023 had a moderate quality score [28,29], and the remaining SRs had a critically low quality score (Table S7). Nury et al. 2021 demonstrated little to no effect of school nutrition interventions on BMI z-score [MD (95% CI): −0.09 (−0.18, 0.00)], BMI [0.03 kg/m2 (−0.10, 0.16)], or overweight and obesity prevalence [OR (95% CI): 1.19 (0.95, 1.49)] (Table 3). CoE was low due to RoB in included studies and imprecision [38]. Results were similar in SRs examining interventions influencing school food environment [29,52] and reducing sugar-sweetened beverage intake in schools [20]. However, three SRs with a critically low quality score found improvements in outcomes from school interventions (Table 3) [23,27,40].
3.4.2. Specific Age Groups
Brown et al. described no difference in BMI z-score [MD (95%CI): −0.04 (−0.09, 0.01)] or BMI [−0.05 kg/m2 (−0.14, 0.05)] for children ≤5 years old participating in nutrition and physical activity interventions in the childcare/preschool setting compared to control groups [22]. Additionally, Brown et al. demonstrated no effect on BMI z-score [MD (95%CI): 0.00 (−0.06, 0.06)] or BMI [−0.02 kg/m2 (−0.10, 0.05)(I2 = 58%)] in 13–18-year-olds (Table 3), but heterogeneity of results was very high (Supplementary Table S10).
Six SRs examined nutrition interventions for obesity prevention in children 6–12 years old [22,25,36,41,42,46]. Brown et al. 2019 and Smit et al. 2023 had a high quality score [22,46], and the remaining SRs had a critically low quality score (Table S7). Smit et al. was more recent, but Brown et al. was more comprehensive and there were only two primary studies that overlapped between these SRs. Brown et al., published in 2019, demonstrated that interventions with both diet and physical activity reduced BMI z-score [−0.04 (−0.08, −0.01)], but there was no difference in BMI [−0.04 kg/m2 (−0.10, 0.02)] [22]. Smit et al. found no effect of primary school-based obesity prevention interventions on BMI z-score [MD (95% CI): −0.08 (−0.20, 0.05)], BMI [0.06 (−0.38, 0.50)], or overweight prevalence (studies not pooled) in children 6–12 years old. Smit rated all outcomes as having very low CoE (Table 3) [46].
Nally et al. 2021 demonstrated an improvement in BMI z-scores and BMI, respectively, in children 5–12 years old [36]. Rochira et al., published in 2020,examined school garden interventions in children 6–13 years old and found an improvement in BMI percentile, but no impact on BMI z-score or BMI [42]. Cerrato-Carretero et al. 2021 and Qi et al. 2021 also found a null impact on BMI z-scores [41] and BMI [25,41].
Based on the current evidence, in all age groups combined, nutrition and physical activity interventions in the school setting may not reduce BMI z-score, BMI, or overweight or obesity prevalence. Interventions in school settings likely reduce BMI z-score in children 6–12 years old.
3.5. Community Setting
Two SRs examined the impact of obesity prevention interventions with nutrition in the community setting in all children combined [21], and in children ≤5 years old [22], 6–12 years old [21,22], and 13–17 years old [22]. One SR reported on the cost-effectiveness of community interventions in Australia [21]. Twenty-three primary studies were identified in these SRs, and there was no overlap between SRs.
3.5.1. All Age Groups
In the SR by Ananthapavan et al. published in 2018, community interventions decreased BMI z-score [MD (95% CI): −0.07 (−0.13, −0.01)] in Australia [21], and CoE was low (Table 4). Using results from included studies, authors analyzed cost-effectiveness and found that the mean incremental cost-effectiveness ratio (ICER) was AUD 8155 (AUD 237 to AUD 81,021) per health-adjusted life year, and there was a 95% probability of interventions being cost-effective at the defined threshold [21]. Evidence certainty was low (Supplementary Table S11).
3.5.2. Specific Age Groups
Brown et al. found that diet and physical activity interventions had no effect on BMI z-score in children ≤5 years old, but reduced BMI by −0.59 kg/m2 (−0.94, −0.24) [22] (Table 3).
