A Body Shape Index and Its Changes in Relation to All-Cause Mortality among the Chinese Elderly: A Retrospective Cohort Study
Abstract
1. Introduction
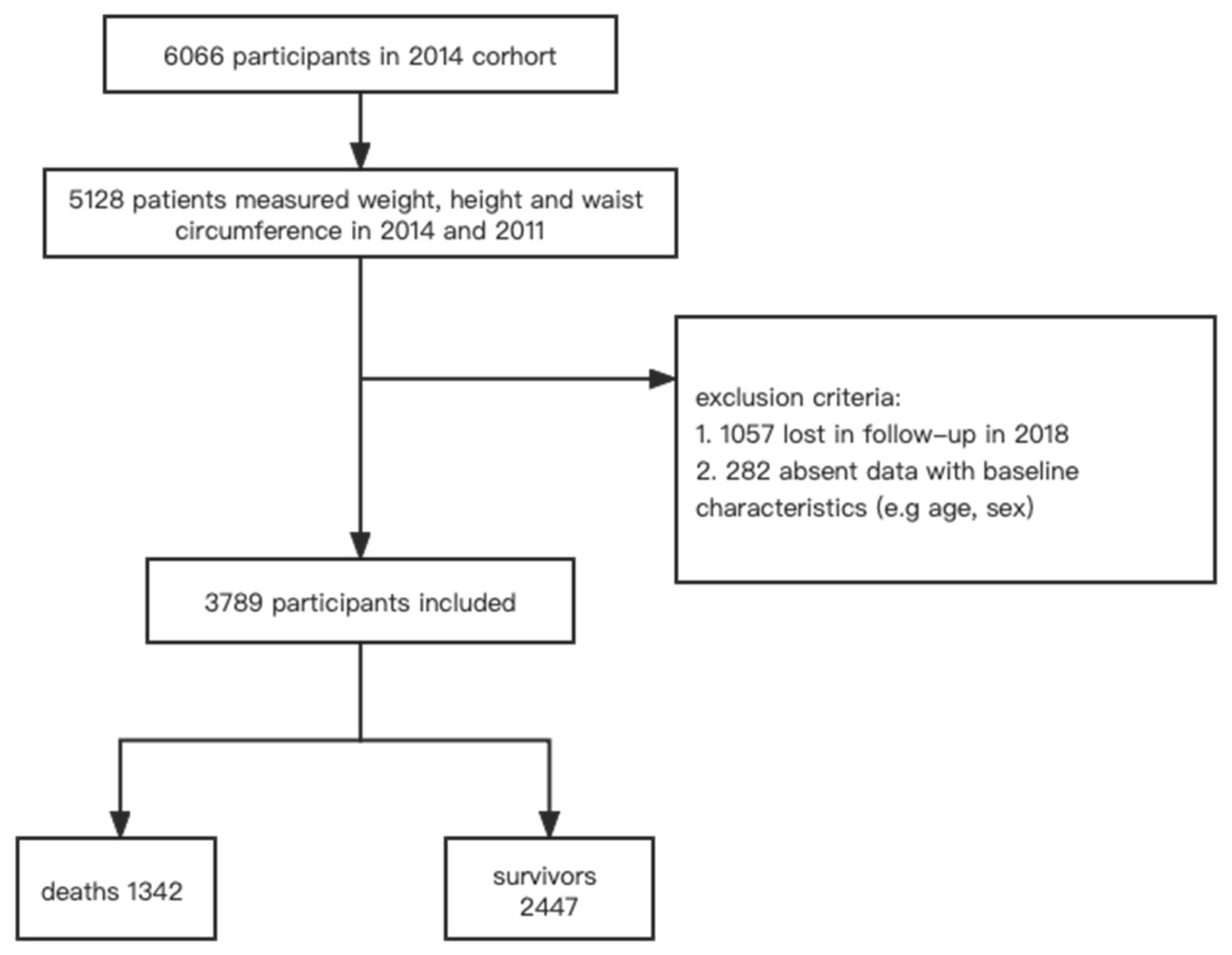
2. Materials and Methods
2.1. Study Design and Setting
2.2. Main Exposure and Outcome
2.3. Covariates
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics of Participants According to Tertiles of A Body Shape Index
3.2. Association of Baseline ABSI with All-Cause Mortality
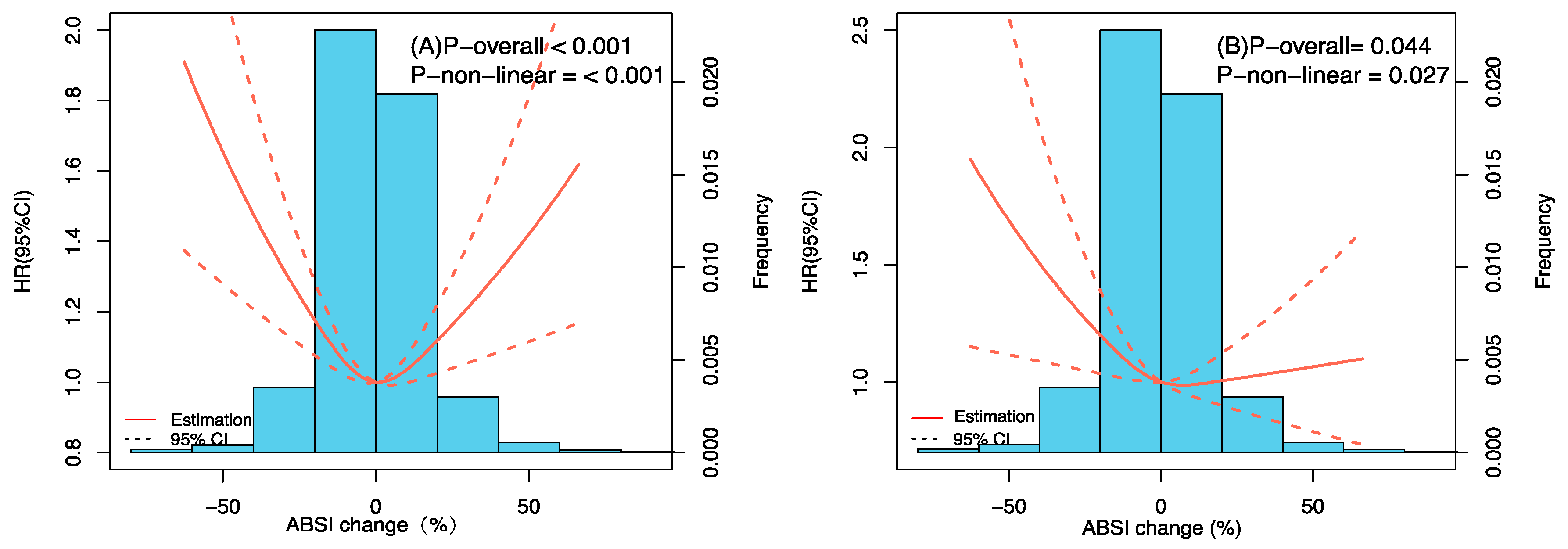
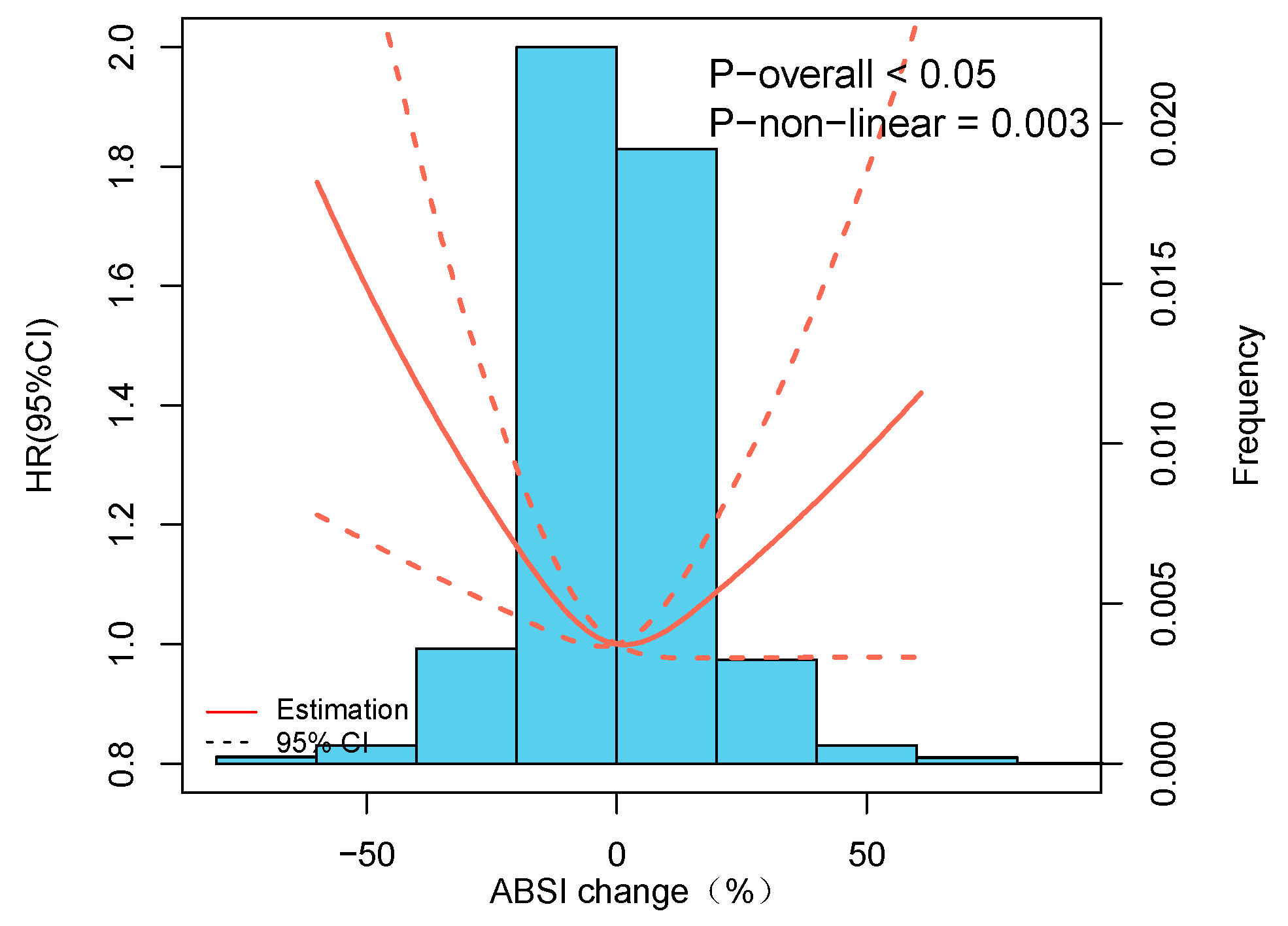
3.3. Association of ABSI Changes (from 2011 to 2014) with Mortality from All Causes
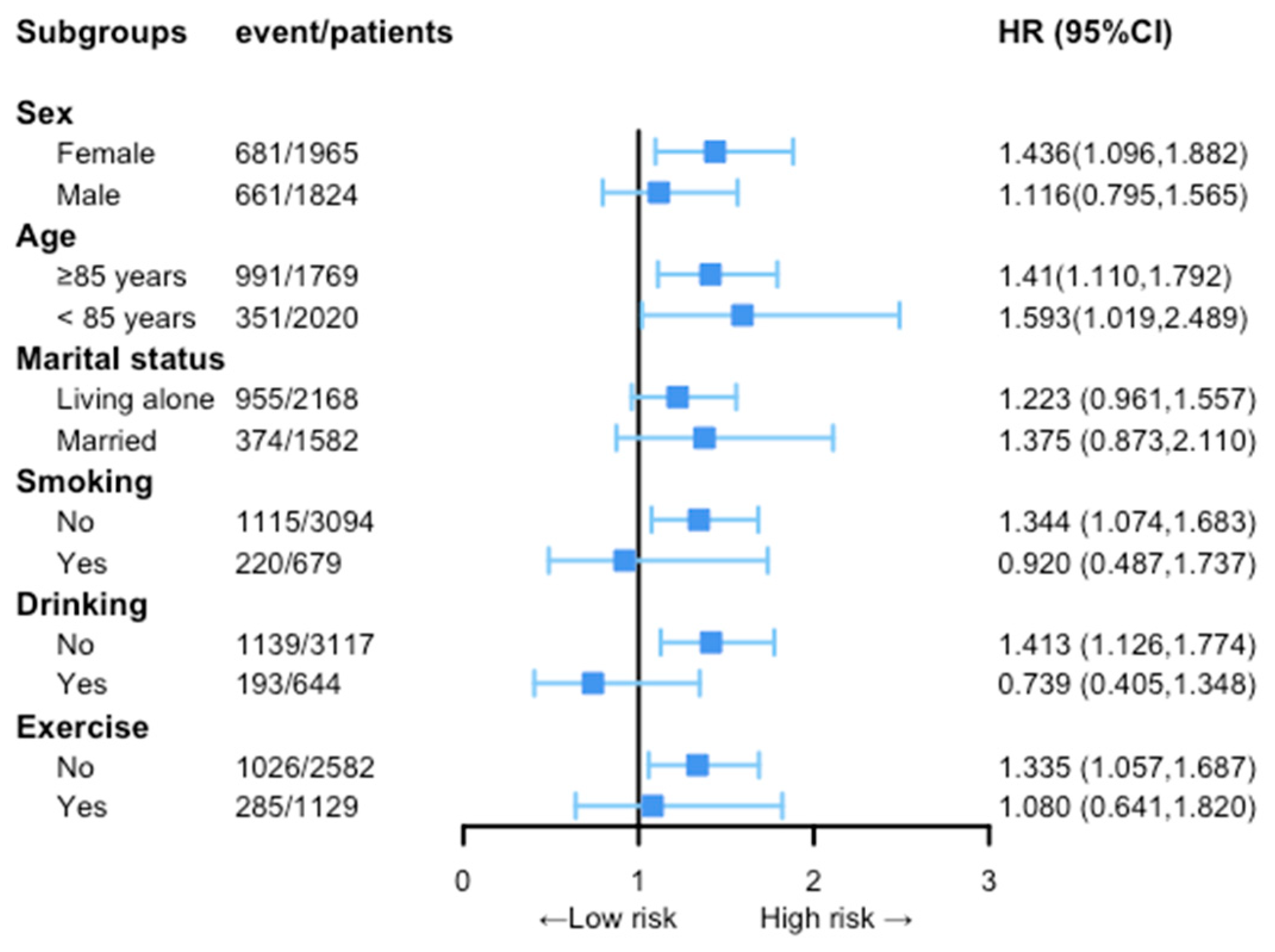
3.4. Subgroup Group Analysis of the Association of Relative ABSI Changes with All-Cause Mortality
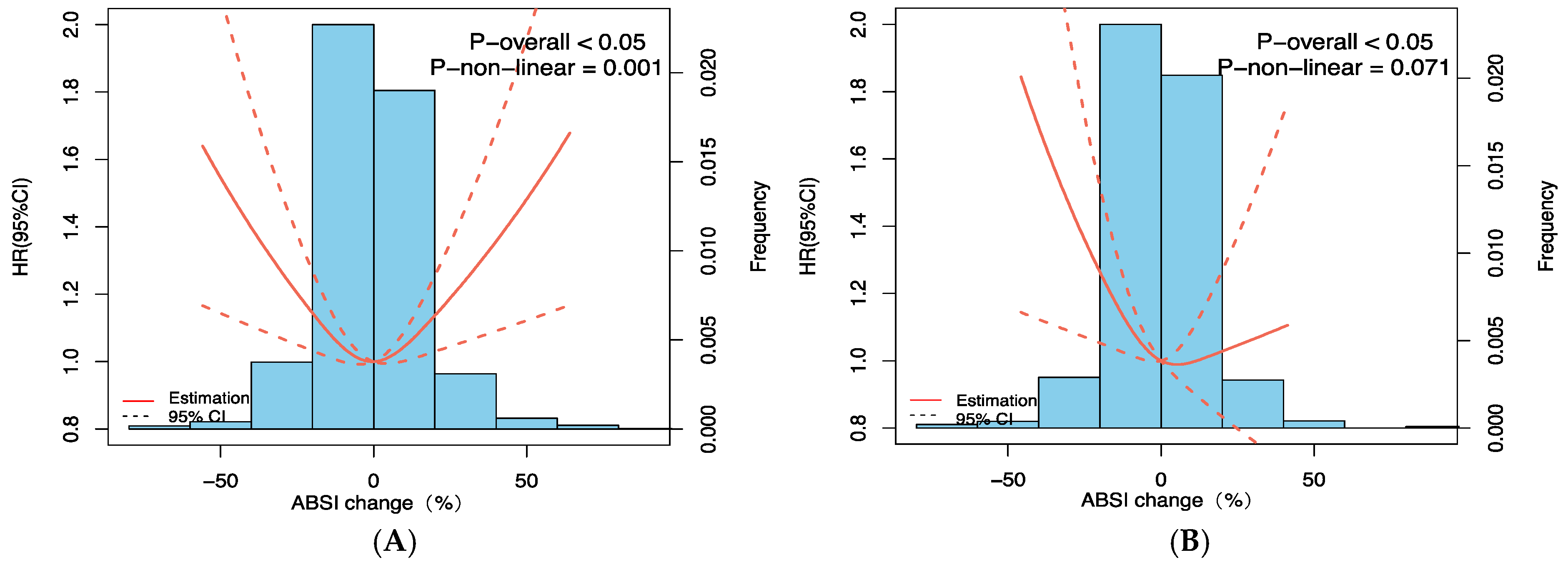
3.5. Sensitivity Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Beard, J.R.; Officer, A.; de Carvalho, I.A.; Sadana, R.; Pot, A.M.; Michel, J.P.; Lloyd-Sherlock, P.; Epping-Jordan, J.E.; Peeters, G.; Mahanani, W.R.; et al. The World report on ageing and health: A policy framework for healthy ageing. Lancet 2016, 387, 2145–2154. [Google Scholar] [CrossRef] [PubMed]
- Enoki, H.; Kuzuya, M.; Masuda, Y.; Hirakawa, Y.; Iwata, M.; Hasegawa, J.; Izawa, S.; Iguchi, A. Anthropometric measurements of mid-upper arm as a mortality predictor for community-dwelling Japanese elderly: The Nagoya Longitudinal Study of Frail Elderly (NLS-FE). Clin. Nutr. 2007, 26, 597–604. [Google Scholar] [CrossRef] [PubMed]
- Rossini-Venturini, A.C.; Veras, L.; Abdalla, P.P.; Santos, A.P.D.; Tasinafo-Junior, M.F.; Silva, L.; Alves, T.C.; Ferriolli, E.; Romo-Perez, V.; Garcia-Soidan, J.L.; et al. Multicompartment body composition analysis in older adults: A cross-sectional study. BMC Geriatr. 2023, 23, 87. [Google Scholar] [CrossRef]
- Bhaskaran, K.; Dos-Santos-Silva, I.; Leon, D.A.; Douglas, I.J.; Smeeth, L. Association of BMI with overall and cause-specific mortality: A population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol. 2018, 6, 944–953. [Google Scholar] [CrossRef]
