Mental Health during the Interpregnancy Period and the Association with Pre-Pregnancy Body Mass Index and Body Composition: Data from the INTER-ACT Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Measurements
2.4. Outcomes
2.5. Data Analyses
3. Results
3.1. Participant Characteristics
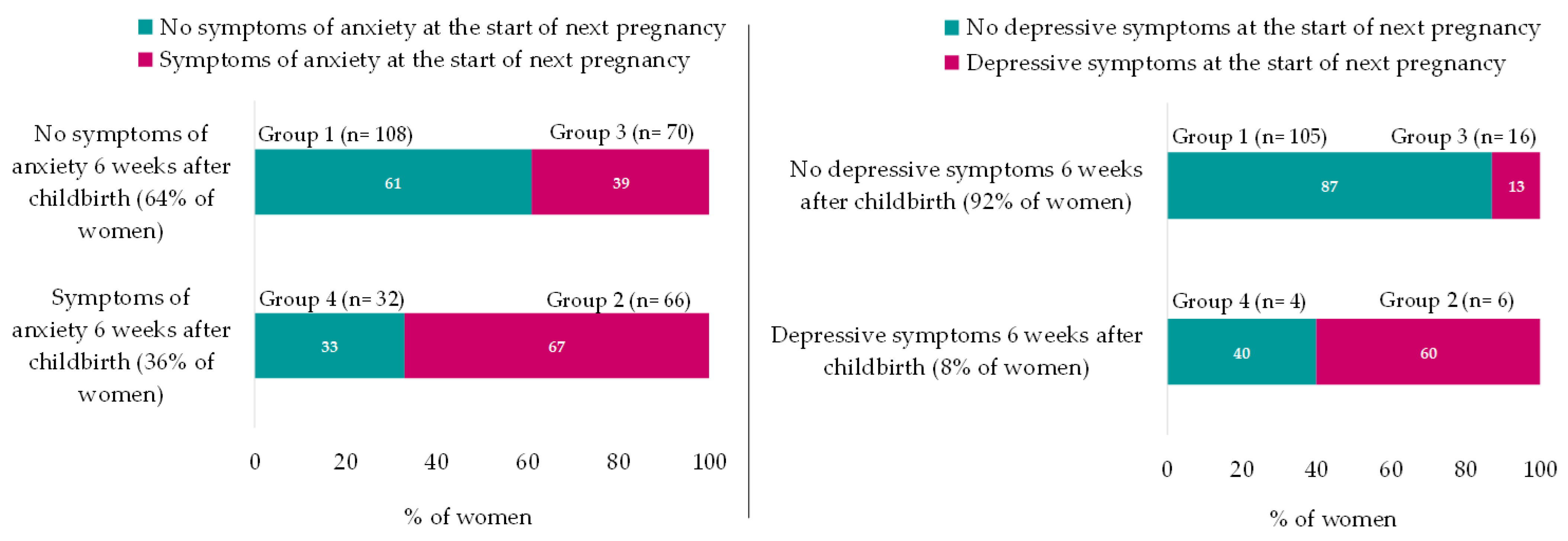
3.2. Differences in Mental Health between 6 Weeks after Childbirth and Start of Next Pregnancy
3.3. Mental-Health-Related Characteristics
3.3.1. Socio-Demographic Factors and Interpregnancy Interval
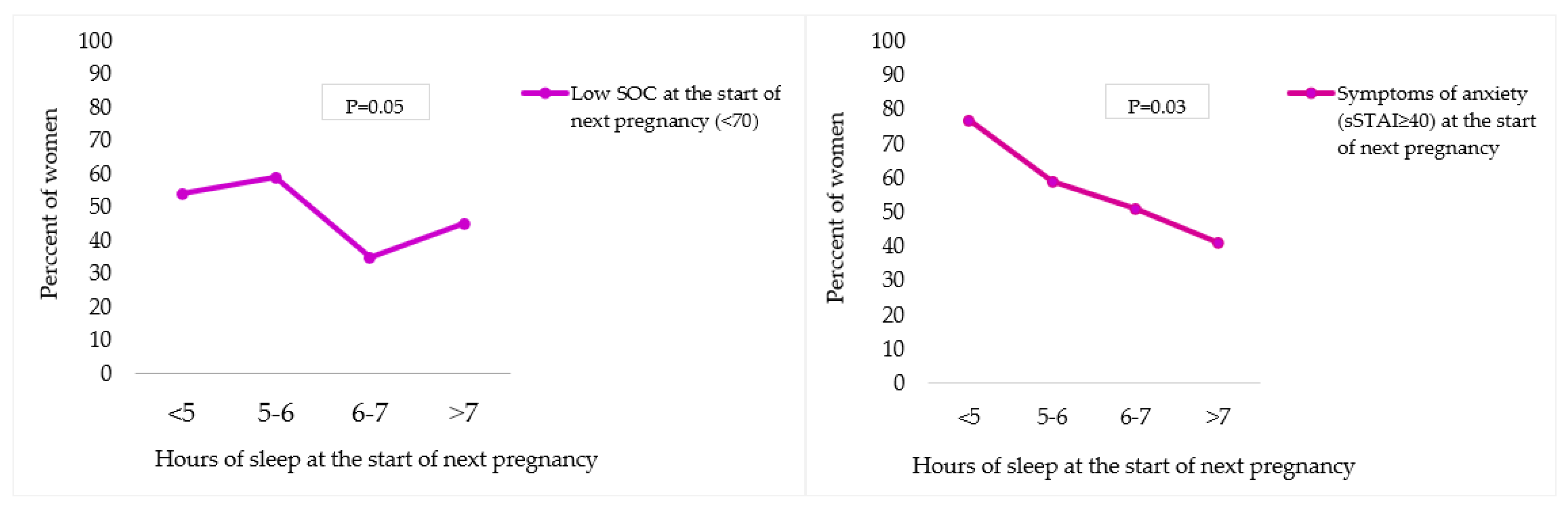
3.3.2. Sleep
3.4. Association with Pre-Pregnancy BMI and Body Composition
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO Guide for Integration of Perinatal Mental Health in Maternal and Child Health Services; World Health Organization (WHO): Geneva, Switzerland, 2022; p. 66. [Google Scholar]
- Geier, M.L.; Hills, N.; Gonzales, M.; Tum, K.; Finley, P.R. Detection and treatment rates for perinatal depression in a state Medicaid population. CNS Spectr. 2015, 20, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Yeaton-Massey, A.; Herrero, T. Recognizing maternal mental health disorders: Beyond postpartum depression. Curr. Opin. Obstet. Gynecol. 2019, 31, 116–119. [Google Scholar] [CrossRef] [PubMed]
- Cox, E.Q.; Sowa, N.A.; Meltzer-Brody, S.E.; Gaynes, B.N. The Perinatal Depression Treatment Cascade: Baby Steps toward Improving Outcomes. J. Clin. Psychiatry 2016, 77, 1189–1200. [Google Scholar] [CrossRef] [PubMed]
- Callanan, F.; Tuohy, T.; Bright, A.M.; Grealish, A. The effectiveness of psychological interventions for pregnant women with anxiety in the antenatal period: A systematic review. Midwifery 2022, 104, 103169. [Google Scholar] [CrossRef]
- Maternal Mental Health Alliance. Perinatal Mental Health. Available online: https://maternalmentalhealthalliance.org/about/perinatal-mental-health/ (accessed on 20 June 2023).
