Comparative Analysis of Dietary and Supplemental Intake of Calcium and Vitamin D among Canadian Older Adults with Heart Disease and/or Osteoporosis in 2004 and 2015
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Analytical Sample
2.3. Dietary and Supplemental Calcium and Vitamin D
2.4. Calcium and Vitamin D Requirements
2.5. Chronic Diseases
2.6. Definitions and Covariates
2.7. Statistical Analyses
- (i)
- The sequence of the 24 h recall, categorized as day 1 or day 2,
- (ii)
- The day of the week when the 24 h recall data were obtained and categorized as weekday or weekend,
- (iii)
- Energy consumption from food during the 24 h recall period.
3. Results
3.1. Sociodemographic Characteristics
3.2. Factors Associated with Osteoporosis and Heart Disease among Canadians Aged 50 and Older in 2004 and 2015
3.3. Dietary and Supplemental Intake of Calcium among Individuals with Heart Disease, Osteoporosis, or Both Conditions in 2004 and 2015, Comparing Supplement Users and Non-Users
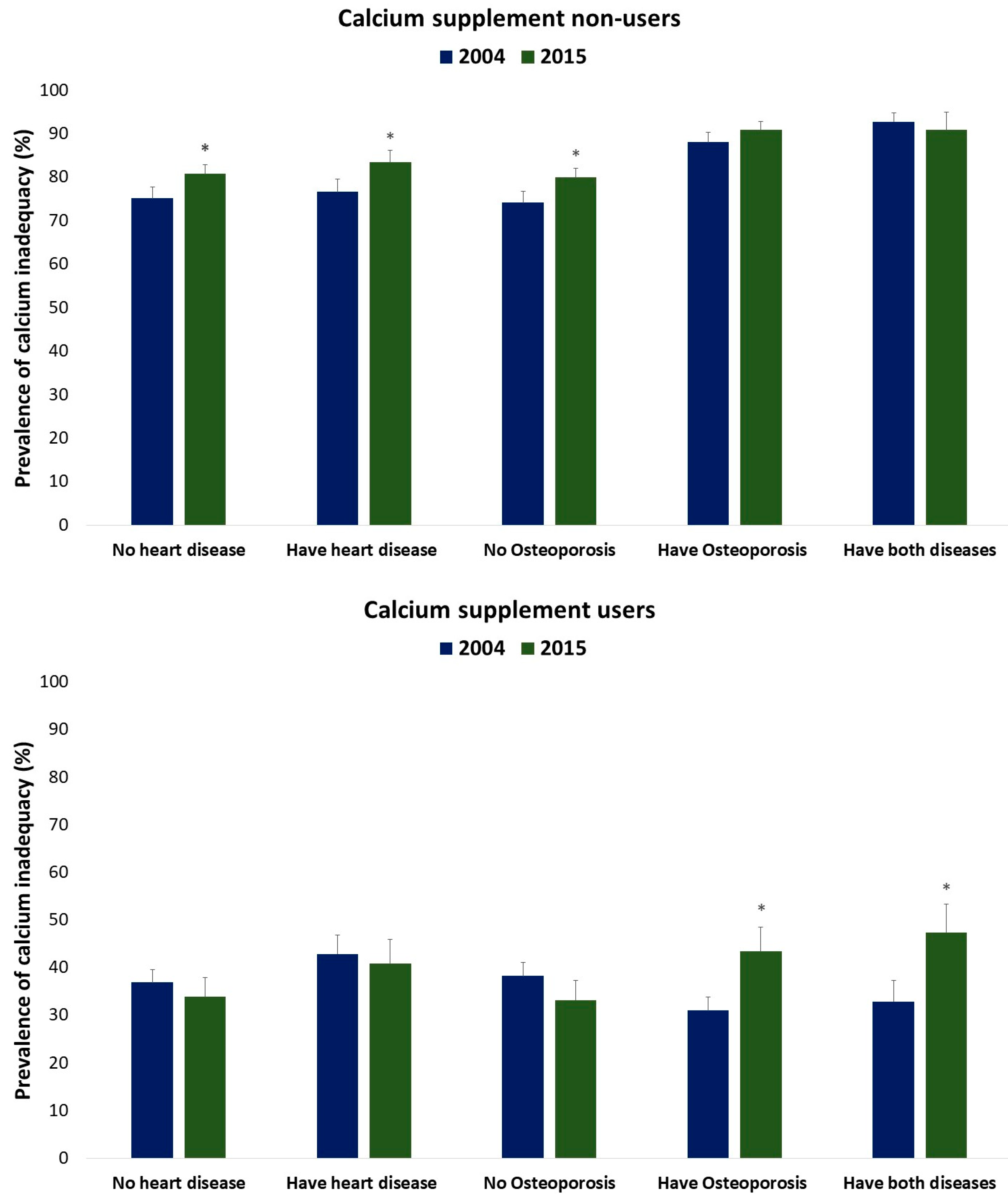
3.4. Prevalence of Calcium Inadequacy among Individuals with Heart Disease, Osteoporosis, or Both Conditions in 2004 and 2015, Comparing Supplement Users and Non-Users
3.5. Dietary and Supplemental Intake of Vitamin D among Individuals with Heart Disease, Osteoporosis, or Both in 2004 and 2015, Comparing Supplement Users and Non-Users
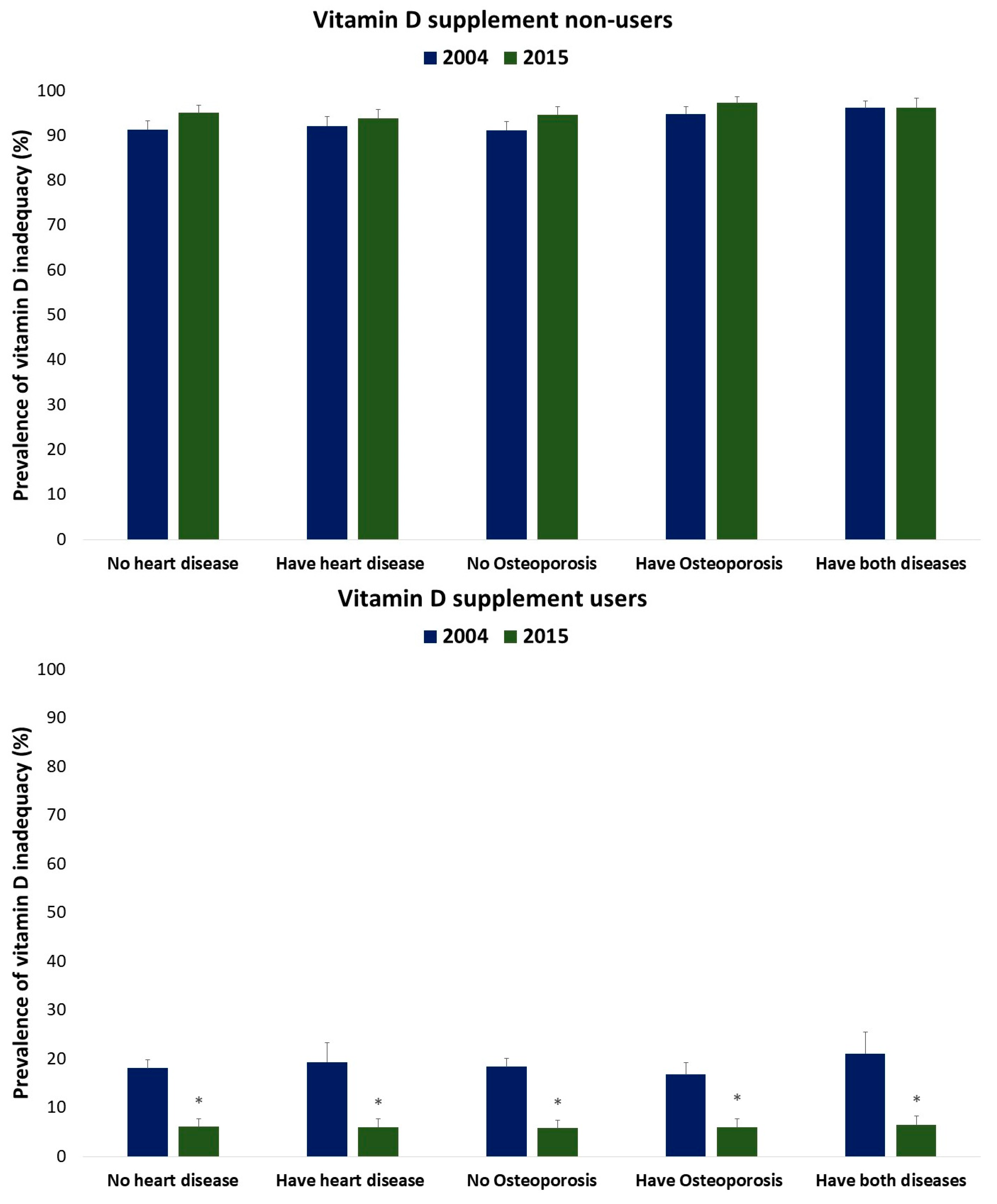
3.6. Prevalence of Vitamin D Inadequacy among Individuals with Heart Disease, Osteoporosis, or Both in 2004 and 2015, Comparing Supplement Users and Non-Users
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Noncommunicable Diseases. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 1 October 2023).
- Beaglehole, R.; Ebrahim, S.; Reddy, S.; Voûte, J.; Leeder, S. Prevention of chronic diseases: A call to action. Lancet 2007, 370, 2152–2157. [Google Scholar] [CrossRef]
- World Health Organization. Noncommunicable Diseases Country Profiles 2018. Available online: https://www.who.int/publications/i/item/9789241514620 (accessed on 1 October 2023).
- Health Canada. How Healthy are Canadians? A Trend Analysis of the Health of Canadians from a Healthy Living and Chronic Disease Perspective. Available online: https://www.canada.ca/en/public-health/services/publications/healthy-living/how-healthy-canadians.html (accessed on 1 October 2023).
- Centers for Disease Control and Prevention. About Heart Disease. Available online: https://www.cdc.gov/heartdisease/about.htm (accessed on 4 December 2023).
- Coughlan, T.; Dockery, F. Osteoporosis and fracture risk in older people. Clin. Med. 2014, 14, 187. [Google Scholar] [CrossRef]
