Risk Factors for Food Insecurity among Older Adults in India: Study Based on LASI, 2017–2018
Abstract
:1. Introduction
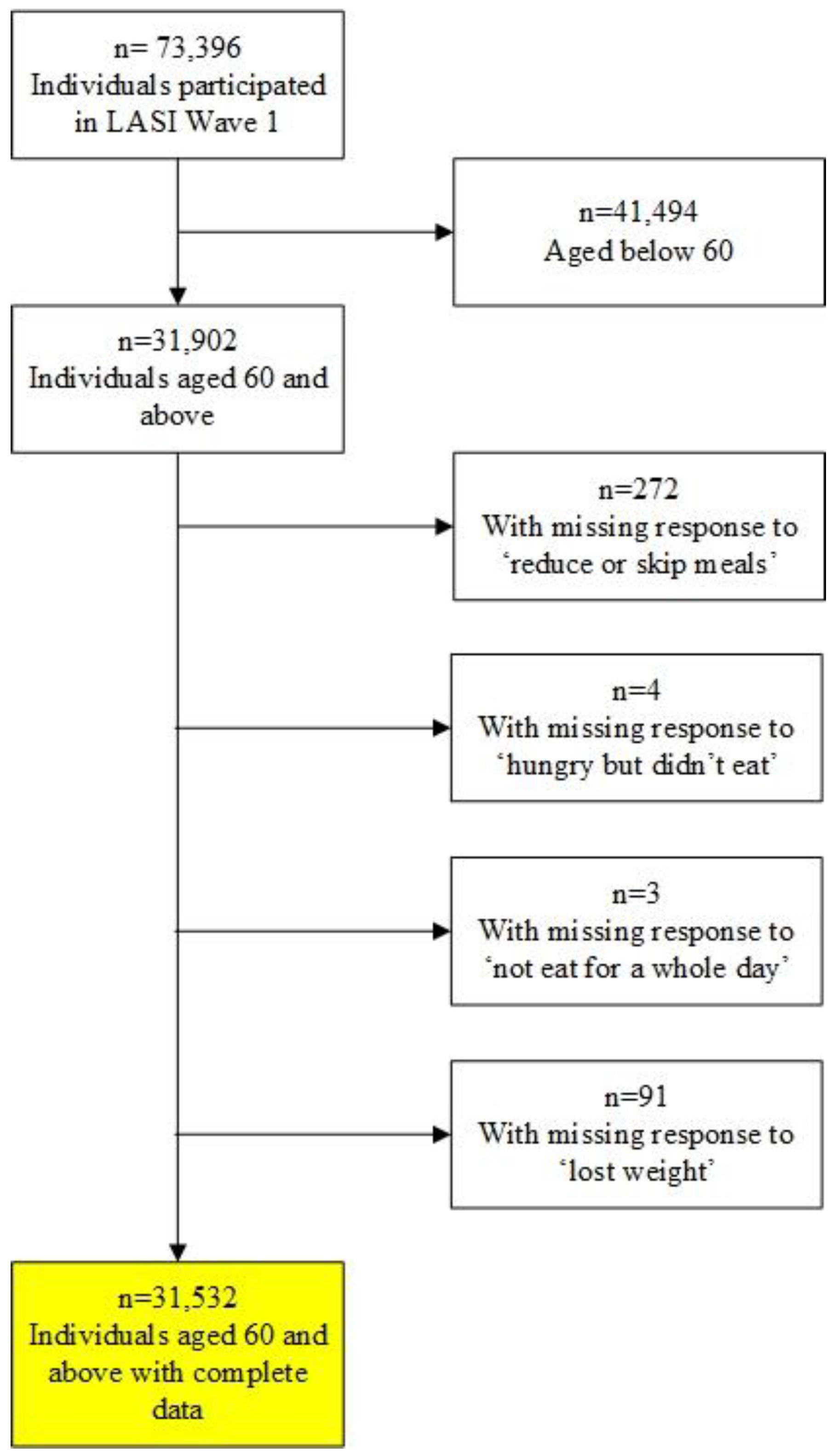
2. Materials and Methods
2.1. Study Design and Sample
2.2. Measures
2.2.1. Outcome Variable
- In the last 12 months, did you reduce the size of your meals or skip meals because there was not enough food at your household?
