Nutritional and Exercise-Focused Lifestyle Interventions and Glycemic Control in Women with Diabetes in Pregnancy: A Systematic Review and Meta-Analysis of Randomized Clinical Trials
Abstract
1. Introduction
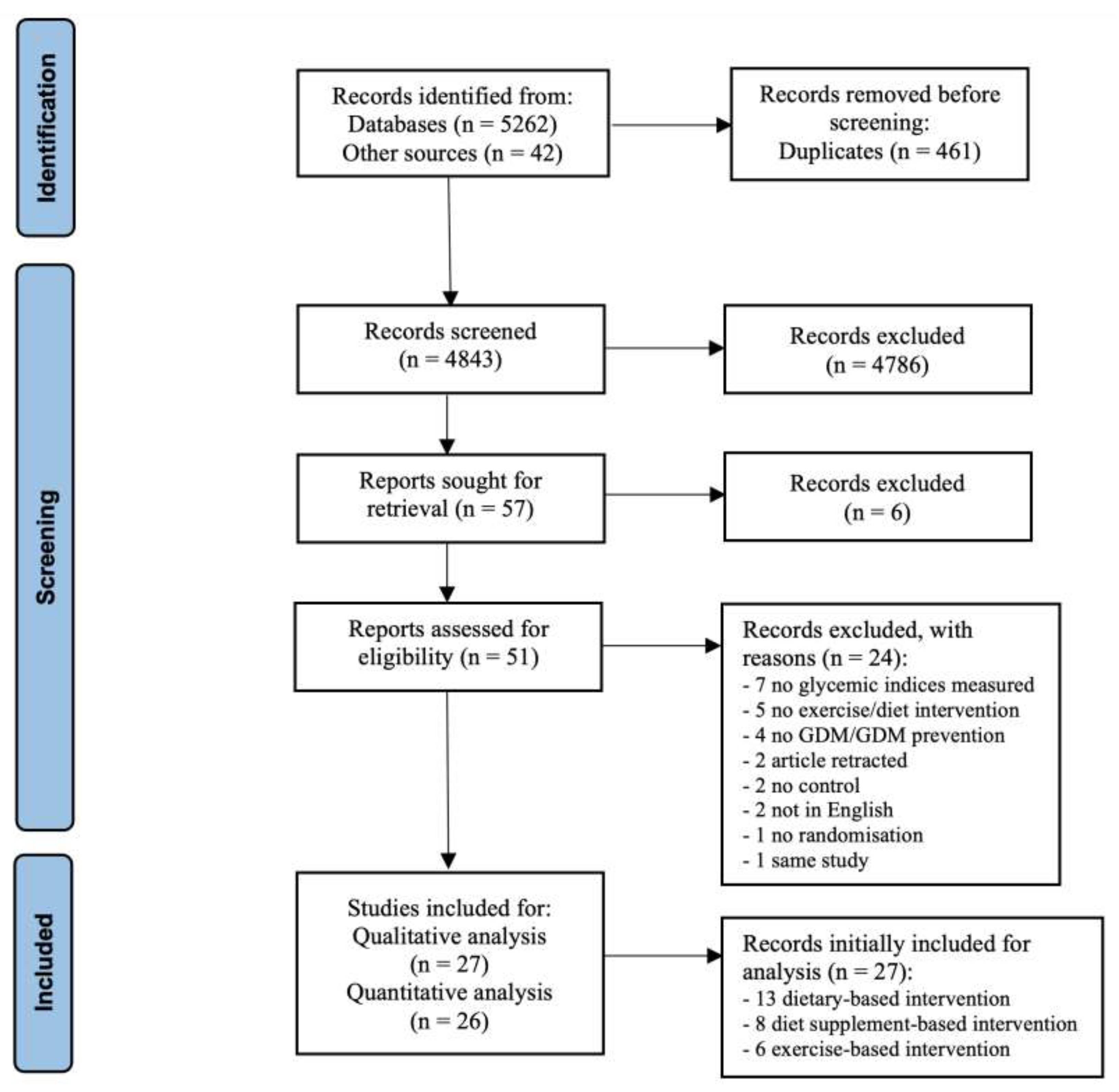
2. Materials and Methods
2.1. Search Strategy and Study Selection
2.2. Data Extraction and Quality Assessment
2.3. Data Analysis
2.4. Grading the Evidence
3. Results
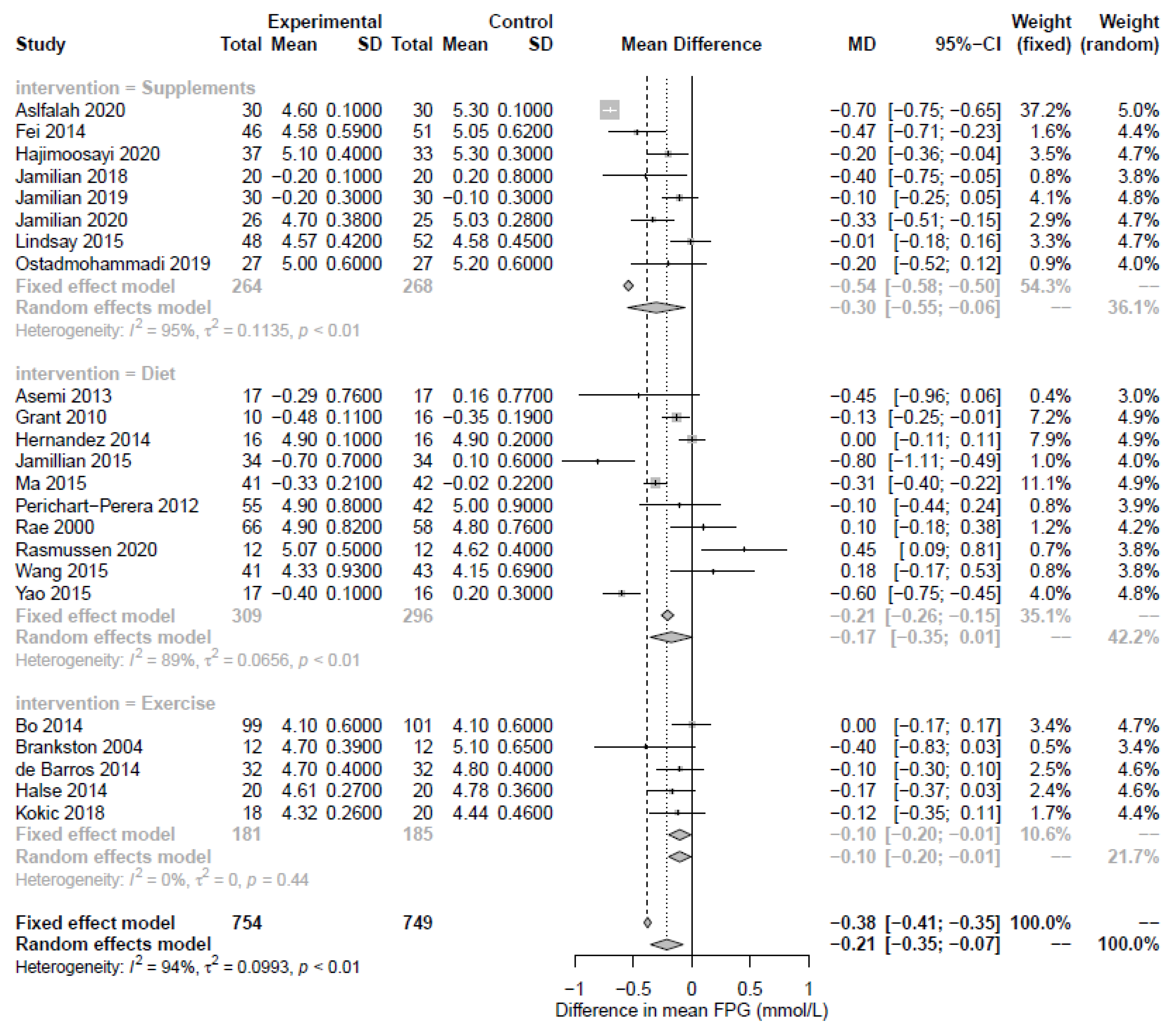
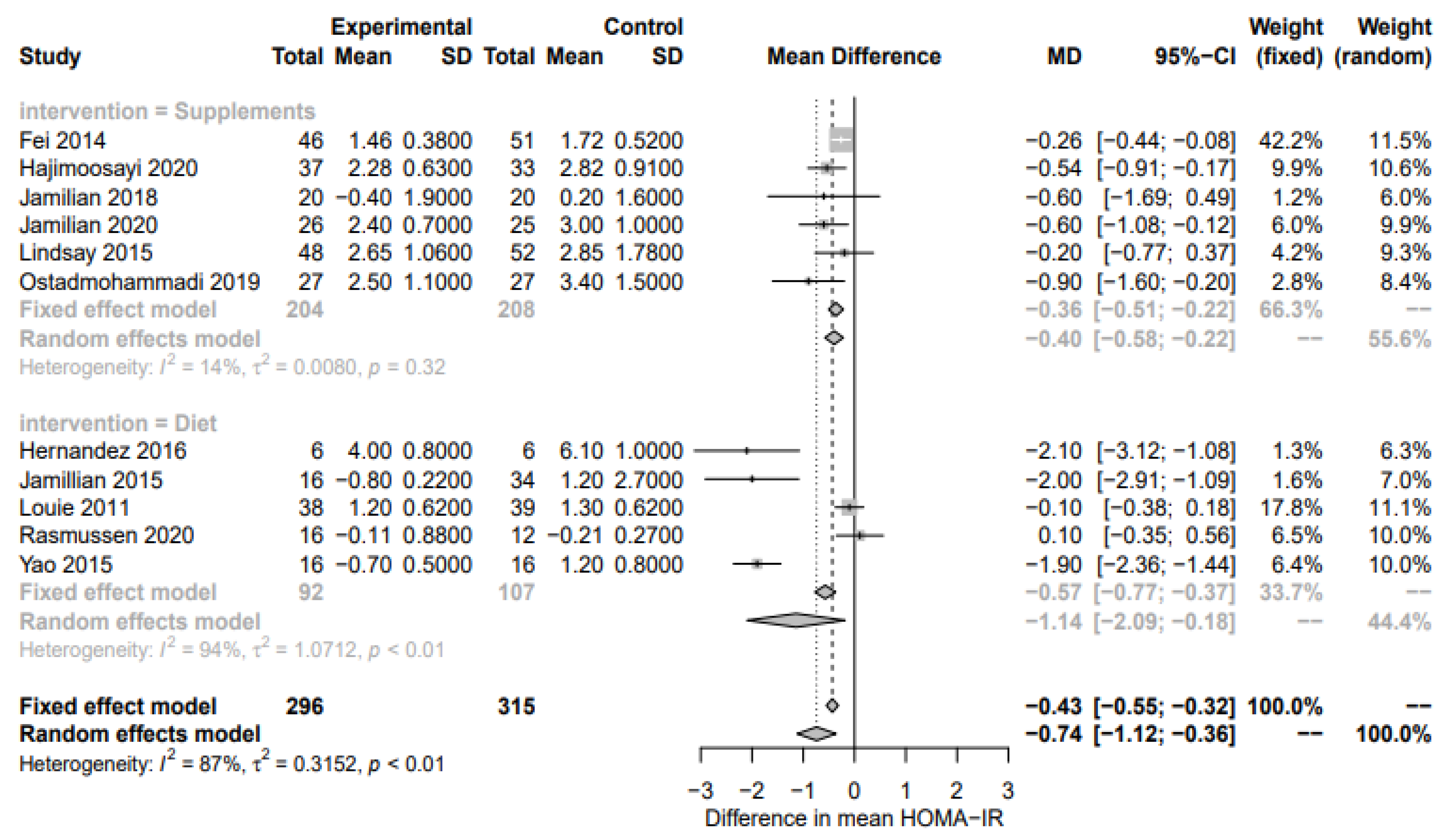
3.1. Nutritional Supplement-Based Interventions
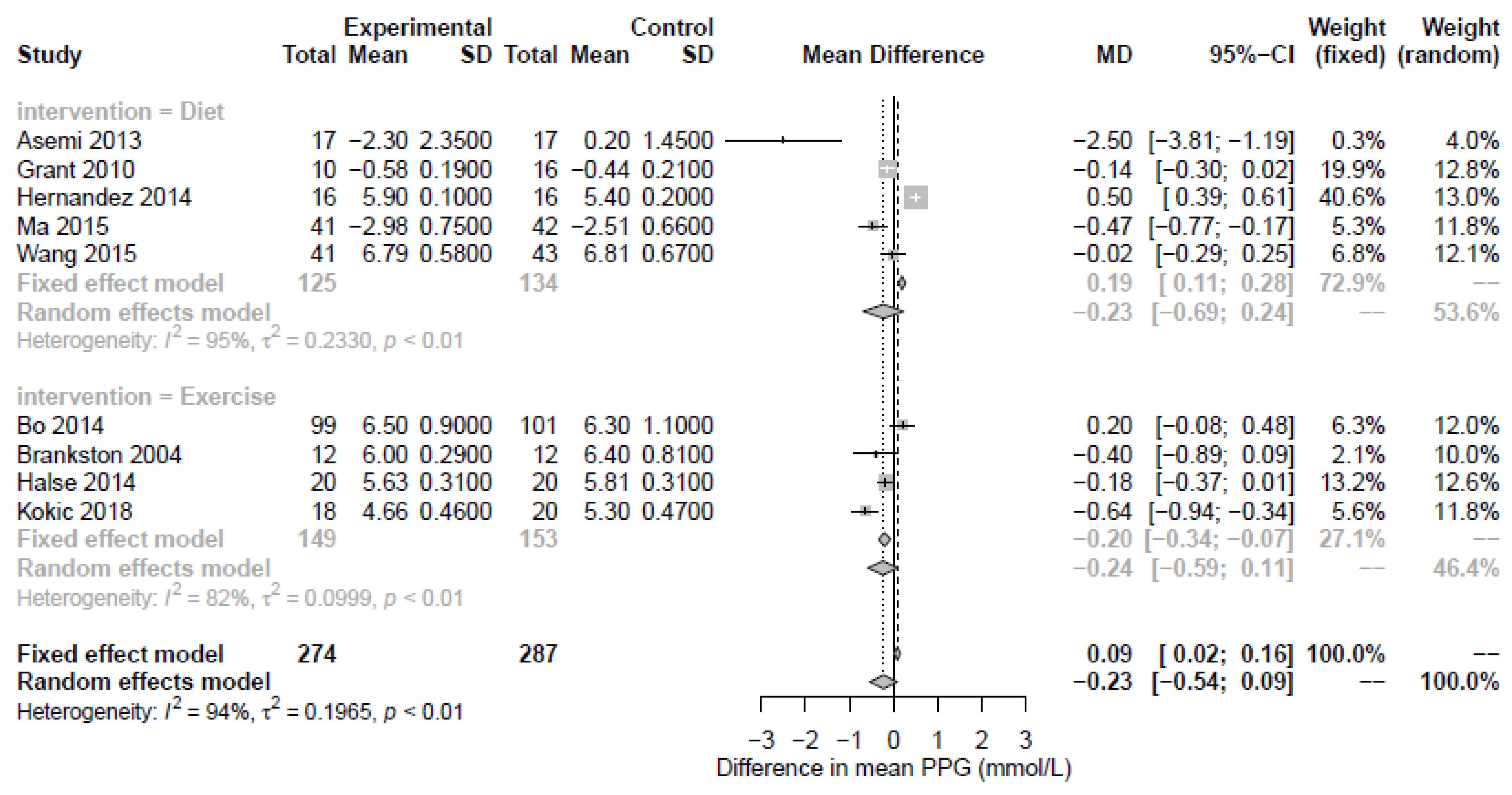
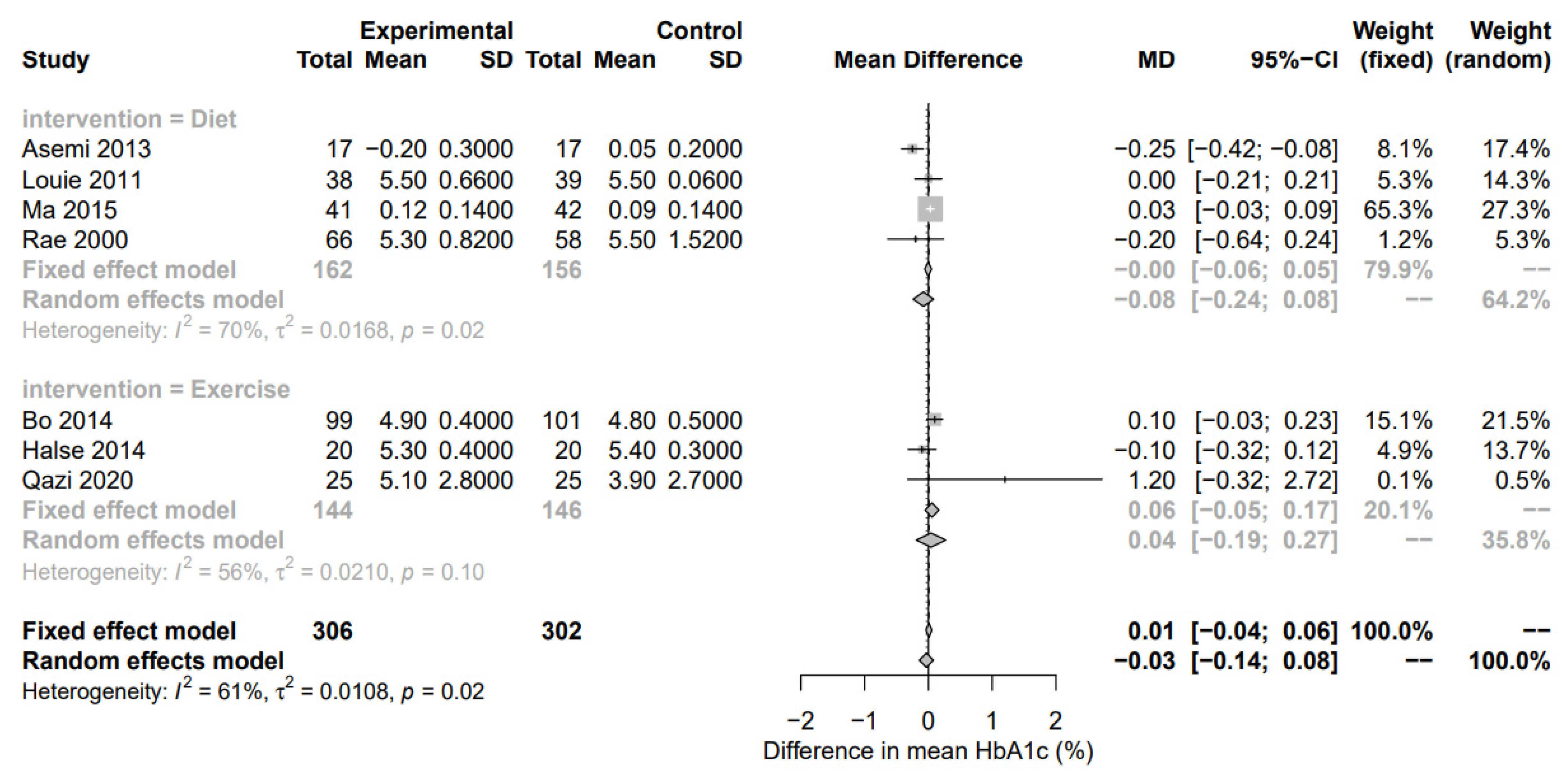
3.2. Diet-Based Interventions
3.3. Exercise-Based Interventions
3.4. Risk of Bias Assessment
3.5. Grading the Evidence
4. Discussion
4.1. Nutritional Supplement-Based Interventions
4.2. Diet-Based Interventions
4.3. Exercise-Based Interventions
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chivese, T.; Hoegfeldt, C.A.; Werfalli, M.; Yuen, L.; Sun, H.; Karuranga, S.; Li, N.; Gupta, A.; Immanuel, J.; Divakar, H.; et al. IDF Diabetes Atlas: The prevalence of pre-existing diabetes in pregnancy—A systematic review and meta-analysis of studies published during 2010–2020. Diabetes Res. Clin. Pract. 2021, 183, 109049. [Google Scholar] [CrossRef] [PubMed]
- Modder, J. CEMACH report on pregnancy risk in women with diabetes. Br. J. Midwifery 2006, 14, 44–45. [Google Scholar] [CrossRef]
- Allehdan, S.S.; Basha, A.; Asali, F.; Tayyem, R.F. Dietary and exercise interventions and glycemic control and maternal and newborn outcomes in women diagnosed with gestational diabetes: Systematic review. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 2775–2784. [Google Scholar] [CrossRef] [PubMed]
- Vargas, R.; Repke, J.T.; Ural, S.H. Type 1 diabetes mellitus and pregnancy. Rev. Obstet. Gynecol. 2010, 3, 92. [Google Scholar]
- Temple, R.; Murphy, H. Type 2 diabetes in pregnancy—An increasing problem. Best Pract. Res. Clin. Endocrinol. Metab. 2010, 24, 591–603. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, J.M.; Kellett, J.E.; Balsells, M.; García-Patterson, A.; Hadar, E.; Solà, I.; Gich, I.; van der Beek, E.M.; Castañeda-Gutiérrez, E.; Heinonen, S. Gestational diabetes mellitus and diet: A systematic review and meta-analysis of randomized controlled trials examining the impact of modified dietary interventions on maternal glucose control and neonatal birth weight. Diabetes Care 2018, 41, 1346–1361. [Google Scholar] [CrossRef] [PubMed]
- De Souza, R.J.; Zulyniak, M.A.; Stearns, J.C.; Wahi, G.; Teo, K.; Gupta, M.; Sears, M.R.; Subbarao, P.; Anand, S.S. The influence of maternal and infant nutrition on cardiometabolic traits: Novel findings and future research directions from four Canadian birth cohort studies. Proc. Nutr. Soc. 2019, 78, 351–361. [Google Scholar] [CrossRef] [PubMed]
- International Association of Diabetes and Pregnancy Study Groups Consensus Panel. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 2010, 33, 676–682. [Google Scholar] [CrossRef]
- Webber, J.; Charlton, M.; Johns, N. Diabetes in pregnancy: Management of diabetes and its complications from preconception to the postnatal period (NG3). Br. J. Diabetes Vasc. Dis. 2015, 15, 107–111. [Google Scholar] [CrossRef]
- American Diabetes Association. 14. Management of diabetes in pregnancy: Standards of medical care in diabetes—2020. Diabetes Care 2020, 43, S183–S192. [Google Scholar] [CrossRef]
- Perichart-Perera, O.; Balas-Nakash, M.; Rodríguez-Cano, A.; Legorreta-Legorreta, J.; Parra-Covarrubias, A.; Vadillo-Ortega, F. Low Glycemic Index Carbohydrates versus All Types of Carbohydrates for Treating Diabetes in Pregnancy: A Randomized Clinical Trial to Evaluate the Effect of Glycemic Control. Int. J. Endocrinol. 2012, 2012, 296017. [Google Scholar] [CrossRef] [PubMed]
- Moses, R.G.; Luebcke, M.; Davis, W.S.; Coleman, K.J.; Tapsell, L.C.; Petocz, P.; Brand-Miller, J. Effect of a low-glycemic-index diet during pregnancy on obstetric outcomes. Am. J. Clin. Nutr. 2006, 84, 807–812. [Google Scholar] [CrossRef] [PubMed]
- Fuller, H.; Moore, J.B.; Iles, M.M.; Zulyniak, M.A. Ethnic-specific associations between dietary consumption and gestational diabetes mellitus incidence: A meta-analysis. PLoS Glob. Public Health 2022, 2, e0000250. [Google Scholar] [CrossRef]
- Bung, P.; Artal, R. Gestational diabetes and exercise: A survey. Semin. Perinatol. 1996, 20, 328–333. [Google Scholar] [CrossRef]
- Prather, H.; Spitznagle, T.; Hunt, D. Benefits of Exercise During Pregnancy. PMR 2012, 4, 845–850. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Zhu, W.; Wei, Y.; Feng, H.; Su, R.; Yang, H. Exercise intervention during pregnancy can be used to manage weight gain and improve pregnancy outcomes in women with gestational diabetes mellitus. BMC Pregnancy Childbirth 2015, 15, 255. [Google Scholar] [CrossRef]
- Voormolen, D.N.; DeVries, J.H.; Sanson, R.M.E.; Heringa, M.P.; de Valk, H.W.; Kok, M.; van Loon, A.J.; Hoogenberg, K.; Bekedam, D.J.; Brouwer, T.C.B. Continuous glucose monitoring during diabetic pregnancy (glucomoms): A multicentre ran-domized controlled trial. Diabetes Obes. Metab. 2018, 20, 1894–1902. [Google Scholar] [CrossRef] [PubMed]
- Murphy, H.R.; Rayman, G.; Duffield, K.; Lewis, K.S.; Kelly, S.; Johal, B.; Fowler, D.; Temple, R.C. Changes in the Glycemic Profiles of Women with Type 1 and Type 2 Diabetes during Pregnancy. Diabetes Care 2007, 30, 2785–2791. [Google Scholar] [CrossRef]
