Affect, Body, and Eating Habits in Children: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Protocol
2.2. Eligibility Criteria
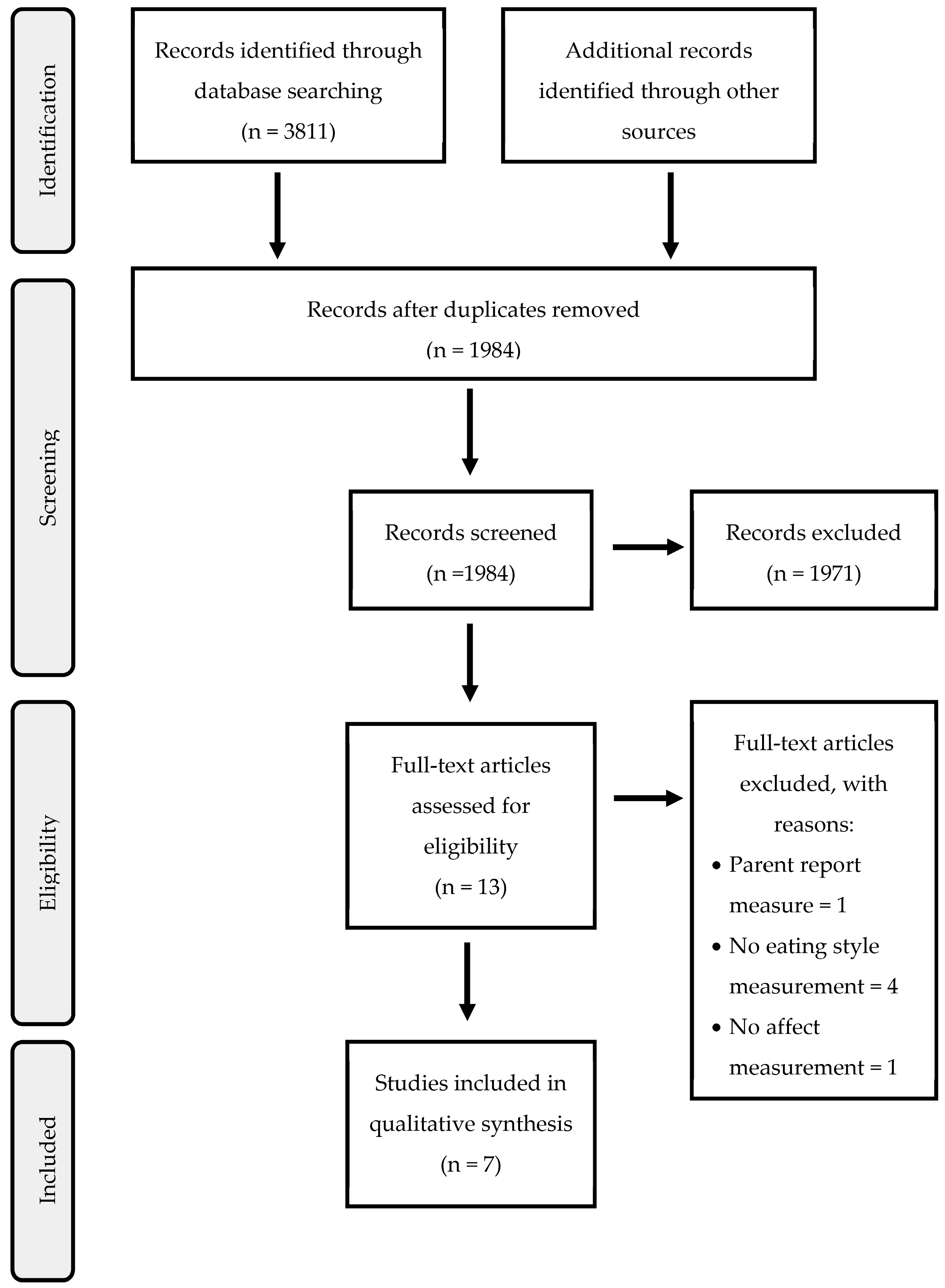
2.3. Study Selection
2.4. Assessment of Quality
2.5. Synthesis and Analysis of Data
3. Results
3.1. Study Characteristics
3.2. Sample Characteristics
3.3. Assessments of Risk of Bias
3.4. Affect, Body, and Eating Habit
3.5. Secondary Outcomes
4. Discussion
Limitations and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Davison, J.; Bunting, B.; Connolly, P.; Lloyd, K.; Dunne, L.; Stewart-Knox, B. Less Screen Time, More Frequent Fruit and Vegetable Intake and Physical Activity Are Associated with Greater Mental Wellbeing in Adolescents. Child Indic. Res. 2022, 15, 1339–1361. [Google Scholar] [CrossRef]
- Masento, N.A.; Golightly, M.; Field, D.T.; Butler, L.T.; Reekum, C.M. Effects of Hydration Status on Cognitive Performance and Mood. Br. J. Nutr. 2014, 111, 1841–1852. [Google Scholar] [CrossRef]
- Mikkilä, V.; Räsänen, L.; Raitakari, O.T.; Pietinen, P.; Viikari, J. Longitudinal Changes in Diet from Childhood into Adulthood with Respect to Risk of Cardiovascular Diseases: The Cardiovascular Risk in Young Finns Study. Eur. J. Clin. Nutr. 2004, 58, 1038–1045. [Google Scholar] [CrossRef] [Green Version]
- Gedeon, R.; Hallit, S.; Wakim, L.H. Food Insecurity and Eating Habits of Lebanese Children Aged 5–11 Years during the COVID-19 Pandemic and the Socioeconomic Crisis: A National Study. BMC Public Health 2022, 22, 1982. [Google Scholar] [CrossRef]
- Bastida, L.; Cea, G.; Moya, A.; Gallego, A.; Gaeta, E.; Sillaurren, S.; Barbosa, P.; Souto, S.; Rodrigues, E.; Torrego-Ellacuría, M.; et al. Promoting Obesity Prevention and Healthy Habits in Childhood: The OCARIoT Experience. IEEE J. Transl. Eng. Health Med. 2023, 11, 261–270. [Google Scholar] [CrossRef] [PubMed]
- Ickes, M.; McMullen, J.; Haider, T.; Sharma, M. Global School-Based Childhood Obesity Interventions: A Review. Int. J. Environ. Res. Public Health 2014, 11, 8940–8961. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ayer, J.; Charakida, M.; Deanfield, J.E.; Celermajer, D.S. Lifetime Risk: Childhood Obesity and Cardiovascular Risk. Eur. Heart J. 2015, 36, 1371–1376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Llewellyn, A.; Simmonds, M.; Owen, C.G.; Woolacott, N. Childhood Obesity as a Predictor of Morbidity in Adulthood: A Systematic Review and Meta-Analysis: Childhood Obesity and Adult Morbidity. Obes. Rev. 2016, 17, 56–67. [Google Scholar] [CrossRef] [PubMed]
- Russell-Mayhew, S.; McVey, G.; Bardick, A.; Ireland, A. Mental Health, Wellness, and Childhood Overweight/Obesity. J. Obes. 2012, 2012, 281801. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Averett, S.L.; Stifel, D.C. Race and Gender Differences in the Cognitive Effects of Childhood Overweight. Appl. Econ. Lett. 2010, 17, 1673–1679. [Google Scholar] [CrossRef]
- Pala, V.; Lissner, L.; Hebestreit, A.; Lanfer, A.; Sieri, S.; Siani, A.; Huybrechts, I.; Kambek, L.; Molnar, D.; Tornaritis, M.; et al. Dietary Patterns and Longitudinal Change in Body Mass in European Children: A Follow-up Study on the IDEFICS Multicenter Cohort. Eur. J. Clin. Nutr. 2013, 67, 1042–1049. [Google Scholar] [CrossRef] [PubMed]
