Tackling (Childhood) Obesity through a Voluntary Food Reformulation Policy: A Repeated Cross-Sectional Study Investigating Nutritional Changes in the Out-of-Home Sector
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Setting
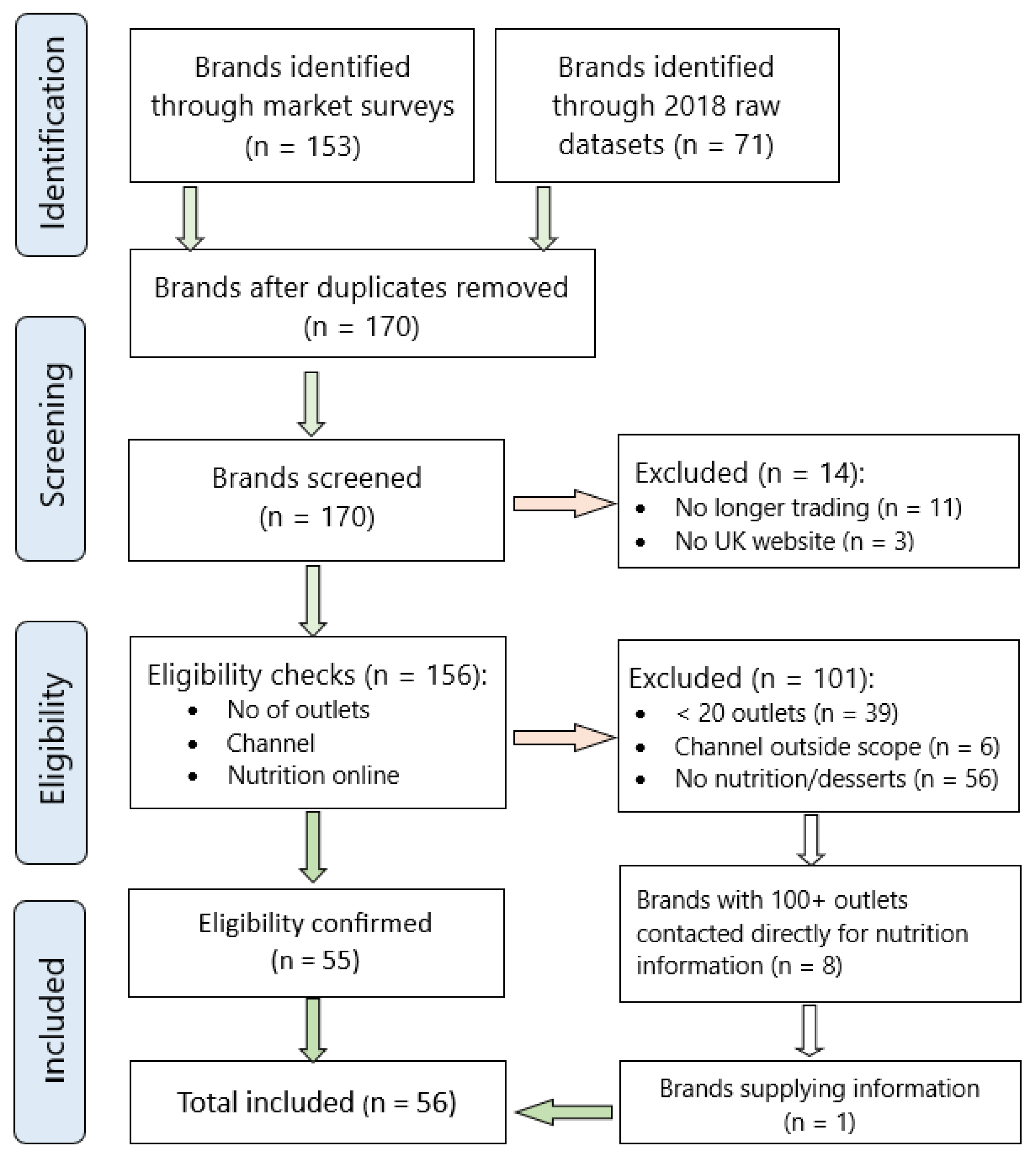
2.1.1. Restaurant Inclusion Criteria
2.1.2. Product Inclusion Criteria
2.2. Data Collection and Extraction
2.3. Data Cleaning and Statistics
2.3.1. Primary Outcome: Progress towards PHE Targets (2017–2020)
2.3.2. Sub-Group Analyses (Secondary Outcomes)
3. Results
3.1. Sample Composition
