Nocturnal Hemodialysis Leads to Improvement in Physical Performance in Comparison with Conventional Hemodialysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Dialysis Treatments
2.3. Outcomes
2.3.1. Physical Performance
2.3.2. Protein-Energy Wasting
2.3.3. Quality of Life and Sleep Parameters
2.4. Statistical Analysis
2.4.1. Sample Size
2.4.2. Analysis of Outcomes
3. Results
3.1. Recruitment
3.2. Baseline Characteristics and Dialysis Treatments
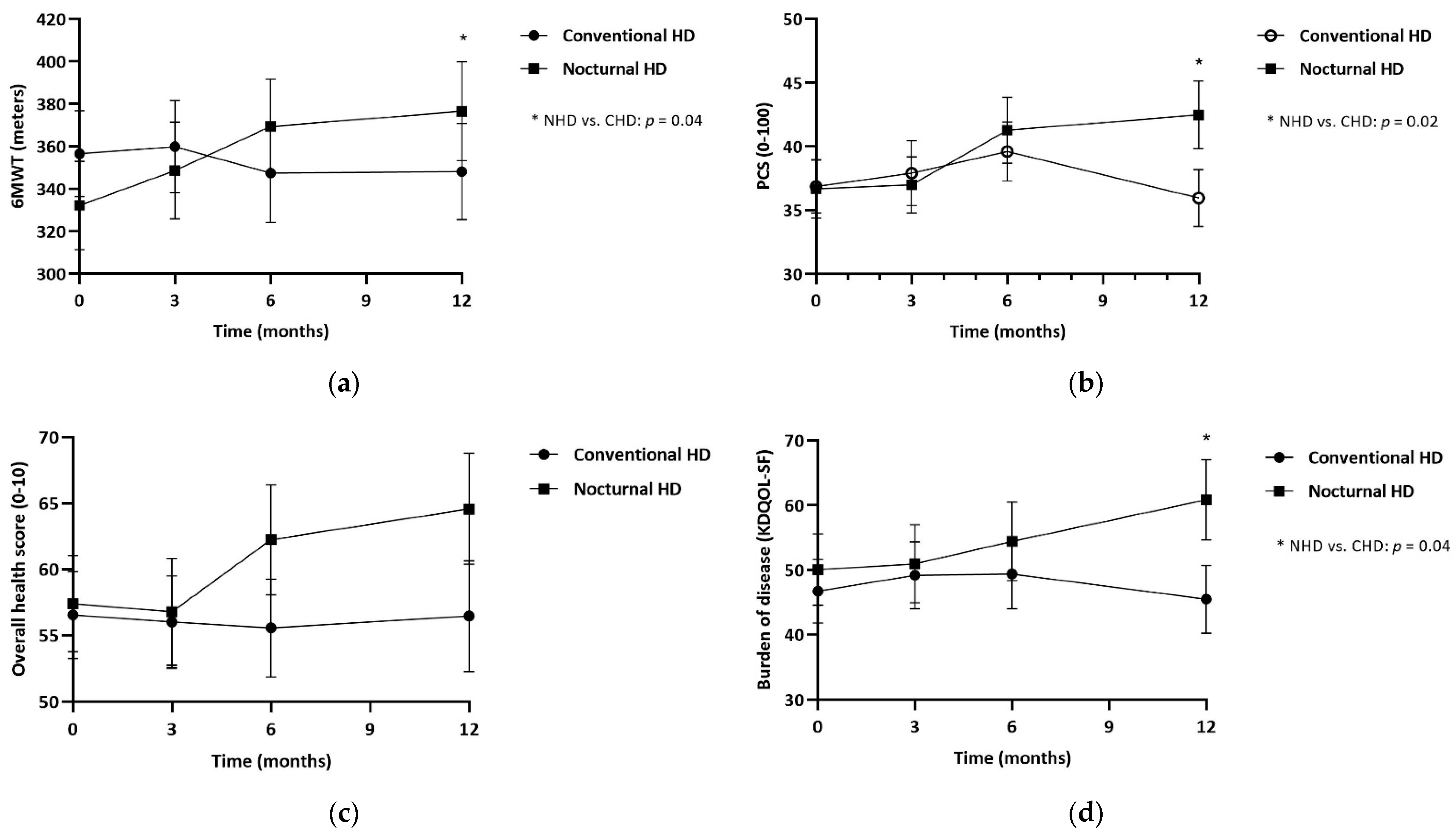
3.3. Physical Performance: Differences between NHD and CHD
3.4. Protein-Energy Wasting: Differences between NHD and CHD
3.5. QOL and Sleep: Differences between NHD and CHD
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sarnak, M.J.; Levey, A.S.; Schoolwerth, A.C.; Coresh, J.; Culleton, B.; Hamm, L.L.; McCullough, P.A.; Kasiske, B.L.; Kelepouris, E.; Klag, M.J.; et al. Kidney disease as a risk factor for development of cardiovascular disease: A statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation 2003, 108, 2154–2169. [Google Scholar] [CrossRef] [PubMed]
- Parfrey, P.S.; Foley, R.N. The clinical epidemiology of cardiac disease in chronic renal failure. J. Am. Soc. Nephrol. 1999, 10, 1606–1615. [Google Scholar] [CrossRef] [PubMed]
- Goodkin, D.A.; Young, E.W.; Kurokawa, K.; Prutz, K.G.; Levin, N.W. Mortality among hemodialysis patients in Europe, Japan, and the United States: Case-mix effects. Am. J. Kidney Dis. 2004, 44 (Suppl S2), 16–21. [Google Scholar] [CrossRef] [PubMed]
- Fukuhara, S.; Lopes, A.A.; Bragg-Gresham, J.L.; Kurokawa, K.; Mapes, D.L.; Akizawa, T.; Bommer, J.; Canaud, B.J.; Port, F.K.; Held, P.J. Health-related quality of life among dialysis patients on three continents: The Dialysis Outcomes and Practice Patterns Study. Kidney Int. 2003, 64, 1903–1910. [Google Scholar] [CrossRef]
- Kaysen, G.A.; Larive, B.; Painter, P.; Craig, A.; Lindsay, R.M.; Rocco, M.V.; Daugirdas, J.T.; Schulman, G.; Chertow, G.M.; FHN Trial Group. Baseline physical performance, health, and functioning of participants in the Frequent Hemodialysis Network (FHN) trial. Am. J. Kidney Dis. 2011, 57, 101–112. [Google Scholar] [CrossRef]
- Johansen, K.L.; Chertow, G.M.; Ng, A.V.; Mulligan, K.; Carey, S.; Schoenfeld, P.Y.; Kent-Braun, J.A. Physical activity levels in patients on hemodialysis and healthy sedentary controls. Kidney Int. 2000, 57, 2564–2570. [Google Scholar] [CrossRef]
- Avesani, C.M.; Trolonge, S.; Deléaval, P.; Baria, F.; Mafra, D.; Faxén-Irving, G.; Chauveau, P.; Teta, D.; Kamimura, M.A.; Cuppari, L.; et al. Physical activity and energy expenditure in haemodialysis patients: An international survey. Nephrol. Dial. Transpl. 2012, 27, 2430–2434. [Google Scholar] [CrossRef]