- Hussain, S.M.; Newman, A.B.; Beilin, L.J.; Tonkin, A.M.; Woods, R.L.; Neumann, J.T.; Nelson, M.; Carr, P.R.; Reid, C.M.; Owen, A.; et al. Associations of Change in Body Size with All-Cause and Cause-Specific Mortality Among Healthy Older Adults. JAMA Netw. Open 2023, 6, e237482. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.F.; Tang, Z.; Guo, J.; Tao, L.X.; Liu, L.; Li, H.B.; Li, D.T.; Guo, X.H.; Yang, X.H. BMI and BMI Changes to All-cause Mortality among the Elderly in Beijing: A 20-year Cohort Study. Biomed. Environ. Sci. BES 2017, 30, 79–87. [Google Scholar] [CrossRef]
- Böhm, A.; Heitmann, B.L. The use of bioelectrical impedance analysis for body composition in epidemiological studies. Eur. J. Clin. Nutr. 2013, 67 (Suppl. S1), S79–S85. [Google Scholar] [CrossRef]
- Ross, R.; Neeland, I.J.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; Cuevas, A.; Hu, F.B.; et al. Waist circumference as a vital sign in clinical practice: A Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 2020, 16, 177–189. [Google Scholar] [CrossRef]
- Krakauer, N.Y.; Krakauer, J.C. A new body shape index predicts mortality hazard independently of body mass index. PLoS ONE 2012, 7, e39504. [Google Scholar] [CrossRef]
- Krakauer, N.Y.; Krakauer, J.C. Dynamic association of mortality hazard with body shape. PLoS ONE 2014, 9, e88793. [Google Scholar] [CrossRef]
- Sun, X.; Cao, L.; Liu, Y.; Huang, W.; Pei, C.; Wang, X.; Feng, S.; Song, B. Sex- and age-specific differences in associations of a body shape index with all-cause and cardiovascular death risks among US adults with diabetes. Nutr. Metab. Cardiovasc. Dis. 2023, 33, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Christakoudi, S.; Tsilidis, K.K.; Muller, D.C.; Freisling, H.; Weiderpass, E.; Overvad, K.; Söderberg, S.; Häggström, C.; Pischon, T.; Dahm, C.C.; et al. A Body Shape Index (ABSI) achieves better mortality risk stratification than alternative indices of abdominal obesity: Results from a large European cohort. Sci. Rep. 2020, 10, 14541. [Google Scholar] [CrossRef]
- Grant, J.F.; Chittleborough, C.R.; Shi, Z.; Taylor, A.W. The association between A Body Shape Index and mortality: Results from an Australian cohort. PLoS ONE 2017, 12, e0181244. [Google Scholar] [CrossRef]
