Influence of Obesity on Bone Turnover Markers and Fracture Risk in Postmenopausal Women
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Population and Study Period
2.3. Variables
2.3.1. Epidemiological Variables
- Age: it was calculated based on the date of birth and the of entry into the study;
- Physical activity: habitual physical activity is defined as that with a minimum duration of 30 min of exercise per day or 60 min on two days;
- Alcohol consumption: It is considered with the intake of more than 5 g per day. We have considered alcohol abuse with an intake of more than 20 g per day;
- Smoking: This variable was considered with a smoking habit of more than 6 months;
- Calcium intake in the diet: Calcium intake was considered based on the dairy rations consumed per day. In total, 200 mg of calcium per dairy ration consumed per day were considered. It was considered a dairy ration (1 glass of milk of 200 mL, 2 yogurts, or 1 portion of 100 g cheese);
- Consumption of vitamin D in the diet: The consumption of vitamin D was considered based on the rations of dairy products consumed per day. In total, 0.2 μg of vitamin D per dairy ration was considered. It was considered a dairy ration (1 glass of milk of 200 mL, 2 yogurts, or 1 portion of 100 g cheese).
2.3.2. Biochemical Variables
- Vitamin D: This was determined by electrochemiluminescence immunoassay. Cobas 6000 e-601 (Roche Diagnostics, Basel, Switzerland) with a measurement range between 3.00–70.0 ng/mL;
- Plasma calcium: Total calcium was determined by the ocresolphthalein Schearzenbach method;
- Bone turnover markers: Three parameters were collected as bone turnover markers. These were beta-crosslap, type I procollagen amino-terminal propeptide (P1NP) and bone non-specific alkaline phosphatase (FA);
- ○
- Beta-Crosslap: This is a marker of bone resorption. The measurement range was 0.010–6.00 ng/mL with a functional sensitivity of 0.07 ng/mL. Normal values are different depending on the stage of life. In the case of a postmenopausal woman, the reference value is 0.556–1.008 ng/mL;
- ○
- P1NP: This bone formation marker is called the amino-terminal propeptide of type I procollagen. The measurement range was 5–1200 μg/L. The reference value in a postmenopausal woman is <76.3 ng/mL;
- ○
- Alkaline phosphatase: Total alkaline phosphatase (not bone-specific) was considered. This is a marker of bone formation.
2.3.3. Anthropometric Variables
2.3.4. Fracture Variables
