Adherence to Mediterranean Diet Is Associated with Multiple Sclerosis Severity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Food Frequency Questionnaire
2.2. Medi-Lite Score
2.3. EDSS and MSSS
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bach-Faig, A.; Berry, E.M.; Lairon, D.; Reguant, J.; Trichopoulou, A.; Dernini, S.; Medina, F.X.; Battino, M.; Belahsen, R.; Miranda, G.; et al. Mediterranean Diet Foundation Expert Group Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr. 2011, 14, 2274–2284. [Google Scholar] [CrossRef] [PubMed]
- Sotos-Prieto, M.; Del Rio, D.; Drescher, G.; Estruch, R.; Hanson, C.; Harlan, T.; Hu, F.B.; Loi, M.; McClung, J.P.; Mojica, A.; et al. Mediterranean diet—Promotion and dissemination of healthy eating: Proceedings of an exploratory seminar at the Radcliffe institute for advanced study. Int. J. Food Sci. Nutr. 2022, 73, 158–171. [Google Scholar] [CrossRef] [PubMed]
- Esposito, S.; Sparaco, M.; Maniscalco, G.T.; Signoriello, E.; Lanzillo, R.; Russo, C.; Carmisciano, L.; Cepparulo, S.; Lavorgna, L.; Gallo, A.; et al. Lifestyle and Mediterranean diet adherence in a cohort of Southern Italian patients with Multiple Sclerosis. Mult. Scler. Relat. Disord. 2021, 47, 102636. [Google Scholar] [CrossRef] [PubMed]
- Flachenecker, P.; Stuke, K. National MS registries. J. Neurol. 2008, 255 (Suppl. S6), 102–108. [Google Scholar] [CrossRef] [PubMed]
- Compston, A.; Coles, A. Multiple sclerosis. Lancet 2002, 359, 1221–1231. [Google Scholar] [CrossRef] [PubMed]
- Tafti, D.; Ehsan, M.; Xixis, K.L. Multiple Sclerosis; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Tsunoda, I.; Fujinami, R.S. Inside-Out versus Outside-In models for virus induced demyelination: Axonal damage triggering demyelination. Springer Semin. Immunopathol. 2002, 24, 105–125. [Google Scholar] [CrossRef]
- International Multiple Sclerosis Genetics Consortium; Wellcome Trust Case Control Consortium, 2; Sawcer, S.; Hellenthal, G.; Pirinen, M.; Spencer, C.C.A.; Patsopoulos, N.A.; Moutsianas, L.; Dilthey, A.; Su, Z.; et al. Genetic risk and a primary role for cell-mediated immune mechanisms in multiple sclerosis. Nature 2011, 476, 214–219. [Google Scholar] [CrossRef]
- Waubant, E.; Lucas, R.; Mowry, E.; Graves, J.; Olsson, T.; Alfredsson, L.; Langer-Gould, A. Environmental and genetic risk factors for MS: An integrated review. Ann. Clin. Transl. Neurol. 2019, 6, 1905–1922. [Google Scholar] [CrossRef]
- Wahls, T.L. Dietary Approaches to Treating Multiple Sclerosis-Related Symptoms. Phys. Med. Rehabil. Clin. North Am. 2022, 33, 605–620. [Google Scholar] [CrossRef]
- Katz Sand, I. The role of diet in multiple sclerosis: Mechanistic connections and current evidence. Curr. Nutr. Rep. 2018, 7, 150–160. [Google Scholar] [CrossRef]
- Keykhaei, F.; Norouzy, S.; Froughipour, M.; Nematy, M.; Saeidi, M.; Jarahi, L.; Amiri, F.; Malek Ahmadi, M.; Norouzy, A. Adherence to healthy dietary pattern is associated with lower risk of multiple sclerosis. J. Cent. Nerv. Syst. Dis. 2022, 14, 11795735221092516. [Google Scholar] [CrossRef] [PubMed]
- Rouzitalab, T.; Shivappa, N.; Daneshzad, E.; Izadi, A.; Sanoobar, M.; Khandouzi, N.; Shiri-Shahsavar, M.R.; Khalili, M. Dietary patterns and risk of multiple sclerosis: Results of a double-center case-control study in Iran. Nutr. Health 2022, 29, 531–539. [Google Scholar] [CrossRef]
