Eating Compulsivity in Inpatients with Severe Obesity and the General Population: The Italian Version of the Measure of Eating Compulsivity (MEC10-IT)
Abstract
1. Introduction
2. Study 1: Factorial Structure of the Italian Version of the MEC10
2.1. Translation and Cultural Adaptation
2.2. Materials and Methods
2.2.1. Sample Size Determination
2.2.2. Procedure
2.2.3. Participants
2.3. Measures
2.3.1. The Measure of Eating Compulsivity (MEC10)—Italian Version
2.3.2. The Modified Yale Food Addiction Scale 2.0 (mYFAS2.0)
2.3.3. The Binge Eating Scale (BES)
2.4. Statistical Analyses
2.5. Results
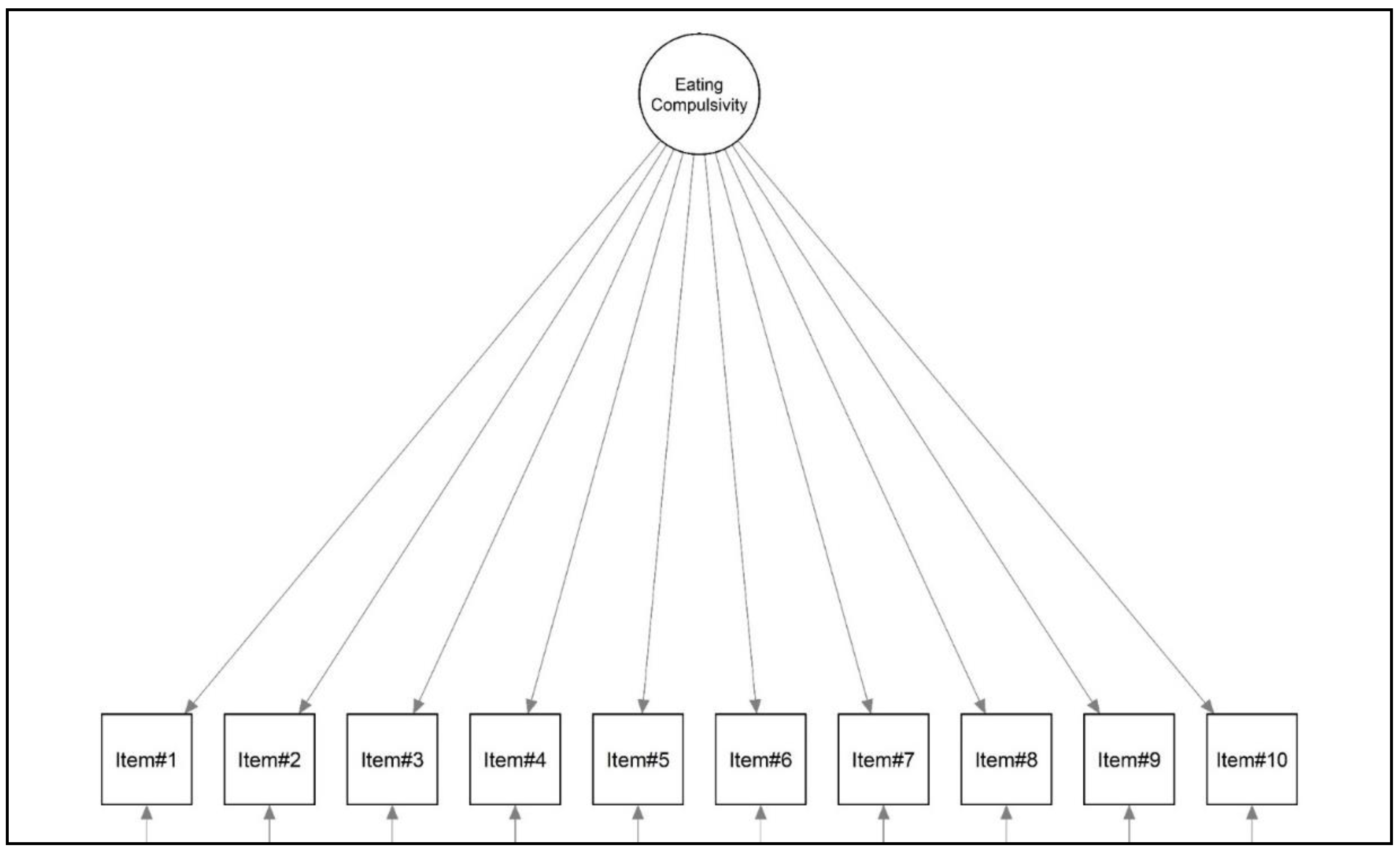
2.5.1. Structural Validity
2.5.2. Internal Consistency
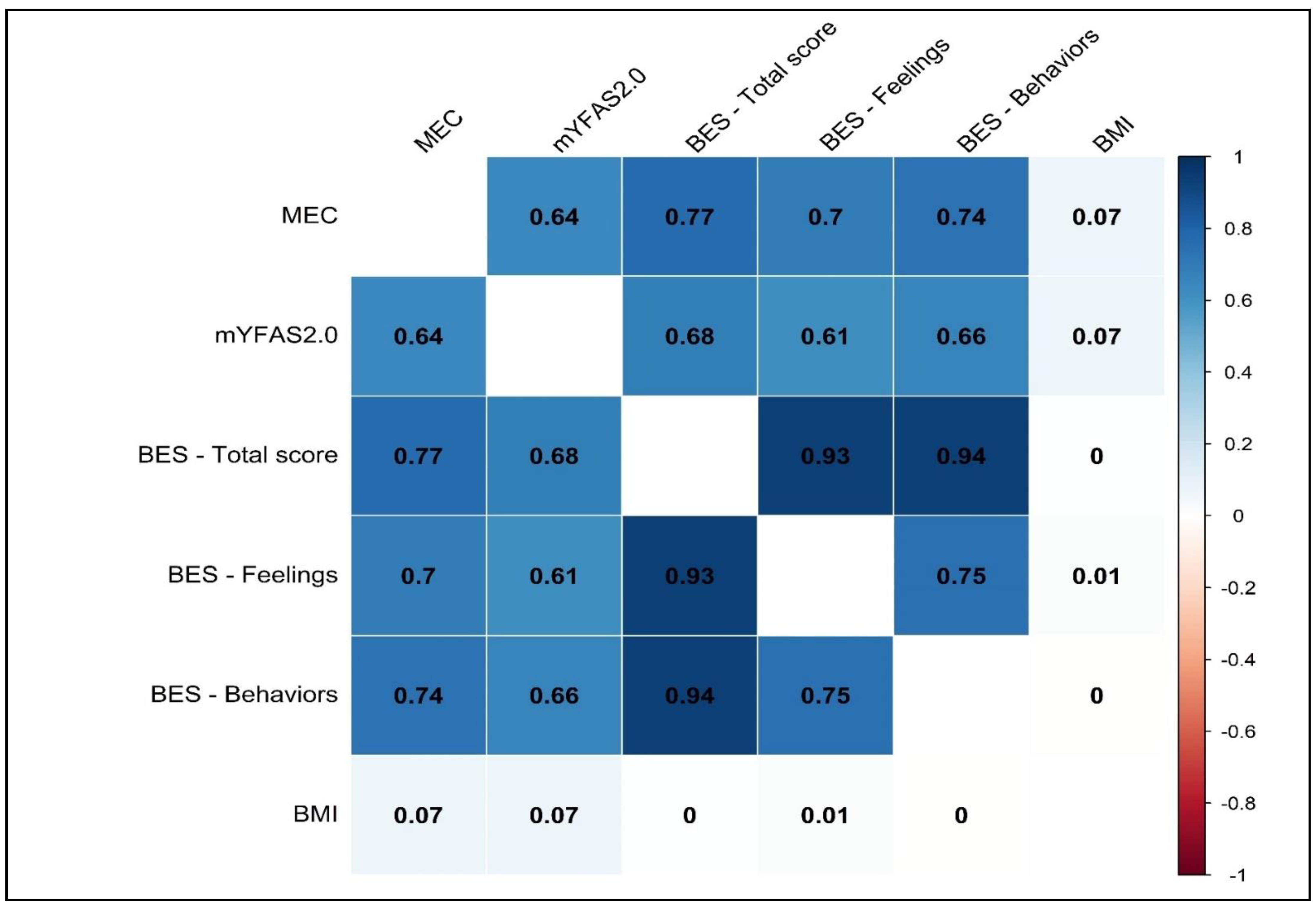
2.5.3. Convergent Validity
3. Study 2: In-Depth Analysis of the MEC10-IT
3.1. Materials and Methods
3.1.1. Sample Size Determination
3.1.2. Procedure
3.1.3. Participants
3.1.4. Measures
3.1.5. Statistical Analysis
3.2. Results
3.2.1. Structural Validity
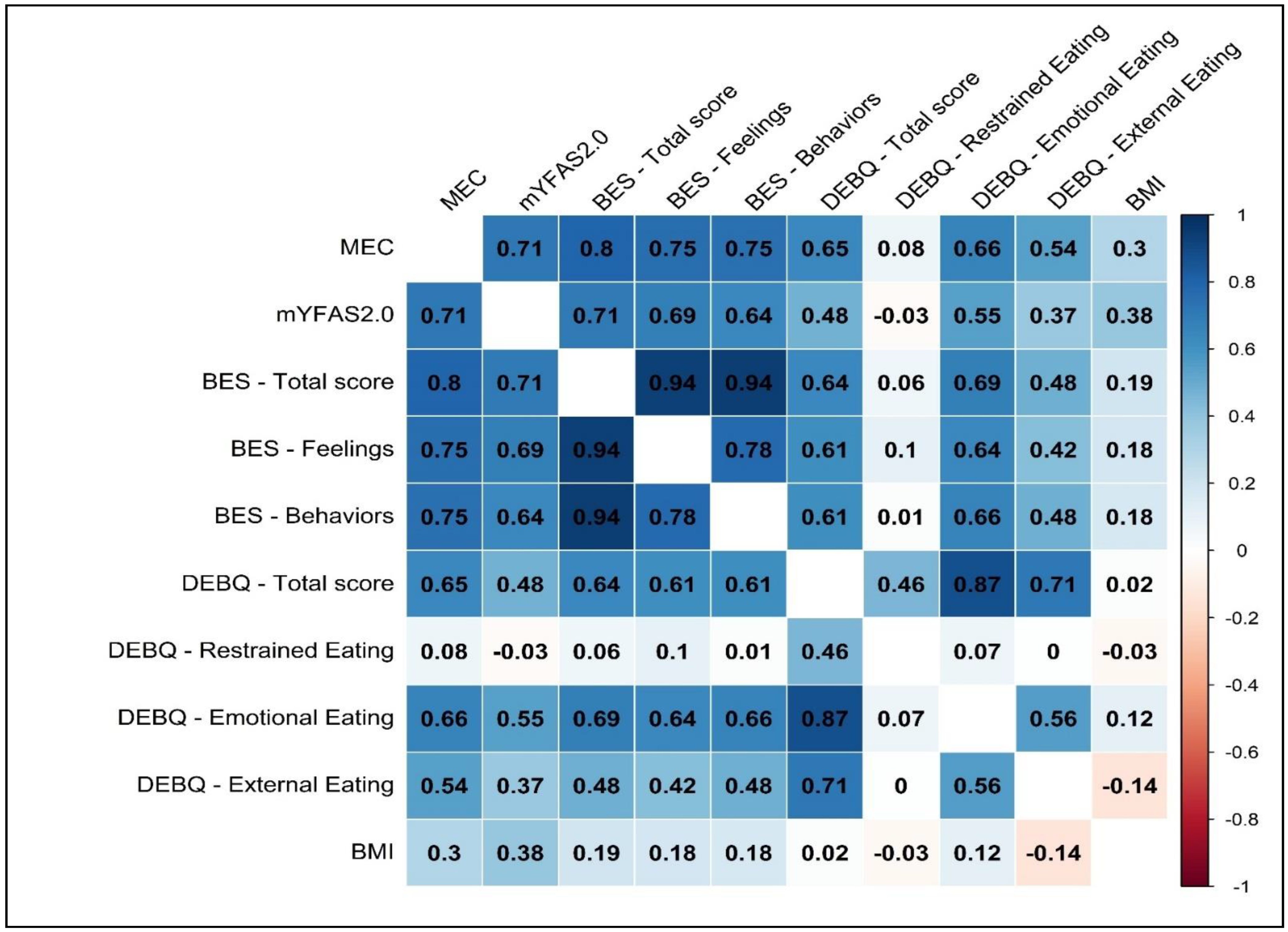
3.2.2. Psychometrics Properties
3.2.3. Measurement Invariance across Samples
3.2.4. Incremental Validity
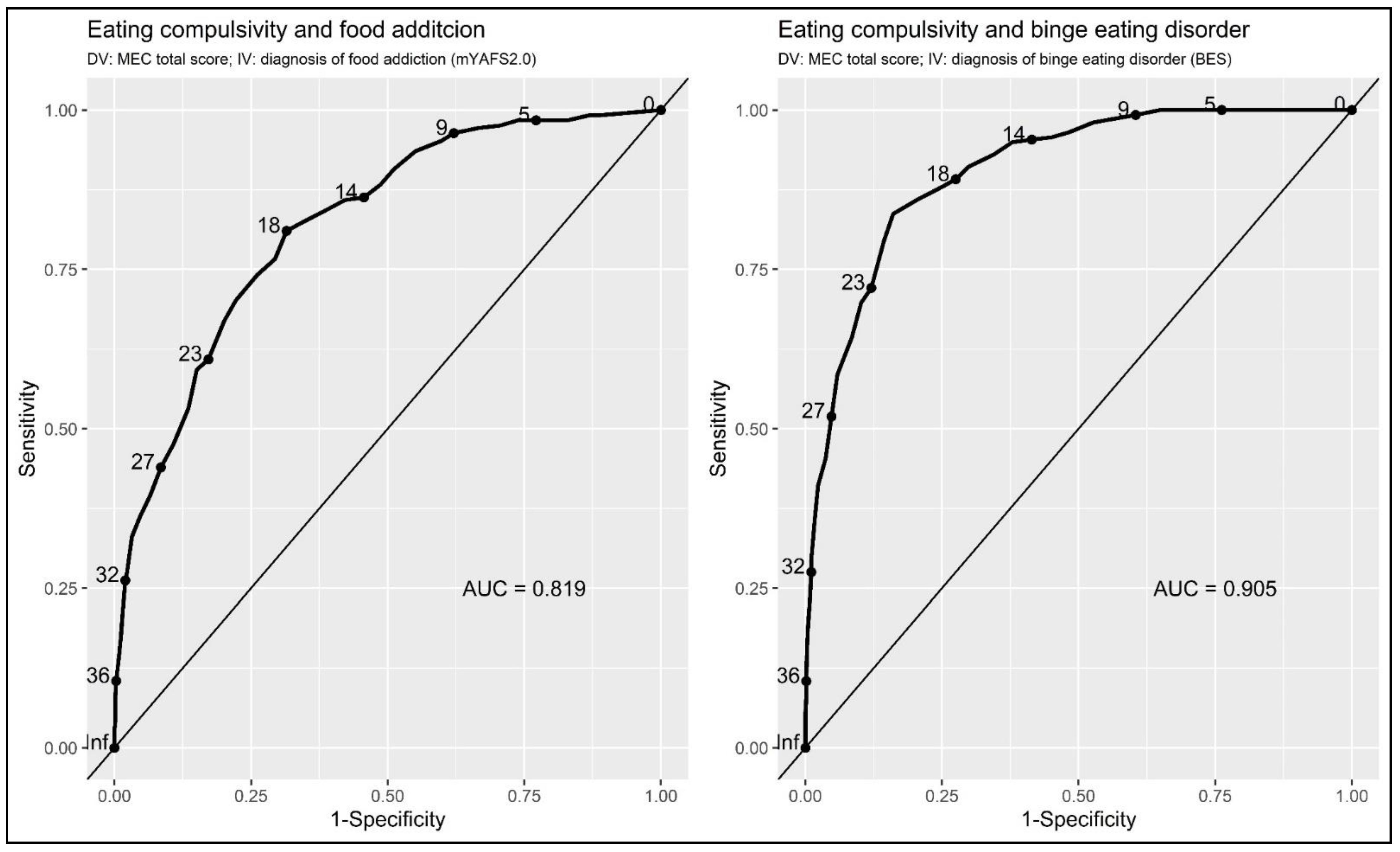
3.2.5. Accuracy of the MEC10-IT as a Screening/Diagnostic Tool
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| 0 COMPLETAMENTE FALSO | 1 FALSO | 2 NÉ FALSO, NÉ VERO | 3 VERO | 4 COMPLETAMENTE VERO | |||||
| 1 | Sento il desiderio di mangiare per la maggior parte del tempo. | 0 | 1 | 2 | 3 | 4 | |||
| 2 | Mi sento a disagio a causa del mio desiderio di mangiare. | 0 | 1 | 2 | 3 | 4 | |||
| 3 | Ho pochissimo controllo sul mio modo di mangiare. | 0 | 1 | 2 | 3 | 4 | |||
| 4 | Spesso temo di perdere il controllo sul mio modo di mangiare. | 0 | 1 | 2 | 3 | 4 | |||
| 5 | In presenza di cibo, non sono in grado di controllare quanto mangio. | 0 | 1 | 2 | 3 | 4 | |||
| 6 | Spesso mi sento fuori controllo in presenza di certi cibi. | 0 | 1 | 2 | 3 | 4 | |||
| 7 | Il cibo è come una droga per me. | 0 | 1 | 2 | 3 | 4 | |||
| 8 | Mi preoccupa quanto poco controllo io abbia sul mio modo di mangiare. | 0 | 1 | 2 | 3 | 4 | |||
| 9 | Quando mi trovo davanti a un cibo molto gustoso, non riesco a smettere di pensarci. | 0 | 1 | 2 | 3 | 4 | |||
| 10 | Mi sento sconfitto dal cibo. | 0 | 1 | 2 | 3 | 4 | |||
References
- GBD 2015 Obesity Collaborators. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.A.; Manzoni, G.M.; Pietrabissa, G.; Di Pauli, D.; Mannarini, S.; Castelnuovo, G. Weight stigma in patients with overweight and obesity: Validation of the Italian Weight Self-Stigma Questionnaire (WSSQ). Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2022, 27, 2459–2472. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Report of the Commission on Ending Childhood Obesity. Implementation Plan: Executive Summary; WHO/NMH/PND/ECHO/17.1; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Blundell, J.E.; Finlayson, G. Food addiction not helpful: The hedonic component-implicit wanting-is important. Addiction 2011, 106, 1216–1218. [Google Scholar] [CrossRef] [PubMed]
- Ferretti, F.; Mariani, M. Simple vs. Complex Carbohydrate Dietary Patterns and the Global Overweight and Obesity Pandemic. Int. J. Environ. Res Public Health 2017, 14, 1174. [Google Scholar] [CrossRef]