- Zanardo, V.; Giliberti, L.; Giliberti, E.; Grassi, A.; Perin, V.; Parotto, M.; Soldera, G.; Straface, G. The role of gestational weight gain disorders in symptoms of maternal postpartum depression. Int. J. Gynaecol. Obstet. 2021, 153, 234–238. [Google Scholar] [CrossRef]
- Cunningham, S.D.; Bs, S.M.; Chai, H.; Lewis, J.B.; Levine, J.; Tobin, J.N.; Ickovics, J.R. Postpartum Depressive Symptoms: Gestational Weight Gain as a Risk Factor for Adolescents Who Are Overweight or Obese. J. Midwifery Women’s Health 2018, 63, 178–184. [Google Scholar] [CrossRef]
- Dachew, B.A.; Ayano, G.; Betts, K.; Alati, R. The impact of pre-pregnancy BMI on maternal depressive and anxiety symptoms during pregnancy and the postpartum period: A systematic review and meta-analysis. J. Affect. Disord. 2021, 281, 321–330. [Google Scholar] [CrossRef]
- Zhao, X.H.; Zhang, Z.H. Risk factors for postpartum depression: An evidence-based systematic review of systematic reviews and meta-analyses. Asian J. Psychiatry 2020, 53, 102353. [Google Scholar]
- Bliddal, M.; Pottegård, A.; Kirkegaard, H.; Olsen, J.; Jørgensen, J.S.; Sørensen, T.I.; Wu, C.; A Nohr, E. Mental disorders in motherhood according to prepregnancy BMI and pregnancy-related weight changes—A Danish cohort study. J. Affect. Disord. 2015, 183, 322–329. [Google Scholar]
- Bazzazian, S.; Riazi, H.; Vafa, M.; Mahmoodi, Z.; Nasiri, M.; Mokhtaryan-Gilani, T.; Ozgoli, G. The relationship between depression, stress, anxiety, and postpartum weight retention: A systematic review. J. Educ. Health Promot. 2021, 10, 230. [Google Scholar]
- Bogaerts, A.F.; Van den Bergh, B.R.; Witters, I.; Devlieger, R. Anxiety during early pregnancy predicts postpartum weight retention in obese mothers. Obesity 2013, 21, 1942–1949. [Google Scholar] [CrossRef] [PubMed]
- Farias, D.R.; Carrilho, T.R.B.; Freitas-Costa, N.C.; Batalha, M.A.; Gonzalez, M.; Kac, G. Maternal mental health and gestational weight gain in a Brazilian Cohort. Sci. Rep. 2021, 11, 10787. [Google Scholar] [CrossRef] [PubMed]
- Ladyman, C.; Sweeney, B.; Sharkey, K.; Bei, B.; Wright, T.; Mooney, H.; Huthwaite, M.; Cunningham, C.; Firestone, R.; Signal, T.L. A scoping review of non-pharmacological perinatal interventions impacting maternal sleep and maternal mental health. BMC Pregnancy Childbirth 2022, 22, 659. [Google Scholar] [CrossRef] [PubMed]
- The International Weight Management in Pregnancy (i-WIP) Collaborative Group. Effect of diet and physical activity based interventions in pregnancy on gestational weight gain and pregnancy outcomes: Meta-analysis of individual participant data from randomised trials. BMJ 2017, 358, j3119. [Google Scholar]
- Ferrara, A.; Hedderson, M.M.; Brown, S.D.; Ehrlich, S.F.; Tsai, A.-L.; Feng, J.; Galarce, M.; Marcovina, S.; Catalano, P.; Quesenberry, C.P. A telehealth lifestyle intervention to reduce excess gestational weight gain in pregnant women with overweight or obesity (GLOW): A randomised, parallel-group, controlled trial. Lancet Diabetes Endocrinol. 2020, 8, 490–500. [Google Scholar] [CrossRef]
- Leonard, S.A.; Rasmussen, K.M.; King, J.C.; Abrams, B. Trajectories of maternal weight from before pregnancy through postpartum and associations with childhood obesity. Am. J. Clin. Nutr. 2017, 106, 1295–1301. [Google Scholar] [CrossRef]