- Stoiloudis, P.; Kesidou, E.; Bakirtzis, C.; Sintila, S.-A.; Konstantinidou, N.; Boziki, M.; Grigoriadis, N. The role of diet and interventions on multiple sclerosis: A review. Nutrients 2022, 14, 1150. [Google Scholar] [CrossRef] [PubMed]
- Esposito, S.; Bonavita, S.; Sparaco, M.; Gallo, A.; Tedeschi, G. The role of diet in multiple sclerosis: A review. Nutr. Neurosci. 2018, 21, 377–390. [Google Scholar] [CrossRef] [PubMed]
- Alfredsson, L.; Olsson, T.; Hedström, A.K. Inverse association between Mediterranean diet and risk of multiple sclerosis. Mult. Scler. 2023, 29, 1118–1125. [Google Scholar] [CrossRef]
- Guglielmetti, M.; Grosso, G.; Ferraris, C.; Bergamaschi, R.; Tavazzi, E.; La Malfa, A.; Wahidah, H.A.-Q.; Tagliabue, A. Ultra-processed foods consumption is associated with multiple sclerosis severity. Front. Neurol. 2023, 14, 1086720. [Google Scholar] [CrossRef]
- Riccio, P.; Rossano, R. Diet, gut microbiota, and vitamins D + A in multiple sclerosis. Neurotherapeutics 2018, 15, 75–91. [Google Scholar] [CrossRef]
- Matveeva, O.; Bogie, J.F.J.; Hendriks, J.J.A.; Linker, R.A.; Haghikia, A.; Kleinewietfeld, M. Western lifestyle and immunopathology of multiple sclerosis. Ann. N. Y. Acad. Sci. 2018, 1417, 71–86. [Google Scholar] [CrossRef]
- Black, L.J.; Rowley, C.; Sherriff, J.; Pereira, G.; Ponsonby, A.-L.; Lucas, R.M. A healthy dietary pattern associates with a lower risk of a first clinical diagnosis of central nervous system demyelination. Mult. Scler. 2019, 25, 1514–1525. [Google Scholar] [CrossRef]
- Azary, S.; Schreiner, T.; Graves, J.; Waldman, A.; Belman, A.; Guttman, B.W.; Aaen, G.; Tillema, J.-M.; Mar, S.; Hart, J.; et al. Contribution of dietary intake to relapse rate in early paediatric multiple sclerosis. J. Neurol. Neurosurg. Psychiatr. 2018, 89, 28–33. [Google Scholar] [CrossRef]
- Marventano, S.; Mistretta, A.; Platania, A.; Galvano, F.; Grosso, G. Reliability and relative validity of a food frequency questionnaire for Italian adults living in Sicily, Southern Italy. Int. J. Food Sci. Nutr. 2016, 67, 857–864. [Google Scholar] [CrossRef]
- Sofi, F.; Dinu, M.; Pagliai, G.; Marcucci, R.; Casini, A. Validation of a literature-based adherence score to Mediterranean diet: The MEDI-LITE score. Int. J. Food Sci. Nutr. 2017, 68, 757–762. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Kurtzke, J.F. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983, 33, 1444–1452. [Google Scholar] [CrossRef] [PubMed]
- Roxburgh, R.H.S.R.; Seaman, S.R.; Masterman, T.; Hensiek, A.E.; Sawcer, S.J.; Vukusic, S.; Achiti, I.; Confavreux, C.; Coustans, M.; le Page, E.; et al. Multiple Sclerosis Severity Score: Using disability and disease duration to rate disease severity. Neurology 2005, 64, 1144–1151. [Google Scholar] [CrossRef] [PubMed]
- Charlson, R.; Herbert, J.; Kister, I. Severity grading in multiple sclerosis: A proposal. Int. J. MS Care 2016, 18, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Agriculture. Food Sovereignty and Forests, C. Food and Nutrition—CREA. Available online: https://www.alimentinutrizione.it/sezioni/tabelle-nutrizionali (accessed on 3 August 2023).