- Lopes, A.A.; Lantz, B.; Morgenstern, H.; Wang, M.; Bieber, B.A.; Gillespie, B.W.; Li, Y.; Painter, P.; Jacobson, S.H.; Rayner, H.C.; et al. Associations of self-reported physical activity types and levels with quality of life, depression symptoms, and mortality in hemodialysis patients: The DOPPS. Clin. J. Am. Soc. Nephrol. 2014, 9, 1702–1712. [Google Scholar] [CrossRef]
- Kutner, N.G.; Zhang, R.; Huang, Y.; Painter, P. Gait Speed and Mortality, Hospitalization, and Functional Status Change Among Hemodialysis Patients: A US Renal Data System Special Study. Am. J. Kidney Dis. 2015, 66, 297–304. [Google Scholar] [CrossRef]
- Painter, P.; Roshanravan, B. The association of physical activity and physical function with clinical outcomes in adults with chronic kidney disease. Curr. Opin. Nephrol. Hypertens. 2013, 22, 615–623. [Google Scholar] [CrossRef]
- Chazot, C.; Ok, E.; Lacson, E., Jr.; Kerr, P.G.; Jean, G.; Misra, M. Thrice-weekly nocturnal hemodialysis: The overlooked alternative to improve patient outcomes. Nephrol. Dial. Transpl. 2013, 28, 2447–2455. [Google Scholar] [CrossRef] [PubMed]
- Lacson, E.; Xu, J.; Suri, R.S.; Nesrallah, G.; Lindsay, R.; Garg, A.X.; Lester, K.; Ofsthun, N.; Lazarus, M.; Hakim, R.M. Survival with three-times weekly in-center nocturnal versus conventional hemodialysis. J. Am. Soc. Nephrol. 2012, 23, 687–695. [Google Scholar] [CrossRef] [PubMed]
- Laurent, G.; Charra, B. The results of an 8 h thrice weekly haemodialysis schedule. Nephrol. Dial. Transpl. 1998, 12, 125–131. [Google Scholar] [CrossRef]
- Ok, E.; Duman, S.; Asci, G.; Tumuklu, M.; Onen Sertoz, O.; Kayikcioglu, M.; Toz, H.; Adam, S.M.; Yilmaz, M.; Tonbul, H.Z.; et al. Comparison of 4- and 8-h dialysis sessions in thrice-weekly in-centre haemodialysis: A prospective, case-controlled study. Nephrol. Dial. Transpl. 2011, 26, 1287–1296. [Google Scholar] [CrossRef]
- Culleton, B.F.W.M.; Klarenbach, S.W.; Mortis, G.; Scott-Douglas, N.; Quinn, R.R. Effect of frequent nocturnal hemodialysis vs conventional hemodialysis on left ventricular mass and quality of life. JAMA 2007, 298, 1291–1299. [Google Scholar] [CrossRef] [PubMed]
- Rocco, M.V.; Lockridge, R.S.; Beck, G.J.; Eggers, P.W.; Gassman, J.J.; Greene, T.; Larive, B.; Chan, C.T.; Chertow, G.M.; Copland, M.; et al. The effects of frequent nocturnal home hemodialysis: The Frequent Hemodialysis Network Nocturnal Trial. Kidney Int. 2011, 80, 1080–1091. [Google Scholar] [CrossRef] [PubMed]
- Schorr, M.; Manns, B.J.; Culleton, B.; Walsh, M.; Klarenbach, S.; Tonelli, M.; Sauve, L.; Chin, R.; Barnieh, L.; Hemmelgarn, B.R. The effect of nocturnal and conventional hemodialysis on markers of nutritional status: Results from a randomized trial. J. Ren. Nutr. 2011, 21, 271–276. [Google Scholar] [CrossRef]
