Evaluation of the Effects of Skin-to-Skin Contact on Newborn Sucking, and Breastfeeding Abilities: A Quasi-Experimental Study Design
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Research Tools and Outcome Definitions
2.3. Training of Nursing Staff
2.4. Statistical Analysis
3. Results
3.1. Clinical Characteristics of Study Participants
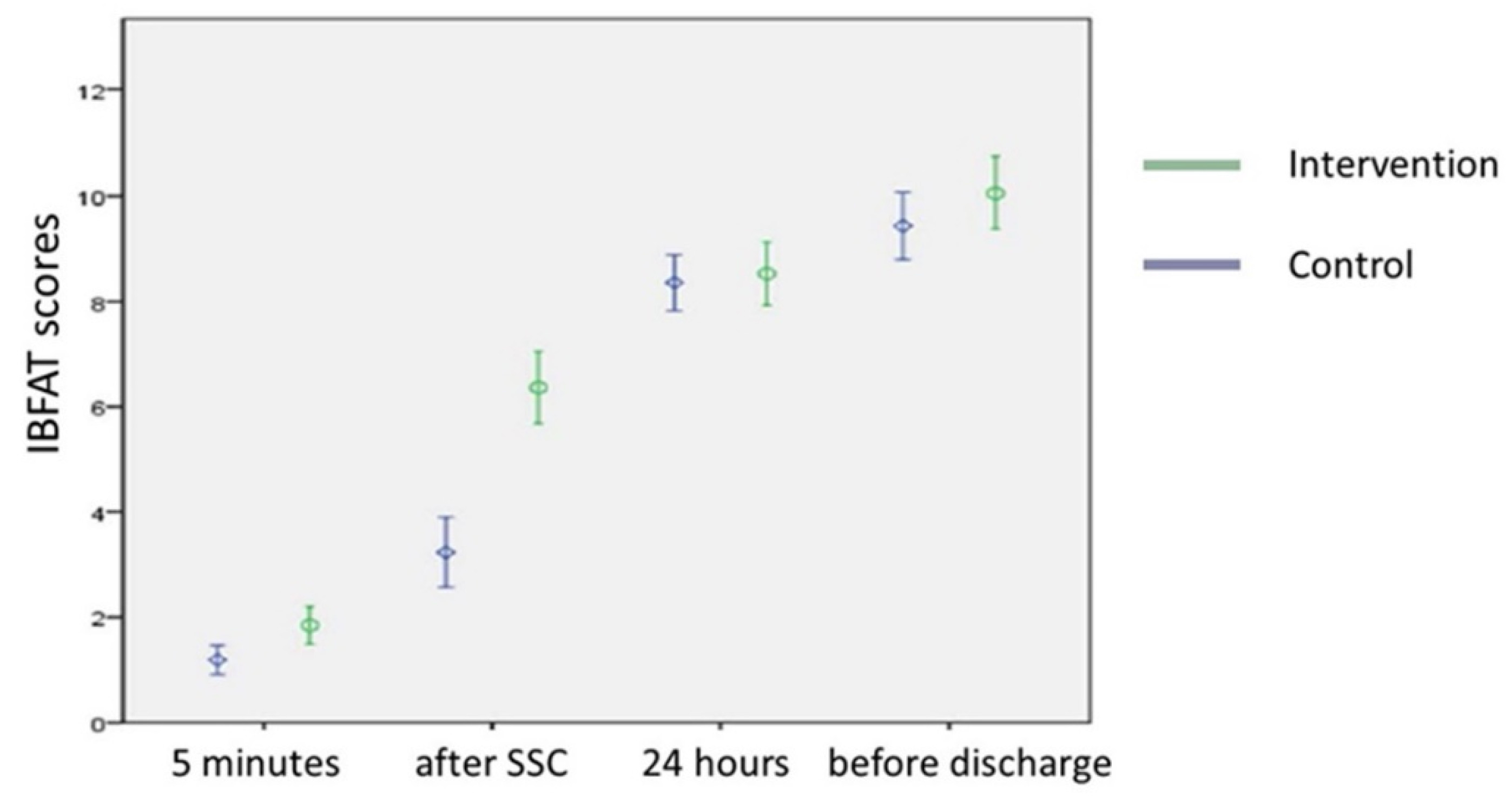
3.2. Analysis of the Effect between the Intervention and Control Groups on Newborn Breastfeeding Ability
3.3. Analysis of the Effect between the Intervention and Control Groups on the Self-Efficacy of Breastfeeding
4. Discussion
4.1. Main Findings
4.2. Effect of the SSC Intervention on Newborn Breastfeeding Ability
4.3. Effect of the SSC Intervention on Postpartum Feeding
4.4. Effect of the SSC Intervention on Breastfeeding Self-Efficacy
4.5. Potential Explanatory Mechanisms for the Benefits from SSC
4.6. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hubbard, J.M.; Gattman, K.R. Parent-infant skin-to-skin contact following birth: History, benefits, and challenges. Neonatal Netw. 2017, 36, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Khan, S.M.; Carvajal-Aguirre, L.; Brodish, P.; Amouzou, A.; Moran, A. The importance of skin-to-skin contact for early initiation of breastfeeding in Nigeria and Bangladesh. J. Glob. Health 2017, 7, 020505. [Google Scholar] [CrossRef]
- Srivastava, S.; Gupta, A.; Bhatnagar, A.; Dutta, S. Effect of very early skin to skin contact on success at breastfeeding and preventing early hypothermia in neonates. Indian J. Public Health 2014, 58, 22–26. [Google Scholar] [CrossRef]
- Arya, S.; Naburi, H.; Kawaza, K.; Newton, S.; Anyabolu, C.H.; Bergman, N.; Rao, S.P.N.; Mittal, P.; Assenga, E.; Gadama, L.; et al. Immediate “Kangaroo Mother Care” and survival of infants with low birth weight. N. Engl. J. Med. 2021, 384, 2028–2038. [Google Scholar] [CrossRef]
- Waits, A.; Guo, C.Y.; Chien, L.Y. Evaluation of factors contributing to the decline in exclusive breastfeeding at 6 months postpartum: The 2011-2016 national surveys in Taiwan. Birth 2018, 45, 184–192. [Google Scholar] [CrossRef] [PubMed]
- Agudelo, S.; Díaz, D.; Maldonado, M.J.; Acuña, E.; Mainero, D.; Pérez, O.; Pérez, L.; Molina, C. Effect of skin-to-skin contact at birth on early neonatal hospitalization. Early Hum. Dev. 2020, 144, 105020. [Google Scholar] [CrossRef]
- Li, Z.; Mannava, P.; Murray, J.C.S.; Sobel, H.L.; Jatobatu, A.; Calibo, A.; Tsevelmaa, B.; Saysanasongkham, B.; Ogaoga, D.; Waramin, E.J.; et al. Association between early essential newborn care and breastfeeding outcomes in eight countries in Asia and the Pacific: A cross-sectional observational -study. BMJ Glob. Health 2020, 5, e002581. [Google Scholar] [CrossRef]