- Lally, P.; van Jaarsveld, C.H.; Potts, H.W.; Wardle, J. How are habits formed: Modelling habit formation in the real world. Eur. J. Soc. Psychol. 2010, 40, 998–1009. [Google Scholar] [CrossRef]
- Bogaerts, A.F.; Devlieger, R.; Nuyts, E.; Witters, I.; Gyselaers, W.; Van den Bergh, B.R. Effects of lifestyle intervention in obese pregnant women on gestational weight gain and mental health: A randomized controlled trial. Int. J. Obes. 2013, 37, 814–821. [Google Scholar] [CrossRef]
- Sanaati, F.; Charandabi, S.M.; Eslamlo, H.F.; Mirghafourvand, M. A randomized controlled trial on the effect of lifestyle education for Iranian women and their husbands on post-partum anxiety and depression. Health Educ. Res. 2018, 33, 416–428. [Google Scholar] [CrossRef]
- Dodd, J.M.; Deussen, A.R.; Louise, J. A Randomised Trial to Optimise Gestational Weight Gain and Improve Maternal and Infant Health Outcomes through Antenatal Dietary, Lifestyle and Exercise Advice: The OPTIMISE Randomised Trial. Nutrients 2019, 11, 2911. [Google Scholar] [CrossRef]
- Altazan, A.D.; Redman, L.M.; Burton, J.H.; Beyl, R.A.; Cain, L.E.; Sutton, E.F.; Martin, C.K. Mood and quality of life changes in pregnancy and postpartum and the effect of a behavioral intervention targeting excess gestational weight gain in women with overweight and obesity: A parallel-arm randomized controlled pilot trial. BMC Pregnancy Childbirth. 2019, 19, 50. [Google Scholar] [CrossRef]
- Chojenta, C.; William, J.; Martin, M.A.; Byles, J.; Loxton, D. The impact of a history of poor mental health on health care costs in the perinatal period. Arch. Women’s Ment. Health 2019, 22, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Van Uytsel, H.; Ameye, L.; Devlieger, R.; Bijlholt, M.; Jacquemyn, Y.; Catry, V.; Schreurs, A.; Bogaerts, A. Mental health after childbirth and the impact on postpartum weight retention and body composition. Data from the INTER-ACT randomized controlled trial. Clin. Obes. 2022, 12, e12550. [Google Scholar] [CrossRef] [PubMed]
- Van Uytsel, H.; Bijlholt, M.; Devlieger, R.; Ameye, L.; Jochems, L.; van Holsbeke, C.; Schreurs, A.; Catry, V.; Bogaerts, A. Effect of the e-health supported INTER-ACT lifestyle intervention on postpartum weight retention and body composition, and associations with lifestyle behavior: A randomized controlled trial. Prev. Med. 2022, 164, 107321. [Google Scholar] [CrossRef] [PubMed]
- Bijlholt, M.; Ameye, L.; Van Uytsel, H.; Devlieger, R.; Bogaerts, A. The INTER-ACT E-Health Supported Lifestyle Intervention Improves Postpartum Food Intake and Eating Behavior, but Not Physical Activity and Sedentary Behavior-A Randomized Controlled Trial. Nutrients 2021, 13, 1287. [Google Scholar] [CrossRef] [PubMed]
- Bijlholt, M.; Ameye, L.; van Uytsel, H.; Devlieger, R.; Bogaerts, A. Evolution of Postpartum Weight and Body Composition after Excessive Gestational Weight Gain: The Role of Lifestyle Behaviors-Data from the INTER-ACT Control Group. Int. J. Environ. Res. Public Health 2021, 18, 6344. [Google Scholar] [CrossRef] [PubMed]
- Bijlholt, M.; Maslin, K.; Ameye, L.; Shawe, J.; Bogaerts, A.; Devlieger, R. Phase Angle and Bio-Impedance Values during the First Year after Delivery in Women with Previous Excessive Gestational Weight Gain: Innovative Data from the Belgian INTER-ACT Study. Int. J. Environ. Res. Public Health 2021, 18, 7482. [Google Scholar] [CrossRef] [PubMed]