- Jansz, T.T.; Özyilmaz, A.; Grooteman, M.P.C.; Hoekstra, T.; Romijn, M.; Blankestijn, P.J.; Bots, M.L.; Van Jaarsveld, B.C. Long-term clinical parameters after switching to nocturnal haemodialysis: A Dutch propensity-score-matched cohort study comparing patients on nocturnal haemodialysis with patients on three-times-a-week haemodialysis/haemodiafiltration. BMJ Open 2018, 8, e019900. [Google Scholar] [CrossRef]
- Jansz, T.T.; Noordzij, M.; Kramer, A.; Laruelle, E.; Couchoud, C.; Collart, F.; Cases, A.; Arici, M.; Helve, J.; Waldum-Grevbo, B.; et al. Survival of patients treated with extended-hours haemodialysis in Europe: An analysis of the ERA-EDTA Registry. Nephrol. Dial. Transpl. 2020, 35, 488–495. [Google Scholar] [CrossRef]
- Graham-Brown, M.P.; Churchward, D.R.; Smith, A.C.; Baines, R.J.; Burton, J.O. A 4-month programme of in-centre nocturnal haemodialysis was associated with improvements in patient outcomes. Clin. Kidney J. 2015, 8, 789–795. [Google Scholar] [CrossRef]
- Dumaine, C.S.; Ravani, P.; Parmar, M.K.; Leung, K.C.W.; MacRae, J.M. In-center nocturnal hemodialysis improves health-related quality of life for patients with end-stage renal disease. J. Nephrol. 2022, 35, 245–253. [Google Scholar] [CrossRef] [PubMed]
- Dam, M.; Weijs, P.J.M.; van Ittersum, F.J.; van Jaarsveld, B.C. Physical performance in patients treated with nocturnal hemodialysis—A systematic review of the evidence. BMC Nephrol. 2019, 20, 317. [Google Scholar] [CrossRef] [PubMed]
- Hall, Y.N.; Larive, B.; Painter, P.; Kaysen, G.A.; Lindsay, R.M.; Nissenson, A.R.; Unruh, M.L.; Rocco, M.V.; Chertow, G.M.; the Frequent Hemodialysis Network Trial Group. Effects of six versus three times per week hemodialysis on physical performance, health, and functioning: Frequent Hemodialysis Network (FHN) randomized trials. Clin. J. Am. Soc. Nephrol. 2012, 7, 782–794. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.T.; Notarius, C.F.; Merlocco, A.C.; Floras, J.S. Improvement in exercise duration and capacity after conversion to nocturnal home haemodialysis. Nephrol. Dial. Transpl. 2007, 22, 3285–3291. [Google Scholar] [CrossRef] [PubMed]
- Van Eps, C.L.; Jeffries, J.K.; Johnson, D.W.; Campbell, S.B.; Isbel, N.M.; Mudge, D.W.; Hawley, C.M. Quality of life and alternate nightly nocturnal home hemodialysis. Hemodial. Int. 2010, 14, 29–38. [Google Scholar] [CrossRef]
- Lockridge, R.S., Jr.; Spencer, M.; Craft, V.; Pipkin, M.; Campbell, D.; McPhatter, L.; Albert, J.; Anderson, H.; Jennings, F.; Barger, T. Nightly home hemodialysis: Five and one-half years of experience in Lynchburg, Virginia. Hemodial. Int. 2004, 8, 61–69. [Google Scholar] [CrossRef]
- Carrero, J.J.; Stenvinkel, P.; Cuppari, L.; Ikizler, T.A.; Kalantar-Zadeh, K.; Kaysen, G.; Mitch, W.E.; Price, S.R.; Wanner, C.; Wang, A.Y.; et al. Etiology of the protein-energy wasting syndrome in chronic kidney disease: A consensus statement from the International Society of Renal Nutrition and Metabolism (ISRNM). J. Ren. Nutr. 2013, 23, 77–90. [Google Scholar] [CrossRef]