Two SRs reported on intervention efficacy in children around 6–12 years old [21,22]. Brown et al. found no effect of community interventions, including nutrition and physical activity, on BMI z-score [−0.04 (−0.39, 0.31); I2 = 94%] or BMI kg/m2 [−0.08 (−0.29, 0.13); I2 = 25%] [22]. Ananthapavan et al. found an improvement in BMI z-score, but their total sample size was unclear. Ananthapavan et al. 2018 found no effect on BMI z-score in adolescents 12–18 years old [MD (95% CI): −0.02 (−0.07, 0.03)] [21]. Brown had a high quality score and Ananthapavan had a critically low quality score. CoE ranged from low to very low (Table 3 and Table S11).
Based on the current evidence, pediatric obesity prevention interventions with nutrition in the community setting may improve BMI z-score and be cost-effective in all age groups combined. Nutrition and physical activity interventions in the community setting may decrease BMI in children ≤5 years old, but interventions were ineffective, or evidence was lacking for older children and adolescents.
3.6. Federal Food Assistance Programs
Six SRs examined the impact of federal food assistance programs on obesity prevention. Programs assessed included the Supplemental Nutrition Program for Women, Infants and Children (WIC) [24], universal school meals [26,27], the Supplemental Nutrition Assistance Program (SNAP) [31], the Child and Adult Care Food Program (CACFP) [32], and food assistance programs in general [39]. Twenty-two primary studies were represented in total and only one study was cited in more than one SR. CoE is described in Supplementary Table S12.
3.6.1. All Age Groups
Hudak et al., published in 2019, investigated the impact of SNAP in participants 2–18 years old. Of the studies that addressed selection bias, results were heterogeneous, including lower risk of overweight or obesity in participants who were boys or younger girls but increased risk for girls 5–18 years old or who were long-term participants. Results were not pooled in the meta-analysis [31].
Kenney et al. 2023 identified one study with 4050 participants ages 2–18 years old that reported that CACFP participation was not associated with the prevalence of overweight and obesity [32].
Both Cohen et al. (2021) and Dabravolskaj et al. (2020) examined the impact of universal school meals. Cohen et al. demonstrated mixed findings for the effect on BMI z-score, and no effect on BMI or obesity prevalence [26]. Dabravolskaj et al. agreed with these findings [27].
3.6.2. Specific Age Groups
Caulfield et al. 2022 examined the impact of the revised 2009 WIC food package for children ≤5 years old and identified three studies with >16 million participants [24]. The authors concluded that the revised food package reduced overweight and obesity prevalence and rated CoE as low.
Olstad et al., published in 2017, evaluated primary studies targeting government policies for disadvantaged populations. Primary studies investigating the SNAP program were excluded, and just one primary quasi-experimental study was identified that reported that the USDA Fresh Fruit and Vegetable Program decreased BMI z-score and BMI in elementary school students after four years [39].
Based on the current evidence, few SRs assessed the impact of federal food assistance programs on the prevention of pediatric obesity. The 2009 revised WIC package reduced obesity prevalence in young children, and a USDA program providing fresh fruits and vegetables outside of the school reduced BMI z-score and BMI in elementary-aged children. The impact of the SNAP program was mixed, depending on the sub-population examined. The CACFP program and universal school meals did not impact BMI outcomes or obesity prevalence.
3.7. Electronic Interventions
Two SRs examined the effects of electronic interventions with nutrition to prevent pediatric obesity [45,48]. There were eight primary studies represented in the SRs with no overlap in primary studies between SRs. Suleiman-Martos et al. 2021 identified five RCTs, three of which demonstrated an improvement of gamification on BMI z-scores and two of which found no effect. Results from two of these trials were pooled, and there was no effect on BMI z-scores [MD (95% CI): −0.05 (−0.21, 0.11)] [48]. Silva et al. 2022 found no effect of computer-based nutrition interventions compared to controls on BMI in 10–19-year-olds in three trials [−0.02 kg/m2 (−0.18, 0.14)] (Table 3, Supplementary Table S13) [45]. There may be no effect of electronic nutrition interventions on BMI or BMI z-score in children and adolescents.