- Popkin, B.M.; Adair, L.S.; Ng, S.W. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 2012, 70, 3–21. [Google Scholar] [CrossRef]
- Swinburn, B.A.; Sacks, G.; Hall, K.D.; McPherson, K.; Finegood, D.T.; Moodie, M.L.; Gortmaker, S.L. The global obesity pandemic: Shaped by global drivers and local environments. Lancet 2011, 378, 804–814. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; DiFeliceantonio, A.G. Highly processed foods can be considered addictive substances based on established scientific criteria. Addiction 2022, 118, 589–598. [Google Scholar] [CrossRef]
- Meule, A. Back by Popular Demand: A Narrative Review on the History of Food Addiction Research. Yale J. Biol. Med. 2015, 88, 295–302. [Google Scholar]
- Meule, A.; Gearhardt, A.N. Food addiction in the light of DSM-5. Nutrients 2014, 6, 3653–3671. [Google Scholar] [CrossRef]
- Pursey, K.M.; Stanwell, P.; Gearhardt, A.N.; Collins, C.E.; Burrows, T.L. The Prevalence of Food Addiction as Assessed by the Yale Food Addiction Scale: A Systematic Review. Nutrients 2014, 6, 4552–4590. [Google Scholar] [CrossRef]
- Jiménez-Murcia, S.; Granero, R.; Wolz, I.; Baño, M.; Mestre-Bach, G.; Steward, T.; Agüera, Z.; Hinney, A.; Diéguez, C.; Casanueva, F.F.; et al. Food Addiction in Gambling Disorder: Frequency and Clinical Outcomes. Front. Psychol. 2017, 8, 473. [Google Scholar] [CrossRef] [PubMed]
- Schulte, E.M.; Smeal, J.K.; Gearhardt, A.N. Foods are differentially associated with subjective effect report questions of abuse liability. PLoS ONE 2017, 12, e0184220. [Google Scholar] [CrossRef]
- Stice, E.; Spoor, S.; Ng, J.; Zald, D.H. Relation of obesity to consummatory and anticipatory food reward. Physiol. Behav. 2009, 97, 551–560. [Google Scholar] [CrossRef]
- Volkow, N.D.; Wang, G.J.; Fowler, J.S.; Telang, F. Overlapping neuronal circuits in addiction and obesity: Evidence of systems pathology. Philos. Trans. R. Soc. B Biol. Sci. 2008, 363, 3191–3200. [Google Scholar] [CrossRef]
- Davis, C.; Levitan, R.D.; Kaplan, A.S.; Kennedy, J.L.; Carter, J.C. Food cravings, appetite, and snack-food consumption in response to a psychomotor stimulant drug: The moderating effect of “food-addiction”. Front. Psychol. 2014, 5, 403. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.; Loxton, N.J.; Levitan, R.D.; Kaplan, A.S.; Carter, J.C.; Kennedy, J.L. “Food addiction” and its association with a dopaminergic multilocus genetic profile. Physiol. Behav. 2013, 118, 63–69. [Google Scholar] [CrossRef]
- Meule, A. A history of “food addiction”. In Compulsive Eating Behavior and Food Addiction; Cottone, P., Moore, C.F., Sabino, V., Koob, G.F., Eds.; Elsevier: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Lacroix, E.; Tavares, H.; von Ranson, K.M. Moving beyond the “eating addiction” versus “food addiction” debate: Comment on Schulte et al. (2017). Appetite 2018, 130, 286–292. [Google Scholar] [CrossRef]
- Moore, C.F.; Sabino, V.; Koob, G.F.; Cottone, P. Pathological Overeating: Emerging Evidence for a Compulsivity Construct. Neuropsychopharmacology 2017, 42, 1375–1389. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.; Carter, J.C. Compulsive overeating as an addiction disorder. A review of theory and evidence. Appetite 2009, 53, 18. [Google Scholar] [CrossRef] [PubMed]