- Fouque, D.; Kalantar-Zadeh, K.; Kopple, J.; Cano, N.; Chauveau, P.; Cuppari, L.; Franch, H.; Guarnieri, G.; Ikizler, T.A.; Kaysen, G.; et al. A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int. 2008, 73, 391–398. [Google Scholar] [CrossRef]
- Kim, J.C.; Kalantar-Zadeh, K.; Kopple, J.D. Frailty and protein-energy wasting in elderly patients with end stage kidney disease. J. Am. Soc. Nephrol. 2013, 24, 337–351. [Google Scholar] [CrossRef]
- Kaysen, G.A.; Greene, T.; Larive, B.; Mehta, R.L.; Lindsay, R.M.; Depner, T.A.; Hall, Y.N.; Daugirdas, J.T.; Chertow, G.M. The effect of frequent hemodialysis on nutrition and body composition: Frequent Hemodialysis Network Trial. Kidney Int. 2012, 82, 90–99. [Google Scholar] [CrossRef]
- Sikkes, M.E.; Kooistra, M.P.; Weijs, P.J. Improved nutrition after conversion to nocturnal home hemodialysis. J. Ren. Nutr. 2009, 19, 494–499. [Google Scholar] [CrossRef] [PubMed]
- Demirci, C.; Ozkahya, M.; Demirci, M.S.; Asci, G.; Kose, T.; Colak, T.; Duman, S.; Toz, H.; Ergin, P.; Adam, S.M.; et al. Effects of three times weekly eight-hour nocturnal hemodialysis on volume and nutritional status. Am. J. Nephrol. 2013, 37, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Ipema, K.J.; van der Schans, C.P.; Vonk, N.; de Vries, J.M.; Westerhuis, R.; Duym, E.; Franssen, C.F. A difference between day and night: Protein intake improves after the transition from conventional to frequent nocturnal home hemodialysis. J. Ren. Nutr. 2012, 22, 365–372. [Google Scholar] [CrossRef]
- David, S.; Kumpers, P.; Eisenbach, G.M.; Haller, H.; Kielstein, J.T. Prospective evaluation of an in-centre conversion from conventional haemodialysis to an intensified nocturnal strategy. Nephrol. Dial. Transpl. 2009, 24, 2232–2240. [Google Scholar] [CrossRef]
- Dam, M.; Neelemaat, F.; Struijk-Wielinga, T.; Weijs, P.J.; van Jaarsveld, B.C. Physical performance and protein-energy wasting in patients treated with nocturnal haemodialysis compared to conventional haemodialysis: Protocol of the DiapriFIT study. BMC Nephrol. 2017, 18, 144. [Google Scholar] [CrossRef]
- Guralnik, J.M.F.L.; Simonsick, E.M.; Salive, M.E.; Wallace, R.B. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. NEJM 1995, 332, 556–561. [Google Scholar] [CrossRef] [PubMed]
- Society, A.T. ATS Statement: Guidelines for the Six-Minute Walk Test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar]
- Voorrips, L.E.; Ravelli, A.C.; Dongelmans, P.C.; Deurenberg, P.A.U.L.; Van Staveren, W.A. A physical activity questionnaire for the elderly. Med. Sci. Sports Exerc. 1991, 23, 974–979. [Google Scholar] [CrossRef]
