Malnutrition with Low Muscle Mass Is Common after Weaning off Home Parenteral Nutrition for Chronic Intestinal Failure
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Definitions
2.3. Data Collection
2.4. Statistical Analysis
3. Results
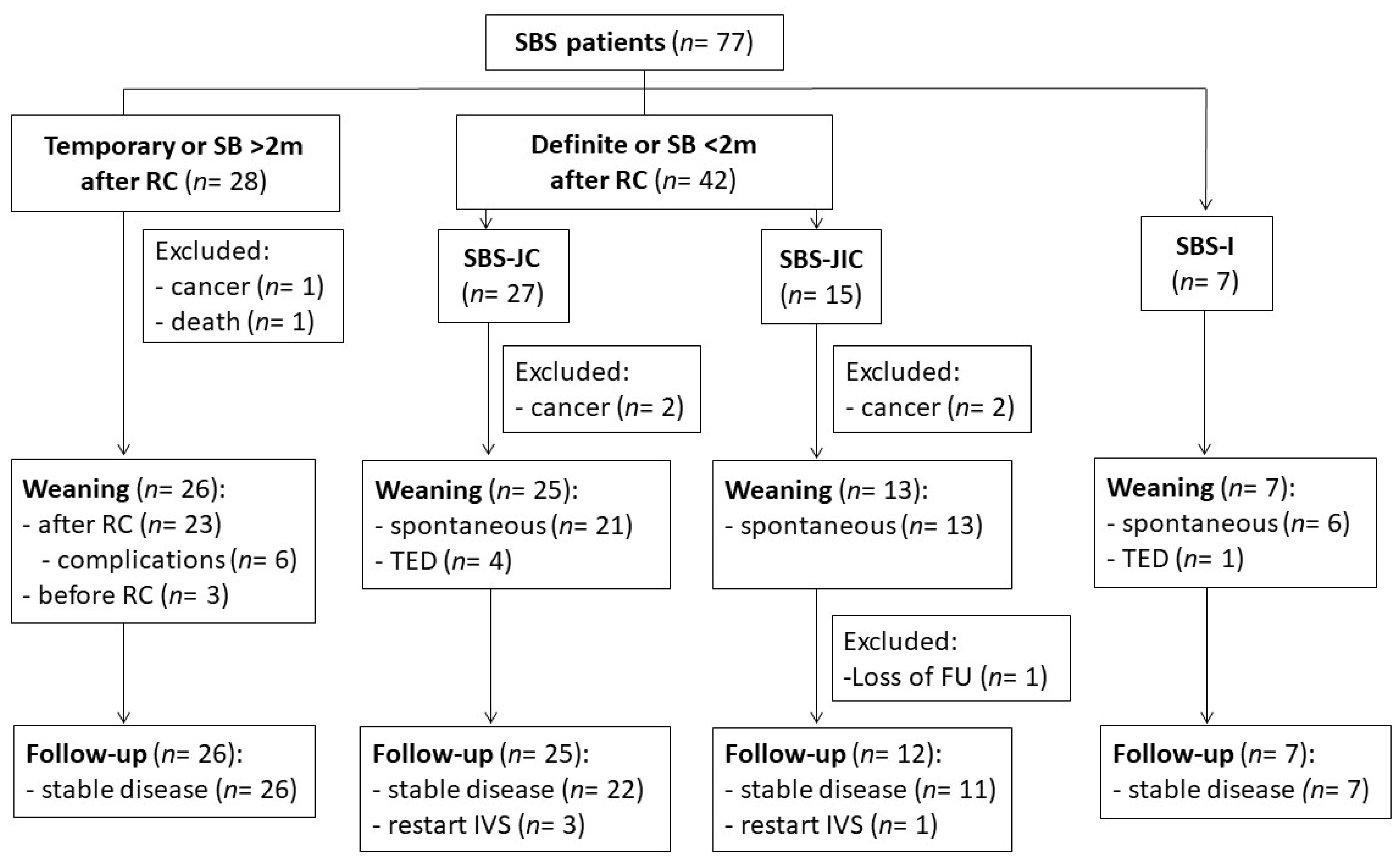
3.1. Study Population
3.2. SBS Patients
3.2.1. Patient Characteristics
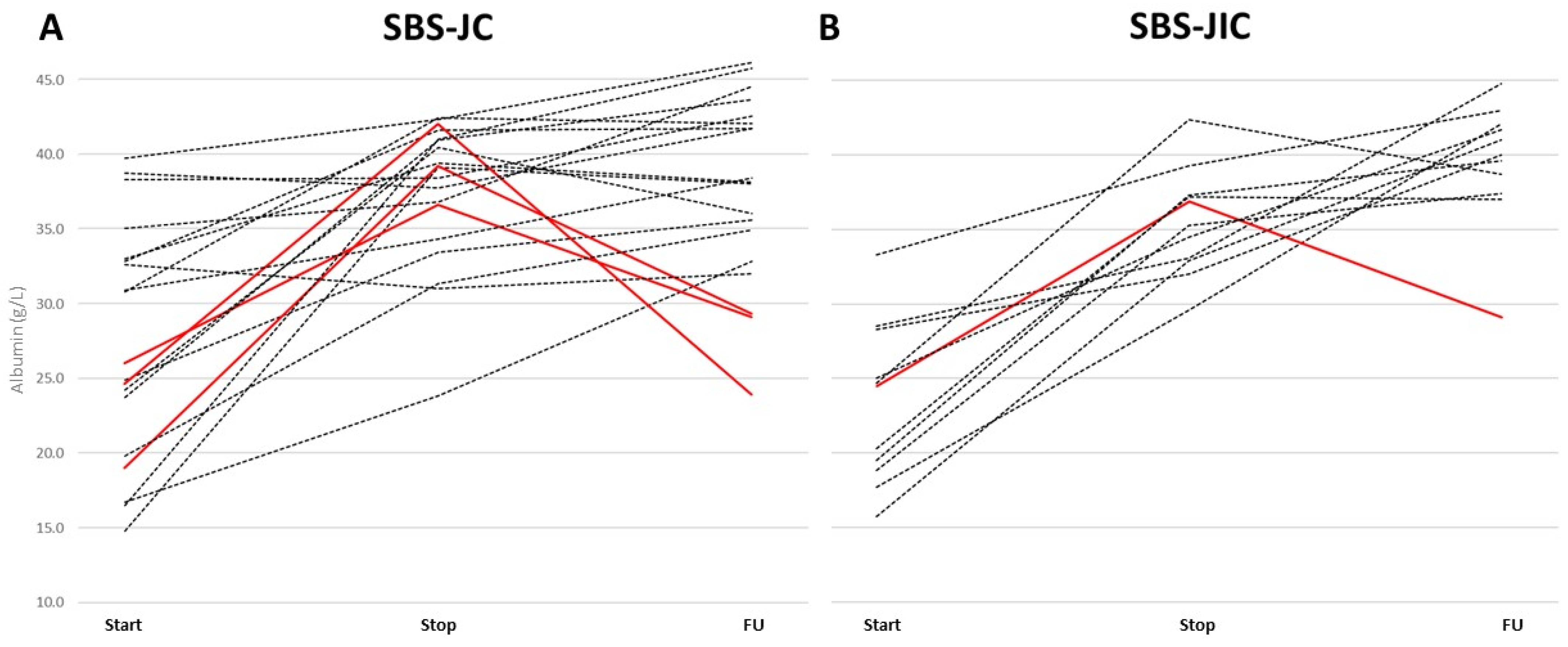
3.2.2. Evolution during IVS
3.2.3. Evolution during FU
3.3. Other Causes Than SBS
3.4. Malnutrition and Sarcopenia
4. Discussion
4.1. Summary
4.2. SBS Anatomy and Evolution during IVS and FU
4.3. SB Length, Treatment or IF Causes, and Need for FU
4.4. Strenghts and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pironi, L.; Arends, J.; Baxter, J.; Bozzetti, F.; Peláez, R.B.; Cuerda, C.; Forbes, A.; Gabe, S.; Gillanders, L.; Holst, M.; et al. ESPEN endorsed recommendations: Definition and classification of intestinal failure in adults. Clin. Nutr. 2015, 34, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Pironi, L.; Arends, J.; Bozzetti, F.; Cuerda, C.; Gillanders, L.; Jeppesen, P.B.; Joly, F.; Kelly, D.; Lal, S.; Staun, M.; et al. ESPEN guidelines on chronic intestinal failure in adults. Clin. Nutr. 2016, 35, 247–307. [Google Scholar] [PubMed]
- Pironi, L.; Steiger, E.; Joly, F.; Wanten, G.J.A.; Chambrier, C.; Aimasso, U.; Sasdelli, A.S.; Szczepanek, K.; Jukes, A.; Theilla, M.; et al. Intravenous supplementation type and volume are associated with 1-year outcome and major complications in patients with chronic intestinal failure. Gut 2020, 69, 1787–1795. [Google Scholar] [CrossRef] [PubMed]
- Pironi, L.; Konrad, D.; Brandt, C.; Joly, F.; Wanten, G.; Agostini, F.; Chambrier, C.; Aimasso, U.; Zeraschi, S.; Kelly, D.; et al. Clinical classification of adult patients with chronic intestinal failure due to benign disease: An international multicenter cross-sectional survey. Clin. Nutr. 2018, 37, 728–738. [Google Scholar] [CrossRef] [PubMed]
