A Positive Impact of an Observational Study on Breastfeeding Rates in Two Neonatal Intensive Care Units
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Setting, and Participants
2.2. The Doal Study
2.3. Breastfeeding Policies in the Participating NICUs
2.4. Breastfeeding Outcomes
2.5. Data Collection
2.6. Statistical Analysis
2.7. Ethics
3. Results
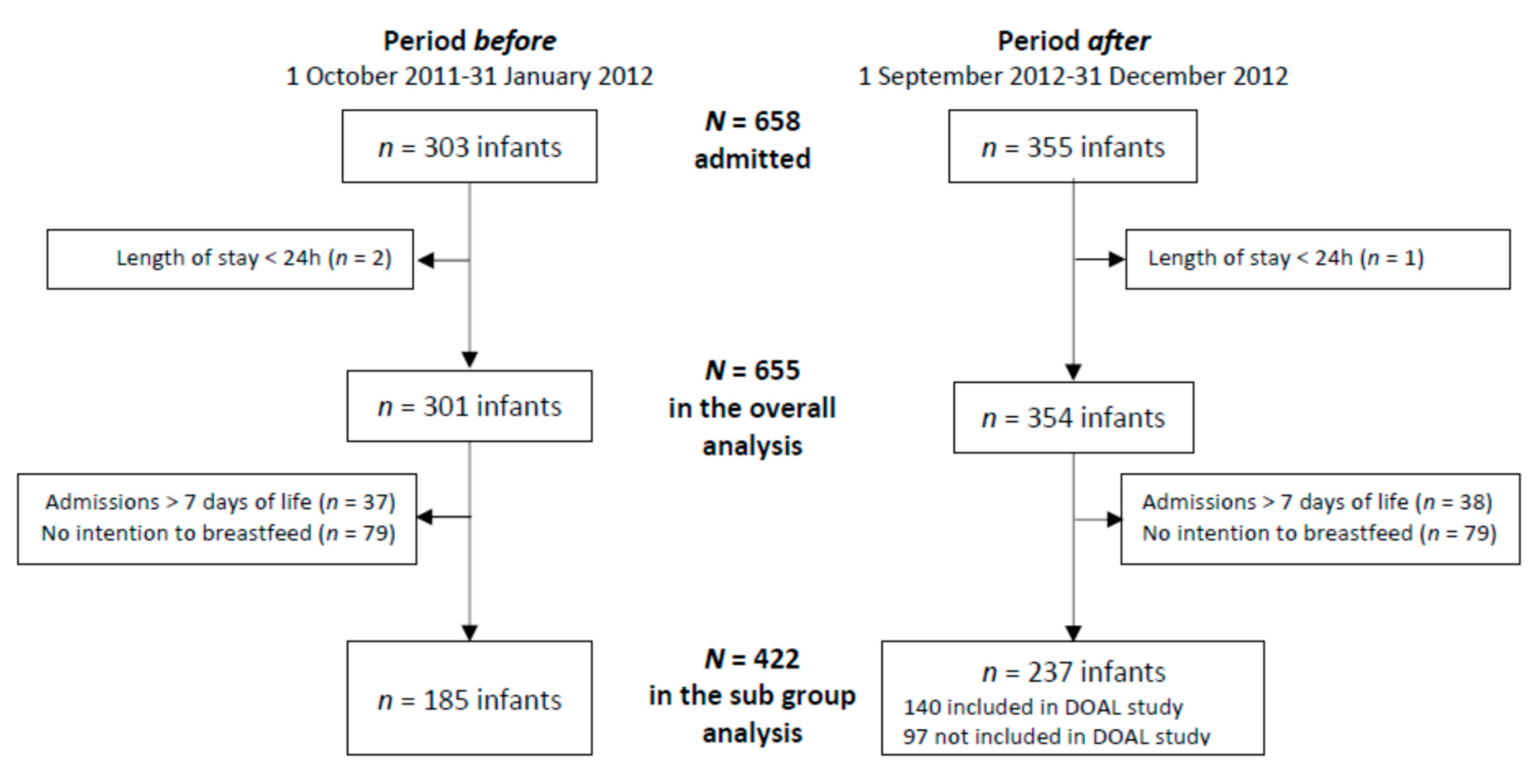
3.1. Population
3.2. Breastfeeding Outcomes in the Total Population According to the Period
3.2.1. Any Breastfeeding
3.2.2. Exclusive Breastfeeding
3.2.3. Breastfeeding Intention
3.3. Breastfeeding Outcomes According to Doal Inclusion Status
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Moro, G.E.; Arslanoglu, S.; Bertino, E.; Corvaglia, L.; Montirosso, R.; Picaud, J.-C.; Polberger, S.; Schanler, R.J.; Steel, C.; van Goudoever, J.; et al. XII. Human Milk in Feeding Premature Infants: Consensus Statement. J. Pediatr. Gastroenterol. Nutr. 2015, 61, S16–S19. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Shukla, V.V.; John, D.; Chen, C. Human Milk Feeding as a Protective Factor for Retinopathy of Prematurity: A Meta-Analysis. Pediatrics 2015, 136, e1576–e1586. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Villamor-Martínez, E.; Pierro, M.; Cavallaro, G.; Mosca, F.; Villamor, E. Mother’s Own Milk and Bronchopulmonary Dysplasia: A Systematic Review and Meta-Analysis. Front. Pediatr. 2019, 7, 224. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.; Tonkin, E.; Damarell, R.A.; McPhee, A.J.; Suganuma, M.; Suganuma, H.; Middleton, P.F.; Makrides, M.; Collins, C.T. A Systematic Review and Meta-Analysis of Human Milk Feeding and Morbidity in Very Low Birth Weight Infants. Nutrients 2018, 10, E707. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Altobelli, E.; Angeletti, P.M.; Verrotti, A.; Petrocelli, R. The Impact of Human Milk on Necrotizing Enterocolitis: A Systematic Review and Meta-Analysis. Nutrients 2020, 12, 1322. [Google Scholar] [CrossRef] [PubMed]
- Lucas, A.; Morley, R.; Cole, T.J.; Lister, G.; Leeson-Payne, C. Breast Milk and Subsequent Intelligence Quotient in Children Born Preterm. Lancet 1992, 339, 261–264. [Google Scholar] [CrossRef]
- Vohr, B.; McGowan, E.; McKinley, L.; Tucker, R.; Keszler, L.; Alksninis, B. Differential Effects of the Single-Family Room Neonatal Intensive Care Unit on 18- to 24-Month Bayley Scores of Preterm Infants. J. Pediatr. 2017, 185, 42–48.e1. [Google Scholar] [CrossRef]