- Clase, C.M.; St Pierre, M.W.; Churchill, D.N. Conversion between bromcresol green- and bromcresol purple-measured albumin in renal disease. Nephrol. Dial. Transpl. 2001, 16, 1925–1929. [Google Scholar] [CrossRef][Green Version]
- Hays, R.D.; Kallich, J.D.; Mapes, D.L.; Coons, S.J.; Amin, N.; Carter, W.B.; Kamberg, C. Kidney Disease Quality of Life Short Form (KDQOL-SF™), Version 1.3: A Manual for Use and Scoring; RAND: Santa Monica, CA, USA, 1997; pp. 1–39. [Google Scholar]
- Lattanzio, F.; Corsonello, A.; Abbatecola, A.M.; Volpato, S.; Pedone, C.; Pranno, L.; Laino, I.; Garasto, S.; Corica, F.; Passarino, G.; et al. Relationship between renal function and physical performance in elderly hospitalized patients. Rejuvenation Res. 2012, 15, 545–552. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Ferrucci, L.; Pieper, C.F.; Leveille, S.G.; Markides, K.S.; Ostir, G.V.; Studenski, S.; Berkman, L.F.; Wallace, R.B. Lower extremity function and subsequent disability: Consistency across studies, predictive models, and value of gait speed alone compared with the Short Physical Performance Battery. J. Gerontol. Med. Sci. 2000, 55, 221–231. [Google Scholar] [CrossRef] [PubMed]
- Painter, P.; Marcus, R.L. Assessing physical function and physical activity in patients with CKD. Clin. J. Am. Soc. Nephrol. 2013, 8, 861–872. [Google Scholar] [CrossRef] [PubMed]
- Fong, E.; Bargman, J.M.; Chan, C.T. Cross-sectional comparison of quality of life and illness intrusiveness in patients who are treated with nocturnal home hemodialysis versus peritoneal dialysis. Clin. J. Am. Soc. Nephrol. 2007, 2, 1195–1200. [Google Scholar] [CrossRef] [PubMed]
- Steiber, A.; Leon, J.B.; Secker, D.; McCarthy, M.; McCann, L.; Serra, M.; Sehgal, A.R.; Kalantar-Zadeh, K. Multicenter study of the validity and reliability of subjective global assessment in the hemodialysis population. J. Ren. Nutr. 2007, 17, 336–342. [Google Scholar] [CrossRef] [PubMed]
- de Mutsert, R.; Grootendorst, D.C.; Boeschoten, E.W.; Brandts, H.; van Manen, J.G.; Krediet, R.T.; Dekker, F.W.; Netherlands Cooperative Study on the Adequacy of Dialysis-2 Study Group. Subjective global assessment of nutritional status is strongly associated with mortality in chronic dialysis patients. Am. J. Clin. Nutr. 2009, 89, 787–793. [Google Scholar] [PubMed]
- Ipema, K.J.; Westerhuis, R.; van der Schans, C.P.; de Jong, P.E.; Gaillard, C.A.; Krijnen, W.P.; Slart, R.H.; Franssen, C.F. Effect of nocturnal haemodialysis on body composition. Nephron. Clin. Pract. 2014, 128, 171–177. [Google Scholar] [CrossRef]
- Spanner, E.; Suri, R.; Heidenheim, A.P.; Lindsay, R.M. The impact of quotidian hemodialysis on nutrition. Am. J. Kidney Dis. 2003, 42, 30–35. [Google Scholar] [CrossRef]