- Pironi, L.; Steiger, E.; Joly, F.; Jeppesen, P.B.; Wanten, G.; Sasdelli, A.S.; Chambrier, C.; Aimasso, U.; Mundi, M.M.; Szczepanek, K.; et al. Characteristics of adult patients with chronic intestinal failure due to short bowel syndrome: An international multicenter survey. Clin. Nutr. ESPEN 2021, 45, 433–441. [Google Scholar]
- Amiot, A.; Messing, B.; Corcos, O.; Panis, Y.; Joly, F. Determinants of home parenteral nutrition dependence and survival of 268 patients with non-malignant short bowel syndrome. Clin. Nutr. 2013, 32, 368–374. [Google Scholar] [CrossRef]
- Adaba, F.; Rajendran, A.; Patel, A.; Cheung, Y.K.; Grant, K.; Vaizey, C.J.; Gabe, S.M.; Warusavitarne, J.; Nightingale, J.M.D. Mesenteric Infarction: Clinical Outcomes After Restoration of Bowel Continuity. Ann. Surg. 2015, 262, 1059–1064. [Google Scholar] [CrossRef]
- Cruz, R.J.; McGurgan, J.; Butera, L.; Poloyac, K.; Roberts, M.; Stein, W.; Minervini, M.; Jorgensen, D.R.; Humar, A. Gastrointestinal Tract Reconstruction in Adults with Ultra-Short Bowel Syndrome: Surgical and Nutritional Outcomes. Surgery 2020, 168, 297–304. [Google Scholar] [CrossRef]
- Kopczynska, M.; Carlson, G.; Teubner, A.; Abraham, A.; Taylor, M.; Burden, S.T.; Hvas, C.L.; Jepsen, P.; Lal, S. Long-Term Outcomes in Patients with Intestinal Failure Due to Short Bowel Syndrome and Intestinal Fistula. Nutrients 2022, 14, 1449. [Google Scholar] [CrossRef]
- Messing, B.; Crenn, P.; Beau, P.; Boutron-Ruault, M.C.; Rambaud, C.; Matuchansky, C. Long-term survival and parenteral nutrition dependence in adult patients with the short bowel syndrome. Gastroenterology 1999, 117, 1043–1050. [Google Scholar] [CrossRef]
- Verbiest, A.; Wauters, L.; Vanuytsel, T. Enterohormone therapy for short bowel syndrome. Curr. Opin. Endocrinol. Diabetes Obes. 2022, 29, 207–218. [Google Scholar] [CrossRef]
- Chiplunker, A.J.; Chen, L.; Levin, M.S.; Warner, B.W.; Davidson, N.O.; Rubin, D.C. Increased Adiposity and Reduced Lean Body Mass in Patients with Short Bowel Syndrome. Dig. Dis. Sci. 2020, 65, 3271–3279. [Google Scholar] [CrossRef]
- Oke, S.M.; Rye, B.; Malietzis, G.; Baldwin-Cleland, R.; Bottle, A.; Gabe, S.M.; Lung, P.F.C. Survival and CT defined sarcopenia in patients with intestinal failure on home parenteral support. Clin. Nutr. 2020, 39, 829–836. [Google Scholar] [CrossRef]