3.2. Primary Outcome—Progress towards PHE Targets
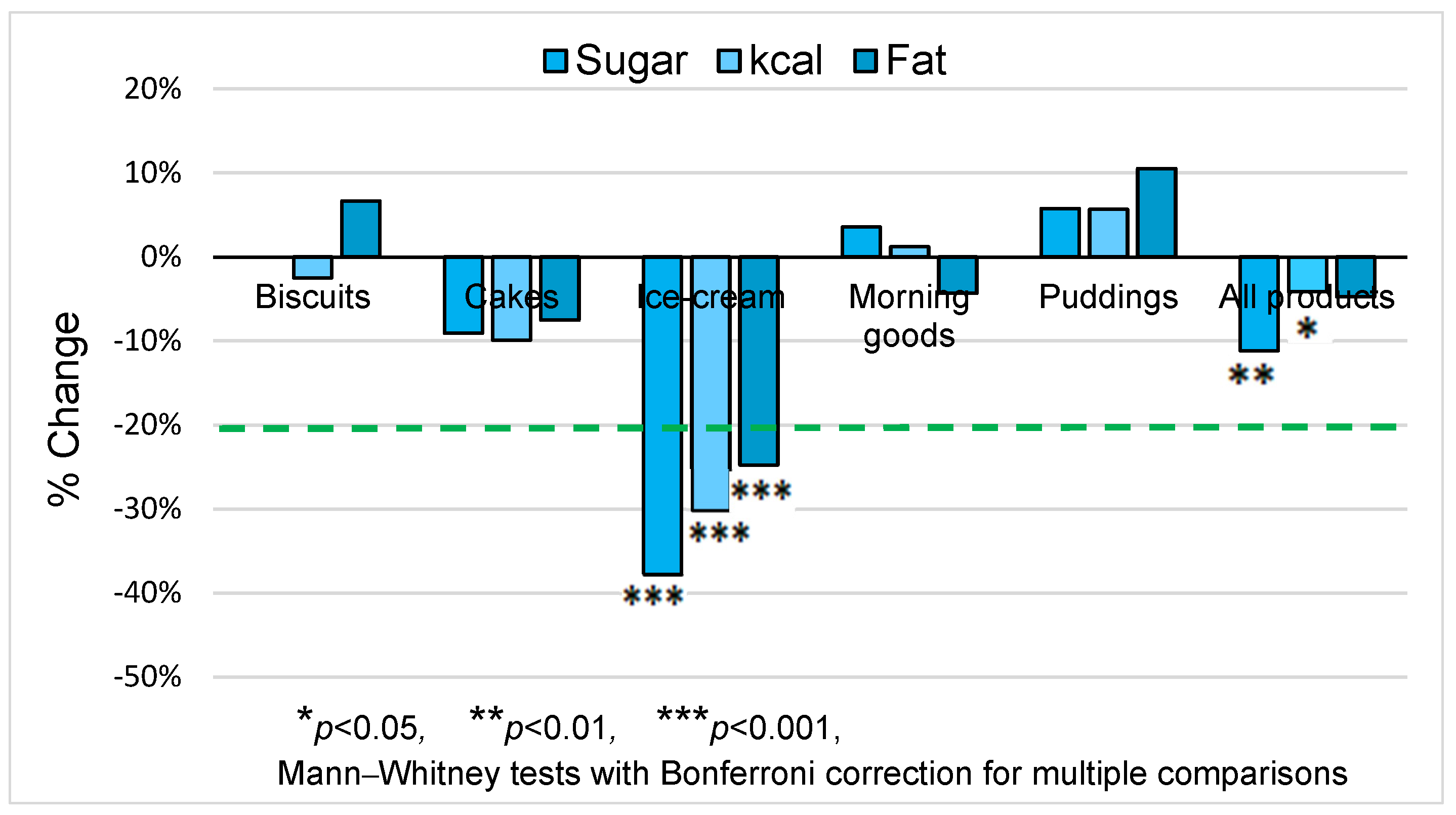
3.2.1. Sugar Reduction: Percentage Change from Baseline
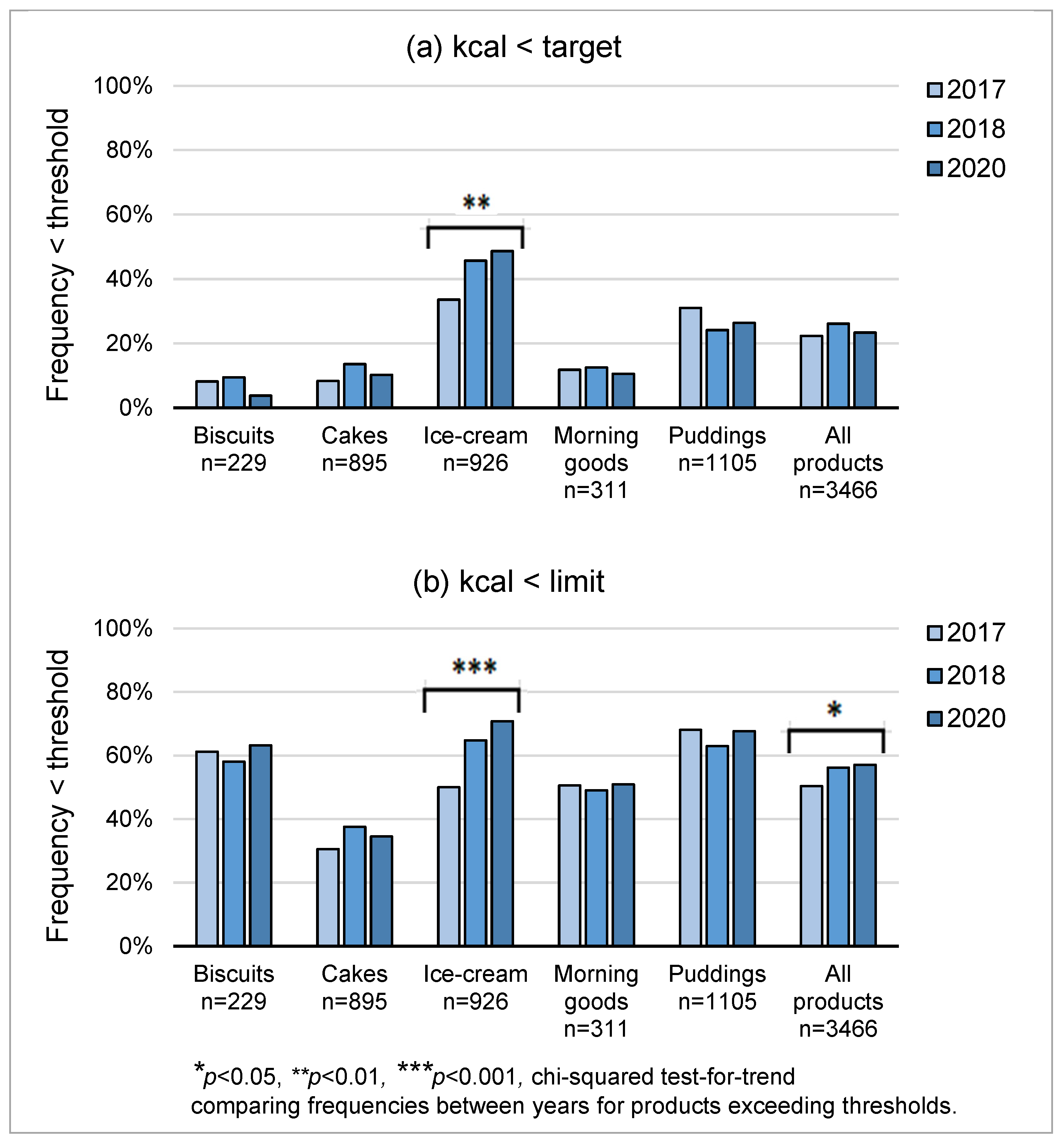
3.2.2. Energy Reduction: Proportions Meeting Category Thresholds
3.3. Secondary Outcomes
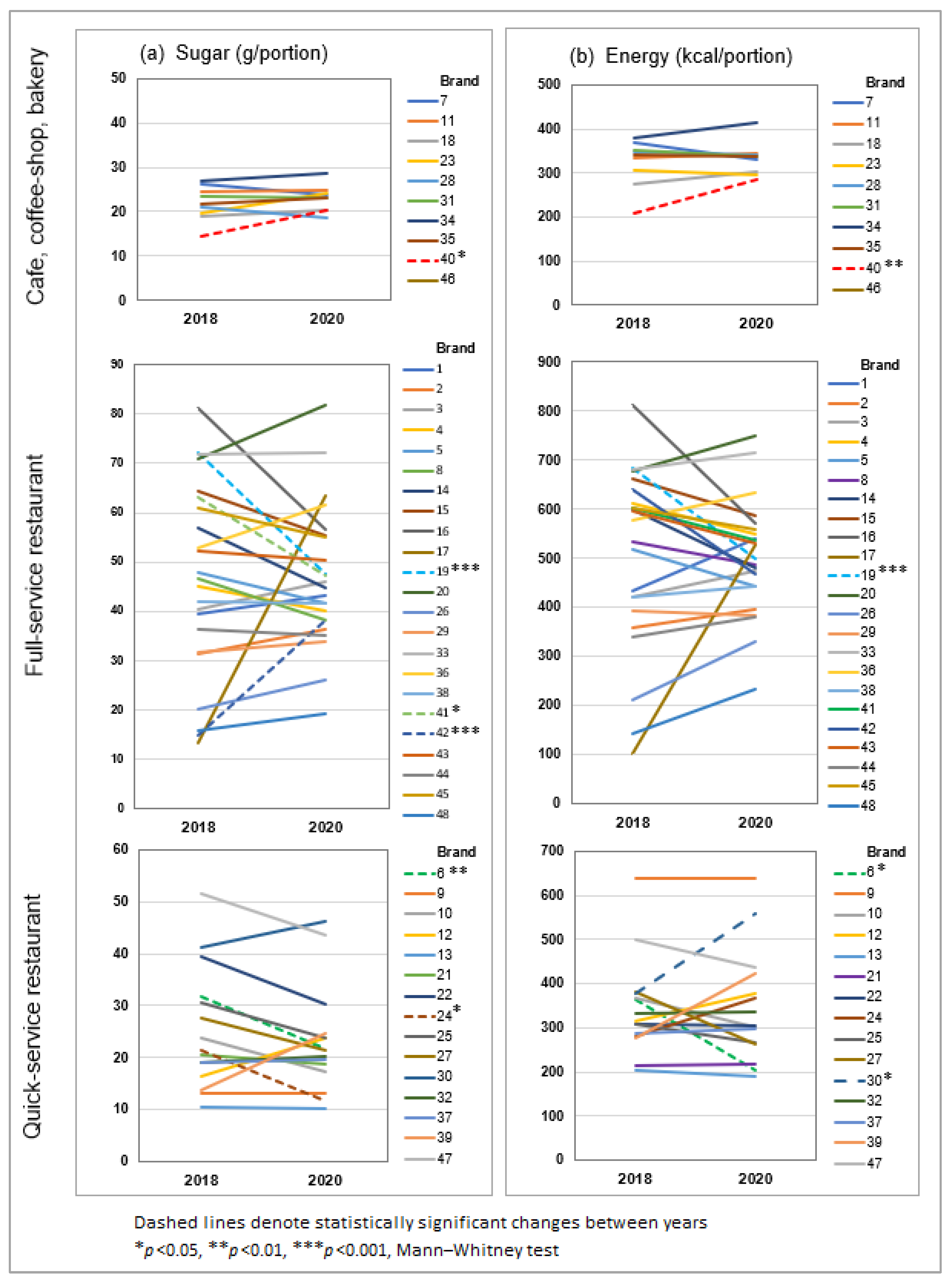
3.3.1. Business Compliance
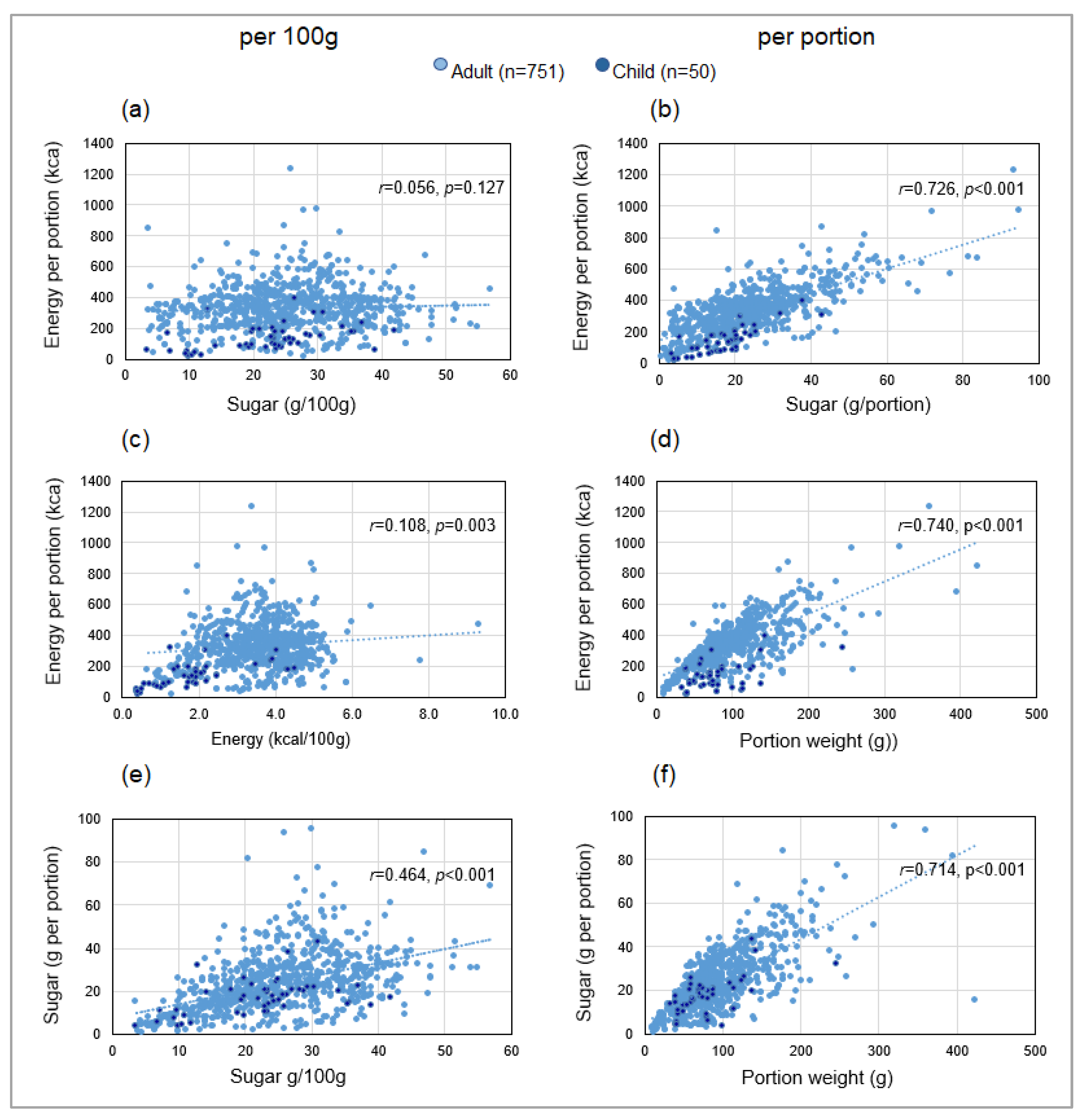
3.3.2. Impact of Nutrients and Portion Weight on Sugar and Energy per Portion
3.3.3. Nutritional Profile in 2020—Comparison of Adults’ and Children’s Products