- Vohr, B.R.; Poindexter, B.B.; Dusick, A.M.; McKinley, L.T.; Higgins, R.D.; Langer, J.C.; Poole, W.K.; for the National Institute of Child Health and Human Development National Research Network. Persistent Beneficial Effects of Breast Milk Ingested in the Neonatal Intensive Care Unit on Outcomes of Extremely Low Birth Weight Infants at 30 Months of Age. Pediatrics 2007, 120, e953–e959. [Google Scholar] [CrossRef] [Green Version]
- Merewood, A.; Brooks, D.; Bauchner, H.; MacAuley, L.; Mehta, S.D. Maternal Birthplace and Breastfeeding Initiation Among Term and Preterm Infants: A Statewide Assessment for Massachusetts. Pediatrics 2006, 118, e1048–e1054. [Google Scholar] [CrossRef]
- Bonet, M.; Blondel, B.; Agostino, R.; Combier, E.; Maier, R.F.; Cuttini, M.; Khoshnood, B.; Zeitlin, J.; MOSAIC research group. Variations in Breastfeeding Rates for Very Preterm Infants between Regions and Neonatal Units in Europe: Results from the MOSAIC Cohort. Arch. Dis. Child.-Fetal Neonatal Ed. 2011, 96, F450–F452. [Google Scholar] [CrossRef]
- Bonnet, C.; Blondel, B.; Piedvache, A.; Wilson, E.; Bonamy, A.E.; Gortner, L.; Rodrigues, C.; Heijst, A.; Draper, E.S.; Cuttini, M.; et al. Low Breastfeeding Continuation to 6 Months for Very Preterm Infants: A European Multiregional Cohort Study. Matern. Child Nutr. 2019, 15, e12657. [Google Scholar] [CrossRef] [PubMed]
- Maastrup, R.; Bojesen, S.N.; Kronborg, H.; Hallström, I. Breastfeeding Support in Neonatal Intensive Care: A National Survey. J. Hum. Lact. 2012, 28, 370–379. [Google Scholar] [CrossRef] [PubMed]
- Nyqvist, K.H.; Häggkvist, A.-P.; Hansen, M.N.; Kylberg, E.; Frandsen, A.L.; Maastrup, R.; Ezeonodo, A.; Hannula, L.; Haiek, L.N. Expansion of the Baby-Friendly Hospital Initiative Ten Steps to Successful Breastfeeding into Neonatal Intensive Care: Expert Group Recommendations. J. Hum. Lact. 2013, 29, 300–309. [Google Scholar] [CrossRef] [PubMed]
- McCambridge, J.; Witton, J.; Elbourne, D.R. Systematic Review of the Hawthorne Effect: New Concepts Are Needed to Study Research Participation Effects. J. Clin. Epidemiol. 2014, 67, 267–277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roethlisberger, F.J.; Dickson, W.J. Management and the Worker; Harvard University Press: Cambridge, MA, USA, 1939. [Google Scholar]
- Srigley, J.A.; Furness, C.D.; Baker, G.R.; Gardam, M. Quantification of the Hawthorne Effect in Hand Hygiene Compliance Monitoring Using an Electronic Monitoring System: A Retrospective Cohort Study. BMJ Qual. Saf. 2014, 23, 974–980. [Google Scholar] [CrossRef] [Green Version]
- Gould, D.; Lindström, H.; Purssell, E.; Wigglesworth, N. Electronic Hand Hygiene Monitoring: Accuracy, Impact on the Hawthorne Effect and Efficiency. J. Infect. Prev. 2020, 21, 136–143. [Google Scholar] [CrossRef]