- Su, X.; Li, K.; Yang, L.; Yang, Y.; Gao, Y.; Gao, Y.; Guo, J.; Lin, J.; Chen, K.; Han, J.; et al. Associations between abdominal obesity and the risk of stroke in Chinese older patients with obstructive sleep apnea: Is there an obesity paradox? Front. Aging Neurosci. 2022, 14, 957396. [Google Scholar] [CrossRef]
- Lv, Y.; Mao, C.; Gao, X.; Ji, J.S.; Kraus, V.B.; Yin, Z.; Yuan, J.; Chen, H.; Luo, J.; Zhou, J.; et al. The obesity paradox is mostly driven by decreased noncardiovascular disease mortality in the oldest old in China: A 20-year prospective cohort study. Nat. Aging 2022, 2, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Ren, Z.; Li, Y.; Li, X.; Shi, H.; Zhao, H.; He, M.; Zha, S.; Qiao, S.; Pu, Y.; Liu, H.; et al. Associations of body mass index, waist circumference and waist-to-height ratio with cognitive impairment among Chinese older adults: Based on the CLHLS. J. Affect. Disord. 2021, 295, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Y.; Feng, Q.; Hesketh, T.; Christensen, K.; Vaupel, J.W. Survival, disabilities in activities of daily living, and physical and cognitive functioning among the oldest-old in China: A cohort study. Lancet 2017, 389, 1619–1629. [Google Scholar] [CrossRef]
- Portero-McLellan, K.C.; Staudt, C.; Silva, F.R.; Delbue Bernardi, J.L.; Baston Frenhani, P.; Leandro Mehri, V.A. The use of calf circumference measurement as an anthropometric tool to monitor nutritional status in elderly inpatients. J. Nutr. Health Aging 2010, 14, 266–270. [Google Scholar] [CrossRef]
- Chen, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Chou, M.Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307.e302. [Google Scholar] [CrossRef]
- Başıbüyük, G.; Ayremlou, P.; Saeidlou, S.N.; Ay, F.; Dalkıran, A.; Simzari, W.; Vitályos, G.; Bektaş, Y. A comparison of the different anthropometric indices for assessing malnutrition among older people in Turkey: A large population-based screening. J. Health Popul. Nutr. 2021, 40, 13. [Google Scholar] [CrossRef]
- Bullock, A.F.; Greenley, S.L.; McKenzie, G.A.G.; Paton, L.W.; Johnson, M.J. Relationship between markers of malnutrition and clinical outcomes in older adults with cancer: Systematic review, narrative synthesis and meta-analysis. Eur. J. Clin. Nutr. 2020, 74, 1519–1535. [Google Scholar] [CrossRef]
