Association between Protein Intake and the Risk of Hypertension among Chinese Men and Women: A Longitudinal Study
Abstract
1. Introduction
2. Materials and Methods
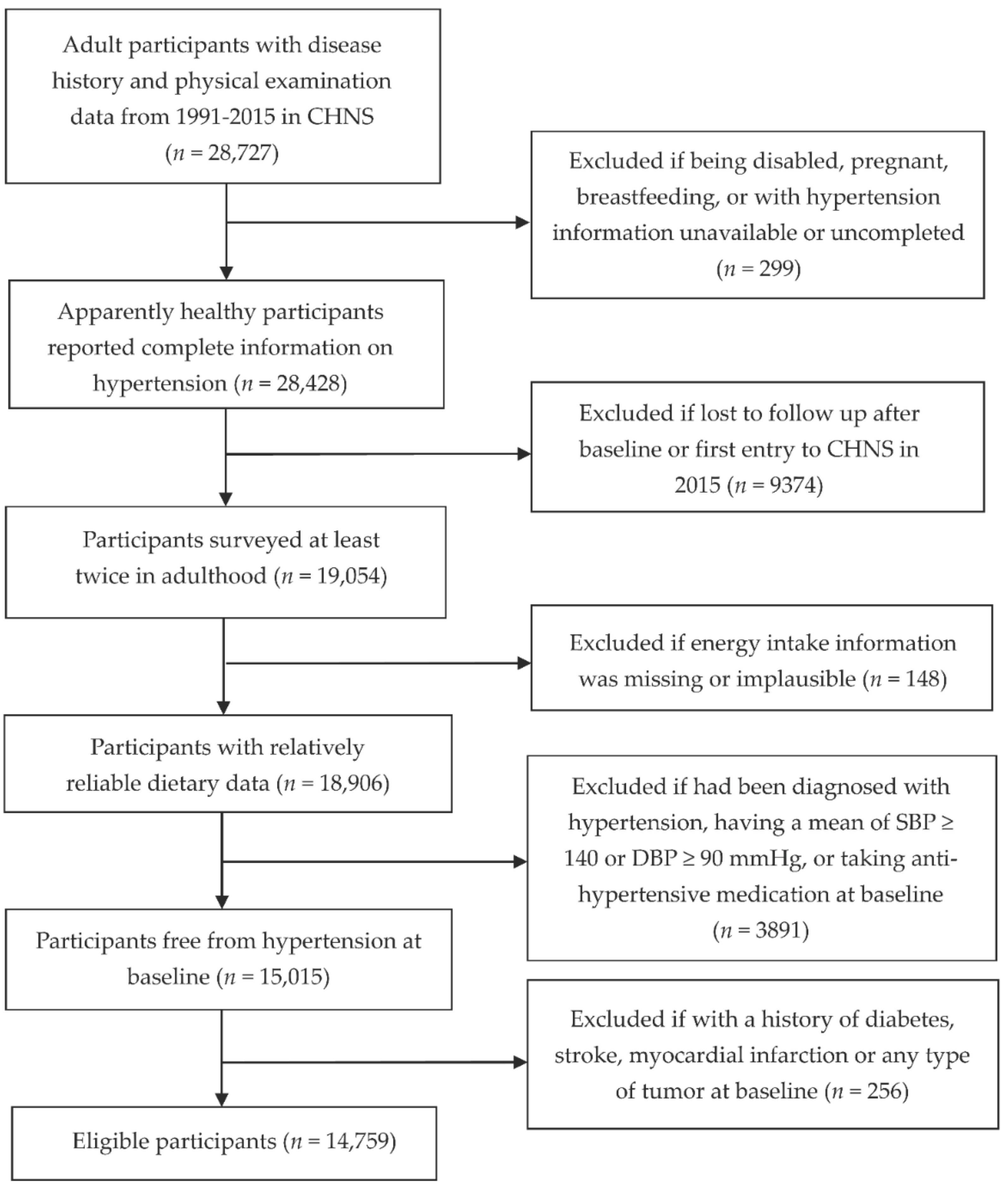
2.1. Study Population
2.2. Ascertainment of Outcome
2.3. Measurement of Dietary Intakes
2.4. Assessment of Non-Dietary Covariates
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Summary
4.2. Comparison with Other Studies
4.3. Possible Explanations and Implications
4.4. Strengths and Weaknesses of Our Study
4.5. Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kennedy, S. The role of diet in lowering blood pressure. Nurs. Stand. 2011, 25, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Appel, L.J.; Brands, M.W.; Daniels, S.R.; Karanja, N.; Elmer, P.J.; Sacks, F.M. Dietary approaches to prevent and treat hypertension: A scientific statement from the American Heart Association. Hypertension 2006, 47, 296–308. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Ikeda, K.; Sullivan, D.H.; Ling, W.; Yamori, Y. Epidemiological evidence of the association between dietary protein intake and blood pressure: A meta-analysis of published data. Hypertens. Res. 2002, 25, 689–695. [Google Scholar] [CrossRef]
- Dasinger, J.H.; Fehrenbach, D.J.; Abais-Battad, J.M. Dietary Protein: Mechanisms Influencing Hypertension and Renal Disease. Curr. Hypertens. Rep. 2020, 22, 13. [Google Scholar] [CrossRef] [PubMed]
- Teunissen-Beekman, K.F.; van Baak, M.A. The role of dietary protein in blood pressure regulation. Curr. Opin. Lipidol. 2013, 24, 65–70. [Google Scholar] [CrossRef]
- van der Kuil, W.A.; Engberink, M.F.; Brink, E.J.; van Baak, M.A.; Bakker, S.J.; Navis, G.; van Veer, V.P.; Geleijnse, J.M. Dietary protein and blood pressure: A systematic review. PLoS ONE 2010, 5, e12102. [Google Scholar] [CrossRef]
- Tielemans, S.M.; van der Kuil, W.A.; Engberink, M.F.; Brink, E.J.; van Baak, M.A.; Bakker, S.J.; Geleijnse, J.M. Intake of total protein, plant protein and animal protein in relation to blood pressure: A meta-analysis of observational and intervention studies. J. Hum. Hypertens. 2013, 27, 564–571. [Google Scholar] [CrossRef]
- Martin, D.S. Dietary protein and hypertension: Where do we stand? Nutrition 2003, 19, 385–386. [Google Scholar] [CrossRef]
- Stamler, J.; Liu, K.; Ruth, K.J.; Pryer, J.; Greenland, P. Eight-year blood pressure change in middle-aged men: Relationship to multiple nutrients. Hypertension 2002, 39, 1000–1006. [Google Scholar] [CrossRef]
- van der Kuil, W.A.; Engberink, M.F.; van Rooij, F.J.; Hofman, A.; van Veer, V.P.; Witteman, J.C.; Geleijnse, J.M. Dietary protein and risk of hypertension in a Dutch older population: The Rotterdam study. J. Hypertens. 2010, 28, 2394–2400. [Google Scholar] [CrossRef]
- Buendia, J.R.; Bradlee, M.L.; Singer, M.R.; Moore, L.L. Diets higher in protein predict lower high blood pressure risk in Framingham Offspring Study adults. Am. J. Hypertens. 2015, 28, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Alonso, A.; Beunza, J.J.; Bes-Rastrollo, M.; Pajares, R.M.; Martínez-González, M.A. Vegetable protein and fiber from cereal are inversely associated with the risk of hypertension in a Spanish cohort. Arch. Med. Res. 2006, 37, 778–786. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.F.; Yancy, W.J.; Yu, D.; Champagne, C.; Appel, L.J.; Lin, P.H. The relationship between dietary protein intake and blood pressure: Results from the PREMIER study. J. Hum. Hypertens. 2008, 22, 745–754. [Google Scholar] [CrossRef] [PubMed]