- Daniels, L.A.; Mallan, K.M.; Battistutta, D.; Nicholson, J.M.; Perry, R.; Magarey, A. Evaluation of an Intervention to Promote Protective Infant Feeding Practices to Prevent Childhood Obesity: Outcomes of the NOURISH RCT at 14 Months of Age and 6 Months Post the First of Two Intervention Modules. Int. J. Obes. 2012, 36, 1292–1298. [Google Scholar] [CrossRef] [Green Version]
- Nicklas, T.A.; Baranowski, T.; Cullen, K.W.; Berenson, G. Eating Patterns, Dietary Quality and Obesity. J. Am. Coll. Nutr. 2001, 20, 599–608. [Google Scholar] [CrossRef]
- Harrist, A.W.; Hubbs-Tait, L.; Topham, G.L.; Shriver, L.H.; Page, M.C. Emotion Regulation Is Related to Children’s Emotional and External Eating. J. Dev. Behav. Pediatr. 2013, 34, 557–565. [Google Scholar] [CrossRef] [PubMed]
- Macht, M. How Emotions Affect Eating: A Five-Way Model. Appetite 2008, 50, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Tanofsky-Kraff, M.; Theim, K.R.; Yanovski, S.Z.; Bassett, A.M.; Burns, N.P.; Ranzenhofer, L.M.; Glasofer, D.R.; Yanovski, J.A. Validation of the Emotional Eating Scale Adapted for Use in Children and Adolescents (EES-C). Int. J. Eat. Disord. 2007, 40, 232–240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kral, T.V.; Rauh, E.M. Eating Behaviors of Children in the Context of Their Family Environment. Physiol. Behav. 2010, 100, 567–573. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haines, J.; Rifas-Shiman, S.L.; Horton, N.J.; Kleinman, K.; Bauer, K.W.; Davison, K.K.; Walton, K.; Austin, S.B.; Field, A.E.; Gillman, M.W. Family Functioning and Quality of Parent-Adolescent Relationship: Cross-Sectional Associations with Adolescent Weight-Related Behaviors and Weight Status. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 68. [Google Scholar] [CrossRef] [Green Version]
- Bruch, H. La Gabbia D’Oro L’Enigma Dell’Anoressia Mentale, 3rd ed.; Feltrinelli: Milano, Italy, 2008; ISBN 978-88-07-81766-3. [Google Scholar]
- Bruch, H. Family Transactions in Eating Disorders. Compr. Psychiatry 1971, 12, 238–248. [Google Scholar] [CrossRef]
- Bruch, H. The Emotional Significance of the Preferred Weight. Am. J. Clin. Nutr. 1957, 5, 192–196. [Google Scholar] [CrossRef]
- Shomaker, L.B.; Tanofsky-Kraff, M.; Matherne, C.E.; Mehari, R.D.; Olsen, C.H.; Marwitz, S.E.; Bakalar, J.L.; Ranzenhofer, L.M.; Kelly, N.R.; Schvey, N.A.; et al. A Randomized, Comparative Pilot Trial of Family-based Interpersonal Psychotherapy for Reducing Psychosocial Symptoms, Disordered-eating, and Excess Weight Gain in At-Risk Preadolescents with Loss-of-control-eating. Int. J. Eat. Disord. 2015, 50, 1084–1094. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, K.A.; Ogden, J.; Vögele, C.; Gibson, E.L. The Role of Parental Control Practices in Explaining Children’s Diet and BMI. Appetite 2008, 50, 252–259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bongers, P.; Jansen, A.; Havermans, R.; Roefs, A.; Nederkoorn, C. Happy Eating. The Underestimated Role of Overeating in a Positive Mood. Appetite 2013, 67, 74–80. [Google Scholar] [CrossRef]
