Cultural and Contextual Drivers of Triple Burden of Malnutrition among Children in India
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measurements
2.2.1. Outcome Variables
2.2.2. Explanatory Variables
2.3. Statistical Analysis
3. Results
3.1. Triple Burden of Malnutrition among under Five Children in India
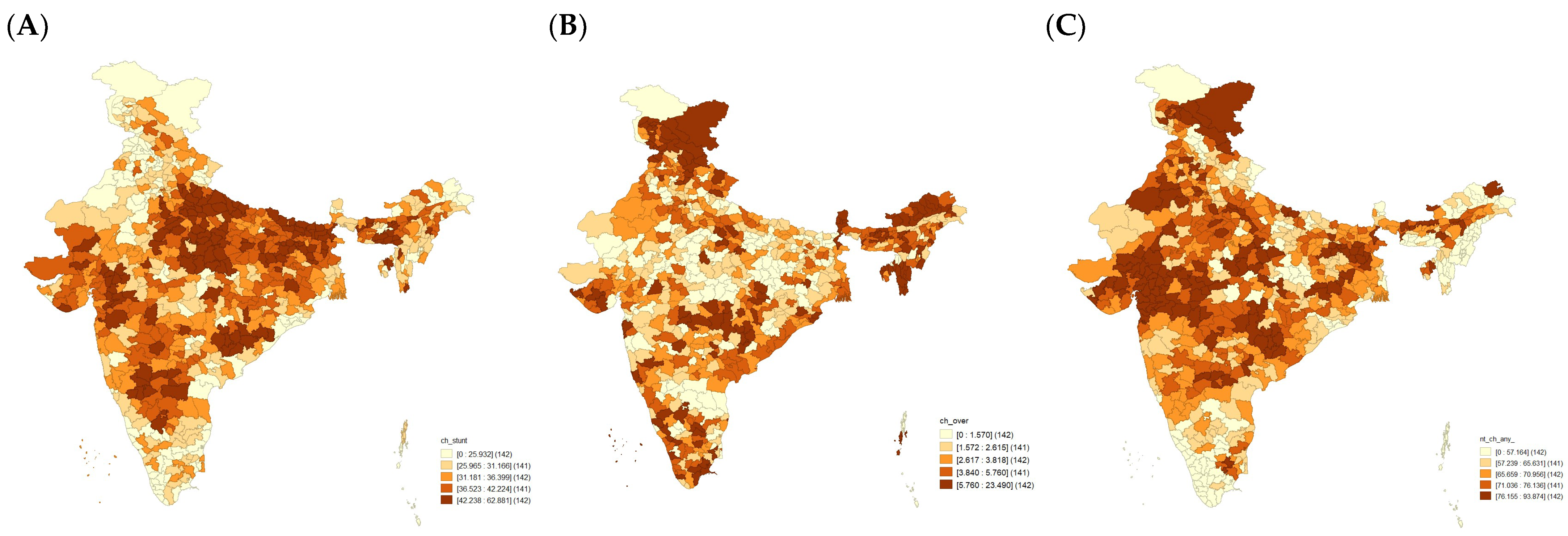
3.2. Spatial Heterogeneity in the Triple Burden of Malnutrition
3.3. Description of the Study Population
3.4. Multi-Level Regression Analysis
4. Discussion
4.1. Possible Mechanism of the Findings
4.2. Policy Implications of These Findings
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Isanaka, S.; Barnhart, D.A.; McDonald, C.M.; Ackatia-Armah, R.S.; Kupka, R.; Doumbia, S.; Brown, K.H.; Menzies, N.A. Cost-effectiveness of communi-ty-based screening and treatment of moderate acute malnutrition in Mali. BMJ Glob. Health 2019, 4, e001227. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davis, J.N.; Oaks, B.M.; Engle-Stone, R. The Double Burden of Malnutrition: A Systematic Review of Operational Definitions. Curr. Dev. Nutr. 2020, 4, nzaa127. [Google Scholar] [CrossRef]
- Mohan, V.; Ranjani, H.; Mehreen, T.; Pradeepa, R.; Anjana, R.M.; Garg, R.; Anand, K. Epidemiology of childhood overweight & obesity in India: A systematic review. Indian J. Med. Res. 2016, 143, 160–174. [Google Scholar] [CrossRef] [Green Version]
- Pelletier, D.L.; Frongillo, E.A. Changes in Child Survival Are Strongly Associated with Changes in Malnutrition in Developing Countries. J. Nutr. 2003, 133, 107–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blankenship, J.L.; Rudert, C.; Aguayo, V.M. Triple trouble: Understanding the burden of child undernutrition, micronutrient deficiencies, and overweight in East Asia and the Pacific. Matern. Child Nutr. 2020, 16, e12950. [Google Scholar] [CrossRef] [PubMed]
- Global Nutrition Report. 2020. Available online: https://www.segeplan.gob.gt/2.0/index.php?option=com_content&view=article&id=472&Itemid=472 (accessed on 10 January 2023).