- Hagel, S.; Reischke, J.; Kesselmeier, M.; Winning, J.; Gastmeier, P.; Brunkhorst, F.M.; Scherag, A.; Pletz, M.W. Quantifying the Hawthorne Effect in Hand Hygiene Compliance Through Comparing Direct Observation With Automated Hand Hygiene Monitoring. Infect. Control. Hosp. Epidemiol. 2015, 36, 957–962. [Google Scholar] [CrossRef] [Green Version]
- Robinson, E.; Hardman, C.A.; Halford, J.C.; Jones, A. Eating under Observation: A Systematic Review and Meta-Analysis of the Effect That Heightened Awareness of Observation Has on Laboratory Measured Energy Intake. Am. J. Clin. Nutr. 2015, 102, 324–337. [Google Scholar] [CrossRef] [Green Version]
- Fischer Fumeaux, C.J.; Denis, A.; Prudon, M.B.; Plaisant, F.; Essomo Megnier-Mbo, C.M.; Fernandes, L.; Touzet, S.; Claris, O.; Laborie, S. Early Use of Mother’s Own Raw Milk, Maternal Satisfaction, and Breastfeeding Continuation in Hospitalised Neonates: A Prospective Cohort Study. Neonatology 2018, 113, 131–139. [Google Scholar] [CrossRef]
- Coombs, S.J.; Smith, I.D. The Hawthorne Effect: Is It a Help or Hindrance in Social Science Research? Change Transform. Educ. 2003, 6, 97–111. [Google Scholar]
- Haas, J.P.; Larson, E.L. Measurement of Compliance with Hand Hygiene. J. Hosp. Infect. 2007, 66, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Cizza, G.; Piaggi, P.; Rother, K.I.; Csako, G.; for the Sleep Extension Study Group. Hawthorne Effect with Transient Behavioral and Biochemical Changes in a Randomized Controlled Sleep Extension Trial of Chronically Short-Sleeping Obese Adults: Implications for the Design and Interpretation of Clinical Studies. PLoS ONE 2014, 9, e104176. [Google Scholar] [CrossRef] [PubMed]
- Campino, A.; Lopez-Herrera, M.C.; Lopez-de-Heredia, I.; Valls-i-Soler, A. Medication Errors in a Neonatal Intensive Care Unit. Influence of Observation on the Error Rate. Acta Paediatr. 2008, 97, 1591–1594. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.F.; Vander Weg, M.W.; Hofmann, D.A.; Reisinger, H.S. The Hawthorne Effect in Infection Prevention and Epidemiology. Infect. Control Hosp. Epidemiol. 2015, 36, 1444–1450. [Google Scholar] [CrossRef]
- Kohli, E.; Ptak, J.; Smith, R.; Taylor, E.; Talbot, E.A.; Kirldand, K.B. Variability in the Hawthorne Effect With Regard to Hand Hygiene Performance in High- and Low-Performing Inpatient Care Units. Infect. Control Hosp. Epidemiol. 2009, 30, 222–225. [Google Scholar] [CrossRef]
- Auerbach, A.D.; Landefeld, C.S.; Shojania, K.G. The Tension between Needing to Improve Care and Knowing How to Do It. N. Engl. J. Med. 2007, 357, 608–613. [Google Scholar] [CrossRef] [Green Version]