- Aune, D.; Norat, T.; Vatten, L.J. Body mass index, abdominal fatness and the risk of gallbladder disease. Eur. J. Epidemiol. 2015, 30, 1009–1019. [Google Scholar] [CrossRef] [PubMed]
- Gurunathan, U.; Myles, P.S. Limitations of body mass index as an obesity measure of perioperative risk. Br. J. Anaesth. 2016, 116, 319–321. [Google Scholar] [CrossRef] [PubMed]
- Jayedi, A.; Soltani, S.; Zargar, M.S.; Khan, T.A.; Shab-Bidar, S. Central fatness and risk of all cause mortality: Systematic review and dose-response meta-analysis of 72 prospective cohort studies. BMJ Clin. Res. Ed. 2020, 370, m3324. [Google Scholar] [CrossRef] [PubMed]
- Carmienke, S.; Freitag, M.H.; Pischon, T.; Schlattmann, P.; Fankhaenel, T.; Goebel, H.; Gensichen, J. General and abdominal obesity parameters and their combination in relation to mortality: A systematic review and meta-regression analysis. Eur. J. Clin. Nutr. 2013, 67, 573–585. [Google Scholar] [CrossRef]
- Biolo, G.; Di Girolamo, F.G.; Breglia, A.; Chiuc, M.; Baglio, V.; Vinci, P.; Toigo, G.; Lucchin, L.; Jurdana, M.; Pražnikar, Z.J.; et al. Inverse relationship between “a body shape index” (ABSI) and fat-free mass in women and men: Insights into mechanisms of sarcopenic obesity. Clin. Nutr. 2015, 34, 323–327. [Google Scholar] [CrossRef]
- Kim, B.; Kim, G.; Kim, E.; Park, J.; Isobe, T.; Sakae, T.; Oh, S. The A Body Shape Index Might Be a Stronger Predictor of Chronic Kidney Disease Than BMI in a Senior Population. Int. J. Environ. Res. Public Health 2021, 18, 12874. [Google Scholar] [CrossRef]
- Duncan, M.J.; Mota, J.; Vale, S.; Santos, M.P.; Ribeiro, J.C. Associations between body mass index, waist circumference and body shape index with resting blood pressure in Portuguese adolescents. Ann. Hum. Biol. 2013, 40, 163–167. [Google Scholar] [CrossRef]
- Bawadi, H.; Abouwatfa, M.; Alsaeed, S.; Kerkadi, A.; Shi, Z. Body Shape Index Is a Stronger Predictor of Diabetes. Nutrients 2019, 11, 1018. [Google Scholar] [CrossRef]
