Abstract
Schizophrenia, a severe mental illness affecting about 1% of the population, manifests during young adulthood, leading to abnormal mental function and behavior. Its multifactorial etiology involves genetic factors, experiences of adversity, infection, and gene–environment interactions. Emerging research indicates that maternal infection or stress during pregnancy may also increase schizophrenia risk in offspring. Recent research on the gut–brain axis highlights the gut microbiome’s potential influence on central nervous system (CNS) function and mental health, including schizophrenia. The gut microbiota, located in the digestive system, has a significant role to play in human physiology, affecting immune system development, vitamin synthesis, and protection against pathogenic bacteria. Disruptions to the gut microbiota, caused by diet, medication use, environmental pollutants, and stress, may lead to imbalances with far-reaching effects on CNS function and mental health. Of interest are short-chain fatty acids (SCFAs), metabolic byproducts produced by gut microbes during fermentation. SCFAs can cross the blood–brain barrier, influencing CNS activity, including microglia and cytokine modulation. The dysregulation of neurotransmitters produced by gut microbes may contribute to CNS disorders, including schizophrenia. This review explores the potential relationship between SCFAs, the gut microbiome, and schizophrenia. Our aim is to deepen the understanding of the gut–brain axis in schizophrenia and to elucidate its implications for future research and therapeutic approaches.
1. Introduction
Schizophrenia is a severe psychiatric condition that results in a combination of hallucinations, delusions, and profoundly chaotic cognitive processes and behavior [1]. Schizophrenia is a multifactorial disease; its etiology involves a combination of genetic factors, as well as experiences of adversity, infection, and interactions between environmental and genetic influences [2,3,4,5,6,7] (Figure 1). The quantity of individuals diagnosed with schizophrenia witnessed a 65% surge in 2019 compared to the figures from 1990 [8]. Notably, there exists compelling evidence that 85% of individuals diagnosed with schizophrenia experienced childhood trauma [9].
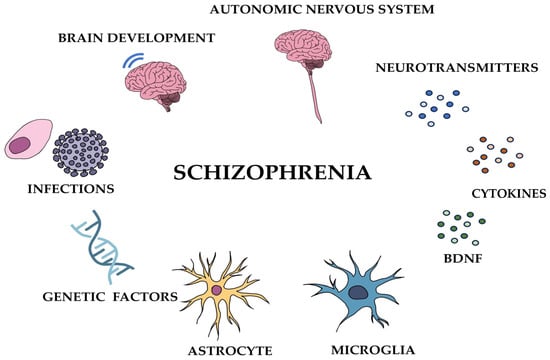
Figure 1.
Various factors that can trigger schizophrenia.
Over the past few decades, the relationship between the gut, microbiota, and the brain has been a subject of significant attention. Extensive experimental evidence highlights the substantial influence that the microbiota can have on both gut and brain functions [10,11]. Communication between the gut and brain occurs in both directions, primarily through various pathways [12]. Recent studies on the gut–brain axis have provided insights into the possible impact of the gut microbiome on the functioning of the central nervous system (CNS) and on mental health conditions such as schizophrenia [13].
The gut microbiota, a diverse community of microorganisms residing in the gastrointestinal tract, plays a crucial role in human physiology and pathology, affecting various biological functions like the maturation of the immune system, the synthesis of essential vitamins, and protection against pathogenic bacteria [14,15,16]. During early life, microbial colonization begins before birth, with delivery mode and environmental factors influencing the composition of the gut microbiota [17,18,19,20]. Disruptions to the gut microbiota, caused by changes in diet, medication use, environmental pollutants, and stress, may lead to imbalances that could have far-reaching effects on CNS function and mental health [21,22].
Especially noteworthy within the context of schizophrenia are short-chain fatty acids (SCFAs), which are metabolic byproducts produced by gut microbes during the fermentation process [23,24,25]. SCFAs have been found to cross the blood–brain barrier and can influence CNS activity, including the modulation of microglia activity and cytokine production [26]. Dysregulation of neurotransmitters like glutamate, γ-aminobutyric acid (GABA), dopamine, and serotonin, produced by gut microbes or their precursor molecules, may also contribute to CNS disorders, including schizophrenia [27,28,29,30,31,32,33,34,35].
The objective of this review is to investigate and elucidate the possible connection involving SCFAs, the gut microbiome, and schizophrenia. By synthesizing the existing literature on this topic, our goal is to deepen our comprehension of the gut–brain axis in schizophrenia and its implications for future research and therapeutic strategies.
3. Exploring the Gut Microbiota and Its Multifaceted Impacts
3.1. The Gut Microbiota: Impacts on Human Physiology, Immune Function, and Brain Health
The microbiota resides in various regions of the body, including the skin, conjunctiva, oral cavity, airway, vagina, and gastrointestinal tract [135]. Among them, the gut microbiota is a multifaceted and constantly changing community of microorganisms that engage with both the surroundings and the human body [136]. The predominant bacterial phyla inhabiting the intestine consist mainly of Firmicutes, which include species like Lactobacillus, Clostridium, and Enterococcus, as well as Bacteroidetes, encompassing species like Bacteroides. In addition, smaller quantities of Actinobacteria (including Bifidobacteria), Proteobacteria (such as Escherichia coli), Fusobacteria, Verrucomicrobia, and Cyanobacteria are also present [137,138,139,140]. Approximately 1014 bacteria reside in the human gut, exceeding the number of human cells by a factor of 10 and possessing more than 100 times the amount of genomic content compared to human genomic DNA [141].
The gut microbiota has a crucial function in human physiology and disease, aiding in the formation of gastric mucus and promoting enzymatic activity within the mucous lining to support the digestive system [14]. Some bacteria in the gut microbiota serve protective functions against pathogenic bacteria, acting as a barrier and defending against toxins [15]. Additionally, they contribute to immune system development, synthesize essential vitamins [16]. Moreover, the gut microbiota influences epithelial cell proliferation [142] and insulin resistance [143], fundamentally impacting immune and metabolic functions, and contributing to the regulation of central nervous system homeostasis [144]. Certain miRNAs, which are responsible for regulating gene expression by triggering gene silencing or inhibiting translation, possess the capability to penetrate bacterial cells and regulate their growth and gene expression. Moreover, the gut microbiota can also impact the intestinal expression of miRNAs [145]. Studies have shown that bacterial peptidoglycan derived from the gut microbiota can travel to the brain and activate specific pattern recognition receptors (PRRs) within the innate immune system [146].
3.2. Early-Life Microbiota: Influences of Birth Mode and Health on Neonatal Gut Microbiota
Microbiota are already present in the placenta, amniotic fluid, and umbilical cord, indicating that microbial colonization begins even before birth [17,18,19]. However, the neonatal gut microbiota closely resemble the microbiota encountered during childbirth, and the mode of delivery significantly influences the composition of the neonatal gut microbiota [20]. Babies delivered vaginally are colonized by bacteria from the maternal feces and vaginal tract, whereas babies born via caesarean section acquire different bacteria from healthcare workers, the surrounding environment, and medical equipment [147]. Embryologically, infants delivered by caesarean section and those born through natural childbirth show variations in their early-life microbiota, and those with compromised health often have a less diverse microbial population [148].
3.3. Influences on Gut Microbiota Composition: Diet, Health, Medications, and Aging
The process of gut microbiota colonization undergoes changes based on variations in diet or health conditions [21]. In other words, the intestinal microflora balance is influenced by multiple external factors, including dietary habits, medication usage, environmental pollutants, and stress [22] (Figure 2). Healthy dietary components like a healthful plant-based diet, vegetables, and magnesium are associated with lower levels of pro-inflammatory bacteria, such as E. coli and Clostridium innocuum, while showing a positive correlation with beneficial anaerobic bacteria like F. prausnitzii and Agathobaculum butyriciproducens [149]. On the contrary, evidence suggests that the consumption of animal-based foods leads to an elevation in the population of bile-tolerant microorganisms (such as Alistipes, Bilophila, and Bacteroides). Additionally, the genes within these bacteria responsible for encoding microbial bile salt hydrolase, a key enzyme for secondary bile acid production, show notably increased activity when included in an animal-based diet [150]. Substantial rises in bile acids and their metabolites found in fecal matter could have played a role in the disruption of the gut microbiota and may have consequences for the risk of colon cancer [151]. Interestingly, it has been noted that a high intake of saturated fats from animal sources can lead to an elevated presence of Biophila wadsworthia, a member of the Desulfovibrionaceae family known for triggering acute inflammation through taurine respiration, resulting in the production of hydrogen sulfide. Conversely, when mice were fed unsaturated fats, such as polyunsaturated fats, there was a notable increase in the abundance of beneficial bacteria like Lactobacillus, known for its probiotic properties, and Akkermansia muciniphila, a species thriving in nutrient-rich environments [152]. A high-fat diet (HFD) induces an imbalance in the gut microbiota and inhibits the metabolism of butyrate, one of the SCFAs produced by the gut microbiota [153]. Furthermore, prolonged deficiency in dietary fiber can result in enduring changes in the composition of the gut microbiome, consequently affecting the development and progression of various diseases [154]. The administration of antibiotics can significantly reduce the richness and diversity of the gut microbiota, leading to reduced levels of serotonin, tryptophan hydroxylase 1, and secondary bile acids in antibiotic-treated rats [155]. The gut microbiota is maintained in a balanced state through enteroendocrine signals and immune responses. When this balance is disrupted, an intestinal bacterial imbalance, also known as “dysbiosis”, occurs, characterized by an increase in specific gut bacteria and elevated enterotoxin levels [156]. This imbalance is associated with an abnormal immune response, leading to the production of inflammatory cytokines [157]. Disruptions in the gut microbiota like these can increase susceptibility to disease [158]. Moreover, the gut microbiota undergoes changes with aging, and there is a significant difference in the microbiota composition between young and elderly adults [159]. A study revealed that certain bacterial species in the aging microbiota promote inflammation when the gut microbiota of an older mouse are transferred to a germ-free young mouse [160].
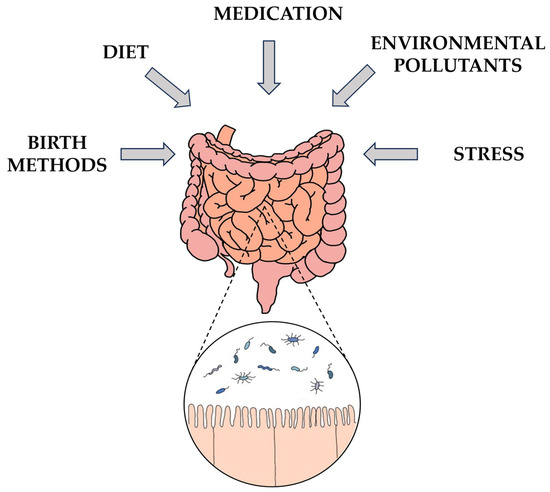
Figure 2.