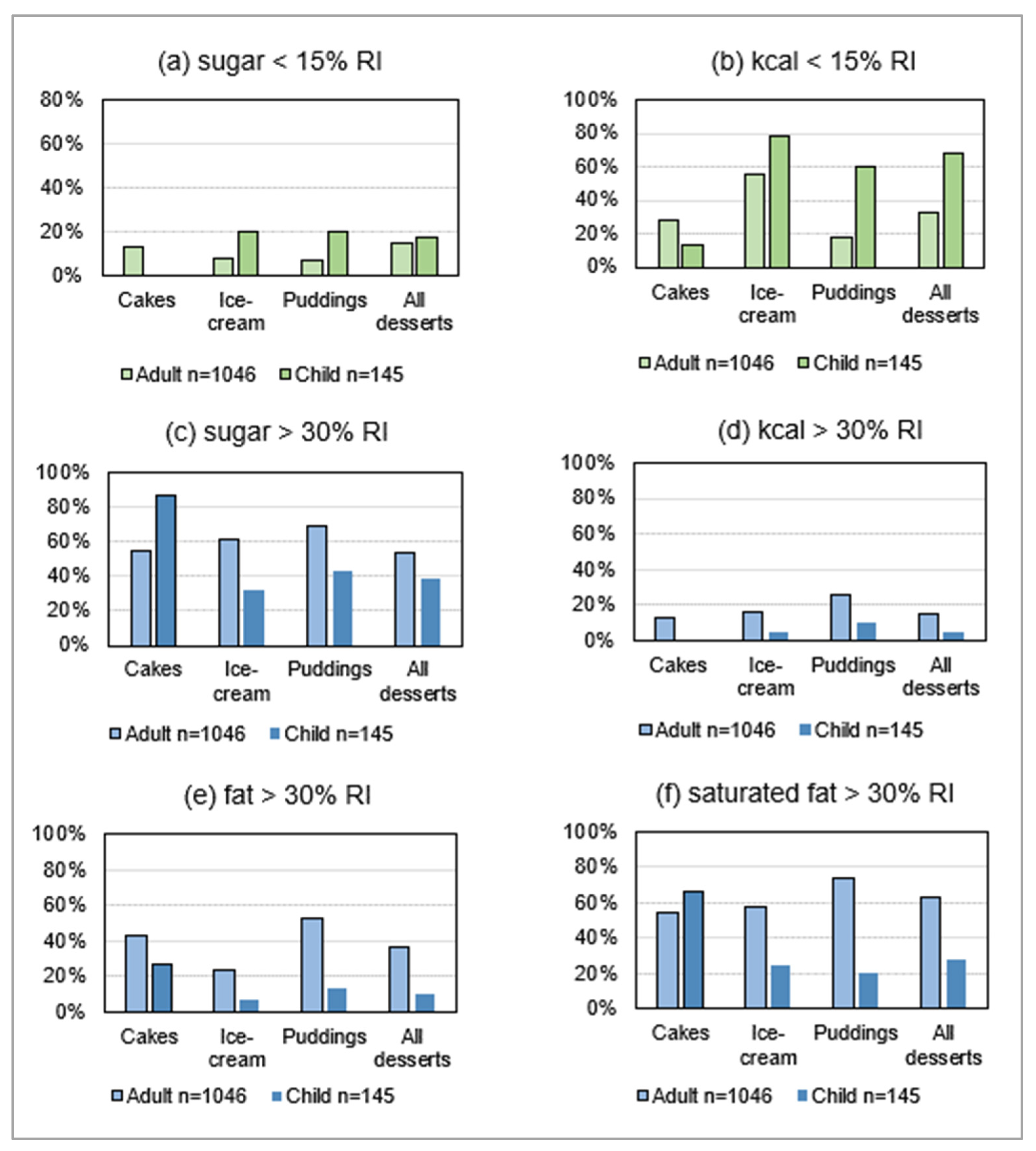
3.3.4. Compliance with Dietary Guidelines
4. Discussion
4.1. Summary and Interpretation of Principle Findings
4.1.1. Sugar and Energy Reduction
4.1.2. Business Compliance
4.1.3. Validation of Primary Outcome: Correlation between Sugar and Energy
4.1.4. Nutritional Profile in 2020 by Menu
4.2. Strengths and Limitations
4.3. Implications for Policy
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- NHS Digital. Health Survey for England 2019; 2020. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/2019 (accessed on 30 July 2021).
