Association between Wine Consumption with Cardiovascular Disease and Cardiovascular Mortality: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
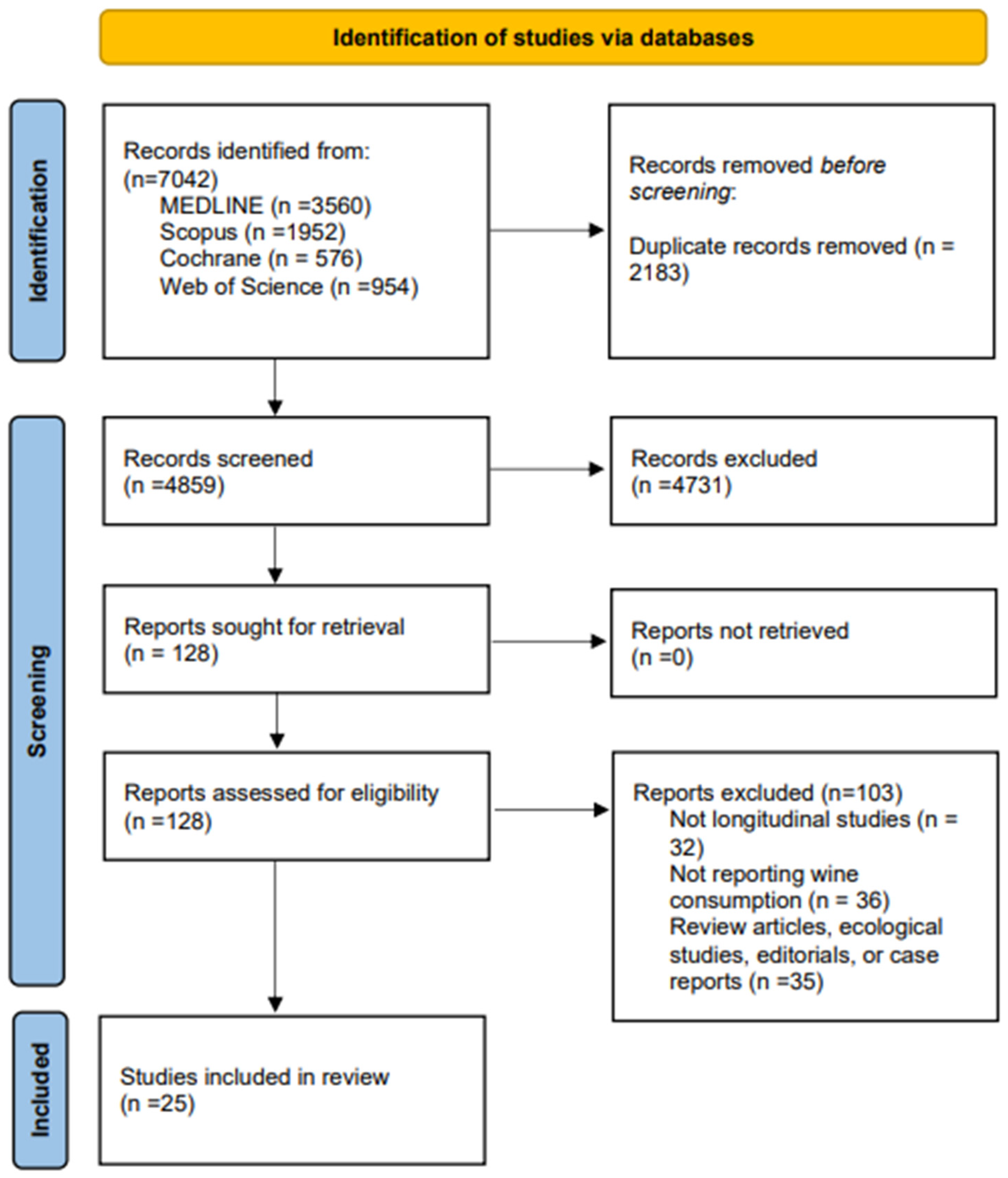
2. Methods
2.1. Search Strategy
2.2. Selection Criteria
2.3. Data Extraction and Risk of Bias Assessment
| Reference | Country | Design of Study | Characteristics of the Participants | Follow Up (Years) | Outcome | ||
|---|---|---|---|---|---|---|---|
| N, Women (%) | Age (SD) | Type of Population | |||||
| Kaufman et al. 1985 [35] | EE.UU. | Case–Control | Cases: 123 Controls: 66 | Cases: 30 to 54 Controls: 30 to 54 | Men | NR | CHD |
| Klatsky et al. 1986 [36] | EE.UU. | Cohort | 13,056 (55.8) | - | General population | 5 | CHD |
| Klatsky et al. 1990 [37] | EE.UU. | Cohort | 28,488 | 40.5 | General population | 8 | CHD CVD |
| Klatsky et al. 1992 [38] | EE.UU. | Cohort | 128,934 (55.9) | 30–70 | General population | 8 | Mortality |
| Klatsky et al. 1993 [39] | EE.UU. | Cohort | 17,527 (60.6) | 41.4 | General population | 8 | Mortality |
| Gronbaek et al. 1995 [40] | Denmark | Cohort | 3498 (54.5) | 30–70 | General population | 11 | Mortality |
| Renaud et al. 1999 [41] | France | Cohort | 22,093 (0) | 49.22 (5.74) | Men | 12–18 | Mortality CVD |
| Theobald et al. 2000 [42] | Sweden | Cohort | 385 | 18–65 | General population | 22 | Mortality |
| Gronbaek et al. 2000 [43] | Denmark | Cohort | 12,846 (44) | 20–98 | General population | NR | CHD |