- Bogaerts, A.; Ameye, L.; Bijlholt, M.; Amuli, K.; Heynickx, D.; Devlieger, R. INTER-ACT: Prevention of pregnancy complications through an e-health driven interpregnancy lifestyle intervention—Study protocol of a multicentre randomised controlled trial. BMC Pregnancy Childbirth 2017, 17, 154. [Google Scholar] [CrossRef]
- Institute of Medicine, National Research Council Committee to Reexamine IOMPWG. The National Academies Collection: Reports funded by National Institutes of Health. In Weight Gain During Pregnancy: Reexamining the Guidelines; Rasmussen, K.M., Yaktine, A.L., Eds.; National Academies Press: Washington, DC, USA, 2009. [Google Scholar]
- Falana, S.D.; Carrington, J.M. Postpartum Depression: Are You Listening? Nurs. Clin. N. Am. 2019, 54, 561–567. [Google Scholar] [CrossRef]
- National Collaborating Centre for Mental Health. Antenatal and Postnatal Mental Health: The NICE Guideline on Clinical Management and Service Guidance; British Psychological Society: Leicester, UK, 2018. [Google Scholar]
- Psouni, E.; Agebjörn, J.; Linder, H. Symptoms of depression in Swedish fathers in the postnatal period and development of a screening tool. Scand. J. Psychol. 2017, 58, 485–496. [Google Scholar]
- Madsen, S.A.; Juhl, T. Paternal depression in the postnatal period assessed with traditional and male depression scales. J. Men’s Health Gend. 2007, 4, 26–31. [Google Scholar] [CrossRef]
- Girardi, P.; Pompili, M.; Innamorati, M.; Serafini, G.; Berrettoni, C.; Angeletti, G.; Koukopoulos, A.; Tatarelli, R.; Lester, D.; Roselli, D.; et al. Temperament, post-partum depression, hopelessness, and suicide risk among women soon after delivering. Women Health 2011, 51, 511–524. [Google Scholar] [CrossRef] [PubMed]
- van der Bij, A.K.; de Weerd, S.; Cikot, R.J.; Steegers, E.A.; Braspenning, J.C. Validation of the dutch short form of the state scale of the Spielberger State-Trait Anxiety Inventory: Considerations for usage in screening outcomes. Community Genet. 2003, 6, 84–87. [Google Scholar] [CrossRef] [PubMed]
- Tendais, I.; Costa, R.; Conde, A.; Figueiredo, B. Screening for depression and anxiety disorders from pregnancy to postpartum with the EPDS and STAI. Span. J. Psychol. 2014, 17, E7. [Google Scholar] [CrossRef]
- Kruyen, P.M.; Emons, W.H.; Sijtsma, K. Shortening the S-STAI: Consequences for research and clinical practice. J. Psychosom. Res. 2013, 75, 167–172. [Google Scholar] [CrossRef]
- Furmli, H.; Seeto, R.A.; Hewko, S.L.; Dalfen, A.; Jones, C.A.; Murphy, K.E.; Bocking, A. Maternal Mental Health in Assisted and Natural Conception: A Prospective Cohort Study. J. Obstet. Gynaecol. Can. 2019, 41, 1608–1615. [Google Scholar] [CrossRef]
- Van Damme, R.; Van Parys, A.S.; Vogels, C.; Roelens, K.; Lemmens, G. Screening en Detectie van Perinatale Mentale Stoornissen: Richtlijn Als Leidraad Voor Het Ontwikkelen van Een Zorgpad; Universitair Ziekenhuis Gent: Brussel, Belgium; Universiteit Gent: Ghent, Belgium, 2018. [Google Scholar]
- Antonovsky, A. Unraveling the Mystery of Health: How People Manage Stress and Stay Well; Jossey-Bass: San Francisco, CA, USA, 1987. [Google Scholar]
- Marchand, M. (Shortened) Sense of Coherence. 2014. Available online: http://docplayer.nl/31755966-Shortened-sense-of-coherence.html (accessed on 20 June 2023).
