The Association of Adherence to the Mediterranean Diet with Depression in Older Adults Longitudinally Taking into Account Cognitive Status: Results from the HELIAD Study
Abstract
1. Introduction
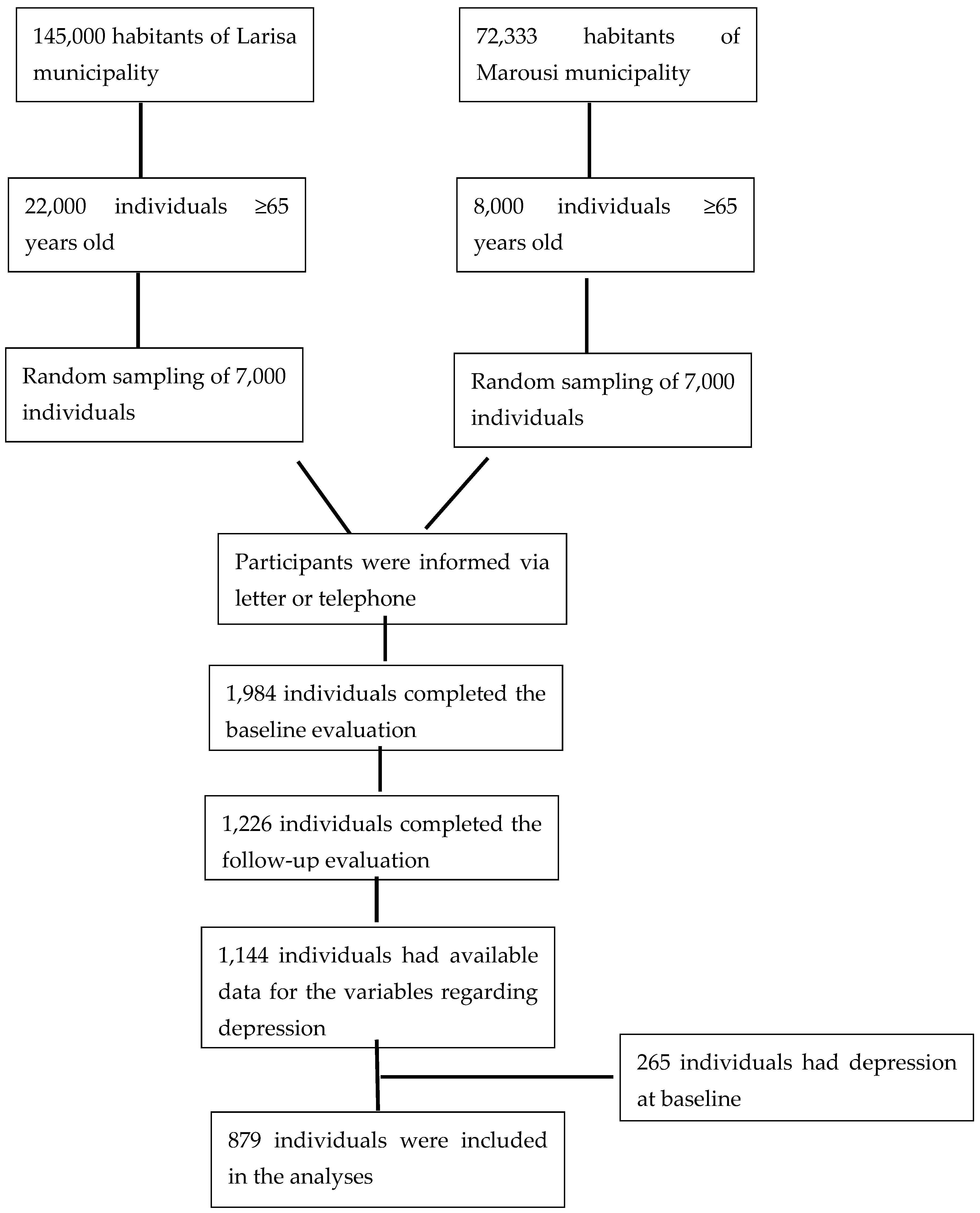
2. Materials and Methods
2.1. Samples and Procedures
2.2. Dietary Assessment
2.3. Assessment of Variables Related to Depression
2.4. Neuropsychological Evaluation and Clinical Diagnosis of Dementia and Mild Cognitive Impairment
2.5. Other Variables
2.6. Statistical Analyses
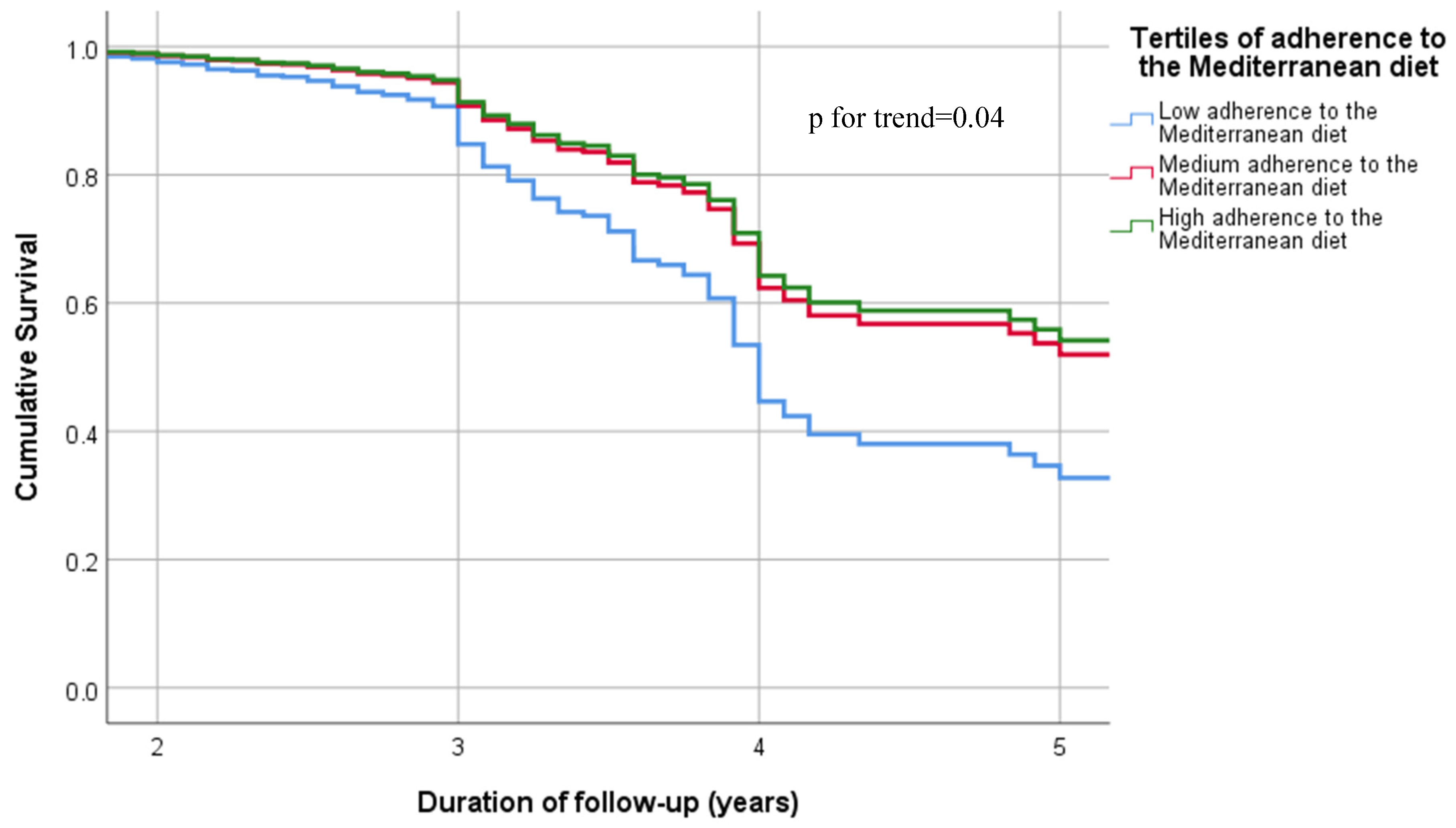
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [CrossRef]
- Blazer, D.G. Depression in late life: Review and commentary. J. Gerontol. A Biol. Sci. Med. Sci. 2003, 58, 249–265. [Google Scholar] [CrossRef] [PubMed]
- Sarris, J.; Thomson, R.; Hargraves, F.; Eaton, M.; de Manincor, M.; Veronese, N.; Solmi, M.; Stubbs, B.; Yung, A.R.; Firth, J. Multiple lifestyle factors and depressed mood: A cross-sectional and longitudinal analysis of the UK Biobank (N = 84,860). BMC Med. 2020, 18, 354. [Google Scholar] [CrossRef]
- Rao, T.S.; Asha, M.R.; Ramesh, B.N.; Rao, K.S. Understanding nutrition, depression and mental illnesses. Indian J. Psychiatry 2008, 50, 77–82. [Google Scholar] [CrossRef]
- Vicinanza, R.; Bersani, F.S.; D’Ottavio, E.; Murphy, M.; Bernardini, S.; Crisciotti, F.; Frizza, A.; Mazza, V.; Biondi, M.; Troisi, G.; et al. Adherence to Mediterranean diet moderates the association between multimorbidity and depressive symptoms in older adults. Arch. Gerontol. Geriatr. 2020, 88, 104022. [Google Scholar] [CrossRef] [PubMed]
- Yin, W.; Löf, M.; Chen, R.; Hultman, C.M.; Fang, F.; Sandin, S. Mediterranean diet and depression: A population-based cohort study. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 153. [Google Scholar] [CrossRef]
- Skarupski, K.A.; Tangney, C.C.; Li, H.; Evans, D.A.; Morris, M.C. Mediterranean diet and depressive symptoms among older adults over time. J. Nutr. Health Aging 2013, 17, 441–445. [Google Scholar] [CrossRef] [PubMed]
- Matison, A.P.; Mather, K.A.; Flood, V.M.; Reppermund, S. Associations between nutrition and the incidence of depression in middle-aged and older adults: A systematic review and meta-analysis of prospective observational population-based studies. Ageing Res. Rev. 2021, 70, 101403. [Google Scholar] [CrossRef]