- World Health Organization. Obesity and Overweight Fact-Sheet. Available online: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 1 September 2022).
- Abarca-Gómez, L.; Abdeen, Z.A.; Hamid, Z.A.; Abu-Rmeileh, N.M.; Acosta-Cazares, B.; Acuin, C.; Adams, R.J.; Aekplakorn, W.; Afsana, K.; Aguilar-Salinas, C.A. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [PubMed]
- Rankin, J.; Matthews, L.; Cobley, S.; Han, A.; Sanders, R.; Wiltshire, H.D.; Baker, J.S. Psychological consequences of childhood obesity: Psychiatric comorbidity and prevention. Adolesc. Health Med. Ther. 2016, 7, 125. [Google Scholar] [CrossRef] [PubMed]
- Morales Camacho, W.J.; Molina Díaz, J.M.; Plata Ortiz, S.; Plata Ortiz, J.E.; Morales Camacho, M.A.; Calderón, B.P. Childhood obesity: Aetiology, comorbidities, and treatment. Diabetes Metab. Res. 2019, 35, e3203. [Google Scholar] [CrossRef] [PubMed]
- Candler, T.P.; Mahmoud, O.; Lynn, R.M.; Majbar, A.A.; Barrett, T.G.; Shield, J. Continuing rise of type 2 diabetes incidence in children and young people in the UK. Diabet. Med. 2018, 35, 737–744. [Google Scholar] [CrossRef]
- Caprio, S.; Santoro, N.; Weiss, R. Childhood obesity and the associated rise in cardiometabolic complications. Nat. Metab. 2020, 2, 223–232. [Google Scholar] [CrossRef]
- Geserick, M.; Vogel, M.; Gausche, R.; Lipek, T.; Spielau, U.; Keller, E.; Pfäffle, R.; Kiess, W.; Körner, A. Acceleration of BMI in early childhood and risk of sustained obesity. N. Engl. J. Med. 2018, 379, 1303–1312. [Google Scholar] [CrossRef]
- Stock, K.; Nagrani, R.; Gande, N.; Bernar, B.; Staudt, A.; Willeit, P.; Geiger, R.; Knoflach, M.; Kiechl-Kohlendorfer, U.; Winder, B.; et al. Birth Weight and Weight Changes from Infancy to Early Childhood as Predictors of Body Mass Index in Adolescence. J. Pediatr. 2020, 222, 120–126.e3. [Google Scholar] [CrossRef]
- Ryder, J.R.; Jacobs, D.R.; Sinaiko, A.R.; Kornblum, A.P.; Steinberger, J. Longitudinal Changes in Weight Status from Childhood and Adolescence to Adulthood. J. Pediatr. 2019, 214, 187–192.e2. [Google Scholar] [CrossRef]
- Reilly, J.J.; Kelly, J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. Int. J. Obes. 2011, 35, 891–898. [Google Scholar] [CrossRef]
- World Health Organization. Report of the Commission on Ending Childhood Obesity. Available online: https://www.who.int/end-childhood-obesity/final-report/en/ (accessed on 20 July 2019).
- World Obesity Federation. Our Policy Priorities. Available online: https://www.worldobesity.org/what-we-do/our-policy-priorities (accessed on 26 September 2022).
- Davies, S.C. Time to Solve Childhood Obesity: An Independent Report by the Chief Medical Officer, 2019; Department of Health and Social Care, 2019.
- Jebb, S.A.; Aveyard, P.N.; Hawkes, C. The evolution of policy and actions to tackle obesity in England. Obes. Rev. 2013, 14, 42–59. [Google Scholar] [CrossRef]
- Adams, J.; Mytton, O.; White, M.; Monsivais, P. Why are some population interventions for diet and obesity more equitable and effective than others? The role of individual agency. PLoS Med. 2016, 13, e1001990. [Google Scholar]
- Dahlgren, G.; Whitehed, M. European Strategies for Tackling Social Inequities in Health. 2006. Available online: https://www.euro.who.int/__data/assets/pdf_file/0018/103824/E89384.pdf (accessed on 30 July 2021).
- Nobles, J.; Summerbell, C.; Brown, T.; Jago, R.; Moore, T. A secondary analysis of the childhood obesity prevention Cochrane Review through a wider determinants of health lens: Implications for research funders, researchers, policymakers and practitioners. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 22. [Google Scholar] [CrossRef]
- Theis, D.; White, M. Is Obesity Policy in England Fit for Purpose? Analysis of Government Strategies and Policies, 1992–2020. Milbank Q. 2021, 99, 126–170. [Google Scholar] [CrossRef] [PubMed]
- Rutter, H.; Bes-Rastrollo, M.; De Henauw, S.; Lahti-Koski, M.; Lehtinen-Jacks, S.; Mullerova, D.; Rasmussen, F.; Rissanen, A.; Visscher, T.L.; Lissner, L. Balancing upstream and downstream measures to tackle the obesity epidemic: A position statement from the european association for the study of obesity. Obes. Facts 2017, 10, 61–63. [Google Scholar] [CrossRef]
- Butland, B.; Jebb, S.; Kopelman, P.; McPherson, K.; Thomas, S.; Mardell, J.; Parry, V. Foresight. Tackling obesities: Future choices. Project report. Obes. Rev. 2007, 8, VI–IX. [Google Scholar]
- Lobstein, T.; Brinsden, T.; Neveux, M. World Obesity Atlas 2022. Available online: https://www.worldobesityday.org/assets/downloads/World_Obesity_Atlas_2022_WEB.pdf (accessed on 24 August 2022).
- Di Cesare, M.; Sorić, M.; Bovet, P.; Miranda, J.J.; Bhutta, Z.; Stevens, G.A.; Laxmaiah, A.; Kengne, A.; Bentham, J. The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action. BMC Med. 2019, 17, 212. [Google Scholar] [CrossRef]
- Ritchie, H.; Roser, M. Obesity. 2017. Available online: https://ourworldindata.org/obesity (accessed on 3 September 2022).
- Harris, J.L.; Pomeranz, J.L.; Lobstein, T.; Brownell, K.D. A crisis in the marketplace: How food marketing contributes to childhood obesity and what can be done. Annu. Rev. Public Health 2009, 30, 211–225. [Google Scholar] [CrossRef]
- Russell, S.J.; Croker, H.; Viner, R.M. The effect of screen advertising on children’s dietary intake: A systematic review and meta-analysis. Obes. Rev. 2019, 20, 554–568. [Google Scholar] [CrossRef]
- Benson, C. Increasing portion size in Britain. Soc. Biol. Hum. Aff. 2009, 74, 4–20. [Google Scholar]
- Are We Suffering from Portions Distortion? Available online: https://www.which.co.uk/news/2020/09/are-we-suffering-from-portion-distortion/ (accessed on 9 September 2020).