- Hone-Blanchet, A.; Fecteau, S. Overlap of food addiction and substance use disorders definitions: Analysis of animal and human studies. Neuropharmacology 2014, 85, 81–90. [Google Scholar] [CrossRef]
- Everitt, B.J.; Robbins, T.W. Neural systems of reinforcement for drug addiction: From actions to habits to compulsion. Nat. Neurosci. 2005, 8, 1481–1489. [Google Scholar] [CrossRef] [PubMed]
- Giuliano, C.; Cottone, P. The role of the opioid system in binge eating disorder. CNS Spectr. 2015, 20, 537–545. [Google Scholar] [CrossRef] [PubMed]
- Robinson, M.J.F.; Burghardt, P.R.; Patterson, C.M.; Nobile, C.W.; Akil, H.; Watson, S.J.; Berridge, K.C.; Ferrario, C.R. Individual Differences in Cue-Induced Motivation and Striatal Systems in Rats Susceptible to Diet-Induced Obesity. Neuropsychopharmacol. Off. Publ. Am. Coll. Neuropsychopharmacol. 2015, 40, 2113–2123. [Google Scholar] [CrossRef] [PubMed]
- Musetti, A.; Gagliardini, G.; Lenzo, V.; Cella, S. From childhood emotional maltreatment to disordered eating: A path analysis. Psychoanal. Psychol. 2023. [Google Scholar] [CrossRef]
- Guerrini Usubini, A.; Cattivelli, R.; Varallo, G.; Castelnuovo, G.; Molinari, E.; Giusti, E.M.; Pietrabissa, G.; Manari, T.; Filosa, M.; Franceschini, C.; et al. The Relationship between Psychological Distress during the Second Wave Lockdown of COVID-19 and Emotional Eating in Italian Young Adults: The Mediating Role of Emotional Dysregulation. J. Pers. Med. 2021, 11, 569. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- el-Guebaly, N.; Mudry, T.; Zohar, J.; Tavares, H.; Potenza, M.N. Compulsive features in behavioural addictions: The case of pathological gambling. Addiction 2012, 107, 1726–1734. [Google Scholar] [CrossRef] [PubMed]
- Robbins, T.W.; Curran, H.V.; de Wit, H. Special issue on impulsivity and compulsivity. Psychopharmacology 2012, 219, 251–252. [Google Scholar] [CrossRef]
- Klatzkin, R.R.; Gaffney, S.; Cyrus, K.; Bigus, E.; Brownley, K.A. Binge eating disorder and obesity: Preliminary evidence for distinct cardiovascular and psychological phenotypes. Physiol. Behav. 2015, 142, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Warschburger, P. The unhappy obese child. Int. J. Obes. 2005, 29, S127–S129. [Google Scholar] [CrossRef] [PubMed]
- Deroche-Gamonet, V.; Belin, D.; Piazza, P.V. Evidence for Addiction-like Behavior in the Rat. Science 2004, 305, 1014–1017. [Google Scholar] [CrossRef]
- Hopf, F.W.; Lesscher, H.M.B. Rodent models for compulsive alcohol intake. Alcohol 2014, 48, 253–264. [Google Scholar] [CrossRef]
- Pelloux, Y.; Everitt, B.J.; Dickinson, A. Compulsive drug seeking by rats under punishment: Effects of drug taking history. Psychopharmacology 2007, 194, 127–137. [Google Scholar] [CrossRef]
- Smith, K.L.; Rao, R.R.; Velázquez-Sánchez, C.; Valenza, M.; Giuliano, C.; Everitt, B.J.; Sabino, V.; Cottone, P. The Uncompetitive N-methyl-D-Aspartate Antagonist Memantine Reduces Binge-Like Eating, Food-Seeking Behavior, and Compulsive Eating: Role of the Nucleus Accumbens Shell. Neuropsychopharmacol. Off. Publ. Am. Coll. Neuropsychopharmacol. 2015, 40, 1163–1171. [Google Scholar] [CrossRef] [PubMed]