| Tavani et al. 2001 [44] | Italy | Case–Control | Cases: 507 (25.4) Controls:478 (37.9) | 45–70 | General population | NR | CHD |
| Mukamal et al. 2003 [45] | EE.UU. | Cohort | 38,077 (0) | 53.9 | Male health professionals | 12 | CHD |
| Marques-Vidal et al. 2004 [46] | France | Cohort |
| 54.9 (2.9) | General population | 4 | CHD |
| Dorn et al. 2007 [47] | EE.UU. | Case–Control | Cases: 33 Controls: 360 | Cases: 56.1 (8.5) Controls: 53.7 (9.8) | Women | 6 | CHD |
| Burke et al. 2007 [48] | Australia | Cohort | 514 (49.8) | 15–88 | General population | 11.6 | CVD |
| Schröder et al. 2007 [49] | Spain | Case–Control | Cases: 244 (0) Controls: 1270 (0) | Cases: 58.8 (10.9) Controls: 50.2 (13.5) | Men | NR | CHD |
| Suadicani et al. 2008 [50] | Denmark | Cohort | 3022 (0) | 40–59 | Men | 16 | Mortality |
| Gémes et al. 2016 [51] | Norway | Cohort | 58,827 (54) | 49.1 (16.9) | General population | 11.6 | CHD |
| Britton et al. 2016 [52] | United Kingdom | Cohort | 7010 (70.66) | 56 (6) | General population | 25 | Mortality |
| Tverdal et al. 2017 [53] | Norway | Cohort | 115,592 (63) | 41 | General population | 6 | CVD |
| Ricci et al. 2018 [23] | Europe | Cohort | 17,594 (43) | 35–70 | General population | 12.5 | CHD |
| Song et al. 2018 [54] | EE.UU. | Cohort | 156,728 (8) | 65.3 (12.1) | Veterans | 2.9 | CHD |
| Panagiotakos et al. 2019 [55] | Greece | Cohort | 3042 (50.2) | 18–88 | General population (The ATTICA study) | 8.4 | CVD |