- Warburton, D.E.; Nicol, C.W.; Gatto, S.N.; Bredin, S.S. Cardiovascular disease and osteoporosis: Balancing risk management. Vasc. Health Risk Manag. 2007, 3, 673. [Google Scholar]
- Sprini, D.; Rini, G.B.; Di Stefano, L.; Cianferotti, L.; Napoli, N. Correlation between osteoporosis and cardiovascular disease. Clin. Cases Miner. Bone Metab. 2014, 11, 117. [Google Scholar] [CrossRef]
- Tarride, J.-E.; Hopkins, R.; Leslie, W.; Morin, S.; Adachi, J.; Papaioannou, A.; Bessette, L.; Brown, J.; Goeree, R. The burden of illness of osteoporosis in Canada. Osteoporos. Int. 2012, 23, 2591–2600. [Google Scholar] [CrossRef]
- Manuel, D.; Leung, M.; Nguyen, K.; Tanuseputro, P.; Johansen, H. Burden of cardiovascular disease in Canada. Can. J. Cardiol. 2003, 19, 997–1004. [Google Scholar]
- Levis, S.; Lagari, V.S. The role of diet in osteoporosis prevention and management. Curr. Osteoporos. Rep. 2012, 10, 296–302. [Google Scholar] [CrossRef]
- Ignarro, L.J.; Balestrieri, M.L.; Napoli, C. Nutrition, physical activity, and cardiovascular disease: An update. Cardiovasc. Res. 2007, 73, 326–340. [Google Scholar] [CrossRef]
- Sunyecz, J.A. The use of calcium and vitamin D in the management of osteoporosis. Ther. Clin. Risk Manag. 2008, 4, 827. [Google Scholar] [CrossRef]
- Garriguet, D. Bone health: Osteoporosis, calcium and vitamin D. Health Rep. 2011, 22, 7. [Google Scholar]
- Ross, A.C.; Manson, J.E.; Abrams, S.A.; Aloia, J.F.; Brannon, P.M.; Clinton, S.K.; Durazo-Arvizu, R.A.; Gallagher, J.C.; Gallo, R.L.; Jones, G. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: What clinicians need to know. J. Clin. Endocrinol. Metab. 2011, 96, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine Committee to Review Dietary Reference Intakes for Vitamin D and Calcium. The National Academies Collection: Reports funded by National Institutes of Health. In Dietary Reference Intakes for Calcium and Vitamin D; Ross, A.C., Taylor, C.L., Yaktine, A.L., Del Valle, H.B., Eds.; National Academies Press (US) Copyright © 2011, National Academy of Sciences: Washington, DC, USA, 2011. [Google Scholar] [CrossRef]
- Whiting, S.J.; Langlois, K.A.; Vatanparast, H.; Greene-Finestone, L.S. The vitamin D status of Canadians relative to the 2011 Dietary Reference Intakes: An examination in children and adults with and without supplement use. Am. J. Clin. Nutr. 2011, 94, 128–135. [Google Scholar] [CrossRef]
- Poliquin, S.; Joseph, L.; Gray-Donald, K. Calcium and vitamin D intakes in an adult Canadian population. Can. J. Diet. Pract. Res. 2009, 70, 21–27. [Google Scholar] [CrossRef]
- Umesawa, M.; Iso, H.; Date, C.; Yamamoto, A.; Toyoshima, H.; Watanabe, Y.; Kikuchi, S.; Koizumi, A.; Kondo, T.; Inaba, Y. Dietary intake of calcium in relation to mortality from cardiovascular disease: The JACC Study. Stroke 2006, 37, 20–26. [Google Scholar] [CrossRef]