4. Discussion
This umbrella review analyzed 31 recent SRs examining the impact of pediatric obesity prevention interventions with a nutrition component. In SRs with pediatric individuals aged 2–17 years combined, interventions with both nutrition and physical activity were effective and cost-effective in all settings combined, and in the community setting specifically. In children ≤5 years old, interventions in the home and family, community, and healthcare settings all demonstrated some efficacy, as did the 2009 revised WIC package. In children 6–12 years old, interventions in schools were most effective and a federal food assistance program providing fresh fruits and vegetables also may be effective. Limited evidence in individuals 13–17 years old did not demonstrate efficacy for nutrition interventions aiming to prevent obesity (Figure 2). CoE was generally low due to RoB in included studies, inconsistency in results between studies, and imprecision in findings.
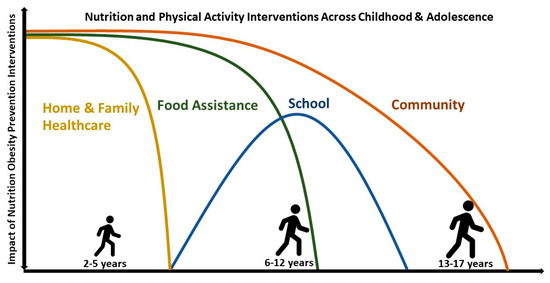
Figure 2.
Impact of obesity pediatric prevention interventions with nutrition according to age and intervention setting. Nutrition and physical activity interventions in all settings and age groups combined are effective in improving BMI measures and overweight and obesity prevalence, as were interventions in all age groups combined in the community setting. Interventions in the home and family setting and in healthcare settings were beneficial for children ≤5 years old, school interventions were most effective for children 6–12 years old, and there is evidence of benefits from food assistance programs in children ≤12 years old. Beyond the impacts of interventions seen in all age groups combined, little is known about effective interventions for adolescents 13–17 years old.
A 2019 umbrella review of pediatric obesity prevention interventions demonstrated that mixed interventions were most effective in improving cardiovascular profile, but had little impact on BMI, though efficacy was not examined according to intervention type or participant age [7]. In another recent umbrella review, Denova-Gutierrez [6] identified five SRs targeting pediatric obesity prevention in children 6–12 years old and described that multi-component interventions, including nutrition, physical activity, and behavior change were most effective in preventing pediatric overweight and obesity [6]. However, the authors also described a gap in methodological quality in primary studies, which prevents the establishment of robust recommendations. This umbrella review supports and expands upon these findings by demonstrating the efficacy of obesity prevention interventions with at least a nutrition component in specific age groups and settings, thus providing a potential path for effective obesity prevention interventions throughout childhood and adolescence.
The impacts of pediatric obesity interventions identified in this umbrella review were heterogeneous, which can be explained by the wide variety of interventions delivered and of methods used to implement interventions. Future SRs and umbrella reviews may focus on the efficacy of specific implementation strategies for nutrition interventions to provide robust guidance on the best methods for delivering interventions to children and adolescents in the general population.
Among the target audiences for this umbrella review are nutrition program funders and policymakers, as these individuals are responsible for facilitating effective interventions to prevent pediatric obesity by using available resources most efficiently. However, there was very little evidence available about the cost-effectiveness of pediatric obesity prevention programs with nutrition to support policy decisions. After the search was performed for this umbrella review, Sultana et al. published a SR in 2023, examining the economic evidence for community-based interventions for pediatric obesity prevention [53]. Authors identified five studies conducting cost-utility analysis, three of which found interventions to be cost-effective. An additional primary study reported a cost-saving return-on-investment ratio [53]. These results were consistent with those found by Ananthapavan et al. in 2019, who reported that community interventions may be cost-effective [21]. Disease prevention may be difficult to prioritize in the context of what seem like more pressing health needs. More research investigating the cost-efficacy of pediatric obesity prevention programs is crucial for demonstrating that facilitating healthy lifestyle behaviors can prevent not only the suffering associated with obesity-related diseases but also the financial costs of treating these diseases.