| Schutte et al. 2020 [56] | United Kingdom | Cohort | 446,439 (53.8) | 56.4 (8.1) | General population | 4 | CHD |
| Maugeri et al. 2020 [57] | Czech Republic | Cohort | 1773 (54.95) | 46.75 | General population | NR | CVD |
| Schutte et al. 2021 [22] | United Kingdom | Cohort | 354,969 (60.4) | 56.7 (8.3) | General population (Alcohol consumers and never drinkers) | 6.9 | CHD CVD |
2.4. Data Synthesis and Statistical Analysis
3. Results
3.1. Systematic Review
3.2. Risk of Bias Assessment
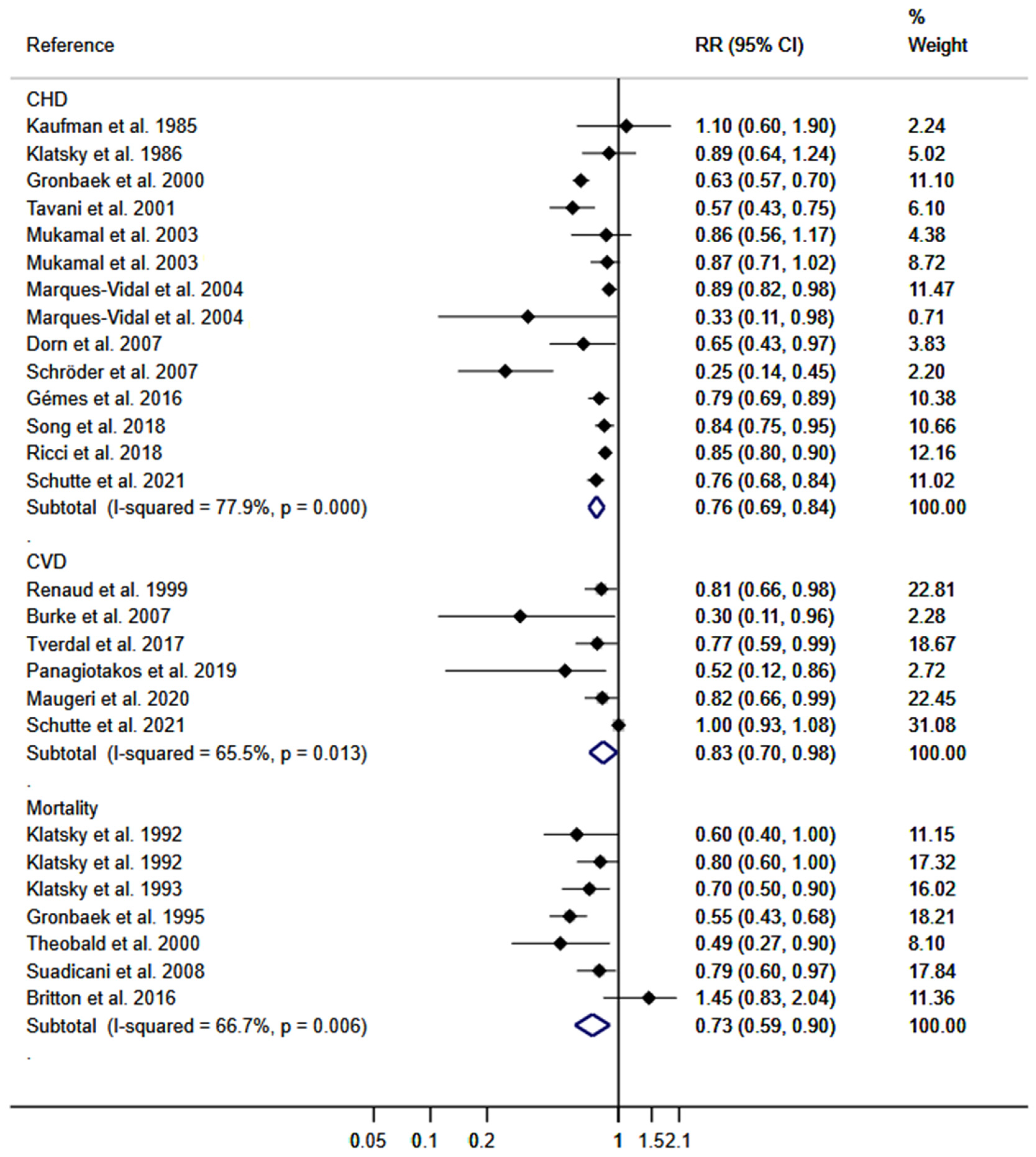
3.3. Meta-Analysis
3.4. Sensitivity Analysis and Meta-Regression Models
3.5. Publication Bias
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Global Status Report on Noncommunicable Diseases 2014; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Council of the European Union. 2586th Council Meeting—Employment, Social Policy, Health and Consumer Affairs. Available online: http://ue.eu.int/Newsroom/ (accessed on 29 November 2004).
- Lozano, R.; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K.; Aboyans, V.; Abraham, J.; Adair, T.; Aggarwal, R.; Ahn, S.Y.; et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2095–2128. [Google Scholar] [CrossRef]
- Petersen, S.; Peto, V.; Rayner, M.; Leal, J.; Luengo-Fernandez, R.; Gray, A. European Cardiovascular Disease Statistics; British Heart Foundation: London, UK, 2005. [Google Scholar]
- Alcohol (who.int) Informe Mundial de Situación sobre Alcohol y Salud; World Health Organization: Geneva, Switzerland, 2018.