- Toma, M.; Dreischulte, T.; Gray, N.M.; Guthrie, B. A Balanced Approach to Identifying, Prioritising and Evaluating All Potential Consequences of Quality Improvement: Modified Delphi Study. BMJ Open 2019, 9, e023890. [Google Scholar] [CrossRef] [Green Version]
- Rosenberg, M.; Pettifor, A.; Twine, R.; Hughes, J.P.; Gomez-Olive, F.X.; Wagner, R.G.; Sulaimon, A.; Tollman, S.; Selin, A.; MacPhail, C.; et al. Evidence for Sample Selection Effect and Hawthorne Effect in Behavioural HIV Prevention Trial among Young Women in a Rural South African Community. BMJ Open 2018, 8, e019167. [Google Scholar] [CrossRef]
- Kwok, Y.L.A.; Juergens, C.P.; McLaws, M.-L. Automated Hand Hygiene Auditing with and without an Intervention. Am. J. Infect. Control 2016, 44, 1475–1480. [Google Scholar] [CrossRef]
- McLaws, M.-L.; Kwok, Y.L.A. Hand Hygiene Compliance Rates: Fact or Fiction? Am. J. Infect. Control 2018, 46, 876–880. [Google Scholar] [CrossRef]
- Wu, K.-S.; Lee, S.S.-J.; Chen, J.-K.; Chen, Y.-S.; Tsai, H.-C.; Chen, Y.-J.; Huang, Y.-H.; Lin, H.-S. Identifying Heterogeneity in the Hawthorne Effect on Hand Hygiene Observation: A Cohort Study of Overtly and Covertly Observed Results. BMC Infect. Dis. 2018, 18, 369. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Period Before n = 301 | Period After n = 354 | p-Value |
|---|---|---|---|
| NICU, n (%) | 0.061 | ||
| Center A | 236 (78.4) | 255 (72.0) | |
| Center B | 65 (21.6) | 99 (28.0) | |
| Maternal age (years), mean (SD) | 30.5 (5.5) | 30.8 (5.4) | 0.498 |
| Parity, mean (SD) | 2.1 (1.1) | 2.2 (1.1) | 0.195 |
| Smoking, n (%) | 0.212 | ||
| No | 153 (50.8) | 223 (63.0) | |
| Yes | 53 (17.6) | 59 (16.7) | |
| Missing data | 95 (31.6) | 72 (20.3) | |
| Male, n (%) | 160 (53.2) | 199 (56.2) | 0.433 |
| Gestational age (weeks), median (range) | 34.6 (24.1–42) | 34.6 (25.6–42.1) | 0.808 |
| Birth weight (g), median (range) | 2050 (490–4320) | 2100 (530–5270) | 0.401 |
| Multiple births, n (%) | 65 (21.6) | 96 (27.1) | 0.102 |
| Outcome at discharge, n (%) | 0.851 | ||
| Home | 175 (58.1) | 202 (57.1) | |
| Other hospital | 118 (39.2) | 140 (39.5) | |
| Death | 8 (2.7) | 12 (3.4) | |
| Length of stay (days), median (range) | 13 (1–144) | 14 (1–143) | 0.729 |
| Characteristics | Any Breastfeeding | Exclusive Breastfeeding | ||
|---|---|---|---|---|
| ORcrude [95%CI] | p-Value | ORcrude [95%CI] | p-Value | |
| Period after (ref: period before) | 1.03 [0.75; 1.40] | 0.8753 | 1.62 [1.05; 2.52] | 0.0310 |
| NICU (ref: center A) | 1.11 [0.78; 1.59] | 0.5611 | 0.52 [0.30; 0.92] | 0.0253 |