- Sofi, F.; Macchi, C.; Abbate, R.; Gensini, G.F.; Casini, A. Mediterranean diet and health status: An updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr. 2014, 17, 2769–2782. [Google Scholar] [CrossRef] [PubMed]
- Matarese, G. The link between obesity and autoimmunity. Science 2023, 379, 1298–1300. [Google Scholar] [CrossRef] [PubMed]
- Stampanoni Bassi, M.; Iezzi, E.; Buttari, F.; Gilio, L.; Simonelli, I.; Carbone, F.; Micillo, T.; De Rosa, V.; Sica, F.; Furlan, R.; et al. Obesity worsens central inflammation and disability in multiple sclerosis. Mult. Scler. 2020, 26, 1237–1246. [Google Scholar] [CrossRef]
- Li, C.; Lin, J.; Yang, T.; Xiao, Y.; Jiang, Q.; Shang, H. Physical activity and risk of multiple sclerosis: A Mendelian randomization study. Front. Immunol. 2022, 13, 872126. [Google Scholar] [CrossRef]
- Wesnes, K.; Myhr, K.-M.; Riise, T.; Cortese, M.; Pugliatti, M.; Boström, I.; Landtblom, A.-M.; Wolfson, C.; Bjørnevik, K. Physical activity is associated with a decreased multiple sclerosis risk: The EnvIMS study. Mult. Scler. 2018, 24, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Ward, M.; Goldman, M.D. Epidemiology and pathophysiology of multiple sclerosis. Continuum 2022, 28, 988–1005. [Google Scholar] [CrossRef] [PubMed]
- Alfredsson, L.; Olsson, T. Lifestyle and environmental factors in multiple sclerosis. Cold Spring Harb. Perspect. Med. 2019, 9, a028944. [Google Scholar] [CrossRef] [PubMed]
- Katz Sand, I.; Levy, S.; Fitzgerald, K.; Sorets, T.; Sumowski, J.F. Mediterranean diet is linked to less objective disability in multiple sclerosis. Mult. Scler. 2023, 29, 248–260. [Google Scholar] [CrossRef] [PubMed]
- Uygun Özel, S.; Bayram, S.; Kılınç, M. The relationship between dietary profile and adherence to the Mediterranean diet with EDSS and quality of life in multiple sclerosis patients: A retrospective cross-sectional study. Nutr. Neurosci. 2023, 18, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Moravejolahkami, A.R.; Paknahad, Z.; Chitsaz, A. Association of dietary patterns with systemic inflammation, quality of life, disease severity, relapse rate, severity of fatigue and anthropometric measurements in MS patients. Nutr. Neurosci. 2020, 23, 920–930. [Google Scholar] [CrossRef]