- Corbatón-Anchuelo, A.; Krakauer, J.C.; Serrano-García, I.; Krakauer, N.Y.; Martínez-Larrad, M.T.; Serrano-Ríos, M. A Body Shape Index (ABSI) and Hip Index (HI) Adjust Waist and Hip Circumferences for Body Mass Index, But Only ABSI Predicts High Cardiovascular Risk in the Spanish Caucasian Population. Metab. Syndr. Relat. Disord. 2021, 19, 352–357. [Google Scholar] [CrossRef]
- Zhao, W.; Tong, J.J.; Cao, Y.T.; Li, J.H. A Linear Relationship Between a Body Shape Index and Risk of Incident Type 2 Diabetes: A Secondary Analysis Based on a Retrospective Cohort Study in Japan. Diabetes Metab. Syndr. Obes. 2020, 13, 2139–2146. [Google Scholar] [CrossRef]
- Eom, B.W.; Joo, J.; Yoon, H.M.; Ryu, K.W.; Kim, Y.W.; Lee, J.H. A body shape index has a good correlation with postoperative complications in gastric cancer surgery. Ann. Surg. Oncol. 2014, 21, 1115–1122. [Google Scholar] [CrossRef]
- Nascimento-Souza, M.A.; Mambrini, J.V.M.; Peixoto, S.V.; Lima-Costa, M.F. Association between “a body shape index” and mortality: Bambuí Cohort Study of Aging, Brazil. Cad. Saude Publica 2021, 37, e00016020. [Google Scholar] [CrossRef] [PubMed]
- He, S.; Zheng, Y.; Wang, H.; Chen, X. Assessing the relationship between a body shape index and mortality in a group of middle-aged men. Clin. Nutr. 2017, 36, 1355–1359. [Google Scholar] [CrossRef]
- Hu, L.; Huang, X.; You, C.; Li, J.; Hong, K.; Li, P.; Wu, Y.; Wu, Q.; Wang, Z.; Gao, R.; et al. Prevalence of overweight, obesity, abdominal obesity and obesity-related risk factors in southern China. PLoS ONE 2017, 12, e0183934. [Google Scholar] [CrossRef] [PubMed]
- Sniderman, A.D.; Bhopal, R.; Prabhakaran, D.; Sarrafzadegan, N.; Tchernof, A. Why might South Asians be so susceptible to central obesity and its atherogenic consequences? The adipose tissue overflow hypothesis. Int. J. Epidemiol. 2007, 36, 220–225. [Google Scholar] [CrossRef]
- Yuan, Y.; Liu, K.; Zheng, M.; Chen, S.; Wang, H.; Jiang, Q.; Xiao, Y.; Zhou, L.; Liu, X.; Yu, Y.; et al. Analysis of Changes in Weight, Waist Circumference, or Both, and All-Cause Mortality in Chinese Adults. JAMA Netw. Open 2022, 5, e2225876. [Google Scholar] [CrossRef] [PubMed]