Influences on gut microbiota composition.
3.4. Intestinal Epithelial Cells and the Microbiota–Gut–Brain Axis: Implications for Immune Function, CNS Disorders, and Overall Health
The gut microbiota play a vital role in regulating brain function and behavior through the “microbiota-gut-brain” (MGB) axis [13] (Figure 3). The interaction between the gut and the brain is a two-way one and primarily takes place through several routes, which include the ANS, specifically the enteric nervous system (ENS) and vagus nerve (VN), the HPA axis, the neuroendocrine system, the immune system, and metabolic pathways [12].
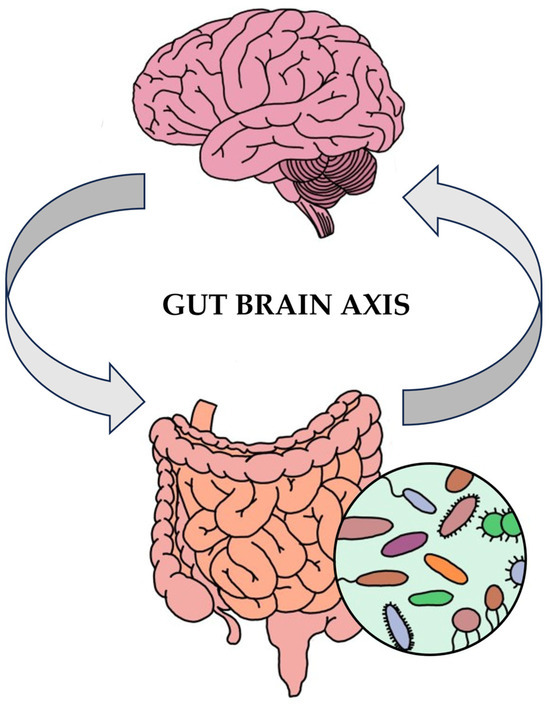
Figure 3.
Microbiota–gut–brain axis.
The ANS governs involuntary physiological functions such as heart rate, blood pressure, respiration, and digestion. It comprises the sympathetic nervous system (SNS), parasympathetic nervous system (PNS), and ENS [161]. Activation of the SNS triggers the “fight or flight” response, leading to increased heart rate and blood pressure, inhibition of glycogenolysis, and reduced gastrointestinal peristalsis. In contrast, activation of the PNS induces the “rest and digest” response, resulting in a lower heart rate and blood pressure and the resumption of gastrointestinal peristalsis and digestion [162]. The ENS regulates most of the intestinal functions to maintain a healthy microbiota [163]. Neurotransmitters and molecules produce signals that are conveyed to the brain via afferent VN fibers associated with the parasympathetic nervous system (PNS). In turn, the brain sends signals to the enterochromaffin cells (ECCs) and enteroendocrine cells (EECs) within the gut wall, which subsequently engage with the mucosal immune system through efferent VN fibers [164]. Stimulating the VN fortifies the intestinal barrier, lessens inflammation in the peripheral system and restrains the release of pro-inflammatory cytokines [165]. The HPA axis is a physiological stress system responsible for producing glucocorticoids [166]. Glucocorticoids have the potential to impact the brain and behavior, with chronic exposure to high levels associated with depression, while low levels are found among patients with post-traumatic stress disorder [92]. Stress, regulated via the HPA axis, can have consequences on the makeup of the gut microbiota and vice versa [167].
Intestinal epithelial cells (IEC) create a physical barrier separating the intestinal lumen from immune cells, and they fulfill diverse immunological roles. They generate and respond to different cytokines, as well as express molecules that interact with lymphocytes, and have pattern-recognition receptors in their composition [168]. Studies comparing the brains of animals that are colonized (specific pathogen-free, SPF) and those that are germ-free (GF) have shown a significant downregulation of genes related to microglia, indicating that the gut microbiota are crucial for microglia maturation and normalization [128]. The structural elements of bacteria engage with the immune system through Toll-like receptors (TLRs), and gut microbes can activate these receptors as well [169]. In the CNS, astrocytes, microglia, and oligodendrocytes express TLRs, which play roles in innate immunity, CNS autoimmunity, neurodegeneration, and tissue damage [170,171]. Activation of TLRs can induce pro- and anti-inflammatory cytokines [172]. As a result, disruptions or irregularities in the gut–brain axis can result in CNS disorders [173], affecting not only intestinal inflammation, chronic abdominal pain syndrome, and eating disorders, but also neurological conditions including Alzheimer’s disease, Parkinson’s disease, autism spectrum disorder, epilepsy, and major depressive disorder [13,35]. In pivotal studies, male germ-free mice exhibited higher stress responses than normal control rats [133]. Germ-free mice also exhibited heightened neuroendocrine reactions to stress, altered levels of neurotrophins in the hippocampus and amygdala, decreased anxiety and nonspatial memory, and altered brain monoamine neurotransmitter levels [174].
3.5. Gut Microbiota Metabolites and Their Impact on CNS Function: Focus on Short-Chain Fatty Acids
The gut microbiota interacts with the CNS not only to regulate food digestion, immune function, and enteroendocrine signal transmission but also through the production of various metabolites, including substances like bile acids, SCFAs, glutamate, norepinephrine, dopamine, GABA, serotonin, and histamine [175]. Among these metabolites, SCFAs have a notable role to play and are generated through the fermentation process of the gut microbiota [25]. SCFAs can pass through the blood–brain barrier (BBB) and engage with microglia, exerting wide-ranging effects on CNS function [26]. SCFAs found in the gut include acetate (C2), propionate (C3), and butyrate (C4) acids, valeric acid (C5), caproic acid (C6), among others, with hydrocarbon tails containing one to six carbon atoms [128,176]. Various bacteria produce different SCFAs. Acetate is generated by bacteria such as Bifidobacterium bifidum, Bifidobacterium infantis, and Bifidobacterium breve. Propionate undergoes three distinct conversions by bacteria. Certain types of bacteria, like Prevotella and Veillonella, are responsible for converting it into a specific compound called succinic acid. The acrylate pathway is utilized by certain bacterial groups, such as Coprococcus, while the propanediol-dependent metabolic pathway is utilized by bacteria like Roseburia inulinivorans and Blautia species. Butyrate is produced by bacteria from the Lachnospiraceae and Ruminococcaceae families [177]. These SCFAs activate G protein-coupled receptors (GPCRs), regulating immune responses, anti-inflammatory processes, reactive oxygen species (ROS) induction, and cellular processes [178].
Butyric acid, one of the SCFAs, especially exerts notable influences on the generation of various factors, including BDNF, which promotes the synthesis of neurotransmitters in the CNS through the VN [168]. Additionally, butyric acid, along with acetic acid and propionic acid, has been demonstrated to reduce the expression of genes in the hypothalamus involved in stress signaling, leading to improved behaviors related to stress reactivity and anxiety when administered to mice [179]. Acetate, another SCFA, alters the levels of neurotransmitters like glutamine, glutamate, and GABA in the hypothalamus and increases the expression of neuropeptides associated with anorexia [180]. Furthermore, SCFAs have a wide range of impacts on the immune system. When the ratio of butyric acid to caproic acid increases, the levels of regulatory T lymphocytes rise, while pro-inflammatory T lymphocytes decrease, promoting immune homeostasis [181]. For instance, sodium butyrate inhibits histone acetylation, a process that plays a vital function in aging and memory decline [182]. The gut microbiota also affects the production of serotonin in the colon by influencing intra-intestinal chromaffin cells through the action of SCFAs [183].
SCFAs have been associated with several mental disorders. For example, patients with neuropathy show decreased levels of serotonin, GABA, and dopamine, as well as reduced levels of butyrate, propionate, and acetate [184]. Additionally, the composition of the gut microbiota and SCFA levels differ when comparing individuals with autism to healthy controls. Transplanting the gut microbiota from autistic mice into healthy mice not only leads to autism-like behavior but also results in lower levels of acetate and butyrate and higher levels of valeric acid in the recipient mice [185].
The gut microbiota has a significant role to play in producing and consuming SCFAs and mammalian neurotransmitters, influencing both the CNS and the ENS [186]. However, specific neurotransmitters like GABA, dopamine, glutamate, and serotonin cannot cross the blood–brain barrier directly. Instead, their precursors, which originate from tyrosine and tryptophan, are transported through the blood–brain barrier and then transformed into neurotransmitters within the brain [35]. Of these precursors, tryptophan is predominantly absorbed by the intestine and metabolized by the gut microbiota through three downstream pathways: the 5-hydroxytryptamine pathway, the kynurenine pathway, and the indole pathway [187]. These metabolic pathways produce aryl hydrocarbon receptor (AHR) agonists, which have the ability to limit inflammation in the CNS by influencing astrocytes [188]. Moreover, the absorption of tryptophan in the intestine has regulatory effects on the serotonin and glutamate systems [82].
