Attitudes, Behaviors, and Barriers among Adolescents Living with Obesity, Caregivers, and Healthcare Professionals in Spain: ACTION Teens Survey Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Survey Development
2.3. Procedures
2.4. Outcomes
2.5. Sample Size
2.6. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Information Sources
3.3. Perceptions of Obesity
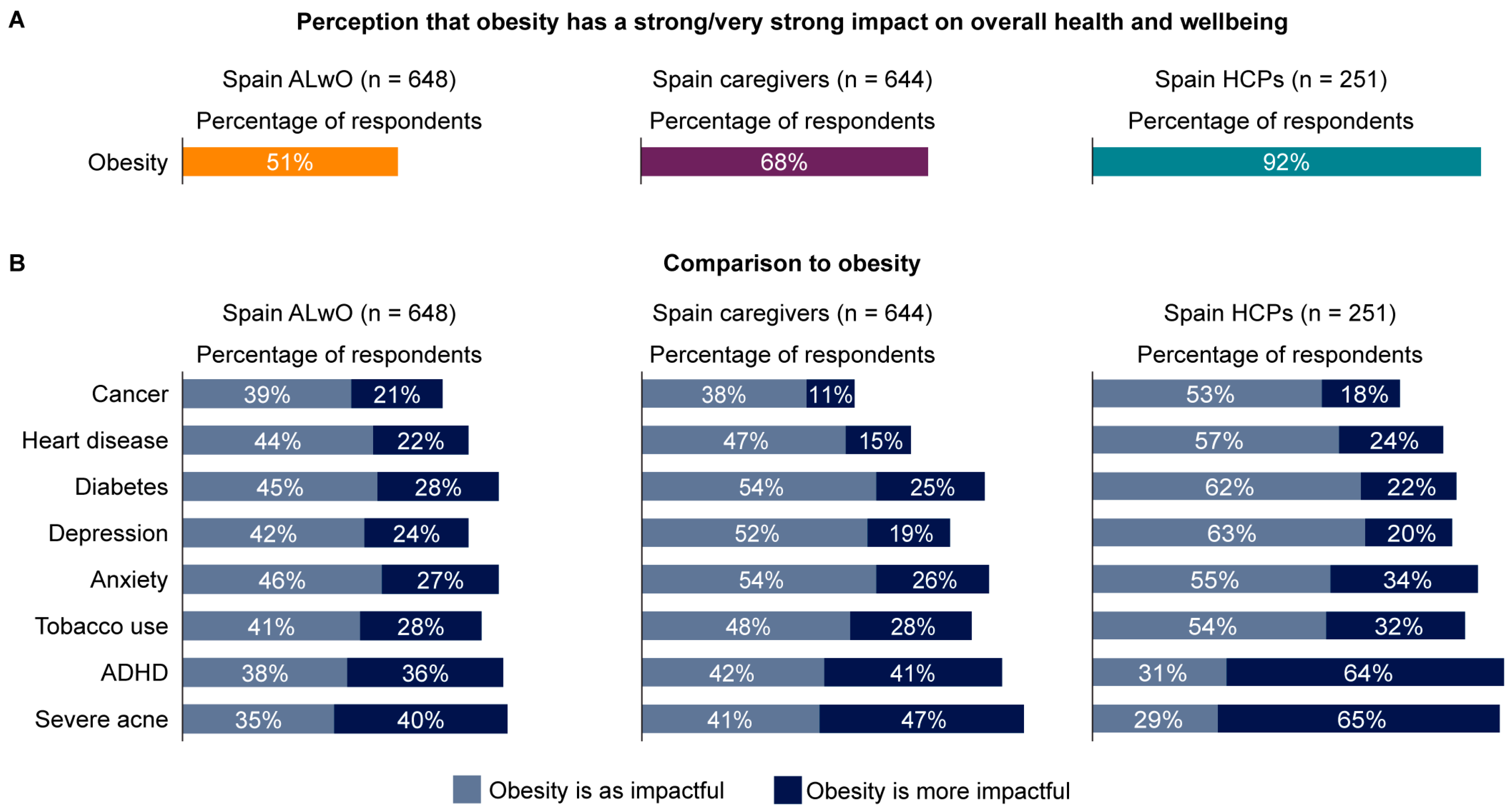
3.4. Impact of Obesity
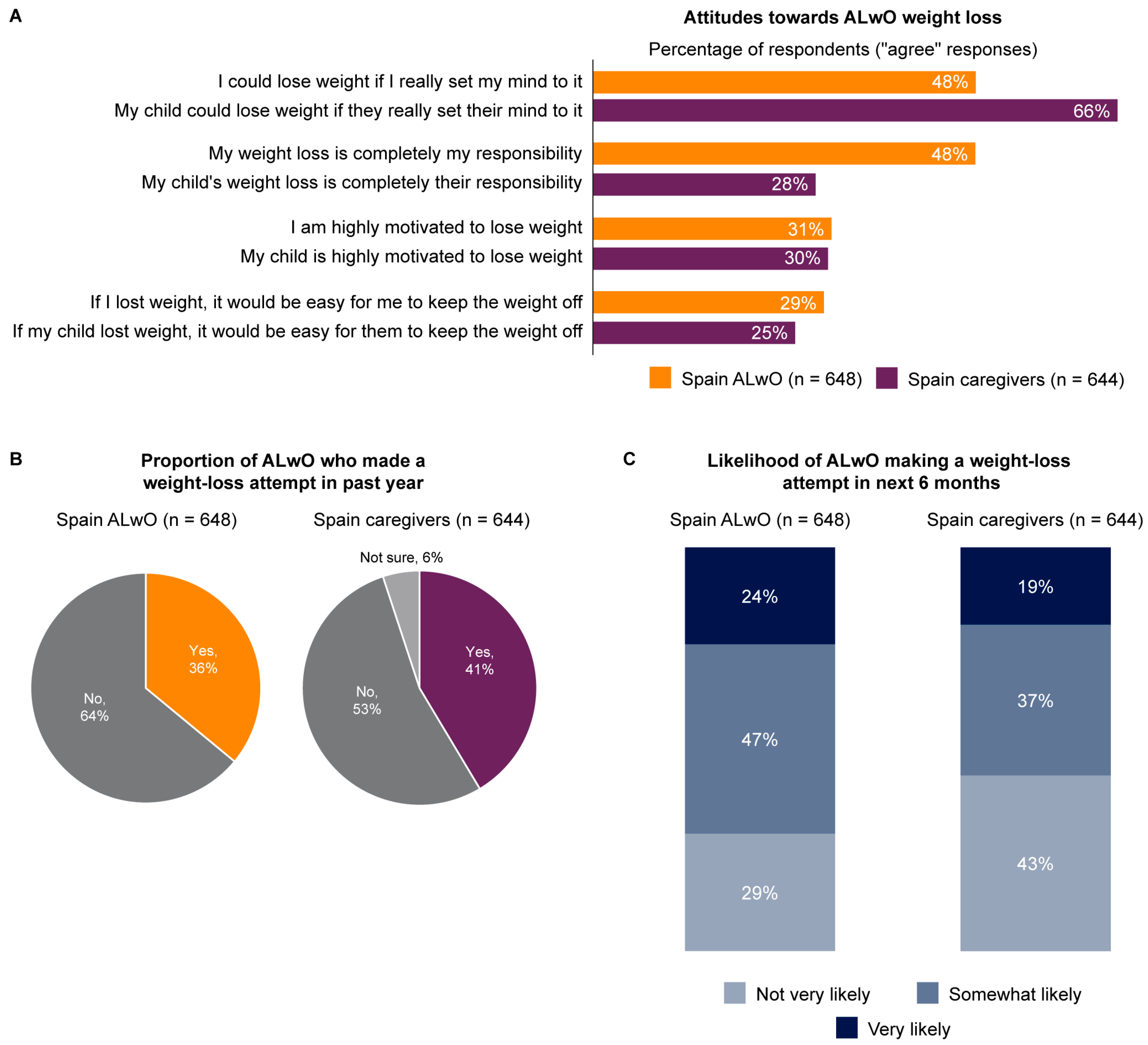
3.5. Weight Loss
3.6. Conversations about Weight
3.7. Weight Management
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [PubMed]
- Bravo-Saquicela, D.M.; Sabag, A.; Rezende, L.F.M.; Rey-Lopez, J.P. Has the prevalence of childhood obesity in Spain plateaued? A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2022, 19, 5240. [Google Scholar] [CrossRef] [PubMed]
- PASOS. Physical Activity, Sedentarism, Lifestyles and Obesity in Spanish Youth. Estudio PASOS 2022—Resultados Preliminares. Available online: https://gasolfoundation.org/wp-content/uploads/2023/01/GF-PASOS-informe-2022-WEB.pdf (accessed on 9 March 2023).