- Skallerup, A.; Nygaard, L.; Olesen, S.S.; Køhler, M.; Vinter-Jensen, L.; Rasmussen, H.H. The prevalence of sarcopenia is markedly increased in patients with intestinal failure and associates with several risk factors. Clin. Nutr. 2018, 37, 2029–2035. [Google Scholar] [CrossRef]
- Joly, F.; Baxter, J.; Staun, M.; Kelly, D.G.; Hwa, Y.L.; Corcos, O.; De Francesco, A.; Agostini, F.; Klek, S.; Santarpia, L.; et al. Five-year survival and causes of death in patients on home parenteral nutrition for severe chronic and benign intestinal failure. Clin. Nutr. 2018, 37, 1415–1422. [Google Scholar] [CrossRef] [PubMed]
- Pironi, L.; Boeykens, K.; Bozzetti, F.; Joly, F.; Klek, S.; Lal, S.; Lichota, M.; Mühlebach, S.; Van Gossum, A.; Wanten, G.; et al. ESPEN guideline on home parenteral nutrition. Clin. Nutr. 2020, 39, 1645–1666. [Google Scholar] [PubMed]
- Amiot, A.; Joly, F.; Alves, A.; Panis, Y.; Bouhnik, Y.; Messing, B. Long-term outcome of chronic intestinal pseudo-obstruction adult patients requiring home parenteral nutrition. Am. J. Gastroenterol. 2009, 104, 1262–1270. [Google Scholar] [CrossRef] [PubMed]
- Cummings, J.H.; James, W.P.T.; Wiggins, H.S. Role of the colon in ileal-resection diarrhoea. Lancet 1973, 301, 344–347. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Peolsson, A.; Massy-Westropp, N.; Desrosiers, J.; Bear-Lehman, J. Reference values for adult grip strength measured with a Jamar dynamometer: A descriptive meta-analysis. Physiotherapy 2006, 92, 11–15. [Google Scholar] [CrossRef]
- Cederholm, T.; Bosaeus, I.; Barazzoni, R.; Bauer, J.; Van Gossum, A.; Klek, S.; Muscaritoli, M.; Nyulasi, I.; Ockenga, J.; Schneider, S.M.; et al. Diagnostic criteria for malnutrition-An ESPEN Consensus Statement. Clin. Nutr. 2015, 34, 335–340. [Google Scholar] [CrossRef]