4. Gut Microbiota Dysbiosis in Schizophrenia and Related Disorders
When comparing the metabolic processes involving glucose and lipids of SCFA-producing bacteria and gut microbiota in schizophrenia patients to healthy individuals, SCFA-producing bacteria were less abundant, and the gut microbiota showed abnormal glucose and lipid metabolism [189]. In the comparison between schizophrenia patients and healthy controls, researchers noted a higher abundance of anaerobic bacteria and oral cavity-associated bacteria in the intestines of the patients than in the healthy controls. Remarkably, when researchers transplanted Streptococcus vestibularis, an oral bacterium, into mice, it led to the development of schizophrenia-like behavior [190]. Out of the 27 cytokines examined, which included Eotaxin, IL-1β, IL-4, IL-6, IL-8, MIP-1a, and TNF-α, 7 cytokines exhibited significant elevations in schizophrenia patients when compared to healthy individuals. Conversely, in the control group, seven other cytokines, such as IFN-γ, IL-9, IL-1ra, IL-13, MCP-1, MIP-1b, and RANTES, notably decreased in schizophrenia patients. It was noted that schizophrenia patients displayed a negative correlation between the reduced levels of Faecalibacterium, Roseburia, and Butyricicoccus, which play a role in butyrate production, and the aforementioned increased cytokines, while showing a positive correlation with the decreased cytokines mentioned earlier [191]. The changes in the gut microbiota result in the hypoactivity of N-methyl-d-aspartate (NMDA) and brain-derived neurotrophic factor (BDNF)/glial-cell derived neurotrophic factor (GDNF) receptors, which regulate brain plasticity, in schizophrenia patients [131,192]. When investigating the connection between the gut microbiota and schizophrenia, researchers compared samples from schizophrenia patients with those from healthy controls. They observed reduced gut microbiota diversity in schizophrenia patients, with 23 operational taxonomic units (OTUs) out of 77 showing increased abundance in the patient group compared to healthy controls. Additionally, when mice were subjected to fecal transplants from individuals with schizophrenia, their neurotransmitter levels in the hippocampus were affected, resulting in reduced levels of glutamate and increased levels of glutamine and GABA [193]. Glutamate plays a crucial role in synaptic plasticity. However, dysfunction in glutamate neurotransmission, particularly disruptions in the signaling of ionotropic glutamate receptors (iGluRs), is associated with schizophrenia and other neurological disorders [194]. Notably, butyrate was also noted for its neuroprotective properties in animal models of Parkinson’s disease, where it reversed reductions in histone acetylation associated with the disease [195,196], and patients with schizophrenia showed a dysregulation of histone deacetylase [196]. Further insights emerged when researchers compared the fecal composition of inpatient schizophrenia patients, distinguishing between those with aggression (ScZ-Ag) and those without (NScZ-Ag). Within the ScZ-Ag group, Prevotella increased, while Bacteroides, Bifidobacterium, Faecalibacterium, Blautia, Collinsella, and Eubacterium_coprostanoligenes decreased. Furthermore, the ScZ-Ag group showed significantly lower levels of acetic acid, propanoic acid, butyric acid, isobutyric acid, isovaleric acid, and isohexanoic acid in their stool compared to the NScZ-Ag group [197]. Moreover, notable changes in the serum concentration of butyric acid were detected in individuals with schizophrenia. Initially, these levels were similar to those in healthy controls, but they increased after treatment [198]. Among the SCFAs produced by gut microbes, valeric acid was found to protect brain cells from excitotoxicity and cell death, while caproic acid, another SCFA, was shown to influence cognitive function, with its levels found to be lower in schizophrenia patients compared to healthy controls [24,199]. In individuals with schizophrenia, the concentration of isovaleric acid was notably elevated compared to healthy controls. Notably, a strong inverse relationship was observed between higher isovaleric acid levels and reduced RBANS scores for both immediate and delayed memory in schizophrenia patients [200]. In patients with schizophrenia, a significant negative correlation was found between the ratio of acetic acid to propionic acid and the sub-scores of working memory and reasoning on the MCCB. This aligns with existing research indicating a connection between SCFA and neurocognitive dysfunction [201].
5. Conclusions
In this review, our primary objective was to explore and shed light on the potential relationship between schizophrenia, the gut microbiota, the gut–brain axis, and SCFAs. We investigated whether SCFA, a metabolite produced by the gut microbiota, might be associated with schizophrenia. Our findings suggest that SCFAs can traverse the blood–brain barrier (BBB) and influence CNS activity, including the modulation of microglia activity and cytokine production. Specifically, butyrate appears to impact epigenetic processes, leading to increased histone acetylation.
It is essential to note that there has been limited research into how the gut microbiota influences mental health, particularly in the context of schizophrenia. Most studies have lacked large-scale human clinical trials, and the considerable variability in gut microbiota composition and SCFA production among individuals makes it challenging to establish a clear association with schizophrenia. Additionally, the precise mechanism through which SCFA influences schizophrenia remains unclear, necessitating further research before considering therapeutic applications.
Despite these limitations, our findings hold promise for potential future developments. As the realm of research on the gut–brain axis and its impact on mental health continues to grow, these studies may serve as potential indicators for identifying and predicting of schizophrenia. Additionally, additional progress in this field could result in the creation of innovative treatment approaches that target the gut microbiota for the management of schizophrenia.
In conclusion, while our review highlights the potential link between SCFA, the gut microbiota, and schizophrenia, it is crucial to acknowledge the current limitations and the need for further research. As the scientific community delves deeper into this field, an improved comprehension of the gut–brain axis in schizophrenia could offer valuable insights into diagnosis, treatment, and patient outcomes.
Author Contributions
Conceptualization, S.J. and T.G.C.; resources, S.J., Y.S., S.H. and J.K.; writing—original draft preparation, S.J., Y.S., S.H. and J.K.; writing—review and editing, S.J., T.G.C. and I.K.; supervision, Y.S., T.G.C., I.K. and S.S.K.; project administration, I.K. and S.S.K.; funding acquisition, S.S.K. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by National Research Foundation of Korea (NRF) grants funded by the Korean government (MEST) (Grant No: NRF-2018R1A6A1A03025124).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kahn, R.S.; Sommer, I.E.; Murray, R.M.; Meyer-Lindenberg, A.; Weinberger, D.R.; Cannon, T.D.; O’Donovan, M.; Correll, C.U.; Kane, J.M.; van Os, J.; et al. Schizophrenia. Nat. Rev. Dis. Primers 2015, 1, 15067. [Google Scholar] [CrossRef] [PubMed]
- Pulver, A.E. Search for schizophrenia susceptibility genes. Biol. Psychiatry 2000, 47, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Brzustowicz, L.M.; Hodgkinson, K.A.; Chow, E.W.; Honer, W.G.; Bassett, A.S. Location of a major susceptibility locus for familial schizophrenia on chromosome 1q21-q22. Science 2000, 288, 678–682. [Google Scholar] [CrossRef] [PubMed]
- Varese, F.; Smeets, F.; Drukker, M.; Lieverse, R.; Lataster, T.; Viechtbauer, W.; Read, J.; van Os, J.; Bentall, R.P. Childhood adversities increase the risk of psychosis: A meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr. Bull. 2012, 38, 661–671. [Google Scholar] [CrossRef]
- Eaton, W.W.; Byrne, M.; Ewald, H.; Mors, O.; Chen, C.Y.; Agerbo, E.; Mortensen, P.B. Association of schizophrenia and autoimmune diseases: Linkage of Danish national registers. Am. J. Psychiatry 2006, 163, 521–528. [Google Scholar] [CrossRef] [PubMed]
- Debost, J.C.; Larsen, J.T.; Munk-Olsen, T.; Mortensen, P.B.; Agerbo, E.; Petersen, L.V. Childhood infections and schizophrenia: The impact of parental SES and mental illness, and childhood adversities. Brain Behav. Immun. 2019, 81, 341–347. [Google Scholar] [CrossRef]
- Tsuang, M.T.; Stone, W.S.; Faraone, S.V. Genes, environment and schizophrenia. Br. J. Psychiatry 2001, 40, s18–s24. [Google Scholar] [CrossRef]