- Booyse, F.M.; Parks, D.A. Moderate wine and alcohol consumption: Beneficial effects on cardiovascular disease. Thromb. Haemost. 2001, 86, 517–528. [Google Scholar]
- Wood, A.M.; Kaptoge, S.; Butterworth, A.S.; Willeit, P.; Warnakula, S.; Bolton, T.; Paige, E.; Paul, D.S.; Sweeting, M.; Burgess, S.; et al. Risk thresholds for alcohol consumption: Combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet 2018, 391, 1513–1523. [Google Scholar] [CrossRef] [PubMed]
- Renaud, S.; de Lorgeril, M. Wine, alcohol, platelets, and the French paradox for coronary heart disease. Lancet 1992, 339, 1523–1526. [Google Scholar] [CrossRef]
- Xu, W.; Wang, H.; Wan, Y.; Tan, C.; Li, J.; Tan, L.; Yu, J.-T. Alcohol consumption and dementia risk: A dose–response meta-analysis of prospective studies. Eur. J. Epidemiol. 2017, 32, 31–42. [Google Scholar] [CrossRef] [PubMed]
- Biddinger, K.J.; Emdin, C.A.; Haas, M.E.; Wang, M.; Hindy, G.; Ellinor, P.T.; Kathiresan, S.; Khera, A.V.; Aragam, K.G. Association of Habitual Alcohol Intake with Risk of Cardiovascular Disease. JAMA Netw. Open 2022, 5, e223849. [Google Scholar] [CrossRef]
- National Institute on Alcohol Abuse and Alcoholism. Harmful Interactions: Mixing Alcohol with Medicines. National Institutes of Health, US Department of Health and Human Services; 2014a. NIH Publication No 13-5329. Available online: http://pubs.niaaa.nih.gov/publications/Medicine/medicine.htm (accessed on 10 June 2023).
- Breslow, R.A.; Dong, C.; White, A. Prevalence of Alcohol-Interactive Prescription Medication Use Among Current Drinkers: United States, 1999 to 2010. Alcohol. Clin. Exp. Res. 2015, 39, 371–379. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, P.; Halaweish, F.; Dwivedi, C. Antioxidant Effects and Drug Interactions of Resveratrol Present in Wine. J. Wine Res. 2007, 18, 59–71. [Google Scholar] [CrossRef]
- Salehi, B.; Mishra, A.P.; Nigam, M.; Sener, B.; Kilic, M.; Sharifi-Rad, M.; Fokou, P.V.T.; Martins, N.; Sharifi-Rad, J. Resveratrol: A Double-Edged Sword in Health Benefits. Biomedicines 2018, 6, 91. [Google Scholar] [CrossRef]
- Borges, G.; Bagge, C.L.; Cherpitel, C.J.; Conner, K.R.; Orozco, R.; Rossow, I. A meta-analysis of acute use of alcohol and the risk of suicide attempt. Psychol. Med. 2017, 47, 949–957. [Google Scholar] [CrossRef]
- Haseeb, S.; Alexander, B.; Baranchuk, A. Wine and Cardiovascular Health: A Comprehensive Review. Circulation 2017, 136, 1434–1448. [Google Scholar] [CrossRef]
- Holmes, M.V.; Dale, C.E.; Zuccolo, L.; Silverwood, R.J.; Guo, Y.; Ye, Z.; Prieto-Merino, D.; Dehghan, A.; Trompet, S.; Wong, A.; et al. Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. BMJ 2014, 349, g4164. [Google Scholar] [CrossRef] [PubMed]
- Chiva-Blanch, G.; Arranz, S.; Lamuela-Raventos, R.M.; Estruch, R. Effects of wine, alcohol and polyphenols on cardiovascular disease risk factors: Evidences from hu-man studies. Alcohol Alcohol. 2013, 48, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Snopek, L.; Mlček, J.; Fic, V.; Hlaváčová, I.; Škrovánková, S.; Fisera, M.; Velichová, H.; Ondrášová, M. Interaction of polyphenols and wine antioxidants with its sulfur dioxide preservative. Potravin. Slovak J. Food Sci. 2018, 12, 180–185. [Google Scholar] [CrossRef]