- Rock, P.L.; Roiser, J.P.; Riedel, W.J.; Blackwell, A.D. Cognitive impairment in depression: A systematic review and meta-analysis. Psychol. Med. 2014, 44, 2029–2040. [Google Scholar] [CrossRef]
- Bhalla, R.K.; Butters, M.A.; Mulsant, B.H.; Begley, A.E.; Zmuda, M.D.; Schoderbek, B.; Pollock, B.G.; Reynolds, C.F., 3rd; Becker, J.T. Persistence of neuropsychologic deficits in the remitted state of late-life depression. Am. J. Geriatr. Psychiatry Off. J. Am. Assoc. Geriatr. Psychiatry 2006, 14, 419–427. [Google Scholar] [CrossRef]
- Ma, L. Depression, Anxiety, and Apathy in Mild Cognitive Impairment: Current Perspectives. Front. Aging Neurosci. 2020, 12, 9. [Google Scholar] [CrossRef] [PubMed]
- Basta, M.; Simos, P.; Vgontzas, A.; Koutentaki, E.; Tziraki, S.; Zaganas, I.; Panagiotakis, S.; Kapetanaki, S.; Fountoulakis, N.; Lionis, C. Associations between sleep duration and cognitive impairment in mild cognitive impairment. J. Sleep Res. 2019, 28, e12864. [Google Scholar] [CrossRef] [PubMed]
- Charisis, S.; Ntanasi, E.; Yannakoulia, M.; Anastasiou, C.A.; Kosmidis, M.H.; Dardiotis, E.; Hadjigeorgiou, G.; Sakka, P.; Scarmeas, N. Mediterranean diet and risk for dementia and cognitive decline in a Mediterranean population. J. Am. Geriatr. Soc. 2021, 69, 1548–1559. [Google Scholar] [CrossRef] [PubMed]
- Scarmeas, N.; Anastasiou, C.A.; Yannakoulia, M. Nutrition and prevention of cognitive impairment. Lancet Neurol. 2018, 17, 1006–1015. [Google Scholar] [CrossRef]
- Bardinet, J.; Chuy, V.; Carriere, I.; Galera, C.; Pouchieu, C.; Samieri, C.; Helmer, C.; Cougnard-Gregoire, A.; Feart, C. Mediterranean Diet Adherence and Risk of Depressive Symptomatology in a French Population-Based Cohort of Older Adults. Nutrients 2022, 14, 4121. [Google Scholar] [CrossRef]
- Anastasiou, C.A.; Yannakoulia, M.; Kosmidis, M.H.; Dardiotis, E.; Hadjigeorgiou, G.M.; Sakka, P.; Arampatzi, X.; Bougea, A.; Labropoulos, I.; Scarmeas, N. Mediterranean diet and cognitive health: Initial results from the Hellenic Longitudinal Investigation of Ageing and Diet. PLoS ONE 2017, 12, e0182048. [Google Scholar] [CrossRef]
- Mamalaki, E.; Anastasiou, C.A.; Ntanasi, E.; Tsapanou, A.; Kosmidis, M.H.; Dardiotis, E.; Hadjigeorgiou, G.M.; Sakka, P.; Scarmeas, N.; Yannakoulia, M. Associations between the mediterranean diet and sleep in older adults: Results from the hellenic longitudinal investigation of aging and diet study. Geriatr. Gerontol. Int. 2018, 18, 1543–1548. [Google Scholar] [CrossRef]