- Law, G.R.; Alnaji, A.; Alrefaii, L.; Endersby, D.; Cartland, S.J.; Gilbey, S.G.; Jennings, P.E.; Murphy, H.R.; Scott, E.M. Subop-timal nocturnal glucose control is associated with large for gestational age in treated gestational diabetes mellitus. Diabetes Care 2019, 42, 810–815. [Google Scholar] [CrossRef]
- Scott, E.M.; Feig, D.S.; Murphy, H.R.; Law, G.R.; Grisoni, J.; Byrne, C.; Neoh, S.; Davenport, K.; Donovan, L.; Gougeon, C.; et al. Continuous Glucose Monitoring in Pregnancy: Importance of Analyzing Temporal Profiles to Understand Clinical Outcomes. Diabetes Care 2020, 43, 1178–1184. [Google Scholar] [CrossRef]
- Murphy, H.R.; Howgate, C.; O’Keefe, J.; Myers, J.; Morgan, M.; Coleman, M.A.; Jolly, M.; Valabhji, J.; Scott, E.M.; Knighton, P.; et al. Characteristics and outcomes of pregnant women with type 1 or type 2 diabetes: A 5-year national population-based cohort study. Lancet Diabetes Endocrinol. 2021, 9, 153–164. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef]
- Drevon, D.; Fursa, S.R.; Malcolm, A.L. Intercoder Reliability and Validity of WebPlotDigitizer in Extracting Graphed Data. Behav. Modif. 2016, 41, 323–339. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M. Rob 2: A revised tool for assessing risk of bias in randomized trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- GRADEpro GDT. Gradepro Guideline Development Tool [Software]; McMaster University: Hamilton, ON, Canada, 2015; p. 435. [Google Scholar]
- Aslfalah, H.; Jamilian, M.; Ansarihadipour, H.; Abdollahi, M.; Khosrowbeygi, A. Effect of alpha-lipoic acid supplementation on the lipid profile and lipid ratios in women with gestational diabetes mellitus: A clinical trial study. Int. J. Reprod. Biomed. (IJRM) 2020, 18, 1029–1038. [Google Scholar] [CrossRef] [PubMed]
- Fei, B.-B.; Ling, L.; Hua, C.; Ren, S.-Y. Effects of soybean oligosaccharides on antioxidant enzyme activities and insulin resistance in pregnant women with gestational diabetes mellitus. Food Chem. 2014, 158, 429–432. [Google Scholar] [CrossRef] [PubMed]
- Hajimoosayi, F.; Jahanian Sadatmahalleh, S.; Kazemnejad, A.; Pirjani, R. Effect of ginger on the blood glucose level of women with gestational diabetes mellitus (gdm) with impaired glucose tolerance test (gtt): A randomized double-blind place-bo-controlled trial. BMC Complement. Med. Ther. 2020, 20, 116. [Google Scholar] [CrossRef] [PubMed]
- Jamilian, M.; Samimi, M.; Mirhosseini, N.; Ebrahimi, F.A.; Aghadavod, E.; Taghizadeh, M.; Asemi, Z. A Randomized Double-Blinded, Placebo-Controlled Trial Investigating the Effect of Fish Oil Supplementation on Gene Expression Related to Insulin Action, Blood Lipids, and Inflammation in Gestational Diabetes Mellitus-Fish Oil Supplementation and Gestational Diabetes. Nutrients 2018, 10, 163. [Google Scholar] [CrossRef] [PubMed]
- Jamilian, M.; Mirhosseini, N.; Eslahi, M.; Bahmani, F.; Shokrpour, M.; Chamani, M.; Asemi, Z. The effects of magnesi-um-zinc-calcium-vitamin d co-supplementation on biomarkers of inflammation, oxidative stress and pregnancy outcomes in gestational diabetes. BMC Pregnancy Childbirth 2019, 19, 107. [Google Scholar] [CrossRef] [PubMed]
- Jamilian, M.; Tabassi, Z.; Reiner, Ž.; Panahandeh, I.; Naderi, F.; Aghadavod, E.; Amirani, E.; Taghizadeh, M.; Shafabakhsh, R.; Satari, M. The effects of n-3 fatty acids from flaxseed oil on genetic and metabolic profiles in patients with gestational diabetes mellitus: A randomized, double-blind, placebo-controlled trial. Br. J. Nutr. 2020, 123, 792–799. [Google Scholar] [CrossRef]
- Lindsay, K.L.; Brennan, L.; Kennelly, M.A.; Maguire, O.C.; Smith, T.; Curran, S.; Coffey, M.; Foley, M.E.; Hatunic, M.; Sha-nahan, F. Impact of probiotics in women with gestational diabetes mellitus on metabolic health: A randomized controlled trial. Am. J. Obstet. Gynecol. 2015, 212, 496.e1. [Google Scholar]
- Ostadmohammadi, V.; Samimi, M.; Mobini, M.; Zarezade Mehrizi, M.; Aghadavod, E.; Chamani, M.; Dastorani, M.; Asemi, Z. The effect of zinc and vitamin e cosupplementation on metabolic status and its related gene expression in patients with gesta-tional diabetes. J. Matern.-Fetal Neonatal Med. 2019, 32, 4120–4127. [Google Scholar] [CrossRef] [PubMed]
- Asemi, Z.; Tabassi, Z.; Samimi, M.; Fahiminejad, T.; Esmaillzadeh, A. Favourable effects of the dietary approaches to stop hypertension diet on glucose tolerance and lipid profiles in gestational diabetes: A randomized clinical trial. Br. J. Nutr. 2013, 109, 2024–2030. [Google Scholar] [CrossRef] [PubMed]
- Grant, S.M.; Wolever, T.M.S.; O’Connor, D.L.; Nisenbaum, R.; Josse, R.G. Effect of a low glycemic index diet on blood glucose in women with gestational hyperglycemia. Diabetes Res. Clin. Pract. 2011, 91, 15–22. [Google Scholar] [CrossRef]
- Hernandez, T.L.; Van Pelt, R.E.; Anderson, M.A.; Daniels, L.J.; West, N.A.; Donahoo, W.T.; Friedman, J.E.; Barbour, L.A. A Higher-Complex Carbohydrate Diet in Gestational Diabetes Mellitus Achieves Glucose Targets and Lowers Postprandial Lipids: A Randomized Crossover Study. Diabetes Care 2014, 37, 1254–1262. [Google Scholar] [CrossRef]
- Hernandez, T.L.; Van Pelt, R.E.; Anderson, M.A.; Reece, M.S.; Reynolds, R.M.; de la Houssaye, B.A.; Heerwagen, M.; Donahoo, W.T.; Daniels, L.J.; Chartier-Logan, C. Women with gestational diabetes mellitus randomized to a higher–complex carbohy-drate/low-fat diet manifest lower adipose tissue insulin resistance, inflammation, glucose, and free fatty acids: A pilot study. Diabetes Care 2016, 39, 39–42. [Google Scholar] [CrossRef]