- Li, X.; Wei, N.; Song, J.; Liu, J.; Yuan, J.; Song, R.; Liu, L.; Mei, L.; Yan, S.; Wu, Y.; et al. The global burden of schizophrenia and the impact of urbanization during 1990–2019: An analysis of the global burden of disease study 2019. Environ. Res. 2023, 232, 116305. [Google Scholar] [CrossRef]
- Larsson, S.; Andreassen, O.A.; Aas, M.; Rossberg, J.I.; Mork, E.; Steen, N.E.; Barrett, E.A.; Lagerberg, T.V.; Peleikis, D.; Agartz, I.; et al. High prevalence of childhood trauma in patients with schizophrenia spectrum and affective disorder. Compr. Psychiatry 2013, 54, 123–127. [Google Scholar] [CrossRef]
- Cryan, J.F.; Dinan, T.G. Gut microbiota: Microbiota and neuroimmune signalling-Metchnikoff to microglia. Nat. Rev. Gastroenterol. Hepatol. 2015, 12, 494–496. [Google Scholar] [CrossRef]
- Skonieczna-Zydecka, K.; Janda, K.; Kaczmarczyk, M.; Marlicz, W.; Loniewski, I.; Loniewska, B. The Effect of Probiotics on Symptoms, Gut Microbiota and Inflammatory Markers in Infantile Colic: A Systematic Review, Meta-Analysis and Meta-Regression of Randomized Controlled Trials. J. Clin. Med. 2020, 9, 999. [Google Scholar] [CrossRef] [PubMed]
- Morais, L.H.; Schreiber, H.L.; Mazmanian, S.K. The gut microbiota–brain axis in behaviour and brain disorders. Nat. Rev. Microbiol. 2021, 19, 241–255. [Google Scholar] [CrossRef]
- Cryan, J.F.; Dinan, T.G. Mind-altering microorganisms: The impact of the gut microbiota on brain and behaviour. Nat. Rev. Neurosci. 2012, 13, 701–712. [Google Scholar] [CrossRef] [PubMed]
- Tomas, J.; Wrzosek, L.; Bouznad, N.; Bouet, S.; Mayeur, C.; Noordine, M.L.; Honvo-Houeto, E.; Langella, P.; Thomas, M.; Cherbuy, C. Primocolonization is associated with colonic epithelial maturation during conventionalization. FASEB J. 2013, 27, 645–655. [Google Scholar] [CrossRef]
- Caballero, S.; Pamer, E.G. Microbiota-mediated inflammation and antimicrobial defense in the intestine. Annu. Rev. Immunol. 2015, 33, 227–256. [Google Scholar] [CrossRef]
- Magnúsdóttir, S.; Ravcheev, D.; de Crécy-Lagard, V.; Thiele, I. Systematic genome assessment of B-vitamin biosynthesis suggests co-operation among gut microbes. Front. Genet. 2015, 6, 148. [Google Scholar] [CrossRef] [PubMed]
- DiGiulio, D.B. Diversity of microbes in amniotic fluid. Semin. Fetal Neonatal Med. 2012, 17, 2–11. [Google Scholar] [CrossRef]
- Jiménez, E.; Fernández, L.; Marín, M.L.; Martín, R.; Odriozola, J.M.; Nueno-Palop, C.; Narbad, A.; Olivares, M.; Xaus, J.; Rodríguez, J.M. Isolation of commensal bacteria from umbilical cord blood of healthy neonates born by cesarean section. Curr. Microbiol. 2005, 51, 270–274. [Google Scholar] [CrossRef]
- Aagaard, K.; Ma, J.; Antony, K.M.; Ganu, R.; Petrosino, J.; Versalovic, J. The placenta harbors a unique microbiome. Sci. Transl. Med. 2014, 6, 237ra265. [Google Scholar] [CrossRef]
- Clemente, J.C.; Ursell, L.K.; Parfrey, L.W.; Knight, R. The impact of the gut microbiota on human health: An integrative view. Cell 2012, 148, 1258–1270. [Google Scholar] [CrossRef]
- Koenig, J.E.; Spor, A.; Scalfone, N.; Fricker, A.D.; Stombaugh, J.; Knight, R.; Angenent, L.T.; Ley, R.E. Succession of microbial consortia in the developing infant gut microbiome. Proc. Natl. Acad. Sci. USA 2011, 108 (Suppl. S1), 4578–4585. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Wu, S.; Zeng, Z.; Fu, Z. Effects of environmental pollutants on gut microbiota. Environ. Pollut. 2017, 222, 1–9. [Google Scholar] [CrossRef] [PubMed]
- McGuinness, A.J.; Davis, J.A.; Dawson, S.L.; Loughman, A.; Collier, F.; O’Hely, M.; Simpson, C.A.; Green, J.; Marx, W.; Hair, C.; et al. A systematic review of gut microbiota composition in observational studies of major depressive disorder, bipolar disorder and schizophrenia. Mol. Psychiatry 2022, 27, 1920–1935. [Google Scholar] [CrossRef] [PubMed]
- Peng, H.; Ouyang, L.; Li, D.; Li, Z.; Yuan, L.; Fan, L.; Liao, A.; Li, J.; Wei, Y.; Yang, Z.; et al. Short-chain fatty acids in patients with schizophrenia and ultra-high risk population. Front. Psychiatry 2022, 13, 977538. [Google Scholar] [CrossRef]
- Martin-Gallausiaux, C.; Marinelli, L.; Blottière, H.M.; Larraufie, P.; Lapaque, N. SCFA: Mechanisms and functional importance in the gut. Proc. Nutr. Soc. 2021, 80, 37–49. [Google Scholar] [CrossRef]
- Wenzel, T.J.; Gates, E.J.; Ranger, A.L.; Klegeris, A. Short-chain fatty acids (SCFAs) alone or in combination regulate select immune functions of microglia-like cells. Mol. Cell Neurosci. 2020, 105, 103493. [Google Scholar] [CrossRef]
- Kesby, J.P.; Eyles, D.W.; McGrath, J.J.; Scott, J.G. Dopamine, psychosis and schizophrenia: The widening gap between basic and clinical neuroscience. Transl. Psychiatry 2018, 8, 30. [Google Scholar] [CrossRef]
- Maki-Marttunen, V.; Andreassen, O.A.; Espeseth, T. The role of norepinephrine in the pathophysiology of schizophrenia. Neurosci. Biobehav. Rev. 2020, 118, 298–314. [Google Scholar] [CrossRef]
- Balu, D.T. The NMDA Receptor and Schizophrenia: From Pathophysiology to Treatment. Adv. Pharmacol. 2016, 76, 351–382. [Google Scholar] [CrossRef]
- Olney, J.W.; Farber, N.B. Glutamate receptor dysfunction and schizophrenia. Arch. Gen. Psychiatry 1995, 52, 998–1007. [Google Scholar] [CrossRef]
- Bustillo, J.R.; Chen, H.; Jones, T.; Lemke, N.; Abbott, C.; Qualls, C.; Canive, J.; Gasparovic, C. Increased glutamine in patients undergoing long-term treatment for schizophrenia: A proton magnetic resonance spectroscopy study at 3 T. JAMA Psychiatry 2014, 71, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Eggers, A.E. A serotonin hypothesis of schizophrenia. Med. Hypotheses 2013, 80, 791–794. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Liu, J.; Chen, Z. The Histaminergic System in Neuropsychiatric Disorders. Biomolecules 2021, 11, 1345. [Google Scholar] [CrossRef] [PubMed]
- Ahn, K.; Gil, R.; Seibyl, J.; Sewell, R.A.; D’Souza, D.C. Probing GABA receptor function in schizophrenia with iomazenil. Neuropsychopharmacology 2011, 36, 677–683. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Xu, J.; Chen, Y. Regulation of Neurotransmitters by the Gut Microbiota and Effects on Cognition in Neurological Disorders. Nutrients 2021, 13, 2099. [Google Scholar] [CrossRef]
- Chien, I.C.; Chou, Y.J.; Lin, C.H.; Bih, S.H.; Chou, P.; Chang, H.J. Prevalence and incidence of schizophrenia among national health insurance enrollees in Taiwan, 1996–2001. Psychiatry Clin. Neurosci. 2004, 58, 611–618. [Google Scholar] [CrossRef]
- Aleman, A.; Kahn, R.S.; Selten, J.P. Sex differences in the risk of schizophrenia: Evidence from meta-analysis. Arch. Gen. Psychiatry 2003, 60, 565–571. [Google Scholar] [CrossRef]
- Lewis, D.A.; Lieberman, J.A. Catching Up on Schizophrenia: Natural History and Neurobiology. Neuron 2000, 28, 325–334. [Google Scholar] [CrossRef]
- Nagappan-Chettiar, S.; Burbridge, T.J.; Umemori, H. Activity-Dependent Synapse Refinement: From Mechanisms to Molecules. Neuroscientist 2023. ahead of print. [Google Scholar] [CrossRef]
- Green, M.F. What are the functional consequences of neurocognitive deficits in schizophrenia? Am. J. Psychiatry 1996, 153, 321–330. [Google Scholar] [CrossRef]
- Abdullah, H.M.; Azeb Shahul, H.; Hwang, M.Y.; Ferrando, S. Comorbidity in Schizophrenia: Conceptual Issues and Clinical Management. Focus 2020, 18, 386–390. [Google Scholar] [CrossRef]
- Vidailhet, P. First-episode psychosis, cognitive difficulties and remediation. Encephale 2013, 39 (Suppl. S2), S83–S92. [Google Scholar] [CrossRef] [PubMed]
- Bozikas, V.P.; Andreou, C. Longitudinal studies of cognition in first episode psychosis: A systematic review of the literature. Aust. N. Z. J. Psychiatry 2011, 45, 93–108. [Google Scholar] [CrossRef] [PubMed]
- McGlashan, T.H. Early detection and intervention in schizophrenia: Research. Schizophr. Bull. 1996, 22, 327–345. [Google Scholar] [CrossRef] [PubMed]
- Norman, R.M.; Lewis, S.W.; Marshall, M. Duration of untreated psychosis and its relationship to clinical outcome. Br. J. Psychiatry 2005, 48, s19–s23. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nimgaonkar, V.L.; Prasad, K.M.; Chowdari, K.V.; Severance, E.G.; Yolken, R.H. The complement system: A gateway to gene-environment interactions in schizophrenia pathogenesis. Mol. Psychiatry 2017, 22, 1554–1561. [Google Scholar] [CrossRef]
- Gottesman, I.I.; Erlenmeyer-Kimling, L. Family and twin strategies as a head start in defining prodromes and endophenotypes for hypothetical early-interventions in schizophrenia. Schizophr. Res. 2001, 51, 93–102. [Google Scholar] [CrossRef]
- van Winkel, R.; van Nierop, M.; Myin-Germeys, I.; van Os, J. Childhood trauma as a cause of psychosis: Linking genes, psychology, and biology. Can. J. Psychiatry 2013, 58, 44–51. [Google Scholar] [CrossRef]