- Burgoine, T.; Sarkar, C.; Webster, C.J.; Monsivais, P. Examining the interaction of fast-food outlet exposure and income on diet and obesity: Evidence from 51,361 UK Biobank participants. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 71. [Google Scholar] [CrossRef]
- Cetateanu, A.; Jones, A. Understanding the relationship between food environments, deprivation and childhood overweight and obesity: Evidence from a cross sectional England-wide study. Health Place 2014, 27, 68–76. [Google Scholar] [CrossRef]
- United Nations Children’s Fund (UNICEF). Prevention of Overweight and Obesity in Children and Adolescents: UNICEF Programming Guidance. 2019. Available online: https://www.unicef.org/media/92336/file/Programming-Guidance-Overweight-Prevention.pdf (accessed on 27 September 2022).
- Gressier, M.; Sassi, F.; Frost, G. Healthy foods and healthy diets. How government policies can steer food reformulation. Nutrients 2020, 12, 1992. [Google Scholar] [CrossRef] [PubMed]
- Te Morenga, L.; Mallard, S.; Mann, J. Dietary sugars and body weight: Systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ 2013, 346, e7492. [Google Scholar] [CrossRef] [PubMed]
- EFSA Panel on Nutrition, Novel Foods and Food Allergens (NDA); Turck, D.; Bohn, T.; Castenmiller, J.; de Henauw, S.; Hirsch-Ernst, K.I.; Knutsen, H.K.; Maciuk, A.; Mangelsdorf, I.; McArdle, H.J. Tolerable upper intake level for dietary sugars. EFSA J. 2022, 20, e07074. [Google Scholar] [PubMed]
- Malik, V.S.; Hu, F.B. The role of sugar-sweetened beverages in the global epidemics of obesity and chronic diseases. Nat. Rev. Endocrinol. 2022, 18, 205–218. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guideline: Sugars Intake for Adults and Children; 2015. Available online: https://www.who.int/publications/i/item/9789241549028 (accessed on 7 November 2022).
- Scientific Advisory Committee on Nutrition (SACN). Carbohydrates and Health; 2015. Available online: https://www.gov.uk/government/publications/sacn-carbohydrates-and-health-report. (accessed on 5 September 2018).
- House of Commons Health Committee. Childhood Obesity—Brave and Bold Action. 2015. Available online: https://publications.parliament.uk/pa/cm201516/cmselect/cmhealth/465/465.pdf (accessed on 25 September 2020).
- HM Government. Childhood Obesity: A Plan for Action; 2016. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/546588/Childhood_obesity_2016__2__acc.pdf (accessed on 25 September 2020).
- Tedstone, A.; Targett, V.; Allen, R. Sugar Reduction: The Evidence for Action; 2015. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/470179/Sugar_reduction_The_evidence_for_action.pdf (accessed on 24 September 2021).
- Tedstone, A. The World’s First Sugar Reduction Programme: Data Challenges; 2018. Available online: https://ukhsa.blog.gov.uk/2018/05/22/the-worlds-first-sugar-reduction-programme-data-challenges/ (accessed on 19 August 2021).
- WHO Regional Office for Europe. Improving Dietary Intake and Achieving Food Product Improvement Policy Opportunities and Challenges for the WHO European Region in Reducing Salt and Sugar in the Diet. 2020. Available online: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/publications/2020/improving-dietary-intake-and-achieving-food-product-improvement-2020 (accessed on 3 January 2022).
- Tedstone, A.; Targett, V.; Owtram, G.; Pyne, V.; Allen, R.; Bathrellou, K.; MacKinlay, B.; Kathryn, E.; Morgan, K.; Swan, G.; et al. Sugar Reduction: Achieving the 20%; 2017. Available online: https://www.gov.uk/government/publications/sugar-reduction-achieving-the-20 (accessed on 27 January 2018).
- Caraher, M.; Perry, I. Sugar, salt, and the limits of self regulation in the food industry. BMJ 2017, 357, j1709. [Google Scholar] [CrossRef] [PubMed]
- Knai, C.; Petticrew, M.; Mays, N. The childhood obesity strategy. BMJ 2016, 354, i4613. [Google Scholar] [CrossRef]
- Buttriss, J.L. Sugars—Part of a bigger picture? Nutr. Bull. 2016, 41, 78–86. [Google Scholar] [CrossRef]
- Griffith, R.; Jenneson, V.; James, J.; Taylor, A. The Impact of a Tax on Added Sugar and Salt; IFS Working Paper No. W21/21; Institute for Fiscal Studies (IFS): London, UK, 2021. [Google Scholar]
- Department of Health and Social Care. Press Release. UK to Spearhead Europe-Wide Initiative to Reduce Sugar and Calorie Intake in Food; 2021. Available online: https://www.gov.uk/government/news/uk-to-spearhead-europe-wide-initiative-to-reduce-sugar-and-calorie-intake-in-food.2021. (accessed on 17 November 2021).
- Office for Health Improvement & Disparities. Sugar Reduction Programme: Industry Progress 2015 to 2020; 2022. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1120731/Sugar-reduction-and-reformulation-progress-report-2015-to-2020.pdf (accessed on 1 December 2022).
- Huang, Y.; Theis, D.R.; Burgoine, T.; Adams, J. Trends in energy and nutrient content of menu items served by large UK chain restaurants from 2018 to 2020: An observational study. BMJ Open 2021, 11, e054804. [Google Scholar] [CrossRef]
- UK Statutory Instruments No. 41. The Soft Drinks Industry Levy Regulations 2018. 2018. Available online: https://www.legislation.gov.uk/uksi/2018/41/contents/made (accessed on 8 September 2021).
- Bakery Cafes in the UK. Available online: https://www.ibisworld.com/united-kingdom/market-research-reports/bakery-cafes-industry/ (accessed on 23 October 2020).
- Takeaway & Fast-Food Restaurants in the UK. Available online: https://www.ibisworld.com/united-kingdom/market-research-reports/takeaway-fast-food-restaurants-industry/ (accessed on 11 December 2020).
- Cafes & Coffee Shops in the UK. Available online: https://www.ibisworld.com/united-kingdom/market-research-reports/cafes-coffee-shops-industry/ (accessed on 23 October 2020).
- Full-Service Restaurants in the UK. Available online: https://www.ibisworld.com/united-kingdom/market-research-reports/full-service-restaurants-industry/ (accessed on 23 October 2020).
- Juice & Smoothie Bars in the UK—Market Research Report. Available online: https://www.ibisworld.com/united-kingdom/market-research-reports/juice-smoothie-bars-industry/ (accessed on 17 August 2021).
- Catering Services in the UK—Market Research Report. Available online: https://www.ibisworld.com/united-kingdom/market-research-reports/catering-services-industry/ (accessed on 17 August 2021).
- Food Markets in the UK—Market Research Report. Available online: https://www.ibisworld.com/united-kingdom/market-research-reports/food-markets-idustry/ (accessed on 17 August 2021).
- Online Food Ordering & Delivery Platforms in the UK. Available online: https://www.ibisworld.com/united-kingdom/market-research-reports/online-food-ordering-delivery-platforms-industry/ (accessed on 23 October 2020).
- Bakery Product Retailing in the UK. Available online: https://www.ibisworld.com/united-kingdom/market-research-reports/bakery-product-retailing-industry/ (accessed on 19 November 2020).
- Government of Ontario. Healthy Menu Choices Act, 2015. S.O. 2015, c. 7, Sched. 1 2016. Available online: https://www.ontario.ca/laws/statute/15h07 (accessed on 10 July 2023).
- Food and Drug Administration, HHS. Food labeling; nutrition labeling of standard menu items in restaurants and similar retail food establishments. Final rule. Fed. Regist. 2014, 79, 71155–71259. [Google Scholar]
- Top 100 UK Operator Profiles. Available online: https://www.mca-insight.com/market-intelligence/operator-data-index/top-100-profiles (accessed on 8 October 2020).
- The Most Popular Dining Brands in the UK. Available online: https://yougov.co.uk/ratings/food/popularity/dining-brands/all (accessed on 8 October 2020).