- Austin, M.P.; Hadzi-Pavlovic, D.; Saint, K.; Parker, G. Antenatal screening for the prediction of postnatal depression: Validation of a psychosocial Pregnancy Risk Questionnaire. Acta Psychiatr. Scand. 2005, 112, 310–317. [Google Scholar] [CrossRef]
- Reilly, N.; Harris, S.; Loxton, D.; Chojenta, C.; Forder, P.; Austin, M.P. The impact of routine assessment of past or current mental health on help-seeking in the perinatal period. Women Birth 2014, 27, e20–e27. [Google Scholar] [CrossRef]
- Guelinckx, I.; Devlieger, R.; Bogaerts, A.; Pauwels, S.; Vansant, G. The effect of pre-pregnancy BMI on intention, initiation and duration of breast-feeding. Public Health Nutr. 2012, 15, 840–848. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Obuchowska, A.; Standyło, A.; Kimber-Trojnar, Ż.; Leszczyńska-Gorzelak, B. The Possibility of Using Bioelectrical Impedance Analysis in Pregnant and Postpartum Women. Diagnostics 2021, 11, 1370. [Google Scholar] [CrossRef] [PubMed]
- Bai, M.; Susic, D.; O’sullivan, A.J.; Henry, A. Reproducibility of Bioelectrical Impedance Analysis in Pregnancy and the Association of Body Composition with the Risk of Gestational Diabetes: A Substudy of MUMS Cohort. J. Obes. 2020, 2020, 3128767. [Google Scholar] [CrossRef] [PubMed]
- Ellegård, L.; Bertz, F.; Winkvist, A.; Bosaeus, I.; Brekke, H.K. Body composition in overweight and obese women postpartum: Bioimpedance methods validated by dual energy X-ray absorptiometry and doubly labeled water. Eur. J. Clin. Nutr. 2016, 70, 1181–1188. [Google Scholar] [CrossRef] [PubMed]
- Vatier, C.; Poitou, C.; Clément, K. Evaluation of Visceral Fat in Massive Obesity. In Nutrition in the Prevention and Treatment of Abdominal Obesity; Elsevier: Amsterdam, The Netherlands, 2014; pp. 67–77. [Google Scholar]
- National HES Manual. Belgium. 2011. Available online: https://ehes.info/manuals/national_manuals/national_manual_Belgium_EN.pdf (accessed on 20 June 2023).
- Mittelmark, M.B.; Bauer, G.F.; Vaandrager, L.; Pelikan, J.M.; Sagy, S.; Eriksson, M.; Lindström, B.; Meier Magistretti, C. (Eds.) The Handbook of Salutogenesis; Springer: Cham, Switzerland, 2017. [Google Scholar]
- Toivonen, K.I.; Oinonen, K.A.; Duchene, K.M. Preconception health behaviours: A scoping review. Prev. Med. 2017, 96, 1–15. [Google Scholar] [CrossRef]
- Opray, N.; Grivell, R.; Deussen, A.R.; Dodd, J. Directed preconception health programs and interventions for improving pregnancy outcomes for women who are overweight or obese. Cochrane Database Syst. Rev. 2015, 7, CD010932. [Google Scholar] [CrossRef]
- World Health Organization. Preconception Care Regional Expert Group Consultation; World Health Organization: New Delhi, India, 2013. [Google Scholar]
- Shawe, J.; Delbaere, I.; Ekstrand, M.; Hegaard, H.K.; Larsson, M.; Mastroiacovo, P.; Stern, J.; Steegers, E.; Stephenson, J.; Tydén, T. Preconception care policy, guidelines, recommendations and services across six European countries: Belgium (Flanders), Denmark, Italy, the Netherlands, Sweden and the United Kingdom. Eur. J. Contracept. Reprod. Health Care 2015, 20, 77–87. [Google Scholar] [CrossRef]