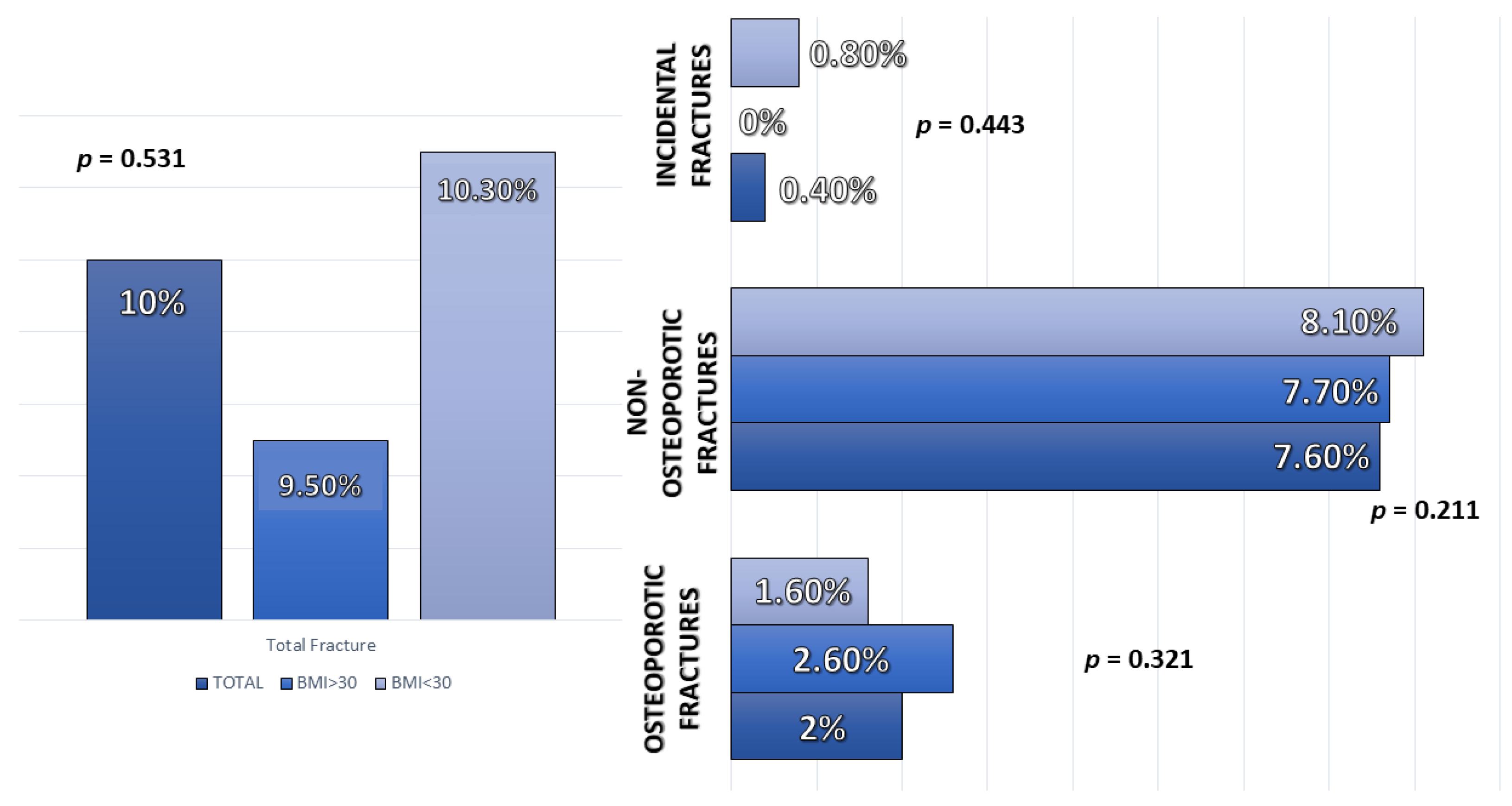
- Osteoporotic-type fracture: For this type of fracture, classic osteoporotic locations were considered (vertebral compression, femoral neck fracture, and distal radius fracture (Colles fracture));
- Non-osteoporotic fracture: Those that were not found in the typical osteoporotic locations already described (fractures due to trauma, or low impact fractures in non-classical locations of osteoporosis);
- Incidental fracture: To detect this type of fracture, the available imaging tests were reviewed in search of fractures that had gone unnoticed.
2.4. Statistical Analysis
3. Results
3.1. Description of the Sample
3.2. Differences in Bone Turnover Biochemical Parameters
3.3. Correlation between BMI and Bone Turnover Biochemical Markers
3.4. Multivariate Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ström, O.; Borgström, F.; Kanis, J.A.; Compston, J.; Cooper, C.; McCloskey, E.V.; Jönsson, B. Osteoporosis: Burden, health care provision and opportunities in the EU: A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch. Osteoporos. 2011, 6, 59–155. [Google Scholar] [CrossRef] [PubMed]
- Hernlund, E.; Svedbom, A.; Ivergård, M.; Compston, J.; Cooper, C.; Stenmark, J.; McCloskey, E.V.; Jönsson, B.; Kanis, J.A. Osteoporosis in the European Union: Medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch. Osteoporos. 2013, 8, 136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fassio, A.; Idolazzi, L.; Rossini, M.; Gatti, D.; Adami, G.; Giollo, A.; Viapiana, O. The obesity paradox and osteoporosis. Eat. Weight Disord. EWD 2018, 23, 293–302. [Google Scholar] [CrossRef] [PubMed]
- Gonnelli, S.; Caffarelli, C.; Nuti, R. Obesity and fracture risk. Clin. Cases Miner. Bone Metab. 2014, 11, 9–14. [Google Scholar] [CrossRef]
- López-Gómez, J.J.; Pérez Castrillón, J.L.; de Luis Román, D.A. Impact of obesity on bone metabolism. Endocrinol. Nutr. 2016, 63, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Greco, E.A.; Lenzi, A.; Migliaccio, S. The obesity of bone. Ther. Adv. Endocrinol. Metab. 2015, 6, 273–286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holecki, M.; Wiecek, A. Relationship between body fat mass and bone metabolism. Pol. Arch. Intern. Med. 2010, 120, 361–367. [Google Scholar] [CrossRef]
- Migliaccio, S.; Di Nisio, A.; Mele, C.; Scappaticcio, L.; Savastano, S.; Colao, A.; Obesity Programs of Nutrition, Education, Research and Assessment (OPERA) Group. Obesity and hypovitaminosis D: Causality or casualty? Int. J. Obes. Suppl. 2019, 9, 20–31. [Google Scholar] [CrossRef]