- Ntanasi, E.; Yannakoulia, M.; Kosmidis, M.H.; Anastasiou, C.A.; Dardiotis, E.; Hadjigeorgiou, G.; Sakka, P.; Scarmeas, N. Adherence to Mediterranean Diet and Frailty. J. Am. Med. Dir. Assoc. 2018, 19, 315–322 e312. [Google Scholar] [CrossRef]
- Bountziouka, V.; Bathrellou, E.; Giotopoulou, A.; Katsagoni, C.; Bonou, M.; Vallianou, N.; Barbetseas, J.; Avgerinos, P.C.; Panagiotakos, D.B. Development, repeatability and validity regarding energy and macronutrient intake of a semi-quantitative food frequency questionnaire: Methodological considerations. Nutr. Metab. Cardiovasc. Dis. NMCD 2012, 22, 659–667. [Google Scholar] [CrossRef]
- Panagiotakos, D.B.; Pitsavos, C.; Stefanadis, C. Dietary patterns: A Mediterranean diet score and its relation to clinical and biological markers of cardiovascular disease risk. Nutr. Metab. Cardiovasc. Dis. 2006, 16, 559–568. [Google Scholar] [CrossRef]
- Yesavage, J.A. Geriatric Depression Scale. Psychopharmacol. Bull. 1988, 24, 709–711. [Google Scholar]
- Fountoulakis, K.N.; Tsolaki, M.; Iacovides, A.; Yesavage, J.; O’Hara, R.; Kazis, A.; Ierodiakonou, C. The validation of the short form of the Geriatric Depression Scale (GDS) in Greece. Aging 1999, 11, 367–372. [Google Scholar] [CrossRef] [PubMed]
- Guze, S.B. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM-IV). Am. J. Psychiatry 1995, 152, 1228. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Vlahou, C.H.; Kosmidis, M.H.; Dardagani, A.; Tsotsi, S.; Giannakou, M.; Giazkoulidou, A.; Zervoudakis, E.; Pontikakis, N. Development of the Greek Verbal Learning Test: Reliability, construct validity, and normative standards. Arch. Clin. Neuropsychol. 2013, 28, 52–64. [Google Scholar] [CrossRef]
- Lezak, M.D. Neuropsychological Assessment; Oxford University Press: New York, NY, USA, 2004. [Google Scholar]
- Kosmidis, M.H.; Vlahou, C.H.; Panagiotaki, P.; Kiosseoglou, G. The verbal fluency task in the Greek population: Normative data, and clustering and switching strategies. J. Int. Neuropsychol. Soc. 2004, 10, 164–172. [Google Scholar] [CrossRef]
- Tsapkini, K.; Vlahou, C.H.; Potagas, C. Adaptation and validation of standardized aphasia tests in different languages: Lessons from the Boston Diagnostic Aphasia Examination—Short Form in Greek. Behav. Neurol. 2010, 22, 111–119. [Google Scholar] [CrossRef]
- Vlahou, C.H.; Kosmidis, M.H. The Greek Trail Making Test: Preliminary norms for clinical and research use. Psychol. J. Hell. Psychol. Soc. 2002, 9, 336–352. [Google Scholar]