- Vanderschuren, L.J.M.J.; Everitt, B.J. Drug Seeking Becomes Compulsive After Prolonged Cocaine Self-Administration. Science 2004, 305, 1017–1019. [Google Scholar] [CrossRef] [PubMed]
- Velázquez-Sánchez, C.; Ferragud, A.; Moore, C.F.; Everitt, B.J.; Sabino, V.; Cottone, P. High Trait Impulsivity Predicts Food Addiction-Like Behavior in the Rat. Neuropsychopharmacol. Off. Publ. Am. Coll. Neuropsychopharmacol. 2014, 39, 2463–2472. [Google Scholar] [CrossRef]
- Schroder, R.; Sellman, J.D.; Adamson, S. Development and Validation of a Brief Measure of Eating Compulsivity (MEC). Subst. Use Misuse 2017, 52, 1918–1924. [Google Scholar] [CrossRef]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef]
- Guillemin, F.; Bombardier, C.; Beaton, D.E. Cross-cultural adaptation of health-related quality of life measures: Literature review and proposed guidelines. J. Clin. Epidemiol. 1993, 46, 1417–1432. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.A.; Panzeri, A.; Mannarini, S. The Italian Version of the Difficulties in Emotion Regulation Scale–Short Form (IT-DERS-SF): A Two-step Validation Study. J. Psychopathol. Behav. Assess. 2022. [CrossRef]
- Parola, A.; Pettignano, M.; Marcionetti, J. Development and Validation of the Teacher Career-Related Support Self-Efficacy (TCSSE) Questionnaire. Behav. Sci. 2023, 13, 36. [Google Scholar] [CrossRef] [PubMed]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Muthén, B.; Asparouhov, T. Latent variable analysis with categorical outcomes: Multiple-group and growth modeling in Mplus. Mplus. Web Notes 2002, 9, 1–22. [Google Scholar]
- Yu, C.Y. Evaluating Cutoff Criteria of Model Fit Indices for Latent Variable Models with Binary and Continuous Outcomes; University of California: Los Angeles, CA, USA, 2002. [Google Scholar]
- Imperatori, C.; Fabbricatore, M.; Lester, D.; Manzoni, G.M.; Castelnuovo, G.; Raimondi, G.; Innamorati, M. Psychometric properties of the modified Yale Food Addiction Scale Version 2.0 in an Italian non-clinical sample. Eat. Weight Disord. 2019, 24, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Schulte, E.M.; Gearhardt, A.N. Development of the Modified Yale Food Addiction Scale Version 2.0. Eur. Eat. Disord. Rev. J. Eat. Disord. Assoc. 2017, 25, 302–308. [Google Scholar] [CrossRef] [PubMed]
- Aloi, M.; Rania, M.; Rodriguez Munoz, R.C.; Jimenez Murcia, S.; Fernandez-Aranda, F.; De Fazio, P.; Segura-Garcia, C. Validation of the Italian version of the Yale Food Addiction Scale 2.0 (I-YFAS 2.0) in a sample of undergraduate students. Eat. Weight Disord. EWD 2017, 22, 527–533. [Google Scholar] [CrossRef]
- Manzoni, G.M.; Rossi, A.; Pietrabissa, G.; Mannarini, S.; Fabbricatore, M.; Imperatori, C.; Innamorati, M.; Gearhardt, A.N.; Castelnuovo, G. Structural validity, measurement invariance, reliability and diagnostic accuracy of the Italian version of the Yale Food Addiction Scale 2.0 in patients with severe obesity and the general population. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2021, 26, 345–366. [Google Scholar] [CrossRef]