- Sun, Q.; Shi, L.; Rimm, E.B.; Giovannucci, E.L.; Hu, F.B.; Manson, J.E.; Rexrode, K.M. Vitamin D intake and risk of cardiovascular disease in US men and women. Am. J. Clin. Nutr. 2011, 94, 534–542. [Google Scholar] [CrossRef]
- Larsson, S.C.; Orsini, N.; Wolk, A. Dietary calcium intake and risk of stroke: A dose-response meta-analysis. Am. Clin. Nutr. 2013, 97, 951–957. [Google Scholar] [CrossRef]
- Xiao, Q.; Murphy, R.A.; Houston, D.K.; Harris, T.B.; Chow, W.-H.; Park, Y. Dietary and supplemental calcium intake and cardiovascular disease mortality: The National Institutes of Health–AARP diet and health study. JAMA Intern. Med. 2013, 173, 639–646. [Google Scholar] [CrossRef]
- Li, K.; Kaaks, R.; Linseisen, J.; Rohrmann, S. Associations of dietary calcium intake and calcium supplementation with myocardial infarction and stroke risk and overall cardiovascular mortality in the Heidelberg cohort of the European Prospective Investigation into Cancer and Nutrition study (EPIC-Heidelberg). Heart 2012, 98, 920–925. [Google Scholar]
- Paik, J.M.; Curhan, G.C.; Sun, Q.; Rexrode, K.M.; Manson, J.; Rimm, E.B.; Taylor, E.N. Calcium supplement intake and risk of cardiovascular disease in women. Osteoporos. Int. 2014, 25, 2047–2056. [Google Scholar] [CrossRef]
- Hsia, J.; Heiss, G.; Ren, H.; Allison, M.; Dolan, N.C.; Greenland, P.; Heckbert, S.R.; Johnson, K.C.; Manson, J.E.; Sidney, S. Calcium/vitamin D supplementation and cardiovascular events. Circulation 2007, 115, 846–854. [Google Scholar] [CrossRef]
- Statistics Canada. Canadian Community Health Survey (CCHS) Cycle 2.2 (2004) Nutrition—General Health (including Vitamin & Mineral Supplements) & 24-Hour Dietary Recall Components User Guide. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwj6nrX9rOX0AhX_FDQIHRfFCuwQFnoECAgQAQ&url=http%3A%2F%2Fwww23.statcan.gc.ca%2Fimdb-bmdi%2Fdocument%2F5049_D24_T9_V1-eng.pdf&usg=AOvVaw3cNyqDCkWzhlHCZyNPmnuq (accessed on 1 October 2023).
- Statistics Canada. Canadian Community Health Survey—Nutrition (CCHS). Available online: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=5049#a1 (accessed on 1 October 2023).
- Health Canada. Eating Well with Canada’s Food Guide. Available online: https://www.canada.ca/en/health-canada/services/canada-food-guide/about/history-food-guide/eating-well-with-canada-food-guide-2007.html (accessed on 1 October 2023).
- National Center for Health Control and Prevention. NHANES Dietary Web Data Tutorial—Advanced Dietary Analyses. 2011. Available online: https://www.cdc.gov/nchs/tutorials/dietary/advanced/ (accessed on 1 October 2023).