- In the last 12 months, were you hungry but didn’t eat because there was not enough food at your household?
- In the past 12 months, did you ever not eat for a whole day because there was not enough food at your household?
- Do you think that you have lost weight in the last 12 months because there was not enough food in your household?
2.2.2. Independent Variables
2.3. Statistical Analysis
3. Results
3.1. General Characteristics of the Study Population
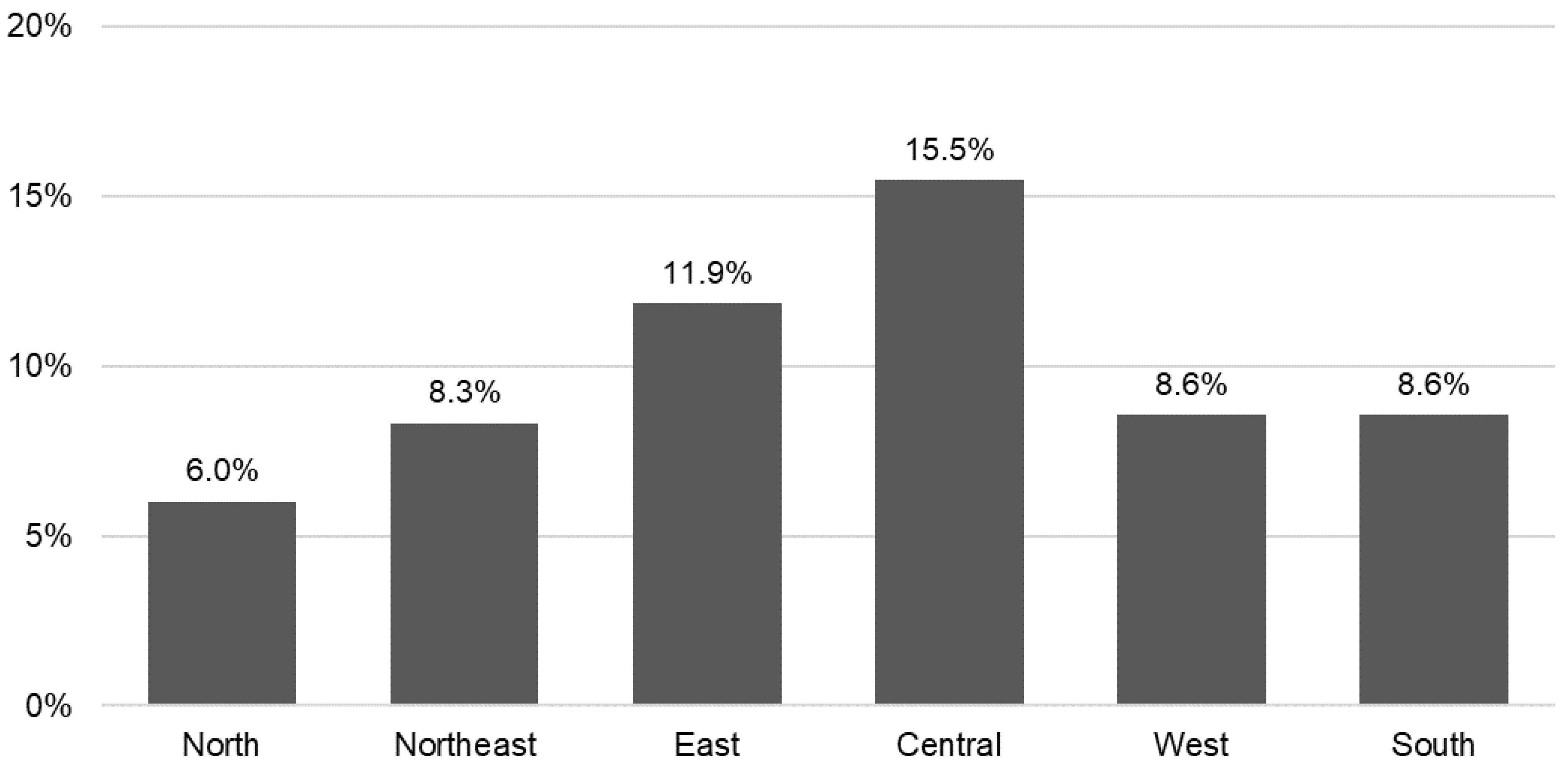
3.2. Prevalence of Food Insecurity and Variation by Region
3.3. Multivariate Regression Results
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Food and Agriculture Organization of the United Nations. Hunger and Food Insecurity; FAO: Rome, Italy, 2023; Available online: https://www.fao.org/hunger/en/ (accessed on 1 July 2023).
