Association between Selenium Intake and Optimal Sleep Duration: A National Longitudinal Study
Abstract
1. Introduction
2. Methods
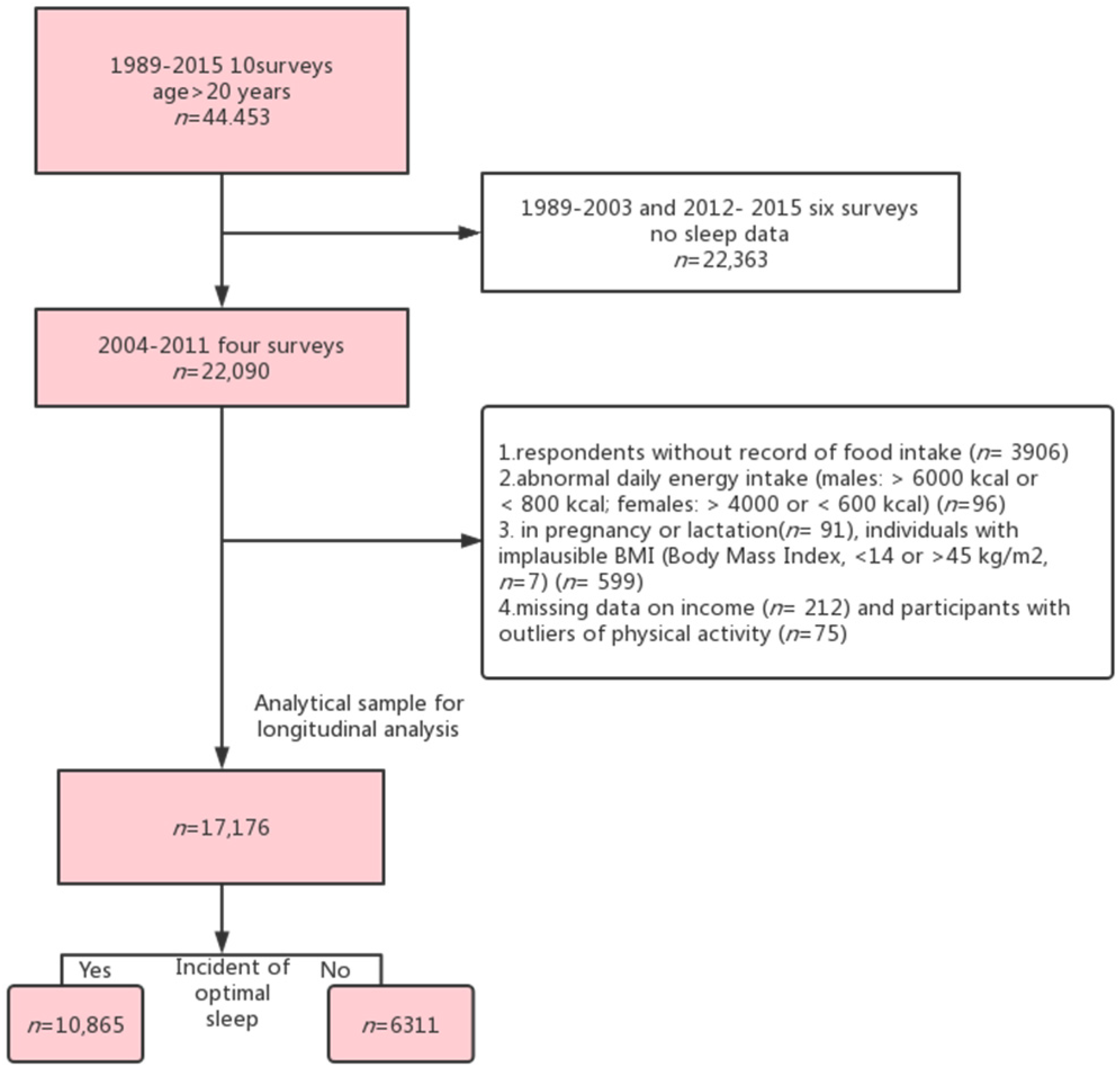
2.1. Study Design and Study Sample
2.2. Outcome Variable: Optimal Sleep Duration
2.3. Exposure Variable: Se Intake
2.4. Covariates
2.5. Statistical Analyses
3. Results
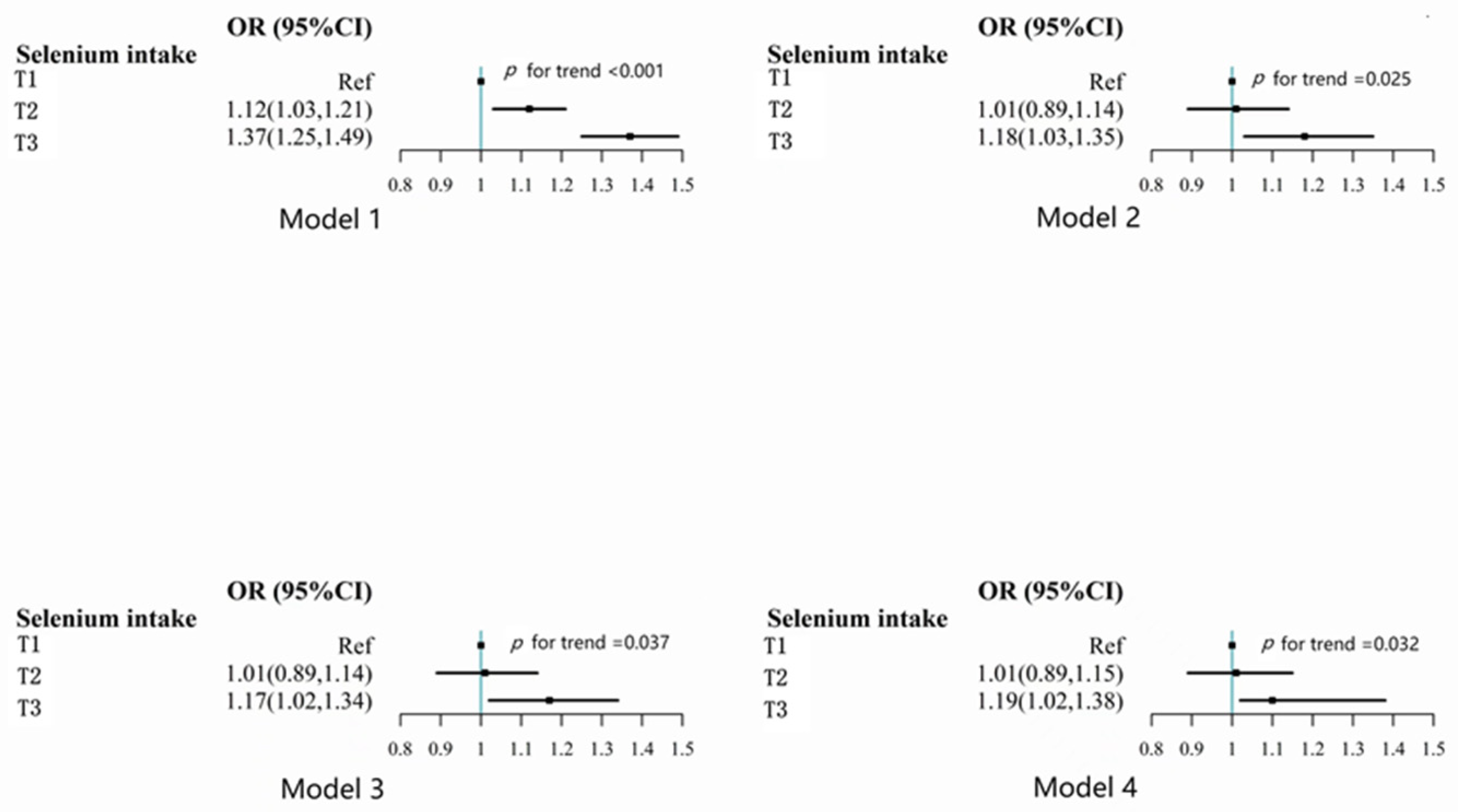
3.1. Association between Se Intake and Self-Reported Optimal Sleep Duration
3.2. Subgroup Analyses of Selenium Consumption with the Optimal Sleep in China Nutrition and Health Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hillman, D.R.; Lack, L.C. Public health implications of sleep loss: The community burden. Med. J. Aust. 2013, 199, S7–S10. [Google Scholar] [CrossRef] [PubMed]
- St-Onge, M.P.; Grandner, M.A.; Brown, D.; Conroy, M.B.; Jean-Louis, G.; Coons, M.; Bhatt, D.L.; On behalf of the American Heart Association Obesity, Behavior Change, Diabetes, and Nutrition Committees of the Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular Disease in the Young; Council on Clinical Cardiology; et al. Sleep Duration and Quality: Impact on Lifestyle Behaviors and Cardiometabolic Health: A Scientific Statement From the American Heart Association. Circulation 2016, 134, e367–e386. [Google Scholar] [CrossRef]
- Wei, L.; Ying, X.; Zhai, M.; Li, J.; Liu, D.; Liu, X.; Yu, B.; Yan, H. The association between peritraumatic distress, perceived stress, depression in pregnancy, and NR3C1 DNA methylation among Chinese pregnant women who experienced COVID-19 lockdown. Front. Immunol. 2022, 13, 966522. [Google Scholar] [CrossRef] [PubMed]
- Klinzing, J.G.; Niethard, N.; Born, J. Mechanisms of systems memory consolidation during sleep. Nat. Neurosci. 2019, 22, 1598–1610. [Google Scholar] [CrossRef] [PubMed]
- Khubchandani, J.; Price, J.H. Short Sleep Duration in Working American Adults, 2010–2018. J Community Health 2020, 45, 219–227. [Google Scholar] [CrossRef]
- Sawyer, E.; Heussler, H.; Gunnarsson, R. Defining short and long sleep duration for future paediatric research: A systematic literature review. J. Sleep Res. 2019, 28, e12839. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Yu, K.; Yang, L.; Wang, H.; Xiao, Y.; Qiu, G.; Liu, X.; Yuan, Y.; Bai, Y.; Li, X.; et al. Sleep duration, midday napping, and sleep quality and incident stroke: The Dongfeng-Tongji cohort. Neurology 2020, 94, e345–e356. [Google Scholar] [CrossRef]