- Most Popular Dining Brands in the UK as of June 2019. Available online: https://www.statista.com/statistics/950444/most-popular-restaurant-brands-in-the-united-kingdom-uk/ (accessed on 8 October 2020).
- Leading 25 Retailers of Baked Products in the United Kingdom (UK) in 2016, Ranked by Number of Outlets. Available online: https://www.statista.com/statistics/297842/leading-retailers-of-baked-products-in-the-united-kingdom-uk/ (accessed on 28 August 2020).
- Leading Coffee Shop Chains Ranked by Number of Outlets in the United Kingdom (UK) as of December 2016. Available online: https://www.statista.com/statistics/297863/leading-coffeehttps://www.statista.com/statistics/297863/leading-coffee-shop-chains-in-the-united-kingdom-uk-store-number/#:~:text=Costa%20ranked%20highest%20with%202%2C121,in%20the%20last%208%20years-s (accessed on 28 August 2020).
- Leading Casual Dining Brands in the United Kingdom (UK) as of December 2016 and December 2017, by Number of Units. Available online: https://www.statista.com/statistics/629796/casual-dining-brands-by-number-of-units-united-kingdom-uk/ (accessed on 28 August 2020).
- Leading Restaurant Chains Ranked by Number of Users in Great Britain from 2018. Available online: https://www.statista.com/statistics/586234/restaurant-chains-usage-in-the-uk-by-number-of-users/ (accessed on 8 August 2020).
- Tedstone, A. Sugar Reduction Timeline; 2017. Available online: https://publichealthmatters.blog.gov.uk/wp-content/uploads/sites/33/2017/03/Sugar-red-timeline-FINAL-30-3-1.png (accessed on 17 June 2021).
- Coyle, N. Dataset OOH_2017; Public Health England: London, UK, 2020.
- Coyle, N. Dataset OOH_2018; Public Health England: London, UK, 2020.
- Tedstone, A.; Coulton, V.; Targett, V.; Bennett, A.; Sweeney, K.; Morgan, K.; Morgan, K.; Clegg, E.; Robinson, M.; Dowd, L.; et al. Sugar Reduction and Wider Reformulation Programme: Progress towards the First 5% Reduction and Next Steps; 2018. Available online: https://www.gov.uk/government/publications/sugar-reduction-report-on-first-year-progress (accessed on 6 May 2019).
- Niblett, P.; Coyle, N.; Little, E.; Beaton, C.; Burton, J.; Chisholm, S.; Tedstone, A.; Targett, V.; Nicholas, J.; Montel, S.; et al. Sugar Reduction: Report on Progress between 2015 and 2018; 2019. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/839756/Sugar_reduction_yr2_progress_report.pdf (accessed on 30 October 2019).
- Coyle, N.; Little, E.; Williamson, S.; Dodhia, S.; Targett, V.; Montel, S.; Niblett, P.; Mildon, A.; Hutchinson, K.; Owtram, G.; et al. Sugar Reduction: Report on Progress between 2015 and 2019; 2020. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/925027/SugarReportY3.pdf (accessed on 7 October 2020).
- Theis, D.R.; Adams, J. Differences in energy and nutritional content of menu items served by popular UK chain restaurants with versus without voluntary menu labelling: A cross-sectional study. PLoS ONE 2019, 14, e0222773. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows; Version 28.0; IBM Corp: Armonk, NY, USA, 2021. [Google Scholar]
- Ghasemi, A.; Zahediasl, S. Normality tests for statistical analysis: A guide for non-statisticians. Int. J. Endocrinol. Metab. 2012, 10, 486. [Google Scholar] [CrossRef] [PubMed]
- Fritz, C.O.; Morris, P.E.; Richler, J.J. Effect Size Estimates: Current Use, Calculations, and Interpretation. J. Exp. Psychol. Gen. 2012, 141, 2–18. [Google Scholar] [CrossRef] [PubMed]
- Regulation (EU) No 1169/2011 of the European Parliament and of the Council of 25 October 2011 on the provision of food information to consumers. Off. J. Eur. Union. 2011, L304, 18–63.
- Public Health England. Encouraging Healthier ‘Out of Home’ Food Provision; 2017. Available online: https://www.gov.uk/government/publications/encouraging-healthier-out-of-home-food-provision (accessed on 19 August 2021).
- Scientific Advisory Committee on Nutrition (SACN). Dietary Reference Values for Energy. Available online: https://www.gov.uk/government/publications/sacn-dietary-reference-values-for-energy (accessed on 7 November 2017).
- Scientific Advisory Committee on Nutrition. Saturated Fats and Health; 2019. Available online: https://www.gov.uk/government/publications/saturated-fats-and-health-sacn-report (accessed on 16 October 2019).
- NHS Digital. National Child Measurement Programme, England 2020/21 School Year. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/national-child-measurement-programme/2020-21-school-year (accessed on 17 November 2021).
- Biguzzi, C.; Schlich, P.; Lange, C. The impact of sugar and fat reduction on perception and liking of biscuits. Food Qual. Prefer. 2014, 35, 41–47. [Google Scholar] [CrossRef]
- Milner, L.; Kerry, J.P.; O’Sullivan, M.G.; Gallagher, E. Physical, textural and sensory characteristics of reduced sucrose cakes, incorporated with clean-label sugar-replacing alternative ingredients. Innov. Food Sci. Emerg. Technol. 2020, 59, 102235. [Google Scholar] [CrossRef]
- Van der Sman, R.; Renzetti, S. Understanding functionality of sucrose in cake for reformulation purposes. Crit. Rev. Food Sci. Nutr. 2020, 61, 2756–2772. [Google Scholar] [CrossRef]
- UK Statutory Instruments No. 3348. The Sweeteners in Food (Amendment) (England) Regulations 2004. 2004. Available online: https://www.legislation.gov.uk/uksi/2004/3348/made (accessed on 10 July 2023).
- Cooper, J. Food and drink reformulation to reduce fat, sugar and salt. Food Sci. Technol. 2017, 31, 38–41. [Google Scholar] [CrossRef]
- Bandy, L.K.; Scarborough, P.; Harrington, R.A.; Rayner, M.; Jebb, S.A. The sugar content of foods in the UK by category and company: A repeated cross-sectional study, 2015–2018. PLoS Med. 2021, 18, e1003647. [Google Scholar] [CrossRef]
- Glanz, K.; Resnicow, K.; Seymour, J.; Hoy, K.; Stewart, H.; Lyons, M.; Goldberg, J. How Major Restaurant Chains Plan Their Menus: The Role of Profit, Demand, and Health. Am. J. Prev. Med. 2007, 32, 383–388. [Google Scholar] [CrossRef]
- World Health Organization. Incentives and Disincentives for Reducing Sugar in Manufactured Foods: An Exploratory Supply Chain Analysis: A Set of Insights for Member States in the Context of the WHO European Food and Nutrition Action Plan 2015–2020; 2017. Available online: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/publications/2017/incentives-and-disincentives-for-reducing-sugar-in-manufactured-foods-2017 (accessed on 17 November 2021).