- Meule, A.; Gearhardt, A.N. Ten Years of the Yale Food Addiction Scale: A Review of Version 2.0. Curr. Addict. Rep. 2019, 6, 218–228. [Google Scholar] [CrossRef]
- Gormally, J.; Black, S.; Daston, S.; Rardin, D. The assessment of binge eating severity among obese persons. Addict. Behav. 1982, 7, 47–55. [Google Scholar] [CrossRef]
- Ricca, V.; Mannucci, E.; Moretti, S.; Di Bernardo, M.; Zucchi, T.; Cabras, P.L.; Rotella, C.M. Screening for binge eating disorder in obese outpatients. Compr. Psychiatry 2000, 41, 111–115. [Google Scholar] [CrossRef]
- Manzoni, G.M.; Rossi, A.; Pietrabissa, G.; Varallo, G.; Molinari, E.; Poggiogalle, E.; Donini, L.M.; Tarrini, G.; Melchionda, N.; Piccione, C.; et al. Validation of the Italian Yale Food Addiction Scale in postgraduate university students. Eat. Weight Disord. 2018, 23, 167–176. [Google Scholar] [CrossRef]
- Imperatori, C.; Innamorati, M.; Lamis, D.A.; Contardi, A.; Continisio, M.; Castelnuovo, G.; Manzoni, G.M.; Fabbricatore, M. Factor Structure of the Binge Eating Scale in a Large Sample of Obese and Overweight Patients Attending Low Energy Diet Therapy. Eur. Eat. Disord. Rev. J. Eat. Disord. Assoc. 2016, 24, 174–178. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2017. [Google Scholar]
- R Core Team. The R project for statistical computing. 2014. Available online: https://www.r-project.org/ (accessed on 6 March 2023).
- Wei, T.; Simko, V. R package “corrplot”: Visualization of a Correlation Matrix, Version 0.84; CRAN Repository: Vienna, Austria, 2017. [Google Scholar]
- Rosseel, Y. lavaan: An R Package for Structural Equation Modeling. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef]
- Rosseel, Y.; Oberski, D.; Byrnes, J.; Vanbrabant, L.; Savalei, V.; Merkle, E.; Hallquist, M.; Rhemtulla, M.; Katsikatsou, M.; Barendse, M. Package ‘lavaan’; R Foundation for Statistical Computing: Vienna, Austria, 2015. [Google Scholar]
- Jackman, S. pscl: Classes and Methods for R Developed in the Political Science Computational Laboratory; R package 1.5.5; United States Studies Centre, University of Sydney: Sydney, NSW, Australia, 2020. [Google Scholar]
- Zeileis, A.; Kleiber, C.; Jackman, S. Regression Models for Count Data in R. J. Stat. Softw. 2008, 27, 1–25. [Google Scholar] [CrossRef]
- Revelle, W. psych: Procedures for Personality and Psychological Research; Northwestern University: Evanston, IL, USA, 2018. [Google Scholar]
- Revelle, W. psychTools: Tools to Accompany the ‘psych’ Package for Psychological Research, 2.0.6; Northwestern University: Evanston, IL, USA, 2020. [Google Scholar]
- semTools Contributors. semTools: Useful Tools for Structural Equation Modeling. R Package Version 0.4-14. 2016. Available online: https://cran.r-project.org/web/packages/semTools/semTools.pdf (accessed on 6 March 2023).
- Wickham, H.; Averick, M.; Bryan, J.; Chang, W.; McGowan, L.D.; François, R.; Grolemund, G.; Hayes, A.; Henry, L.; Hester, J.; et al. Welcome to the tidyverse. J. Open Source Softw. 2019, 4, 1686. [Google Scholar] [CrossRef]
- Epskamp, S. semPlot: Path Diagrams and Visual Analysis of Various SEM Packages’ Output, 1.1.2. 2019. Available online: https://cran.r-project.org/web/packages/semPlot/semPlot.pdf (accessed on 6 March 2023).