- Yang, L.; Yang, H.; He, M.; Pan, A.; Li, X.; Min, X.; Zhang, C.; Xu, C.; Zhu, X.; Yuan, J.; et al. Longer Sleep Duration and Midday Napping Are Associated with a Higher Risk of CHD Incidence in Middle-Aged and Older Chinese: The Dongfeng-Tongji Cohort Study. Sleep 2016, 39, 645–652. [Google Scholar] [CrossRef]
- Barchielli, G.; Capperucci, A.; Tanini, D. The Role of Selenium in Pathologies: An Updated Review. Antioxidants 2022, 11, 251. [Google Scholar] [CrossRef]
- Hatfield, D.L.; Tsuji, P.A.; Carlson, B.A.; Gladyshev, V.N. Selenium and selenocysteine: Roles in cancer, health, and development. Trends Biochem. Sci. 2014, 39, 112–120. [Google Scholar] [CrossRef]
- Forceville, X. Seleno-enzymes and seleno-compounds: The two faces of selenium. Crit. Care 2006, 10, 180. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jones, G.D.; Droz, B.; Greve, P.; Gottschalk, P.; Poffet, D.; McGrath, S.P.; Seneviratne, S.I.; Smith, P.; Winkel, L.H. Selenium deficiency risk predicted to increase under future climate change. Proc. Natl. Acad. Sci. USA 2017, 114, 2848–2853. [Google Scholar] [CrossRef] [PubMed]
- Dinh, Q.T.; Cui, Z.; Huang, J.; Tran, T.A.T.; Wang, D.; Yang, W.; Zhou, F.; Wang, M.; Yu, D.; Liang, D. Selenium distribution in the Chinese environment and its relationship with human health: A review. Environ. Int. 2018, 112, 294–309. [Google Scholar] [CrossRef]
- Pau, M.C.; Mangoni, A.A.; Zinellu, E.; Pintus, G.; Carru, C.; Fois, A.G.; Pirina, P.; Zinellu, A. Circulating Superoxide Dismutase Concentrations in Obstructive Sleep Apnoea (OSA): A Systematic Review and Meta-Analysis. Antioxidants 2021, 10, 1764. [Google Scholar] [CrossRef] [PubMed]
- Stanek, A.; Brożyna-Tkaczyk, K.; Myśliński, W. Oxidative Stress Markers among Obstructive Sleep Apnea Patients. Oxidative Med. Cell. Longev. 2021, 2021, 9681595. [Google Scholar] [CrossRef]
- Grandner, M.A.; Jackson, N.; Gerstner, J.R.; Knutson, K.L. Dietary nutrients associated with short and long sleep duration. Data from a nationally representative sample. Appetite 2013, 64, 71–80. [Google Scholar] [CrossRef]
- Saruhan, E.; Sertoglu, E.; Unal, Y.; Bek, S.; Kutlu, G. The role of antioxidant vitamins and selenium in patients with obstructive sleep apnea. Sleep Breath 2021, 25, 923–930. [Google Scholar] [CrossRef]