- Cederholm, T.; Jensen, G.L.; Correia, M.I.T.D.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.; et al. GLIM criteria for the diagnosis of malnutrition–A consensus report from the global clinical nutrition community. Clin. Nutr. 2019, 38, 207–217. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Fuglsang, K.A.; Brandt, C.F.; Scheike, T.; Jeppesen, P.B. Differences in methodology impact estimates of survival and dependence on home parenteral support of patients with nonmalignant short bowel syndrome. Am. J. Clin. Nutr. 2020, 111, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Pironi, L.; Corcos, O.; Forbes, A.; Holst, M.; Joly, F.; Jonkers, C.; Klek, S.; Lal, S.; Blaser, A.R.; Rollins, K.; et al. Intestinal failure in adults: Recommendations from the ESPEN expert groups. Clin. Nutr. 2018, 37, 1798–1809. [Google Scholar] [CrossRef]
- Jeppesen, P.B.; Mortensen, P.B. Colonic Digestion and Absorption of Energy from Carbohydrates and Medium-Chain Fat in Small Bowel Failure. J. Parenter. Enter. Nutr. 1999, 23, S101–S105. [Google Scholar] [CrossRef]
- Jeppesen, P.B.; Mortensen, P.B. The influence of a preserved colon on the absorption of medium chain fat in patients with small bowel resection. Gut 1998, 43, 478–483. [Google Scholar] [CrossRef] [PubMed]
- Tjellesen, L.; Staun, M.; Nielsen, P.K. Body Composition Changes Measured by Dual-Energy X-ray Absorptiometry in Patients Receiving Home Parenteral Nutrition. Scand. J. Gastroenterol. 1997, 32, 686–690. [Google Scholar] [CrossRef]
- Køhler, M.; Olesen, S.S.; Rasmussen, H.H. Body composition predicts clinical outcome in patients with intestinal failure on long-term home parenteral nutrition. Clin. Nutr. ESPEN 2018, 28, 193–200. [Google Scholar] [CrossRef]
- Barril, G.; Nogueira, A.; Alvarez-García, G.; Núñez, A.; Sánchez-González, C.; Ruperto, M. Nutritional Predictors of Mortality after 10 Years of Follow-Up in Patients with Chronic Kidney Disease at a Multidisciplinary Unit of Advanced Chronic Kidney Disease. Nutrients 2022, 14, 3848. [Google Scholar] [CrossRef] [PubMed]
- Kyle, U.G.; Soundar, E.P.; Genton, L.; Pichard, C. Can phase angle determined by bioelectrical impedance analysis assess nutritional risk? A comparison between healthy and hospitalized subjects. Clin. Nutr. 2012, 31, 875–881. [Google Scholar] [CrossRef]