- Chalvon-Demersay, T.; Azzout-Marniche, D.; Arfsten, J.; Egli, L.; Gaudichon, C.; Karagounis, L.G.; Tomé, D. A Systematic Review of the Effects of Plant Compared with Animal Protein Sources on Features of Metabolic Syndrome. J. Nutr. 2017, 147, 281–292. [Google Scholar] [CrossRef] [PubMed]
- Iseki, K.; Iseki, C.; Itoh, K.; Sanefuji, M.; Uezono, K.; Ikemiya, Y.; Fukiyama, K.; Kawasaki, T. Estimated protein intake and blood pressure in a screened cohort in Okinawa, Japan. Hypertens. Res. 2003, 26, 289–294. [Google Scholar] [CrossRef][Green Version]
- Zhang, B.; Zhai, F.Y.; Du, S.F.; Popkin, B.M. The China Health and Nutrition Survey, 1989–2011. Obes. Rev. 2014, 15, 2–7. [Google Scholar] [CrossRef]
- Popkin, B.M.; Du, S.; Zhai, F.; Zhang, B. Cohort Profile: The China Health and Nutrition Survey--monitoring and understanding socio-economic and health change in China, 1989–2011. Int. J. Epidemiol. 2010, 39, 1435–1440. [Google Scholar] [CrossRef]
- Du, S.; Batis, C.; Wang, H.; Zhang, B.; Zhang, J.; Popkin, B.M. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. Am. J. Clin. Nutr. 2014, 99, 334–343. [Google Scholar] [CrossRef]
- Wang, Z.; Huang, Q.; Wang, L.; Jiang, H.; Wang, Y.; Wang, H.; Zhang, J.; Zhai, F.; Zhang, B. Moderate Intake of Lean Red Meat was Associated with Lower Risk of Elevated Blood Pressure in Chinese Women: Results from the China Health and Nutrition Survey, 1991–2015. Nutrients 2020, 12, 1369. [Google Scholar] [CrossRef]
- Zhai, F.Y.; Du, S.F.; Wang, Z.H.; Zhang, J.G.; Du, W.W.; Popkin, B.M. Dynamics of the Chinese diet and the role of urbanicity, 1991–2011. Obes. Rev. 2014, 15 (Suppl. S1), 16–26. [Google Scholar] [CrossRef]
- Yao, M.; Lichtenstein, A.H.; Roberts, S.B.; Ma, G.; Gao, S.; Tucker, K.L.; McCrory, M.A. Relative influence of diet and physical activity on cardiovascular risk factors in urban Chinese adults. Int. J. Obes. 2003, 27, 920–932. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.C.; Howe, G.R.; Kushi, L.H. Adjustment for total energy intake in epidemiologic studies. Am. J. Clin. Nutr. 1997, 65, 1220S–1228S. [Google Scholar] [CrossRef]
- Hu, F.B.; Stampfer, M.J.; Rimm, E.; Ascherio, A.; Rosner, B.A.; Spiegelman, D.; Willett, W.C. Dietary fat and coronary heart disease: A comparison of approaches for adjusting for total energy intake and modeling repeated dietary measurements. Am. J. Epidemiol. 1999, 149, 531–540. [Google Scholar] [CrossRef] [PubMed]
- Desquilbet, L.; Mariotti, F. Dose-response analyses using restricted cubic spline functions in public health research. Stat. Med. 2010, 29, 1037–1057. [Google Scholar] [CrossRef] [PubMed]
- Shang, X.; Scott, D.; Hodge, A.; English, D.R.; Giles, G.G.; Ebeling, P.R.; Sanders, K.M. Dietary protein from different food sources, incident metabolic syndrome and changes in its components: An 11-year longitudinal study in healthy community-dwelling adults. Clin. Nutr. 2017, 36, 1540–1548. [Google Scholar] [CrossRef]