- Farzinmehr, S.; Hosseini, S.; Kamali, H.; Moghadasi, A.N.; Poursadeghfard, M.; Sharifi, M.H. Association of self-reported adherence to the Mediterranean diet with anthropometric indices, comorbidities, and degree of disability in patients with multiple sclerosis. Mult. Scler. Relat. Disord. 2022, 66, 104060. [Google Scholar] [CrossRef]
- Snetselaar, L.G.; Cheek, J.J.; Fox, S.S.; Healy, H.S.; Schweizer, M.L.; Bao, W.; Kamholz, J.; Titcomb, T.J. Efficacy of Diet on Fatigue and Quality of Life in Multiple Sclerosis: A Systematic Review and Network Meta-analysis of Randomized Trials. Neurology 2023, 100, e357–e366. [Google Scholar] [CrossRef]
- Katz Sand, I.; Benn, E.K.T.; Fabian, M.; Fitzgerald, K.C.; Digga, E.; Deshpande, R.; Miller, A.; Gallo, S.; Arab, L. Randomized-controlled trial of a modified Mediterranean dietary program for multiple sclerosis: A pilot study. Mult. Scler. Relat. Disord. 2019, 36, 101403. [Google Scholar] [CrossRef]
- Bohlouli, J.; Namjoo, I.; Borzoo-Isfahani, M.; Poorbaferani, F.; Moravejolahkami, A.R.; Clark, C.C.T.; Hojjati Kermani, M.A. Modified Mediterranean diet v. traditional Iranian diet: Efficacy of dietary interventions on dietary inflammatory index score, fatigue severity and disability in multiple sclerosis patients. Br. J. Nutr. 2022, 128, 1274–1284. [Google Scholar] [CrossRef]
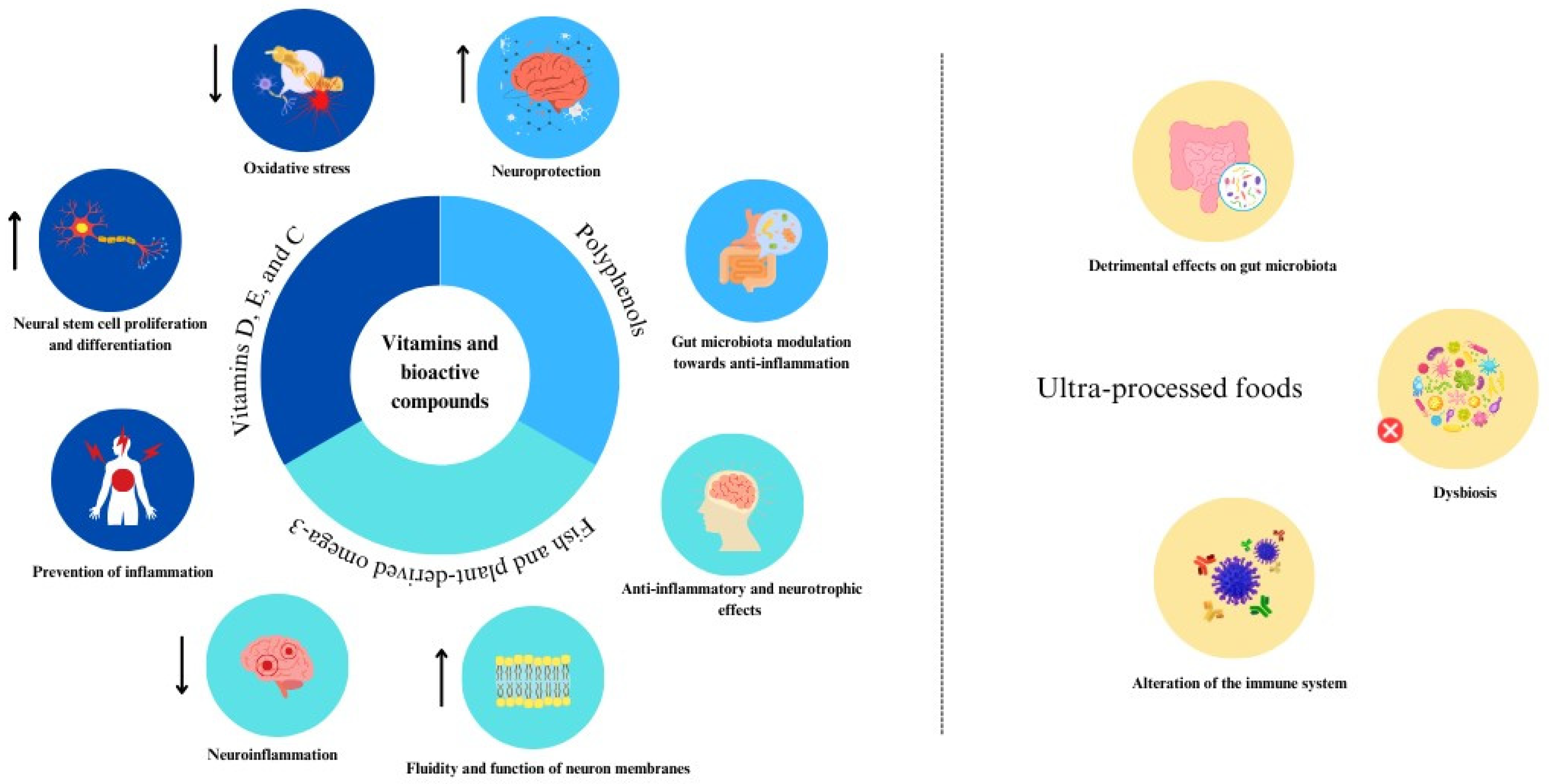
- Kurowska, A.; Ziemichód, W.; Herbet, M.; Piątkowska-Chmiel, I. The role of diet as a modulator of the inflammatory process in the neurological diseases. Nutrients 2023, 15, 1436. [Google Scholar] [CrossRef]
- Di Majo, D.; Cacciabaudo, F.; Accardi, G.; Gambino, G.; Giglia, G.; Ferraro, G.; Candore, G.; Sardo, P. Ketogenic and modified mediterranean diet as a tool to counteract neuroinflammation in multiple sclerosis: Nutritional suggestions. Nutrients 2022, 14, 2384. [Google Scholar] [CrossRef]
- Sangha, A.; Quon, M.; Pfeffer, G.; Orton, S.-M. The role of vitamin D in neuroprotection in multiple sclerosis: An update. Nutrients 2023, 15, 2978. [Google Scholar] [CrossRef]