- de Onis, M.; Blössner, M. The World Health Organization Global Database on Child Growth and Malnutrition: Methodology and applications. Int. J. Epidemiol. 2003, 32, 518–526. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biesalski, H.K. The 1000-Day Window and Cognitive Development. In World Review of Nutrition and Dietetics; Karger International: Basel, Switzerland, 2016; Volume 115, pp. 1–15. [Google Scholar] [CrossRef]
- Mkhize, M.; Sibanda, M. A Review of Selected Studies on the Factors Associated with the Nutrition Status of Children under the Age of Five Years in South Africa. Int. J. Environ. Res. Public Health 2020, 17, 7973. [Google Scholar] [CrossRef]
- Akombi, B.J.; Agho, K.E.; Merom, D.; Renzaho, A.M.; Hall, J.J. Child malnutrition in sub-Saharan Africa: A meta-analysis of demographic and health surveys (2006–2016). PLoS ONE 2017, 12, e0177338. [Google Scholar]
- Gödecke, T.; Stein, A.J.; Qaim, M. The global burden of chronic and hidden hunger: Trends and determinants. Glob. Food Secur. 2018, 17, 21–29. [Google Scholar] [CrossRef]
- Miglioli, T.C.; Fonseca, V.M.; Junior, S.C.G.; Da Silva, K.S.; De Lira, P.I.C.; Filho, M.B.; Gomes, S.C.; Batista, M. Factors associated with the nutritional status of children less than 5 years of age. Rev. Saude Publica 2015, 49, 59. [Google Scholar] [CrossRef] [Green Version]
- Mittal, A.; Singh, J.; Ahluwalia, S. Effect of maternal factors on nutritional status of 1–5-year-old children in urban slum population. Indian J. Community Med. 2007, 32, 264. [Google Scholar] [CrossRef]
- Dey, I.; Chaudhuri, R.N. Gender inequality in nutritional status among under five children in a village in Hooghly district, West Bengal. Indian J. Public Health 2009, 52, 218–220. [Google Scholar]
- Jayant, D.D.; Purushottam, G.A.; Deepak, P.B.; Vaishali, P.D.; Piyush, K.; Aarif, S.M. Socio-cultural practices in relation to breastfeeding, weaning and child rearing among Indian mothers and assessment of nutritional status of children under five in rural India. Australas. Med. J. 2010, 3, 618–624. [Google Scholar]
- Nguyen, P.H.; Scott, S.; Headey, D.; Singh, N.; Tran, L.M.; Menon, P.; Ruel, M.T. The double burden of malnutrition in India: Trends and inequalities (2006–2016). PLoS ONE 2021, 16, e0247856. [Google Scholar] [CrossRef]
- Pomati, M.; Mendoza-Quispe, D.; Anza-Ramirez, C.; Hernández-Vásquez, A.; Larco, R.M.C.; Fernandez, G.; Nandy, S.; Miranda, J.J.; Bernabé-Ortiz, A. Trends and patterns of the double burden of malnutrition (DBM) in Peru: A pooled analysis of 129,159 mother–child dyads. Int. J. Obes. 2021, 45, 609–618. [Google Scholar] [CrossRef] [PubMed]
- Doak, C.M.; Adair, L.S.; Bentley, M.; Monteiro, C.; Popkin, B.M. The dual burden household and the nutrition transition paradox. Int. J. Obes. 2005, 29, 129–136. [Google Scholar] [CrossRef] [Green Version]
- Popkin, B.M.; Corvalan, C.; Grummer-Strawn, L.M. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet 2020, 395, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Longitudinal Ageing Study in India (LASI). India Report National Programme for Health Care of Elderly; International Institute for Population Sciences Ministry of Health & Family Welfare Government of India: Mumbai, India, 2020.