- Teissedre, P.L.; Stockley, C.; Boban, M.; Gambert, P.; Alba, M.O.; Flesh, M.; Ruf, J.C. The effects of wine consumption on cardiovascular disease and associated risk factors: A narrative review. OENO One 2018, 52, 67–79. [Google Scholar] [CrossRef]
- Rimm, E.B.; Klatsky, A.; Grobbee, D.; Stampfer, M.J. Review of moderate alcohol consumption and reduced risk of coronary heart disease: Is the effect due to beer, wine, or spirits? BMJ 1996, 312, 731–736. [Google Scholar] [CrossRef]
- Schutte, R.; Smith, L.; Wannamethee, G. Alcohol—The myth of cardiovascular protection. Clin. Nutr. 2021, 41, 348–355. [Google Scholar] [CrossRef]
- Ricci, C.; Wood, A.; Muller, D.; Gunter, M.J.; Agudo, A.; Boeing, H.; van der Schouw, Y.T.; Warnakula, S.; Saieva, C.; Spijkerman, A.; et al. Alcohol intake in relation to non-fatal and fatal coronary heart disease and stroke: EPIC-CVD case-cohort study. BMJ 2018, 361, k934. [Google Scholar] [CrossRef]
- Rasines-Perea, Z.; Teissedre, P.-L. Grape Polyphenols’ Effects in Human Cardiovascular Diseases and Diabetes. Molecules 2017, 22, 68. [Google Scholar] [CrossRef] [PubMed]
- Zheng, H.; Guo, H.; Hong, Y.; Zheng, F.; Wang, J. The effects of age and resveratrol on the hypoxic preconditioning protection against hypoxia–reperfusion injury: Studies in rat hearts and human cardiomyocytes. Eur. J. Cardio Thorac. Surg. 2015, 48, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Mankowski, R.T.; You, L.; Buford, T.W.; Leeuwenburgh, C.; Manini, T.M.; Schneider, S.; Qiu, P.; Anton, S.D. Higher dose of resveratrol elevated cardiovascular disease risk biomarker levels in overweight older adults—A pilot study. Exp. Gerontol. 2020, 131, 110821. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, S.; Dudley, J.I.; Das, D.K. Dose-Dependency of Resveratrol in Providing Health Benefits. Dose-Response 2010, 8, 478–500. [Google Scholar] [CrossRef]
- Jang, M.; Cai, L.; Udeani, G.O.; Slowing, K.V.; Thomas, C.F.; Beecher, C.W.W.; Fong, H.H.S.; Farnsworth, N.R.; Kinghorn, A.D.; Mehta, R.G.; et al. Cancer Chemopreventive Activity of Resveratrol, a Natural Product Derived from Grapes. Science 1997, 275, 218–220. [Google Scholar] [CrossRef]
- Sabia, S.; Fayosse, A.; Dumurgier, J.; Dugravot, A.; Akbaraly, T.; Britton, A.; Kivimäki, M.; Singh-Manoux, A. Alcohol consumption and risk of dementia: 23 year follow-up of Whitehall II cohort study. BMJ 2018, 362, k2927. [Google Scholar] [CrossRef] [PubMed]
- Boffetta, P.; Garfinkel, L. Alcohol Drinking and Mortality among Men Enrolled in an American Cancer Society Prospective Study. Epidemiology 1990, 1, 342–348. [Google Scholar] [CrossRef]
- Costanzo, S.; Di Castelnuovo, A.; Donati, M.B.; Iacoviello, L.; de Gaetano, G. Wine, beer or spirit drinking in relation to fatal and non-fatal cardiovascular events: A meta-analysis. Eur. J. Epidemiol. 2011, 26, 833–850. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (Updated March 2011); The Cochrane Collaboration: London, UK, 2011. [Google Scholar]
- Meta-Analysis of Observational Studies in Epidemiology (MOOSE) Group. Meta-analysis of observational studies in epidemiology: A proposal for reporting. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. National Heart, Lung, and Blood Institute. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 20 February 2022).