This umbrella review utilized a social-ecological model to examine the contexts in which interventions were most effective. However, a space that is not typically represented in the social-ecological framework is that of digital and electronic media, which extend throughout home, school, and community settings and are an integral part of food assistance programs. There were very few SRs examining the efficacy of electronic interventions, and neither of those included in this study found that electronic interventions were efficacious in preventing obesity. More research is needed to leverage the time children and adolescents are spending with electronic devices to contribute to healthy lifestyle behaviors.
4.1. Strengths and Limitations
Results from this umbrella review provide a comprehensive picture of the impact of pediatric obesity prevention programs with a nutrition component and demonstrate the need for a multi-faceted approach to establishing healthy habits that are dynamic according to needs and preferences throughout childhood and adolescence. This umbrella review utilized rigorous methods, including a systematic search, a screening process, and rigorous evidence synthesis. The wide breadth of research examined allows for the comparison of quantitative evidence from the highest-quality SRs available and can guide policymakers to support evidence-based programs. Finally, although it was not possible to perform novel meta-analyses due to the lack of information reported in many SRs, this umbrella review graded a CoE for each age group in each setting, which provides a common metric by which to compare evidence availability and efficacy.
A limitation of this umbrella review was the gap in the underlying research, particularly on effective interventions for teenagers in the general population, which was also demonstrated in an overview of SRs by Flodgren et al. published 2020 [9], and in research on electronic and food assistance interventions. Another limitation was the limited outcomes examined in this umbrella review. Although focusing on BMI measures and overweight and obesity prevalence allowed for the inclusion of a broad evidence base and comparisons between SRs, the goal of obesity prevention programs is not to change a number on a scale or chart, but rather to improve the health and well-being of children and adolescents now and in their futures. Thus, future studies and SRs should aim to assess outcomes that are more client-centered such as the development of T2DM, quality of life, or academic achievements.
4.2. Implications for Practice
Nutrition practitioners are a key target audience of this umbrella review. This review highlights that efforts to prevent pediatric obesity may be successful when delivered in the context of multi-component interventions that include nutrition. Although interventions ideally include interdisciplinary practitioners, nutrition practitioners can and should encourage the meeting of national physical activity recommendations [54] in addition to providing nutrition interventions. Practitioners should be aware that the efficacy of certain interventions varies greatly according to participant age. Thus, a life-course approach to obesity prevention should be implemented to consistently deliver the most effective interventions and the most optimal developmental stage to ensure long-term benefits into adulthood. Nutrition practitioners, funders, and policymakers should advocate for increased access to effective prevention services for children across developmental stages and settings [4].
5. Conclusions
Multi-component pediatric obesity prevention interventions with a nutrition component may improve BMI outcomes and overweight and obesity prevalence and may be cost-effective. Interventions in different settings may have varying efficacy for different age groups, and obesity prevention approaches should be tailored to developmental stages to ensure appropriateness and efficacy. Although interventions in the home, healthcare, and community settings have proven efficacious for young children and school interventions have proven efficacious for elementary-aged children, it is unclear which type of interventions may be effective for teens. Program funders and policymakers can facilitate investment in a life-course approach to disease prevention by advocating for the implementation of interventions tailored to developmental stages and research investigating effective methods in adolescents.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu15245097/s1.
Author Contributions
Conceptualization, M.R. and D.H.; Methodology, M.R.; Analysis, M.R.; Data Curation, M.R. and D.H.; Writing—Original Draft Preparation, M.R.; Writing—Review and Editing, M.R. and D.H.; Visualization, M.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Acknowledgments
The authors would like to acknowledge the content experts who contributed to the original umbrella review and the Position Paper that it supported, including Deanna M. Hoelscher; Lynn S. Brann; and Sara O’Brien.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Balasundaram, P.; Krishna, S. Obesity Effects on Child Health. StatPerls. 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK570613/ (accessed on 1 December 2023).
- U.S. Department of Health and Human Services. Healthy People 2030. Available online: https://health.gov/healthypeople/objectives-and-data/browse-objectives/overweight-and-obesity/reduce-proportion-children-and-adolescents-obesity-nws-04 (accessed on 18 October 2023).