- Knezevic, A. Overlapping confidence intervals and statistical significance. StatNews Cornell Univ. Stat. Consult. Unit 2008, 73, 141. [Google Scholar]
- Bolland, M.J.; Barber, P.A.; Doughty, R.N.; Mason, B.; Horne, A.; Ames, R.; Gamble, G.D.; Grey, A.; Reid, I.R. Vascular events in healthy older women receiving calcium supplementation: Randomised controlled trial. BMJ 2008, 336, 262–266. [Google Scholar] [CrossRef]
- Vatanparast, H.; Islam, N.; Patil, R.P.; Shafiee, M.; Whiting, S.J. Calcium intake from food and supplemental sources decreased in the Canadian population from 2004 to 2015. J. Nutr. 2020, 150, 833–841. [Google Scholar] [CrossRef]
- Machado, M.C.; Bruce-Mensah, A.; Whitmire, M.; Rizvi, A.A. Hypercalcemia associated with calcium supplement use: Prevalence and characteristics in hospitalized patients. J. Clin. Med. 2015, 4, 414–424. [Google Scholar] [CrossRef]
- Sabbagh, Z.; Vatanparast, H. Is calcium supplementation a risk factor for cardiovascular diseases in older women? Nutr. Rev. 2009, 67, 105–108. [Google Scholar] [CrossRef]
- Reid, I.R.; Bolland, M.J.; Avenell, A.; Grey, A. Cardiovascular effects of calcium supplementation. Osteoporos. Int. 2011, 22, 1649–1658. [Google Scholar] [CrossRef]
- Bolland, M.J.; Avenell, A.; Baron, J.A.; Grey, A.; MacLennan, G.S.; Gamble, G.D.; Reid, I.R. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: Meta-analysis. BMJ 2010, 341, c3691. [Google Scholar] [CrossRef]
- Tu, K.N.; Lie, J.D.; Wan, C.K.V.; Cameron, M.; Austel, A.G.; Nguyen, J.K.; Van, K.; Hyun, D. Osteoporosis: A review of treatment options. Pharm. Ther. 2018, 43, 92. [Google Scholar]
- Michaëlsson, K.; Melhus, H.; Lemming, E.W.; Wolk, A.; Byberg, L. Long term calcium intake and rates of all cause and cardiovascular mortality: Community based prospective longitudinal cohort study. BMJ 2013, 346, f228. [Google Scholar] [CrossRef] [PubMed]
- Bolland, M.J.; Grey, A.; Avenell, A.; Gamble, G.D.; Reid, I.R. Calcium supplements with or without vitamin D and risk of cardiovascular events: Reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ 2011, 342, d2040. [Google Scholar] [CrossRef]
- Wang, X.; Chen, H.; Ouyang, Y.; Liu, J.; Zhao, G.; Bao, W.; Yan, M. Dietary calcium intake and mortality risk from cardiovascular disease and all causes: A meta-analysis of prospective cohort studies. BMC Med. 2014, 12, 158. [Google Scholar] [CrossRef]
- Wang, L.; Manson, J.E.; Song, Y.; Sesso, H.D. Systematic review: Vitamin D and calcium supplementation in prevention of cardiovascular events. Ann. Intern. Med. 2010, 152, 315–323. [Google Scholar] [CrossRef]
- Lewis, J.R.; Radavelli-Bagatini, S.; Rejnmark, L.; Chen, J.S.; Simpson, J.M.; Lappe, J.M.; Mosekilde, L.; Prentice, R.L.; Prince, R.L. The effects of calcium supplementation on verified coronary heart disease hospitalization and death in postmenopausal women: A collaborative meta-analysis of randomized controlled trials. J. Bone Miner. Res. 2015, 30, 165–175. [Google Scholar] [CrossRef]
- Kopecky, S.L.; Bauer, D.C.; Gulati, M.; Nieves, J.W.; Singer, A.J.; Toth, P.P.; Underberg, J.A.; Wallace, T.C.; Weaver, C.M. Lack of evidence linking calcium with or without vitamin D supplementation to cardiovascular disease in generally healthy adults: A clinical guideline from the National Osteoporosis Foundation and the American Society for Preventive Cardiology. Ann. Intern. Med. 2016, 165, 867–868. [Google Scholar] [CrossRef]
- Chung, M.; Tang, A.M.; Fu, Z.; Wang, D.D.; Newberry, S.J. Calcium intake and cardiovascular disease risk: An updated systematic review and meta-analysis. Ann. Intern. Med. 2016, 165, 856–866. [Google Scholar] [CrossRef]
- Jolma, P.; Kööbi, P.; Kalliovalkama, J.; Kähönen, M.; Fan, M.; Saha, H.; Helin, H.; Lehtimäki, T.; Pörsti, I. Increased calcium intake reduces plasma cholesterol and improves vasorelaxation in experimental renal failure. Am. J. Physiol. Heart Circ. Physiol. 2003, 285, H1882–H1889. [Google Scholar] [CrossRef]
- Ruidavets, J.-B.; Bongard, V.; Simon, C.; Dallongeville, J.; Ducimetière, P.; Arveiler, D.; Amouyel, P.; Bingham, A.; Ferrières, J. Independent contribution of dairy products and calcium intake to blood pressure variations at a population level. J. Hypertens. 2006, 24, 671–681. [Google Scholar] [CrossRef]