- Kaufman, D.W.; Rosenberg, L.; Helmrich, S.P.; Shapiro, S. Alcoholic beverages and myocardial infarction in young men1. Am. J. Epidemiol. 1985, 121, 548–554. [Google Scholar] [CrossRef]
- Klatsky, A.L.; Armstrong, M.A.; Friedman, G.D. Relations of alcoholic beverage use to subsequent coronary artery disease hospitalization. Am. J. Cardiol. 1986, 58, 710–714. [Google Scholar] [CrossRef]
- Klatsky, A.L.; Armstrong, M.A.; Friedman, G.D. Risk of cardiovascular mortality in alcohol drinkers, ex-drinkers and nondrinkers. Am. J. Cardiol. 1990, 66, 1237–1242. [Google Scholar] [CrossRef]
- Klatsky, A.L.; Armstrong, M.A.; Friedman, G.D. Alcohol and Mortality. Ann. Intern. Med. 1992, 117, 646–654. [Google Scholar] [CrossRef]
- Klatsky, A.L.; Armstrong, M.A. Alcoholic beverage choice and risk of coronary artery disease mortality: Do red wine drinkers fare best? Am. J. Cardiol. 1993, 71, 467–469. [Google Scholar] [CrossRef] [PubMed]
- Gronbaek, M.; Deis, A.; Sorensen, T.I.; Becker, U.; Schnohr, P.; Jensen, G. Mortality associated with moderate intakes of wine, beer, or spirits. BMJ 1995, 310, 1165–1169. [Google Scholar] [CrossRef] [PubMed]
- Renaud, S.C.; Guéguen, R.; Siest, G.; Salamon, R. Wine, Beer, and Mortality in Middle-aged Men from Eastern France. Arch. Intern. Med. 1999, 159, 1865–1870. [Google Scholar] [CrossRef]
- Theobald, H.; Bygren, L.O.; Carstensen, J.; Engfeldt, P. A moderate intake of wine is associated with reduced total mortality and reduced mortality from cardiovascular disease. J. Stud. Alcohol 2000, 61, 652–656. [Google Scholar] [CrossRef]
- Grønbæk, M.K.; Becker, U.; Johansen, D.; Gottschau, A.; Schnohr, P.; Hein, H.O.; Jensen, G.; Sørensen, T.I. Type of Alcohol Consumed and Mortality from All Causes, Coronary Heart Disease, and Cancer. Ann. Intern. Med. 2000, 133, 411–419. [Google Scholar] [CrossRef]
- Tavani, A.; Bertuzzi, M.; Negri, E.; Sorbara, L.; La Vecchia, C. Alcohol, smoking, coffee and risk of non-fatal acute myocardial infarction in Italy. Eur. J. Epidemiol. 2001, 17, 1131–1137. [Google Scholar] [CrossRef]
- Mukamal, K.J.; Conigrave, K.M.; Mittleman, M.A.; Camargo, C.A., Jr.; Stampfer, M.J.; Willett, W.C.; Rimm, E.B. Roles of Drinking Pattern and Type of Alcohol Consumed in Coronary Heart Disease in Men. N. Engl. J. Med. 2003, 348, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Marques-Vidal, P.; Montaye, M.; Arveiler, D.; Evans, A.; Bingham, A.; Ruidavets, J.-B.; Amouyel, P.; Haas, B.; Yarnell, J.; Ducimetière, P.; et al. Alcohol consumption and cardiovascular disease: Differential effects in France and Northern Ireland. The PRIME study. Eur. J. Prev. Cardiol. 2004, 11, 336–343. [Google Scholar] [CrossRef]
- Dorn, J.M.; Hovey, K.; Williams, B.A.; Freudenheim, J.L.; Russell, M.; Nochajski, T.H.; Trevisan, M. Alcohol drinking pattern and non-fatal myocardial infarction in women. Addiction 2007, 102, 730–739. [Google Scholar] [CrossRef]
- Burke, V.; Lee, A.H.; Hunter, E.; Spargo, R.; Smith, R.; Beilin, L.J.; Puddey, I.B. Alcohol intake and incidence of coronary disease in australian aborigines. Alcohol Alcohol. 2007, 42, 119–124. [Google Scholar] [CrossRef]
- Schröder, H.; Masabeu, A.; Marti, M.J.; Cols, M.; Lisbona, J.M.; Romagosa, C.; Carión, T.; Vilert, E.; Marrugat, J. Myocardial infarction and alcohol consumption: A population-based case-control study. Nutr. Metab. Cardiovasc. Dis. 2007, 17, 609–615. [Google Scholar] [CrossRef]
- Suadicani, P.; Hein, H.O.; Gyntelberg, F. Wine intake, ABO phenotype, and risk of ischemic heart disease and all-cause mortality: The Copenhagen Male Study—A 16-year follow-up. Alcohol 2008, 42, 575–582. [Google Scholar] [CrossRef]