- Jeppesen, P.B.; Hartmann, B.; Hansen, B.S.; Thulesen, J.; Holst, J.J.; Mortensen, P.B. Impaired meal stimulated glucagon-like peptide 2 response in ileal resected short bowel patients with intestinal failure. Gut 1999, 45, 559–563. [Google Scholar] [CrossRef] [PubMed]
- Jeppesen, P.B.; Hartmann, B.; Thulesen, J.; Hansen, B.S.; Holst, J.J.; Poulsen, S.S.; Mortensen, P.B. Elevated plasma glucagon-like peptide 1 and 2 concentrations in ileum resected short bowel patients with a preserved colon. Gut 2000, 47, 370–376. [Google Scholar] [CrossRef]
- Iyer, K.R.; Kunecki, M.; Boullata, J.I.; Fujioka, K.; Joly, F.; Gabe, S.; Pape, U.F.; Schneider, S.M.; Virgili Casas, M.N.; Ziegler, T.R.; et al. Independence from Parenteral Nutrition and Intravenous Fluid Support During Treatment with Teduglutide Among Patients with Intestinal Failure Associated With Short Bowel Syndrome. J. Parenter. Enter. Nutr. 2017, 41, 946–951. [Google Scholar] [CrossRef]
- Bioletto, F.; D’eusebio, C.; Merlo, F.D.; Aimasso, U.; Ossola, M.; Pellegrini, M.; Ponzo, V.; Chiarotto, A.; De Francesco, A.; Ghigo, E.; et al. Efficacy of Teduglutide for Parenteral Support Reduction in Patients with Short Bowel Syndrome: A Systematic Review and Meta-Analysis. Nutrients 2022, 14, 796. [Google Scholar] [CrossRef] [PubMed]
- Zaczek, Z.; Jurczak-Kobus, P.; Panczyk, M.; Braszczyńska-Sochacka, J.; Majewska, K.; Kunecki, M.; Dąbrowska, K.; Sobocki, J. Changes in Parenteral Nutrition Requirements and BMI in Patients with Parenteral Nutrition-Dependent Short Bowel Syndrome after Stopping Teduglutide-9 Years of Follow-Up. Nutrients 2022, 14, 1634. [Google Scholar] [CrossRef] [PubMed]
- Gondolesi, G.E.; Doeyo, M.; Lic, C.E.; Lobos, F.; Rubio, S.; Rumbo, C.; Ramisch, D.; Crivelli, A.; Schelotto, P.B.; Solar, H. Results of Surgical and Medical Rehabilitation for Adult Patients with Type III Intestinal Failure in a Comprehensive Unit Today: Building a New Model to Predict Parenteral Nutrition Independency. J. Parenter. Enter. Nutr. 2020, 44, 703–713. [Google Scholar] [CrossRef] [PubMed]