- Ma, B.; Lawson, A.B.; Liese, A.D.; Bell, R.A.; Mayer-Davis, E.J. Dairy, magnesium, and calcium intake in relation to insulin sensitivity: Approaches to modeling a dose-dependent association. Am. J. Epidemiol. 2006, 164, 449–458. [Google Scholar] [CrossRef]
- Czernichow, S.; Fan, T.; Nocea, G.; Sen, S.S. Calcium and vitamin D intake by postmenopausal women with osteoporosis in France. Curr. Med. Res. Opin. 2010, 26, 1667–1674. [Google Scholar] [CrossRef] [PubMed]
- Fan, T.; Nocea, G.; Modi, A.; Stokes, L.; Sen, S.S. Calcium and vitamin D intake by postmenopausal women with osteoporosis in Spain: An observational calcium and vitamin D intake (CaVIT) study. Clin. Interv. Aging 2013, 8, 689. [Google Scholar]
- Vatanparast, H.; Patil, R.P.; Islam, N.; Shafiee, M.; Whiting, S.J. Vitamin D intake from supplemental sources but not from food sources has increased in the Canadian population over time. J. Nutr. 2020, 150, 526–535. [Google Scholar] [CrossRef]
- Mirhosseini, N.; Rainsbury, J.; Kimball, S.M. Vitamin D supplementation, serum 25 (OH) D concentrations and cardiovascular disease risk factors: A systematic review and meta-analysis. Front. Cardiovasc. Med. 2018, 5, 87. [Google Scholar] [CrossRef]
- Ford, J.A.; MacLennan, G.S.; Avenell, A.; Bolland, M.; Grey, A.; Witham, M.; Group, R.T. Cardiovascular disease and vitamin D supplementation: Trial analysis, systematic review, and meta-analysis. Am. J. Clin. Nutr. 2014, 100, 746–755. [Google Scholar] [CrossRef]
- Vacek, J.L.; Vanga, S.R.; Good, M.; Lai, S.M.; Lakkireddy, D.; Howard, P.A. Vitamin D deficiency and supplementation and relation to cardiovascular health. Am. J. Cardiol. 2012, 109, 359–363. [Google Scholar] [CrossRef]
- Schöttker, B.; Jorde, R.; Peasey, A.; Thorand, B.; Jansen, E.H.; De Groot, L.; Streppel, M.; Gardiner, J.; Ordóñez-Mena, J.M.; Perna, L. Vitamin D and mortality: Meta-analysis of individual participant data from a large consortium of cohort studies from Europe and the United States. BMJ 2014, 348, g3656. [Google Scholar] [CrossRef]
- Zittermann, A.; Gummert, J.F. Sun, vitamin D, and cardiovascular disease. J. Photochem. Photobiol. B Biol. 2010, 101, 124–129. [Google Scholar] [CrossRef]
- Kendrick, J.; Targher, G.; Smits, G.; Chonchol, M. 25-Hydroxyvitamin D deficiency is independently associated with cardiovascular disease in the Third National Health and Nutrition Examination Survey. Atherosclerosis 2009, 205, 255–260. [Google Scholar] [CrossRef]
- Fiscella, K.; Franks, P. Vitamin D, race, and cardiovascular mortality: Findings from a national US sample. Ann. Fam. Med. 2010, 8, 11–18. [Google Scholar] [CrossRef][Green Version]
- Giovannucci, E.; Liu, Y.; Hollis, B.W.; Rimm, E.B. 25-hydroxyvitamin D and risk of myocardial infarction in men: A prospective study. Arch. Intern. Med. 2008, 168, 1174–1180. [Google Scholar] [CrossRef]
- Leu, M.; Giovannucci, E. Vitamin D: Epidemiology of cardiovascular risks and events. Best Pract. Res. Clin. Endocrinol. Metab. 2011, 25, 633–646. [Google Scholar] [CrossRef]
- Temmerman, J.C. Vitamin D and cardiovascular disease. J. Am. Coll. Nutr. 2011, 30, 167–170. [Google Scholar] [CrossRef]
- Barbarawi, M.; Kheiri, B.; Zayed, Y.; Barbarawi, O.; Dhillon, H.; Swaid, B.; Yelangi, A.; Sundus, S.; Bachuwa, G.; Alkotob, M.L. Vitamin D supplementation and cardiovascular disease risks in more than 83,000 individuals in 21 randomized clinical trials: A meta-analysis. JAMA Cardiol. 2019, 4, 765–776. [Google Scholar] [CrossRef]
- Michos, E.D.; Kalyani, R.R.; Blackford, A.L.; Sternberg, A.L.; Mitchell, C.M.; Juraschek, S.P.; Schrack, J.A.; Wanigatunga, A.A.; Roth, D.L.; Christenson, R.H. The relationship of falls with achieved 25-hydroxyvitamin D levels from vitamin D supplementation: The STURDY Trial. J. Endocr. Soc. 2022, 6, bvac065. [Google Scholar] [CrossRef]
- Grant, W.B.; Al Anouti, F.; Boucher, B.J.; Dursun, E.; Gezen-Ak, D.; Jude, E.B.; Karonova, T.; Pludowski, P. A Narrative Review of the Evidence for Variations in Serum 25-Hydroxyvitamin D Concentration Thresholds for Optimal Health. Nutrients 2022, 14, 639. [Google Scholar] [CrossRef]