- Albuquerque, R.G.; Tufik, S.; Andersen, M.L. Benefits of selenium in the treatment of depression and sleep disorders: Commentaries of the article “The selenium-containing compound 3-((4-chlorophenyl)selanyl)-1-methyl-1H-indole reverses depressive-like behavior induced by acute restraint stress in mice: Modulation of oxido-nitrosative stress and inflammatory pathway”. Sleep Breath 2019, 23, 933–934. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, C.; Luo, J.; Dibaba, D.T.; Fly, A.D.; Haas, D.M.; Shikany, J.M.; Kahe, K. Long-chain omega-3 fatty acids, selenium, and mercury in relation to sleep duration and sleep quality: Findings from the CARDIA study. Eur. J. Nutr. 2021, 61, 753–762. [Google Scholar] [CrossRef]
- Lee, B.; Hirst, J.J.; Walker, D.W. Prostaglandin D synthase in the prenatal ovine brain and effects of its inhibition with selenium chloride on fetal sleep/wake activity in utero. J. Neurosci. Off. J. Soc. Neurosci. 2002, 22, 5679–5686. [Google Scholar] [CrossRef]
- D’Amato, R.; Regni, L.; Falcinelli, B.; Mattioli, S.; Benincasa, P.; Dal Bosco, A.; Pacheco, P.; Proietti, P.; Troni, E.; Santi, C.; et al. Current Knowledge on Selenium Biofortification to Improve the Nutraceutical Profile of Food: A Comprehensive Review. J. Agric. Food Chem. 2020, 68, 4075–4097. [Google Scholar] [CrossRef] [PubMed]
- Kipp, A.P.; Strohm, D.; Brigelius-Flohé, R.; Schomburg, L.; Bechthold, A.; Leschik-Bonnet, E.; Heseker, H. Revised reference values for selenium intake. J. Trace Elem. Med. Biol. Organ Soc. Miner. Trace Elem. (GMS) 2015, 32, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.; Liu, Q.; Li, Y.; Zhao, F.; Chang, H.; Lyu, J. Longitudinal study of the relationship between sleep duration and hypertension in Chinese adult residents (CHNS 2004-2011). Sleep Med. 2019, 58, 88–92. [Google Scholar] [CrossRef] [PubMed]
- Watson, N.F.; Badr, M.S.; Belenky, G.; Bliwise, D.L.; Buxton, O.M.; Buysse, D.; Dinges, D.F.; Gangwisch, J.; Grandner, M.A.; Kushida, C.; et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep 2015, 38, 843–844. [Google Scholar] [CrossRef]