- Alderman, H.; Headey, D.D. How Important is Parental Education for Child Nutrition? World Dev. 2017, 94, 448–464. [Google Scholar] [CrossRef]
- Khan, J.; Mohanty, S.K. Spatial heterogeneity and correlates of child malnutrition in districts of India. BMC Public Health 2018, 18, 1027. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puri, P.; Khan, J.; Shil, A.; Ali, M. A cross-sectional study on selected child health out-comes in India: Quantifying the spatial variations and identification of the parental risk factors. Sci. Rep. 2020, 10, 6645. [Google Scholar]
- Dhingra, S.; Pingali, P.L. Effects of short birth spacing on birth-order differences in child stunting: Evidence from India. Proc. Natl. Acad. Sci. USA 2021, 118, e2017834118. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.S.; Howlader, T.; Masud, M.S. Association of Low-Birth Weight with Malnutrition in Children under Five Years in Bangladesh: Do Mother’ s Education, Socio-Economic Status, and Birth Interval Matter? PLoS ONE 2016, 23, e0157814. [Google Scholar]
- Sk, R.; Banerjee, A.; Rana, J. Nutritional status and concomitant factors of stunting among pre-school children in Malda, India: A micro-level study using a multilevel approach. BMC Public Health 2021, 21, 1690. [Google Scholar] [CrossRef]
- Sserwanja, Q.; Kamara, K.; Mutisya, L.M.; Musaba, M.W.; Ziaei, S. Rural and Urban Correlates of Stunting among under-Five Children in Sierra Leone: A 2019 Nationwide Cross-Sectional Survey. Nutr. Metab. Insights 2021, 14, 11786388211047056. [Google Scholar] [CrossRef]
- Onyeneho, N.G.; Ozumba, B.C.; Subramanian, S.V. Determinants of Childhood Anemia in India. Sci. Rep. 2019, 9, 16540. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moestue, H.; Huttly, S. Adult education and child nutrition: The role of family and community. J. Epidemiol. Community Health 2008, 62, 153–159. [Google Scholar] [CrossRef]
- Nguyen, P.H.; Kachwaha, S.; Tran, L.M.; Sanghvi, T.; Ghosh, S.; Kulkarni, B.; Beesabathuni, K.; Menon, P.; Sethi, V. Maternal Diets in India: Gaps, Barriers, and Opportunities. Nutrients 2021, 13, 3534. [Google Scholar] [CrossRef]
- Singh, S.K.; Taillie, L.S.; Gupta, A.; Bercholz, M.; Popkin, B.; Murukutla, N. Front-of-Package Labels on Unhealthy Pack-aged Foods in India: Evidence from a Randomized Field Experiment. Nutrients 2022, 14, 3128. [Google Scholar] [CrossRef]
- Choudhury, S.; Shankar, B.; Aleksandrowicz, L.; Tak, M.; Dangour, A. Caste-Based Inequality in Fruit and Vegetable Consumption in India. Food Nutr. Bull. 2021, 42, 451–459. [Google Scholar] [CrossRef]
- India NP of National Nutrition Mission. 2018. Available online: https://www.india.gov.in/national-nutrition-mission (accessed on 5 February 2023).