- Walsh, J.S.; Evans, A.L.; Bowles, S.; Naylor, K.E.; Jones, K.S.; Schoenmakers, I.; Jacques, R.M.; Eastell, R. Free 25-hydroxyvitamin D is low in obesity, but there are no adverse associations with bone health. Am. J. Clin. Nutr. 2016, 103, 1465–1471. [Google Scholar] [CrossRef] [Green Version]
- Reid, I.R. Relationships among body mass, its components, and bone. Bone 2002, 31, 547–555. [Google Scholar] [CrossRef]
- Gower, B.A.; Casazza, K. Divergent effects of obesity on bone health. J. Clin. Densitom. 2013, 16, 450–454. [Google Scholar] [CrossRef] [Green Version]
- Collins, K.H.; Herzog, W.; Macdonald, G.Z.; Reimer, R.A.; Rios, J.L.; Smith, I.C.; Zernicke, R.F.; Hart, D.A. Obesity, Metabolic Syndrome, and Musculoskeletal Disease: Common Inflammatory Pathways Suggest a Central Role for Loss of Muscle Integrity. Front. Physiol. 2018, 9, 112. [Google Scholar] [CrossRef]
- Jain, R.K.; Vokes, T. Fat Mass Has Negative Effects on Bone, Especially in Men: A Cross-Sectional Analysis of NHANES 2011–2018. J. Clin. Endocrinol. Metab. 2022, dgac040. [Google Scholar] [CrossRef]
- Yao, W.J.; Wu, C.H.; Wang, S.T.; Chang, C.J.; Chiu, N.T.; Yu, C.Y. Differential changes in regional bone mineral density in healthy Chinese: Age-related and sex-dependent. Calcif. Tissue Int. 2001, 68, 330–336. [Google Scholar] [CrossRef]
- Zhao, L.-J.; Jiang, H.; Papasian, C.J.; Maulik, D.; Drees, B.; Hamilton, J.; Deng, H.-W. Correlation of obesity and osteoporosis: Effect of fat mass on the determination of osteoporosis. J. Bone Miner. Res. 2008, 23, 17–29. [Google Scholar] [CrossRef] [Green Version]
- Corina, M.; Vulpoi, C.; Brănişteanu, D. Relationship between bone mineral density, weight, and estrogen levels in pre and postmenopausal women. Med.-Surg. J. 2012, 116, 946–950. [Google Scholar]
- Savvidis, C.; Tournis, S.; Dede, A.D. Obesity and bone metabolism. Hormones 2018, 17, 205–217. [Google Scholar] [CrossRef]
- Johansson, H.; Kanis, J.A.; Odén, A.; McCloskey, E.; Chapurlat, R.D.; Christiansen, C.; Cummings, S.R.; Diez-Perez, A.; Eisman, J.A.; Fujiwara, S.; et al. A meta-analysis of the association of fracture risk and body mass index in women. J. Bone Miner. Res. 2014, 29, 223–233. [Google Scholar] [CrossRef]
- Compston, J.E.; Watts, N.B.; Chapurlat, R.; Cooper, C.; Boonen, S.; Greenspan, S.; Pfeilschifter, J.; Silverman, S.; Díez-Pérez, A.; Lindsay, R.; et al. Obesity is not protective against fracture in postmenopausal women: GLOW. Am. J. Med. 2011, 124, 1043–1050. [Google Scholar] [CrossRef] [Green Version]