- Dayan, F.; Javadifar, N.; Tadayon, M.; Malehi, A.S.; Sani, H.K. The Relationship between Gestational Weight Gain and Postpartum Depression in Normal and Overweight Pregnant Women. J. Pregnancy 2018, 2018, 9315320. [Google Scholar] [CrossRef]
- Witt, W.P.; Wisk, L.E.; Cheng, E.R.; Hampton, J.M.; Creswell, P.D.; Hagen, E.W.; Spear, H.A.; Maddox, T.; DeLeire, T. Poor prepregnancy and antepartum mental health predicts postpartum mental health problems among US women: A nationally representative population-based study. Womens Health Issues 2011, 21, 304–313. [Google Scholar] [CrossRef]
- Witt, W.P.; Wisk, L.E.; Cheng, E.R.; Hampton, J.M.; Hagen, E.W. Preconception mental health predicts pregnancy complications and adverse birth outcomes: A national population-based study. Matern. Child Health J. 2012, 16, 1525–1541. [Google Scholar] [CrossRef]
- Olsson, C.A.; Spry, E.A.; Alway, Y.; Moreno-Betancur, M.; Youssef, G.; Greenwood, C.; Letcher, P.; Macdonald, J.A.; McIntosh, J.; Hutchinson, D.; et al. Preconception depression and anxiety symptoms and maternal-infant bonding: A 20-year intergenerational cohort study. Arch. Women’s Ment. Health 2021, 24, 513–523. [Google Scholar] [CrossRef]
- Fusar-Poli, P.; de Pablo, G.S.; De Micheli, A.; Nieman, D.H.; Correll, C.U.; Kessing, L.V.; Pfennig, A.; Bechdolf, A.; Borgwardt, S.; Arango, C.; et al. What is good mental health? A scoping review. Eur. Neuropsychopharmacol. 2020, 31, 33–46. [Google Scholar] [CrossRef] [PubMed]
- Aydin, B.; Yalçin, S.S. Changes in maternal anthropometric measurements in the first postpartum month and associated factors. Am. J. Hum. Biol. 2022, 34, e23580. [Google Scholar] [CrossRef] [PubMed]
- Deputy, N.P.; Sharma, A.J.; Kim, S.Y.; Hinkle, S. Prevalence and characteristics associated with gestational weight gain adequacy. Obstet. Gynecol. 2015, 125, 773–781. [Google Scholar] [CrossRef] [PubMed]
- Han, E.; Abrams, B.; Sridhar, S.; Xu, F.; Hedderson, M. Validity of Self-Reported Pre-Pregnancy Weight and Body Mass Index Classification in an Integrated Health Care Delivery System. Paediatr. Perinat. Epidemiol. 2016, 30, 314–319. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.M.; Oken, E.; Rifas-Shiman, S.L.; Téllez-Rojo, M.; Just, A.; Svensson, K.; Deierlein, A.L.; Chandler-Laney, P.C.; Miller, R.C.; McNamara, C.; et al. Do Women Know Their Prepregnancy Weight? Obesity 2019, 27, 1161–1167. [Google Scholar] [CrossRef]

| Depression | Anxiety | SOC | QoL | |||
|---|---|---|---|---|---|---|
| EPDS | GMDS | sSTAI-6 | EDS-3A | SOC-13 | QoL | |
| Items | 10 | 13 | 6 | 3 | 13 | 1 |
| Scale | 4-point Likert Scale | 4-point Likert Scale | 4-point Likert Scale | 4-point Likert Scale | 7-point Likert Scale | Linear Analogue Scale |
| Range numeric score | 0–30 ᵃ | 0–39 a | 20–80 a | 0–9 a | 13–91 b | 0–100 a |
| Cut-off score | ≥10 | <13 13–26 ≥27 | ≥40 | ≥5 | <70 | Median c |
| Model 1: BMI change between 2 pregnancies * | |||
| Explanatory variables | ß | SE | p-value |