- World Health Organization. Guideline: Protecting, Promoting and Supporting Breastfeeding in Facilities Providing Maternity and Newborn Services; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Abdulghani, N.; Edvardsson, K.; Amir, L.H. Worldwide prevalence of mother-infant skin-to-skin contact after vaginal birth: A systematic review. PLoS ONE 2018, 13, e0205696. [Google Scholar] [CrossRef]
- Mahmood, I.; Jamal, M.; Khan, N. Effect of mother-infant early skin-to-skin contact on breastfeeding status: A randomized controlled trial. J. Coll. Physicians Surg. Pak. 2011, 21, 601–605. [Google Scholar] [CrossRef] [PubMed]
- Gallegos, D.; Parkinson, J.; Duane, S.; Domegan, C.; Jansen, E.; Russell-Bennett, R. Understanding breastfeeding behaviours: A cross-sectional analysis of associated factors in Ireland, the United Kingdom and Australia. Int. Breastfeed. J. 2020, 15, 103. [Google Scholar] [CrossRef]
- Sharma, A. Efficacy of early skin-to-skin contact on the rate of exclusive breastfeeding in term neonates: A randomized controlled trial. Afr. Health Sci. 2016, 16, 790–797. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agudelo, S.I.; Molina, C.F.; Gamboa, O.A.; Acuña, E. Comparison of the Effects of Different Skin-to-Skin Contact Onset Times on Breastfeeding Behavior. Breastfeed. Med. 2021, 16, 971–977. [Google Scholar] [CrossRef]
- Des Jarlais, D.C.; Lyles, C.; Crepaz, N.; Group, T. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: The TREND statement. Am. J. Public Health 2004, 94, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Safari, K.; Saeed, A.A.; Hasan, S.S.; Moghaddam-Banaem, L. The effect of mother and newborn early skin-to-skin contact on initiation of breastfeeding, newborn temperature and duration of third stage of labor. Int. Breastfeed. J. 2018, 13, 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zangmo, K.; Wangmo, D.; Tobgay, T.; Gurung, M.S. Breastfeeding problems: An analysis of secondary data from Lactation Management Unit at the national referral hospital in Bhutan from 2014 to 2016. Bhutan Health J. 2018, 4, 8–12. [Google Scholar] [CrossRef]
- Matthews, M.K. Developing an instrument to assess infant breastfeeding behaviour in the early neonatal period. Midwifery 1988, 4, 154–165. [Google Scholar] [CrossRef]
- Dennis, C.L.; Faux, S. Development and psychometric testing of the breastfeeding self-efficacy scale. Res. Nurs. Health 1999, 22, 399–409. [Google Scholar] [CrossRef]
- Wu, Y.H.; Ho, Y.J.; Han, J.P.; Chen, S.Y. The Influence of Breastfeeding Self-Efficacy and Breastfeeding Intention on Breastfeeding Behavior in Postpartum Women. Hu Li Za Zhi 2018, 65, 42–50. [Google Scholar] [CrossRef]