- Galea, M.; Gauci, G.; Calleja-Agius, J.; Schembri-Wismayer, P. Peritoneal biomarkers in the early detection of ovarian cancer. Minerva Ginecol. 2017, 69, 84–99. [Google Scholar] [CrossRef] [PubMed]
- Schwabl, P.; Bucsics, T.; Soucek, K.; Mandorfer, M.; Bota, S.; Blacky, A.; Hirschl, A.M.; Ferlitsch, A.; Trauner, M.; Peck-Radosavljevic, M.; et al. Risk factors for development of spontaneous bacterial peritonitis and subsequent mortality in cirrhotic patients with ascites. Liver Int. 2015, 35, 2121–2128. [Google Scholar] [CrossRef]
- Tey, S.L.; Huynh, D.T.T.; Berde, Y.; Baggs, G.; How, C.H.; Low, Y.L.; Cheong, M.; Chow, W.L.; Tan, N.C.; Chew, S.T.H. Prevalence of low muscle mass and associated factors in community-dwelling older adults in Singapore. Sci. Rep. 2021, 11, 23071. [Google Scholar] [CrossRef]
- Tarnowski, M.; Stein, E.; Marcadenti, A.; Fink, J.; Rabito, E.; Silva, F.M. Calf Circumference Is a Good Predictor of Longer Hospital Stay and Nutritional Risk in Emergency Patients: A Prospective Cohort Study. J. Am. Coll. Nutr. 2020, 39, 645–649. [Google Scholar] [CrossRef] [PubMed]
- Murphy, R.A.; Wilke, M.S.; Perrine, M.; Pawlowicz, M.; Mourtzakis, M.; Lieffers, J.R.; Maneshgar, M.; Bruera, E.; Clandinin, M.T.; Baracos, V.E.; et al. Loss of adipose tissue and plasma phospholipids: Relationship to survival in advanced cancer patients. Clin. Nutr. 2010, 29, 482–487. [Google Scholar] [CrossRef] [PubMed]
- Gill, C.M.; Torriani, M.; Murphy, R.; Harris, T.B.; Miller, K.K.; Klibanski, A.; Bredella, M.A. Fat Attenuation at CT in Anorexia Nervosa. Radiology 2016, 279, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Silva, C.; Zhang, Q.; Bone, J.N.; Amed, S. Anthropometric Measurements and Laboratory Investigations in Children and Youth with Type 1 Diabetes Before and During the COVID-19 Pandemic. Can. J. Diabetes 2022, 46, 683–690. [Google Scholar] [CrossRef]
- Ko, H.J.; Cho, Y.J.; Kim, K.K.; Kang, J.H.; Kim, Y.S.; Haam, J.H.; Hur, Y.I.; Choi, H.I.; Lee, K.R.; Park, J.H.; et al. COVID-19 and related social distancing measures induce significant metabolic complications without prominent weight gain in Korean adults. Front. Med. 2022, 9, 951793. [Google Scholar] [CrossRef]


| Characteristics | Total | T1 ≤0.080 | T2 0.081~0.088 | T3 ≥0.089 | p |