- Miguel, E.D.S.; Lopes, S.O.; Araujo, S.P.; Priore, S.E.; Alfenas, R.D.; Hermsdorff, H.H. Association between food insecurity and cardiometabolic risk in adults and the elderly: A systematic review. J. Glob. Health 2020, 10, 020402. [Google Scholar] [CrossRef] [PubMed]
- Morales, M.E.; Berkowitz, S.A. The relationship between food insecurity, dietary patterns, and obesity. Curr. Nutr. Rep. 2016, 5, 54–60. [Google Scholar] [CrossRef]
- Kandapan, B.; Pradhan, I.; Pradhan, J. Food insecurity and malnutrition among Indian older adults: Findings from longitudinal ageing study in India, 2017–18. J. Popul. Ageing. 2022, Aug 3, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Moradi, S.; Mirzababaei, A.; Dadfarma, A.; Rezaei, S.; Mohammadi, H.; Jannat, B.; Mirzaei, K. Food insecurity and adult weight abnormality risk: A systematic review and meta-analysis. Eur. J. Nutr. 2019, 58, 45–61. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Eicher-Miller, H.A. Food insecurity and cardiovascular disease risk. Curr. Atheroscler. Rep. 2021, 23, 1–12. [Google Scholar] [CrossRef]
- Mendy, V.L.; Vargas, R.; Cannon-Smith, G.; Payton, M.; Enkhmaa, B.; Zhang, L. Food insecurity and cardiovascular disease risk factors among Mississippi adults. Int. J. Environ. Res. Public Health 2018, 15, 2016. [Google Scholar] [CrossRef]
- Beltran, S.; Pharel, M.; Montgomery, C.T.; Lopez-Hinojosa, I.J.; Arenas, D.J.; Delisser, H.M. Food insecurity and hypertension: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0241628. [Google Scholar] [CrossRef]
- Abdurahman, A.A.; Chaka, E.E.; Nedjat, S.; Dorosty, A.R.; Majdzadeh, R. The association of household food insecurity with the risk of type 2 diabetes mellitus in adults: A systematic review and meta-analysis. Eur. J. Nutr. 2019, 58, 1341–1350. [Google Scholar] [CrossRef]
- Vaccaro, J.A.; Huffman, F.G. Sex and race/ethnic disparities in food security and chronic diseases in U.S. older adults. Gerontol. Geriatr. Med. 2017, 3, 2333721417718344. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Zepeda, M.U.; Castrejón-Pérez, R.C.; Wynne-Bannister, E.; García-Peña, C. Frailty and food insecurity in older adults. Public Health Nutr. 2016, 19, 2844–2849. [Google Scholar] [CrossRef]
- Chaudhary, M. Association of food insecurity with frailty among older adults in India. J. Public Health 2018, 26, 321–330. [Google Scholar] [CrossRef]
- Muhammad, T.; Saravanakumar, P.; Sharma, A.; Srivastava, S.; Irshad, C.V. Association of food insecurity with physical frailty among older adults: Study based on LASI, 2017–18. Arch. Gerontol. Geriatr. 2022, 103, 104762. [Google Scholar] [CrossRef]
- Arenas, D.J.; Thomas, A.; Wang, J.; DeLisser, H.M. A systematic review and meta-analysis of depression, anxiety, and sleep disorders in US adults with food insecurity. J. Gen. Intern. Med. 2019, 34, 2874–2882. [Google Scholar] [CrossRef]
- Pourmotabbed, A.; Moradi, S.; Babaei, A.; Ghavami, A.; Mohammadi, H.; Jalili, C.; Symonda, M.E.; Miraghajani, M. Food insecurity and mental health: A systematic review and meta-analysis. Public Health Nutr. 2020, 23, 1778–1790. [Google Scholar] [CrossRef] [PubMed]