- Grossman, D.C.; Bibbins-Domingo, K.; Curry, S.J.; Barry, M.J.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W., Jr.; Kemper, A.R.; Krist, A.H.; Kurth, A.E.; et al. Screening for Obesity in Children and Adolescents: US Preventive Services Task Force Recommendation Statement. JAMA 2017, 317, 2417–2426. [Google Scholar] [CrossRef] [PubMed]
- Hoelscher, D.M.; Brann, L.S.; O’Brien, S.; Handu, D.; Rozga, M. Prevention of Pediatric Overweight and Obesity: Position of the Academy of Nutrition and Dietetics Based on an Umbrella Review of Systematic Reviews. J. Acad. Nutr. Diet 2022, 122, 410–423.e416. [Google Scholar] [CrossRef] [PubMed]
- Satter, E. Child Feeding Ages and Stages. Available online: https://www.ellynsatterinstitute.org/how-to-feed/child-feeding-ages-and-stages/ (accessed on 18 October 2023).
- Denova-Gutiérrez, E.; González-Rocha, A.; Méndez-Sánchez, L.; Araiza-Nava, B.; Balderas, N.; López, G.; Tolentino-Mayo, L.; Jauregui, A.; Hernández, L.; Unikel, C.; et al. Overview of Systematic Reviews of Health Interventions for the Prevention and Treatment of Overweight and Obesity in Children. Nutrients 2023, 15, 773. [Google Scholar] [CrossRef] [PubMed]
- Bahia, L.; Schaan, C.W.; Sparrenberger, K.; Abreu, G.A.; Barufaldi, L.A.; Coutinho, W.; Schaan, B.D. Overview of meta-analysis on prevention and treatment of childhood obesity. J. Pediatr. 2019, 95, 385–400. [Google Scholar] [CrossRef] [PubMed]
- Rozga, M.; Handu, D. Current Systems-Level Evidence on Nutrition Interventions to Prevent and Treat Cardiometabolic Risk in the Pediatric Population: An Evidence Analysis Center Scoping Review. J. Acad. Nutr. Diet 2021, 121, 2501–2523. [Google Scholar] [CrossRef] [PubMed]
- Flodgren, G.M.; Helleve, A.; Lobstein, T.; Rutter, H.; Klepp, K.-I. Primary prevention of overweight and obesity in adolescents: An overview of systematic reviews. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2020, 21, e13102. [Google Scholar] [CrossRef] [PubMed]
- Ohri-Vachaspati, P.; DeLia, D.; DeWeese, R.S.; Crespo, N.C.; Todd, M.; Yedidia, M.J. The relative contribution of layers of the Social Ecological Model to childhood obesity. Public Health Nutr. 2015, 18, 2055–2066. [Google Scholar] [CrossRef]
- Pollock, M.F.R.; Becker, L.A.; Pieper, D.; Hartling, L. Chapter V: Overviews of Reviews. In Cochrane Handbook for Systematic Reviews of Interventions Version 6.2; Higgins, J.P.T.T.J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: London, UK, 2021; Available online: https://training.cochrane.org/handbook/current/chapter-v (accessed on 30 November 2023).
- Handu, D.; Moloney, L.; Wolfram, T.; Ziegler, P.; Acosta, A.; Steiber, A. Academy of Nutrition and Dietetics Methodology for Conducting Systematic Reviews for the Evidence Analysis Library. J. Acad. Nutr. Diet 2016, 116, 311–318. [Google Scholar] [CrossRef]
- Gates, M.; Gates, A.; Pieper, D.; Fernandes, R.M.; Tricco, A.C.; Moher, D.; Brennan, S.E.; Li, T.; Pollock, M.; Lunny, C.; et al. Reporting guideline for overviews of reviews of healthcare interventions: Development of the PRIOR statement. BMJ 2022, 378, e070849. [Google Scholar] [CrossRef]
- Rozga, M.; Handu, D. Interventions to Prevent Pediatric Overweight and Obesity: An Umbrella Review of Systematic Reviews. Available online: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=443033 (accessed on 13 October 2023).