- Huang, Y.Y.; Lee, J.T.; Huang, C.M.; Gau, M.L. Factors related to maternal perception of milk supply while in the hospital. J. Nurs. Res. 2009, 17, 179–188. [Google Scholar] [CrossRef]
- Liang, K.Y.; Zeger, S.L. Longitudinal data analysis using generalized linear models. Biometrika 1986, 73, 13–22. [Google Scholar] [CrossRef]
- Widström, A.M.; Brimdyr, K.; Svensson, K.; Cadwell, K.; Nissen, E. Skin-to-skin contact the first hour after birth, underlying implications and clinical practice. Acta Paediatr. 2019, 108, 1192–1204. [Google Scholar] [CrossRef] [Green Version]
- Chiou, S.T.; Chen, L.C.; Yeh, H.; Wu, S.R.; Chien, L.Y. Early skin-to-skin contact, rooming-in, and breastfeeding: A comparison of the 2004 and 2011 national surveys in Taiwan. Birth 2014, 41, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Callahan, S.; Séjourné, N.; Denis, A. Fatigue and breastfeeding: An inevitable partnership? J. Hum. Lact. 2006, 22, 182–187. [Google Scholar] [CrossRef]
- Akman, I.; Kuscu, M.K.; Yurdakul, Z.; Ozdemir, N.; Solakoğlu, M.; Orhon, L.; Karabekiroğlu, A.; Ozek, E. Breastfeeding duration and postpartum psychological adjustment: Role of maternal attachment styles. J. Paediatr. Child Health 2008, 44, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Bramson, L.; Lee, J.W.; Moore, E.; Montgomery, S.; Neish, C.; Bahjri, K.; Melcher, C.L. Effect of early skin-to-skin mother--Infant contact during the first 3 hours following birth on exclusive breastfeeding during the maternity hospital stay. J. Hum. Lact. 2010, 26, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Bevan, G.; Brown, M. Interventions in exclusive breastfeeding: A systematic review. Br. J. Nurs. 2014, 23, 86–89. [Google Scholar] [CrossRef] [Green Version]
- Brown, A.; Raynor, P.; Lee, M. Maternal control of child-feeding during breast and formula feeding in the first 6 months post-partum. J. Hum. Nutr. Diet. 2011, 24, 177–186. [Google Scholar] [CrossRef] [Green Version]
- Chang, P.C.; Li, S.F.; Yang, H.Y.; Wang, L.C.; Weng, C.Y.; Chen, K.F.; Chen, W.; Fan, S.Y. Factors associated with cessation of exclusive breastfeeding at 1 and 2 months postpartum in Taiwan. Int. Breastfeed. J. 2019, 14, 18. [Google Scholar] [CrossRef] [Green Version]
- Brandon, D.H.; Tully, K.P.; Silva, S.G.; Malcolm, W.F.; Murtha, A.P.; Turner, B.S.; Holditch-Davis, D. Emotional responses of mothers of late-preterm and term infants. J. Obstet. Gynecol. Neonatal Nurs. 2011, 40, 719–731. [Google Scholar] [CrossRef] [Green Version]