- Hruby, A.; Jacques, P.F. Dietary protein and changes in markers of cardiometabolic health across 20 years of follow-up in middle-aged Americans. Public Health Nutr. 2018, 21, 2998–3010. [Google Scholar] [CrossRef]
- van der Kuil, W.A.; Engberink, M.F.; Geleijnse, J.M.; Boer, J.M.; Monique, V.W. Sources of dietary protein and risk of hypertension in a general Dutch population. Br. J. Nutr. 2012, 108, 1897–1903. [Google Scholar] [CrossRef]
- Tielemans, S.M.; Kromhout, D.; van der Kuil, W.A.; Geleijnse, J.M. Associations of plant and animal protein intake with 5-year changes in blood pressure: The Zutphen Elderly Study. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 1228–1233. [Google Scholar] [CrossRef]
- Zhou, B.; Zhang, X.; Zhu, A.; Zhao, L.; Zhu, S.; Ruan, L.; Zhu, L.; Liang, S. The relationship of dietary animal protein and electrolytes to blood pressure: A study on three Chinese populations. Int. J. Epidemiol. 1994, 23, 716–722. [Google Scholar] [CrossRef]
- Liu, L.; Ikeda, K.; Yamori, Y. Inverse relationship between urinary markers of animal protein intake and blood pressure in Chinese: Results from the WHO Cardiovascular Diseases and Alimentary Comparison (CARDIAC) Study. Int. J. Epidemiol. 2002, 31, 227–233. [Google Scholar] [CrossRef]
- Liu, R.; Dang, S.; Yan, H.; Wang, D.; Zhao, Y.; Li, Q.; Liu, X. Association between dietary protein intake and the risk of hypertension: A cross-sectional study from rural western China. Hypertens. Res. 2013, 36, 972–979. [Google Scholar] [CrossRef] [PubMed]
- Umesawa, M.; Sato, S.; Imano, H.; Kitamura, A.; Shimamoto, T.; Yamagishi, K.; Tanigawa, T.; Iso, H. Relations between protein intake and blood pressure in Japanese men and women: The Circulatory Risk in Communities Study (CIRCS). Am. J. Clin. Nutr. 2009, 90, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Gambardella, J.; Khondkar, W.; Morelli, M.B.; Wang, X.; Santulli, G.; Trimarco, V. Arginine and Endothelial Function. Biomedicines 2020, 8, 277. [Google Scholar] [CrossRef] [PubMed]
- Shan, L.; Wang, B.; Gao, G.; Cao, W.; Zhang, Y. L-Arginine supplementation improves antioxidant defenses through L-arginine/nitric oxide pathways in exercised rats. J. Appl. Physiol. 2013, 115, 1146–1155. [Google Scholar] [CrossRef] [PubMed]
- Poggiogalle, E.; Fontana, M.; Giusti, A.M.; Pinto, A.; Iannucci, G.; Lenzi, A.; Donini, L.M. Amino Acids and Hypertension in Adults. Nutrients 2019, 11, 1459. [Google Scholar] [CrossRef]
- Ardiansyah, N.; Shirakawa, H.; Inagawa, Y.; Koseki, T.; Komai, M. Regulation of blood pressure and glucose metabolism induced by L-tryptophan in stroke-prone spontaneously hypertensive rats. Nutr. Metab. 2011, 8, 45. [Google Scholar] [CrossRef]
- De Miguel, C.; Lund, H.; Mattson, D.L. High dietary protein exacerbates hypertension and renal damage in Dahl SS rats by increasing infiltrating immune cells in the kidney. Hypertension 2011, 57, 269–274. [Google Scholar] [CrossRef]
- Villa-Etchegoyen, C.; Lombarte, M.; Matamoros, N.; Belizán, J.M.; Cormick, G. Mechanisms Involved in the Relationship between Low Calcium Intake and High Blood Pressure. Nutrients 2019, 11, 1112. [Google Scholar] [CrossRef]
- Cao, J.J.; Nielsen, F.H. Acid diet (high-meat protein) effects on calcium metabolism and bone health. Curr. Opin. Clin. Nutr. 2010, 13, 698–702. [Google Scholar] [CrossRef]