- Conner, T.S.; Brookie, K.L.; Carr, A.C.; Mainvil, L.A.; Vissers, M.C.M. Let Them Eat Fruit! The Effect of Fruit and Vegetable Consumption on Psychological Well-Being in Young Adults: A Randomized Controlled Trial. PLoS ONE 2017, 12, e0171206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farrow, C.V.; Haycraft, E.; Blissett, J.M. Teaching Our Children When to Eat: How Parental Feeding Practices Inform the Development of Emotional Eating—A Longitudinal Experimental Design. Am. J. Clin. Nutr. 2015, 101, 908–913. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scaglioni, S.; Arrizza, C.; Vecchi, F.; Tedeschi, S. Determinants of Children’s Eating Behavior. Am. J. Clin. Nutr. 2011, 94, 2006–2011. [Google Scholar] [CrossRef] [Green Version]
- Tan, C.C.; Holub, S.C. Children’s Self-Regulation in Eating: Associations with Inhibitory Control and Parents’ Feeding Behavior. J. Pediatr. Psychol. 2010, 36, 340–345. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caccialanza, R.; Nicholls, D.; Cena, H.; Maccarini, L.; Rezzani, C.; Antonioli, L.; Dieli, S.; Roggi, C. Validation of the Dutch Eating Behaviour Questionnaire Parent Version (DEBQ-P) in the Italian Population: A Screening Tool to Detect Differences in Eating Behaviour among Obese, Overweight and Normal-Weight Preadolescents. Eur. J. Clin. Nutr. 2004, 58, 1217–1222. [Google Scholar] [CrossRef]
- Madowitz, J.; Liang, J.; Peterson, C.B.; Rydell, S.; Zucker, N.L.; Tanofsky-Kraff, M.; Harnack, L.; Boutelle, K.N. Concurrent and Convergent Validity of the Eating in the Absence of Hunger Questionnaire and Behavioral Paradigm in Overweight Children. Int. J. Eat. Disord. 2013, 47, 287–295. [Google Scholar] [CrossRef] [Green Version]
- Michels, N.; Sioen, I.; Braet, C.; Eiben, G.; Hebestreit, A.; Huybrechts, I.; Vanaelst, B.; Vyncke, K.; De Henauw, S. Stress, Emotional Eating Behaviour and Dietary Patterns in Children. Appetite 2012, 59, 762–769. [Google Scholar] [CrossRef] [Green Version]
- Olson, K.L.; Emery, C.F. Mindfulness and Weight Loss. Psychosom. Med. 2015, 77, 59–67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davis, C.; Patte, K.; Levitan, R.; Reid, C.; Tweed, S.; Curtis, C. From Motivation to Behaviour: A Model of Reward Sensitivity, Overeating, and Food Preferences in the Risk Profile for Obesity. Appetite 2007, 48, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Vriendt, T.; Moreno, L.; Henauw, S. Chronic stress and obesity in adolescents: Scientific evidence and methodological issues for epidemiological research. Nutr. Metab. Cardiovasc. Dis. 2009, 19, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Blissett, J.; Haycraft, E.; Farrow, C. Inducing Preschool Children’s Emotional Eating: Relations with Parental Feeding Practices. Am. J. Clin. Nutr. 2010, 92, 359–365. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ranzenhofer, L.M.; Hannallah, L.; Field, S.E.; Shomaker, L.B.; Stephens, M.; Sbrocco, T.; Kozlosky, M.; Reynolds, J.; Yanovski, J.A.; Tanofsky-Kraff, M. Pre-Meal Affective State and Laboratory Test Meal Intake in Adolescent Girls with Loss of Control Eating. Appetite 2013, 68, 30–37. [Google Scholar] [CrossRef] [Green Version]