- Ekramzadeh, M.; Santoro, D.; Kopple, J.D. The Effect of Nutrition and Exercise on Body Composition, Exercise Capacity, and Physical Functioning in Advanced CKD Patients. Nutrients 2022, 14, 2129. [Google Scholar] [CrossRef]

| Characteristics | CHD (n = 33) | NHD (n = 32) | p-Value |
|---|---|---|---|
| Male, n (%) | 16 (49%) | 18 (56%) | 0.4 |
| Age, years | 60 ± 13.9 | 50 ± 15.3 | 0.01 |
| Race, n (%) White Black Asian Other/mixed | 21 (63.6%) 3 (9.1%) 3 (9.1%) 6 (18.2%) | 19 (59%) 8 (25%) 1 (3%) 4 (12.5%) | 0.3 |
| Causes of End-Stage Kidney Disease, n (%) Diabetes mellitus Hypertension Polycystic kidney disease Other | 8 (24%) 6 (18%) 1 (3%) 18 (55%) | 5 (16%) 6 (19%) 3 (9%) 18 (56%) | 0.6 |
| Charlson comorbidity index, n (%) 2 (no comorbidity except ESKD) 3–4 (intermediate comorbidity) ≥5 (high comorbidity) | 7 (21.2%) 14 (42.5%) 12 (36.4%) | 11 (34.4%) 11 (34.4%) 10 (31.3%) | 0.5 |
| Body weight, kg | 77.4 ± 18.6 | 81.8 ± 20.3 | 0.4 |
| Body Mass Index, kg/m2 | 27 ± 6.4 | 28 ± 6.7 | 0.5 |
| Systolic blood pressure, mm Hg | 134 ± 24.7 | 141 ± 21.9 | 0.3 |
| Diastolic blood pressure, mm Hg | 72 ± 12.4 | 79 ± 12.3 | 0.02 |
| History of renal replacement therapy (RRT vintage), months | 40 (15–123) | 21 (9–75) | 0.1 |
| Previous renal transplant, n (%) | 10 (30.3%) | 9 (28.1%) | 0.9 |
| Anuria, n (%) | 16 (48.5%) | 10 (31.3%) | 0.3 |
| Characteristics | CHD (n = 33) | NHD (n = 32) | p-Value |
|---|---|---|---|
| Dialysis frequency, times/week | |||
| Baseline | 2.8 ± 0.5 | 2.9 ± 0.3 | 0.3 |
| 6 months | 2.9 ± 0.5 | 2.9 ± 0.3 | 1 |
| 12 months | 2.9 ± 0.4 | 2.8 ± 0.4 | 0.8 |
| Dialysis duration per session, hours | |||
| Baseline | 3.9 ± 0.4 | 3.9 ± 0.3 | 0.5 |
| 6 months | 3.9 ± 0.4 | 8.0 ± 0.2 | <0.001 |
| 12 months | 3.9 ± 0.5 | 7.9 ± 0.3 | <0.001 |
| Dialysis dose (standardized Kt/V week) | |||
| Baseline | 5.9 ± 1.3 | 6.0 ± 1.0 | 0.8 |
| 6 months | 6.5 ± 1.1 | 7.6 ± 0.9 | <0.001 |
| 12 months | 6.8 ± 1.2 | 7.9 ± 0.6 | <0.001 |
| Physical Performance | ||||||
|---|---|---|---|---|---|---|
| Baseline | 3 Months | 6 Months | 12 Months | Linear Mixed Models with 1-Year Treatment Effect of NHD Compared to CHD * | ||
| Mean (SE) a | Mean (SE) a | Mean (SE) a | Mean (SE) a | Effect (95% CI) | p-Value | |
| Short physical performance battery, scale, 1–12 CHD NHD | 9.53 (0.29) 9.59 (0.31) | 9.42 (0.31) 9.78 (0.34) | 9.42 (0.32) 9.57 (0.34) | 9.66 (0.33) 10.1 (0.35) | 0.24 (−0.51 to 0.99) | 0.5 |
| 6-minute walk test, meters CHD NHD | 356 (20.3) 332 (20.9) | 360 (21.8) 349 (22.8) | 347 (23.3) 369 (22.4) | 348 (22.7) 377 (23.4) | 54.3 (7.78 to 100.8) | 0.02 |
| Physical activity monitor, min/day CHD NHD | 63.2 (8.28) 78.7 (8.53) | 51.2 (10.1) 81.9 (10.9) | 37.7 (11.7) 76.6 (10.6) | 47.1 (10.3) 71.4 (11.2) | 14.7 (−14.6 to 44.2) | 0.3 |