- Bernstein, A.M.; Treyzon, L.; Li, Z. Are high-protein, vegetable-based diets safe for kidney function? A review of the literature. J. Am. Diet. Assoc. 2007, 107, 644–650. [Google Scholar] [CrossRef]

| Quintiles of Animal Protein Intake | p for Trend | Quintiles of Plant Protein Intake | p for Trend | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| No. of participants | 1401 | 1401 | 1402 | 1401 | 1402 | 1401 | 1401 | 1402 | 1401 | 1402 | ||
| Age (year) | 37.4 ± 15.4 | 36.4 ± 14 | 37.3 ± 14.3 | 37.2 ± 14.3 | 37.2 ± 14.1 | 0.7711 | 38.6 ± 14.8 | 36.5 ± 14 | 37.3 ± 14.1 | 36.0 ± 14.2 | 37.0 ± 14.9 | 0.003 |
| BMI (kg/m2) | 21.3 ± 2.6 | 21.6 ± 2.7 | 21.8 ± 2.8 | 22 ± 2.9 | 22.5 ± 3.4 | <0.0001 | 22.3 ± 3.3 | 21.8 ± 3.0 | 21.7 ± 3.0 | 21.6 ± 2.7 | 21.7 ± 2.6 | <0.0001 |
| PAL (×BMR) | 2.0 ± 0.2 | 1.9 ± 0.3 | 1.8 ± 0.3 | 1.7 ± 0.3 | 1.6 ± 0.3 | <0.0001 | 1.6 ± 0.3 | 1.7 ± 0.3 | 1.8 ± 0.3 | 1.9 ± 0.3 | 1.9 ± 0.3 | <0.0001 |
| Urban residential area, n (%) | 162 (11.6%) | 335 (23.9%) | 487 (34.7%) | 657 (46.9%) | 891 (63.6%) | <0.0001 | 766 (54.7%) | 593 (42.3%) | 496 (35.4%) | 405 (28.9%) | 272 (19.4%) | <0.0001 |
| Education level, n (%) | <0.0001 | <0.0001 | ||||||||||
| Low | 753 (53.7%) | 608 (43.4%) | 449 (32%) | 332 (23.7%) | 214 (15.3%) | 308 (22.0%) | 392 (28.0%) | 489 (34.9%) | 524 (37.4%) | 643 (45.9%) | ||
| Medium | 640 (45.7%) | 758 (54.1%) | 871 (62.1%) | 945 (67.5%) | 939 (67%) | 872 (62.2%) | 898 (64.1%) | 831 (59.3%) | 823 (58.7%) | 729 (52.0%) | ||
| High | 8 (0.6%) | 35 (2.5%) | 82 (5.8%) | 124 (8.9%) | 249 (17.8%) | 221 (15.8%) | 111 (7.9%) | 82 (5.8%) | 54 (3.9%) | 30 (2.1%) | ||
| Household income level, n (%) | <0.0001 | <0.0001 | ||||||||||
| Low | 807 (57.6%) | 560 (40.0%) | 378 (27.0%) | 247 (17.6%) | 119 (8.5%) | 166 (11.8%) | 305 (21.8%) | 429 (30.6%) | 519 (37.0%) | 692 (49.4%) | ||
| Medium | 377 (26.9%) | 470 (33.5%) | 435 (31.0%) | 402 (28.7%) | 296 (21.1%) | 265 (18.9%) | 426 (30.4%) | 437 (31.2%) | 430 (30.7%) | 422 (30.1%) | ||
| High | 165 (11.8%) | 234 (16.7%) | 364 (26.0%) | 402 (28.7%) | 407 (29.0%) | 399 (28.5%) | 376 (26.8%) | 321 (22.9%) | 287 (20.5%) | 189 (13.5%) | ||
| Very high | 52 (3.7%) | 137 (9.8%) | 225 (16.0%) | 350 (25.0%) | 580 (41.4%) | 571 (40.8%) | 294 (21.0%) | 215 (15.3%) | 165 (11.8%) | 99 (7.1%) | ||
| Ever and current smoker, n (%) | 931 (66.5%) | 903 (64.5%) | 868 (61.9%) | 841 (60.0%) | 845 (60.3%) | <0.0001 | 894 (63.8%) | 859 (61.3%) | 866 (61.8%) | 865 (61.7%) | 904 (64.5%) | 0.666 |
| Alcohol consumer, n (%) | 840 (60.0%) | 835 (59.6%) | 900 (64.2%) | 858 (61.2%) | 888 (63.3%) | 0.041 | 895 (63.9%) | 848 (60.5%) | 867 (61.8%) | 867 (61.9%) | 844 (60.2%) | 0.143 |
| SBP (mm Hg) | 113.0 ± 11.5 | 113.0 ± 11.3 | 114.1 ± 10.9 | 114.2 ± 10.9 | 115.8 ± 10.5 | <0.0001 | 115.6 ± 10.6 | 114.0 ± 11.2 | 113.3 ± 11.1 | 113.2 ± 10.8 | 113.9 ± 11.4 | <0.0001 |
| TE (kcal/day) | 2665.0 ± 645.9 | 2512.1 ± 545.9 | 2485.4 ± 561 | 2465.6 ± 546.2 | 2404.2 ± 603.2 | <0.0001 | 2436.0 ± 656.2 | 2471.2 ± 530.8 | 2483.1 ± 524.9 | 2497.8 ± 548.5 | 2644.0 ± 644.6 | <0.0001 |
| Protein (g/day) | 67.8 ± 10.8 | 68.4 ± 9.5 | 71.2 ± 9.1 | 76.2 ± 8.5 | 89.5 ± 13.8 | <0.0001 | 74.1 ± 16.2 | 73.5 ± 12.6 | 73.0 ± 12.3 | 73.4 ± 11.6 | 79.1 ± 11.9 | <0.0001 |