- Zhang, Y.; Ye, M.; Zhao, Y.; Xiong, Y.; Shen, S.; Yu, Q.; Lu, Y.; Shi, Z.; Lei, X. Higher Dietary Se Intake Is Associated With the Risk of New-Onset Fracture: A National Longitudinal Study for 20 Years. Front. Nutr. 2021, 8, 719147. [Google Scholar] [CrossRef]
- Zhou, B. [Predictive values of body mass index and waist circumference to risk factors of related diseases in Chinese adult population]. Zhonghua Liu Xing Bing Xue Za Zhi 2002, 23, 5–10. [Google Scholar]
- Xie, C.; Xian, J.; Zeng, M.; Cai, Z.; Li, S.; Zhao, Y.; Shi, Z. Regional Difference in the Association between the Trajectory of Selenium Intake and Hypertension: A 20-Year Cohort Study. Nutrients 2021, 13, 1501. [Google Scholar] [CrossRef]
- Singer, J.D.; Willet, J.B. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence; Oxford University Press: New York, NY, USA, 2003. [Google Scholar]
- Wu, C.C.; Wang, C.K.; Yang, A.M.; Lu, C.S.; Lin, C.Y. Selenium status is independently related to bone mineral density, FRAX score, and bone fracture history: NHANES, 2013 to 2014. Bone 2021, 143, 115631. [Google Scholar] [CrossRef]
- Chen, P.C.; Guo, C.H.; Tseng, C.J.; Wang, K.C.; Liu, P.J. Blood trace minerals concentrations and oxidative stress in patients with obstructive sleep apnea. J. Nutr. Health Aging 2013, 17, 639–644. [Google Scholar] [CrossRef]
- Matsumura, H.; Takahata, R.; Hayaishi, O. Inhibition of sleep in rats by inorganic selenium compounds, inhibitors of prostaglandin D synthase. Proc. Natl. Acad. Sci. USA 1991, 88, 9046–9050. [Google Scholar] [CrossRef]
- Razaghi, A.; Poorebrahim, M.; Sarhan, D.; Björnstedt, M. Selenium stimulates the antitumour immunity: Insights to future research. Eur. J. Cancer 2021, 155, 256–267. [Google Scholar] [CrossRef] [PubMed]
- Alzoubi, K.H.; Khabour, O.F.; Albawaana, A.S.; Alhashimi, F.H.; Athamneh, R.Y. Tempol prevents chronic sleep-deprivation induced memory impairment. Brain Res. Bull. 2016, 120, 144–150. [Google Scholar] [CrossRef]
- Kanagasabai, T.; Riddell, M.C.; Ardern, C.I. Inflammation, Oxidative Stress, and Antioxidant Micronutrients as Mediators of the Relationship Between Sleep, Insulin Sensitivity, and Glycosylated Hemoglobin. Front. Public Health 2022, 10, 888331. [Google Scholar] [CrossRef] [PubMed]
- Albuquerque, R.G.; Hirotsu, C.; Tufik, S.; Andersen, M.L. Why Should We Care About Selenium in Obstructive Sleep Apnea? J. Clin. Sleep Med. JCSM Off. Publ. Am. Acad. Sleep Med. 2017, 13, 931–932. [Google Scholar] [CrossRef] [PubMed]