- Li, X.; Gong, X.; Jiang, W. Abdominal obesity and risk of hip fracture: A meta-analysis of prospective studies. Osteoporos. Int. 2017, 28, 2747–2757. [Google Scholar] [CrossRef]
- Sadeghi, O.; Saneei, P.; Nasiri, M.; Larijani, B.; Esmaillzadeh, A. Abdominal Obesity and Risk of Hip Fracture: A Systematic Review and Meta-Analysis of Prospective Studies. Adv. Nutr. 2017, 8, 728–738. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- López-Gómez, J.J.; Izaola-Jauregui, O.; Primo-Martín, D.; Torres-Torres, B.; Gómez-Hoyos, E.; Ortolá-Buigues, A.; Martín-Ferrero, M.A.; Pérez-Castrillón, J.L.; De Luis-Román, D.A. Effect of weight loss on bone metabolism in postmenopausal obese women with osteoarthritis. Obes. Res. Clin. Pract. 2019, 13, 378–384. [Google Scholar] [CrossRef] [PubMed]
| TOTAL | BMI > 30 | BMI < 30 | p-Value | |
|---|---|---|---|---|
| BMI 1 (kg/m2) | 32.27 (24.14–39.59) | 39.49 (5.13) | 24.14 (2.87) | p < 0.01 |
| Age (years) | 56.17 (3.91) | 56.99 (4.48) | 55.33 (3.01) | p < 0.01 |
| Alcohol (%) | 18 (7.2%) | 13 (10.3%) | 5 (4%) | 0.055 |
| Smoking (%) | 59 (23.6%) Exfum 27 (10.8%) | 18 (14.4%) 4 (3.2%) | 41 (33.1%) 23 (18.5%) | <0.01 |
| Physical activity (%) | 144 (57.6%) | 38 (30.2%) | 106 (85.5%) | <0.01 |
| Dietary calcium (mg) | 742.50 (330.18) | 857.50 (302.16) | 633.52 (322.53) | <0.01 |
| Dietary vitamin D3 (μg) | 1.05 (1.39) | 1.58 (1.95) | 0.63 (0.32) | <0.01 |
| Q1 (<53 Years) | Q2 (53–56 Years) | Q3 (56–59 Years) | Q4 (>60 Years) | |||||
|---|---|---|---|---|---|---|---|---|
| Variable | BMI 1 > 30 | BMI 1 < 30 | BMI 1 > 30 | BMI 1 < 30 | BMI 1 > 30 | BMI 1 < 30 | BMI 1 > 30 | BMI 1 < 30 |
| Calcium (mg/dL) | 9.4 (9.15–9.59) | 9.48 (9.27–9.66) | 9.5 (9.28–9.77) | 9.43 (9.24–9.67) | 9.60 (9.50–9.90) | 9.45 (9.29–9.67) | 9.40 (9.30–9.67) | 9.71 (9.62–9.81) |
| 25OHvitamin D (ng/mL) | 17.30 (7.46) | 23.56 (10.35) | 16.59 (8.86) | 25.66 (8.95) | 18.24 (8.66) | 24.39 (9.54) | 16.48 (6.01) | 26.42 (7.21) |
| PTH (pg/mL) | 54.36 (40.77–64.44) | 36.23 (28.74–42.01) | 51.89 (37.34–69.52) | 29.9 (24.72–39.90) | 51.27 (38.68–68.96) | 36.39 (24.04–46.04) | 54 (38.06–60.55) | 48.13 (31.18–48.18) |
| P1NP (ng/mL) | 46.11 (29.91–55.81) | 65.49 (50.64–85.55) | 43.40 (32.86–46.40) | 56.04 (44.78–70.01) | 48.35 (37.89–62.08) | 47.84 (40.55–56.83) | 43.49 (34.91–59.63) | 61.16 (30.42–77.01) |