| Protein (%TE) | 11.0 ± 1.7 | 11.2 ± 1.5 | 11.7 ± 1.5 | 12.5 ± 1.5 | 14.7 ± 2.4 | <0.0001 | 12.2 ± 2.8 | 12.1 ± 2.2 | 12.0 ± 2.1 | 12.0 ± 2.0 | 12.9 ± 2.0 | <0.0001 |
| Animal protein (g/day) | 1.9 (0.0, 4.1) | 10.7 (8.6, 12.7) | 18.9 (16.8, 20.9) | 27.4 (25.2, 29.9) | 41 (36.2, 48.2) | <0.0001 | 33.0 (24.1, 43.4) | 25.5 (18.2, 32.9) | 19.2 (11.5, 27.1) | 12.2 (5.6, 20.6) | 4.7 (0.5, 11.3) | <0.0001 |
| Animal protein (%TE) | 0.3 (0.0, 0.7) | 1.7 (1.4, 2.1) | 3.1 (2.7, 3.5) | 4.5 (4.1, 5.0) | 6.9 (6.0, 8.3) | <0.0001 | 5.5 (3.9, 7.3) | 4.1 (3.0, 5.5) | 3.1 (1.9, 4.5) | 2.0 (0.9, 3.4) | 0.8 (0.1, 1.8) | <0.0001 |
| Plant protein (g/day) | 63.6 ± 10.7 | 55.7 ± 9.7 | 50.0 ± 9.1 | 46.0 ± 8.5 | 41.8 ± 10.1 | <0.0001 | 35.3 ± 5.7 | 44.7 ± 1.7 | 50.5 ± 1.7 | 57.2 ± 2.2 | 69.4 ± 7.3 | <0.0001 |
| Plant protein (%TE) | 10.4 ± 1.8 | 9.1 ± 1.6 | 8.2 ± 1.5 | 7.5 ± 1.4 | 6.8 ± 1.6 | <0.0001 | 5.8 ± 0.9 | 7.3 ± 0.3 | 8.2 ± 0.3 | 9.3 ± 0.4 | 11.3 ± 1.2 | <0.0001 |
| CHO (%TE) | 71.3 ± 8.1 | 63.5 ± 7.9 | 58.2 ± 8.0 | 54.5 ± 7.8 | 49.2 ± 9.3 | <0.0001 | 47.1 ± 9.3 | 56.1 ± 7.3 | 60.1 ± 7.9 | 64.3 ± 8.4 | 69.1 ± 8.6 | <0.0001 |
| SFA (%TE) | 3.5 ± 2.3 | 5.6 ± 2.5 | 6.7 ± 2.4 | 7.7 ± 2.5 | 8.6 ± 2.8 | <0.0001 | 9.3 ± 3.1 | 7.4 ± 2.3 | 6.4 ± 2.3 | 5.2 ± 2.2 | 3.7 ± 2.0 | <0.0001 |
| PUFA (%TE) | 3.8 (2.4, 6.1) | 4.6 (3.1, 7.3) | 5.5 (3.6, 8.0) | 5.8 (4.1, 8.2) | 6.5 (4.6, 9.3) | <0.0001 | 6.9 (4.6, 10.1) | 5.6 (3.8, 8.0) | 5.0 (3.3, 8.0) | 5.0 (3.0, 7.4) | 4.1 (2.8, 6.2) | <0.0001 |
| MUFA (%TE) | 6.3 ± 3.5 | 9.6 ± 3.6 | 11.9 ± 3.7 | 13.5 ± 3.7 | 14.9 ± 4.5 | <0.0001 | 16.2 ± 4.4 | 13.0 ± 3.4 | 11.1 ± 3.4 | 9.1 ± 3.4 | 6.7 ± 3.4 | <0.0001 |
| Dietary fiber (g/day) | 14.7 (10.9, 18.1) | 12.1 (9.4, 15.2) | 10.5 (8.4, 13.5) | 9.9 (7.9, 12.7) | 9.8 (7.5, 13.2) | <0.0001 | 9.0 (7.0, 11.8) | 9.6 (7.8, 12.3) | 10.4 (8.5, 13) | 12.0 (9.9, 14.8) | 16.1 (13.4, 19.0) | <0.0001 |
| Cholesterol (mg/day) | 25.6 (0.0, 65.4) | 126.8 (79.3, 194.0) | 195.8 (130.4, 286.7) | 258.2 (190.0, 355.7) | 356.2 (269.5, 489.2) | <0.0001 | 295.9 (201.5, 422.7) | 239.7 (154.2, 343.0) | 193.7 (116.7, 292.4) | 135.9 (64.5, 236.3) | 60.0 (11.3, 156.4) | <0.0001 |
| Sodium (mg/day) | 6369 ± 3024 | 6473 ± 2835 | 6094 ± 2843 | 6095 ± 2631 | 6060 ± 2914 | <0.0001 | 6332 ± 3247 | 5955 ± 2470 | 6219 ± 2706 | 6256 ± 2772 | 6327 ± 3012 | 0.240 |
| Calcium (mg/day) | 405.4 ± 173.1 | 411.8 ± 164.4 | 414.0 ± 155.0 | 424.4 ± 162.9 | 494.7 ± 266.4 | <0.0001 | 409.1 ± 189.9 | 413.5 ± 154.8 | 422.7 ± 220.8 | 434.8 ± 167.7 | 470.4 ± 211.0 | <0.0001 |
| Magnesium (mg/day) | 389.2 ± 100.4 | 345.6 ± 78.1 | 325.6 ± 68.0 | 320.6 ± 63.6 | 326.2 ± 69.1 | <0.0001 | 286.5 ± 57.5 | 312.4 ± 52.8 | 329.5 ± 58.6 | 362.5 ± 69.6 | 416.3 ± 91.7 | <0.0001 |
| Potassium (mg/day) | 1786.9 ± 547.4 | 1670.1 ± 450.5 | 1671.8 ± 410.6 | 1734.0 ± 381.4 | 1935.2 ± 483.9 | <0.0001 | 1700.7 ± 446.2 | 1689.5 ± 401.3 | 1698.0 ± 383.5 | 1773.4 ± 409.6 | 1936.2 ± 616.7 | <0.0001 |
| Quintiles of Animal Protein Intake | p for Trend | Quintiles of Plant Protein Intake | p for Trend | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| No. of participants | 1550 | 1550 | 1551 | 1550 | 1551 | 1550 | 1550 | 1551 | 1550 | 1551 | ||