- Mundi, M.S.; Vallumsetla, N.; Davidson, J.B.; McMahon, M.T.; Bonnes, S.L.; Hurt, R.T. Use of Home Parenteral Nutrition in Post-Bariatric Surgery-Related Malnutrition. J. Parenter. Enter. Nutr. 2017, 41, 1119–1124. [Google Scholar] [CrossRef]
- Neelis, E.; Olieman, J.; Rizopoulos, D.; Wijnen, R.; Rings, E.; de Koning, B.; Hulst, J. Growth, Body Composition, and Micronutrient Abnormalities During and After Weaning Off Home Parenteral Nutrition. J. Pediatr. Gastroenterol. Nutr. 2018, 67, e95–e100. [Google Scholar] [CrossRef]

| Variable | Total (n = 98) | |
|---|---|---|
| Age (years) | Median (IQR) | 54.8 (43.1; 65) |
| Gender | Female (%) | 54 (55) |
| Weight (kg) | Median (IQR) | 61 (52.2; 72) |
| BMI (kg/m2) | Median (IQR) | 24.1 (21.7; 31.9) |
| Mechanism of IF | SBS (%) | 77 (78.6) |
| Mot (%) | 9 (9.1) | |
| O (%) | 5 (5.1) | |
| MD (%) | 4 (4.1) | |
| F (%) | 3 (3.1) | |
| Severity of IF (max) | FE (%) | 5 (5.1) |
| PN1 (≤1 L) | 9 (9.1) | |
| PN2 (1–2 L) | 46 (46.9) | |
| PN3 (2–3 L) | 16 (16.3) | |
| PN4 (>3 L) | 22 (22.4) | |
| IVS duration (weeks) | Median (IQR) | 30.8 (13.7; 58.3) |
| FU duration (weeks) | Median (IQR) | 40.1 (14.7; 69.9) |
| Class | Variable | Temporary SBS (n = 26) | SBS-JC (n = 21) | SBS-JIC (n = 12) | SBS-I (n = 6) | SBS + TED (n = 5) | p-Value |
|---|---|---|---|---|---|---|---|
| Demo-graphics | Age (years) | 58 (49; 69) | 64 (45; 74) | 57 (43; 69) | 50 (32; 63) | 56 (47;64) | 0.57 |
| Gender (female) | 13 (50) | 17 (81) | 8 (61.5) | 1 (16.7) | 1 (20) | 0.02 | |
| Etiology (%) | Ischemia (A/V) | 11/6 (65.4) | 10/0 (47.6) | 3/4 (53.8) | 1 (16.7) | 1/1 (40) | 0.25 |
| IBD (CD/UC) | 6/1 (26.9) | 4/0 (19) | 1 (7.7) | 5 (83.3) | 0 (0) | <0.01 | |
| Radiation | 1 (3.8) | 3 (14.3) | 2 (15.4) | 0 (0) | 0 (0) | 0.48 | |
| Surgical/adhesion | 1 (3.8) | 3 (14.3) | 2 (15.4) | 0 (0) | 3 (60) | 0.01 | |
| Trauma/volvulus | 0 (0) | 1 (4.8) | 1 (7) | 0 (0) | 0 (0) | 0.65 | |
| IF class (%) | FE | 2 (7.7) | 0 (0) | 0 (0) | 3 (50) | 0 (0) | <0.001 |
| PN1 (≤1 L) | 2 (7.7) | 2 (9.5) | 0 (0) | 0 (0) | 0 (0) | 0.69 | |
| PN2 (1–2 L) | 10 (38.5) | 8 (38.1) | 4 (30.8) | 3 (50) | 0 (0) | 0.46 | |