- Rodgers, R.F.; Paxton, S.J.; Massey, R.; Campbell, K.J.; Wertheim, E.H.; Skouteris, H.; Gibbons, K. Maternal Feeding Practices Predict Weight Gain and Obesogenic Eating Behaviors in Young Children: A Prospective Study. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 24. [Google Scholar] [CrossRef] [Green Version]
- Braet, C.; Van Strien, T. Assessment of Emotional, Externally Induced and Restrained Eating Behaviour in Nine to Twelve-Year-Old Obese and Non-Obese Children. Behav. Res. Ther. 1997, 35, 863–873. [Google Scholar] [CrossRef]
- Czaja, J.; Rief, W.; Hilbert, A. Emotion Regulation and Binge Eating in Children. Int. J. Eat. Disord. 2009, 42, 356–362. [Google Scholar] [CrossRef]
- Goldschmidt, A.B.; Wall, M.; Choo, T.H.J.; Becker, C.; Neumark-Sztainer, D. Shared Risk Factors for Mood-, Eating-, and Weight-Related Health Outcomes. Health Psychol. 2016, 35, 245–252. [Google Scholar] [CrossRef]
- Van Strien, T.; Beijers, R.; Smeekens, S.; Winkens, L.H.H. Duration of Breastfeeding Is Associated with Emotional Eating through Its Effect on Alexithymia in Boys, but Not Girls. Appetite 2019, 132, 97–105. [Google Scholar] [CrossRef] [Green Version]
- Bergmeier, H.; Skouteris, H.; Hetherington, M. Systematic Research Review of Observational Approaches Used to Evaluate Mother-Child Mealtime Interactions during Preschool Years. Am. J. Clin. Nutr. 2015, 101, 7–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Braet, C.; Beyers, W.; Goossens, L.; Verbeken, S.; Moens, E. Subtyping Children and Adolescents Who Are Overweight Based on Eating Pathology and Psychopathology. Eur. Eat. Disord. Rev. 2011, 20, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Vannucci, A.; Tanofsky-Kraff, M.; Crosby, R.D.; Ranzenhofer, L.M.; Shomaker, L.B.; Field, S.E.; Mooreville, M.; Reina, S.A.; Kozlosky, M.; Yanovski, S.Z.; et al. Latent Profile Analysis to Determine the Typology of Disinhibited Eating Behaviors in Children and Adolescents. J. Consult. Clin. Psychol. 2013, 81, 494–507. [Google Scholar] [CrossRef] [Green Version]
- Pidgeon, A.; Lacota, K.; Champion, J. The Moderating Effects of Mindfulness on Psychological Distress and Emotional Eating Behaviour. Aust. Psychol. 2013, 48, 262–269. [Google Scholar] [CrossRef]
- Steinsbekk, S.; Barker, E.D.; Llewellyn, C.; Fildes, A.; Wichstrøm, L. Emotional Feeding and Emotional Eating: Reciprocal Processes and the Influence of Negative Affectivity. Child Dev. 2017, 89, 1234–1246. [Google Scholar] [CrossRef] [Green Version]
- Michels, N.; Sioen, I.; Boone, L.; Braet, C.; Vanaelst, B.; Huybrechts, I.; Henauw, S. Longitudinal Association between Child Stress and Lifestyle. Health Psychol. 2015, 34, 40–50. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 Explanation and Elaboration: Updated Guidance and Exemplars for Reporting Systematic Reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Hong, Q.N.; Pluye, P.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Vedel, I. Mixed Methods Appraisal Tool (MMAT), version 2018; McGill University: Montreal, QC, Canada, 2018; Volume 34, 285–291.