| Age (year) | 38.6 ± 15.3 | 37.3 ± 13.1 | 37.7 ± 13.5 | 37.9 ± 13.7 | 38.5 ± 14.0 | 0.662 | 38.3 ± 14.3 | 37.8 ± 13.5 | 37.7 ± 13.4 | 38 ± 13.6 | 38.3 ± 15.0 | 0.746 |
| BMI (kg/m2) | 21.9 ± 2.9 | 22.0 ± 3.1 | 21.9 ± 3 | 22.1 ± 3.1 | 22.4 ± 3.5 | <0.0001 | 22.2 ± 3.2 | 22.0 ± 3.1 | 21.9 ± 3.2 | 22.0 ± 3.0 | 22.2 ± 3.2 | 0.562 |
| PAL (×BMR) | 1.8 ± 0.2 | 1.7 ± 0.2 | 1.6 ± 0.2 | 1.6 ± 0.2 | 1.5 ± 0.2 | <0.0001 | 1.5 ± 0.2 | 1.6 ± 0.2 | 1.7 ± 0.2 | 1.7 ± 0.2 | 1.7 ± 0.2 | <0.0001 |
| Urban residential area, n (%) | 220 (14.2%) | 365 (23.5%) | 560 (36.1%) | 747 (48.2%) | 1006 (64.9%) | <0.0001 | 888 (57.3%) | 683 (44.1%) | 528 (34.0%) | 452 (29.2%) | 347 (22.4%) | <0.0001 |
| Education level, n (%) | <0.0001 | <0.0001 | ||||||||||
| Low | 1076 (69.4%) | 895 (57.7%) | 680 (43.8%) | 530 (34.2%) | 321 (20.7%) | 402 (25.9%) | 594 (38.3%) | 752 (48.5%) | 831 (53.6%) | 923 (59.5%) | ||
| Medium | 463 (29.9%) | 625 (40.3%) | 794 (51.2%) | 914 (59.0%) | 990 (63.8%) | 950 (61.3%) | 844 (54.5%) | 733 (47.3%) | 677 (43.7%) | 582 (37.5%) | ||
| High | 11 (0.7%) | 30 (1.9%) | 77 (5.0%) | 106 (6.8%) | 240 (15.5%) | 198 (12.8%) | 112 (7.2%) | 66 (4.3%) | 42 (2.7%) | 46 (3.0%) | ||
| Household income level, n (%) | <0.0001 | <0.0001 | ||||||||||
| Low | 875 (56.5%) | 600 (38.7%) | 436 (28.1%) | 256 (16.5%) | 136 (8.8%) | 174 (11.2%) | 329 (21.2%) | 487 (31.4%) | 581 (37.5%) | 732 (47.2%) | ||
| Medium | 426 (27.5%) | 504 (32.5%) | 486 (31.3%) | 456 (29.4%) | 296 (19.1%) | 297 (19.2%) | 471 (30.4%) | 486 (31.3%) | 467 (30.1%) | 447 (28.8%) | ||
| High | 182 (11.7%) | 281 (18.1%) | 374 (24.1%) | 455 (29.4%) | 476 (30.7%) | 484 (31.2%) | 406 (26.2%) | 344 (22.2%) | 303 (19.5%) | 231 (14.9%) | ||
| Very high | 67 (4.3%) | 165 (10.6%) | 255 (16.4%) | 383 (24.7%) | 643 (41.5%) | 595 (38.4%) | 344 (22.2%) | 234 (15.1%) | 199 (12.8%) | 141 (9.1%) | ||
| Ever and current smoker, n (%) | 77 (5.0%) | 69 (4.5%) | 59 (3.8%) | 48 (3.1%) | 36 (2.3%) | <0.0001 | 44 (2.8%) | 49 (3.2%) | 51 (3.3%) | 62 (4.0%) | 83 (5.4%) | 0.0001 |
| Alcohol consumer, n (%) | 152 (9.8%) | 164 (10.6%) | 178 (11.5%) | 201 (13.0%) | 232 (15.0%) | <0.0001 | 220 (14.2%) | 190 (12.3%) | 192 (12.4%) | 166 (10.7%) | 159 (10.3%) | 0.0003 |
| SBP (mm Hg) | 110.1 ± 12.1 | 109.0 ± 12.0 | 110.1 ± 11.9 | 110.1 ± 11.6 | 111.0 ± 12.1 | 0.002 | 110.9 ± 12.1 | 109.7 ± 11.7 | 109.7 ± 11.9 | 109.2 ± 11.8 | 110.6 ± 12.2 | 0.459 |
| TE (kcal/day) | 2221.3 ± 576.1 | 2123.8 ± 515.3 | 2086.9 ± 478.1 | 2042.4 ± 480.9 | 2002.6 ± 532.5 | <0.0001 | 1998.7 ± 549.9 | 2073.4 ± 484.2 | 2105.8 ± 468.6 | 2108.9 ± 516.0 | 2190.0 ± 571.9 | <0.0001 |
| Protein (g/day) | 58.2 ± 8.8 | 59.3 ± 8.0 | 62.1 ± 8.0 | 66.6 ± 7.8 | 78.7 ± 13.4 | <0.0001 | 65.0 ± 15.0 | 64.1 ± 10.8 | 63.2 ± 10.7 | 63.4 ± 10.6 | 69.2 ± 11.5 | <0.0001 |
| Protein (%TE) | 11.1 ± 1.6 | 11.4 ± 1.6 | 12.0 ± 1.6 | 12.9 ± 1.6 | 15.2 ± 2.7 | <0.0001 | 12.6 ± 3.0 | 12.4 ± 2.2 | 12.2 ± 2.2 | 12.2 ± 2.1 | 13.2 ± 2.3 | <0.0001 |
| Animal protein (g/day) | 2.2 (0.0, 4.1) | 9.5 (7.7, 11.2) | 16.5 (14.8, 18.2) | 24.1 (21.9, 26.2) | 35.8 (31.7, 42.9) | <0.0001 | 28.9 (21.6, 37.7) | 21.9 (16.4, 28.7) | 16.4 (10.2, 23.8) | 10.3 (5.3, 17.3) | 4.9 (1.0, 11.1) | <0.0001 |