- Pedersen, C.B.; Mortensen, P.B. Evidence of a dose-response relationship between urbanicity during upbringing and schizophrenia risk. Arch. Gen. Psychiatry 2001, 58, 1039–1046. [Google Scholar] [CrossRef]
- Babulas, V.; Factor-Litvak, P.; Goetz, R.; Schaefer, C.A.; Brown, A.S. Prenatal exposure to maternal genital and reproductive infections and adult schizophrenia. Am. J. Psychiatry 2006, 163, 927–929. [Google Scholar] [CrossRef]
- Bale, T.L. Epigenetic and transgenerational reprogramming of brain development. Nat. Rev. Neurosci. 2015, 16, 332–344. [Google Scholar] [CrossRef] [PubMed]
- Spencer, S.J.; Meyer, U. Perinatal programming by inflammation. Brain Behav. Immun. 2017, 63, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Torrey, E.F.; Yolken, R.H. Toxoplasma gondii and schizophrenia. Emerg. Infect. Dis. 2003, 9, 1375–1380. [Google Scholar] [CrossRef] [PubMed]
- Bhadra, R.; Cobb, D.A.; Weiss, L.M.; Khan, I.A. Psychiatric disorders in toxoplasma seropositive patients—The CD8 connection. Schizophr. Bull. 2013, 39, 485–489. [Google Scholar] [CrossRef]
- Carruthers, V.B.; Suzuki, Y. Effects of Toxoplasma gondii infection on the brain. Schizophr. Bull. 2007, 33, 745–751. [Google Scholar] [CrossRef]
- Prandovszky, E.; Gaskell, E.; Martin, H.; Dubey, J.P.; Webster, J.P.; McConkey, G.A. The neurotropic parasite Toxoplasma gondii increases dopamine metabolism. PLoS ONE 2011, 6, e23866. [Google Scholar] [CrossRef]
- Arias, I.; Sorlozano, A.; Villegas, E.; de Dios Luna, J.; McKenney, K.; Cervilla, J.; Gutierrez, B.; Gutierrez, J. Infectious agents associated with schizophrenia: A meta-analysis. Schizophr. Res. 2012, 136, 128–136. [Google Scholar] [CrossRef]
- Molloy, M.J.; Grainger, J.R.; Bouladoux, N.; Hand, T.W.; Koo, L.Y.; Naik, S.; Quinones, M.; Dzutsev, A.K.; Gao, J.L.; Trinchieri, G.; et al. Intraluminal containment of commensal outgrowth in the gut during infection-induced dysbiosis. Cell Host Microbe 2013, 14, 318–328. [Google Scholar] [CrossRef]
- Bitanihirwe, B.K.; Woo, T.U. Perineuronal nets and schizophrenia: The importance of neuronal coatings. Neurosci. Biobehav. Rev. 2014, 45, 85–99. [Google Scholar] [CrossRef]
- de Faria, O., Jr.; Pivonkova, H.; Varga, B.; Timmler, S.; Evans, K.A.; Karadottir, R.T. Periods of synchronized myelin changes shape brain function and plasticity. Nat. Neurosci. 2021, 24, 1508–1521. [Google Scholar] [CrossRef]
- Keshavan, M.S.; Anderson, S.; Pettegrew, J.W. Is schizophrenia due to excessive synaptic pruning in the prefrontal cortex? The Feinberg hypothesis revisited. J. Psychiatr. Res. 1994, 28, 239–265. [Google Scholar] [CrossRef]
- Zhang, K.; Sejnowski, T.J. A universal scaling law between gray matter and white matter of cerebral cortex. Proc. Natl. Acad. Sci. USA 2000, 97, 5621–5626. [Google Scholar] [CrossRef] [PubMed]
- Bartzokis, G. Schizophrenia: Breakdown in the well-regulated lifelong process of brain development and maturation. Neuropsychopharmacology 2002, 27, 672–683. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bartzokis, G.; Nuechterlein, K.H.; Lu, P.H.; Gitlin, M.; Rogers, S.; Mintz, J. Dysregulated brain development in adult men with schizophrenia: A magnetic resonance imaging study. Biol. Psychiatry 2003, 53, 412–421. [Google Scholar] [CrossRef]
- Kelly, S.; Jahanshad, N.; Zalesky, A.; Kochunov, P.; Agartz, I.; Alloza, C.; Andreassen, O.A.; Arango, C.; Banaj, N.; Bouix, S.; et al. Widespread white matter microstructural differences in schizophrenia across 4322 individuals: Results from the ENIGMA Schizophrenia DTI Working Group. Mol. Psychiatry 2018, 23, 1261–1269. [Google Scholar] [CrossRef] [PubMed]
- Liu, N.; Xiao, Y.; Zhang, W.; Tang, B.; Zeng, J.; Hu, N.; Chandan, S.; Gong, Q.; Lui, S. Characteristics of gray matter alterations in never-treated and treated chronic schizophrenia patients. Transl. Psychiatry 2020, 10, 136. [Google Scholar] [CrossRef] [PubMed]
- Rizo, J. Mechanism of neurotransmitter release coming into focus. Protein Sci. 2018, 27, 1364–1391. [Google Scholar] [CrossRef]
- Yang, X.; Lou, J.; Shan, W.; Ding, J.; Jin, Z.; Hu, Y.; Du, Q.; Liao, Q.; Xie, R.; Xu, J. Pathophysiologic Role of Neurotransmitters in Digestive Diseases. Front. Physiol. 2021, 12, 567650. [Google Scholar] [CrossRef]
- Miller, M.W. Dopamine as a Multifunctional Neurotransmitter in Gastropod Molluscs: An Evolutionary Hypothesis. Biol. Bull. 2020, 239, 189–208. [Google Scholar] [CrossRef]
- Prokopová, I. Noradrenaline and behavior. Cesk Fysiol. 2010, 59, 51–58. [Google Scholar]
- Bari, B.A.; Chokshi, V.; Schmidt, K. Locus coeruleus-norepinephrine: Basic functions and insights into Parkinson’s disease. Neural Regen. Res. 2020, 15, 1006–1013. [Google Scholar] [CrossRef]
- Gershon, S.; Hekimian, L.J.; Floyd, A., Jr.; Hollister, L.E. Alpha-methyl-p-tyrosine (AMT) in schizophrenia. Psychopharmacologia 1967, 11, 189–194. [Google Scholar] [CrossRef]
- Zhou, Y.; Danbolt, N.C. Glutamate as a neurotransmitter in the healthy brain. J. Neural Transm. 2014, 121, 799–817. [Google Scholar] [CrossRef] [PubMed]
- Hertz, L.; Rothman, D.L. Glucose, Lactate, β-Hydroxybutyrate, Acetate, GABA, and Succinate as Substrates for Synthesis of Glutamate and GABA in the Glutamine-Glutamate/GABA Cycle. Adv. Neurobiol. 2016, 13, 9–42. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, H.; Singh, S.K.; Mancusso, R.; Gouaux, E. Subunit arrangement and function in NMDA receptors. Nature 2005, 438, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Papouin, T.; Oliet, S.H. Organization, control and function of extrasynaptic NMDA receptors. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2014, 369, 20130601. [Google Scholar] [CrossRef] [PubMed]
- Panatier, A.; Theodosis, D.T.; Mothet, J.P.; Touquet, B.; Pollegioni, L.; Poulain, D.A.; Oliet, S.H. Glia-derived d-serine controls NMDA receptor activity and synaptic memory. Cell 2006, 125, 775–784. [Google Scholar] [CrossRef] [PubMed]
- McCullumsmith, R.E.; O’Donovan, S.M.; Drummond, J.B.; Benesh, F.S.; Simmons, M.; Roberts, R.; Lauriat, T.; Haroutunian, V.; Meador-Woodruff, J.H. Cell-specific abnormalities of glutamate transporters in schizophrenia: Sick astrocytes and compensating relay neurons? Mol. Psychiatry 2016, 21, 823–830. [Google Scholar] [CrossRef]
- Karlsson, R.M.; Tanaka, K.; Heilig, M.; Holmes, A. Loss of glial glutamate and aspartate transporter (excitatory amino acid transporter 1) causes locomotor hyperactivity and exaggerated responses to psychotomimetics: Rescue by haloperidol and metabotropic glutamate 2/3 agonist. Biol. Psychiatry 2008, 64, 810–814. [Google Scholar] [CrossRef]
- Berger, M.; Gray, J.A.; Roth, B.L. The expanded biology of serotonin. Annu. Rev. Med. 2009, 60, 355–366. [Google Scholar] [CrossRef]
- Roth, W.; Zadeh, K.; Vekariya, R.; Ge, Y.; Mohamadzadeh, M. Tryptophan Metabolism and Gut-Brain Homeostasis. Int. J. Mol. Sci. 2021, 22, 2973. [Google Scholar] [CrossRef] [PubMed]
- Barry, S.; Clarke, G.; Scully, P.; Dinan, T.G. Kynurenine pathway in psychosis: Evidence of increased tryptophan degradation. J. Psychopharmacol. 2009, 23, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.; Chen, Z. The roles of histamine and its receptor ligands in central nervous system disorders: An update. Pharmacol. Ther. 2017, 175, 116–132. [Google Scholar] [CrossRef] [PubMed]
- Prell, G.D.; Green, J.P.; Kaufmann, C.A.; Khandelwal, J.K.; Morrishow, A.M.; Kirch, D.G.; Linnoila, M.; Wyatt, R.J. Histamine metabolites in cerebrospinal fluid of patients with chronic schizophrenia: Their relationships to levels of other aminergic transmitters and ratings of symptoms. Schizophr. Res. 1995, 14, 93–104. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Xu, C.; Wang, L.; An, D.; Jiang, L.; Zheng, Y.; Xu, Y.; Wang, Y.; Wang, Y.; Zhang, K.; et al. Histamine H(1) receptor deletion in cholinergic neurons induces sensorimotor gating ability deficit and social impairments in mice. Nat. Commun. 2021, 12, 1142. [Google Scholar] [CrossRef] [PubMed]
- Ma, Q.; Jiang, L.; Chen, H.; An, D.; Ping, Y.; Wang, Y.; Dai, H.; Zhang, X.; Wang, Y.; Chen, Z.; et al. Histamine H(2) receptor deficit in glutamatergic neurons contributes to the pathogenesis of schizophrenia. Proc. Natl. Acad. Sci. USA 2023, 120, e2207003120. [Google Scholar] [CrossRef]
- Sharma, P.; Sharma, B.S.; Raval, H.; Singh, V. Endocytosis of GABA receptor: Signaling in nervous system. Prog. Mol. Biol. Transl. Sci. 2023, 196, 125–139. [Google Scholar] [CrossRef]
- Fujibayashi, M.; Matsumoto, T.; Kishida, I.; Kimura, T.; Ishii, C.; Ishii, N.; Moritani, T. Autonomic nervous system activity and psychiatric severity in schizophrenia. Psychiatry Clin. Neurosci. 2009, 63, 538–545. [Google Scholar] [CrossRef]