- Fuster, M.; Handley, M.A.; Alam, T.; Fullington, L.A.; Elbel, B.; Ray, K.; Huang, T.T.-K. Facilitating Healthier Eating at Restaurants: A Multidisciplinary Scoping Review Comparing Strategies, Barriers, Motivators, and Outcomes by Restaurant Type and Initiator. Int. J. Environ. Res. Public Health 2021, 18, 1479. [Google Scholar] [CrossRef] [PubMed]
- Hobin, E.; White, C.; Li, Y.; Chiu, M.; O’Brien, M.F.; Hammond, D. Nutritional quality of food items on fast-food ‘kids’ menus’: Comparisons across countries and companies. Public Health Nutr. 2014, 17, 2263–2269. [Google Scholar] [CrossRef]
- Alessandrini, R.; He, F.J.; Hashem, K.M.; Tan, M.; MacGregor, G.A. Reformulation and priorities for reducing energy density; Results from a cross-sectional survey on fat content in pre-packed cakes and biscuits sold in British supermarkets. Nutrients 2019, 11, 1216. [Google Scholar] [CrossRef] [PubMed]
- Reeves, S.; Wake, Y.; Zick, A. Nutrition labeling and portion size information on children’s menus in fast-food and table-service chain restaurants in London, UK. J. Nutr. Educ. Behav. 2011, 43, 543–547. [Google Scholar] [CrossRef] [PubMed]
- Young, M.; Coppinger, T.; Reeves, S. The Nutritional Value of Children’s Menus in Chain Restaurants in the United Kingdom and Ireland. J. Nutr. Educ. Behav. 2019, 51, 817–825. [Google Scholar] [CrossRef]
- Swan, G.E.; Powell, N.A.; Knowles, B.L.; Bush, M.T.; Levy, L.B. A definition of free sugars for the UK. Public Health Nutr. 2018, 21, 1636–1638. [Google Scholar] [CrossRef]
- The Food and You Survey Wave 5. Available online: https://www.food.gov.uk/research/food-and-you/food-and-you-wave-five (accessed on 29 September 2021).
- Avison, Z. Foodservice Insights: Eating-Out Review 2019; Agriculture and Horticulture Development Board: Warwickshire, UK, 2019. [Google Scholar]
- Robinson, E.; Jones, A.; Whitelock, V.; Mead, B.R.; Haynes, A. (Over)eating out at major UK restaurant chains: Observational study of energy content of main meals. BMJ 2018, 363, k4982. [Google Scholar] [CrossRef]
- Muc, M.; Jones, A.; Roberts, C.; Sheen, F.; Haynes, A.; Robinson, E. A bit or a lot on the side? Observational study of the energy content of starters, sides and desserts in major UK restaurant chains. BMJ Open 2019, 9, e029679. [Google Scholar] [CrossRef]
- Berger, N.; Cummins, S.; Smith, R.D.; Cornelsen, L. Recent trends in energy and nutrient content of take-home food and beverage purchases in Great Britain: An analysis of 225 million food and beverage purchases over 6 years. BMJ Nutr. Prev. Health 2019, 2, 63–71. [Google Scholar] [CrossRef]
- Cornelsen, L.; Berger, N.; Smith, R.; Cummins, S. OP41 Nutritional content of household food purchases: Study of trends and socio-economic inequalities in Britain 2012–2017. J. Epidemiol. Community Health 2018, 72 (Suppl. S1), A20–A21. [Google Scholar]
- Defra Statistics. Family Food 2018/19. 2020. Available online: https://www.gov.uk/government/statistics/family-food-201819 (accessed on 27 July 2021).
- Hancock, A.; Evans, J. Consumers Sweet on Desserts as Pandemic Spurs Home Deliveries. Financial Times. 2020. Available online: https://www.ft.com/content/a7ae1c3c-bb68-499b-9664-441902a10fe5 (accessed on 17 September 2021).
- Knai, C.; Petticrew, M.; Douglas, N.; Durand, M.A.; Eastmure, E.; Nolte, E.; Mays, N. The public health responsibility deal: Using a systems-level analysis to understand the lack of impact on alcohol, food, physical activity, and workplace health sub-systems. Int. J. Environ. Res. Public Health 2018, 15, 2895. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Angell, S.Y.; Lang, T.; Rivera, J.A. Role of government policy in nutrition—Barriers to and opportunities for healthier eating. BMJ 2018, 361, k2426. [Google Scholar] [CrossRef] [PubMed]
- Department of Health & Social Care. Mandating Calorie Labelling in the Out-of-Home Sector Government Response to Public Consultation. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/903714/Calorie_Labelling_-_Consultation_Response.pdf (accessed on 26 February 2021).
- Department of Health. Nutrient Profiling Technical Guidance; 2011. Available online: https://www.gov.uk/government/publications/the-nutrient-profiling-model (accessed on 17 March 2023).
- Poon, T.; Labonté, M.; Mulligan, C.; Ahmed, M.; Dickinson, K.M.; L’Abbé, M.R. Comparison of nutrient profiling models for assessing the nutritional quality of foods: A validation study. Br. J. Nutr. 2018, 120, 567–582. [Google Scholar] [CrossRef] [PubMed]
- WHO Regional Office for Europe. Nutrient Profile Model: Second Edition. Available online: https://www.who.int/europe/publications/i/item/WHO-EURO-2023-6894-46660-68492 (accessed on 13 March 2023).
- Department of Health & Social Care. Calorie Labelling in the Out of Home Sector: Implementation Guidance. Available online: https://www.gov.uk/government/publications/calorie-labelling-in-the-out-of-home-sector (accessed on 16 March 2023).
- Pyne, V.; Montel, S.; Targett, V.; Little, E.; Owtram, G.; Tedstone, A.; O’Kennedy, E. Calorie Reduction Technical Report: Guidelines for Industry, 2017 Baseline in Key Foods and Next Steps. Available online: https://www.gov.uk/government/publications/calorie-reduction-guidelines-for-the-food-industry (accessed on 17 June 2021).
- Public Health England. Salt Targets 2017: Progress Report. A Report on the Food Industry’s Progress towards Meeting the 2017 Salt Targets; 2018. Available online: https://www.gov.uk/government/publications/salt-targets-2017-progress-report (accessed on 22 January 2019).
- Hollands, G.J.; Shemilt, I.; Marteau, T.M.; Jebb, S.A.; Lewis, H.B.; Wei, Y.; Higgins, J.P.; Ogilvie, D. Portion, package or tableware size for changing selection and consumption of food, alcohol and tobacco. Cochrane Database Syst. Rev. 2015, 2018, CD011045. [Google Scholar] [CrossRef]
- Bauer, J.M.; Nielsen, K.S.; Hofmann, W.; Reisch, L.A. Healthy eating in the wild: An experience-sampling study of how food environments and situational factors shape out-of-home dietary success. Soc. Sci. Med. 2022, 299, 114869. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
| Product Category | Menu | 2017 1 | 2018 | 2020 | Total | ||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||
| Biscuits | Adult’s | 70 | 101 | 172 | |||||
| Child’s | 4 | 5 | 9 | ||||||
| Total | 49 | 5.9% | 74 | 5.1% | 106 | 8.9% | 229 | 6.6% | |