| Animal protein (%TE) | 0.4 (0.0, 0.8) | 1.8 (1.5, 2.2) | 3.2 (2.8, 3.6) | 4.7 (4.3, 5.2) | 7.2 (6.2, 8.7) | <0.0001 | 5.7 (4.2, 7.6) | 4.3 (3.1, 5.7) | 3.2 (1.9, 4.7) | 2.0 (1, 3.4) | 0.9 (0.2, 2.2) | <0.0001 |
| Plant protein (g/day) | 54.4 ± 9.0 | 47.9 ± 8.2 | 43.6 ± 8.3 | 40.2 ± 7.7 | 36.5 ± 8.8 | <0.0001 | 30.9 ± 4.5 | 38.8 ± 1.5 | 43.8 ± 1.4 | 49.3 ± 1.9 | 59.8 ± 6.5 | <0.0001 |
| Plant protein (%TE) | 10.4 ± 1.7 | 9.2 ± 1.6 | 8.3 ± 1.6 | 7.7 ± 1.5 | 7.0 ± 1.7 | <0.0001 | 5.9 ± 0.9 | 7.4 ± 0.3 | 8.4 ± 0.3 | 9.4 ± 0.4 | 11.5 ± 1.2 | <0.0001 |
| CHO (%TE) | 71.0 ± 7.7 | 63.6 ± 7.8 | 58.9 ± 7.3 | 54.8 ± 7.3 | 49.3 ± 8.7 | <0.0001 | 48.3 ± 8.6 | 56.6 ± 7.2 | 60.5 ± 8.1 | 64.2 ± 8.3 | 68.1 ± 9.1 | <0.0001 |
| SFA (%TE) | 3.6 ± 2.2 | 5.6 ± 2.5 | 6.8 ± 2.2 | 7.8 ± 2.4 | 8.9 ± 2.7 | <0.0001 | 9.4 ± 2.9 | 7.5 ± 2.3 | 6.4 ± 2.2 | 5.4 ± 2.2 | 4.0 ± 2.2 | <0.0001 |
| PUFA (%TE) | 3.9 (2.4, 6.2) | 5.2 (3.4, 8.0) | 5.6 (3.8, 8.1) | 6.1 (4.1, 8.7) | 7.1 (4.9, 9.9) | <0.0001 | 7.3 (4.9, 10.9) | 5.9 (4.0, 8.4) | 5.3 (3.5, 8.3) | 5.2 (3.2, 7.8) | 4.5 (2.9, 6.6) | <0.0001 |
| MUFA (%TE) | 6.6 ± 3.5 | 9.8 ± 3.7 | 12.0 ± 3.6 | 13.6 ± 3.7 | 15.0 ± 4.4 | <0.0001 | 16.3 ± 4.3 | 13.1 ± 3.5 | 11.2 ± 3.4 | 9.3 ± 3.4 | 7.1 ± 3.5 | <0.0001 |
| Dietary fiber (g/day) | 12.9 (9.8, 15.8) | 10.9 (8.5, 13.8) | 9.9 (7.6, 12.4) | 9.2 (7.2, 12.2) | 9.2 (7.1, 12.6) | <0.0001 | 8.4 (6.7, 11.2) | 8.7 (7.0, 11.3) | 9.8 (7.8, 12.2) | 11.2 (9.0, 13.6) | 14.1 (11.8, 16.9) | <0.0001 |
| Cholesterol (mg/day) | 27.6 (4.0, 68.7) | 118.2 (71.4, 181.2) | 179 (118.4, 260.3) | 229.5 (169.6, 322.8) | 333.9 (245.3, 460.9) | <0.0001 | 271.1 (185.6, 387.4) | 212.1 (140.0, 307.8) | 168.2 (100.3, 270.5) | 127.3 (59.9, 218.3) | 64.6 (15.0, 160.7) | <0.0001 |
| Sodium (mg/day) | 5576 ± 2767 | 5540 ± 2500 | 5242 ± 2355 | 5233 ± 2261 | 5221 ± 2328 | <0.0001 | 5352 ± 2632 | 5225 ± 2196 | 5413 ± 2268 | 5435 ± 2451 | 5387 ± 2680 | 0.220 |
| Calcium (mg/day) | 361.7 ± 146.3 | 363.8 ± 141.3 | 375.9 ± 157.9 | 395.9 ± 171.2 | 471.4 ± 214.7 | <0.0001 | 394.9 ± 201.0 | 375.2 ± 145.9 | 383.5 ± 167 | 396.2 ± 162.0 | 419.0 ± 181.6 | <0.0001 |
| Magnesium (mg/day) | 333.4 ± 84.6 | 302.2 ± 65.0 | 288.6 ± 60.7 | 285.2 ± 63.7 | 292.3 ± 64.0 | <0.0001 | 255.4 ± 52.8 | 274.5 ± 49.4 | 294.0 ± 56.1 | 316.2 ± 63.6 | 361.5 ± 74.8 | <0.0001 |
| Potassium (mg/day) | 1544.4 ± 457.3 | 1495.8 ± 383.0 | 1507.4 ± 376.8 | 1584.8 ± 439.6 | 1784.3 ± 467.3 | <0.0001 | 1567.5 ± 451.7 | 1509.3 ± 389.6 | 1551.3 ± 420.6 | 1580.0 ± 391.8 | 1708.5 ± 505.8 | <0.0001 |
| Quintiles of Intake in Men | p for Trend | Quintiles of Intake in Women | p for Trend | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| (n = 1401) | (n = 1401) | (n = 1402) | (n = 1401) | (n = 1402) | (n = 1550) | (n = 1550) | (n = 1551) | (n = 1550) | (n = 1551) | |||
| Animal protein | ||||||||||||
| Median intake (g/day) | 1.9 | 10.7 | 18.9 | 27.4 | 41.0 | 2.2 | 9.5 | 16.5 | 24.1 | 35.8 | ||
| Cases/person-years | 673/13,487 | 529/15,623 | 494/14,584 | 495/14,048 | 395/10,711 | 689/14,309 | 544/17,203 | 456/15,928 | 380/15,207 | 307/11,935 | ||
| Model 1 | 1 (ref) | 0.70 (0.62, 0.78) | 0.68 (0.60, 0.76) | 0.71 (0.63, 0.80) | 0.75 (0.66, 0.85) | <0.0001 | 1 (ref) | 0.69 (0.61, 0.77) | 0.61 (0.54, 0.69) | 0.55 (0.48, 0.62) | 0.57 (0.50, 0.66) | <0.0001 |