- Jamilian, M.; Asemi, Z. The Effect of Soy Intake on Metabolic Profiles of Women with Gestational Diabetes Mellitus. J. Clin. Endocrinol. Metab. 2015, 100, 4654–4661. [Google Scholar] [CrossRef]
- Louie, J.C.Y.; Markovic, T.P.; Perera, N.; Foote, D.; Petocz, P.; Ross, G.P.; Brand-Miller, J.C. A Randomized Controlled Trial Investigating the Effects of a Low–Glycemic Index Diet on Pregnancy Outcomes in Gestational Diabetes Mellitus. Diabetes Care 2011, 34, 2341–2346. [Google Scholar] [CrossRef]
- Aberer, F.; Lichtenegger, K.M.; Smajic, E.; Donsa, K.; Malle, O.; Samonigg, J.; Höll, B.; Beck, P.; Pieber, T.R.; Plank, J.; et al. Glucotab-guided insulin therapy using insulin glargine u300 enables glycemic control with low risk of hypoglycaemia in hos-pitalized patients with type 2 diabetes. Diabetes Obes. Metab. 2019, 21, 584–591. [Google Scholar] [CrossRef]
- Rae, A.; Bond, D.; Evans, S.; North, F.; Roberman, B.; Walters, B. A randomized controlled trial of dietary energy restriction in the management of obese women with gestational diabetes. Aust. N. Z. J. Obstet. Gynaecol. 2000, 40, 416–422. [Google Scholar] [CrossRef]
- Rasmussen, L.; Christensen, M.L.; Poulsen, C.W.; Rud, C.; Christensen, A.S.; Andersen, J.R.; Kampmann, U.; Ovesen, P.G. Effect of high versus low carbohydrate intake in the morning on glycemic variability and glycemic control measured by con-tinuous blood glucose monitoring in women with gestational diabetes mellitus—A randomized crossover study. Nutrients 2020, 12, 475. [Google Scholar] [CrossRef] [PubMed]
- Valentini, R.; Dalfrà, M.G.; Masin, M.; Barison, A.; Marialisa, M.; Pegoraro, E.; Lapolla, A. A Pilot Study on Dietary Approaches in Multiethnicity: Two Methods Compared. Int. J. Endocrinol. 2012, 2012, 985136. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Jiang, H.; Yang, L.; Zhang, M. Impacts of dietary fat changes on pregnant women with gestational diabetes mellitus: A randomized controlled study. Asia Pac. J. Clin. Nutr. 2015, 24, 58–64. [Google Scholar]
- Yao, J.; Cong, L.; Zhu, B.; Wang, T. Effect of dietary approaches to stop hypertension diet plan on pregnancy outcome patients with gestational diabetes mellitus. Bangladesh J. Pharmacol. 2015, 10, 732–738. [Google Scholar] [CrossRef]
- Bo, S.; Rosato, R.; Ciccone, G.; Canil, S.; Gambino, R.; Poala, C.B.; Leone, F.; Valla, A.; Grassi, G.; Ghigo, E.; et al. Simple lifestyle recommendations and the outcomes of gestational diabetes. A 2×2 factorial randomized trial. Diabetes Obes. Metab. 2014, 16, 1032–1035. [Google Scholar] [CrossRef]
- Brankston, G.N.; Mitchell, B.; Ryan, E.A.; Okun, N.B. Resistance exercise decreases the need for insulin in overweight women with gestational diabetes mellitus. Am. J. Obstet. Gynecol. 2004, 190, 188–193. [Google Scholar] [CrossRef]
- De Barros, M.C.; Lopes, M.A.; Francisco, R.P.V.; Sapienza, A.D.; Zugaib, M. Resistance exercise and glycemic control in women with gestational diabetes mellitus. Am. J. Obstet. Gynecol. 2010, 203, 556.e1–556.e6. [Google Scholar] [CrossRef] [PubMed]
- Halse, R.; Wallman, K.E.; Newnham, J.; Guelfi, K. Home-Based Exercise Training Improves Capillary Glucose Profile in Women with Gestational Diabetes. Med. Sci. Sports Exerc. 2014, 46, 1702–1709. [Google Scholar] [CrossRef]
- Kokic, I.S.; Ivanisevic, M.; Biolo, G.; Simunic, B.; Kokic, T.; Pisot, R. Combination of a structured aerobic and resistance exercise improves glycemic control in pregnant women diagnosed with gestational diabetes mellitus. A randomized controlled trial. Women Birth 2018, 31, e232–e238. [Google Scholar] [CrossRef]
- Qazi, W.A.; Babur, M.N.; Malik, A.N.; Begum, R. Effects of structured exercise regime on glycosylated hemoglobin and c re-active protein in patients with gestational diabetes mellitus-a randomized controlled trial. Pak. J. Med. Sci. 2020, 36, 1449. [Google Scholar] [CrossRef]
- Pan, Y.-Q.; Zheng, Q.-X.; Jiang, X.-M.; Chen, X.-Q.; Zhang, X.-Y.; Wu, J.-L. Probiotic Supplements Improve Blood Glucose and Insulin Resistance/Sensitivity among Healthy and GDM Pregnant Women: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Evid. -Based Complement. Altern. Med. 2021, 2021, 9830200. [Google Scholar] [CrossRef] [PubMed]
- Raviv, S.; Wilkof-Segev, R.; Maor-Sagie, E.; Naeh, A.; Yoeli, Y.; Hallak, M.; Gabbay-Benziv, R. Hypoglycemia during the oral glucose tolerance test in pregnancy—Maternal characteristics and neonatal outcomes. Int. J. Gynecol. Obstet. 2022, 158, 585–591. [Google Scholar] [CrossRef] [PubMed]
- Ojo, O.; Weldon, S.M.; Thompson, T.; Vargo, E.J. The effect of vitamin d supplementation on glycemic control in women with gestational diabetes mellitus: A systematic review and meta-analysis of randomized controlled trials. Int. J. Environ. Res. Public Health 2019, 16, 1716. [Google Scholar] [CrossRef] [PubMed]
- Qu, Q.; Rong, R.; Yu, J. Effect of magnesium supplementation on pregnancy outcome in gestational diabetes mellitus patients: A meta-analysis of randomized controlled trials. Food Sci. Nutr. 2022, 10, 3193–3202. [Google Scholar] [CrossRef] [PubMed]
- Poel, Y.; Hummel, P.; Lips, P.; Stam, F.; van der Ploeg, T.; Simsek, S. Vitamin D and gestational diabetes: A systematic review and meta-analysis. Eur. J. Intern. Med. 2012, 23, 465–469. [Google Scholar] [CrossRef]
- He, Y.; Ma, R.C.W.; McIntyre, H.D.; Sacks, D.A.; Lowe, J.; Catalano, P.M.; Tam, W.H. Comparing IADPSG and NICE Diagnostic Criteria for GDM in Predicting Adverse Pregnancy Outcomes. Diabetes Care 2022, 45, 2046–2054. [Google Scholar] [CrossRef]