- Champagne, B.; Arora, M.; ElSayed, A.; Løgstrup, S.; Naidoo, P.; Shilton, T.; McGhie, D.V.; Armstrong-Walenczak, K.; Berteletti, F.; Ganesan, S.; et al. World heart federation policy brief: Front-of-pack labelling: Unhealthy changes in the global food system. Glob. Heart 2020, 15, 70. [Google Scholar] [CrossRef]
- Vassilakou, T. Childhood Malnutrition: Time for Action. Children 2021, 8, 103. [Google Scholar] [CrossRef] [PubMed]


| Background Characteristics | Weighted Percentage (N = 198,335) | Stunting, % | Overweight, % | Anaemia, % |
|---|---|---|---|---|
| Child Characteristics | ||||
| Age of children (months) | ||||
| 6–23 | 32.89 | 33.96 | 4.36 | 79.05 |
| 24–35 | 22.08 | 38.16 | 2.50 | 71.81 |
| 36–59 | 45.02 | 37.25 | 2.56 | 58.71 |
| Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | ||
| Sex of child | ||||
| Male | 51.92 | 37.03 | 3.26 | 68.14 |
| Female | 48.08 | 35.68 | 3.02 | 68.16 |
| Chi-square p-value < 0.000 | Chi-square p-value < 0.010 | Chi-square p-value > 0.10 | ||
| Birth Order | ||||
| 1 | 39.07 | 31.93 | 3.65 | 66.35 |
| 2 to 3 | 33.94 | 35.52 | 3.08 | 68.06 |
| 4+ | 27.00 | 43.82 | 2.49 | 70.81 |
| Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | ||
| Birth Size and Weight Composite Index * | ||||
| Low | 35.98 | 41.45 | 2.59 | 69.95 |
| Normal or Above Average | 64.02 | 33.39 | 3.47 | 67.11 |
| Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | ||
| Household Characteristics | ||||
| Place of residence | ||||
| Urban | 27.18 | 30.63 | 4.09 | 64.93 |
| Rural | 72.82 | 38.44 | 2.80 | 69.29 |
| Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | ||
| Religion | ||||
| Hindu | 79.33 | 36.36 | 3.06 | 68.74 |
| Muslim | 16.32 | 37.88 | 3.39 | 67.74 |
| Christian | 2.08 | 32.12 | 3.5 | 53.78 |
| Others | 2.27 | 30.45 | 3.95 | 71.48 |
| Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | ||
| Caste | ||||
| Scheduled Caste/Tribes | 33.00 | 40.83 | 2.78 | 71.59 |
| Other Backward Classes | 43.40 | 35.97 | 2.96 | 66.31 |
| Others | 23.60 | 30.80 | 3.99 | 66.61 |
| Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | ||
| Wealth | ||||
| Poorest | 24.17 | 47.87 | 2.38 | 72.66 |
| Poorer | 21.55 | 40.90 | 2.56 | 69.92 |
| Middle | 19.52 | 35.08 | 3.12 | 67.77 |
| Richer | 18.54 | 28.60 | 3.53 | 64.87 |
| Richest | 16.21 | 23.00 | 4.74 | 62.84 |
| Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | ||
| Mother’s Characteristics | ||||
| Mother’s Age at Birth (in years) | ||||
| Below 19 | 34.32 | 40.92 | 2.68 | 72.32 |
| 20–24 | 49.35 | 35.76 | 3.13 | 66.62 |
| 25–49 | 16.33 | 28.51 | 4.19 | 63.82 |
| Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | ||