- Kosmidis, M.H.; Tsotsi, S.; Karambela, O.; Takou, E.; Vlahou, C.H. Cultural factors influencing performance on visuoperceptual neuropsychological tasks. Behav. Neurol. 2010, 23, 245–247. [Google Scholar] [CrossRef]
- Bozikas, V.P.; Giazkoulidou, A.; Hatzigeorgiadou, M.; Karavatos, A.; Kosmidis, M.H. Do age and education contribute to performance on the clock drawing test? Normative data for the Greek population. J. Clin. Exp. Neuropsychol. 2008, 30, 199–203. [Google Scholar] [CrossRef]
- McKhann, G.; Drachman, D.; Folstein, M.; Katzman, R.; Price, D.; Stadlan, E.M. Clinical diagnosis of Alzheimer’s disease: Report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 1984, 34, 939–944. [Google Scholar] [CrossRef] [PubMed]
- Petersen, R.C.; Doody, R.; Kurz, A.; Mohs, R.C.; Morris, J.C.; Rabins, P.V.; Ritchie, K.; Rossor, M.; Thal, L.; Winblad, B. Current concepts in mild cognitive impairment. Arch. Neurol. 2001, 58, 1985–1992. [Google Scholar] [CrossRef]
- Kavouras, S.A.; Maraki, M.I.; Kollia, M.; Gioxari, A.; Jansen, L.T.; Sidossis, L.S. Development, reliability and validity of a physical activity questionnaire for estimating energy expenditure in Greek adults. Sci. Sport. 2016, 31, e47–e53. [Google Scholar] [CrossRef]
- Kessler, R.C.; Birnbaum, H.; Bromet, E.; Hwang, I.; Sampson, N.; Shahly, V. Age differences in major depression: Results from the National Comorbidity Survey Replication (NCS-R). Psychol. Med. 2010, 40, 225–237. [Google Scholar] [CrossRef] [PubMed]
- Hu, T.; Zhao, X.; Wu, M.; Li, Z.; Luo, L.; Yang, C.; Yang, F. Prevalence of depression in older adults: A systematic review and meta-analysis. Psychiatry Res. 2022, 311, 114511. [Google Scholar] [CrossRef]
- Mukku, S.S.R.; Dahale, A.B.; Muniswamy, N.R.; Muliyala, K.P.; Sivakumar, P.T.; Varghese, M. Geriatric Depression and Cognitive Impairment—An Update. Indian J. Psychol. Med. 2021, 43, 286–293. [Google Scholar] [CrossRef]
- Basta, M.; Micheli, K.; Simos, P.; Zaganas, I.; Panagiotakis, S.; Koutra, K.; Krasanaki, C.; Lionis, C.; Vgontzas, A. Frequency and risk factors associated with depression in elderly visiting Primary Health Care (PHC) settings: Findings from the Cretan Aging Cohort. J. Affect. Disord. Rep. 2021, 4, 100109. [Google Scholar] [CrossRef]