- Farrow, C.; Haycraft, E.; Meyer, C. Similarities between Eating Attitudes Among Friendship Groups in Childhood: The Moderating Role of Child Anxiety. J. Pediatr. Psychol. 2011, 36, 1144–1152. [Google Scholar] [CrossRef]
- Houldcroft, L.; Farrow, C.; Haycraft, E. Perceptions of Parental Pressure to Eat and Eating Behaviours in Preadolescents: The Mediating Role of Anxiety. Appetite 2014, 80, 61–69. [Google Scholar] [CrossRef] [Green Version]
- Holt, K.; Ricciardelli, L.A. Social Comparisons and Negative Affect as Indicators of Problem Eating and Muscle Preoccupation among Children. J. Appl. Dev. Psychol. 2002, 23, 285–304. [Google Scholar] [CrossRef]
- Morgan, C.M.; Yanovski, S.Z.; Nguyen, T.T.; McDuffie, J.; Sebring, N.G.; Jorge, M.R.; Keil, M.; Yanovski, J.A. Loss of Control over Eating, Adiposity, and Psychopathology in Overweight Children. Int. J. Eat. Disord. 2002, 31, 430–441. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saling, M.; Ricciardelli, L.A.; McCabe, M.P. A Prospective Study of Individual Factors in the Development of Weight and Muscle Concerns Among Preadolescent Children. J. Youth Adolesc. 2005, 34, 651–661. [Google Scholar] [CrossRef]
- Tan, C.C.; Holub, S.C. The Effects of Happiness and Sadness on Children’s Snack Consumption. Appetite 2018, 123, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Kirk, S.F.; Kuhle, S.; McIsaac, J.-L.D.; Williams, P.L.; Rossiter, M.; Ohinmaa, A.; Veugelers, P.J. Food Security Status among Grade 5 Students in Nova Scotia, Canada and Its Association with Health Outcomes. Public Health Nutr. 2015, 18, 2943–2951. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crowe, M.; Sheppard, L. A Review of Critical Appraisal Tools Show They Lack Rigor: Alternative Tool Structure Is Proposed. J. Clin. Epidemiol. 2011, 64, 79–89. [Google Scholar] [CrossRef] [PubMed]
- Ortuño-Sierra, J.; Bañuelos, M.; Albéniz, A.; Molina, B.L.; Fonseca-Pedrero, E. The Study of Positive and Negative Affect in Children and Adolescents: New Advances in a Spanish Version of the PANAS. PLoS ONE 2019, 14, e0221696. [Google Scholar] [CrossRef]
- Kemp, E.; Bui, M.; Grier, S. When Food Is More than Nutrition: Understanding Emotional Eating and Overconsumption. J. Consum. Behav. 2013, 12, 204–213. [Google Scholar] [CrossRef]
- Davis, M.; Suveg, C. Focusing on the Positive: A Review of the Role of Child Positive Affect in Developmental Psychopathology. Clin. Child Fam. Psychol. Rev. 2013, 17, 97–124. [Google Scholar] [CrossRef]
- Bergmeier, H.; Skouteris, H.; Horwood, S.; Hooley, M.; Richardson, B. Associations between Child Temperament, Maternal Feeding Practices and Child Body Mass Index during the Preschool Years: A Systematic Review of the Literature. Obes. Rev. 2013, 15, 9–18. [Google Scholar] [CrossRef]