| Maternal age (+1 year) | 1.01 [0.98; 1.04] | 0.5817 | 1.00 [0.96; 1.04] | 0.8865 |
| Smoking (ref: no) | 0.47 [0.31; 0.72] | 0.0005 | 0.87 [0.49; 1.56] | 0.6456 |
| Parity (+1 infant) | 0.92 [0.80; 1.05] | 0.2158 | 0.83 [0.68; 1.03] | 0.0871 |
| Sex (ref: male) | 1.03 [0.75; 1.41] | 0.8668 | 1.04 [0.68; 1.59] | 0.8598 |
| Gestational age (+1 week) | 1.08 [1.03; 1.12] | 0.0003 | 1.00 [0.95; 1.06] | 0.9577 |
| Birth weight (+100 g) | 1.03 [1.01; 1.05] | 0.0028 | 1.00 [0.97; 1.02] | 0.7773 |
| Multiple gestation (ref: no) | 1.14 [0.79; 1.64] | 0.4968 | 0.49 [0.28; 0.88] | 0.0174 |
| Length of stay (+7 days) | 0.96 [0.91; 1.00] | 0.0552 | 1.06 [1.00; 1.12] | 0.0498 |
| Outcome at discharge (ref: Home): | ||||
| Other hospital | 1.02 [0.74; 1.41] | 0.8995 | 0.52 [0.32; 0.82] | 0.0056 |
| Death | 0.53 [0.21; 1.31] | 0.1675 | 0 [0; infinity] | 0.9996 |
| Period Before | Period After | |||
|---|---|---|---|---|
| Characteristics | n = 185 | Study Patients n = 140 | Non-Study NICU Patients n = 97 | p-Value |
| NICU, n (%) | 0.086 | |||
| Center A | 154 (83.2) | 104 (74.3) | 72 (74.2) | |
| Center B | 31 (16.8) | 36 (25.7) | 25 (25.8) | |
| Maternal age (years), mean (SD) | 30 (5.1) | 31.2 (5.5) | 31 (5) | 0.104 |
| Parity, mean (SD) | 2 (1.1) | 2.3 (1.1) | 2.1 (1.2) | 0.057 |
| Smoking, n (%) | 26 (14.1) | 21 (15) | 15 (15.5) | 0.420 |
| Male, n (%) | 104 (56.2) | 77 (55) | 49 (50.5) | 0.652 |
| Gestational age (weeks), median (range) | 35.0 (25.3–41.3) | 33.8 (27.0–42.1) | 37.0 (26.9–41.9) | <10−3 |
| Birth weight (g), median (range) | 2100 (514–4320) | 1935 (594–5270) | 2800 (685–4300) | <10−3 |
| Multiple birth, n (%) | 41 (22.2) | 51 (36.4) | 12 (12.4) | <10−3 |
| Outcome at discharge, n (%) | <10−3 | |||
| Home | 113 (61.1) | 111 (79.3) | 27 (27.8) | |
| Other hospital | 70 (37.8) | 29 (20.7) | 64 (66) | |
| Death | 2 (1.1) | 0 (0) | 6 (6.2) | |
| Length of stay (days), median (range) | 14 (1–144) | 31 (2–102) | 5 (1–127) | <10−3 |
| Any Breastfeeding | Exclusive Breastfeeding | |||
|---|---|---|---|---|
| Characteristics | ORcrude [95%CI] | p-Value | ORcrude [95%CI] | p-Value |
| Study period (ref before) | 1.02 [0.75; 1.40] | 0.8966 | 1.64 [1.00; 2.67] | 0.0496 |
| Study group (ref before) | 0.0560 † | 0.0041 † | ||
| After included | 0.55 [0.3; 0.99] | 0.0444 | 2.21 [1.30; 3.77] | 0.0034 |
| After not included | 1.17 [0.54; 2.49] | 0.6930 | 0.95 [0.48; 1.86] | 0.8698 |
| Maternal age (+1 year) | 1.01 [0.96; 1.06] | 0.7198 | 1.00 [0.95; 1.04] | 0.9445 |
| Smoking (ref No) | 0.64 [0.32; 1.28] | 0.2036 | 1.13 [0.59; 2.16] | 0.7110 |
| Parity (+1 child) | 0.95 [0.76; 1.19] | 0.6559 | 0.87 [0.70; 1.08] | 0.2176 |