- Marcus, C.; Danielsson, P.; Hagman, E. Pediatric obesity—Long-term consequences and effect of weight loss. J. Intern. Med. 2022, 292, 870–891. [Google Scholar] [CrossRef] [PubMed]
- Nicolucci, A.; Maffeis, C. The adolescent with obesity: What perspectives for treatment? Ital. J. Pediatr. 2022, 48, 9. [Google Scholar] [CrossRef]
- Cabeza, J.F.; Aristizábal-Duque, C.H.; Sánchez, I.M.B.; Ortiz, M.R.; Almodóvar, A.R.; Ortega, M.D.; Martínez, F.E.; Saldaña, M.R.; Del Pozo, F.J.F.; Álvarez-Ossorio, M.P.; et al. Relationship between overweight and obesity and cardiac dimensions and function in a paediatric population. Eur. J. Pediatr. 2022, 181, 1943–1949. [Google Scholar] [CrossRef]
- Rankin, J.; Matthews, L.; Cobley, S.; Han, A.; Sanders, R.; Wiltshire, H.D.; Baker, J.S. Psychological consequences of childhood obesity: Psychiatric comorbidity and prevention. Adolesc. Health Med. Ther. 2016, 7, 125–146. [Google Scholar] [CrossRef]
- Simmonds, M.; Burch, J.; Llewellyn, A.; Griffiths, C.; Yang, H.; Owen, C.; Duffy, S.; Woolacott, N. The use of measures of obesity in childhood for predicting obesity and the development of obesity-related diseases in adulthood: A systematic review and meta-analysis. Health Technol. Assess. 2015, 19, 1–336. [Google Scholar] [CrossRef]
- Llewellyn, A.; Simmonds, M.; Owen, C.G.; Woolacott, N. Childhood obesity as a predictor of morbidity in adulthood: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 56–67. [Google Scholar] [CrossRef]
- Twig, G.; Yaniv, G.; Levine, H.; Leiba, A.; Goldberger, N.; Derazne, E.; Ben-Ami Shor, D.; Tzur, D.; Afek, A.; Shamiss, A.; et al. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. N. Engl. J. Med. 2016, 374, 2430–2440. [Google Scholar] [CrossRef]
- Reinehr, T.; Kleber, M.; Lass, N.; Toschke, A.M. Body mass index patterns over 5 y in obese children motivated to participate in a 1-y lifestyle intervention: Age as a predictor of long-term success. Am. J. Clin. Nutr. 2010, 91, 1165–1171. [Google Scholar] [CrossRef]
- Hagman, E.; Danielsson, P.; Lindberg, L.; Marcus, C.; BORIS Steering Committee. Paediatric obesity treatment during 14 years in Sweden: Lessons from the Swedish Childhood Obesity Treatment Register-BORIS. Pediatr. Obes. 2020, 15, e12626. [Google Scholar] [CrossRef]
- Caterson, I.D.; Alfadda, A.A.; Auerbach, P.; Coutinho, W.; Cuevas, A.; Dicker, D.; Hughes, C.; Iwabu, M.; Kang, J.H.; Nawar, R.; et al. Gaps to bridge: Misalignment between perception, reality and actions in obesity. Diabetes Obes. Metab. 2019, 21, 1914–1924. [Google Scholar] [CrossRef]
- Halford, J.C.G.; Bereket, A.; Bin-Abbas, B.; Chen, W.; Fernández-Aranda, F.; Garibay Nieto, N.; López Siguero, J.P.; Maffeis, C.; Mooney, V.; Osorto, C.K.; et al. Misalignment among adolescents living with obesity, caregivers, and healthcare professionals: ACTION Teens global survey study. Pediatr. Obes. 2022, 17, e12957. [Google Scholar] [CrossRef]
- World Health Organization: Growth Reference Data—BMI-For-Age (5–19 Years). 2007. Available online: https://www.who.int/tools/growth-reference-data-for-5to19-years/indicators/bmi-for-age (accessed on 15 June 2023).