- Marx, W.; Lane, M.; Hockey, M.; Aslam, H.; Berk, M.; Walder, K.; Borsini, A.; Firth, J.; Pariante, C.M.; Berding, K.; et al. Diet and depression: Exploring the biological mechanisms of action. Mol. Psychiatry 2021, 26, 134–150. [Google Scholar] [CrossRef]
- Tsigalou, C.; Konstantinidis, T.; Paraschaki, A.; Stavropoulou, E.; Voidarou, C.; Bezirtzoglou, E. Mediterranean Diet as a Tool to Combat Inflammation and Chronic Diseases. An Overview. Biomedicines 2020, 8, 201. [Google Scholar] [CrossRef]
- Taylor, A.M.; Holscher, H.D. A review of dietary and microbial connections to depression, anxiety, and stress. Nutr. Neurosci. 2020, 23, 237–250. [Google Scholar] [CrossRef]
- Gea, A.; Martinez-Gonzalez, M.A.; Toledo, E.; Sanchez-Villegas, A.; Bes-Rastrollo, M.; Nuñez-Cordoba, J.M.; Sayon-Orea, C.; Beunza, J.J. A longitudinal assessment of alcohol intake and incident depression: The SUN project. BMC Public Health 2012, 12, 954. [Google Scholar] [CrossRef] [PubMed]
- Gea, A.; Beunza, J.J.; Estruch, R.; Sanchez-Villegas, A.; Salas-Salvado, J.; Buil-Cosiales, P.; Gomez-Gracia, E.; Covas, M.I.; Corella, D.; Fiol, M.; et al. Alcohol intake, wine consumption and the development of depression: The PREDIMED study. BMC Med. 2013, 11, 192. [Google Scholar] [CrossRef] [PubMed]
- Lundgaard, I.; Wang, W.; Eberhardt, A.; Vinitsky, H.S.; Reeves, B.C.; Peng, S.; Lou, N.; Hussain, R.; Nedergaard, M. Beneficial effects of low alcohol exposure, but adverse effects of high alcohol intake on glymphatic function. Sci. Rep. 2018, 8, 2246. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi, O.; Keshteli, A.H.; Afshar, H.; Esmaillzadeh, A.; Adibi, P. Adherence to Mediterranean dietary pattern is inversely associated with depression, anxiety and psychological distress. Nutr. Neurosci. 2021, 24, 248–259. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Fernández, S.; Gurpegui, M.; Díaz-Atienza, F.; Pérez-Costillas, L.; Gerstenberg, M.; Correll, C.U. Oxidative stress and antioxidant parameters in patients with major depressive disorder compared to healthy controls before and after antidepressant treatment: Results from a meta-analysis. J. Clin. Psychiatry 2015, 76, 1658–1667. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.L. The methylation, neurotransmitter, and antioxidant connections between folate and depression. Altern. Med. Rev. A J. Clin. Ther. 2008, 13, 216–226. [Google Scholar]