- Ip, W.Y.; Gao, L.L.; Choi, K.C.; Chau, J.P.; Xiao, Y. The Short Form of the Breastfeeding Self-Efficacy Scale as a Prognostic Factor of Exclusive Breastfeeding among Mandarin-Speaking Chinese Mothers. J. Hum. Lact. 2016, 32, 711–720. [Google Scholar] [CrossRef]
- Awaliyah, S.N.; Rachmawati, I.N.; Rahmah, H. Breastfeeding self-efficacy as a dominant factor affecting maternal breastfeeding satisfaction. BMC Nurs. 2019, 18, 30. [Google Scholar] [CrossRef] [PubMed]
- Moberg, K.U.; Handlin, L.; Petersson, M. Neuroendocrine mechanisms involved in the physiological effects caused by skin-to-skin contact—With a particular focus on the oxytocinergic system. Infant Behav. Dev. 2020, 61, 101482. [Google Scholar] [CrossRef] [PubMed]
- Matthiesen, A.S.; Ransjö-Arvidson, A.B.; Nissen, E.; Uvnäs-Moberg, K. Postpartum maternal oxytocin release by newborns: Effects of infant hand massage and sucking. Birth 2001, 28, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Bystrova, K.; Matthiesen, A.S.; Vorontsov, I.; Widström, A.M.; Ransjö-Arvidson, A.B.; Uvnäs-Moberg, K. Maternal axillar and breast temperature after giving birth: Effects of delivery ward practices and relation to infant temperature. Birth 2007, 34, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, M.; Lundeberg, T.; Uvnäs-Moberg, K. Studies on cutaneous blood flow in the mammary gland of lactating rats. Acta Physiol. Scand. 1996, 158, 1–6. [Google Scholar] [CrossRef] [Green Version]

| Variables | Intervention (n = 52) | Control (n = 52) | p Value † |
|---|---|---|---|
| Maternal age (years) | 33.6 ± 5.3 | 32 ± 4.8 | 0.11 |
| Parity | 0.32 | ||
| 1 | 24 (46.2%) | 23 (44.2%) | |
| 2 | 17 (32.7%) | 23 (44.2%) | |
| 3 or more | 11 (21.1%) | 6 (11.6%) | |
| Maternal education | 0.31 | ||
| College or above | 40 (76.9%) | 45 (86.5%) | |
| Marital status | 1 | ||
| Married | 51 (98.1%) | 51 (98.1%) | |
| Employment status | 1 | ||
| Employed | 38 (73.1%) | 38 (73.1%) | |
| Parental leave | 0.3 | ||
| Yes | 20 (38.5%) | 15 (28.8%) | |
| Breastfeeding experience | 0.85 | ||
| Yes | 28 (53.8%) | 27 (51.9%) | |
| Ever heard of SSC | 0.49 | ||
| Yes | 49 (94.2%) | 46 (88.5%) | |
| Pain control | 0.83 | ||
| Yes | 21 (40.4%) | 20 (38.5%) | |
| Delivery assistance | 0.21 | ||
| Medication | 39 (75%) | 45 (86.5%) |
| Variables | Intervention (n = 52) | Control (n = 52) | p Value † |
|---|---|---|---|
| Gestational age | 0.23 | ||
| 37–38 weeks | 25 (48%) | 19 (36.5%) | |
| 39–40 weeks | 27 (52%) | 33 (63.5%) | |
| Male sex | 23 (44.2%) | 28 (53.8%) | 0.33 |
| Birth weight (gm) | 3102 ± 301 | 3114.2 ± 287.2 | 0.83 |
| Birth body height (cm) | 50.9 ± 1.7 | 51.1 ± 1.3 | 0.7 |
| Apgar score (1 min) | 9 (1) | 9 (1) | 0.38 |
| Apgar score (5 min) | 10 (1) | 10 (1) | 1 |