- Cornette, R.E. The Emotional Impact of Obesity on Children. In Global Perspectives on Childhood Obesity; Elsevier: Amsterdam, The Netherlands, 2011; pp. 257–264. [Google Scholar]
- Heiman, T.; Olenik-Shemesh, D. Perceived Body Appearance and Eating Habits: The Voice of Young and Adult Students Attending Higher Education. Int. J. Environ. Res. Public Health 2019, 16, 451. [Google Scholar] [CrossRef] [Green Version]
- Mitchell, T.B.; Steele, R.G. The Effect of Body Mass Index, Negative Affect, and Disordered Eating on Health-Related Quality of Life in Preadolescent Youth. J. Pediatr. Psychol. 2016, 41, 768–776. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Birch, D.L.; Savage, J.S.; Ventura, A. Influences on the Development of Children’s Eating Behaviours: From Infancy to Adolescence. Can. J. Diet. Pract. Res. 2007, 68, s1–s56. [Google Scholar] [PubMed]
- Scaglioni, S.; Cosmi, V.; Ciappolino, V.; Parazzini, F.; Brambilla, P.; Agostoni, C. Factors Influencing Children’s Eating Behaviours. Nutrients 2018, 10, 706. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fismen, A.; Buoncristiano, M.; Williams, J.; Helleve, A.; Abdrakhmanova, S.; Bakacs, M.; Bergh, I.H.; Boymatova, K.; Duleva, V.; Fijałkowska, A.; et al. Socioeconomic Differences in Food Habits among 6- to 9-year-old Children from 23 Countries—WHO European Childhood Obesity Surveillance Initiative (COSI 2015/2017). Obes. Rev. 2021, 22, e13211. [Google Scholar] [CrossRef]
- Dinour, L.M.; Bergen, D.; Yeh, M.-C. The Food Insecurity–Obesity Paradox: A Review of the Literature and the Role Food Stamps May Play. J. Am. Diet. Assoc. 2007, 107, 1952–1961. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A. Obesity and the Food Environment. Am. J. Prev. Med. 2004, 27, 154–162. [Google Scholar] [CrossRef]
- Costa, A.; Oliveira, A. Parental Feeding Practices and Children’s Eating Behaviours: An Overview of Their Complex Relationship. Healthcare 2023, 11, 400. [Google Scholar] [CrossRef]
- Bruch, H. Psychological Aspects of Overeating And Obesity. Psychosomatics 1964, 5, 269–274. [Google Scholar] [CrossRef] [PubMed]
- Granieri, A.; Schimmenti, A. Mind–Body Splitting and Eating Disorders: A Psychoanalytic Perspective. Psychoanal. Psychother. 2014, 28, 52–70. [Google Scholar] [CrossRef]
- Jenkins, P.E.; O’Connor, H. Discerning Thoughts From Feelings: The Cognitive-Affective Division in Eating Disorders. Eat. Disord. 2012, 20, 144–158. [Google Scholar] [CrossRef]
- Berking, M.; Eichler, E.; Luhmann, M.; Diedrich, A.; Hiller, W.; Rief, W. Affect Regulation Training Reduces Symptom Severity in Depression—A Randomized Controlled Trial. PLoS ONE 2019, 14, e0220436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luomala, H.T.; Sirieix, L.; Tahir, R. Exploring Emotional-Eating Patterns in Different Cultures: Toward a Conceptual Framework Model. J. Int. Consum. Mark. 2009, 21, 231–245. [Google Scholar] [CrossRef]
| Database | Records | Syntax |
|---|---|---|