- Da Cunha Germano, B.C.; de Morais, L.C.C.; Idalina Neta, F.; Fernandes, A.C.L.; Pinheiro, F.I.; do Rego, A.C.M.; Araújo Filho, I.; de Azevedo, E.P.; de Paiva Cavalcanti, J.R.L.; Guzen, F.P.; et al. Vitamin E and its molecular effects in experimental models of neurodegenerative diseases. Int. J. Mol. Sci. 2023, 24, 1191. [Google Scholar] [CrossRef]
- Grosso, G.; Bei, R.; Mistretta, A.; Marventano, S.; Calabrese, G.; Masuelli, L.; Giganti, M.G.; Modesti, A.; Galvano, F.; Gazzolo, D. Effects of vitamin C on health: A review of evidence. Front. Biosci. 2013, 18, 1017–1029. [Google Scholar] [CrossRef]
- Caruso, G.; Torrisi, S.A.; Mogavero, M.P.; Currenti, W.; Castellano, S.; Godos, J.; Ferri, R.; Galvano, F.; Leggio, G.M.; Grosso, G.; et al. Polyphenols and neuroprotection: Therapeutic implications for cognitive decline. Pharmacol. Ther. 2022, 232, 108013. [Google Scholar] [CrossRef]
- Annunziata, G.; Sureda, A.; Orhan, I.E.; Battino, M.; Arnone, A.; Jiménez-García, M.; Capó, X.; Cabot, J.; Sanadgol, N.; Giampieri, F.; et al. The neuroprotective effects of polyphenols, their role in innate immunity and the interplay with the microbiota. Neurosci. Biobehav. Rev. 2021, 128, 437–453. [Google Scholar] [CrossRef] [PubMed]
- Parolini, C. Marine n-3 polyunsaturated fatty acids: Efficacy on inflammatory-based disorders. Life Sci. 2020, 263, 118591. [Google Scholar] [CrossRef]
- Grosso, G.; Galvano, F.; Marventano, S.; Malaguarnera, M.; Bucolo, C.; Drago, F.; Caraci, F. Omega-3 fatty acids and depression: Scientific evidence and biological mechanisms. Oxid. Med. Cell. Longev. 2014, 2014, 313570. [Google Scholar] [CrossRef] [PubMed]
- Zahoor, I.; Giri, S. Specialized Pro-Resolving Lipid Mediators: Emerging Therapeutic Candidates for Multiple Sclerosis. Clin. Rev. Allergy Immunol. 2021, 60, 147–163. [Google Scholar] [CrossRef] [PubMed]
- Dinu, M.; Tristan Asensi, M.; Pagliai, G.; Lotti, S.; Martini, D.; Colombini, B.; Sofi, F. Consumption of Ultra-Processed Foods Is Inversely Associated with Adherence to the Mediterranean Diet: A Cross-Sectional Study. Nutrients 2022, 14, 2073. [Google Scholar] [CrossRef] [PubMed]
- Godos, J.; Giampieri, F.; Al-Qahtani, W.H.; Scazzina, F.; Bonaccio, M.; Grosso, G. Ultra-Processed Food Consumption and Relation with Diet Quality and Mediterranean Diet in Southern Italy. Int. J. Environ. Res. Public Health 2022, 19, 1360. [Google Scholar] [CrossRef] [PubMed]