- Gémes, K.; Janszky, I.; Laugsand, L.E.; László, K.D.; Ahnve, S.; Vatten, L.J.; Mukamal, K.J. Alcohol consumption is associated with a lower incidence of acute myocardial infarction: Results from a large prospective population-based study in Norway. J. Intern. Med. 2016, 279, 365–375. [Google Scholar] [CrossRef]
- Britton, A.; O’neill, D.; Bell, S. Underestimating the Alcohol Content of a Glass of Wine: The Implications for Estimates of Mortality Risk. Alcohol Alcohol. 2016, 51, 609–614. [Google Scholar] [CrossRef] [PubMed]
- Tverdal, A.; Magnus, P.; Selmer, R.; Thelle, D. Consumption of alcohol and cardiovascular disease mortality: A 16 year follow-up of 115,592 Norwegian men and women aged 40–44 years. Eur. J. Epidemiol. 2017, 32, 775–783. [Google Scholar] [CrossRef]
- Song, R.J.; Nguyen, X.-M.T.; Quaden, R.; Ho, Y.-L.; Justice, A.C.; Gagnon, D.R.; Cho, K.; O’Donnell, C.J.; Concato, J.; Gaziano, J.M.; et al. Alcohol Consumption and Risk of Coronary Artery Disease (from the Million Veteran Program). Am. J. Cardiol. 2018, 121, 1162–1168. [Google Scholar] [CrossRef]
- Panagiotakos, D.B.; Kouli, G.-M.; Magripis, E.; Kyrou, I.; Georgousopoulou, E.N.; Chrysohoou, C.; Tsigos, C.; Tousoulis, D.; Pitsavos, C. Beer, wine consumption, and 10-year CVD incidence: The ATTICA study. Eur. J. Clin. Nutr. 2019, 73, 1015–1023. [Google Scholar] [CrossRef] [PubMed]
- Schutte, R.; Papageorgiou, M.; Najlah, M.; Huisman, H.W.; Ricci, C.; Zhang, J.; Milner, N.; Schutte, A.E. Drink types unmask the health risks associated with alcohol intake—Prospective evidence from the general population. Clin. Nutr. 2020, 39, 3168–3174. [Google Scholar] [CrossRef] [PubMed]
- Maugeri, A.; Hlinomaz, O.; Agodi, A.; Barchitta, M.; Kunzova, S.; Bauerova, H.; Sochor, O.; Medina-Inojosa, J.R.; Lopez-Jimenez, F.; Vinciguerra, M.; et al. Is Drinking Alcohol Really Linked to Cardiovascular Health? Evidence from the Kardiovize 2030 Project. Nutrients 2020, 12, 2848. [Google Scholar] [CrossRef]
- National Institutes of Health. Quality Assessment of Case-Control Studies. National Heart, Lung, and Blood Institute. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 19 February 2022).
- Sxtare, J.; Maucort-Boulch, D. Odds Ratio, Hazard Ratio and Relative Risk. Adv. Methodol. Stat. 2016, 13, 59–67. [Google Scholar]
- DerSimonian, R.; Kacker, R. Random-effects model for meta-analysis of clinical trials: An update. Contemp. Clin. Trials 2007, 28, 105–114. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Stettler, C.; Allemann, S.; Wandel, S.; Kastrati, A.; Morice, M.C.; Schömig, A.; Pfisterer, M.E.; Stone, G.W.; Leon, M.B.; De Lezo, J.S.; et al. Drug eluting and bare metal stents in people with and without diabetes: Collaborative network meta-analysis. BMJ 2008, 337, a1331. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Egger, M.; Smith, G.D. Systematic reviews in health care: Investigating and dealing with publication and other biases in meta-analysis. BMJ 2001, 323, 101–105. [Google Scholar] [CrossRef] [PubMed]
- St Leger, A.; Cochrane, A.L.; Moore, F. Factors associated with cardiac mortality in developed countries with particular reference to the consumption of wine. Lancet 1979, 313, 1017–1020. [Google Scholar] [CrossRef]
- Fragopoulou, E.; Choleva, M.; Antonopoulou, S.; Demopoulos, C.A. Wine and its metabolic effects. A comprehensive review of clinical trials. Metabolism 2018, 83, 102–119. [Google Scholar] [CrossRef]
- Frankel, E.; German, J.; Kinsella, J.; Parks, E.; Kanner, J. Inhibition of oxidation of human low-density lipoprotein by phenolic substances in red wine. Lancet 1993, 341, 454–457. [Google Scholar] [CrossRef]