- Major, C.A.; Henry, M.J.; DE Veciana, M.; Morgan, M.A. The Effects of Carbohydrate Restriction in Patients with Diet-Controlled Gestational Diabetes. Obstet. Gynecol. 1998, 91, 600–604. [Google Scholar] [CrossRef]
- American Diabetes, A. Management of diabetes in pregnancy. Obstet. Gynecol. Surv. 2017, 72, 264–266. [Google Scholar] [CrossRef]
- Louie, J.C.Y.; Brand-Miller, J.C.; Markovic, T.P.; Ross, G.P.; Moses, R.G. Glycemic Index and Pregnancy: A Systematic Literature Review. J. Nutr. Metab. 2010, 2010, 282464. [Google Scholar] [CrossRef]
- Brown, J.; Ceysens, G.; Boulvain, M. Exercise for pregnant women with gestational diabetes for improving maternal and fetal outcomes. Cochrane Database Syst. Rev. 2017, 2017, CD012202. [Google Scholar] [CrossRef]
- Cremona, A.; O’Gorman, C.; Cotter, A.; Saunders, J.; Donnelly, A. Effect of exercise modality on markers of insulin sensitivity and blood glucose control in pregnancies complicated with gestational diabetes mellitus: A systematic review. Obes. Sci. Pract. 2018, 4, 455–467. [Google Scholar] [CrossRef] [PubMed]
- Bird, S.R.; Hawley, J.A. Update on the effects of physical activity on insulin sensitivity in humans. BMJ Open Sport Exerc. Med. 2017, 2, e000143. [Google Scholar] [CrossRef] [PubMed]
- Ryder, J.; Chibalin, A.; Zierath, J. Intracellular mechanisms underlying increases in glucose uptake in response to insulin or exercise in skeletal muscle. Acta Physiol. Scand. 2001, 171, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Turcotte, L.P.; Fisher, J.S. Skeletal Muscle Insulin Resistance: Roles of Fatty Acid Metabolism and Exercise. Phys. Ther. 2008, 88, 1279–1296. [Google Scholar] [CrossRef] [PubMed]
| Country | n | Estimated Sample Size | Definition of GDM (Diagnostics Criteria) | Intervention Duration | Design Intervention Description | Participant Characteristics | Outcomes Measures | |
|---|---|---|---|---|---|---|---|---|
| Aslfalah et al., (2020) [26] | Iran | 60 (n = 30 for both groups) | Not reported | American Diabetes Association guidelines | 8 weeks | RCT double-blinded Intervention: received ALA (100 mg/day) Control: received cellulose acetate (100 mg/day) | Age Intervention: 30.96 ± 0.93 Control: 31.10 ± 0.92 Wks of gestation at baseline Intervention: 26.28 ± 0.23 Control: 26.51 ± 0.24 BMI (pre-pregnancy) Intervention: 26.64 ± 0.71 Control: 26.95 ± 0.73 | Fasting plasma glucose and glycated haemoglobin |
| Fei et al., (2014) [27] | China | 97 (n = 46 for I and n = 51 for C) | Not reported | National Diabetes Data group guidelines | 8 weeks | RCT Intervention: treated with the combination of insulin, regular diet, and soybean oligosaccharides (SBOS) Control: regular diet and insulin treatment | Not reported | Fasting plasma glucose and HOMA index |
| Hajimoosayi et al., (2020) [28] | Iran | 70 (n = 37 for I and n = 33 for C) | Considering a 99% CI, power of 90%, and 30% dropout rate, a sample size of 38 per group was determined. | International Association of the Diabetes in Pregnancy Study Group guidelines | 6 weeks | RCT double-blinded Intervention: received 126 tablets of ginger, Control: received 126 tablets of placebo | Age Intervention: 29.68 ± 5.05 Control: 31.15 ± 5.26 Wks of gestation at baseline Intervention: 27.72 ± 3.6 Control: 27.78 ± 3.60 BMI (at baseline) Intervention: 29.60 ± 3.6 Control: 29.50 ± 4.30 | Fasting plasma glucose, postprandial glucose and HOMA index |
| Jamilian et al., (2018) [29] | Iran | 40 (n = 20 for both groups) | Not reported | American Diabetes Association guidelines | 6 weeks | RCT double-blind Intervention: 1000 mg fish oil capsules, containing 180 mg eicosapentaenoic acid and 120 mg docosahexaenoic acid twice a day Control: placebo | Age 30.8 ± 2.4 Wks of gestation at baseline 25.3 ± 1.1 BMI (at baseline) 27.0 ± 3.1 | Fasting plasma glucose and HOMA index |
| Jamilian et al., (2019) [30] | Iran | 60 (n = 30 for both groups) | Considering a type 1 error of 5%, power of 80%, and hs-CRP mean distinction of 3.2 mg/L as outcome, a sample size of 25 per group was determined. | American Diabetes Association guidelines | 6 weeks | RCT double-blind Intervention: magnesium-zinc-calcium-vitamin D supplements Control: placebo | Age Intervention: 27.7 ± 4.0 Control: 29.1 ± 4.1 BMI (at baseline) Intervention: 25.8 ± 3.7 Control: 25.3 ± 2.5 | Fasting plasma glucose |
| Jamilian et al., (2020) [31] | Iran | 60 (n = 26 for I and n = 25 for C) | Considering a type 1 error of 5%, power of 80%, and PPAR-y change of 0.20 as outcome, a sample size of 25 per group was determined. | American Diabetes Association guidelines | 6 weeks | RCT double-blinded Intervention: 2 × 1000 mg/d n-3 fatty acids from flaxseed oil containing 400 mg α-linolenic acid in each capsule Control: placebo | Age Intervention: 29.5 ± 5 Control: 28.5 ± 4.1 BMI (at baseline) Intervention: 28.9 ± 4.8 Control: 27.3 ± 4.1 | Fasting plasma glucose and HOMA index |
| Lindsay et al., (2015) [32] | Ireland | 100 (n = 48 for I and n = 52 for C) | Considering a type 1 error of 5%, power of 80%, and 0.4 mmol/L reduction in fasting plasma glucose as outcome, a sample size of 50 per group was determined. | Based on a 100 g-oral glucose tolerance test (Carpenter and Coustan, 1982) | Diagnosis until delivery | RCT double-blinded Intervention: daily probiotic (Lactobacillus salivarius UCC118) from diagnosis until delivery Control: placebo capsule from diagnosis until delivery | Age Intervention: 33.5 ± 5.0 Control: 32.6 ± 4.5 Wks of gestation at baseline Intervention: 29.8 ± 2.5 Control: 29.5 ± 2.4 BMI (at baseline) Intervention: 29.06 ± 6.70 Control: 28.94 ± 5.79 | Fasting plasma glucose and HOMA index |