- Frongillo, E.A.; Nguyen, H.T.; Smith, M.D.; Coleman-Jensen, A. Food insecurity is associated with subjective well-being among individuals from 138 countries in the 2014 Gallup World Poll. J. Nutr. 2017, 147, 680–687. [Google Scholar] [CrossRef] [PubMed]
- Pengpid, S.; Peltzer, K. Food insecurity and health outcomes among community-dwelling middle-aged and older adults in India. Sci. Rep. 2023, 13, 1136. [Google Scholar] [CrossRef]
- Kumar, S.; Bansal, A.; Shri, N.; Nath, N.J.; Dosaya, D. Effect of food insecurity on the cognitive problems among elderly in India. BMC Geriatr. 2021, 21, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Koyanagi, A.; Veronese, N.; Stubbs, B.; Vancampfort, D.; Stickley, A.; Oh, H.; Shin, J.I.; Jackson, S.; Smith, L.; Lara, E. Food insecurity is associated with mild cognitive impairment among middle-aged and older adults in South Africa: Findings from a nationally representative survey. Nutrients 2019, 11, 749. [Google Scholar] [CrossRef]
- Lee, J.S.; Frongillo, E.A., Jr. Factors associated with food insecurity among US elderly persons: Importance of functional impairments. J. Gerontol. B Psychol. Sci. Soc. Sci. 2001, 56, S94–S99. [Google Scholar] [CrossRef]
- Vilar-Compte, M.; Martinez-Martinez, O.; Orta-Aleman, D.; Perez-Escamilla, R. Functional limitations, depression, and cash assistance are associated with food insecurity among older urban adults in Mexico City. J. Health Care Poor Underserved 2016, 27, 1537–1554. [Google Scholar] [CrossRef]
- Bishop, N.J.; Wang, K. Food insecurity, comorbidity, and mobility limitations among older US adults: Findings from the Health and Retirement Study and Health Care and Nutrition Study. Prev. Med. 2018, 114, 180–187. [Google Scholar] [CrossRef]
- Quine, S.; Morrell, S. Food insecurity in community-dwelling older Australians. Public Health Nutr. 2016, 9, 219–224. [Google Scholar] [CrossRef]
- Jih, J.; Stijacic-Cenzer, I.; Seligman, H.K.; Boscardin, W.J.; Nguyen, T.T.; Ritchie, C.S. Chronic disease burden predicts food insecurity among older adults. Public Health Nutr. 2018, 21, 1737–1742. [Google Scholar] [CrossRef]
- Kim, K.; Kim, M.K.; Shin, Y.J.; Lee, S.S. Factors related to household food insecurity in the Republic of Korea. Public Health Nutr. 2011, 14, 1080–1087. [Google Scholar] [CrossRef]
- Burris, M.; Kihlstrom, L.; Arce, K.S.; Prendergast, K.; Dobbins, J.; McGrath, E.; Renda, A.; Shannon, E.; Cordier, T.; Song, Y.; et al. Food insecurity, loneliness, and social support among older adults. J. Hunger Environ. 2021, 16, 29–44. [Google Scholar] [CrossRef]
- Meza-Valderrama, D.; Marco, E.; Davalos-Yerovi, V.; Muns, M.D.; Tejero-Sanchez, M.; Duarte, E.; Sanchez-Rodriguez, D. Sarcopenia, malnutrition, and cachexia: Adapting definitions and terminology of nutritional disorders in older people with cancer. Nutrients 2021, 13, 761. [Google Scholar] [CrossRef]
- Corcoran, C.; Murphy, C.; Culligan, E.P.; Walton, J.; Sleator, R.D. Malnutrition in the elderly. Sci Prog. 2019, 102, 171–180. [Google Scholar] [CrossRef]
- United Nations. UN DESA Policy Brief No. 153: India Overtakes China as the World’s Most Populous Country; United Nations: New York, NY, USA, 2023; Available online: https://www.un.org/development/desa/dpad/publication/un-desa-policy-brief-no-153-india-overtakes-china-as-the-worlds-most-populous-country/ (accessed on 1 July 2023).