| Mother’s education | ||||
| No education | 21.23 | 47.75 | 2.57 | 72.83 |
| Primary | 12.28 | 42.88 | 2.61 | 70.5 |
| Secondary | 50.72 | 34.09 | 3.08 | 67.53 |
| Higher | 15.77 | 22.97 | 4.58 | 61.71 |
| Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | ||
| Mother’s BMI | ||||
| Underweight | 19.78 | 44.36 | 2.12 | 72.91 |
| Normal | 60.96 | 36.5 | 3.14 | 68.51 |
| Overweight or Obese | 19.26 | 27.71 | 4.17 | 62.02 |
| Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | ||
| Mass Media Exposure | ||||
| No exposure | 28.39 | 45.57 | 2.52 | 72.11 |
| Any Media Exposure | 71.61 | 32.72 | 3.39 | 66.57 |
| Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | Chi-square p-value < 0.000 | ||
| Mother’s Anaemia | ||||
| No Anaemia | 40.37 | 60.94 | ||
| Anaemia | 59.63 | 72.99 |
| Background Characteristics | Adjusted Odds Ratio (95% Confidence Interval) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Childhood Stunting | Childhood Overweight | Childhood Anaemia | |||||||
| Model-1 | Model-2 | Model-3 | Model-1 | Model-2 | Model-3 | Model-1 | Model-2 | Model-3 | |
| Age of children (months) | |||||||||
| 6–23® | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| 24–35 | 1.27 *** (1.22, 1.31) | 1.27 *** (1.22, 1.31) | 0.45 *** (0.41, 0.49) | 0.44 *** (0.41, 0.49) | 0.60 *** (0.58, 0.62) | 0.60 *** (0.58, 0.63) | |||
| 36–59 | 1.19 *** (1.16, 1.23) | 1.19 *** (1.17, 1.23) | 0.49 *** (0.46, 0.53) | 0.49 *** (0.46, 0.53) | 0.30 *** (0.29, 0.31) | 0.30 *** (0.29, 0.31) | |||
| Sex of child | |||||||||
| Male® | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| Female | 0.86 *** (0.84, 0.89) | 0.86 *** (0.84, 0.89) | 0.92 ** (0.87, 0.98) | 0.92 * (0.86, 0.98) | 0.98 (0.95, 1.00) | 0.98 (0.95, 1.00) | |||
| Birth Order | |||||||||
| 1® | 1.00 | 1 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| 2 to 3 | 1.16 *** (1.13, 1.19) | 1.16 *** (1.13, 1.19) | 0.85 *** (0.79, 0.90) | 0.84 *** (0.78, 0.89) | 1.06 *** (1.03, 1.09) | 1.06 *** (1.04, 1.09) | |||
| 4+ | 1.28 *** (1.23, 1.34) | 1.25 *** (1.20, 1.31) | 0.83 *** (0.74, 0.93) | 0.83 *** (0.74, 0.93) | 1.09 *** (1.04, 1.14) | 1.08 *** (1.03, 1.13) | |||
| Birth Size/Weight | |||||||||
| Low® | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| Normal or Above Average | 0.68 *** (0.67, 0.71) | 0.69 *** (0.68, 0.71) | 1.29 *** (1.20, 1.37) | 1.27 *** (1.19, 1.37) | 0.94 *** (0.91, 0.96) | 0.94 *** (0.92, 0.97) | |||
| Place of residence | |||||||||
| Urban® | 1.00 | 1.00 | 1.00 | ||||||
| Rural | 1.94 ** (1.90, 1.99) | 0.87 *** (0.79, 0.95) | 1.04 * (1.01, 1.08) | ||||||
| Religion | |||||||||