- Song, Z.; Song, R.; Liu, Y.; Wu, Z.; Zhang, X. Effects of ultra-processed foods on the microbiota-gut-brain axis: The bread-and-butter issue. Food Res. Int. 2023, 167, 112730. [Google Scholar] [CrossRef] [PubMed]
| Medi-Lite Score | ||||
|---|---|---|---|---|
| Low (n = 40) | Medium (n = 38) | High (n = 28) | p-Value | |
| Age, mean (SD) | 49.2 (13.4) | 48.1 (10.3) | 52.2 (11.9) | 0.382 |
| Sex, n (%) | 0.740 | |||
| Men | 16 (40.0) | 12 (31.6) | 10 (35.7) | |
| Women | 24 (60.0) | 26 (68.4) | 18 (64.3) | |
| Smoking status, n (%) | 0.325 | |||
| Non-smokers | 19 (47.5) | 21 (55.3) | 20 (71.4) | |
| Smokers | 10 (25.0) | 7 (18.4) | 5 (17.9) | |
| Ex smokers | 11 (27.5) | 10 (26.3) | 3 (10.7) | |
| Educational level, n (%) | 0.175 | |||
| Low | 10 (25.0) | 3 (7.9) | 6 (21.4) | |
| Moderate | 21 (52.5) | 20 (52.6) | 11 (39.3) | |
| High | 9 (22.5) | 15 (39.5) | 11 (39.3) | |
| Marital status, n (%) | 0.426 | |||
| Unmarried/widowed | 17 (42.5) | 12 (31.6) | 13 (46.4) | |
| Married | 23 (57.5) | 26 (68.4) | 15 (53.6) | |
| Physical activity level, n (%) | 0.235 | |||
| Low | 17 (42.5) | 19 (50.0) | 9 (32.1) | |
| Moderate | 17 (42.5) | 12 (31.6) | 9 (32.1) | |
| High | 6 (15.0) | 7 (18.4) | 10 (35.7) | |
| BMI status, n (%) | 0.485 | |||
| Normal | 29 (72.5) | 27 (71.1) | 15 (53.6) | |
| Overweight | 10 (25.0) | 9 (23.7) | 11 (39.3) | |
| Obese | 1 (2.5) | 2 (5.3) | 2 (7.1) | |
| Current therapy, n (%) | 0.389 | |||
| No | 16 (40.0) | 10 (26.3) | 8 (28.6) | |
| Yes | 24 (60.0) | 28 (73.7) | 20 (71.4) | |
| Therapy type, n (%) | 0.571 | |||
| First line | 17 (70.8) | 22 (78.6) | 16 (84.2) | |
| High potency | 7 (29.2) | 6 (21.4) | 3 (15.8) |
| Medi-Lite Score | ||||
|---|---|---|---|---|
| Low | Medium | High | p-Value | |
| Cereals (g/d) | 148.1 (109.6) | 190.0 (105.5) | 266.2 (73.8) | <0.001 |
| Whole grains (g/d) | 24.4 (48.6) | 63.3 (81.9) | 78.9 (90.4) | 0.008 |
| Vegetables (g/d) | 135.0 (75.0) | 213.8 (93.7) | 338.8 (196.3) | <0.001 |
| Fruit (g/d) | 249.3 (188.9) | 329.8 (226.1) | 590.9 (204.5) | <0.001 |
| Legumes (g/d) | 24.3 (35.6) | 46.8 (51.2) | 50.3 (42.4) | 0.024 |
| Nuts (g/d) | 18.0 (27.7) | 15.4 (18.9) | 23.3 (40.6) | 0.556 |
| Fish (g/d) | 35.5 (30.1) | 46.5 (37.1) | 64.7 (32.4) | 0.003 |