- Brown, T.A. Confirmatory Factor Analysis for Applied Research, 2nd ed.; The Guilford Press: New York, NY, USA, 2015. [Google Scholar]
- Hoyle, R.H. Handbook of Strucural Equation Modeling; The Guilford Press: New York, NY, USA, 2012. [Google Scholar]
- Kline, R.B. Principles and Practice of Structural Equation Modeling; The Guilford Press: New York, NY, USA, 2016. [Google Scholar]
- Lionetti, F.; Keijsers, L.; Dellagiulia, A.; Pastore, M. Evidence of factorial validity of parental knowledge, control and solicitation, and adolescent disclosure scales: When the ordered nature of Likert scales matters. Front. Psychol. 2016, 7, 941. [Google Scholar] [CrossRef] [PubMed]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 8th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2017. [Google Scholar]
- van de Schoot, R.; Lugtig, P.; Hox, J. A checklist for testing measurement invariance. Eur. J. Dev. Psychol. 2012, 9, 486–492. [Google Scholar] [CrossRef]
- McDonald, R.P. Test Theory: A Unified Treatment; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1999. [Google Scholar]
- McDonald, R.P.; Ho, M.-H.R. Principles and practice in reporting structural equation analyses. Psychol. Methods 2002, 7, 64–82. [Google Scholar] [CrossRef]
- McDonald, R.P.; Mulaik, S.A. Determinacy of common factors. Psychol. Bull. 1979, 86, 297–306. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics; Pearson: Harlow, UK, 2014. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1988. [Google Scholar]
- Consoli, S.; Rossi, A.; Thompson, L.Y.; Volpi, C.; Mannarini, S.; Castelnuovo, G.; Molinari, E. Assessing Psychometric Properties of the Italian Version of the Heartland Forgiveness Scale. Front. Psychol. 2020, 11, 596501. [Google Scholar] [CrossRef]
- Van Strien, T.; Frijters, J.E.R.; Bergers, G.P.A.; Defares, P.B. The Dutch Eating Behaviour Questionnaire (DEBQ) for assessment of restrained, emotional and external eating behaviour. Int. J. Eat. Disord. 1986, 5, 747–755. [Google Scholar] [CrossRef]
- Dakanalis, A.; Zanetti, M.A.; Clerici, M.; Madeddu, F.; Riva, G.; Caccialanza, R. Italian version of the Dutch Eating Behavior Questionnaire. Psychometric proprieties and measurement invariance across sex, BMI-status and age. Appetite 2013, 71, 187–195. [Google Scholar] [CrossRef]
- Van Strien, T.; Herman, C.P.; Verheijden, M.W. Eating style, overeating and weight gain. A prospective 2-year follow-up study in a representative Dutch sample. Appetite 2013, 59, 782–789. [Google Scholar] [CrossRef] [PubMed]
- Riva, G.; Molinari, E. Clinical Psychology of Obesity; Boringhieri, B., Ed.; Bollati Boringhieri: Turin, Italy, 2004. [Google Scholar]
- Wickham, H. ggplot2: Elegant Graphics for Data Analysis; Springer-Verlag: New York, NY, USA, 2016. [Google Scholar]
- Sachs, M.C. plotROC: A Tool for Plotting ROC Curves. J. Stat. Softw. 2017, 79, 1–19. [Google Scholar] [CrossRef]
- Robin, X.; Turck, N.; Hainard, A.; Tiberti, N.; Lisacek, F.; Sanchez, J.; Müller, M. pROC: An open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinform. 2011, 12, 77. [Google Scholar] [CrossRef]
- Vandenberg, R.J.; Lance, C.E. A Review and Synthesis of the Measurement Invariance Literature: Suggestions, Practices, and Recommendations for Organizational Research. Organ. Res. Methods 2000, 3, 4–70. [Google Scholar] [CrossRef]
- Meredith, W. Measurement invariance, factor analysis and factorial invariance. Psychometrika 1993, 58, 525–543. [Google Scholar] [CrossRef]
- Millsap, R.E. Statistical Approaches to Measurement Invariance; Routledge: New York, NY, USA, 2012; pp. 1–368. [Google Scholar]
- Millsap, R.E.; Yun-Tein, J. Assessing Factorial Invariance in Ordered-Categorical Measures. Multivar. Behav. Res. 2004, 39, 479–515. [Google Scholar] [CrossRef]
- Rossi, A.A.; Panzeri, A.; Taccini, F.; Parola, A.; Mannarini, S. The Rising of the Shield Hero. Development of the Post-Traumatic Symptom Questionnaire (PTSQ) and Assessment of the Protective Effect of Self-Esteem from Trauma-Related Anxiety and Depression. J. Child Adolesc. Trauma 2022. [Google Scholar] [CrossRef]
- Cheung, G.W.; Rensvold, R.B. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct. Equ. Model. 2002, 9, 233–255. [Google Scholar] [CrossRef]
- Shevlin, M.; Butter, S.; McBride, O.; Murphy, J.; Gibson-Miller, J.; Hartman, T.K.; Levita, L.; Mason, L.; Martinez, A.P.; McKay, R.; et al. Measurement invariance of the Patient Health Questionnaire (PHQ-9) and Generalized Anxiety Disorder scale (GAD-7) across four European countries during the COVID-19 pandemic. BMC Psychiatry 2022, 22, 154. [Google Scholar] [CrossRef]
- Chiorri, C. Teoria e Tecnica Psicometrica. Costruire un Test Psicologico; McGraw-Hill Companies: New York, NY, USA, 2011. [Google Scholar]
- Ebel, R.L. Measuring Educational Achievement; Prentice-Hall: Englewood Cliffs, NJ, USA, 1965. [Google Scholar]
- Pallant, J. SPSS Survival Manual; McGraw-Hill Education: New York, NY, USA, 2013. [Google Scholar]
- Howell, D.C. Statistical Methods for Psychology; Wadsworth, Cengage Learning: Belmont, CA, USA, 2013. [Google Scholar]