| CROSSLAPS (ng/mL) | 0.32 (0.16) | 0.38 (0.17) | 0.32 (0.11) | 0.30 (0.98) | 0.35 (0.13) | 0.29 (0.12) | 0.39 (0.14) | 0.24 (0.09) |
| Alcaline Phosphatase (mg/dL) | 77.10 (23.66) | 92.65 (20.96) | 75.92 (17.80) | 81.21 (25.79) | 83.61 (20.97) | 82.39 (17.19) | 75.83 (21.21) | 85.66 (29.29) |
| Calcium (mg/dL) | 25OHvitamin D (ng/mL) | PTH 1 Intact (pg/mL) | P1NP1 2 (ng/mL) | Crosslaps (ng/mL) | Alcaline Phosphatase (mg/dL) | |
|---|---|---|---|---|---|---|
| TOTAL | r = 0.09 p = 0.17 | r = −0.39 p < 0.01 | r = 0.52 p < 0.01 | r = −0.29 p < 0.01 | r = 0.04 p = 0.24 | r = −0.13 p = 0.04 |
| Q1 (<53 years) | r = −0.22 p = 0.04 | r = −0.34 p < 0.01 | r = 0.55 p < 0.01 | r = −0.37 p < 0.01 | r = −0.128 p = 0.24 | r = −0.27 p = 0.01 |
| Q2 (53–56 years) | r = 0.03 p = 0.81 | r = −0.43 p < 0.01 | r = 0.53 p < 0.01 | r = −0.39 p < 0.01 | r = 0.04 p = 0.77 | r = −0.06 p = 0.63 |
| Q3 (56–59 years) | r = 0.23 p = 0.08 | r = −0.35 p < 0.01 | r = 0.51 p < 0.01 | r = 0.08 p = 0.54 | r = 0.27 p = 0.03 | r = 0.06 p = 0.65 |
| Q4 (>59 years) | r = −0.14 p = 0.49 | r = −0.47 p = 0.01 | r = 0.32 p = 0.23 | r = −0.20 p = 0.31 | r = 0.11 p = 0.59 | r = −0.01 p = 0.96 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Gómez, J.J.; Pérez-Castrillón, J.L.; García de Santos, I.; Pérez-Alonso, M.; Izaola-Jauregui, O.; Primo-Martín, D.; De Luis-Román, D.A. Influence of Obesity on Bone Turnover Markers and Fracture Risk in Postmenopausal Women. Nutrients 2022, 14, 1617. https://doi.org/10.3390/nu14081617
López-Gómez JJ, Pérez-Castrillón JL, García de Santos I, Pérez-Alonso M, Izaola-Jauregui O, Primo-Martín D, De Luis-Román DA. Influence of Obesity on Bone Turnover Markers and Fracture Risk in Postmenopausal Women. Nutrients. 2022; 14(8):1617. https://doi.org/10.3390/nu14081617
Chicago/Turabian StyleLópez-Gómez, Juan J., José L. Pérez-Castrillón, Isabel García de Santos, María Pérez-Alonso, Olatz Izaola-Jauregui, David Primo-Martín, and Daniel A. De Luis-Román. 2022. "Influence of Obesity on Bone Turnover Markers and Fracture Risk in Postmenopausal Women" Nutrients 14, no. 8: 1617. https://doi.org/10.3390/nu14081617
APA StyleLópez-Gómez, J. J., Pérez-Castrillón, J. L., García de Santos, I., Pérez-Alonso, M., Izaola-Jauregui, O., Primo-Martín, D., & De Luis-Román, D. A. (2022). Influence of Obesity on Bone Turnover Markers and Fracture Risk in Postmenopausal Women. Nutrients, 14(8), 1617. https://doi.org/10.3390/nu14081617