- Folts, J.D.; Demrow, H.S.; Slane, P.R. 2 glasses of red but not white wine inhibits ex-vivo platelet-aggregation and increases bleeding-time in human volunteers. J. Am. Coll. Cardiol. 1994, 655, A66. [Google Scholar]
- Wang, Z.; Du, A.; Liu, H.; Wang, Z.; Hu, J. Systematic Analysis of the Global, Regional and National Burden of Cardiovascular Diseases from 1990 to 2017. J. Epidemiol. Glob. Health 2022, 12, 92–103. [Google Scholar] [CrossRef]
- Roth, G.A.; Johnson, C.; Abajobir, A.; Abd-Allah, F.; Abera, S.F.; Abyu, G.; Ahmed, M.; Aksut, B.; Alam, T.; Alam, K.; et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017, 70, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Di Castelnuovo, A.; Rotondo, S.; Iacoviello, L.; Donati, M.B.; De Gaetano, G. Meta-Analysis of Wine and Beer Consumption in Relation to Vascular Risk. Circulation 2002, 105, 2836–2844. [Google Scholar] [CrossRef] [PubMed]
- Marcos, A.; Serra-Majem, L.; Pérez-Jiménez, F.; Pascual, V.; Tinahones, F.J.; Estruch, R. Moderate Consumption of Beer and Its Effects on Cardiovascular and Metabolic Health: An Updated Review of Recent Scientific Evidence. Nutrients 2021, 13, 879. [Google Scholar] [CrossRef]
- Costanzo, S.; Di Castelnuovo, A.; Donati, M.B.; Iacoviello, L.; de Gaetano, G. Cardiovascular and Overall Mortality Risk in Relation to Alcohol Consumption in Patients with Cardiovascular Disease. Circulation 2010, 121, 1951–1959. [Google Scholar] [CrossRef]
- Rehm, J.; Sempos, C.T.; Trevisan, M. Alcohol and cardiovascular disease--more than one paradox to consider. Average volume of alcohol consumption, patterns of drinking and risk of coronary heart disease--a review. J. Cardiovasc. Risk 2003, 10, 15–20. [Google Scholar] [CrossRef]
- Bagnardi, V.; Zatonski, W.; Scotti, L.; La Vecchia, C.; Corrao, G. Does drinking pattern modify the effect of alcohol on the risk of coronary heart disease? Evidence from a meta-analysis. J. Epidemiol. Community Health 2008, 62, 615–619. [Google Scholar] [CrossRef]
- Criqui, M.H.; Ringel, B.L. Does diet or alcohol explain the French paradox? Lancet 1994, 344, 1719–1723. [Google Scholar] [CrossRef] [PubMed]
- Broustet, J.-P. Wine and health. Heart 1999, 81, 459–460. [Google Scholar] [CrossRef]
- Wollin, S.D.; Jones, P.J.H. Alcohol, Red Wine and Cardiovascular Disease. J. Nutr. 2001, 131, 1401–1404. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lucerón-Lucas-Torres, M.; Saz-Lara, A.; Díez-Fernández, A.; Martínez-García, I.; Martínez-Vizcaíno, V.; Cavero-Redondo, I.; Álvarez-Bueno, C. Association between Wine Consumption with Cardiovascular Disease and Cardiovascular Mortality: A Systematic Review and Meta-Analysis. Nutrients 2023, 15, 2785. https://doi.org/10.3390/nu15122785
Lucerón-Lucas-Torres M, Saz-Lara A, Díez-Fernández A, Martínez-García I, Martínez-Vizcaíno V, Cavero-Redondo I, Álvarez-Bueno C. Association between Wine Consumption with Cardiovascular Disease and Cardiovascular Mortality: A Systematic Review and Meta-Analysis. Nutrients. 2023; 15(12):2785. https://doi.org/10.3390/nu15122785
Chicago/Turabian StyleLucerón-Lucas-Torres, Maribel, Alicia Saz-Lara, Ana Díez-Fernández, Irene Martínez-García, Vicente Martínez-Vizcaíno, Iván Cavero-Redondo, and Celia Álvarez-Bueno. 2023. "Association between Wine Consumption with Cardiovascular Disease and Cardiovascular Mortality: A Systematic Review and Meta-Analysis" Nutrients 15, no. 12: 2785. https://doi.org/10.3390/nu15122785
APA StyleLucerón-Lucas-Torres, M., Saz-Lara, A., Díez-Fernández, A., Martínez-García, I., Martínez-Vizcaíno, V., Cavero-Redondo, I., & Álvarez-Bueno, C. (2023). Association between Wine Consumption with Cardiovascular Disease and Cardiovascular Mortality: A Systematic Review and Meta-Analysis. Nutrients, 15(12), 2785. https://doi.org/10.3390/nu15122785