| Cake | Adult’s | 328 | 318 | 646 | |||||
| Child’s | 18 | 15 | 33 | ||||||
| Total | 216 | 26.2% | 346 | 23.8% | 333 | 28.0% | 895 | 25.8% | |
| Ice-cream | Adult’s | 262 | 172 | 434 | |||||
| Child’s | 147 | 95 | 242 | ||||||
| Total | 250 | 30.3% | 409 | 28.2% | 267 | 22.4% | 926 | 26.7% | |
| Morning goods | Adult’s | 104 | 114 | 218 | |||||
| Child’s | 0 | 0 | 0 | ||||||
| Total | 93 | 11.3% | 104 | 7.2% | 114 | 9.6% | 311 | 9.0% | |
| Puddings | Adult’s | 466 | 341 | 807 | |||||
| Child’s | 52 | 30 | 82 | ||||||
| Total | 216 | 26.2% | 518 | 35.7% | 371 | 31.2% | 1105 | 31.9% | |
| Total | Adult’s | 1230 | 1046 | 2277 | |||||
| Child’s | 221 | 145 | 366 | ||||||
| Total | 824 | 100% | 1451 | 100% | 1191 | 100% | 3466 | 100% | |
| Menu | Control Variable | Correlation with kcal/portion | Sugar g/100 g | Fat g/100 g | Energy kcal/100 g | Sugar g/portion | Fat g/portion | Portion Weight (g) | Kcal per Portion |
|---|---|---|---|---|---|---|---|---|---|
| Adult’s | None | Pearson’s r | 0.056 | 0.205 | 0.108 | 0.726 | 0.872 | 0.74 | 1.000 |
| Significance 2 | 0.127 | <0.001 | 0.003 | <0.001 | <0.001 | <0.001 | |||
| df | 749 | 749 | 749 | 749 | 749 | 749 | 0 | ||
| Portion weight | Pearson’s r | 0.29 | 0.712 | 0.834 | 0.42 | 0.857 | 1.000 | ||
| Significance 2 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||
| df | 748 | 748 | 748 | 748 | 748 | 0 | |||
| Child’s | None | Pearson’s r | 0.479 | 0.621 | 0.671 | 0.825 | 0.869 | 0.456 | 1.000 |
| Significance 2 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.001 | |||
| df | 48 | 48 | 48 | 48 | 48 | 48 | 0.000 | ||
| Portion weight | Pearson’s r | 0.717 | 0.808 | 0.913 | 0.775 | 0.87 | 1.000 | ||
| Significance 2 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||
| df | 47 | 47 | 47 | 47 | 47 | 0 |
| Category | Nutrient | Menu | N | Median | IQR | % Diff | p-Value 3 | Effect Size r |
|---|---|---|---|---|---|---|---|---|
| All desserts | Sugar | Adult’s | 1046 | 28.7 | 18.1–42.1 | |||
| Child’s | 145 | 18.6 | 12.6–28.5 | −35% | <0.001 | −0.18 | ||
| kcal | Adult’s | 1046 | 372 | 265–513 | ||||
| Child’s | 145 | 171 | 94–272 | −54% | <0.001 | −0.37 | ||
| Fat | Adult’s | 1046 | 17.6 | 11.0–25.0 | ||||
| Child’s | 145 | 5.9 | 2.7–9.9 | −67% | <0.001 | −0.37 | ||
| Saturated fat | Adult’s | 1046 | 7.8 | 4.2–12.5 | ||||
| Child’s | 145 | 3.1 | 1.0–5.5 | −60% | <0.001 | −0.31 | ||
| Biscuits | Sugar | Adult’s | 101 | 19.4 | 13.0–29.0 | |||
| Child’s | 5 | 14.2 | 9.2–19.2 | −27% | 0.177 | −0.13 | ||
| kcal | Adult’s | 101 | 273 | 199–356 | ||||
| Child’s | 5 | 181 | 109–239 | −34% | 0.030 | −0.21 | ||
| Fat | Adult’s | 101 | 13.2 | 8.5–18.0 | ||||
| Child’s | 5 | 4.8 | 2.4–6.2 | −64% | 0.001 | −0.31 | ||
| Saturated fat | Adult’s | 101 | 6.6 | 3.9–9.3 | ||||
| Child’s | 5 | 1.8 | 1.0–2.7 | −73% | 0.002 | −0.30 | ||
| Cake | Sugar | Adult’s | 318 | 28.7 | 21.5–39 7 | |||
| Child’s | 15 | 32.5 | 27.2–47.2 | 13% | 0.180 | 0.07 | ||
| kcal | Adult’s | 318 | 388 | 292–488 | ||||
| Child’s | 15 | 353 | 291–392 | −9% | 0.082 | −0.12 | ||
| Fat | Adult’s | 318 | 19.6 | 12.9–25.1 | ||||
| Child’s | 15 | 14.3 | 13.8–18.9 | −27% | 0.048 | −0.11 | ||
| Saturated fat | Adult’s | 318 | 6.6 | 3.7–11.7 | ||||
| Child’s | 15 | 5.5 | 4.4–6.5 | −17% | 0.392 | −0.05 | ||
| Ice-cream | Sugar | Adult’s | 172 | 32.9 | 20.1–51.8 | |||
| Child’s | 95 | 16.6 | 11.9–24.0 | −49% | <0.001 | −0.43 | ||
| kcal | Adult’s | 172 | 275 | 164–475 | ||||
| Child’s | 95 | 117 | 94–214 | −58% | <0.001 | −0.46 | ||
| Fat | Adult’s | 172 | 11.8 | 6.0–19.9 | ||||
| Child’s | 95 | 4.6 | 1.3–8.5 | −61% | <0.001 | −0.41 | ||
| Saturated fat | Adult’s | 172 | 7.0 | 3.9–11.9 | ||||
| Child’s | 95 | 3.1 | 0.8–4.9 | −55% | <0.001 | −0.41 | ||
| Morning goods | Sugar | Adult’s | 114 | 14.5 | 8.5–20.1 | - | - | - |
| Child’s | 0 | - | - | |||||
| kcal | Adult’s | 114 | 324 | 270–381 | - | - | - | |
| Child’s | 0 | - | - | |||||
| Fat | Adult’s | 114 | 14.4 | 10.8–18.2 | - | - | - | |
| Child’s | 0 | - | - | |||||
| Saturated fat | Adult’s | 114 | 8.5 | 4.3–10.3 | ||||
| Child’s | 0 | - | - | |||||
| Puddings | Sugar | Adult’s | 341 | 35.8 | 24.0–54.7 | |||
| Child’s | 30 | 18.8 | 15.3–28.8 | −48% | <0.001 | −0.24 | ||
| kcal | Adult’s | 341 | 471 | 350–606 | ||||
| Child’s | 30 | 194 | 72–274 | −59% | <0.001 | −0.34 | ||
| Fat | Adult’s | 341 | 22.1 | 14.8–29.2 | ||||
| Child’s | 30 | 5.7 | 0.9–7.7 | −74% | <0.001 | −0.36 | ||
| Saturated fat | Adult’s | 341 | 10.5 | 5.9–16.0 | ||||
| Child’s | 30 | 2.6 | 0.4–4.3 | −75% | <0.001 | −0.32 |
| This Study 2017 vs. 2020 (Two Years’ Data) | OHID [49] 2017 vs. 2020 (Two Years’ Data) | Huang et al. [50] 2018–2020 (Three Years’ Data) | ||||
|---|---|---|---|---|---|---|
| Sugar /portion (n = 2642) | Kcal /portion (n = 2642) | Sugar /100 g (n = 1478) | Kcal /portion (n = 2930) | Sugar /portion (n = 1536) | Kcal /portion (n = 1536) | |
| Biscuits | 0% | −3% | 0% | 3% | ||
| Cakes | −9% | −10% | −8% | −16% | ||
| Ice-cream | −38% | −30% | 1% | −19% | ||
| Morning goods | 4% | 1% | −4% | −2% | ||
| Puddings | 6% | 6% | 0% | −9% | ||
| All desserts | −11% | −4% | 0% | −11% | −16% | −19% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pepper, T.; Hart, K.H.; Hodgkins, C.E. Tackling (Childhood) Obesity through a Voluntary Food Reformulation Policy: A Repeated Cross-Sectional Study Investigating Nutritional Changes in the Out-of-Home Sector. Nutrients 2023, 15, 3149. https://doi.org/10.3390/nu15143149
Pepper T, Hart KH, Hodgkins CE. Tackling (Childhood) Obesity through a Voluntary Food Reformulation Policy: A Repeated Cross-Sectional Study Investigating Nutritional Changes in the Out-of-Home Sector. Nutrients. 2023; 15(14):3149. https://doi.org/10.3390/nu15143149
Chicago/Turabian StylePepper, Tammy, Kathryn H. Hart, and Charo E. Hodgkins. 2023. "Tackling (Childhood) Obesity through a Voluntary Food Reformulation Policy: A Repeated Cross-Sectional Study Investigating Nutritional Changes in the Out-of-Home Sector" Nutrients 15, no. 14: 3149. https://doi.org/10.3390/nu15143149
APA StylePepper, T., Hart, K. H., & Hodgkins, C. E. (2023). Tackling (Childhood) Obesity through a Voluntary Food Reformulation Policy: A Repeated Cross-Sectional Study Investigating Nutritional Changes in the Out-of-Home Sector. Nutrients, 15(14), 3149. https://doi.org/10.3390/nu15143149