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Academy of Nutrition and Dietetics Evidence Analysis Library. Pediatric Overweight and Obesity Prevention. Available online: https://www.andeal.org/topic.cfm?menu=5296&cat=6132 (accessed on 18 October 2023).
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef]
- Abdel Rahman, A.; Jomaa, L.; Kahale, L.A.; Adair, P.; Pine, C. Effectiveness of behavioral interventions to reduce the intake of sugar-sweetened beverages in children and adolescents: A systematic review and meta-analysis. Nutr. Rev. 2018, 76, 88–107. [Google Scholar] [CrossRef]
- Ananthapavan, J.; Nguyen, P.K.; Bowe, S.J.; Sacks, G.; Mantilla Herrera, A.M.; Swinburn, B.; Brown, V.; Sweeney, R.; Lal, A.; Strugnell, C.; et al. Cost-effectiveness of community-based childhood obesity prevention interventions in Australia. Int. J. Obes. 2019, 43, 1102–1112. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.; Moore, T.H.; Hooper, L.; Gao, Y.; Zayegh, A.; Ijaz, S.; Elwenspoek, M.; Foxen, S.C.; Magee, L.; O’Malley, C.; et al. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2019, 7, Cd001871. [Google Scholar] [CrossRef] [PubMed]
- Buchanan, L.R.; Wethington, H.R.; Finnie, R.K.C.; Mercer, S.L.; Merlo, C.; Michael, S.; Sliwa, S.; Pratt, C.A.; Ochiai, E. A Community Guide Systematic Review: School Dietary and Physical Activity Interventions. Am. J. Prev. Med. 2023, 64, 441–451. [Google Scholar] [CrossRef] [PubMed]
- Caulfield, L.E.; Bennett, W.L.; Gross, S.M.; Hurley, K.M.; Ogunwole, S.M.; Venkataramani, M.; Lerman, J.L.; Zhang, A.; Sharma, R.; Bass, E.B. AHRQ Comparative Effectiveness Reviews. In Maternal and Child Outcomes Associated With the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC); Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2022. [Google Scholar]
- Cerrato-Carretero, P.; Roncero-Martín, R.; Pedrera-Zamorano, J.D.; López-Espuela, F.; Puerto-Parejo, L.M.; Sánchez-Fernández, A.; Canal-Macías, M.L.; Moran, J.M.; Lavado-García, J.M. Long-Term Dietary and Physical Activity Interventions in the School Setting and Their Effects on BMI in Children Aged 6–12 Years: Meta-Analysis of Randomized Controlled Clinical Trials. Healthcare 2021, 9, 396. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.F.W.; Hecht, A.A.; McLoughlin, G.M.; Turner, L.; Schwartz, M.B. Universal School Meals and Associations with Student Participation, Attendance, Academic Performance, Diet Quality, Food Security, and Body Mass Index: A Systematic Review. Nutrients 2021, 13, 911. [Google Scholar] [CrossRef] [PubMed]
- Dabravolskaj, J.; Montemurro, G.; Ekwaru, J.P.; Wu, X.Y.; Storey, K.; Campbell, S.; Veugelers, P.J.; Ohinmaa, A. Effectiveness of school-based health promotion interventions prioritized by stakeholders from health and education sectors: A systematic review and meta-analysis. Prev. Med. Rep. 2020, 19, 101138. [Google Scholar] [CrossRef]
- Durão, S.; Wilkinson, M.; Davids, E.L.; Gerritsen, A.; Kredo, T. Effects of policies or interventions that influence the school food environment on children’s health and nonhealth outcomes: A systematic review. Nutr. Rev. 2023, nuad059. [Google Scholar] [CrossRef]
- Gonçalves, V.S.S.; Figueiredo, A.; Silva, S.A.; Silva, S.U.; Ronca, D.B.; Dutra, E.S.; Carvalho, K.M.B. The food environment in schools and their immediate vicinities associated with excess weight in adolescence: A systematic review and meta-analysis. Health Place 2021, 71, 102664. [Google Scholar] [CrossRef] [PubMed]