- Winther, K.H.; Rayman, M.P.; Bonnema, S.J.; Hegedüs, L. Selenium in thyroid disorders—Essential knowledge for clinicians. Nat. Rev. Endocrinol. 2020, 16, 165–176. [Google Scholar] [CrossRef]
- Doherty, R.; Madigan, S.; Warrington, G.; Ellis, J. Sleep and Nutrition Interactions: Implications for Athletes. Nutrients 2019, 11, 822. [Google Scholar] [CrossRef]
- Nieman, D.C.; Mitmesser, S.H. Potential Impact of Nutrition on Immune System Recovery from Heavy Exertion: A Metabolomics Perspective. Nutrients 2017, 9, 513. [Google Scholar] [CrossRef]
- Santos, R.V.; Tufik, S.; De Mello, M.T. Exercise, sleep and cytokines: Is there a relation? Sleep Med. Rev. 2007, 11, 231–239. [Google Scholar] [CrossRef]
- Coussens, L.M.; Werb, Z. Inflammation and cancer. Nature 2002, 420, 860–867. [Google Scholar] [CrossRef]
- Arulselvan, P.; Fard, M.T.; Tan, W.S.; Gothai, S.; Fakurazi, S.; Norhaizan, M.E.; Kumar, S.S. Role of Antioxidants and Natural Products in Inflammation. Oxidative Med. Cell. Longev. 2016, 2016, 5276130. [Google Scholar] [CrossRef]
- Jiang, Y.; Wang, M.H. Different solvent fractions of Acanthopanax senticosus harms exert antioxidant and anti-inflammatory activities and inhibit the human Kv1.3 channel. J. Med. Food 2015, 18, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Taheri, S.; Lin, L.; Austin, D.; Young, T.; Mignot, E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004, 1, e62. [Google Scholar] [CrossRef] [PubMed]
- Dashti, H.S.; Ordovás, J.M. Genetics of Sleep and Insights into Its Relationship with Obesity. Annu. Rev. Nutr. 2021, 41, 223–252. [Google Scholar] [CrossRef] [PubMed]
- Zhong, Q.; Lin, R.; Nong, Q. Adiposity and Serum Selenium in U.S. Adults. Nutrients 2018, 10, 727. [Google Scholar] [CrossRef] [PubMed]
- Schomburg, L. Selenium Deficiency Due to Diet, Pregnancy, Severe Illness, or COVID-19-A Preventable Trigger for Autoimmune Disease. Int. J. Mol. Sci. 2021, 22, 8532. [Google Scholar] [CrossRef]
| Factors | T1 | T2 | T3 | p-Value |
|---|---|---|---|---|
| n = 6380 | n = 5009 | n = 5787 | ||
| Se intake (µg/day), mean (SD) | 23.9 (6.1) | 39.2 (3.8) | 68.0 (44.8) | <0.001 |
| Energy intake (kcal/day), mean (SD) | 1716.3 (536.3) | 2072.4 (566.5) | 2464.7 (669.6) | <0.001 |