| Eggs (g/d) | 1.1 (1.0) | 1.6 (1.4) | 1.2 (0.9) | 0.126 |
| Red meat (g/d) | 15.5 (17.6) | 17.3 (12.9) | 13.5 (10.6) | 0.572 |
| Processed meat (g/d) | 12.8 (13.3) | 11.4 (10.9) | 10.3 (12.3) | 0.690 |
| Dairy products (g/d) | 225.4 (193.4) | 195.1 (151.9) | 221.9 (150.4) | 0.698 |
| Alcohol (g/d) | 7.4 (15.8) | 0.7 (1.3) | 6.8 (8.2) | 0.555 |
| Olive oil (g/d) | 6.6 (3.5) | 8.9 (2.1) | 8.4 (2.4) | 0.001 |
| Medi-Lite Score | ||||
|---|---|---|---|---|
| Low | Medium | High | p-Value | |
| Energy intake (kcal/d) | 1596.0 (489.3) | 2005.1 (602.2) | 2322.5 (496.2) | <0.001 |
| Energy intake (kJ/d) | 6488.3 (2076.3) | 8123.3 (2569.7) | 9458.7 (2051.0) | <0.001 |
| Protein (g/d) | 63.5 (20.7) | 80.6 (28.2) | 94.2 (22.5) | <0.001 |
| Fat (g/d) | 55.1 (21.2) | 68.6 (26.5) | 67.9 (24.8) | 0.027 |
| Cholesterol (mg/d) | 150.5 (83.7) | 169.9 (95.9) | 168.5 (64.5) | 0.535 |
| Saturated fatty acids (%) | 22.2 (10.7) | 26.5 (14.3) | 25.8 (10.6) | 0.256 |
| MUFA (%) | 22.8 (8.3) | 28.7 (9.3) | 28.5 (9.4) | 0.007 |
| PUFA (%) | 9.2 (4.1) | 11.9 (4.9) | 12.7 (5.4) | 0.006 |
| Carbohydrates (g/d) | 219.0 (80.8) | 276.5 (84.5) | 350.1 (73.0) | <0.001 |
| Total fiber (g/d) | 20.1 (8.4) | 30.8 (10.5) | 41.2 (13.4) | <0.001 |
| Vitamin A retinol eq (μg/d) | 642.3 (247.3) | 870.8 (264.3) | 1230.2 (520.6) | <0.001 |
| Vitamin C (mg/d) | 115.3 (49.1) | 167.3 (89.8) | 238.6 (97.1) | <0.001 |
| Vitamin E (mg/d) | 6.8 (2.7) | 9.1 (2.8) | 10.9 (3.8) | <0.001 |
| Vitamin D (μg/d) | 3.2 (2.8) | 4.2 (3.5) | 5.1 (2.9) | 0.053 |
| Vitamin B12 (μg/d) | 4.4 (2.2) | 5.2 (2.9) | 5.9 (3.0) | 0.067 |
| Thiamin (mg/d) | 1.3 (0.6) | 1.8 (0.6) | 2.2 (1.0) | <0.001 |
| Riboflavin (mg/d) | 1.7 (0.8) | 2.1 (0.8) | 2.7 (1.0) | <0.001 |
| Niacin (mg/d) | 16.3 (4.9) | 21.3 (5.9) | 26.5 (7.0) | <0.001 |
| Pyridoxine (mg/d) | 1277.6 (393.0) | 1478.4 (418.2) | 1456.2 (449.1) | 0.076 |
| Vitamin B9 (μg/d) | 264.9 (84.7) | 388.2 (126.3) | 506.2 (184.0) | <0.001 |
| Sodium (mg/d) | 1872.9 (782.7) | 2303.2 (832.0) | 2457.9 (541.7) | 0.004 |
| Potassium (mg/d) | 2644.3 (798.6) | 3517.7 (994.7) | 4632.7 (1373.6) | <0.001 |
| Iron (mg/d) | 10.3 (3.6) | 15.0 (4.6) | 18.7 (5.6) | <0.001 |
| Calcium (mg/d) | 698.8 (341.1) | 841.6 (496.2) | 989.5 (326.5) | 0.015 |