- Basta, M.; Belogianni, C.; Yannakoulia, M.; Zaganas, I.; Panagiotakis, S.; Simos, P.; Vgontzas, A.N. Poor Diet, Long Sleep, and Lack of Physical Activity Are Associated with Inflammation among Non-Demented Community-Dwelling Elderly. Healthcare 2022, 10, 143. [Google Scholar] [CrossRef]
| All Participants N = 879 | Participants without Depression at Follow Up N = 709 | Participants with Depression at Follow Up N = 170 | p-Value * | |
|---|---|---|---|---|
| Age (years) | 73.3 ± 5.0 | 73.1 ± 4.9 | 74.0 ± 5.2 | 0.057 |
| Sex (% women) | 55.4 | 54.5 | 68.3 | 0.003 |
| Education (years) | 8.3 ± 5.0 | 8.5 ± 4.9 | 7.2 ± 4.9 | 0.002 |
| Duration of follow-up (years) | 3.0 ± 0.8 | 3.0 ± 0.8 | 3.1 ± 0.8 | 0.211 |
| Diagnosis of MCI at follow-up (%yes) | 17.3 | 14.3 | 21.4 | 0.033 |
| Diagnosis of dementia at follow-up (%yes) | 4.9 | 3.9 | 9.0 | <0.001 |
| Global Cognition Score | −0.1 ± 0.8 | −0.1 ± 0.7 | −0.3 ± 0.8 | 0.006 |
| Living alone (%yes) | 16.2 | 16.3 | 19.5 | 0.321 |
| Smoking status (%yes) | 10.9 | 10.9 | 11.2 | 0.123 |
| Body Mass Index (kg/m2) | 28.8 ± 4.3 | 28.8 ± 4.2 | 28.7 ± 4.5 | 0.777 |
| Number of co-morbidities | 2.0 ± 1.4 | 2.0 ± 1.4 | 2.2 ± 1.4 | 0.221 |
| Physical Activity (/200 MET-min/day) | 65.6 ± 9.1 | 65.5 ± 9.1 | 66.0 ± 9.1 | 0.521 |
| MedDietScore (0–55) | 33.7 ± 4.5 | 34.1 ± 5.0 | 32.3 ± 5.0 | <0.001 |
| Non refined cereals (portions/day) | 1.0 ± 1.4 | 1.0 ± 1.5 | 0.9 ± 1.5 | 0.605 |
| Cereals (portions/day) | 4.7 ± 2.0 | 4.6 ± 2.0 | 4.9 ± 1.8 | 0.149 |
| Fruits (portions/day) | 2.1 ± 1.3 | 2.1 ± 1.3 | 1.8 ± 1.2 | 0.003 |
| Vegetables (portions/day) | 2.0 ± 0.9 | 2.0 ± 0.9 | 1.8 ± 0.8 | 0.002 |
| Legumes (portions/day) | 0.5 ± 0.3 | 0.5 ± 0.3 | 0.4 ± 0.3 | 0.456 |
| Dairy products (portions/day) | 1.7 ± 0.9 | 1.7 ± 0.9 | 1.6 ± 0.8 | 0.081 |
| Fish (portions/day) | 0.6 ± 0.4 | 0.6 ± 0.4 | 0.6 ± 0.4 | 0.522 |
| Red meat (portions/day) | 0.8 ± 0.5 | 0.8 ± 0.5 | 0.8 ± 0.5 | 0.642 |
| Alcoholic drinks (portions/day) | 0.4 ± 0.7 | 0.5 ± 0.8 | 0.2 ± 0.5 | <0.001 |
| Sweets (portions/day) | 0.4 ± 0.5 | 0.4 ± 0.5 | 0.2 ± 0.4 | 0.651 |
| Adherence to the Mediterranean Diet as a Continuous Variable | Adherence to the Mediterranean Diet as Tertiles | |||||
|---|---|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | p for Trend | ||
| Basic Model (N = 879) | 0.947 (0.915–0.981) | 0.002 | 1st (reference) | 0.002 | ||
| 2nd | 0.577 (0.393–0.878) | 0.009 | ||||
| 3rd | 0.535 (0.350–0.816) | 0.004 | ||||
| Model 1 (N = 854) | 0.948 (0.915–0.98) | 0.003 | 1st (reference) | 0.002 | ||
| 2nd | 0.588 (0.393–0.878) | 0.009 | ||||