- United Nations Department of Economic and Social Affairs, Population Division. World Population Prospects 2022: Summary of Results; UN DESA/POP/2022/TR/NO. 3; United Nations: New York, NY, USA, 2022. [Google Scholar]
- von Grebmer, K.; Bernstein, J.; Wiemers, M.; Reiner, L.; Bachmeier, M.; Hanano, A.; Towey, O.; Cheilleachair, R.N.; Foley, C.; Gitter, S.; et al. 2022 Global Hunger Index: Food Systems Transformation and Local Governance; Deutsche Welthungerhilfe: Dublin, Ireland, 2022. [Google Scholar]
- International Institute of Population Sciences (IIPS); National Programme for Health Care of Elderly (NPHCE); MoHFW, Harvard, T.H. Chan School of Public Health (HSPH); University of Southern California (USC). Longitudinal Ageing Study in India (LASI) Wave 1, 2017–18; India Report; International Institute of Population Sciences (IIPS): Mumbai, India, 2020. [Google Scholar]
- Lee, J.S.; Johnson, M.A.; Brown, A.; Nord, M. Food security of older adults requesting older Americans act nutrition program in Georgia can be validly measured using a short form of the U.S. household food security survey module. J. Nutr. 2011, 141, 1362–1368. [Google Scholar] [CrossRef] [PubMed]
- Sethi, V.; Maitra, C.; Avula, R.; Unisa, S.; Bhalla, S. Internal validity and reliability of experience-based household food insecurity scales in Indian settings. Agric. Food Secur. 2017, 6, 21. [Google Scholar] [CrossRef]
- Subramanian, S.V.; Nandy, S.; Irving, M.; Gordon, D.; Smith, G.D. Role of socioeconomic markers and state prohibition policy in predicting alcohol consumption among men and women in India: A multilevel statistical analysis. Bull. World Health Organ. 2005, 83, 829–836. [Google Scholar]
- Savage, R.D.; Wu, W.; Li, J.; Lawson, A.; Bronskill, S.E.; Chamberlain, S.A.; Grieve, J.; Gruneir, A.; Reppas-Rindlisbacher, C.; Stall, N.M.; et al. Loneliness among older adults in the community during COVID-19: A cross-sectional survey in Canada. BMJ Open 2021, 11, e044517. [Google Scholar] [CrossRef]
- Bhuyan, B.; Sahoo, B.K.; Suar, D. Food insecurity dynamics in India: A synthetic panel approach. Soc. Sci. Humanit. Open 2020, 2, 100029. [Google Scholar] [CrossRef]
- World Bank. India States Briefs; The World Bank Group: Washington, DC, USA, 2018; Available online: https://www.worldbank.org/en/news/feature/2016/05/26/india-states-briefs (accessed on 1 July 2023).