| Phosphorus (mg/d) | 1070.9 (374.2) | 1365.7 (486.8) | 1634.0 (465.5) | <0.001 |
| Magnesium (mg/d) | 296.6 (97.0) | 407.0 (118.4) | 515.6 (148.8) | <0.001 |
| Zinc (mg/d) | 8.5 (2.7) | 11.2 (3.8) | 13.9 (3.8) | <0.001 |
| Copper (mg/d) | 1.5 (0.5) | 2.1 (0.7) | 2.6 (0.9) | <0.001 |
| Selenium (μg/d) | 74.6 (35.8) | 100.4 (39.2) | 121.2 (25.7) | <0.001 |
| Mild-to-Moderate Multiple Sclerosis, OR (95% C.I.) | |||
|---|---|---|---|
| Low | Medium | High | |
| Mediterranean diet adherence | |||
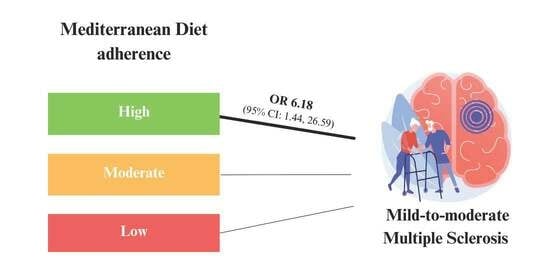
| Model 1 * | 1 | 2.83 (1.03, 7.75) | 5.28 (1.58, 17.69) |
| Model 2 ** | 1 | 3.12 (0.97, 10.01) | 6.18 (1.44, 26.59) |
| Mild-to-Moderate Multiple Sclerosis, OR (95% C.I.) | |
|---|---|
| Mediterranean diet components | |
| Fruit (>1 serv/d, 150 g/d) | 0.95 (0.18, 4.92) |
| Vegetable (>1 serv/d, 100 g/d) | 0.38 (0.11, 1.39) |
| Legume (>1 serv/w, 70 g/w) | 1.98 (0.69, 5.76) |
| Cereals (>1 serv/d, 130 g/d) | 1.30 (0.53, 3.14) |
| Fish (>1 serv/w, 100 g/w) | 1.36 (0.28, 6.66) |
| Meat (<1.5 serv/d, 120 g/d) | 1.30 (0.38, 4.41) |
| Dairy products (<1 serv/d, 180 g/d) | 0.47 (0.20, 1.11) |
| Alcohol (1–2 AU/d, 12 g/d) | 0.51 (0.29, 9.31) |
| Olive oil (>1 portion/d, 5 g/d) | 2.05 (0.35, 11.72) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guglielmetti, M.; Al-Qahtani, W.H.; Ferraris, C.; Grosso, G.; Fiorini, S.; Tavazzi, E.; Greco, G.; La Malfa, A.; Bergamaschi, R.; Tagliabue, A. Adherence to Mediterranean Diet Is Associated with Multiple Sclerosis Severity. Nutrients 2023, 15, 4009. https://doi.org/10.3390/nu15184009
Guglielmetti M, Al-Qahtani WH, Ferraris C, Grosso G, Fiorini S, Tavazzi E, Greco G, La Malfa A, Bergamaschi R, Tagliabue A. Adherence to Mediterranean Diet Is Associated with Multiple Sclerosis Severity. Nutrients. 2023; 15(18):4009. https://doi.org/10.3390/nu15184009
Chicago/Turabian StyleGuglielmetti, Monica, Wahidah H. Al-Qahtani, Cinzia Ferraris, Giuseppe Grosso, Simona Fiorini, Eleonora Tavazzi, Giacomo Greco, Alessandro La Malfa, Roberto Bergamaschi, and Anna Tagliabue. 2023. "Adherence to Mediterranean Diet Is Associated with Multiple Sclerosis Severity" Nutrients 15, no. 18: 4009. https://doi.org/10.3390/nu15184009