- Haigh, S.M.; Walford, T.P.; Brosseau, P. Heart Rate Variability in Schizophrenia and Autism. Front. Psychiatry 2021, 12, 760396. [Google Scholar] [CrossRef]
- Anacker, C.; O’Donnell, K.J.; Meaney, M.J. Early life adversity and the epigenetic programming of hypothalamic-pituitary-adrenal function. Dialogues Clin. Neurosci. 2014, 16, 321–333. [Google Scholar] [CrossRef]
- Meyer, J.S. Early adrenalectomy stimulates subsequent growth and development of the rat brain. Exp. Neurol. 1983, 82, 432–446. [Google Scholar] [CrossRef] [PubMed]
- Lupien, S.J.; McEwen, B.S.; Gunnar, M.R.; Heim, C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat. Rev. Neurosci. 2009, 10, 434–445. [Google Scholar] [CrossRef] [PubMed]
- Koenig, J.I.; Kirkpatrick, B.; Lee, P. Glucocorticoid hormones and early brain development in schizophrenia. Neuropsychopharmacology 2002, 27, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Miller, B.J.; Buckley, P.; Seabolt, W.; Mellor, A.; Kirkpatrick, B. Meta-analysis of cytokine alterations in schizophrenia: Clinical status and antipsychotic effects. Biol. Psychiatry 2011, 70, 663–671. [Google Scholar] [CrossRef]
- Lin, J.X.; Leonard, W.J. Fine-Tuning Cytokine Signals. Annu. Rev. Immunol. 2019, 37, 295–324. [Google Scholar] [CrossRef]
- Dantzer, R.; O’Connor, J.C.; Freund, G.G.; Johnson, R.W.; Kelley, K.W. From inflammation to sickness and depression: When the immune system subjugates the brain. Nat. Rev. Neurosci. 2008, 9, 46–56. [Google Scholar] [CrossRef]
- Biesmans, S.; Bouwknecht, J.A.; Ver Donck, L.; Langlois, X.; Acton, P.D.; De Haes, P.; Davoodi, N.; Meert, T.F.; Hellings, N.; Nuydens, R. Peripheral Administration of Tumor Necrosis Factor-Alpha Induces Neuroinflammation and Sickness but Not Depressive-Like Behavior in Mice. Biomed. Res. Int. 2015, 2015, 716920. [Google Scholar] [CrossRef]
- Kohman, R.A.; Rhodes, J.S. Neurogenesis, inflammation and behavior. Brain Behav. Immun. 2013, 27, 22–32. [Google Scholar] [CrossRef]
- Eroglu, C.; Barres, B.A. Regulation of synaptic connectivity by glia. Nature 2010, 468, 223–231. [Google Scholar] [CrossRef]
- Facci, L.; Barbierato, M.; Marinelli, C.; Argentini, C.; Skaper, S.D.; Giusti, P. Toll-like receptors 2, -3 and -4 prime microglia but not astrocytes across central nervous system regions for ATP-dependent interleukin-1beta release. Sci. Rep. 2014, 4, 6824. [Google Scholar] [CrossRef]
- Tay, T.L.; Savage, J.C.; Hui, C.W.; Bisht, K.; Tremblay, M.E. Microglia across the lifespan: From origin to function in brain development, plasticity and cognition. J. Physiol. 2017, 595, 1929–1945. [Google Scholar] [CrossRef] [PubMed]
- Hodes, G.E.; Kana, V.; Menard, C.; Merad, M.; Russo, S.J. Neuroimmune mechanisms of depression. Nat. Neurosci. 2015, 18, 1386–1393. [Google Scholar] [CrossRef] [PubMed]
- Gallego, J.A.; Blanco, E.A.; Husain-Krautter, S.; Madeline Fagen, E.; Moreno-Merino, P.; Del Ojo-Jimenez, J.A.; Ahmed, A.; Rothstein, T.L.; Lencz, T.; Malhotra, A.K. Cytokines in cerebrospinal fluid of patients with schizophrenia spectrum disorders: New data and an updated meta-analysis. Schizophr. Res. 2018, 202, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Catts, V.S.; Sheedy, D.; McCrossin, T.; Kril, J.J.; Shannon Weickert, C. Cortical grey matter volume reduction in people with schizophrenia is associated with neuro-inflammation. Transl. Psychiatry 2016, 6, e982. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.; Lee, E.E.; Martin, A.S.; Soontornniyomkij, B.; Soontornniyomkij, V.; Achim, C.L.; Reuter, C.; Irwin, M.R.; Eyler, L.T.; Jeste, D.V. Abnormalities in chemokine levels in schizophrenia and their clinical correlates. Schizophr. Res. 2017, 181, 63–69. [Google Scholar] [CrossRef]
- Kwak, J.Y.; Mamura, M.; Barlic-Dicen, J.; Grage-Griebenow, E. Pathophysiological roles of cytokine-chemokine immune network. J. Immunol. Res. 2014, 2014, 615130. [Google Scholar] [CrossRef]
- Schizophrenia Working Group of the Psychiatric Genomics Consortium. Biological insights from 108 schizophrenia-associated genetic loci. Nature 2014, 511, 421–427. [Google Scholar] [CrossRef]
- Liddelow, S.A.; Barres, B.A. Reactive Astrocytes: Production, Function, and Therapeutic Potential. Immunity 2017, 46, 957–967. [Google Scholar] [CrossRef]
- Goshi, N.; Morgan, R.K.; Lein, P.J.; Seker, E. A primary neural cell culture model to study neuron, astrocyte, and microglia interactions in neuroinflammation. J. Neuroinflammation 2020, 17, 155. [Google Scholar] [CrossRef]
- Gotoh, M.; Miyamoto, Y.; Ikeshima-Kataoka, H. Astrocytic Neuroimmunological Roles Interacting with Microglial Cells in Neurodegenerative Diseases. Int. J. Mol. Sci. 2023, 24, 1599. [Google Scholar] [CrossRef]
- Chung, W.S.; Allen, N.J.; Eroglu, C. Astrocytes Control Synapse Formation, Function, and Elimination. Cold Spring Harb. Perspect. Biol. 2015, 7, a020370. [Google Scholar] [CrossRef] [PubMed]
- Verkhratsky, A.; Nedergaard, M. Physiology of Astroglia. Physiol. Rev. 2018, 98, 239–389. [Google Scholar] [CrossRef] [PubMed]
- Liddelow, S.A.; Guttenplan, K.A.; Clarke, L.E.; Bennett, F.C.; Bohlen, C.J.; Schirmer, L.; Bennett, M.L.; Munch, A.E.; Chung, W.S.; Peterson, T.C.; et al. Neurotoxic reactive astrocytes are induced by activated microglia. Nature 2017, 541, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Lima, A.; Sardinha, V.M.; Oliveira, A.F.; Reis, M.; Mota, C.; Silva, M.A.; Marques, F.; Cerqueira, J.J.; Pinto, L.; Sousa, N.; et al. Astrocyte pathology in the prefrontal cortex impairs the cognitive function of rats. Mol. Psychiatry 2014, 19, 834–841. [Google Scholar] [CrossRef] [PubMed]
- Katsel, P.; Byne, W.; Roussos, P.; Tan, W.; Siever, L.; Haroutunian, V. Astrocyte and glutamate markers in the superficial, deep, and white matter layers of the anterior cingulate gyrus in schizophrenia. Neuropsychopharmacology 2011, 36, 1171–1177. [Google Scholar] [CrossRef]
- Kim, R.; Healey, K.L.; Sepulveda-Orengo, M.T.; Reissner, K.J. Astroglial correlates of neuropsychiatric disease: From astrocytopathy to astrogliosis. Prog. Neuropsychopharmacol. Biol. Psychiatry 2018, 87 Pt A, 126–146. [Google Scholar] [CrossRef]
- Tarasov, V.V.; Svistunov, A.A.; Chubarev, V.N.; Sologova, S.S.; Mukhortova, P.; Levushkin, D.; Somasundaram, S.G.; Kirkland, C.E.; Bachurin, S.O.; Aliev, G. Alterations of Astrocytes in the Context of Schizophrenic Dementia. Front. Pharmacol. 2019, 10, 1612. [Google Scholar] [CrossRef]
- Trépanier, M.O.; Hopperton, K.E.; Mizrahi, R.; Mechawar, N.; Bazinet, R.P. Postmortem evidence of cerebral inflammation in schizophrenia: A systematic review. Mol. Psychiatry 2016, 21, 1009–1026. [Google Scholar] [CrossRef]
- Windrem, M.S.; Osipovitch, M.; Liu, Z.; Bates, J.; Chandler-Militello, D.; Zou, L.; Munir, J.; Schanz, S.; McCoy, K.; Miller, R.H.; et al. Human iPSC Glial Mouse Chimeras Reveal Glial Contributions to Schizophrenia. Cell Stem Cell 2017, 21, 195–208.e196. [Google Scholar] [CrossRef]
- Maguire, E.; Connor-Robson, N.; Shaw, B.; O’Donoghue, R.; Stoberl, N.; Hall-Roberts, H. Assaying Microglia Functions In Vitro. Cells 2022, 11, 3414. [Google Scholar] [CrossRef]
- Guo, S.; Wang, H.; Yin, Y. Microglia Polarization From M1 to M2 in Neurodegenerative Diseases. Front. Aging Neurosci. 2022, 14, 815347. [Google Scholar] [CrossRef] [PubMed]
- Graeber, M.B.; Streit, W.J. Microglia: Biology and pathology. Acta Neuropathol. 2010, 119, 89–105. [Google Scholar] [CrossRef]
- Fontainhas, A.M.; Wang, M.; Liang, K.J.; Chen, S.; Mettu, P.; Damani, M.; Fariss, R.N.; Li, W.; Wong, W.T. Microglial morphology and dynamic behavior is regulated by ionotropic glutamatergic and GABAergic neurotransmission. PLoS ONE 2011, 6, e15973. [Google Scholar] [CrossRef] [PubMed]
- Hinwood, M.; Morandini, J.; Day, T.A.; Walker, F.R. Evidence that microglia mediate the neurobiological effects of chronic psychological stress on the medial prefrontal cortex. Cereb. Cortex 2012, 22, 1442–1454. [Google Scholar] [CrossRef] [PubMed]
- Perry, V.H.; Holmes, C. Microglial priming in neurodegenerative disease. Nat. Rev. Neurol. 2014, 10, 217–224. [Google Scholar] [CrossRef]
- Giovanoli, S.; Engler, H.; Engler, A.; Richetto, J.; Voget, M.; Willi, R.; Winter, C.; Riva, M.A.; Mortensen, P.B.; Feldon, J.; et al. Stress in puberty unmasks latent neuropathological consequences of prenatal immune activation in mice. Science 2013, 339, 1095–1099. [Google Scholar] [CrossRef]
- van Berckel, B.N.; Bossong, M.G.; Boellaard, R.; Kloet, R.; Schuitemaker, A.; Caspers, E.; Luurtsema, G.; Windhorst, A.D.; Cahn, W.; Lammertsma, A.A.; et al. Microglia activation in recent-onset schizophrenia: A quantitative (R)-[11C]PK11195 positron emission tomography study. Biol. Psychiatry 2008, 64, 820–822. [Google Scholar] [CrossRef]