| PN3 (2–3 L) | 8 (30.8) | 4 (19) | 2 (15.4) | 0 (0) | 1 (20) | 0.50 | |
| PN4 (>3 L) | 4 (15.4) | 7 (33.3) | 7 (53.8) | 0 (0) | 4 (80) | <0.01 | |
| Total SB (cm) | 300 (240; 330) | 105 (70; 160) | 160 (70; 190) | 250 (200; 300) | 75 (69; 80) | <0.0001 | |
| Anatomy | Ileum (cm) | 120 (13; 235) | 0 (0; 0) | 50 (25; 120) | NA | 0 (0; 10) | <0.0001 |
| Colon (%) | 100 (86; 100) | 75 (70; 90) | 100 (100; 100) | NA | 80 (63; 88) | <0.0001 | |
| Duration | IVS (weeks) | 10.5 (7; 14) | 40 (28.5; 67) | 23 (14.5; 64) | 62.5 (35; 141) | 166 (93.5; 376) | <0.0001 |
| FU (weeks) | 29 (15; 48) | 39 (12.5:84.5) | 22 (15; 83.5) | 40.5 (9; 45) | 137 (76; 156) | 0.04 |
| Variable | Time | Temporary SBS (n = 26) | SBS-JC (n = 21) | SBS-JIC (n = 12) | SBS-I (n = 6) | SBS + TED (n = 5) | p-Value |
|---|---|---|---|---|---|---|---|
| BW (kg) | Start IVS | 71.4 (55.8; 81) | 65 (54; 74) | 58.6 (52.2; 83) | 60.7 (56; 65) | 55 (47; 67) | |
| Stop IVS | 73.8 (60; 79.3) | 68.8 (57; 79.8) | 65.5 (54; 77.4) | 76 (64.3; 79.3) | 66 (59.8; 71) | 0.02 | |
| FU | 77 (61.5; 87.3) | 62 (53.5; 72) | 66 (54.5; 76.3) | 73 (62.4; 80.5) | 69 (57.5; 71.5) | 0.0001 | |
| BMI (kg/m2) | Start IVS | 24 (20.4; 28.8) | 23.6 (18.8; 28.8) | 21.1 (18.4; 30.5) | 17.8 (17; 20.4) | 18.7 (17.5; 20.9) | |
| Stop IVS | 24.5 (22.2; 27.8) | 24.7 (22; 29.6) | 23.2 (20.1; 27.4) | 23 (20.8; 24.6) | 22.3 (21.6; 22.8) | 0.03 | |
| FU | 26.9 (23.2; 31.2) | 22.6 (20.9; 25.7) | 22.6 (20.3; 28.7) | 22 (19.8; 24.4) | 22.9 (20.7; 23.4) | 0.0001 | |
| Albumin (g/L) | Start IVS | 23.4 (20.3; 28) | 25.5 (20.7; 33) | 23.7 (19; 27.5) | 26.7 (22.4; 38) | 32.1 (28.3; 32.6) | |
| Stop IVS | 36.3 (32; 40.9) | 38.8 (34.9; 41) | 34.9 (32.2; 37.3) | 39.9 (37.2; 41.9) | 43 (36.4; 48.6) | 0.91 | |
| FU | 39.2 (36.5; 44.4) | 38.1 (32.8; 42.5) | 40 (37.4; 42.1) | 40.3 (38.8; 42.2) | 40.9 (37.9; 45.8) | 0.09 | |
| CRP (mg/L) | Start IVS | 8 (2.8; 17) | 2 (1; 11) | 3.5 (2; 16.8) | 8.5 (2.5; 24.8) | 8 (1; 26) | |
| Stop IVS | 2.5 (1; 8) | 1 (1; 2.9) | 5 (2.3; 6.8) | 1 (1; 13) | 1 (1; 6.5) | 0.47 | |
| FU | 1 (1; 6.8) | 1 (1; 3) | 1 (1; 7) | 4 (2; 24) | 1 (1; 1) | 0.4 |