- National Institutes of Health. Vitamin D Fact Sheet for Consumers. Available online: https://ods.od.nih.gov/factsheets/VitaminD-Consumer/ (accessed on 1 October 2023).
- Garriguet, D. Comparison of results from the Canadian Community Health Surveys-Nutrition 2004 vs 2015. In Proceedings of the CCHS Webinar Series, Ottawa, ON, USA, 25 September 2018. [Google Scholar]
| Sociodemographic Variables | Osteoporosis | Heart Disease | ||||||
|---|---|---|---|---|---|---|---|---|
| 2004 (n = 1,061,034) (11.3%) | 2015 (n = 1,375,730) (10.6%) | 2004 (n = 1,028,909) (10.9%) | 2015 (n = 1,211,896) (9.3%) | |||||
| % ± SE | 95% CI | % ± SE | 95% CI | % ± SE | 95% CI | % ± SE | 95% CI | |
| Age | ||||||||
| 50–70 years | 54.1 ± 2.0 | (50.2, 58.1) | 55.4 ± 2.4 | (50.6, 60.1) | 48.0 ± 2.2 | (43.4, 52.6) | 48.6 ± 2.9 | (42.9, 54.4) |
| ≥71 years | 45.9 ± 2.0 | (42.0, 49.8) | 44.6 ± 2.4 | (39.9, 49.4) | 52.0 ± 2.2 | (46.8, 56.0) | 51.4 ± 2.9 | (45.6, 57.1) |
| Sex | ||||||||
| Male | 11.0 ± 1.4 | (8.2, 13.8) | 15.6 ± 1.8 ¥ | (12.1, 19.2) | 57.4 ± 2.1 | (53.4, 61.5) | 55.6 ± 2.9 | (49.9, 61.3) |
| Female | 89.0 ± 1.4 | (86.2, 91.8) | 84.4 ± 1.8 ¥ | (80.8, 88.0) | 42.6 ± 2.1 | (38.5, 46.6) | 44.4 ± 2.9 | (38.7, 50.1) |
| Ethnicity | ||||||||
| Non-indigenous | 98.6 ± 0.4 | (97.7, 99.4) | 97.3 ± 0.8 | (95.7, 99.0) | 97.9 ± 0.5 | (97.0, 98.9) | 97.7 ± 0.8 | (96.2, 99.3) |
| Indigenous | 1.5 ± 0.4 | (0.6, 2.3) | 2.7 ± 0.8 | (1.0, 4.3) | 2.1 ± 0.5 | (1.1, 3.0) | 2.3 ± 0.8 | (0.7, 3.8) |
| Immigrant | ||||||||
| Yes | 27.3 ± 2.3 | (22.5, 31.5) | 24.0 ± 4.4 | (18.8, 29.3) | 20.6 ± 1.9 | (16.9, 24.3) | 24.0 ± 2.8 | (18.5, 29.4) |
| No | 73.3 ± 2.3 | (68.5, 77.5) | 76.0 ± 3.3 | (70.8, 81.2) | 79.5 ± 1.9 | (75.8, 83.2) | 76.0 ± 2.8 | (70.6, 81.5) |
| Calcium Supplement user | ||||||||
| Yes | 56.5 ± 1.2 | (52.1, 60.8) | 45.2 ± 4.4 ¥ | (39.2, 51.2) | 33.9 ± 1.9 | (29.5, 38.2) | 24.5 ± 2.6 ¥ | (19.5, 29.6) |
| No | 43.5 ± 0.2 | (39.2, 47.9) | 54.8 ± 3.3 ¥ | (48.8, 60.8) | 66.2 ± 0.2 | (61.8, 70.5) | 75.5 ± 2.6 ¥ | (70.4, 80.5) |
| Vitamin D Supplement user | ||||||||
| Yes | 55.1 ± 1.3 | (50.7, 59.5) | 56.5 ± 4.4 | (50.5, 62.5) | 32.9 ± 1.2 | (28.7, 37.2) | 38.0 ± 2.9 | (32.2, 43.7) |
| No | 44.9 ± 0.3 | (40.5, 49.4) | 43.5 ± 3.3 | (37.5, 49.5) | 67.1 ± 0.2 | (62.8, 71.3) | 62.0 ± 2.9 | (56.3, 67.8) |
| Weight Status | ||||||||
| Normal weight | 39.7 ± 4.3 | (34.4, 45.0) | 37.5 ± 4.7 | (30.3, 44.8) | 26.7 ± 4.2 | (21.3, 32.1) | 28.0 ± 3.5 | (21.1, 34.8) |
| Overweight | 38.5 ± 5.3 | (33.3, 43.7) | 38.9 ± 5.1 | (31.0, 46.9) | 43.3 ± 5.4 | (37.2, 49.5) | 42.7 ± 4.3 | (34.3, 51.0) |
| Obese | 21.8 ± 6.2 | (16.8, 26.8) | 23.5 ± 6.8 | (18.1, 29.0) | 30.0 ± 6.3 | (24.1, 35.9) | 29.4 ± 3.9 | (21.8, 37.0) |
| Smoking status | ||||||||
| Yes | 12.5 ± 1.4 | (9.9, 15.2) | 20.2 ± 3.0 ¥ | (14.3, 26.1) | 18.6 ± 2.0 | (14.6, 22.6) | 15.6 ± 2.4 | (10.9, 20.3) |
| No | 87.5 ± 1.4 | (84.8, 90.1) | 79.8 ± 3.0 ¥ | (73.9, 85.8) | 81.4 ± 2.0 | (77.5, 85.4) | 84.4 ± 2.4 | (79.8, 89.1) |
| Education | ||||||||
| <secondary graduate | 41.7 ± 2.4 | (37.1, 46.4) | 26.3 ± 2.5 ¥ | (21.5, 31.2) | 44.7 ± 2.3 | (40.2, 49.1) | 29.6 ± 2.7 ¥ | (24.4, 34.8) |
| secondary graduate | 16.1 ± 1.8 | (12.6, 19.5) | 32.6 ± 3.0 ¥ | (26.8, 38.4) | 13.4 ± 1.4 | (10.7, 16.2) | 24.0 ± 2.5 ¥ | (19.1, 28.9) |
| some post-secondary graduate | 5.1 ± 0.9 | (3.4, 6.8) | 29.1 ± 2.7 ¥ | (23.7, 34.5) | 5.4 ± 0.9 | (3.6, 7.2) | 30.5 ± 3.1 ¥ | (24.4, 36.6) |
| university graduate | 37.1 ± 2.2 | (32.8, 41.4) | 12.0 ± 1.6 ¥ | (8.8, 15.2) | 36.5 ± 2.1 | (32.3, 40.7) | 15.9 ± 2.3 ¥ | (11.3, 20.5) |
| Region of residence | ||||||||
| Atlantic | 7.5 ± 0.8 | (5.9, 7.7) | 8.2 ± 0.8 | (6.6, 8.8) | 10.0 ± 0.9 | (8.2, 10.9) | 10.9 ± 1.0 | (9.0, 12.9) |
| Quebec | 24.3 ± 2.2 | (20.0, 24.2) | 24.7 ± 2.6 | (19.6, 24.7) | 24.4 ± 2.2 | (20.1, 24.6) | 29.7 ± 3.0 | (23.7, 35.7) |
| Ontario | 38.6 ± 2.0 | (34.7, 38.4) | 41.1 ± 2.8 | (35.5, 41.6) | 36.6 ± 1.9 | (33.0, 36.3) | 35.5 ± 3.0 | (29.5, 41.4) |
| Prairies | 16.6 ± 1.3 | (14.1, 16.1) | 15.1 ± 1.6 | (12.0, 15.3) | 13.6 ± 1.2 | (11.3, 13.0) | 14.3 ± 1.6 | (11.1, 17.4) |