| Handgrip muscle strength, kg CHD NHD | 30 (1.38) 29 (1.47) | 30 (1.41) 30 (1.54) | 31 (1.44) 29 (1.54) | 30 (1.44) 30 (1.57) | 1.35 (−0.98 to 3.68) | 0.3 |
| Physical component score, score 0–100 CHD NHD | 37 (2.07) 37 (2.31) | 38 (2.55) 37 (2.20) | 40 (2.31) 41 (2.58) | 36 (2.24) 42 (2.65) | 5.61 (−0.51 to 10.7) | 0.03 |
| LAPAQ activity questionnaire, min/day CHD NHD | 122 (15.4) 123 (16.2) | 115 (15.9) 138 (18.1) | 103 (17.5) 117 (18.2) | 102 (17.2) 112 (19.5) | 12.6 (−33.9 to 59.2) | 0.6 |
| Protein-Energy Wasting | ||||||
|---|---|---|---|---|---|---|
| Baseline | 3 Months | 6 Months | 12 Months | Linear Mixed Models with 1-Year Treatment Effect between NHD and CHD * | ||
| Mean (SE) a | Mean (SE) a | Mean (SE) a | Mean (SE) a | Effect (95% CI) | p-Value | |
| Protein intake, g/day CHD NHD | 70.4 (3.94) 76.4 (4.39) | - | - | 69.7 (4.51) 76.0 (4.99) | 0.33 (−12.9 to 13.6) | 1.0 |
| Protein, g/kg CHD NHD | 0.94 (0.07) 1.00 (0.08) | 0.98 (0.08) 1.02 (0.08) | −0.08 (−0.03 to 0.10) | 0.4 | ||
| Phosphorus intake, mg/day CHD NHD | 1159 (102) 1367 (113) | - | - | 1267 (123) 1334 (135) | −142 (−577 to 292) | 0.5 |
| Energy intake, kcal/day CHD NHD | 1758 (106) 1870 (117) | - | - | 1637 (136) 1916 (123) | 167 (−222 to 557) | 0.4 |
| Body weight, kg CHD NHD | 77.1 (3.30) 82.0 (3.53) | 77.1 (3.31) 80.8 (3.55) | 76.8 (3.32) 80.5 (3.55) | 76.4 (3.31) 79.9 (3.56) | −1.39 (−3.14 to 0.35) | 0.1 |
| Body mass index, kg/m2 CHD NHD | 26.7 (1.11) 28.4 (1.18) | 26.7 (1.11) 28.0 (1.19) | 26.6 (1.11) 27.9 (1.19) | 26.5 (1.19) 27.7 (1.12) | −0.46 (−1.08 to 0.13) | 0.1 |
| DXA- Appendicular skeletal muscle mass, kg CHD NHD | 21.2 (1.05) 22.3 (0.95) | - | - | 20.1 (1.08) 21.8 (0.99) | 0.53 (−0.64 to 1.71) | 0.3 |
| DXA- Fat mass, % CHD NHD | 34.4 (1.40) 34.4 (1.35) | - | - | 35.8 (1.51) 35.4 (1.41) | −0.37 (−2.49 to 1.74) | 0.7 |
| BIS- Lean tissue mass, kg CHD NHD | 39.3 (1.40) 37.3 (1.40) | 38.3 (1.45) 35.4 (1.51) | 38.8 (1.53) 36.9 (1.51) | 37.2 (1.57) 36.9 (1.60) | 1.29 (−1.98 to 4.58) | 0.4 |
| Appetite, VAS 0–10 cm CHD NHD | 7.5 (0.37) 7.3 (0.39) | 7.3 (0.38) 7.5 (0.44) | 7.1 (0.41) 7.7 (0.44) | 7.6 (0.42) 8.0 (0.47) | 0.78 (−0.33 to 1.90) | 0.2 |
| Subjective global assessment, score 1–7 CHD NHD | 5.8 (0.13) 5.6 (0.14) | 5.7 (0.13) 6.1 (0.15) | 5.7 (0.15) 6.2 (0.14) | 5.9 (0.16) 6.3 (0.14) | 0.71 (0.36 to 1.05) | <0.001 |
| Mid-upper arm muscle circumference, cm CHD NHD | 25.4 (0.59) 25.1 (0.63) | 25.4 (0.59) 25.8 (0.66) | 25.3 (0.62) 25.4 (0.66) | 25.1 (0.62) 25.1 (0.67) | 0.46 (−0.59 to 1.52) | 0.4 |
| Albumin, g/L CHD NHD | 40.3 (0.52) 40.2 (0.56) | 40.4 (0.59) 39.9 (0.59) | 39.8 (0.59) 41.3 (0.54) | 40.2 (0.55) 40.7 (0.61) | 1.04 (−0.07 to 2.14) | 0.06 |
| C-reactive protein, mg/L CHD NHD | 8.74 (2.03) 7.77 (2.32) | 9.03 (2.13) 7.62 (2.47) | 11.6 (2.27) 4.99 (2.44) | 7.63 (2.32) 7.53 (2.73) | −1.66 (−8.35 to 5.03) | 0.6 |