| Sex (ref male) | 0.9 [0.53; 1.53] | 0.6993 | 1.02 [0.64; 1.64] | 0.9197 |
| Gestational age (+1 week) | 1.25 [1.16; 1.35] | <0.0001 | 1.02 [0.96; 1.08] | 0.5326 |
| Birth weight (+100 g) | 1.1 [1.06; 1.14] | <0.0001 | 1.00 [0.98; 1.03] | 0.8789 |
| Multiple birth | 0.83 [0.46; 1.5] | 0.5357 | 0.42 [0.22; 0.81] | 0.0099 |
| Length of stay (+7 days) | 0.81 [0.76; 0.87] | <0.0001 | 1.03 [0.96; 1.09] | 0.4152 |
| Outcome at discharge (ref: home) | 0.0144 † | 0.0433 | ||
| Other hospital | 2.33 [1.26; 4.32] | 0.0071 | 0.52 [0.31; 0.87] | 0.0122 |
| Death | 0.71 [0.14; 3.62] | 0.6798 | 0 | 0.9997 |
| Center (reference A) | 0.88 [0.46; 1.7] | 0.7024 | 0.45 [0.23; 0.90] | 0.0228 |
| Characteristics | Any Breastfeeding | Exclusive Breastfeeding | ||
|---|---|---|---|---|
| ORadjusted [95% CI] | p-Value * | ORadjusted [95% CI] | p-Value | |
| Period (ref: period before) | 0.2073 | <0.0001 | ||
| Period after not included | 0.61 [0.40; 0.92] | 0.0193 | 0.90 [0.59; 1.39] | 0.6438 |
| Period after included | 0.57 [0.24; 1.36] | 0.2073 | 2.84 [2.16; 3.73] | <0.0001 |
| Sex (ref: male) | 1.13 [1.01; 1.26] | 0.0302 | ||
| Multiple birth | 1.42 [0.90; 2.24] | 0.1349 | 0.30 [0.29; 0.30] | <0.0001 |
| Smoking | 0.42 [0.40; 0.44] | <0.0001 | ||
| Gestational age (+1 week) | 1.18 [1.11; 1.25] | <0.0001 | ||
| Length of stay (+7 days) | 0.90 [0.89; 0.92] | <0.0001 | ||
| Outcome at discharge (ref: Home) | 0.0010 | |||
| Other health structure | 2.18 [1.37; 3.47] | 0.0010 | ||
| Death | 0.60 [0.53; 0.68] | <0.0001 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Laborie, S.; Abadie, G.; Denis, A.; Touzet, S.; Fischer Fumeaux, C.J. A Positive Impact of an Observational Study on Breastfeeding Rates in Two Neonatal Intensive Care Units. Nutrients 2022, 14, 1145. https://doi.org/10.3390/nu14061145
Laborie S, Abadie G, Denis A, Touzet S, Fischer Fumeaux CJ. A Positive Impact of an Observational Study on Breastfeeding Rates in Two Neonatal Intensive Care Units. Nutrients. 2022; 14(6):1145. https://doi.org/10.3390/nu14061145
Chicago/Turabian StyleLaborie, Sophie, Géraldine Abadie, Angélique Denis, Sandrine Touzet, and Céline J. Fischer Fumeaux. 2022. "A Positive Impact of an Observational Study on Breastfeeding Rates in Two Neonatal Intensive Care Units" Nutrients 14, no. 6: 1145. https://doi.org/10.3390/nu14061145
APA StyleLaborie, S., Abadie, G., Denis, A., Touzet, S., & Fischer Fumeaux, C. J. (2022). A Positive Impact of an Observational Study on Breastfeeding Rates in Two Neonatal Intensive Care Units. Nutrients, 14(6), 1145. https://doi.org/10.3390/nu14061145