| British Columbia | 13.1 ± 1.4 | (10.3, 13.1) | 10.9 ± 1.5 | (8.0, 10.9) | 15.3 ± 1.7 | (12.0, 15.6) | 9.7 ± 1.5 ¥ | (6.7, 12.6) |
| Met daily grain product requirement | ||||||||
| Yes | 23.2 ± 2.2 | (18.2, 27.5) | 18.0 ± 2.4 ¥ | (13.4, 22.6) | 23.6 ± 2.2 | (19.2, 28.0) | 19.5 ± 2.6 | (14.4, 24.6) |
| No | 76.8 ± 2.2 | (72.8, 81.1) | 82.0 ± 2.4 ¥ | (77.4, 86.6) | 76.4 ± 2.2 | (72.0, 80.8) | 80.5 ± 2.6 | (75.5, 85.6) |
| Met daily meat and alternatives requirement | ||||||||
| Yes | 30.7 ± 2.2 | (26.4, 35.0) | 24.5 ± 4.6 ¥ | (19.4, 29.6) | 23.1 ± 1.9 | (19.4, 26.8) | 20.6 ± 2.7 | (15.2, 25.9) |
| No | 69.3 ± 2.2 | (65.0, 73.6) | 75.5 ± 3.6 ¥ | (70.4, 80.6) | 76.9 ± 1.9 | (73.2, 80.6) | 79.4 ± 2.7 | (74.1, 84.8) |
| Met daily milk and alternatives requirement | ||||||||
| Yes | 9.3 ± 1.0 | (7.3, 11.3) | 11.0 ± 1.7 | (7.7, 14.4) | 14.9 ± 1.7 | (11.5, 18.3) | 9.6 ± 1.7 ¥ | (6.3, 13.0) |
| No | 90.7 ± 1.0 | (88.7, 92.7) | 89.0 ± 1.7 | (85.6, 92.3) | 85.1 ± 1.7 | (81.7, 88.5) | 90.4 ± 1.7 ¥ | (87.1, 93.7) |
| Met daily vegetable and fruit requirement | ||||||||
| Yes | 20.9 ± 1.8 | (17.4, 24.3) | 16.9 ± 2.6 | (11.9, 22.0) | 21.8 ± 1.9 | (18.1, 25.4) | 14.8 ± 2.2 ¥ | (10.4, 19.1) |
| No | 79.1 ± 1.8 | (75.7, 82.6) | 83.1 ± 2.6 | (78.0, 88.1) | 78.2 ± 1.9 | (74.6, 81.9) | 85.2 ± 2.2 ¥ | (80.9, 89.6) |
| Income decile | ||||||||
| Decile 1–2 | 6.2 ± 1.8 | (2.7, 6.7) | 33.3 ± 3.1 ¥ | (27.2, 39.5) | 3.3 ± 0.7 | (1.8, 4.7) | 28.0 ± 2.5 ¥ | (23.1, 32.9) |
| Decile 3–4 | 11.4 ± 1.4 | (8.6, 11.3) | 21.1 ± 2.0 ¥ | (17.1, 25.0) | 13.5 ± 1.6 | (10.4, 16.6) | 29.3 ± 3.0 ¥ | (23.5, 35.1) |
| Decile 5–6 | 30.5 ± 2.2 | (26.2, 30.7) | 23.2 ± 2.5 ¥ | (18.2, 28.2) | 36.3 ± 2.3 | (31.7, 40.8) | 22.2 ± 2.7 ¥ | (16.9, 27.4) |
| Decile 7–8 | 34.7 ± 2.5 | (29.9, 34.6) | 14.0 ± 2.4 ¥ | (9.4, 18.7) | 28.8 ± 2.2 | (24.6, 33.1) | 10.8 ± 1.7 ¥ | (7.5, 14.1) |
| Decile 9–10 | 17.2 ± 2.1 | (13.1, 17.2) | 8.4 ± 1.6 ¥ | (5.3, 11.5) | 18.2 ± 2.0 | (14.4, 22.0) | 9.7 ± 2.3 ¥ | (5.1, 14.3) |
| Osteoporosis | Heart Disease | |||
|---|---|---|---|---|
| 2004 (n = 1,061,034) (11.3%) | 2015 (n = 1,375,730) (10.6%) | 2004 (n = 1,028,909) (10.9%) | 2015 (n = 1,211,896) (9.3%) | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Age | ||||
| 50–70 years | 1 | 1 | 1 | 1 |
| ≥71 years | 2.3 * (1.8, 2.9) | 2.3 * (1.7, 3.1) | 3.1 * (2.4, 4) | 3.4 * (2.4, 4.8) |
| Sex | ||||
| Male 2 | 1 | 1 | 1.7 * (1.3, 2.2) | 1.6 * (1.2, 2.2) |
| Female 3 | 8.1 * (5.5, 12) | 4.6 * (3.1, 6.6) | 1 | 1 |
| Ethnicity | ||||
| Indigenous 4 | 1 | 1 | 1 | 1 |
| Non-indigenous | 0.6 (0.2, 1.6) | 0.6 (0.3, 1.3) | 0.8 (0.4, 1.8) | 0.995 (0.4, 2.6) |
| Immigrant | ||||
| No 4 | 1 | 1 | 1 | 1 |
| Yes | 1.1 (0.8, 1.5) | 0.8 (0.5, 1.3) | 0.8 (0.6, 1) | 0.9 (0.6, 1.3) |
| Calcium supplement User | ||||
| No 4 | 1 | 1 | 1 | 1 |
| Yes | 1.1 (0.8, 1.6) | 1.2 (0.8, 1.7) | 1 (0.6, 1.6) | 0.8 (0.5, 1.3) |
| Vitamin D supplement User | ||||
| No 4 | 1 | 1 | 1 | 1 |
| Yes | 1.9 * (1.3, 2.8) | 1.5 (1.0, 2.1) | 0.9 (0.6, 1.5) | 1.1 (0.7, 1.8) |
| Weight Status | ||||
| Normal weight 4 | 1 | 1 | 1 | 1 |
| Overweight | 0.9 (0.7, 1.2) | 1.1 (0.8, 1.6) | 1.2 (0.9, 1.6) | 1.1 (0.7, 1.6) |
| Obese | 0.7 (0.5, 0.9) | 0.9 (0.6, 1.3) | 1.4 (1, 1.9) | 1.5 (1, 2.2) |
| Smoking status | ||||
| No 4 | 1 | 1 | 1 | 1 |
| Yes | 0.8 (0.6, 1.1) | 1.6 (1, 2.5) | 1.04 (0.7, 1.5) | 1.1 (0.7, 1.8) |
| Education | ||||
| University graduate 4 | 1 | 1 | 1 | 1 |
| <Secondary graduate | 1.3 (1, 1.8) | 1.6 (1, 2.6) | 1.2 (0.9, 1.7) | 1.1 (0.7, 1.7) |
| Secondary graduate | 0.9 (0.6, 1.3) | 1.2 (0.8, 1.8) | 1 (0.7, 1.4) | 0.8 (0.5, 1.1) |
| Some post-secondary graduate | 1.1 (0.7, 1.8) | 1.7 (1, 2.9) | 0.9 (0.6, 1.5) | 0.9 (0.6, 1.5) |
| Region of residence | ||||
| Ontario 4 | 1 | 1 | 1 | 1 |
| Atlantic | 1 (0.7, 1.4) | 1 (0.7, 1.5) | 0.9 (0.7, 1.3) | 1.6 * (1.1, 2.5) |
| Quebec | 1 (0.7, 1.5) | 0.9 (0.6, 1.4) | 0.8 (0.6, 1) | 1.4 (0.9, 2.3) |
| Prairies | 1.2 (0.9, 1.6) | 0.9 (0.6, 1.3) | 0.8 (0.6, 1) | 1.2 (0.8, 1.8) |
| British Columbia | 0.7 (0.5, 1.1) | 0.8 (0.5, 1.2) | 1.2 (0.8, 1.8) | 0.9 (0.6, 1.5) |
| Income | ||||