| Intercept | 2.607 | 0.530 | <0.0001 |
| Level of education | −0.498 | 0.246 | 0.04 |
| Sense of coherence at that start of next pregnancy | −0.527 | 0.211 | 0.01 |
| Model 2: Pre-pregnancy BMI next pregnancy * | |||
| Explanatory variables | ß | SE | p-value |
| Intercept | 3.628 | 0.938 | 0.0001 |
| Pre-pregnancy BMI previous pregnancy | 0.965 | 0.027 | <0.0001 |
| Level of education | −0.530 | 0.248 | 0.03 |
| Sense of coherence at the start of next pregnancy | −0.577 | 0.214 | 0.008 |
| Model 3: Visceral fat at the start of the next pregnancy * | |||
| Explanatory variables | ß | SE | p-value |
| Intercept | −8.100 | 0.572 | <0.0001 |
| Pre-pregnancy BMI previous pregnancy | 0.465 | 0.019 | <0.0001 |
| Exclusive breastfeeding at 6 months after childbirth | 0.401 | 0.176 | 0.02 |
| Model 4: Waist circumference at the start of the next pregnancy * | |||
| Explanatory variables | ß | SE | p-value |
| Intercept | 33.799 | 3.033 | <0.0001 |
| Pre-pregnancy BMI previous pregnancy | 1.878 | 0.092 | <0.0001 |
| Exclusive breastfeeding at 6 months after childbirth | 1.830 | 0.835 | 0.03 |
| Interpregnancy interval (months) | −2.173 | 0.722 | 0.003 |
| Model 5: Fat percentage at the start of the next pregnancy * | |||
| Explanatory variables | ß | SE | p-value |
| Intercept | 2.039 | 2.254 | 0.367 |
| Pre-pregnancy BMI previous pregnancy | 1.130 | 0.066 | <0.0001 |
| Exclusive breastfeeding at 6 months after childbirth | 1.952 | 0.609 | 0.002 |
| Sense of coherence at the start of next pregnancy | −1.200 | 0.528 | 0.02 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van Uytsel, H.; Ameye, L.; Devlieger, R.; Jacquemyn, Y.; Van Holsbeke, C.; Schreurs, A.; Bogaerts, A. Mental Health during the Interpregnancy Period and the Association with Pre-Pregnancy Body Mass Index and Body Composition: Data from the INTER-ACT Randomized Controlled Trial. Nutrients 2023, 15, 3152. https://doi.org/10.3390/nu15143152
Van Uytsel H, Ameye L, Devlieger R, Jacquemyn Y, Van Holsbeke C, Schreurs A, Bogaerts A. Mental Health during the Interpregnancy Period and the Association with Pre-Pregnancy Body Mass Index and Body Composition: Data from the INTER-ACT Randomized Controlled Trial. Nutrients. 2023; 15(14):3152. https://doi.org/10.3390/nu15143152
Chicago/Turabian StyleVan Uytsel, Hanne, Lieveke Ameye, Roland Devlieger, Yves Jacquemyn, Caroline Van Holsbeke, Annick Schreurs, and Annick Bogaerts. 2023. "Mental Health during the Interpregnancy Period and the Association with Pre-Pregnancy Body Mass Index and Body Composition: Data from the INTER-ACT Randomized Controlled Trial" Nutrients 15, no. 14: 3152. https://doi.org/10.3390/nu15143152
APA StyleVan Uytsel, H., Ameye, L., Devlieger, R., Jacquemyn, Y., Van Holsbeke, C., Schreurs, A., & Bogaerts, A. (2023). Mental Health during the Interpregnancy Period and the Association with Pre-Pregnancy Body Mass Index and Body Composition: Data from the INTER-ACT Randomized Controlled Trial. Nutrients, 15(14), 3152. https://doi.org/10.3390/nu15143152