| Fat intake (g/day), mean (SD) | 55.3 (30.8) | 71.0 (32.5) | 87.3 (40.4) | <0.001 |
| Protein intake (g/day), mean (SD) | 48.9 (14.5) | 65.3 (16.2) | 86.3 (26.2) | <0.001 |
| Carbohydrate intake (g/day), mean (SD) | 252.6 (100.8) | 288.4 (107.3) | 325.9 (118.5) | <0.001 |
| Age (years), mean (SD) | 48.5 (16.3) | 46.4 (15.0) | 45.3 (14.4) | <0.001 |
| BMI (kg/m2), mean (SD) | 22.9 (3.5) | 23.3 (3.4) | 23.8 (3.4) | <0.001 |
| Gender | <0.001 | |||
| Men | 2482 (38.9%) | 2363 (47.2%) | 3359 (58.0%) | |
| Women | 3898 (61.1%) | 2646 (52.8%) | 2428 (42.0%) | |
| Smoking | <0.001 | |||
| Non-smoker | 4632 (72.8%) | 3434 (68.7%) | 3602 (62.3%) | |
| Ex-smoker | 232 (3.6%) | 168 (3.4%) | 253 (4.4%) | |
| Current smoker | 1503 (23.6%) | 1393 (27.9%) | 1929 (33.4%) | |
| Income | <0.001 | |||
| Low | 3039 (47.6%) | 1720 (34.3%) | 1683 (29.1%) | |
| Medium | 1892 (29.7%) | 1696 (33.9%) | 1916 (33.1%) | |
| High | 1449 (22.7%) | 1593 (31.8%) | 2188 (37.8%) | |
| Urbanization | <0.001 | |||
| Low | 2701 (42.3%) | 1473 (29.4%) | 1497 (25.9%) | |
| Medium | 1797 (28.2%) | 1560 (31.1%) | 1703 (29.4%) | |
| High | 1882 (29.5%) | 1976 (39.4%) | 2587 (44.7%) | |
| SURVEY YEAR | <0.001 | |||
| 2004 | 3355 (52.6%) | 2483 (49.6%) | 2750 (47.5%) | |
| 2006 | 725 (11.4%) | 628 (12.5%) | 756 (13.1%) | |
| 2009 | 706 (11.1%) | 645 (12.9%) | 850 (14.7%) | |
| 2011 | 1594 (25.0%) | 1253 (25.0%) | 1431 (24.7%) | |
| Education | <0.001 | |||
| Low | 4876 (76.6%) | 3324 (66.5%) | 3450 (59.7%) | |
| Medium | 698 (11.0%) | 749 (15.0%) | 1032 (17.9%) | |
| High | 792 (12.4%) | 923 (18.5%) | 1297 (22.4%) | |
| Hypertension | 1379 (21.6%) | 987 (19.7%) | 1091 (18.9%) | <0.001 |
| Diabetes | 156 (2.5%) | 132 (2.6%) | 149 (2.6%) | 0.90 |
| Alcohol drinking | 1727 (27.1%) | 1671 (33.4%) | 2452 (42.4%) | <0.001 |
| Region | <0.001 | |||
| South | 3991 (62.6%) | 3040 (60.7%) | 3080 (53.2%) | |
| North | 2389 (37.4%) | 1969 (39.3%) | 2707 (46.8%) | |
| Overweight | 2151 (33.7%) | 1963 (39.2%) | 2550 (44.1%) | <0.001 |
| Physical activity (MET-h/week), mean (SD) | 168.3 (96.6) | 156.4 (91.1) | 153.5 (86.7) | <0.001 |
| Optimal sleep duration | 3860 (60.5%) | 3251 (64.9%) | 3754 (64.9%) | <0.001 |
| T1 | T2 | T3 | p Trend | p for Interaction | |||
|---|---|---|---|---|---|---|---|
| Income | 0.563 | ||||||
| Low | 1.00 | 0.99 | (0.81–1.21) | 1.19 | (0.95–1.48) | 0.129 | |