- Hayba, N.; Elkheir, S.; Hu, J.; Allman-Farinelli, M. Effectiveness of Lifestyle Interventions for Prevention of Harmful Weight Gain among Adolescents from Ethnic Minorities: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 6059. [Google Scholar] [CrossRef] [PubMed]
- Hudak, K.M.; Racine, E.F. The Supplemental Nutrition Assistance Program and Child Weight Status: A Review. Am. J. Prev. Med. 2019, 56, 882–893. [Google Scholar] [CrossRef] [PubMed]
- Kenney, E.L.; Tucker, K.; Plummer, R.S.; Mita, C.; Andreyeva, T. The Child and Adult Care Food Program and young children’s health: A systematic review. Nutr. Rev. 2023, 81, nuad016. [Google Scholar] [CrossRef] [PubMed]
- Kornet-van der Aa, D.A.; Altenburg, T.M.; van Randeraad-van der Zee, C.H.; Chinapaw, M.J. The effectiveness and promising strategies of obesity prevention and treatment programmes among adolescents from disadvantaged backgrounds: A systematic review. Obes. Rev. 2017, 18, 581–593. [Google Scholar] [CrossRef] [PubMed]
- Long, Q.; Zhang, T.; Chen, F.; Wang, W.; Chen, X.; Ma, M. Effectiveness of dietary interventions on weight outcomes in childhood: A systematic review meta-analysis of randomized controlled trials. Transl. Pediatr. 2021, 10, 701–714. [Google Scholar] [CrossRef] [PubMed]
- Morgan, E.H.; Schoonees, A.; Sriram, U.; Faure, M.; Seguin-Fowler, R.A. Caregiver involvement in interventions for improving children’s dietary intake and physical activity behaviors. Cochrane Database Syst. Rev. 2020, 1, Cd012547. [Google Scholar] [CrossRef]
- Nally, S.; Carlin, A.; Blackburn, N.E.; Baird, J.S.; Salmon, J.; Murphy, M.H.; Gallagher, A.M. The Effectiveness of School-Based Interventions on Obesity-Related Behaviours in Primary School Children: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Children 2021, 8, 489. [Google Scholar] [CrossRef]
- Narzisi, K.; Simons, J. Interventions that prevent or reduce obesity in children from birth to five years of age: A systematic review. J. Child Health Care 2020, 25, 320–334. [Google Scholar] [CrossRef]
- Nury, E.; Stadelmaier, J.; Morze, J.; Nagavci, B.; Grummich, K.; Schwarzer, G.; Hoffmann, G.; Angele, C.M.; Steinacker, J.M.; Wendt, J.; et al. Effects of nutritional intervention strategies in the primary prevention of overweight and obesity in school settings: Systematic review and network meta-analysis. BMJ Med. 2022, 1, e000346. [Google Scholar] [CrossRef] [PubMed]
- Olstad, D.L.; Ancilotto, R.; Teychenne, M.; Minaker, L.M.; Taber, D.R.; Raine, K.D.; Nykiforuk, C.I.J.; Ball, K. Can targeted policies reduce obesity and improve obesity-related behaviours in socioeconomically disadvantaged populations? A systematic review. Obes. Rev. 2017, 18, 791–807. [Google Scholar] [CrossRef] [PubMed]
- Pineda, E.; Bascunan, J.; Sassi, F. Improving the school food environment for the prevention of childhood obesity: What works and what doesn’t. Obes. Rev. 2021, 22, e13176. [Google Scholar] [CrossRef] [PubMed]
- Qi, Y.; Hamzah, S.H.; Gu, E.; Wang, H.; Xi, Y.; Sun, M.; Rong, S.; Lin, Q. Is School Gardening Combined with Physical Activity Intervention Effective for Improving Childhood Obesity? A Systematic Review and Meta-Analysis. Nutrients 2021, 13, 2605. [Google Scholar] [CrossRef] [PubMed]
- Rochira, A.; Tedesco, D.; Ubiali, A.; Fantini, M.P.; Gori, D. School Gardening Activities Aimed at Obesity Prevention Improve Body Mass Index and Waist Circumference Parameters in School-Aged Children: A Systematic Review and Meta-Analysis. Child. Obes. 2020, 16, 154–173. [Google Scholar] [CrossRef]