| Hindu® | 1.00 | 1.00 | 1.00 | ||||||
| Muslim | 1.13 *** (1.07, 1.18) | 1.03 (0.92, 1.16) | 1.07 ** (1.02, 1.13) | ||||||
| Christian | 0.83 *** (0.77, 0.89) | 1.29 *** (1.08, 1.53) | 0.74 *** (0.68, 0.80) | ||||||
| Others | 0.86 *** (0.79, 0.94) | 1.56 *** (1.31, 1.86) | 0.99 (0.92, 1.08) | ||||||
| Caste | |||||||||
| Scheduled Caste/Tribes® | 1.00 | 1.00 | 1.00 | ||||||
| Other Backward Classes | 0.89 *** (0.86, 0.92) | 0.88 *** (0.81, 0.96) | 0.84 *** (0.82, 0.87) | ||||||
| Others | 0.75 *** (0.71, 0.78) | 1.04 (0.94, 1.16) | 0.99 (0.92, 1.08) | ||||||
| Wealth | |||||||||
| Poorest® | 1.00 | 1.00 | 1.00 | ||||||
| Poorer | 0.82 *** (0.79, 0.86) | 1.07 (0.96, 1.19) | 0.90 *** (0.86, 0.94) | ||||||
| Middle | 0.71 *** (0.68, 0.74) | 1.16 * (1.03, 1.30) | 0.88 *** (0.84, 0.92) | ||||||
| Richer | 0.55 *** (0.53, 0.58) | 1.18 * (1.04, 1.34) | 0.83 *** (0.79, 0.88) | ||||||
| Richest | 0.45 *** (0.42, 0.48) | 1.48 *** (1.27, 1.72) | 0.79 *** (0.74, 0.84) | ||||||
| Mother’s Age at Birth (in years) | |||||||||
| 15–24® | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| 25–34 | 0.92 *** (0.89, 0.95) | 0.94 *** (0.94, 1.03) | 1.05 (0.97, 1.13) | 1.04 (0.97, 1.12) | 0.97 (0.95, 1.00) | 0.98 (0.95, 1.01) | |||
| 35–49 | 0.82 *** (0.78, 0.85) | 0.86 *** (0.83, 0.89) | 1.12 * (1.02, 1.23) | 1.07 (0.97, 1.18) | 0.97(0.93, 1.00) | 0.99 (0.94, 1.03) | |||
| Mother’s education | |||||||||
| No education® | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| Primary | 0.96 * (0.91, 0.99) | 0.98 (0.94, 1.03) | 0.97 (0.85, 1.01) | 0.95 (0.84, 1.07) | 0.94 ** (0.89, 0.98) | 0.95 * (0.91, 0.99) | |||
| Secondary | 0.71 *** (0.69, 0.75) | 0.82 *** (0.79, 0.86) | 0.93 (0.84, 1.03) | 0.88 * (0.80, 0.98) | 0.84 *** (0.81, 0.88) | 0.89 *** (0.86, 0.92) | |||
| Higher | 0.49 *** (0.47, 0.52) | 0.67 *** (0.63, 0.71) | 1.16 * (1.03, 1.32) | 1.01 (0.88, 1.15) | 0.73 *** (0.69, 0.77) | 0.81 *** (0.77, 0.86) | |||
| Mother’s BMI | |||||||||
| Underweight® | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| Normal | 0.75 *** (0.73, 0.78) | 0.78 *** (0.75, 0.81) | 1.50 *** (1.37, 1.65) | 1.47 *** (1.34, 1.62) | 0.91 *** (0.88, 0.94) | 0.92 *** (0.88, 0.95) | |||
| Overweight or Obese | 0.57 *** (0.54, 0.59) | 0.63 *** (0.59, 0.66) | 2.02 *** (1.81, 2.27) | 1.92 *** (1.71, 2.15) | 0.83 *** (0.79, 0.87) | 0.86 *** (0.82, 0.89) | |||
| Mass Media Exposure | |||||||||
| No exposure® | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||
| Any Media Exposure | 0.81 *** (0.78, 0.84) | 0.91 *** (0.88, 0.95) | 1.06 (0.98, 1.15) | 1.00 (0.92, 1.09) | 0.91 *** (0.88, 0.94) | 0.95 ** (0.92, 0.98) | |||