| Ostadmohammadi et al., (2019) [33] | Iran | 54 (n = 27 for both groups) | Not reported | American Diabetes Association guidelines | 6 weeks | RCT double-blind Intervention: 233 mg/day Zinc Gluconate plus 400-IU/day vitamin E supplements Control: placebo | Age Intervention: 31.1 ± 5.1 Control: 30.5 ± 3.1 Wks of gestation at baseline Intervention: 25.7 ± 1.40 Control: 25.3 ± 1.3 BMI (at baseline) Intervention: 29.3 Control: 28.5 | Fasting plasma glucose, postprandial glucose and HOMA index |
| Author, Year (Ref.) | Country | n | Estimated Sample Size | Definition of GDM (Diagnostics Criteria) | Intervention Duration | Design Intervention Description | Participant Characteristics | Outcomes Measures |
|---|---|---|---|---|---|---|---|---|
| Asemi et al., (2013) [34] | Iran | 34 (n = 17 for both groups) | Considering a type I error of 5%, power of 80% and serum HDL cholesterol levels as outcome, a sample size of 16 per group was determined. | American Diabetes Association guidelines | 4 Weeks | RCT Intervention: DASH diet Control: control diet contained 45–55% carbohydrates, 15–20% protein and 25–30% total fat | Age Intervention: 30.7 ± 6.7 Control: 29.4 ± 6·2 BMI (at baseline) Intervention: 29.0 ± 3.2 Control: 31.4 ± 5.7 | Fasting plasma glucose, postprandial glucose and glycated haemoglobin |
| Grant et al., (2011) [35] | Canada | 26 (n = 10 for I and n = 16 for C for GDM) (IGTP; n = 12) | Considering 85% power and to detect a difference of 0.6 mmol/L in capillary glucose between groups, a sample size of 50 was determined. | Canadian Diabetes Association guidelines | ~8 weeks | RCT Intervention: low glycemic index dietary intervention as a supplement to the standard medical nutrition therapy (Canadian guidelines) Control: standard medical nutrition therapy (Canadian guidelines) | Age Intervention: 34 ± 0.1 Control: 34 ± 1.1 Wks of gestation at baseline Intervention: 29 ± 0.7 Control: 29 ± 0.5 BMI (pre-pregnancy) Intervention: 27 ± 1 Control: 26 ± 1 | Fasting plasma glucose, Postprandial glucose and glycated haemoglobin |
| Hernandez et al., (2014) [36] | USA | 16 | Considering a type 1 error of 5%, power of 80%, and AUC as outcome, a sample size of 16 was determined. | American College of Obstetricians and Gynaecologists guidelines | 3 days | Randomized crossover Intervention: Higher complex CHO/Lower fat diet Control: conventional low-carbohydrate/higher-fat diet | Age 28.4 ± 1.0 Wks of gestation at baseline 31.2 ± 0.5 BMI (pre-pregnancy) 30.6 ± 1.3 | Fasting plasma glucose |
| Hernandez et al., (2016) [37] | USA | 12 (n = 6 for both groups) | Not reported | Based on a 100 g-oral glucose tolerance test (Carpenter and Coustan, 1982) | ~7 weeks | RCT Intervention: a higher–complex carbohydrate/lower-fat diet (60% carbohydrate/25% fat/15% protein) Control: conventional low-carbohydrate/higher-fat diet (40% carbohydrate/45% fat/15% protein) | Age Intervention: 30 ± 1.0 Control: 28 ± 2.0 Wks of gestation at enrolment Intervention: 31.7 ± 1.0 Control: 31.2 ± 0.4 BMI (at baseline) Intervention: 34.3 ± 1.6 Control: 33.4 ± 1.4 | HOMA index |
| Jamilian et al., (2015) [38] | Iran | 68 (n = 34 for both groups) | Considering the type 1 error of 5% power of 80%, a sample size of 28 per group was determined. | American Diabetes Association guidelines | 6 weeks | RCT Intervention: soy diet containing the same amount of protein with 35% animal protein, 35% soy protein, and 30% other plant proteins Control: control diet containing 0.8-g/kg protein (70% animal and 30% plant proteins) | Age Intervention: 28.2 ± 4.6 Control: 29.3 ± 4.2 Wks of gestation at baseline Intervention: 29 ± 0.7 Control: 29 ± 0.5 BMI (at baseline) Intervention: 28.9 ± 5.0 Control: 28.4 ± 3.4 | Fasting plasma glucose and HOMA index |
| Louie et al., (2011) [39] | Australia | 77 (n = 38 for I and n = 39 for C) | Considering power of 80% and to detect a ∼260 g difference in birth weight, a sample size of 60 per group was determined. | Australasian Diabetes in Pregnancy Society (ADIPS) guidelines | ~6–7 weeks | RCT Both diets consisted of similar protein (15–25%), fat (25–30%), and carbohydrate (40–45%) content Intervention: an Low- glycemic index (target GI ≤ 50) Control: a high-fibre content and moderate GI, similar to the Australian population average (target GI ∼60) | Age Intervention: 34.0 ± 4.1 Control: 32.4 ± 4.5 Wks of gestation at baseline Intervention: 29.0 ± 4.0 Control: 29.7 ± 3.5 BMI (pre-pregnancy) Intervention: 23.9 ± 4.4 Control: 24.1 ± 5.7 | HOMA index and glycated haemoglobin |
| Ma et al., (2014) [40] | China | 83 (n = 41 for I and n = 42 for C) | Not reported | Chinese Medical Association and the American Diabetes Association guidelines | Every 2 weeks from 24–26 weeks of gestation to delivery | RCT Intervention: intensive low-GL intervention Control: individualized general dietary intervention | Age Intervention: 30.1 ± 3.8 Control: 30.0 ± 3.5 Wks of gestation at baseline Intervention: 27.5 ± 1.1 Control: 27.9 ± 1.1 BMI (pre-pregnancy) Intervention: 21.90 ± 3.14 Control: 21.15 ± 2.75 | Fasting plasma glucose, postprandial glucose, and glycated haemoglobin |