| 3rd | 0.537 (0.350–0.819) | 0.004 | ||||
| Model 2 (N = 736) | 0.937 (0.903–0.973) | 0.001 | 1st (reference) | 0.003 | ||
| 2nd | 0.590 (0.395–0.885) | 0.009 | ||||
| 3rd | 0.539 (0.359–0.816) | 0.004 | ||||
| Model 3 (N = 736) | 0.938 (0.903–0.974) | 0.001 | 1st (reference) | 0.004 | ||
| 2nd | 0.586 (0.391–0.879) | 0.010 | ||||
| 3rd | 0.549(0.359–0.840) | 0.006 | ||||
| Consumption of Specific Food Groups | HR (95% CI) | p |
|---|---|---|
| Non refined cereals | 0.907 (0.799–1.029) | 0.133 |
| Fruits | 0.848 (0.741–0.972) | 0.018 |
| Vegetables | 0.847 (0.697–1.029) | 0.094 |
| Legumes | 0.972 (0.480–1.966) | 0.937 |
| Fish | 0.774 (0.492–1.217) | 0.267 |
| Red meat | 0.795 (0.548–1.152) | 0.225 |
| Alcoholic drinks | 0.687 (0.472–0.991) | 0.047 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mamalaki, E.; Ntanasi, E.; Hatzimanolis, A.; Basta, M.; Kosmidis, M.H.; Dardiotis, E.; Hadjigeorgiou, G.M.; Sakka, P.; Scarmeas, N.; Yannakoulia, M. The Association of Adherence to the Mediterranean Diet with Depression in Older Adults Longitudinally Taking into Account Cognitive Status: Results from the HELIAD Study. Nutrients 2023, 15, 359. https://doi.org/10.3390/nu15020359
Mamalaki E, Ntanasi E, Hatzimanolis A, Basta M, Kosmidis MH, Dardiotis E, Hadjigeorgiou GM, Sakka P, Scarmeas N, Yannakoulia M. The Association of Adherence to the Mediterranean Diet with Depression in Older Adults Longitudinally Taking into Account Cognitive Status: Results from the HELIAD Study. Nutrients. 2023; 15(2):359. https://doi.org/10.3390/nu15020359
Chicago/Turabian StyleMamalaki, Eirini, Eva Ntanasi, Alexandros Hatzimanolis, Maria Basta, Mary H. Kosmidis, Efthimios Dardiotis, Giorgos M. Hadjigeorgiou, Paraskevi Sakka, Nikolaos Scarmeas, and Mary Yannakoulia. 2023. "The Association of Adherence to the Mediterranean Diet with Depression in Older Adults Longitudinally Taking into Account Cognitive Status: Results from the HELIAD Study" Nutrients 15, no. 2: 359. https://doi.org/10.3390/nu15020359
APA StyleMamalaki, E., Ntanasi, E., Hatzimanolis, A., Basta, M., Kosmidis, M. H., Dardiotis, E., Hadjigeorgiou, G. M., Sakka, P., Scarmeas, N., & Yannakoulia, M. (2023). The Association of Adherence to the Mediterranean Diet with Depression in Older Adults Longitudinally Taking into Account Cognitive Status: Results from the HELIAD Study. Nutrients, 15(2), 359. https://doi.org/10.3390/nu15020359