- Pepe, M.S. The Statistical Evaluation of Medical Tests for Classification and Prediction; Oxford Universtiy Press: New York, NY, USA, 2003. [Google Scholar]
- Zhou, X.H.; Obuchowski, N.A.; McClish, D. Statistical Methods in Diagnostic Medicine; Wiley: New York, NY, USA, 2002. [Google Scholar]
- Swets, J.A. Measuring the accuracy of diagnostic systems. Science 1998, 240, 1285–1293. [Google Scholar] [CrossRef]
- Zweig, M.H.; Campbell, G. Receiver-operating characteristic (ROC) plots: A fundamental evaluation tool in clinical medicine. Clin. Chem. 1993, 39, 561–577. [Google Scholar] [CrossRef]
- Davis, C. From Passive Overeating to “Food Addiction”: A Spectrum of Compulsion and Severity. Int. Sch. Res. Not. 2013, 2013, 435027. [Google Scholar] [CrossRef]
- Meule, A. Food addiction and body-mass-index: A non-linear relationship. Med. Hypotheses 2012, 79, 508–511. [Google Scholar] [CrossRef] [PubMed]
- Steiger, J.H. Structural Model Evaluation and Modification: An Interval Estimation Approach. Multivar. Behav. Res. 1990, 25, 173–180. [Google Scholar] [CrossRef]
- Bentler, P.M. Comparative fit indexes in structural models. Psychol. Bull. 1990, 107, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Bentler, P.M.; Bonett, D.G. Significance tests and goodness of fit in the analysis of covariance structures. Psychol. Bull. 1980, 88, 588–606. [Google Scholar] [CrossRef]
- Manzoni, G.M.; Rossi, A.; Marazzi, N.; Agosti, F.; De Col, A.; Pietrabissa, G.; Castelnuovo, G.; Molinari, E.; Sartorio, A. Feasibility, Validity, and Reliability of the Italian Pediatric Quality of Life Inventory Multidimensional Fatigue Scale for Adults in Inpatients with Severe Obesity. Obes. Facts 2018, 11, 25–36. [Google Scholar] [CrossRef] [PubMed]
- Pietrabissa, G.; Rossi, A.; Borrello, M.; Manzoni, G.M.; Mannarini, S.; Castelnuovo, G.; Molinari, E. Development and Validation of a Self-Determination Theory-Based Measure of Motivation to Exercise and Diet in Children. Front. Psychol. 2020, 11, 1299. [Google Scholar] [CrossRef] [PubMed]
- Davis, C. A narrative review of binge eating and addictive behaviors: Shared associations with seasonality and personality factors. Front. Psychiatry 2013, 4, 183. [Google Scholar] [CrossRef] [PubMed]
- Dingemans, A.E.; Bruna, M.J.; van Furth, E.F. Binge eating disorder: A review. Int. J. Obes. Relat. Metab. Disord. 2002, 26, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.; Curtis, C.; Levitan, R.D.; Carter, J.C.; Kaplan, A.S.; Kennedy, J.L. Evidence that ’food addiction’ is a valid phenotype of obesity. Appetite 2011, 57, 711–717. [Google Scholar] [CrossRef]
- Rossi, A.A.; Mannarini, S.; Castelnuovo, G.; Pietrabissa, G. Disordered Eating Behaviors Related to Food Addiction/Eating Addiction in Inpatients with Obesity and the General Population: The Italian Version of the Addiction-like Eating Behaviors Scale (AEBS-IT). Nutrients 2023, 15, 104. [Google Scholar] [CrossRef] [PubMed]
- Gearhardt, A.N.; White, M.A.; Masheb, R.M.; Morgan, P.T.; Crosby, R.D.; Grilo, C.M. An examination of the food addiction construct in obese patients with binge eating disorder. Int. J. Eat. Disord. 2012, 45, 657–663. [Google Scholar] [CrossRef] [PubMed]
- Castelnuovo, G.; Pietrabissa, G.; Cattivelli, R.; Manzoni, G.M.; Molinari, E. Not Only Clinical Efficacy in Psychological Treatments: Clinical Psychology Must Promote Cost-Benefit, Cost-Effectiveness, and Cost-Utility Analysis. Front. Psychol. 2016, 7, 563. [Google Scholar] [CrossRef]
| Descriptive Statistics | CFA | ||||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Sk | K | λ | R2 | ||
| 1 | I have urges to eat a lot of the time | 1.111 | 1.160 | 0.709 | −0.560 | 0.809 | 0.655 |
| Sento il desiderio di mangiare per la maggior parte del tempo | |||||||
| 2 | I feel disturbed about my urges to eat | 1.235 | 1.227 | 0.586 | −0.858 | 0.778 | 0.605 |
| Mi sento a disagio a causa del mio desiderio di mangiare | |||||||
| 3 | I have very little control over my eating | 1.741 | 1.302 | 0.114 | −1.161 | 0.828 | 0.686 |
| Ho pochissimo controllo sul mio modo di mangiare | |||||||
| 4 | I often fear losing control of my eating | 1.735 | 1.373 | 0.089 | −1.309 | 0.869 | 0.756 |
| Spesso temo di perdere il controllo sul mio modo di mangiare | |||||||
| 5 | I am not able to control how much I eat in the presence of any food | 1.588 | 1.229 | 0.205 | −1.015 | 0.847 | 0.718 |
| In presenza di cibo, non sono in grado di controllare quanto mangio | |||||||
| 6 | I often feel out of control around certain foods | 1.788 | 1.318 | 0.046 | −1.192 | 0.816 | 0.666 |
| Spesso mi sento fuori controllo in presenza di certi cibi | |||||||
| 7 | Food is like a drug to me | 1.369 | 1.321 | 0.560 | −0.871 | 0.838 | 0.702 |
| Il cibo è come una droga per me | |||||||
| 8 | It worries me how little control I have over my eating | 1.759 | 1.327 | 0.113 | −1.164 | 0.851 | 0.724 |
| Mi preoccupa quanto poco controllo io abbia sul mio modo di mangiare | |||||||
| 9 | When I come across a very tasty food I can’t stop thinking about it | 1.973 | 1.293 | −0.130 | −1.085 | 0.766 | 0.587 |
| Quando mi trovo davanti a un cibo molto gustoso, non riesco a smettere di pensarci | |||||||