| Perichart-Perera et al., (2012) [11] | Mexico | 107 (n = 55 for I and n = 42 for C) | Considering the type 1 error of 5% power of 80%, and 10 mg/dL difference in glucose, a sample size of 32 per group was determined. | American Diabetes Association guidelines | Not reported | RCT Intervention: Women received an individual food plan based on CHO restriction (only low glycemic index (GI) carbohydrates (CHO)) Control: Women received an individual food plan based on CHO restriction (all types of CHO) | Age Intervention: 32.3 ± 4.8 Control: 31.8 ± 5.3 Wks of gestation at enrolment Intervention: 22.5 ± 4.9 Control: 20.7 ± 6.7 BMI at baseline Intervention: 30.5 ± 5.2 Control: 32.0 ± 6.3 | Fasting plasma glucose |
| Rae et al., (2000) [41] | Australia | 124 (n = 66 for I and n = 58 for C) | Considering the type 1 error of 5% power of 80%, and frequency of insulin and macrosomia use as outcomes, a sample size of 60 per group was determined. | Not reported | Treatment until delivery (not further specified) | RCT Intervention: a moderately energy restricted diabetic diet providing between 1590–1776 kilocalories. Representing 70% of the RDI for pregnant women (National Health and Medical Research Council of Australia) Control: a diabetic diet which was not energy restricted | Age Intervention: 30.2 Control: 30.8 Wks of gestation at diagnosis Intervention: 28.1 ± 5.8 Control: 28.3 ± 4.6 BMI (at diagnosis) Intervention: 37.9 ± 0.7 Control: 38.0 ± 0.7 | Fasting glucose and glycated haemoglobin |
| Rasmussen et al., (2020) [42] | Denmark | 12 | Considering the power of 80%, and to detect 5% between groups based on Dalfra (2013), a sample size of 12 was determined. | WHO diagnostic criteria | 4 days | Randomised crossover Study Low carbohydrate morning intake vs. high carbohydrate morning intake | Age 33.6 Gestational age 33.5 BMI (pre-pregnancy) 25.2 | Fasting blood glucose |
| Valentini et al., (2012) [43] | Italy | 20 (n = 10 for both groups) | Pilot study | American Diabetes Association guidelines | Not reported | RCT Intervention: an ethnic meal plan (EMP), a food plan that included dishes typical of the foreign women’s original countries Control: a standard meal plan (SMP) prepared according to the ADA guidelines | Age Intervention: 28.9 ± 3.3 Control: 30.2 ± 4.7 BMI (pre-pregnancy) Intervention: 25.7 ± 3.6 Control: 24.1 ± 4.7 | Fasting plasma glucose, postprandial glucose and glycated haemoglobin |
| Wang et al., (2015) [44] | China | 84 (n = 41 for I and n = 43 for C) | Not reported | Based on a 75 g-oral glucose tolerance test | ~6–8 weeks | RCT Intervention: an oil-rich diet, with sunflower oil (45–50 g daily) used as cooking oil Control: a low-oil diet, with sunflower oil (20 g daily) used as cooking oil | Age Intervention: 30.29 ± 4.17 Control: 29.72 ± 4.64 Wks of gestation at baseline Intervention: 27.41 ± 1.52 Control: 27.34 ± 1.96 BMI (pre-pregnancy) Intervention: 21.36 ± 3.0 Control: 22.18 ± 3.60 | Fasting plasma glucose and postprandial glucose |
| Yao et al., (2015) [45] | China | 33 (n = 17 for I and n = 16 for C) | Considering a 75 g birthweight difference between groups, a sample size of 21 per group was determined. | American Diabetes Association guidelines | 4 weeks | RCT Intervention: DASH diet Control: control diet including 45–55% carbohydrates, 15–20% protein and 25–30% total fat. | Age Intervention: 30.7 ± 5.6 Control: 28.3 ± 5.1 Wks of gestation at baseline Intervention: 26.9 ± 1.4 Control: 25.7 ± 1.3 BMI (pre-pregnancy) Intervention: 29.6 ± 5.3 Control: 30.9 ± 4.3 | Fasting blood glucose and HOMA index |
| Author, Year (Ref.) | Country | n | Estimated Sample Size | Definition of GDM (Diagnostics Criteria) | Intervention Duration | Design Intervention Description | Participant Characteristics | Outcomes Measures |
|---|---|---|---|---|---|---|---|---|
| Bo et al., (2014) [46] | Italy | 200 (n = 99 for I and n = 101 for C) | Considering an effect size of 0.50, power of 95%, and a 10% reduction in fasting plasma glucose as outcome, a sample size of 200 was determined. | Based on a 75 g-oral glucose tolerance test | ~12–14 weeks | 2 × 2 design single-blinded All women were given the same diet (carbohydrates 48–50%, proteins 18–20%, fats 30–35%, fiber 20–25 g/day, no alcohol Intervention: received dietary recommendations Control: instructed to briskly walk 20-min/day | Age Intervention: 35.9 ± 4.8 Control: 33.9 ± 5.3 BMI (pre-pregnancy) Intervention: 25.1 ± 4.6 Control: 24.8 ± 4.2 | Fasting plasma glucose, postprandial glucose and HOMA index |
| Brankston et al., (2004) [47] | Canada | 24 (n = 12 for both groups) | Considering a type 1 error of 5%, power of 80%, and insulin use reduced to 25% as outcome, a sample size of 32 per group was determined. | Canadian Diabetes Association guidelines | At least 4 weeks | RCT Intervention: circuit-type resistance training three times per week and same standard diet. Control: standard diabetic diet that consisted of 40% carbohydrate, 20% protein, and 40% fat. | Age Intervention: 30.5 ± 4.4 Control: 31.3 ± 5.0 Wks of gestation at baseline Intervention: 29.0 ± 2.0 Control: 29.6 ± 2.1 BMI (pre-pregnancy) Intervention: 26.4 ± 7.1 Control: 25.2 ± 6.7 | Fasting plasma glucose and postprandial plasma glucose |
| de Barros et al., (2010) [48] | Brasil | 64 (n = 32 for both groups) | Considering a type 1 error of 5%, power of 80%, and insulin use required up to 20%, a sample size of 30 per group was determined. | Based on a 2 hr-75 g- or 3 hr-100 g- oral glucose tolerance test | ~6 weeks | RCT Intervention: resistance exercise program Control: no resistance exercise program | Age Intervention: 31.81 ± 4.87 Control: 32.40 ± 5.40 Wks of gestation at baseline Intervention: 31.56 ± 2.29 Control: 31.06 ± 2.30 BMI (pre-gestational) Intervention: 25.34 ± 4.16 Control: 25.39 ± 3.81 | Fasting plasma glucose |