|---|---|---|---|---|---|
| N | 3789 | 1262 | 1264 | 1263 | |
| Relative body shape index (%) | −0.74 ± 15.98 | −11.15 ± 15.07 | −0.2 ± 11.12 | 9.15 ± 14.48 | <0.001 |
| Calf circumference (cm) | 30.81 ± 6.49 | 30.70 ± 6.77 | 31.32 ± 6.50 | 30.41 ± 6.16 | 0.002 |
| Body mass index (kg/m2) | 21.81 ± 3.71 | 22.67 ± 3.72 | 22.11 ± 3.53 | 20.65 ± 3.60 | <0.001 |
| Waist circumference (cm) | 80.98 ± 11.88 | 73.30 ± 11.52 | 82.40 ± 9.40 | 87.24 ± 10.10 | <0.001 |
| Age (year) | 84.43 ± 10.00 | 83.64 ± 10.24 | 83.04 ± 9.61 | 83.61 ± 9.81 | <0.001 |
| Gender (n, %) | <0.001 | ||||
| Male | 1824(48.1%) | 658(17.4%) | 661(17.4%) | 505(13.3%) | |
| Female | 1965(51.9%) | 604(15.9%) | 603(15.9%) | 758(20.01%) | |
| Marital status (n, %) | <0.001 | ||||
| Married | 1582(42.2%) | 545(14.5%) | 579(15.4%) | 458(12.2%) | |
| Living alone | 2168(57.8%) | 708(18.9%) | 668 (17.8%) | 792(21.1%) | |
| Residence (n, %) | 0.198 | ||||
| City | 479(12.6%) | 149(3.9%) | 174(4.6%) | 156(4.1%) | |
| Town | 1313(34.7%) | 422(11.1%) | 428(11.3%) | 463(12.2%) | |
| Rural | 1997(52.7%) | 691(18.2%) | 662(17.5%) | 644(17.0%) | |
| Drinking (n, %) | 0.005 | ||||
| Yes | 644(17.1%) | 226(6.0%) | 239(6.4%) | 179(4.8%) | |
| No | 3117(82.9%) | 1023(27.2%) | 1022(27.2%) | 1072(28.5%) | |
| Smoking (n, %) | 0.003 | ||||
| Yes | 679(18.0%) | 251(6.7%) | 240(6.4%) | 188 (5.0%) | |
| No | 3094(82.0%) | 1009(26.7%) | 1019(27.0%) | 1066(28.3%) | |
| Exercise (n, %) | 0.033 | ||||
| Yes | 1129(30.4%) | 373(10.1%) | 396(10.7%) | 360(9.7%) | |
| No | 2582(69.6%) | 854(23.0%) | 847(22.8%) | 881(23.7%) | |
| Hypertension (n, %) | 1287(35.9%) | 408(11.4%) | 467(13.0%) | 412(11.5%) | 0.01 |
| Diabetes (n, %) | 244(6.4%) | 68(1.9%) | 88(2.5%) | 68(1.9%) | 0.132 |
| Heart disease (n, %) | 498(14.0%) | 147(4.1%) | 167(4.7%) | 184(5.2%) | 0.061 |
| Stroke or CVD (n, %) | 308(8.7%) | 101(2.9%) | 106(3.0%) | 101(2.9%) | 0.923 |
| Vital status (n, %) | <0.001 | ||||
| Dead | 1342(35.4%) | 449(11.9%) | 385(10.2%) | 508(13.4%) | |
| Alive | 2447(64.6%) | 813(21.5%) | 879(23.2%) | 755(19.9%) |
| Total (n) | Death (n) | Crude Model | Model 1 | Model 2 | Model 3 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | |||