- Erny, D.; Hrabe de Angelis, A.L.; Jaitin, D.; Wieghofer, P.; Staszewski, O.; David, E.; Keren-Shaul, H.; Mahlakoiv, T.; Jakobshagen, K.; Buch, T.; et al. Host microbiota constantly control maturation and function of microglia in the CNS. Nat. Neurosci. 2015, 18, 965–977. [Google Scholar] [CrossRef]
- Severini, C. Neurotrophic Factors in Health and Disease. Cells 2022, 12, 47. [Google Scholar] [CrossRef]
- Monteggia, L.M.; Barrot, M.; Powell, C.M.; Berton, O.; Galanis, V.; Gemelli, T.; Meuth, S.; Nagy, A.; Greene, R.W.; Nestler, E.J. Essential role of brain-derived neurotrophic factor in adult hippocampal function. Proc. Natl. Acad. Sci. USA 2004, 101, 10827–10832. [Google Scholar] [CrossRef]
- Nieto, R.; Kukuljan, M.; Silva, H. BDNF and schizophrenia: From neurodevelopment to neuronal plasticity, learning, and memory. Front. Psychiatry 2013, 4, 45. [Google Scholar] [CrossRef] [PubMed]
- Green, M.J.; Matheson, S.L.; Shepherd, A.; Weickert, C.S.; Carr, V.J. Brain-derived neurotrophic factor levels in schizophrenia: A systematic review with meta-analysis. Mol. Psychiatry 2011, 16, 960–972. [Google Scholar] [CrossRef] [PubMed]
- Sudo, N.; Chida, Y.; Aiba, Y.; Sonoda, J.; Oyama, N.; Yu, X.N.; Kubo, C.; Koga, Y. Postnatal microbial colonization programs the hypothalamic-pituitary-adrenal system for stress response in mice. J. Physiol. 2004, 558 Pt 1, 263–275. [Google Scholar] [CrossRef] [PubMed]
- Savignac, H.M.; Corona, G.; Mills, H.; Chen, L.; Spencer, J.P.; Tzortzis, G.; Burnet, P.W. Prebiotic feeding elevates central brain derived neurotrophic factor, N-methyl-d-aspartate receptor subunits and d-serine. Neurochem. Int. 2013, 63, 756–764. [Google Scholar] [CrossRef]
- Grice, E.A.; Segre, J.A. The human microbiome: Our second genome. Annu. Rev. Genom. Hum. Genet. 2012, 13, 151–170. [Google Scholar] [CrossRef]
- Matthewman, C.; Narin, A.; Huston, H.; Hopkins, C.E. Systems to model the personalized aspects of microbiome health and gut dysbiosis. Mol. Asp. Med. 2023, 91, 101115. [Google Scholar] [CrossRef]
- Dethlefsen, L.; McFall-Ngai, M.; Relman, D.A. An ecological and evolutionary perspective on human–microbe mutualism and disease. Nature 2007, 449, 811–818. [Google Scholar] [CrossRef]
- El Aidy, S.; Derrien, M.; Aardema, R.; Hooiveld, G.; Richards, S.E.; Dane, A.; Dekker, J.; Vreeken, R.; Levenez, F.; Doré, J.; et al. Transient inflammatory-like state and microbial dysbiosis are pivotal in establishment of mucosal homeostasis during colonisation of germ-free mice. Benef. Microbes 2014, 5, 67–77. [Google Scholar] [CrossRef]
- Qin, J.; Li, R.; Raes, J.; Arumugam, M.; Burgdorf, K.S.; Manichanh, C.; Nielsen, T.; Pons, N.; Levenez, F.; Yamada, T.; et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature 2010, 464, 59–65. [Google Scholar] [CrossRef]
- Lankelma, J.M.; Nieuwdorp, M.; de Vos, W.M.; Wiersinga, W.J. The gut microbiota in internal medicine: Implications for health and disease. Neth. J. Med. 2015, 73, 61–68. [Google Scholar]
- Thursby, E.; Juge, N. Introduction to the human gut microbiota. Biochem. J. 2017, 474, 1823–1836. [Google Scholar] [CrossRef] [PubMed]
- Hou, K.; Wu, Z.-X.; Chen, X.-Y.; Wang, J.-Q.; Zhang, D.; Xiao, C.; Zhu, D.; Koya, J.B.; Wei, L.; Li, J.; et al. Microbiota in health and diseases. Signal Transduct. Target. Ther. 2022, 7, 135. [Google Scholar] [CrossRef] [PubMed]
- Kelly, C.J.; Zheng, L.; Campbell, E.L.; Saeedi, B.; Scholz, C.C.; Bayless, A.J.; Wilson, K.E.; Glover, L.E.; Kominsky, D.J.; Magnuson, A.; et al. Crosstalk between Microbiota-Derived Short-Chain Fatty Acids and Intestinal Epithelial HIF Augments Tissue Barrier Function. Cell Host Microbe 2015, 17, 662–671. [Google Scholar] [CrossRef] [PubMed]
- Pluznick, J.L. Gut microbes and host physiology: What happens when you host billions of guests? Front. Endocrinol. 2014, 5, 91. [Google Scholar] [CrossRef]
- Dominguez-Bello, M.G.; Costello, E.K.; Contreras, M.; Magris, M.; Hidalgo, G.; Fierer, N.; Knight, R. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc. Natl. Acad. Sci. USA 2010, 107, 11971–11975. [Google Scholar] [CrossRef]
- Arentsen, T.; Qian, Y.; Gkotzis, S.; Femenia, T.; Wang, T.; Udekwu, K.; Forssberg, H.; Diaz Heijtz, R. The bacterial peptidoglycan-sensing molecule Pglyrp2 modulates brain development and behavior. Mol. Psychiatry 2017, 22, 257–266. [Google Scholar] [CrossRef]
- Faa, G.; Gerosa, C.; Fanni, D.; Nemolato, S.; van Eyken, P.; Fanos, V. Factors influencing the development of a personal tailored microbiota in the neonate, with particular emphasis on antibiotic therapy. J. Matern. Fetal Neonatal Med. 2013, 26 (Suppl. S2), 35–43. [Google Scholar] [CrossRef]
- Dinan, T.G.; Cryan, J.F. The impact of gut microbiota on brain and behaviour: Implications for psychiatry. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 552–558. [Google Scholar] [CrossRef]
- Wang, Y.; Ma, W.; Mehta, R.; Nguyen, L.H.; Song, M.; Drew, D.A.; Asnicar, F.; Huttenhower, C.; Segata, N.; Wolf, J.; et al. Diet and gut microbial associations in irritable bowel syndrome according to disease subtype. Gut Microbes 2023, 15, 2262130. [Google Scholar] [CrossRef]
- David, L.A.; Maurice, C.F.; Carmody, R.N.; Gootenberg, D.B.; Button, J.E.; Wolfe, B.E.; Ling, A.V.; Devlin, A.S.; Varma, Y.; Fischbach, M.A. Diet rapidly and reproducibly alters the human gut microbiome. Nature 2014, 505, 559–563. [Google Scholar] [CrossRef]
- Nagengast, F.; Grubben, M.; Van Munster, I. Role of bile acids in colorectal carcinogenesis. Eur. J. Cancer 1995, 31, 1067–1070. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Wan, J.; Choe, U.; Pham, Q.; Schoene, N.W.; He, Q.; Li, B.; Yu, L.; Wang, T.T.Y. Interactions Between Food and Gut Microbiota: Impact on Human Health. Annu. Rev. Food Sci. Technol. 2019, 10, 389–408. [Google Scholar] [CrossRef] [PubMed]
- Shao, X.; Liu, L.; Zhou, Y.; Zhong, K.; Gu, J.; Hu, T.; Yao, Y.; Zhou, C.; Chen, W. High-fat diet promotes colitis-associated tumorigenesis by altering gut microbial butyrate metabolism. Int. J. Biol. Sci. 2023, 19, 5004–5019. [Google Scholar] [CrossRef] [PubMed]
- Harrison, C.A.; Taren, D. How poverty affects diet to shape the microbiota and chronic disease. Nat. Rev. Immunol. 2018, 18, 279–287. [Google Scholar] [CrossRef]
- Ge, X.; Ding, C.; Zhao, W.; Xu, L.; Tian, H.; Gong, J.; Zhu, M.; Li, J.; Li, N. Antibiotics-induced depletion of mice microbiota induces changes in host serotonin biosynthesis and intestinal motility. J. Transl. Med. 2017, 15, 13. [Google Scholar] [CrossRef]
- Brown, G.C. The endotoxin hypothesis of neurodegeneration. J. Neuroinflammation 2019, 16, 180. [Google Scholar] [CrossRef]
- Schirmer, M.; Smeekens, S.P.; Vlamakis, H.; Jaeger, M.; Oosting, M.; Franzosa, E.A.; Ter Horst, R.; Jansen, T.; Jacobs, L.; Bonder, M.J.; et al. Linking the Human Gut Microbiome to Inflammatory Cytokine Production Capacity. Cell 2016, 167, 1125–1136.e1128. [Google Scholar] [CrossRef]
- Cryan, J.F.; O’Mahony, S.M. The microbiome-gut-brain axis: From bowel to behavior. Neurogastroenterol. Motil. 2011, 23, 187–192. [Google Scholar] [CrossRef]
- Zwielehner, J.; Liszt, K.; Handschur, M.; Lassl, C.; Lapin, A.; Haslberger, A.G. Combined PCR-DGGE fingerprinting and quantitative-PCR indicates shifts in fecal population sizes and diversity of Bacteroides, bifidobacteria and Clostridium cluster IV in institutionalized elderly. Exp. Gerontol. 2009, 44, 440–446. [Google Scholar] [CrossRef]
- Fransen, F.; van Beek, A.A.; Borghuis, T.; Aidy, S.E.; Hugenholtz, F.; van der Gaast-de Jongh, C.; Savelkoul, H.F.J.; De Jonge, M.I.; Boekschoten, M.V.; Smidt, H.; et al. Aged Gut Microbiota Contributes to Systemical Inflammaging after Transfer to Germ-Free Mice. Front. Immunol. 2017, 8, 1385. [Google Scholar] [CrossRef]
- Karemaker, J.M. An introduction into autonomic nervous function. Physiol. Meas. 2017, 38, R89–R118. [Google Scholar] [CrossRef] [PubMed]
- Koopman, F.A.; Stoof, S.P.; Straub, R.H.; Van Maanen, M.A.; Vervoordeldonk, M.J.; Tak, P.P. Restoring the balance of the autonomic nervous system as an innovative approach to the treatment of rheumatoid arthritis. Mol. Med. 2011, 17, 937–948. [Google Scholar] [CrossRef] [PubMed]
- Lake, J.I.; Heuckeroth, R.O. Enteric nervous system development: Migration, differentiation, and disease. Am. J. Physiol. Gastrointest. Liver Physiol. 2013, 305, G1–G24. [Google Scholar] [CrossRef] [PubMed]
- Baj, A.; Moro, E.; Bistoletti, M.; Orlandi, V.; Crema, F.; Giaroni, C. Glutamatergic Signaling Along The Microbiota-Gut-Brain Axis. Int. J. Mol. Sci. 2019, 20, 1482. [Google Scholar] [CrossRef] [PubMed]
- George, M.S.; Nahas, Z.; Borckardt, J.J.; Anderson, B.; Burns, C.; Kose, S.; Short, E.B. Vagus nerve stimulation for the treatment of depression and other neuropsychiatric disorders. Expert Rev. Neurother. 2007, 7, 63–74. [Google Scholar] [CrossRef]