| Halse et al., (2014) [49] | Australia | 40 (n = 20 for both groups) | Considering a type 1 error of 5%, power of 80%, and to detect a minimum 0.3 mM difference in fasting plasma glucose, a sample size of 20 per group was determined. | Based on a 75 g-oral glucose tolerance test (Australian criteria) | ~6 weeks (until week 34 of pregnancy) | RCT Intervention: home-based exercise training in combination with conventional management Control: conventional management alone | Age Intervention: 34 ± 5 Control: 32 ± 3 Wks of gestation at enrolment Intervention: 28.8 ± 0.8 Control: 28.8 ± 1 BMI (pre-pregnancy) Intervention: 26.4 ± 7.1 Control: 25.2 ± 6.7 | Fasting plasma glucose, postprandial glucose and glycated haemoglobin |
| Kokic et al., (2018) [50] | Croatia | 38 (n = 18 for I and n = 20 for C) | Not reported | International Association of the Diabetes and Pregnancy Study Groups guidelines | From the time of diagnosis of GDM until birth (minimum 6 weeks) | RCT single-blinded Intervention: standard antenatal care for GDM, and regular supervised exercise programme (two times per week 50–55 min; mixed exercises) plus daily brisk walks of at least 30 min. Control: only standard antenatal care for GDM. | Age Intervention: 32.78 ± 3.83 Control: 31.95 ± 4.91 Wks of gestation at baseline Intervention: 22.44 ± 6.55 Control: 20.80 ± 6.05 BMI (at baseline) Intervention: 24.39 ± 4.89 Control: 25.29 ± 4.65 | Fasting plasma glucose and postprandial glucose |
| Qazi et al., (2020) [51] | Pakistan | 50 (n = 25 for both groups) | Considering a CI of 95% and power of 80%, a sample size of 27 per group was determined. | Based on a 75 g-oral glucose tolerance test | 5 weeks | RCT Intervention: combination of moderate intensity aerobics, stabilization and pelvic floor muscles exercises twice a week for 5 weeks (40 min per session) along with dietary and medical interventions Control: only medical and dietary interventions with postural education | Age Intervention: 34.36 ± 5.21 Control: 35.92 ± 5.24 | Glycated haemoglobin |
| Category | Outcome Measure | RCTs (n) | MD | 95% CI | p-Value | I2 |
|---|---|---|---|---|---|---|
| Fasting Plasma Glucose (FPG, mmol/L) | ||||||
| Main analysis | Overall | 8 | −0.30 | (−0.55, −0.06) | 0.02 | 95 |
| Maternal Age 1 | <Mean age | 4 | −0.33 | (−0.76, 0.10) | 0.13 | 96 |
| ≥Mean age | 3 | −0.20 | (−0.33, −0.07) | 0.002 | 45 | |
| Gestational Age 2 | <28 weeks | 4 | −0.39 | (−0.72, −0.05) | 0.02 | 93 |
| ≥28 weeks | 1 | −0.01 | (−0.18, 0.16) | 0.905 | NA | |
| Weight (pre-pregnancy) 3 (kg/m2) | Normal weight (<25) | 5 | −0.18 | (−0.31, −0.05) | 0.005 | 55 |
| Overweight (≥25) | 1 | −0.70 | (−75, −0.65) | <0.0001 | NA | |
| Diagnostic Criteria for GDM | ADA | 5 | −0.35 | (−0.66, −0.04) | 0.03 | 94 |
| Other | 3 | −0.30 | (−0.39, 0.02) | 0.08 | 79 | |
| Geographic Region | Western country | 1 | −0.01 | (−0.18, 0.16) | 0.905 | NA |
| Non-western country | 7 | −0.35 | (−0.59, −0.10) | 0.005 | 94 | |
| HOMA-IR | ||||||
| Main analysis | Overall | 6 | −0.40 | (−0.58, −0.22) | <0.0001 | 14 |
| Maternal Age 1 | <Mean age | 2 | −0.56 | (−0.86, −0.27) | 0.002 | 0 |
| ≥Mean age | 3 | −0.51 | (−0.96, −0.05) | 0.03 | 15 | |
| Gestational Age 2 | <28 weeks | 3 | −0.62 | (−0.93, −0.30) | 0.0001 | 0 |
| ≥28 weeks | 1 | −0.2 | (−0.77, 0.37) | 0.501 | NA | |
| Diagnostic Criteria for GDM | ADA | 3 | −0.68 | (−1.05, −0.31) | 0.0003 | 0 |
| Other | 3 | −0.30 | (−0.46, −0.15) | 0.0001 | 0 | |
| Geographic Region | Western country | 1 | −0.2 | (−0.77, 0.37) | 0.501 | NA |
| Non-western country | 5 | −0.45 | (−0.67, −0.23) | <0.0001 | 27 | |
| Category | Outcome Measure | RCTs (n) | MD | 95% CI | p-Value | I2 |
|---|---|---|---|---|---|---|
| Fasting Plasma Glucose (FPG, mmol/L) | ||||||
| Main analysis | Overall | 10 | −0.17 | (−0.35, 0.01) | 0.06 | 89 |
| Maternal Age | <Mean age | 7 | −0.26 | (−0.50, −0.03) | 0.03 | 91 |
| ≥Mean age | 3 | 0.05 | (−0.29, 0.81) | 0.79 | 78 | |
| Gestational Age 1 | <28 weeks | 5 | −0.25 | (−0.51, 0.01) | 0.06 | 86 |
| ≥28 weeks | 4 | −0.08 | (−0.33, 0.16) | 0.51 | 88 | |
| Weight (pre-pregnancy) (kg/m2) | Normal weight (<25) | 3 | −0.32 | (−0.74, 0.10) | 0.14 | 88 |
| Overweight (≥25) | 7 | −0.11 | (−0.34, 0.12) | 0.35 | 89 | |
| Diagnostic Criteria for GDM 2 | ADA | 4 | −0.51 | (−0.78, −0.24) | 0.0003 | 69 |
| Other | 5 | −0.02 | (−0.21, 0.17) | 0.83 | 88 | |
| Geographic Region | Western country | 5 | 0.02 | (−0.13, 0.16) | 0.83 | 63 |
| Non-western country | 5 | −0.41 | (−0.66, −0.15) | 0.002 | 85 | |
| Study Duration 3 | Acute | 2 | 0.19 | (−0.25, 0.63) | 0.39 | 82 |
| Longitudinal | 7 | −0.29 | (−0.49, −0.08) | 0.006 | 88 | |
| Postprandial Glucose (PPG, mmol/L) | ||||||
| Main analysis | Overall | 5 | −0.23 | (−0.69, 0.24) | 0.34 | 95 |
| Maternal Age | <Mean age | 4 | −0.32 | (−0.97, 0.32) | 0.33 | 95 |
| ≥Mean age | 1 | −0.14 | (−0.30, 0.02) | 0.10 | NA | |
| Gestational Age 1 | <28 weeks | 2 | 0.18 | (−0.44, 0.81) | 0.57 | 98 |
| ≥28 weeks | 2 | −0.24 | (−0.68, 0.20) | 0.29 | 79 | |
| Weight (pre-pregnancy) (kg/m2) | Normal weight (<25) | 2 | −0.24 | (−0.68, 0.20 | 0.29 | 79 |
| Overweight (≥25) | 3 | −0.25 | (−0.92, 0.42) | 0.46 | 97 | |