| Mother’s Anaemia | |||||||||
| No Anaemia® | 1.00 | 1.00 | |||||||
| Anaemia | 1.67 *** (1.63, 1.72) | 1.66 *** (1.62, 1.71) | |||||||
| Constant | 0.42 *** (0.401–0.435) | 1.06 * (0.996–1.132) | 1.31 *** (1.217–1.422) | 0.01 *** (0.008, 0.012) | 0.01 *** (0.006, 0.102) | 0.01 *** (0.008, 0.0115) | 2.25 *** (2.146, 2.361) | 4.97 *** (4.600, 5.370) | 5.45 *** (4.987, 5.957) |
| Random intercept parameter | |||||||||
| Var (district) | 0.417 (0.401–0.434) | 0.129 (0.112–0.149) | 0.113 (0.098–0.132) | 0.642 (0.549, 0.749) | 0.607 (0.517, 0.713) | 0.555 (0.469, 0.655) | 0.37 (0.325, 0.412) | 0.34 (0.301, 0.385) | 0.32 (0.28, 0.36) |
| Var (PSU) | 0.462 (0.432–0.493) | 0.403 (0.375–0.434) | 0.397 (0.369–0.428) | 1.483 (1.337, 1.644) | 1.572 (1.415, 1.747) | 1.568 (1.411, 1.741) | 0.48 (0.452, 0.507) | 0.51 (0.482, 0.544) | 0.51 (0.48, 0.54) |
| Var (HHs) | 1.071 (0.987–1.162) | 1.003 (0.920–1.094) | 0.977 (0.895–1.068) | 1.579 (1.277, 1.955) | 1.741 (1.415, 2.142) | 1.728 (1.403, 2.128) | 0.14 (0.093, 0.210) | 0.29 (0.231, 0.370) | 0.29 (0.23, 0.37) |
| ICC (district) (%) | 4.621 | 2.67 | 2.38 | 9.17 | 8.42 | 7.77 | 8.56 | 7.67 | 7.16 |
| ICC (PSU) (%) | 13.75 | 11.04 | 10.69 | 30.37 | 30.22 | 29.72 | 19.76 | 19.22 | 18.68 |
| ICC (HHs) (%) | 34.93 | 31.83 | 31.16 | 52.96 | 54.37 | 53.92 | 23.03 | 25.82 | 25.25 |
| Model fit statistics | |||||||||
| Wald test X2 | 3820.63 | 4583.49 | 761.65 | 833.12 | 6778.54 | 6897.73 | |||
| LR test vs. logistic regression: p-value | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Singh, S.K.; Chauhan, A.; Sharma, S.K.; Puri, P.; Pedgaonkar, S.; Dwivedi, L.K.; Taillie, L.S. Cultural and Contextual Drivers of Triple Burden of Malnutrition among Children in India. Nutrients 2023, 15, 3478. https://doi.org/10.3390/nu15153478
Singh SK, Chauhan A, Sharma SK, Puri P, Pedgaonkar S, Dwivedi LK, Taillie LS. Cultural and Contextual Drivers of Triple Burden of Malnutrition among Children in India. Nutrients. 2023; 15(15):3478. https://doi.org/10.3390/nu15153478
Chicago/Turabian StyleSingh, Shri Kant, Alka Chauhan, Santosh Kumar Sharma, Parul Puri, Sarang Pedgaonkar, Laxmi Kant Dwivedi, and Lindsey Smith Taillie. 2023. "Cultural and Contextual Drivers of Triple Burden of Malnutrition among Children in India" Nutrients 15, no. 15: 3478. https://doi.org/10.3390/nu15153478
APA StyleSingh, S. K., Chauhan, A., Sharma, S. K., Puri, P., Pedgaonkar, S., Dwivedi, L. K., & Taillie, L. S. (2023). Cultural and Contextual Drivers of Triple Burden of Malnutrition among Children in India. Nutrients, 15(15), 3478. https://doi.org/10.3390/nu15153478