| Quality of Life | ||||||
|---|---|---|---|---|---|---|
| Baseline | 3 Months | 6 Months | 12 Months | Linear Mixed Models with 1-Year Treatment Effect between NHD and CHD * | ||
| Mean (SE) a | Mean (SE) a | Mean (SE) a | Mean (SE) a | Effect (95% CI) | p-Value | |
| Mental component summary score, scale 0–100 CHD NHD | 53 (1.96) 53 (2.16) | 54 (2.18) 51 (2.57) | 51 (2.37) 50 (2.62) | 51 (2.25) 50 (2.73) | −1.65 (−8.23 to 4.93) | 0.6 |
| Overall health score, scale 0–10 CHD NHD | 56.5 (3.30) 57.4 (3.65) | 56.0 (3.50) 56.8 (4.05) | 55.6 (3.68) 62.3 (4.15) | 56.5 (3.60) 64.6 (4.21) | 7.10 (−1.08 to 15.3) | 0.08 |
| Sleep quality, score 0–9 CHD NHD | 2.22 (0.32) 2.09 (0.33) | 1.52 (0.33) 2.15 (0.37) | 1.54 (0.54) 2.04 (0.37) | 1.66 (0.35) 1.33 (0.41) | 0.15 (−0.82 to 1.11) | 0.8 |
| Causes of sleep disturbances, score 0–6 CHD NHD | 0.63 (0.19) 0.85 (0.20) | 0.96 (0.19) 0.90 (0.23) | 0.88 (0.22) 0.71 (0.23) | 0.72 (0.22) 0.56 (0.53) | −0.41 (−1.05 to 0.23) | 0.2 |
| Effect of sleeping disturbance on day-time functioning, score 0–9 CHD NHD | 2.26 (0.35) 2.79 (0.37) | 2.38 (0.43) 3.92 (0.36) | 2.72 (0.39) 3.02 (0.42) | 2.95 (0.39) 3.11 (0.45) | −0.32 (−1.39 to 0.76) | 0.6 |
| Restless legs/anxiety during sleep, VAS 0–10 cm CHD NHD | 2.62 (0.45) 2.07 (0.47) | 2.16 (0.47) 2.05 (0.55) | 1.49 (0.52) 2.36 (0.55) | 1.52 (0.52) 1.85 (0.62) | 1.19 (−0.43 to 2.83) | 0.2 |
| Fatigue after sleep, VAS 0–10 cm CHD NHD | 4.47 (0.78) 5.08 (0.82) | 4.66 (0.95) 5.03 (0.82) | 6.05 (0.91) 4.77 (0.95) | 5.00 (1.06) 3.63 (0.91) | −2.03 (−4.88 to 0.83) | 0.2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dam, M.; Weijs, P.J.M.; van Ittersum, F.J.; Hoekstra, T.; Douma, C.E.; van Jaarsveld, B.C. Nocturnal Hemodialysis Leads to Improvement in Physical Performance in Comparison with Conventional Hemodialysis. Nutrients 2023, 15, 168. https://doi.org/10.3390/nu15010168
Dam M, Weijs PJM, van Ittersum FJ, Hoekstra T, Douma CE, van Jaarsveld BC. Nocturnal Hemodialysis Leads to Improvement in Physical Performance in Comparison with Conventional Hemodialysis. Nutrients. 2023; 15(1):168. https://doi.org/10.3390/nu15010168
Chicago/Turabian StyleDam, Manouk, Peter J. M. Weijs, Frans J. van Ittersum, Tiny Hoekstra, Caroline E. Douma, and Brigit C. van Jaarsveld. 2023. "Nocturnal Hemodialysis Leads to Improvement in Physical Performance in Comparison with Conventional Hemodialysis" Nutrients 15, no. 1: 168. https://doi.org/10.3390/nu15010168
APA StyleDam, M., Weijs, P. J. M., van Ittersum, F. J., Hoekstra, T., Douma, C. E., & van Jaarsveld, B. C. (2023). Nocturnal Hemodialysis Leads to Improvement in Physical Performance in Comparison with Conventional Hemodialysis. Nutrients, 15(1), 168. https://doi.org/10.3390/nu15010168