| Type | TS (%) | Ferritin (µg/L) | FA (nmol/L) | Vit B12 (pmol/L) | Vit A (µmol/L) | Vit D (pmol/L) | Vit E (µmol/L) | Cu (µmol/L) | Se (µmol/L) | Zn (µmol/L) | CRP (mg/L) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| SBS-JC | 3 | 13 | 19.1 | 334 | 1.1 | 22.4 | 25.9 | 9.4 | 0.8 | 25.5 | 1 |
| SBS-JC | 13 | 140 | 27.6 | 368 | 1 | 28.6 | 21 | 17.3 | 1.1 | 16.3 | 12 |
| SBS-JC | 50 | 126 | 11.5 | 230 | 1.1 | <10 | 18.4 | 6.3 | 0.9 | 18.7 | 1 |
| SBS-JIC | 86 | 583 | 9.8 | 441 | 0.7 | 61.8 | 23.8 | 7.5 | 0.6 | 8.4 | 3 |
| CIPO | 20 | 235 | 27.4 | 107 | 2.78 | 37.7 | 32.8 | 11.27 | 1.29 | 12.57 | 1 |
| Normal values | 20–40 | 26–388 | 6.8–45.4 | 139–651 | 1.5–2.7 | 75–200 | 21–35 | 12.7–22.2 | 0.9–1.5 | 12.5–18 | <6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wauters, L.; Dermine, S.; de Dreuille, B.; Bettolo, J.; Hutinet, C.; Mohamed, A.; Lecoq, E.; Billiauws, L.; Nuzzo, A.; Corcos, O.; et al. Malnutrition with Low Muscle Mass Is Common after Weaning off Home Parenteral Nutrition for Chronic Intestinal Failure. Nutrients 2023, 15, 338. https://doi.org/10.3390/nu15020338
Wauters L, Dermine S, de Dreuille B, Bettolo J, Hutinet C, Mohamed A, Lecoq E, Billiauws L, Nuzzo A, Corcos O, et al. Malnutrition with Low Muscle Mass Is Common after Weaning off Home Parenteral Nutrition for Chronic Intestinal Failure. Nutrients. 2023; 15(2):338. https://doi.org/10.3390/nu15020338
Chicago/Turabian StyleWauters, Lucas, Solène Dermine, Brune de Dreuille, Joanna Bettolo, Coralie Hutinet, Ashiq Mohamed, Emilie Lecoq, Lore Billiauws, Alexandre Nuzzo, Olivier Corcos, and et al. 2023. "Malnutrition with Low Muscle Mass Is Common after Weaning off Home Parenteral Nutrition for Chronic Intestinal Failure" Nutrients 15, no. 2: 338. https://doi.org/10.3390/nu15020338
APA StyleWauters, L., Dermine, S., de Dreuille, B., Bettolo, J., Hutinet, C., Mohamed, A., Lecoq, E., Billiauws, L., Nuzzo, A., Corcos, O., & Joly, F. (2023). Malnutrition with Low Muscle Mass Is Common after Weaning off Home Parenteral Nutrition for Chronic Intestinal Failure. Nutrients, 15(2), 338. https://doi.org/10.3390/nu15020338