| ABSI z-score | 3789 | 1342 | 1.071 (1.015, 1.131) | 0.013 | 1.397 (1.159, 1.683) | <0.001 | 1.223 (1.005, 1.489) | 0.045 | 1.293 (1.046, 1.599) | 0.018 |
| ABSI tertiles | ||||||||||
| T3 | 1263 | 508 | Reference | Reference | Reference | Reference | ||||
| T2 | 1264 | 385 | 0.715 (0.626, 0.816) | <0.001 | 0.906 (0.777, 1.056) | 0.206 | 0.916 (0.783, 1.071) | 0.270 | 0.874 (0.738, 1.053) | 0.118 |
| T1 | 1262 | 449 | 0.847 (0.746, 0.96) | 0.010 | 0.992 (0.809, 1.218) | 0.942 | 1.003 (0.813, 1.237) | 0.978 | 0.925 (0.735, 1.164) | 0.505 |
| Per 10% Increase in ABSI | Per 10% Reduction in ABSI | |||
|---|---|---|---|---|
| HRs | 95% CI | HRs | 95% CI | |
| Crude model | 1.062 | 1.059–1.065 | 1.096 | 1.091–1.100 |
| Model 1 | 1.026 | 1.025–1.027 | 1.044 | 1.042–1.045 |
| Model 2 | 1.027 | 1.026–1.028 | 1.038 | 1.037–1.040 |
| Model 3 | 1.043 | 1.041–1.045 | 1.054 | 1.052–1.057 |
| Model 4 | 1.019 | 1.018–1.020 | 1.094 | 1.090–1.099 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, N.; Zhuo, J.; Xie, S.; Qu, Z.; Li, W.; Li, Z.; Guo, P.; Gao, M.; Qin, H.; Han, T. A Body Shape Index and Its Changes in Relation to All-Cause Mortality among the Chinese Elderly: A Retrospective Cohort Study. Nutrients 2023, 15, 2943. https://doi.org/10.3390/nu15132943
Yang N, Zhuo J, Xie S, Qu Z, Li W, Li Z, Guo P, Gao M, Qin H, Han T. A Body Shape Index and Its Changes in Relation to All-Cause Mortality among the Chinese Elderly: A Retrospective Cohort Study. Nutrients. 2023; 15(13):2943. https://doi.org/10.3390/nu15132943
Chicago/Turabian StyleYang, Ning, Jialu Zhuo, Suyi Xie, Zhihua Qu, Wei Li, Zixiang Li, Panpan Guo, Mingbo Gao, Huanlong Qin, and Ting Han. 2023. "A Body Shape Index and Its Changes in Relation to All-Cause Mortality among the Chinese Elderly: A Retrospective Cohort Study" Nutrients 15, no. 13: 2943. https://doi.org/10.3390/nu15132943
APA StyleYang, N., Zhuo, J., Xie, S., Qu, Z., Li, W., Li, Z., Guo, P., Gao, M., Qin, H., & Han, T. (2023). A Body Shape Index and Its Changes in Relation to All-Cause Mortality among the Chinese Elderly: A Retrospective Cohort Study. Nutrients, 15(13), 2943. https://doi.org/10.3390/nu15132943