| PubMed | 986 | (“Affect regulation” [Title/Abstract] OR “Affect dysregulation” [Title/Abstract] OR “Affect recognition” [Title/Abstract] OR “Alexithymia” [Title/Abstract] OR “Anxiety” [Title/Abstract] OR “Depression” [Title/Abstract] OR “Emotional awareness” [Title/Abstract] OR “Emotional control” [Title/Abstract] OR “Emotional dysregulation” [Title/Abstract] OR “Emotional expressi*” [Title/Abstract] OR “Emotional modulation” [Title/Abstract] OR “Emotional regulation” [Title/Abstract] OR “Mood” [Title/Abstract]) AND (“Obesity” [Title/Abstract] OR “Overweight” [Title/Abstract]) AND (“Child*” [Title/Abstract]) AND (“Weight control” [Title/Abstract] OR “Weight management” [Title/Abstract] OR “Weight modulation” [Title/Abstract] OR “External eating” [Title/Abstract] OR “Binge eating” [Title/Abstract] OR “Affective eating” [Title/Abstract] OR “Body mass index” [Title/Abstract] OR “BMI” [Title/Abstract] OR “Eating attitude” [Title/Abstract] OR “Eating behavior” [Title/Abstract] OR “Eating habit” [Title/Abstract] OR “Eating practice” [Title/Abstract] OR “Eating style” [Title/Abstract] OR “Emotional eating” [Title/Abstract]) |
| Scopus | 1454 | TITLE-ABS (“Affect regulation” OR “Affect dysregulation” OR “Affect recognition” OR “Alexithymia” OR “Anxiety” OR “Depression” OR “Emotional awareness” OR “Emotional control” OR “Emotional dysregulation” OR “emotional expressi*” OR “Emotional modulation” OR “Emotional regulation” OR “Mood”) AND (“Obesity” OR “Overweight”) AND (“child*”) AND (“Weight control” OR “Weight management” OR “Weight modulation” OR “External eating” OR “Binge eating” OR “Affective eating” OR “Body mass index” OR “BMI” OR “Eating attitude” OR “Eating behavior” OR “Eating habit” OR “Eating practice” OR “Eating style” OR “Emotional eating”) |
| Web of Science | 1371 | TI = (“Affect regulation” OR “Affect dysregulation” OR “Affect recognition” OR “Alexithymia” OR “Anxiety” OR “Depression” OR “Emotional awareness” OR “Emotional control” OR “Emotional dysregulation” OR “emotional expressi*” OR “Emotional modulation” OR “Emotional regulation” OR “Mood”) AND (“Obesity” OR “Overweight”) AND (“child*”) AND (“Weight control” OR “Weight management” OR “Weight modulation” OR “External eating” OR “Binge eating” OR “Affective eating” OR “Body mass index” OR “BMI” OR “Eating attitude” OR “Eating behavior” OR “Eating habit” OR “Eating practice” OR “Eating style” OR “Emotional eating”) NOT “adoles*” NOT “infant”) OR AB = (“Affect regulation” OR “Affect dysregulation” OR “Affect recognition” OR “Alexithymia” OR “Anxiety” OR “Depression” OR “Emotional awareness” OR “Emotional control” OR “Emotional dysregulation” OR “emotional expressi*” OR “Emotional modulation” OR “Emotional regulation” OR “Mood”) AND (“Obesity” OR “Overweight”) AND (“child*”) AND (“Weight control” OR “Weight management” OR “Weight modulation” OR “External eating” OR “Binge eating” OR “Affective eating” OR “Body mass index” OR “BMI” OR “Eating attitude” OR “Eating behavior” OR “Eating habit” OR “Eating practice” OR “Eating style” OR “Emotional eating”) |
| Authors | Year | Country | Study Aim | Sample | Instruments | |||
|---|---|---|---|---|---|---|---|---|
| n | Age Range M (SD) | Gender | Emotion/Affect | Eating Habits | ||||