| Diagnostic Criteria for GDM | ADA | 1 | −2.5 | (−3.81, −1.19) | 0.0007 | NA |
| Other | 4 | −0.02 | (−0.46, 0.42) | 0.93 | 96 | |
| Geographic Region | Western country | 2 | 0.18 | (−0.44, 0.81) | 0.57 | 98 |
| Non-western country | 3 | −0.63 | (−1.33, 0.06) | 0.07 | 88 | |
| Study Duration | Acute | 1 | 0.50 | (0.39, 0.61) | <0.0001 | NA |
| Longitudinal | 4 | −0.36 | (−0.73, 0.02) | 0.06 | 82 | |
| Glycated haemoglobin (HbA1c, %) | ||||||
| Main analysis | Overall | 4 | −0.08 | (−0.23, 0.08) | 0.34 | 70 |
| Maternal Age | <Mean age | 3 | −0.11 | (−0.34, 0.12) | 0.33 | 80 |
| ≥Mean age | 1 | 0.00 | (−0.20, 0.20) | 1 | NA | |
| Gestational Age 1 | <28 weeks | 1 | −0.20 | (−0.64, 0.24) | 0.356 | NA |
| ≥28 weeks | 2 | −0.03 | (−0.21, 0.15) | 0.71 | 0 | |
| Weight (pre-pregnancy) (kg/m2) | Normal weight (<25) | 2 | 0.03 | (−0.03, 0.09) | 0.35 | 0 |
| Overweight (≥25) | 2 | −0.24 | (−0.40, −0.08) | 0.003 | 0 | |
| Diagnostic Criteria for GDM 2 | ADA | 1 | −0.25 | (−0.42, −0.07) | 0.007 | NA |
| Other | 2 | 0.03 | (−0.03, 0.09) | 0.35 | 0 | |
| Geographic Region | Western country | 2 | −0.03 | (−0.21, 0.15) | 0.71 | 0 |
| Non-western country | 2 | −0.10 | (−0.37, 0.18) | 0.48 | 89 | |
| HOMA-IR | ||||||
| Main analysis | Overall | 5 | −1.15 | (−2.12, −0.17) | 0.02 | 94 |
| Maternal Age | <Mean age | 3 | −1.94 | (−2.33, −1.56) | <0.0001 | 0 |
| ≥Mean age | 2 | −0.06 | (−0.30, 0.19) | 0.66 | 0 | |
| Gestational Age | <28 weeks | 1 | −1.9 | (−2.36, −1.44) | <0.0001 | NA |
| ≥28 weeks | 4 | −0.91 | (−1.84, 0.02) | 0.05 | 90 | |
| Weight (pre-pregnancy) (kg/m2) | Normal weight (<25) | 2 | −1.00 | (−2.86, 0.86) | 0.29 | 93 |
| Overweight (≥25) | 3 | −1.27 | (−2.77, 0.22) | 0.10 | 94 | |
| Diagnostic Criteria for GDM | ADA | 2 | −1.92 | (−2.33, −1.51) | <0.0001 | 0 |
| Other | 3 | −0.54 | (−1.39, 0.31) | 0.22 | 87 | |
| Geographic Region | Western country | 3 | −0.54 | (−1.39, 0.31) | 0.22 | 87 |
| Non-western country | 2 | −1.92 | (−2.33, −1.51) | <0.0001 | 0 | |
| Study Duration | Acute | 1 | 0.10 | (−0.42, 0.62) | 0.699 | NA |
| Longitudinal | 4 | −1.48 | (−2.71, −0.26) | 0.02 | 95 | |
| Category | Outcome Measure | RCTs (n) | MD | 95% CI | p-Value | I2 |
|---|---|---|---|---|---|---|
| Fasting Plasma Glucose (FPG, mmol/L) | ||||||
| Main analysis | Overall | 5 | −0.10 | (−0.20, −0.01) | 0.04 | 0 |
| Maternal Age | <Mean age | 4 | −0.15 | (−0.27, −0.04) | 0.01 | 0 |
| ≥Mean age | 1 | 0.00 | (−0.17, 0.17) | 1.00 | NA | |
| Gestational Age 1 | <28 weeks | 1 | −0.12 | (−0.35, 0.11) | 0.336 | NA |
| ≥28 weeks | 3 | −0.16 | (−0.29, −0.03) | 0.02 | 0 | |
| Weight (pre-pregnancy) (kg/m2) | Normal weight (<25) | 3 | −0.16 | (−0.29, −0.03) | 0.02 | 0 |
| Overweight (≥25) | 2 | −0.04 | (−0.18, 0.10) | 0.56 | 0 | |
| Diagnostic Criteria for GDM | 75 g OGTT | 2 | −0.08 | (−0.24, 0.09) | 0.37 | 40 |
| Other | 3 | −0.12 | (−0.16, −0.07) | 0.17 | 36 | |
| Postprandial Glucose (PPG, mmol/L) | ||||||
| Main analysis | Overall | 4 | −0.24 | (−0.59, 0.12) | 0.17 | 82 |
| Maternal Age | <Mean age | 3 | −0.39 | (−0.71, −0.07) | 0.02 | 70 |
| ≥Mean age | 1 | 0.20 | (−0.08, 0.48) | 0.161 | NA | |
| Gestational Age 1 | <28 weeks | 1 | −0.64 | (−0.94, −0.34) | 0.0002 | NA |
| ≥28 weeks | 2 | −0.21 | (−0.39, −0.03) | 0.02 | 0 | |
| Weight (pre-pregnancy) (kg/m2) | Normal weight (<25) | 2 | −0.21 | (−0.39, −0.03) | 0.02 | 0 |
| Overweight (≥25) | 2 | −0.22 | (−1.04, 0.60) | 0.60 | 94 | |
| Diagnostic Criteria for GDM | 75 g OGTT | 2 | 0.00 | (−0.38, 0.37) | 0.98 | 79 |
| Other | 2 | −0.58 | (−0.83, −0.32) | <0.0001 | 0 | |
| Glycated haemoglobin (HbA1c, %) | ||||||
| Main analysis | Overall | 3 | 0.04 | (−0.19, 0.27) | 0.73 | 56 |
| Maternal Age | <Mean age | 1 | −0.10 | (−0.32, 0.12) | 0.377 | NA |
| ≥Mean age | 2 | 0.38 | (−0.56, 1.31) | 0.43 | 50 | |
| Weight (pre-pregnancy) 2 (kg/m2) | Normal weight (<25) | 1 | 0.1 | (−0.03, 0.23) | 0.12 | NA |
| Overweight (≥25) | 1 | −0.10 | (−0.32, 0.12) | 0.377 | NA | |
| Geographic Region | Western country | 2 | 0.02 | (−0.17, 0.21) | 0.83 | 59 |
| Non-western country | 1 | 1.2 | (−0.32, 2.72) | 0.130 | NA | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dingena, C.F.; Arofikina, D.; Campbell, M.D.; Holmes, M.J.; Scott, E.M.; Zulyniak, M.A. Nutritional and Exercise-Focused Lifestyle Interventions and Glycemic Control in Women with Diabetes in Pregnancy: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Nutrients 2023, 15, 323. https://doi.org/10.3390/nu15020323
Dingena CF, Arofikina D, Campbell MD, Holmes MJ, Scott EM, Zulyniak MA. Nutritional and Exercise-Focused Lifestyle Interventions and Glycemic Control in Women with Diabetes in Pregnancy: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Nutrients. 2023; 15(2):323. https://doi.org/10.3390/nu15020323
Chicago/Turabian StyleDingena, Cassy F., Daria Arofikina, Matthew D. Campbell, Melvin J. Holmes, Eleanor M. Scott, and Michael A. Zulyniak. 2023. "Nutritional and Exercise-Focused Lifestyle Interventions and Glycemic Control in Women with Diabetes in Pregnancy: A Systematic Review and Meta-Analysis of Randomized Clinical Trials" Nutrients 15, no. 2: 323. https://doi.org/10.3390/nu15020323
APA StyleDingena, C. F., Arofikina, D., Campbell, M. D., Holmes, M. J., Scott, E. M., & Zulyniak, M. A. (2023). Nutritional and Exercise-Focused Lifestyle Interventions and Glycemic Control in Women with Diabetes in Pregnancy: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Nutrients, 15(2), 323. https://doi.org/10.3390/nu15020323