| Model 2 | 1 (ref) | 0.68 (0.60, 0.76) | 0.63 (0.55, 0.71) | 0.65 (0.57, 0.74) | 0.66 (0.57, 0.76) | <0.00001 | 1 (ref) | 0.70 (0.62, 0.78) | 0.61 (0.54, 0.69) | 0.53 (0.46, 0.61) | 0.56 (0.47, 0.65) | <0.0001 |
| Model 3 | 1 (ref) | 0.75 (0.66, 0.85) | 0.73 (0.63, 0.84) | 0.77 (0.66, 0.91) | 0.78 (0.65, 0.95) | 0.137 | 1 (ref) | 0.80 (0.70, 0.90) | 0.75 (0.65, 0.87) | 0.70 (0.59, 0.83) | 0.76 (0.62, 0.93) | 0.010 |
| Plant protein | ||||||||||||
| Median intake (g/day) | 37.0 | 44.8 | 50.5 | 57.1 | 67.7 | 32.1 | 38.9 | 43.7 | 49.2 | 58.4 | ||
| Cases/person-years | 408/10,205 | 483/15,082 | 496/15,481 | 559/14,678 | 640/13,007 | 280/11,574 | 403/16,187 | 490/16,922 | 554/16,223 | 649/13,676 | ||
| Model 1 | 1 (ref) | 0.86 (0.76, 0.99) | 0.84 (0.73, 0.96) | 1.07 (0.93, 1.22) | 1.29 (1.13, 1.46) | <0.0001 | 1 (ref) | 1.01 (0.86, 1.18) | 1.12 (0.97, 1.31) | 1.34 (1.16, 1.56) | 1.80 (1.55, 2.08) | <0.0001 |
| Model 2 | 1 (ref) | 0.88 (0.77, 1.01) | 0.87 (0.76, 1.00) | 1.11 (0.97, 1.28) | 1.36 (1.19, 1.56) | <0.0001 | 1 (ref) | 0.98 (0.84, 1.15) | 1.08 (0.92, 1.26) | 1.33 (1.14, 1.55) | 1.71 (1.46, 1.99) | <0.0001 |
| Model 3 | 1 (ref) | 0.83 (0.72, 0.95) | 0.78 (0.67, 0.91) | 0.93 (0.79, 1.10) | 1.11 (0.91, 1.36) | 0.031 | 1 (ref) | 0.89 (0.76, 1.05) | 0.92 (0.77, 1.08) | 1.07 (0.89, 1.28) | 1.29 (1.04, 1.59) | 0.0003 |
| Total protein | ||||||||||||
| Median intake (g/day) | 60.0 | 67.6 | 73.4 | 79.4 | 90.5 | 52.1 | 58.7 | 63.4 | 68.8 | 79.3 | ||
| Cases/person-years | 540/12,887 | 531/15,563 | 552/16,146 | 516/13,799 | 447/10,058 | 514/14,132 | 522/17,435 | 514/17,042 | 469/15,248 | 357/10,725 | ||
| Model 1 | 1 (ref) | 0.84 (0.74, 0.95) | 0.85 (0.75, 0.95) | 0.92 (0.82, 1.04) | 1.11 (0.97, 1.26) | 0.050 | 1 (ref) | 0.82 (0.73, 0.93) | 0.81 (0.72, 0.92) | 0.85 (0.75, 0.97) | 0.95 (0.83, 1.09) | 0.590 |
| Model 2 | 1 (ref) | 0.81 (0.72, 0.92) | 0.85 (0.75, 0.96) | 0.92 (0.81, 1.04) | 1.08 (0.94, 1.23) | 0.095 | 1 (ref) | 0.85 (0.75, 0.96) | 0.85 (0.75, 0.97) | 0.88 (0.78, 1.01) | 1.02 (0.88, 1.18) | 0.773 |
| Model 3 | 1 (ref) | 0.80 (0.71, 0.90) | 0.81 (0.72, 0.92) | 0.87 (0.76, 0.99) | 0.97 (0.84, 1.13) | 0.832 | 1 (ref) | 0.85 (0.75, 0.96) | 0.83 (0.73, 0.95) | 0.85 (0.74, 0.98) | 0.97 (0.83, 1.14) | 0.692 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
He, J.; Yu, S.; Fang, A.; Shen, X.; Li, K. Association between Protein Intake and the Risk of Hypertension among Chinese Men and Women: A Longitudinal Study. Nutrients 2022, 14, 1276. https://doi.org/10.3390/nu14061276
He J, Yu S, Fang A, Shen X, Li K. Association between Protein Intake and the Risk of Hypertension among Chinese Men and Women: A Longitudinal Study. Nutrients. 2022; 14(6):1276. https://doi.org/10.3390/nu14061276
Chicago/Turabian StyleHe, Jingjing, Siwang Yu, Aiping Fang, Xin Shen, and Keji Li. 2022. "Association between Protein Intake and the Risk of Hypertension among Chinese Men and Women: A Longitudinal Study" Nutrients 14, no. 6: 1276. https://doi.org/10.3390/nu14061276
APA StyleHe, J., Yu, S., Fang, A., Shen, X., & Li, K. (2022). Association between Protein Intake and the Risk of Hypertension among Chinese Men and Women: A Longitudinal Study. Nutrients, 14(6), 1276. https://doi.org/10.3390/nu14061276