| Farrow et al. [50] | 2011 | UK | Explore the similarities between unhealthy weight and shape related attitudes and behaviors in a sample of 8–11-year males and females, and evaluate whether individual levels of anxiety are related to children’s susceptibility to peer influences on dysfunctional eating. | 154 | 8–11 10.47 (0.88) | 78 girls 75 boys | SCAS | EPI-C |
| Holt and Ricciardelli [52] | 2002 | Australia | Examine the utilization of social comparisons and negative affect as indicators of body dissatisfaction and problem eating, exercising, and muscle concerns for boys and girls separately. | 236 | 8–10 Girls = 8.89 (0.69) Boys = 8.94 (0.72) | 69 girls 47 boys | PANAS-C | ChEAT |
| Houldcroft et al. [51] | 2014 | UK | Examine the potential relationship between preadolescents’ perceptions of controlling parental feeding practices and their reports of anxiety and depression symptomology. | 356 | 7.25–10.25 8.75 (0.57) | 172 girls 184 boys | SCAS CDI:S | EPI-C KCFQ |
| Kirk et al. [56] | 2015 | Canada | Explore the relationship between food security, diet quality, weight status, and psychosocial outcomes. | 5853 | 10–11 | – | Ten questions created ad hoc | US HFSSM DQI YAQ Canadian Nutrient File |
| Morgan et al. [53] | 2002 | USA | Investigate self-reported binge eating behaviors in overweight children. | 112 | 6–10 | 60 girls 52 boys | CDI STAIC | ChEAT |
| Saling et al. [54] | 2005 | Australia | Investigate whether low self-esteem, perceived parent and peer relations, negative affect and/or perfectionism predicted dieting, food preoccupation or muscle preoccupation are observed in 8–10-year-old preadolescent children over a 10-month period. | 326 | 8–10 | 150 girls 176 boys | PANAS-C | ChEAT |
| Tan and Holub [55] | 2018 | USA | Examine the effects of happiness and sadness on children’s observed snack consumption and their interaction effect on children’s characteristics (i.e., weight, gender, and age). | 91 | 4.5–9 6.8 (1.2) | 43 girls 48 boys | Experimental mood induction (three 3-min video clips eliciting happiness, sadness, and neutral emotions) | Observed emotional eating |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdoli, M.; Scotto Rosato, M.; Cipriano, A.; Napolano, R.; Cotrufo, P.; Barberis, N.; Cella, S. Affect, Body, and Eating Habits in Children: A Systematic Review. Nutrients 2023, 15, 3343. https://doi.org/10.3390/nu15153343
Abdoli M, Scotto Rosato M, Cipriano A, Napolano R, Cotrufo P, Barberis N, Cella S. Affect, Body, and Eating Habits in Children: A Systematic Review. Nutrients. 2023; 15(15):3343. https://doi.org/10.3390/nu15153343
Chicago/Turabian StyleAbdoli, Marzieh, Marco Scotto Rosato, Annarosa Cipriano, Rosanna Napolano, Paolo Cotrufo, Nadia Barberis, and Stefania Cella. 2023. "Affect, Body, and Eating Habits in Children: A Systematic Review" Nutrients 15, no. 15: 3343. https://doi.org/10.3390/nu15153343
APA StyleAbdoli, M., Scotto Rosato, M., Cipriano, A., Napolano, R., Cotrufo, P., Barberis, N., & Cella, S. (2023). Affect, Body, and Eating Habits in Children: A Systematic Review. Nutrients, 15(15), 3343. https://doi.org/10.3390/nu15153343