| Variables | Intervention (n = 52) | Control (n = 52) | p Value † |
|---|---|---|---|
| IBFAT score | |||
| After 5 min of SSC | 1.85 ± 1.27 | 1.19 ± 0.99 | 0.005 |
| After skin contact | 6.37 ± 2.47 | 3.23 ± 2.38 | <0.001 |
| 24 h after birth | 8.54 ± 2.17 | 8.37 ± 1.92 | 0.48 |
| Before discharge | 10.06 ± 2.4 | 9.44 ± 2.28 | 0.15 |
| BSES-SF score | |||
| Before discharge | 3.01 ± 0.84 | 3.1 ± 0.91 | 0.19 |
| Successful breastfeeding after SSC | |||
| Yes | 35 (67.3%) | 15 (28.8%) | <0.001 |
| Exclusive breastfeeding rate | |||
| First day of birth | 33 (63.5%) | 25 (48.1%) | 0.12 |
| Second day of birth | 18 (34.6%) | 17 (32.7%) | 0.84 |
| Before discharge | 16 (30.8%) | 15 (28.8%) | 0.83 |
| Parameters | GEE1 (Main Effect) | GEE2 (Interaction) | ||||
|---|---|---|---|---|---|---|
| ꞵ | SE | p Value | ꞵ | SE | p Value | |
| Group effect (Intervention vs. control) | 1.18 | 0.28 | <0.001 | 0.65 | 0.22 | 0.003 |
| After skin contact vs. after 5 min of SSC | 3.28 | 0.22 | <0.001 | 2.04 | 0.29 | <0.001 |
| 24 h after birth vs. after 5 min of SSC | 6.93 | 0.22 | <0.001 | 7.17 | 0.3 | <0.001 |
| Before discharge vs. after 5 min of SSC | 8.23 | 0.25 | <0.001 | 8.25 | 0.35 | <0.001 |
| Group*time | ||||||
| After skin contact vs. after 5 min of SSC | 2.48 | 0.38 | <0.001 | |||
| 24 h after birth vs. after 5 min of SSC | −0.48 | 0.45 | 0.29 | |||
| Before discharge vs. after 5 min of SSC | 0.08 | 0.48 | 0.87 | |||
| Control variable | ||||||
| Breastfeeding self-efficacy scale scores | 0.18 | 0.17 | 0.003 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, J.-Z.; Chen, C.-N.; Lee, C.-P.; Kao, C.-H.; Hsu, H.-C.; Chou, A.-K. Evaluation of the Effects of Skin-to-Skin Contact on Newborn Sucking, and Breastfeeding Abilities: A Quasi-Experimental Study Design. Nutrients 2022, 14, 1846. https://doi.org/10.3390/nu14091846
Huang J-Z, Chen C-N, Lee C-P, Kao C-H, Hsu H-C, Chou A-K. Evaluation of the Effects of Skin-to-Skin Contact on Newborn Sucking, and Breastfeeding Abilities: A Quasi-Experimental Study Design. Nutrients. 2022; 14(9):1846. https://doi.org/10.3390/nu14091846
Chicago/Turabian StyleHuang, Jia-Zhen, Chi-Nien Chen, Chih-Ping Lee, Chien-Huei Kao, Heng-Cheng Hsu, and An-Kuo Chou. 2022. "Evaluation of the Effects of Skin-to-Skin Contact on Newborn Sucking, and Breastfeeding Abilities: A Quasi-Experimental Study Design" Nutrients 14, no. 9: 1846. https://doi.org/10.3390/nu14091846
APA StyleHuang, J.-Z., Chen, C.-N., Lee, C.-P., Kao, C.-H., Hsu, H.-C., & Chou, A.-K. (2022). Evaluation of the Effects of Skin-to-Skin Contact on Newborn Sucking, and Breastfeeding Abilities: A Quasi-Experimental Study Design. Nutrients, 14(9), 1846. https://doi.org/10.3390/nu14091846