- Howe-Burris, M.; Giroux, S.; Waldman, K.; DeBruicker Valliant, J.; Babb, A.; Czebotar, K.; Fobi, D.; Stafford, P.; Knudsen, D.C. The Interactions of Food Security, Health, and Loneliness among Rural Older Adults before and after the Onset of COVID-19. Nutrients 2022, 14, 5076. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Total | Food Insecure | p-Value | |
|---|---|---|---|---|
| No | Yes | |||
| Number of respondents | 31,532 | 28,229 | 3303 | |
| (in %) | (100%) | (89.5%) | (10.5%) | |
| Age groups | 0.657 | |||
| 60–64 | 30.0% | 29.8% | 31.7% | |
| 65–69 | 28.8% | 28.9% | 27.4% | |
| 70–74 | 18.8% | 18.8% | 18.7% | |
| 75–79 | 11.2% | 11.1% | 11.4% | |
| 80 and above | 11.3% | 11.4% | 10.7% | |
| Sex | 0.741 | |||
| Male | 47.2% | 47.2% | 46.7% | |
| Female | 52.8% | 52.8% | 53.3% | |
| Marital status | <0.001 | |||
| Married/cohabiting | 61.9% | 62.5% | 56.7% | |
| Others | 38.1% | 37.5% | 43.3% | |
| Education | <0.001 | |||
| None | 56.8% | 55.3% | 68.9% | |
| Less than primary | 11.5% | 11.4% | 12.7% | |
| Primary | 11.2% | 11.6% | 8.1% | |
| Secondary or higher | 20.5% | 21.7% | 10.3% | |
| Caste | <0.001 | |||
| SC/ST | 27.3% | 26.2% | 36.0% | |
| OBC | 45.3% | 45.6% | 43.3% | |
| No caste/tribe | 27.4% | 28.2% | 20.7% | |
| Place of residence | <0.001 | |||
| Urban | 29.0% | 30.5% | 16.3% | |
| Rural | 71.0% | 69.5% | 83.7% | |
| Region | <0.001 | |||
| North | 12.7% | 13.3% | 7.3% | |
| Northeast | 3.0% | 3.1% | 2.4% | |
| East | 23.7% | 23.3% | 26.8% | |
| Central | 21.2% | 20.0% | 31.3% | |
| West | 17.1% | 17.5% | 14.0% | |
| South | 22.4% | 22.9% | 18.3% | |
| Currently working | <0.001 | |||
| No | 69.2% | 69.7% | 64.6% | |
| Yes | 30.8% | 30.3% | 35.4% | |
| MPCE quintile | <0.001 | |||
| Poorest | 21.8% | 21.0% | 27.8% | |
| Poorer | 21.8% | 21.6% | 23.1% | |
| Middle | 20.7% | 20.9% | 18.3% | |
| Richer | 19.3% | 19.6% | 17.1% | |
| Richest | 16.5% | 16.8% | 13.7% | |
| Receive occupational pension | <0.001 | |||
| No | 94.3% | 93.9% | 97.9% | |
| Yes | 5.7% | 6.1% | 2.1% | |
| Receive financial help | 0.047 | |||
| No | 85.0% | 85.2% | 83.2% | |
| Yes | 15.0% | 14.8% | 16.8% | |
| Childhood SES | <0.001 | |||
| Pretty well off | 8.4% | 8.7% | 6.2% | |
| Average | 48.8% | 50.0% | 39.1% | |
| Poor | 42.7% | 41.4% | 54.7% | |
| Living arrangement | <0.001 | |||
| With spouse | 60.8% | 61.4% | 56.0% | |
| With others (but not spouse) | 33.5% | 33.7% | 32.3% | |
| Live alone | 5.7% | 5.0% | 11.7% | 0.673 |
| Number of children | 3.7 | 3.7 | 3.8 | |
| (SD) | (2.0) | (1.9) | (2.1) | |
| Social isolation | <0.001 | |||
| Not isolated | 85.5% | 86.9% | 73.4% | |
| Isolated | 14.5% | 13.1% | 26.6% | |
| Physical impairment | <0.001 | |||
| No | 94.1% | 94.7% | 89.6% | |
| Yes | 5.9% | 5.3% | 10.4% | |
| ADL limitation | <0.001 | |||
| No | 76.3% | 77.6% | 65.0% | |
| One limitation | 9.6% | 9.1% | 13.9% | |