- Inclán-López, P.; Bartolomé-Gutiérrez, R.; Martínez-Castillo, D.; Rabanales-Sotos, J.; Guisado-Requena, I.M.; Martínez-Andrés, M. Parental perception of weight and feeding practices in schoolchildren: A cross-sectional study. Int. J. Environ. Res. Public Health 2021, 18, 4014. [Google Scholar] [CrossRef]
- Ramos Salas, X.; Buoncristiano, M.; Williams, J.; Kebbe, M.; Spinelli, A.; Nardone, P.; Rito, A.; Duleva, V.; Musić Milanović, S.; Kunesova, M.; et al. Parental Perceptions of Children’s Weight Status in 22 Countries: The WHO European Childhood Obesity Surveillance Initiative: COSI 2015/2017. Obes. Facts 2021, 14, 658–674. [Google Scholar] [CrossRef]
- Regber, S.; Novak, M.; Eiben, G.; Bammann, K.; De Henauw, S.; Fernández-Alvira, J.M.; Gwozdz, W.; Kourides, Y.; Moreno, L.A.; Molnár, D.; et al. Parental perceptions of and concerns about child’s body weight in eight European countries—The IDEFICS study. Pediatr. Obes. 2013, 8, 118–129. [Google Scholar] [CrossRef]
- Wang, J.; Winkley, K.; Wei, X.; Cao, Y.; Chang, Y.S. The relationships between caregivers’ self-reported and visual perception of child weight and their non-responsive feeding practices: A systematic review and meta-analysis. Appetite 2023, 180, 106343. [Google Scholar] [CrossRef]
- Robinson, E. Overweight but unseen: A review of the underestimation of weight status and a visual normalization theory. Obes. Rev. 2017, 18, 1200–1209. [Google Scholar] [CrossRef]
- Martínez, M.; Rico, S.; Rodríguez, F.J.; Guadalupe, G.; Calderón, J.F. Influence of family environment on the development of childhood overweight and obesity in Valverde de Leganes. Eur. J. Child Dev. Educ. Psychopathol. 2016, 4, 17–29. [Google Scholar] [CrossRef]
- Ariza, C.; Ortega-Rodríguez, E.; Sánchez-Martínez, F.; Valmayor, S.; Juárez, O.; Pasarín, M.I. Childhood obesity prevention from a community view. Aten. Primaria 2015, 47, 246–255. [Google Scholar] [CrossRef]
- Grannell, A.; Fallon, F.; Al-Najim, W.; le Roux, C. Obesity and responsibility: Is it time to rethink agency? Obes. Rev. 2021, 22, e13270. [Google Scholar] [CrossRef] [PubMed]
- Hampl, S.E.; Hassink, S.G.; Skinner, A.C.; Armstrong, S.C.; Barlow, S.E.; Bolling, C.F.; Avila Edwards, K.C.; Eneli, I.; Hamre, R.; Joseph, M.M.; et al. Clinical practice guideline for the evaluation and treatment of children and adolescents with obesity. Pediatrics 2023, 151, e2022060640. [Google Scholar] [CrossRef] [PubMed]
- Lechuga Sancho, A.; Palomo Atance, E.; Rivero Martin, M.J.; Gil-Campos, M.; Leis Trabazo, R.; Bahíllo Curieses, M.P.; Bueno Lozano, G. Spanish collaborative study: Description of usual clinical practice in infant obesity. An. Pediatr. 2018, 88, 340–349. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Sanidad y Política Social. Clinical Practice Guideline on the Prevention and Treatment of Obesity in Children and Adolescents. Ministerio de Ciencia e Innovación. 2009. Available online: https://portal.guiasalud.es/wp-content/uploads/2018/12/GPC_452_obes_infantojuv_AATRM_compl.pdf (accessed on 22 June 2023).