- de Weerth, C. Do bacteria shape our development? Crosstalk between intestinal microbiota and HPA axis. Neurosci. Biobehav. Rev. 2017, 83, 458–471. [Google Scholar] [CrossRef]
- Clarke, G.; O’Mahony, S.M.; Dinan, T.G.; Cryan, J.F. Priming for health: Gut microbiota acquired in early life regulates physiology, brain and behaviour. Acta Paediatr. 2014, 103, 812–819. [Google Scholar] [CrossRef]
- Round, J.L.; Mazmanian, S.K. The gut microbiota shapes intestinal immune responses during health and disease. Nat. Rev. Immunol. 2009, 9, 313–323. [Google Scholar] [CrossRef]
- McCusker, R.H.; Kelley, K.W. Immune-neural connections: How the immune system’s response to infectious agents influences behavior. J. Exp. Biol. 2013, 216 Pt 1, 84–98. [Google Scholar] [CrossRef]
- Bsibsi, M.; Ravid, R.; Gveric, D.; van Noort, J.M. Broad expression of Toll-like receptors in the human central nervous system. J. Neuropathol. Exp. Neurol. 2002, 61, 1013–1021. [Google Scholar] [CrossRef]
- Kielian, T. Toll-like receptors in central nervous system glial inflammation and homeostasis. J. Neurosci. Res. 2006, 83, 711–730. [Google Scholar] [CrossRef] [PubMed]
- Takeda, K.; Akira, S. Toll-like receptors in innate immunity. Int. Immunol. 2005, 17, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Lv, F.; Chen, S.; Wang, L.; Jiang, R.; Tian, H.; Li, J.; Yao, Y.; Zhuo, C. The role of microbiota in the pathogenesis of schizophrenia and major depressive disorder and the possibility of targeting microbiota as a treatment option. Oncotarget 2017, 8, 100899–100907. [Google Scholar] [CrossRef]
- Desbonnet, L.; Clarke, G.; Shanahan, F.; Dinan, T.G.; Cryan, J.F. Microbiota is essential for social development in the mouse. Mol. Psychiatry 2014, 19, 146–148. [Google Scholar] [CrossRef] [PubMed]
- Dicks, L.M.T. Gut Bacteria and Neurotransmitters. Microorganisms 2022, 10, 1838. [Google Scholar] [CrossRef] [PubMed]
- van der Hee, B.; Wells, J.M. Microbial Regulation of Host Physiology by Short-chain Fatty Acids. Trends Microbiol. 2021, 29, 700–712. [Google Scholar] [CrossRef]
- Fusco, W.; Lorenzo, M.B.; Cintoni, M.; Porcari, S.; Rinninella, E.; Kaitsas, F.; Lener, E.; Mele, M.C.; Gasbarrini, A.; Collado, M.C.; et al. Short-Chain Fatty-Acid-Producing Bacteria: Key Components of the Human Gut Microbiota. Nutrients 2023, 15, 2211. [Google Scholar] [CrossRef]
- Tan, J.; McKenzie, C.; Potamitis, M.; Thorburn, A.N.; Mackay, C.R.; Macia, L. The role of short-chain fatty acids in health and disease. Adv. Immunol. 2014, 121, 91–119. [Google Scholar] [CrossRef]
- van de Wouw, M.; Boehme, M.; Lyte, J.M.; Wiley, N.; Strain, C.; O’Sullivan, O.; Clarke, G.; Stanton, C.; Dinan, T.G.; Cryan, J.F. Short-chain fatty acids: Microbial metabolites that alleviate stress-induced brain-gut axis alterations. J. Physiol. 2018, 596, 4923–4944. [Google Scholar] [CrossRef]
- Frost, G.; Sleeth, M.L.; Sahuri-Arisoylu, M.; Lizarbe, B.; Cerdan, S.; Brody, L.; Anastasovska, J.; Ghourab, S.; Hankir, M.; Zhang, S.; et al. The short-chain fatty acid acetate reduces appetite via a central homeostatic mechanism. Nat. Commun. 2014, 5, 3611. [Google Scholar] [CrossRef]
- Saresella, M.; Marventano, I.; Barone, M.; La Rosa, F.; Piancone, F.; Mendozzi, L.; d’Arma, A.; Rossi, V.; Pugnetti, L.; Roda, G.; et al. Alterations in Circulating Fatty Acid Are Associated With Gut Microbiota Dysbiosis and Inflammation in Multiple Sclerosis. Front. Immunol. 2020, 11, 1390. [Google Scholar] [CrossRef] [PubMed]
- Garcez, M.L.; de Carvalho, C.A.; Mina, F.; Bellettini-Santos, T.; Schiavo, G.L.; da Silva, S.; Campos, A.; Varela, R.B.; Valvassori, S.S.; Damiani, A.P.; et al. Sodium butyrate improves memory and modulates the activity of histone deacetylases in aged rats after the administration of d-galactose. Exp. Gerontol. 2018, 113, 209–217. [Google Scholar] [CrossRef]
- Reigstad, C.S.; Salmonson, C.E.; Rainey, J.F., 3rd; Szurszewski, J.H.; Linden, D.R.; Sonnenburg, J.L.; Farrugia, G.; Kashyap, P.C. Gut microbes promote colonic serotonin production through an effect of short-chain fatty acids on enterochromaffin cells. FASEB J. 2015, 29, 1395–1403. [Google Scholar] [CrossRef] [PubMed]
- Prochazkova, P.; Roubalova, R.; Dvorak, J.; Kreisinger, J.; Hill, M.; Tlaskalova-Hogenova, H.; Tomasova, P.; Pelantova, H.; Cermakova, M.; Kuzma, M.; et al. The intestinal microbiota and metabolites in patients with anorexia nervosa. Gut Microbes 2021, 13, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Li, E.; Sun, Z.; Fu, D.; Duan, G.; Jiang, M.; Yu, Y.; Mei, L.; Yang, P.; Tang, Y.; et al. Altered gut microbiota and short chain fatty acids in Chinese children with autism spectrum disorder. Sci. Rep. 2019, 9, 287. [Google Scholar] [CrossRef]
- Strandwitz, P. Neurotransmitter modulation by the gut microbiota. Brain Res. 2018, 1693 Pt B, 128–133. [Google Scholar] [CrossRef]
- Agus, A.; Planchais, J.; Sokol, H. Gut Microbiota Regulation of Tryptophan Metabolism in Health and Disease. Cell Host Microbe 2018, 23, 716–724. [Google Scholar] [CrossRef]
- Rothhammer, V.; Mascanfroni, I.D.; Bunse, L.; Takenaka, M.C.; Kenison, J.E.; Mayo, L.; Chao, C.-C.; Patel, B.; Yan, R.; Blain, M.; et al. Type I interferons and microbial metabolites of tryptophan modulate astrocyte activity and central nervous system inflammation via the aryl hydrocarbon receptor. Nat. Med. 2016, 22, 586–597. [Google Scholar] [CrossRef]
- Li, Z.; Qing, Y.; Cui, G.; Li, M.; Liu, T.; Zeng, Y.; Zhou, C.; Hu, X.; Jiang, J.; Wang, D.; et al. Shotgun metagenomics reveals abnormal short-chain fatty acid-producing bacteria and glucose and lipid metabolism of the gut microbiota in patients with schizophrenia. Schizophr. Res. 2023, 255, 59–66. [Google Scholar] [CrossRef]
- Zhu, F.; Ju, Y.; Wang, W.; Wang, Q.; Guo, R.; Ma, Q.; Sun, Q.; Fan, Y.; Xie, Y.; Yang, Z.; et al. Metagenome-wide association of gut microbiome features for schizophrenia. Nat. Commun. 2020, 11, 1612. [Google Scholar] [CrossRef]
- Ling, Z.; Jin, G.; Yan, X.; Cheng, Y.; Shao, L.; Song, Q.; Liu, X.; Zhao, L. Fecal Dysbiosis and Immune Dysfunction in Chinese Elderly Patients With Schizophrenia: An Observational Study. Front. Cell Infect. Microbiol. 2022, 12, 886872. [Google Scholar] [CrossRef] [PubMed]
- Coyle, J.T. NMDA receptor and schizophrenia: A brief history. Schizophr. Bull. 2012, 38, 920–926. [Google Scholar] [CrossRef] [PubMed]
- Zheng, P.; Zeng, B.; Liu, M.; Chen, J.; Pan, J.; Han, Y.; Liu, Y.; Cheng, K.; Zhou, C.; Wang, H.; et al. The gut microbiome from patients with schizophrenia modulates the glutamate-glutamine-GABA cycle and schizophrenia-relevant behaviors in mice. Sci. Adv. 2019, 5, eaau8317. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.H.; Lane, H.Y. Early Identification and Intervention of Schizophrenia: Insight From Hypotheses of Glutamate Dysfunction and Oxidative Stress. Front. Psychiatry 2019, 10, 93. [Google Scholar] [CrossRef]
- Sharma, S.; Taliyan, R.; Singh, S. Beneficial effects of sodium butyrate in 6-OHDA induced neurotoxicity and behavioral abnormalities: Modulation of histone deacetylase activity. Behav. Brain Res. 2015, 291, 306–314. [Google Scholar] [CrossRef]
- St Laurent, R.; O’Brien, L.M.; Ahmad, S.T. Sodium butyrate improves locomotor impairment and early mortality in a rotenone-induced Drosophila model of Parkinson’s disease. Neuroscience 2013, 246, 382–390. [Google Scholar] [CrossRef]
- Deng, H.; He, L.; Wang, C.; Zhang, T.; Guo, H.; Zhang, H.; Song, Y.; Chen, B. Altered gut microbiota and its metabolites correlate with plasma cytokines in schizophrenia inpatients with aggression. BMC Psychiatry 2022, 22, 629. [Google Scholar] [CrossRef]
- Li, X.; Fan, X.; Yuan, X.; Pang, L.; Hu, S.; Wang, Y.; Huang, X.; Song, X. The Role of Butyric Acid in Treatment Response in Drug-Naïve First Episode Schizophrenia. Front. Psychiatry 2021, 12, 724664. [Google Scholar] [CrossRef]
- Atmaca, M. Valproate and neuroprotective effects for bipolar disorder. Int. Rev. Psychiatry 2009, 21, 410–413. [Google Scholar] [CrossRef]
- Kowalski, K.; Szponar, B.; Bochen, P.; Zebrowska-Rozanska, P.; Laczmanski, L.; Samochowiec, J.; Misiak, B. Altered levels of fecal short-chain fatty acids are associated with subclinical inflammation and worse cognitive performance in patients with schizophrenia. J. Psychiatr. Res. 2023, 165, 298–304. [Google Scholar] [CrossRef]
- Li, X.; Yuan, X.; Pang, L.; Zhang, S.; Li, Y.; Huang, X.; Fan, X.; Song, X. The effect of serum lipids and short-chain fatty acids on cognitive functioning in drug-naïve, first episode schizophrenia patients. Psychiatry Res. 2022, 313, 114582. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).