| 2 or more limitation | 14.2% | 13.4% | 21.1% | |
| Poor self-rated health | <0.001 | |||
| No | 76.3% | 77.6% | 65.8% | |
| Yes | 23.7% | 22.4% | 34.2% | |
| Angina/heart disease | 0.070 | |||
| No | 94.8% | 94.7% | 96.0% | |
| Yes | 5.2% | 5.3% | 4.0% | |
| Arthritis | 0.021 | |||
| No | 80.4% | 80.7% | 77.6% | |
| Yes | 19.6% | 19.3% | 22.4% | |
| Chronic lung disease | 0.156 | |||
| No | 91.5% | 91.7% | 90.2% | |
| Yes | 8.5% | 8.3% | 9.8% | |
| Diabetes | <0.001 | |||
| No | 85.8% | 85.1% | 90.9% | |
| Yes | 14.2% | 14.9% | 9.1% | |
| Hypertension | 0.006 | |||
| No | 67.2% | 66.8% | 70.8% | |
| Yes | 32.8% | 33.2% | 29.2% | |
| Stroke | 0.063 | |||
| No | 97.3% | 97.4% | 96.6% | |
| Yes | 2.7% | 2.6% | 3.4% | |
| Cancer | 0.483 | |||
| No | 99.3% | 99.3% | 99.4% | |
| Yes | 0.7% | 0.7% | 0.6% | |
| OR (95% CI) | ||||
|---|---|---|---|---|
| Variable | Model 1 | Model 2 | Model 3 | Model 4 |
| Age groups: 60–64 (ref.) | ||||
| 65–69 | 0.86 | 0.87 | 0.88 | 0.86 |
| (0.73–1.00) | (0.74–1.02) | (0.75–1.03) | (0.73–1.00) | |
| 70–74 | 0.85 | 0.88 | 0.89 | 0.85 |
| (0.70–1.02) | (0.73–1.06) | (0.74–1.08) | (0.70–1.03) | |
| 75–79 | 0.84 | 0.87 | 0.88 | 0.79 * |
| (0.67–1.05) | (0.69–1.10) | (0.70–1.11) | (0.63–0.99) | |
| 80 and above | 0.71 ** | 0.74 * | 0.77 * | 0.65 *** |
| (0.56–0.89) | (0.58–0.95) | (0.60–0.98) | (0.50–0.83) | |
| Female | 0.80 ** | 0.82 * | 0.80 ** | 0.80 ** |
| (0.69–0.93) | (0.70–0.96) | (0.69–0.94) | (0.69–0.94) | |
| Married/cohabiting | 0.74 *** | 0.74 *** | 0.60 | 0.59 * |
| (0.64–0.86) | (0.64–0.86) | (0.35–1.02) | (0.35–0.99) | |
| Education: None (ref.) | ||||
| Less than primary | 0.96 | 0.98 | 0.97 | 0.96 |
| (0.79–1.17) | (0.80–1.19) | (0.80–1.19) | (0.79–1.18) | |
| Primary | 0.63 *** | 0.67 *** | 0.68 ** | 0.70 ** |
| (0.50–0.80) | (0.53–0.85) | (0.54–0.86) | (0.55–0.87) | |
| Secondary or higher | 0.46 *** | 0.55 *** | 0.54 *** | 0.58 *** |
| (0.37–0.58) | (0.44–0.70) | (0.43–0.68) | (0.47–0.73) | |
| Caste: SC/ST (ref.) | ||||
| OBC | 0.80 ** | 0.83 * | 0.83 * | 0.83 * |
| (0.69–0.92) | (0.71–0.96) | (0.71–0.96) | (0.72–0.97) | |
| No caste/tribe | 0.75 *** | 0.80 * | 0.82 * | 0.82 * |
| (0.63–0.89) | (0.68–0.96) | (0.69–0.98) | (0.69–0.98) | |
| Rural | 1.64 *** | 1.63 *** | 1.58 *** | 1.53 *** |
| (1.42–1.91) | (1.40–1.89) | (1.35–1.84) | (1.31–1.78) | |
| Region: North (ref.) | ||||
| Northeast | 1.36 * | 1.38 * | 1.47 ** | 1.45 ** |
| (1.06–1.75) | (1.07–1.78) | (1.14–1.90) | (1.12–1.87) | |
| East | 1.98 *** | 1.83 *** | 1.84 *** | 1.63 *** |
| (1.66–2.37) | (1.53–2.20) | (1.53–2.20) | (1.35–1.97) | |
| Central | 2.73 *** | 2.60 *** | 2.54 *** | 2.43 *** |
| (2.24–3.32) | (2.12–3.18) | (2.07–3.10) | (1.98–2.98) | |
| West | 1.62 *** | 1.47 ** | 1.48 ** | 1.33 * |
| (1.29–2.04) | (1.17–1.86) | (1.17–1.88) | (1.05–1.69) | |
| South | 1.58 *** | 1.66 *** | 1.47 *** | 1.25 * |