| Decile 9–10 4 | 1 | 1 | 1 | 1 |
| Decile 1–2 | 2.9 * (1.2, 6.9) | 2.4 * (1.3, 4.5) | 1.7 (0.9, 3.4) | 1.8 (0.9, 3.6) |
| Decile 3–4 | 1.7 * (1, 2.7) | 1.6 (0.9, 2.8) | 2.7 * (1.7, 4.2) | 1.6 (0.8, 3.2) |
| Decile 5–6 | 1.7 * (1.2, 2.5) | 2.5 * (1.3, 4.5) | 2 * (1.4, 2.8) | 1.5 (0.7, 3) |
| Decile 7–8 | 1.7 * (1.2, 2.4) | 1.9 (1, 3.5) | 1.4 (1, 1.9) | 0.9 (0.5, 1.9) |
| Met daily grain product requirement | ||||
| No 4 | 1 | 1 | 1 | 1 |
| Yes | 1.1 (0.8, 1.6) | 1.1 (0.7, 1.7) | 1.3 (0.9, 1.8) | 0.9 (0.6, 1.4) |
| Met daily meat and alternatives requirement | ||||
| No 4 | 1 | 1 | 1 | 1 |
| Yes | 1 (0.7, 1.3) | 0.8 (0.6, 1.2) | 0.8 (0.6, 1.1) | 0.8 (0.5, 1.1) |
| Meet daily milk and alternatives requirement | ||||
| No 4 | 1 | 1 | 1 | 1 |
| Yes | 0.7 (0.5, 1.1) | 1.2 (0.7, 2.1) | 1.3 (0.9, 2) | 1 (0.6, 1.7) |
| Meet daily vegetable and fruit requirement | ||||
| No 4 | 1 | 1 | 1 | 1 |
| Yes | 0.8 (0.6, 1.1) | 1.2 (0.8, 1.9) | 1 (0.7, 1.3) | 1 (0.7, 1.6) |
| Calcium Supplement Non-Users | Calcium Supplement Users | |||||
|---|---|---|---|---|---|---|
| 2004 (61.5%) | 2015 (67.9%) | 2004 (38.5%) | 2015 (32.1%) | |||
| Chronic Diseases | Calcium (mg) from Food | Calcium (mg) from Food | Calcium (mg) from Food | Calcium (mg) from Food and Supplements | Calcium (mg) from Food | Calcium (mg) from Food and Supplements |
| No heart disease | 732.9 ± 30.0 | 654.8 ± 26.0 ¥ | 733.5 ± 33.5 | 1244.7 ± 37.6 | 738.4 ± 38.8 | 1193.9 ± 57.0 |
| Have heart disease | 720.4 ± 32.7 | 641.7 ± 34.6 ¥ | 657.8 ± 34.3 | 1169.4 ± 56.6 | 671.0 ± 41.5 | 1126.3 ± 57.7 |
| No Osteoporosis | 737.9 ± 30.1 | 662.7 ± 25.8 ¥ | 736.8 ± 34.0 | 1204.5 ± 38.1 | 744.1 ± 39.4 | 1203.3 ± 57.2 |
| Have Osteoporosis | 648.3 ± 31.9 | 580.6 ± 27.8 ¥ | 668.1 ± 34.0 | 1419.4 ± 46.2 | 649.6 ± 36.4 | 1117.6 ± 56.1 ¥ |
| Have both diseases | 594.8 ± 32.0 | 592.9 ± 47.8 | 637.9 ± 35.0 | 1337.9 ± 67.9 | 602.8 ± 47.0 | 1082.9 ± 61.1 ¥ |
| Vitamin D Supplement Non-Users | Vitamin D Supplement Users | |||||
|---|---|---|---|---|---|---|
| 2004 (63.7%) | 2015 (58.0%) | 2004 (36.3%) | 2015 (42.0%) | |||
| Chronic Diseases | Vitamin D (µg) from Food | Vitamin D (µg) from Food | Vitamin D (µg) from Food | Vitamin D (µg) from Food and Supplements | Vitamin D (µg) from Food | Vitamin D (µg) from Food and Supplements |
| No heart disease | 5.4 ± 0.3 | 4.7 ± 0.4 | 5.3 ± 0.5 | 16.6 ± 0.6 | 4.8 ± 0.5 | 39.6 ± 3.3 ¥ |
| Heart Disease | 5.3 ± 0.4 | 4.8 ± 0.4 | 4.8 ± 0.4 | 16.5 ± 1.2 | 4.3 ± 0.5 | 38.6 ± 3.3 ¥ |
| No Osteoporosis | 5.4 ± 0.3 | 4.8 ± 0.4 | 5.4 ± 0.5 | 16.1 ± 0.5 | 4.8 ± 0.5 | 39.9 ± 3.3 ¥ |
| Have Osteoporosis | 4.8 ± 0.3 | 4.2 ± 0.4 | 4.8 ± 0.4 | 19.3 ± 1.1 | 4.4 ± 0.4 | 38.9 ± 3.3 ¥ |
| Have both diseases | 4.6 ± 0.3 | 4.5 ± 0.5 | 4.4 ± 0.4 | 18.6 ± 3.3 | 4.0 ± 0.4 | 39.0 ± 3.2 ¥ |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vatanparast, H.; Lane, G.; Islam, N.; Patil, R.P.; Shafiee, M.; Whiting, S.J. Comparative Analysis of Dietary and Supplemental Intake of Calcium and Vitamin D among Canadian Older Adults with Heart Disease and/or Osteoporosis in 2004 and 2015. Nutrients 2023, 15, 5066. https://doi.org/10.3390/nu15245066
Vatanparast H, Lane G, Islam N, Patil RP, Shafiee M, Whiting SJ. Comparative Analysis of Dietary and Supplemental Intake of Calcium and Vitamin D among Canadian Older Adults with Heart Disease and/or Osteoporosis in 2004 and 2015. Nutrients. 2023; 15(24):5066. https://doi.org/10.3390/nu15245066
Chicago/Turabian StyleVatanparast, Hassan, Ginny Lane, Naorin Islam, Rashmi Prakash Patil, Mojtaba Shafiee, and Susan J. Whiting. 2023. "Comparative Analysis of Dietary and Supplemental Intake of Calcium and Vitamin D among Canadian Older Adults with Heart Disease and/or Osteoporosis in 2004 and 2015" Nutrients 15, no. 24: 5066. https://doi.org/10.3390/nu15245066
APA StyleVatanparast, H., Lane, G., Islam, N., Patil, R. P., Shafiee, M., & Whiting, S. J. (2023). Comparative Analysis of Dietary and Supplemental Intake of Calcium and Vitamin D among Canadian Older Adults with Heart Disease and/or Osteoporosis in 2004 and 2015. Nutrients, 15(24), 5066. https://doi.org/10.3390/nu15245066