- Alto Comisionado Para la Lucha contra la Pobreza Infantil. National Strategic Plan to Reduce Childhood Obesity (2022–2030). 2022. Available online: https://www.comisionadopobrezainfantil.gob.es/sites/default/files/Plan_obesidad_Completo_DIGITAL_paginas_1.pdf (accessed on 22 June 2023).



| Demographic/Characteristic | Spain ALwO | Spain Caregivers | Spain HCPs |
|---|---|---|---|
| Full-country sample, n | 648 | 644 | 251 |
| Matched pair (ALwO and caregiver), n (%) | 55 (8) | 55 (9) | N/A |
| Unmatched, n (%) | 593 (92) | 589 (91) | N/A |
| Age in years, mean (SD) | 15.0 (1.8) | 40.7 (8.9) | 43.2 (11.2) |
| Female, n (%) a | 231 (36) | 289 (45) | 116 (46) |
| Male, n (%) a | 417 (64) | 355 (55) | 135 (54) |
| BMI classification of ALwO b | |||
| Obesity Class I | 83% (n = 538) | 80% (n = 517) | 62% (SD: 19.9) |
| Obesity Class II | 8% (n = 51) | 13% (n = 85) | 26% (SD: 12.3) |
| Obesity Class III | 9% (n = 59) | 7% (n = 42) | 13% (SD: 11.1) |
| BMI classification of caregivers and HCPs, n (%) c | |||
| Underweight (<18.5 kg/m2) | N/A | 7 (1) | 5 (2) |
| Healthy weight (18.5–24.9 kg/m2) | N/A | 257 (40) | 147 (67) |
| Overweight (25.0–29.9 kg/m2) | N/A | 251 (39) | 53 (24) |
| Obesity Class I–III (≥30 kg/m2) | N/A | 129 (20) | 14 (6) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López Siguero, J.P.; Ramon-Krauel, M.; Pérez López, G.; Buiza Fernández, M.V.; Assaf Balut, C.; Fernández-Aranda, F. Attitudes, Behaviors, and Barriers among Adolescents Living with Obesity, Caregivers, and Healthcare Professionals in Spain: ACTION Teens Survey Study. Nutrients 2023, 15, 3005. https://doi.org/10.3390/nu15133005
López Siguero JP, Ramon-Krauel M, Pérez López G, Buiza Fernández MV, Assaf Balut C, Fernández-Aranda F. Attitudes, Behaviors, and Barriers among Adolescents Living with Obesity, Caregivers, and Healthcare Professionals in Spain: ACTION Teens Survey Study. Nutrients. 2023; 15(13):3005. https://doi.org/10.3390/nu15133005
Chicago/Turabian StyleLópez Siguero, Juan Pedro, Marta Ramon-Krauel, Gilberto Pérez López, Maria Victoria Buiza Fernández, Carla Assaf Balut, and Fernando Fernández-Aranda. 2023. "Attitudes, Behaviors, and Barriers among Adolescents Living with Obesity, Caregivers, and Healthcare Professionals in Spain: ACTION Teens Survey Study" Nutrients 15, no. 13: 3005. https://doi.org/10.3390/nu15133005
APA StyleLópez Siguero, J. P., Ramon-Krauel, M., Pérez López, G., Buiza Fernández, M. V., Assaf Balut, C., & Fernández-Aranda, F. (2023). Attitudes, Behaviors, and Barriers among Adolescents Living with Obesity, Caregivers, and Healthcare Professionals in Spain: ACTION Teens Survey Study. Nutrients, 15(13), 3005. https://doi.org/10.3390/nu15133005