| 10 | I feel defeated by food | 1.529 | 1.302 | 0.282 | −1.095 | 0.843 | 0.711 |
| Mi sento sconfitto dal cibo. | |||||||
| Inpatients with Severe Obesity | |||||||||
| Descriptive Statistics | Items Psychometric Properties | CFA | |||||||
| Mean | SD | SK | K | t | d | r(it-tot) | λ | R2 | |
| Item#1 | 1.17 | 1.197 | 0.687 | −0.548 | −21.68 | 2.92 | 0.704 | 0.788 | 0.620 |
| Item#2 | 1.30 | 1.299 | 0.546 | −1.034 | −26.75 | 3.59 | 0.720 | 0.792 | 0.627 |
| Item#3 | 1.77 | 1.266 | −0.004 | −1.151 | −29.45 | 3.92 | 0.780 | 0.848 | 0.719 |
| Item#4 | 1.76 | 1.334 | 0.083 | −1.239 | −29.38 | 3.92 | 0.763 | 0.837 | 0.700 |
| Item#5 | 1.64 | 1.268 | 0.182 | −1.070 | −29.47 | 3.95 | 0.800 | 0.866 | 0.750 |
| Item#6 | 1.83 | 1.336 | 0.037 | −1.237 | −33.66 | 4.49 | 0.798 | 0.874 | 0.764 |
| Item#7 | 1.42 | 1.342 | 0.481 | −1.024 | −29.55 | 3.97 | 0.798 | 0.870 | 0.758 |
| Item#8 | 1.83 | 1.335 | 0.047 | −1.190 | −27.35 | 3.63 | 0.787 | 0.843 | 0.711 |
| Item#9 | 2.04 | 1.315 | −0.171 | −1.088 | −23.89 | 3.18 | 0.738 | 0.809 | 0.655 |
| Item#10 | 1.58 | 1.375 | 0.369 | −1.097 | −28.39 | 3.79 | 0.766 | 0.833 | 0.694 |
| General Population | |||||||||
| Descriptive Statistics | Items Psychometric Properties | CFA | |||||||
| Mean | SD | SK | K | t | d | r(it-tot) | λ | R2 | |
| Item#1 | 1.18 | 1.026 | 0.527 | −0.616 | −15.76 | 2.52 | 0.650 | 0.737 | 0.543 |
| Item#2 | 0.79 | 1.081 | 1.264 | 0.615 | −15.94 | 2.52 | 0.758 | 0.861 | 0.742 |
| Item#3 | 0.99 | 1.063 | 1.020 | 0.438 | −15.68 | 2.49 | 0.689 | 0.770 | 0.592 |
| Item#4 | 1.13 | 1.261 | 0.776 | −0.658 | −23.62 | 3.75 | 0.743 | 0.836 | 0.698 |
| Item#5 | 1.03 | 1.003 | 0.786 | 0.064 | −21.81 | 3.48 | 0.790 | 0.866 | 0.750 |
| Item#6 | 1.25 | 1.226 | 0.575 | −0.843 | −25.01 | 3.98 | 0.742 | 0.825 | 0.680 |
| Item#7 | 0.98 | 1.151 | 1.040 | 0.156 | −17.70 | 2.80 | 0.769 | 0.857 | 0.735 |
| Item#8 | 0.77 | 1.097 | 1.383 | 0.995 | −18.35 | 2.90 | 0.831 | 0.929 | 0.863 |
| Item#9 | 1.38 | 1.214 | 0.458 | −0.772 | −20.48 | 3.27 | 0.696 | 0.778 | 0.606 |
| Item#10 | 0.68 | 1.080 | 1.517 | 1.316 | −14.13 | 2.24 | 0.746 | 0.864 | 0.746 |
| First Regression Analysis (ZINB GML)—Dependent Variable: mYFAS2.0 Symptom Count | |||||||
| Predictors | β | se | z | p-Value | pseudoR2 | ΔpseudoR2 | |
| Block 1 | BES FC(CM) | 0.080 | 0.017 | 4.770 | <0.001 | ||
| BES B(CM) | 0.017 | 0.015 | 1.152 | 0.249 | |||
| DEBQ EE(CM) | 0.116 | 0.079 | 1.467 | 0.142 | |||
| DEBQ ExE(CM) | 0.101 | 0.065 | 1.560 | 0.119 | |||
| BES FC(ZI) | −0.188 | 0.065 | −2.898 | 0.003 | |||
| BES B (ZI) | −0.145 | 0.072 | −1.995 | 0.046 | |||
| DEBQ EE (ZI) | 0.602 | 0.311 | 1.932 | 0.053 | |||
| DEBQ ExE (ZI) | −0.401 | 0.243 | −1.652 | 0.098 | 0.476 | ||
| Block 2 | BES FC(CM) | 0.053 | 0.016 | 3.283 | 0.001 | ||
| BES B(CM) | 0.008 | 0.014 | 0.553 | 0.580 | |||
| DEBQ EE(CM) | 0.094 | 0.060 | 1.557 | 0.119 | |||
| DEBQ ExE(CM) | −0.007 | 0.078 | −0.095 | 0.924 | |||
| MEC(CM) | 0.030 | 0.007 | 4.135 | 0.001 | |||
| BES FC(ZI) | −0.098 | 0.071 | −1.374 | 0.169 | |||
| BES B(ZI) | −0.018 | 0.071 | −0.260 | 0.795 | |||
| DEBQ EE(ZI) | −0.185 | 0.275 | −0.673 | 0.501 | |||
| DEBQ ExE(ZI) | 0.870 | 0.344 | 2.527 | 0.011 | |||
| MEC(ZI) | −0.144 | 0.031 | −4.672 | <0.001 | 0.549 | 0.074 | |
| Second Regression Analysis (LM)—Dependent Variable: Binge Eating Tendencies (BES) | |||||||
| Predictors | β | se | t | p-Value | Radj2 | ΔRadj2 | |
| Block 1 | DEBQ EE | 3.033 | 0.332 | 9.143 | <0.001 | ||
| DEBQ ExE | 1.085 | 0.430 | 2.523 | 0.012 | |||
| mYFAS2.0 | 1.608 | 0.120 | 13.385 | <0.001 | 0.653 | ||
| Block 2 | DEBQ EE | 1.970 | 0.316 | 6.230 | <0.001 | ||
| DEBQ ExE | 0.071 | 0.399 | 0.179 | 0.858 | |||
| mYFAS2.0 | 0.923 | 0.128 | 7.184 | <0.001 | |||
| MEC | 0.367 | 0.038 | 9.708 | <0.001 | 0.722 | 0.069 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rossi, A.A.; Pietrabissa, G.; Gearhardt, A.N.; Musetti, A.; Castelnuovo, G.; Mannarini, S. Eating Compulsivity in Inpatients with Severe Obesity and the General Population: The Italian Version of the Measure of Eating Compulsivity (MEC10-IT). Nutrients 2023, 15, 1378. https://doi.org/10.3390/nu15061378
Rossi AA, Pietrabissa G, Gearhardt AN, Musetti A, Castelnuovo G, Mannarini S. Eating Compulsivity in Inpatients with Severe Obesity and the General Population: The Italian Version of the Measure of Eating Compulsivity (MEC10-IT). Nutrients. 2023; 15(6):1378. https://doi.org/10.3390/nu15061378
Chicago/Turabian StyleRossi, Alessandro Alberto, Giada Pietrabissa, Ashley N. Gearhardt, Alessandro Musetti, Gianluca Castelnuovo, and Stefania Mannarini. 2023. "Eating Compulsivity in Inpatients with Severe Obesity and the General Population: The Italian Version of the Measure of Eating Compulsivity (MEC10-IT)" Nutrients 15, no. 6: 1378. https://doi.org/10.3390/nu15061378
APA StyleRossi, A. A., Pietrabissa, G., Gearhardt, A. N., Musetti, A., Castelnuovo, G., & Mannarini, S. (2023). Eating Compulsivity in Inpatients with Severe Obesity and the General Population: The Italian Version of the Measure of Eating Compulsivity (MEC10-IT). Nutrients, 15(6), 1378. https://doi.org/10.3390/nu15061378