- Salam, R.A.; Padhani, Z.A.; Das, J.K.; Shaikh, A.Y.; Hoodbhoy, Z.; Jeelani, S.M.; Lassi, Z.S.; Bhutta, Z.A. Effects of Lifestyle Modification Interventions to Prevent and Manage Child and Adolescent Obesity: A Systematic Review and Meta-Analysis. Nutrients 2020, 12, 2208. [Google Scholar] [CrossRef]
- Seral-Cortes, M.; De Miguel-Etayo, P.; Zapata, P.; Miguel-Berges, M.L.; Moreno, L.A. Effectiveness and process evaluation in obesity and type 2 diabetes prevention programs in children: A systematic review and meta-analysis. BMC Public Health 2021, 21, 348. [Google Scholar] [CrossRef]
- Beck Silva, K.B.; Miranda Pereira, E.; Santana, M.L.P.; Costa, P.R.F.; Silva, R.C.R. Effects of computer-based interventions on food consumption and anthropometric parameters of adolescents: A systematic review and metanalysis. Crit. Rev. Food Sci. Nutr. 2022, 1–13. [Google Scholar] [CrossRef]
- Smit, M.S.; Boelens, M.; Mölenberg, F.J.M.; Raat, H.; Jansen, W. The long-term effects of primary school-based obesity prevention interventions in children: A systematic review and meta-analysis. Pediatr. Obes. 2023, 18, e12997. [Google Scholar] [CrossRef]
- Specchia, M.L.; Barbara, A.; Campanella, P.; Parente, P.; Mogini, V.; Ricciardi, W.; Damiani, G. Highly-integrated programs for the prevention of obesity and overweight in children and adolescents: Results from a systematic review and meta-analysis. Ann. Ist. Super Sanita 2018, 54, 332–339. [Google Scholar] [CrossRef]
- Suleiman-Martos, N.; García-Lara, R.A.; Martos-Cabrera, M.B.; Albendín-García, L.; Romero-Béjar, J.L.; Cañadas-De la Fuente, G.A.; Gómez-Urquiza, J.L. Gamification for the Improvement of Diet, Nutritional Habits, and Body Composition in Children and Adolescents: A Systematic Review and Meta-Analysis. Nutrients 2021, 13, 2478. [Google Scholar] [CrossRef] [PubMed]
- Tissot, H.; Pfarrwaller, E.; Haller, D.M. Primary care prevention of cardiovascular risk behaviors in adolescents: A systematic review. Prev. Med. 2021, 142, 106346. [Google Scholar] [CrossRef] [PubMed]
- Whitehead, L.; Kabdebo, I.; Dunham, M.; Quinn, R.; Hummelshoj, J.; George, C.; Denney-Wilson, E. The effectiveness of nurse-led interventions to prevent childhood and adolescent overweight and obesity: A systematic review of randomised trials. J. Adv. Nurs. 2021, 77, 4612–4631. [Google Scholar] [CrossRef] [PubMed]
- Hayba, N.; Rissel, C.; Allman Farinelli, M. Effectiveness of lifestyle interventions in preventing harmful weight gain among adolescents: A systematic review of systematic reviews. Obes. Rev. 2021, 22, e13109. [Google Scholar] [CrossRef]
- Durao, S.; Visser, M.E.; Ramokolo, V.; Oliveira, J.M.; Schmidt, B.-M.; Balakrishna, Y.; Brand, A.; Kristjansson, E.; Schoonees, A. Community-level interventions for improving access to food in low- and middle-income countries. Cochrane Database Syst. Rev. 2020, 8, CD011504. [Google Scholar] [CrossRef] [PubMed]
- Sultana, M.; Nichols, M.; Moodie, M.; Allender, S.; Brown, V. A systematic review of economic evidence for community-based obesity prevention interventions in children. Obes. Rev. 2023, 24, e13592. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans; U.S. Department of Health and Human Services: Washington, DC, USA, 2008. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).