| (1.30–1.93) | (1.36–2.03) | (1.20–1.81) | (1.02–1.54) | |
| Currently working | 1.07 | 1.06 | 1.21* | |
| (0.92–1.25) | (0.91–1.24) | (1.04–1.42) | ||
| MPCE quintile: Poorest (ref.) | ||||
| Poorer | 0.86 | 0.89 | 0.89 | |
| (0.72–1.02) | (0.75–1.07) | (0.75–1.07) | ||
| Middle | 0.77 ** | 0.77 ** | 0.77 ** | |
| (0.64–0.91) | (0.65–0.92) | (0.65–0.92) | ||
| Richer | 0.82 | 0.82 | 0.81 * | |
| (0.67–1.01) | (0.67–1.00) | (0.66–1.00) | ||
| Richest | 0.87 | 0.84 | 0.82 | |
| (0.71–1.07) | (0.68–1.03) | (0.67–1.02) | ||
| Receiving occupational pension | 0.59 ** | 0.59 ** | 0.62 ** | |
| (0.42–0.84) | (0.42–0.84) | (0.43–0.88) | ||
| Receiving financial help | 1.11 | 1.03 | 1.01 | |
| (0.95–1.29) | (0.88–1.21) | (0.86–1.18) | ||
| Childhood SES: Pretty well off (ref.) | ||||
| Average | 0.91 | 0.88 | 0.92 | |
| (0.70–1.19) | (0.68–1.15) | (0.71–1.19) | ||
| Poor | 1.23 | 1.20 | 1.20 | |
| (0.94–1.62) | (0.92–1.58) | (0.92–1.57) | ||
| Living arrangement: With spouse (ref.) | ||||
| With others (but not spouse) | 0.62 | 0.61 | ||
| (0.37–1.06) | (0.37–1.04) | |||
| Living alone | 1.26 | 1.25 | ||
| (0.71–2.24) | (0.71–2.20) | |||
| Number of children | 0.99 | 0.99 | ||
| (0.95–1.02) | (0.95–1.02) | |||
| Socially isolated | 2.27 *** | 2.09 *** | ||
| (1.95–2.63) | (1.80–2.43) | |||
| Has physical impairment | 1.68 *** | |||
| (1.34–2.11) | ||||
| ADL limitation: No (ref.) | ||||
| One limitation | 1.53 *** | |||
| (1.29–1.81) | ||||
| 2 or more limitations | 1.72 *** | |||
| (1.41–2.08) | ||||
| Poor self-rated health | 1.47 *** | |||
| (1.27–1.69) | ||||
| Angina/heart disease | 0.97 | |||
| (0.71–1.32) | ||||
| Arthritis | 1.18 * | |||
| (1.01–1.38) | ||||
| Chronic lung disease | 1.14 | |||
| (0.90–1.44) | ||||
| Diabetes | 0.79 * | |||
| (0.65–0.97) | ||||
| Hypertension | 1.07 | |||
| (0.93–1.24) | ||||
| Stroke | 1.02 | |||
| (0.73–1.43) | ||||
| Cancer | 1.06 | |||
| (0.57–2.00) | ||||
| N (unweighted) | 31,532 | 31,532 | 31,532 | 31,532 |
| R-squared | 0.042 | 0.047 | 0.068 | 0.086 |
| AIC | 2396.08 | 2383.19 | 2331.00 | 2286.85 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fong, J.H. Risk Factors for Food Insecurity among Older Adults in India: Study Based on LASI, 2017–2018. Nutrients 2023, 15, 3794. https://doi.org/10.3390/nu15173794
Fong JH. Risk Factors for Food Insecurity among Older Adults in India: Study Based on LASI, 2017–2018. Nutrients. 2023; 15(17):3794. https://doi.org/10.3390/nu15173794
Chicago/Turabian StyleFong, Joelle H. 2023. "Risk Factors for Food Insecurity among Older Adults in India: Study Based on LASI, 2017–2018" Nutrients 15, no. 17: 3794. https://doi.org/10.3390/nu15173794
APA StyleFong, J. H. (2023). Risk Factors for Food Insecurity among Older Adults in India: Study Based on LASI, 2017–2018. Nutrients, 15(17), 3794. https://doi.org/10.3390/nu15173794