| Medium | 1.00 | 1.08 | (0.89–1.31) | 1.29 | (1.05–1.59) | 0.015 | |
| High | 1.00 | 1.01 | (0.73–1.40) | 1.16 | (0.83–1.63) | 0.287 | |
| Urbanization | 0.168 | ||||||
| Low | 1.00 | 1.00 | (0.85–1.18) | 1.18 | (0.98–1.42) | 0.097 | |
| Medium | 1.00 | 1.27 | (1.02–1.57) | 1.31 | (1.04–1.65) | 0.023 | |
| High | 1.00 | 0.74 | (0.51–1.07) | 1.04 | (0.71–1.53) | 0.385 | |
| Education | 0.549 | ||||||
| Low | 1.00 | 1.04 | (0.90–1.19) | 1.19 | (1.02–1.38) | 0.021 | |
| Medium | 1.00 | 1.37 | (0.95–1.99) | 1.39 | (0.95–2.02) | 0.107 | |
| High | 1.00 | 0.70 | (0.44–1.10) | 1.27 | (0.78–2.06) | 0.125 | |
| Region | 0.226 | ||||||
| South | 1.00 | 1.07 | (0.92–1.26) | 1.37 | (1.15–1.64) | <0.001 | |
| North | 1.00 | 1.11 | (0.90–1.36) | 1.15 | (0.94–1.42) | 0.226 | |
| Gender | 0.766 | ||||||
| Men | 1.00 | 1.01 | (0.83–1.24) | 1.36 | (1.10–1.67) | 0.001 | |
| Women | 1.00 | 1.13 | (0.96–1.34) | 1.22 | (1.02–1.47) | 0.017 | |
| Overweight | 0.018 | ||||||
| No | 1.00 | 1.07 | (0.92–1.24) | 1.21 | (1.03–1.43) | 0.128 | |
| Yes | 1.00 | 1.14 | (0.91–1.42) | 1.51 | (1.19–1.91) | <0.001 | |
| Hypertension | 0.647 | ||||||
| No | 1.00 | 1.04 | (0.90–1.20) | 1.23 | (1.06–1.43) | 0.005 | |
| Yes | 1.00 | 1.26 | (0.98–1.61) | 1.64 | (1.25–2.15) | <0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, L.; Li, S.; Zhu, Y.; Wang, T.; Su, Y.; Shi, Z.; Zhang, Y.; Zhao, Y. Association between Selenium Intake and Optimal Sleep Duration: A National Longitudinal Study. Nutrients 2023, 15, 397. https://doi.org/10.3390/nu15020397
Zhao L, Li S, Zhu Y, Wang T, Su Y, Shi Z, Zhang Y, Zhao Y. Association between Selenium Intake and Optimal Sleep Duration: A National Longitudinal Study. Nutrients. 2023; 15(2):397. https://doi.org/10.3390/nu15020397
Chicago/Turabian StyleZhao, Lingxi, Shengping Li, Yuzhao Zhu, Tiankun Wang, Yu Su, Zumin Shi, Yangchang Zhang, and Yong Zhao. 2023. "Association between Selenium Intake and Optimal Sleep Duration: A National Longitudinal Study" Nutrients 15, no. 2: 397. https://doi.org/10.3390/nu15020397
APA StyleZhao, L., Li, S., Zhu, Y., Wang, T., Su, Y., Shi, Z., Zhang, Y., & Zhao, Y. (2023). Association between Selenium Intake and Optimal Sleep Duration: A National Longitudinal Study. Nutrients, 15(2), 397. https://doi.org/10.3390/nu15020397







