Abstract
Background: Obesity is a growing epidemic among university students, and the high levels of stress reported by this population could contribute to this issue. Singular relationships between perceived stress; engagement in restrained, uncontrolled, and emotional eating; sleep; dietary risk; and body mass index (BMI) have been reported in the current body of literature; however, these constructs interact with each other, and the complex relationships among them are infrequently examined. Therefore, the aim of the present study was to explore the complex relationships between these constructs using mediation and moderation analyses stratified by gender. Methods: A cross-sectional study, enrolling university students from the United States (U.S.), the Netherlands, South Korea, Malaysia, Ireland, Ghana, and China, was conducted between October 2020 and January 2021 during the COVID-19 pandemic. Perceived stress; maladaptive eating behaviors including restrained, uncontrolled, and emotional eating; sleep duration and quality; dietary risk; and BMI were assessed using validated questionnaires, which were distributed through an online platform. Results: A total of 1392 students completed the online survey (379 male, 973 female, and 40 who self-identified as “other”). Uncontrolled and emotional eating mediated the relationship between perceived stress and dietary risk for both males and females; higher sleep quality weakened this relationship among female students but not males. Emotional eating mediated the relationship between perceived stress and BMI for both males and females, but higher sleep quality weakened this relationship only among females. Conclusions: Our findings suggest that students in higher education are likely to benefit from interventions to reduce uncontrolled and emotional eating. Programs that improve sleep quality, especially during highly stressful periods, may be helpful.
Keywords:
restrained eating; uncontrolled eating; emotional eating; obesity; sleep; diet; college; COVID-19; international 1. Introduction
One in four university students are either overweight or obese worldwide [1]. Factors associated with excess adiposity among university students include, but are not limited to, dietary behaviors, poorer mental health [2], and high levels of stress [3,4,5]. These weight-gain promoting factors often co-exist [6,7,8]; for example, higher stress is associated with less healthy eating behaviors, such as higher energy intake [9], higher fat intake [10,11], more frequent consumption of sweets [12], and lower fruit and vegetable intake [13]. Conversely, an interventional study demonstrated a temporal relationship between stress and dietary choices, where decreased perceived stress through a stress management intervention reduced sweet snack intake [14]. Due to the complex nature of the relationships between stress and dietary behaviors, examining singular relationships between one independent and dependent variable can lead to an overly simplistic understanding of how these variables interact.
Further adding to the complexity of the relationships between weight status, dietary intake, and stress, a number of cognitive factors are also known to contribute to weight gain, and these can also be influenced by stress [15,16,17,18]. Three of these factors, restrained, uncontrolled, and emotional eating [19], are measured by the Three Factor Eating Questionnaire (TFEQ) [20]. These factors are also referred to as maladaptive eating behaviors [20]. Restrained eating refers to consciously avoiding or limiting the intake of certain foods [21,22,23], often with a goal to reduce body weight [24]. Restrained eating often leads to binge eating [25], as the act of dieting makes individuals vulnerable to disinhibition, which can result in overeating [23]. Uncontrolled eating can be described as a loss of control when eating certain foods [26], whereas emotional eating often refers to an over-consumption of food while experiencing negative emotions [27]. Females are reported to be more vulnerable to restrained, uncontrolled, and emotional eating behaviors [28,29,30,31]. These behaviors increase the risk of engaging in eating unhealthy foods, defined in this study and others as dietary risk [32,33], and promote weight gain [32,34]. Numerous studies indicate that individuals with restrained, uncontrolled, and emotional eating tend to overeat foods that are not consistent with health [35,36,37]. Additionally, individuals who frequently engage in restrained, uncontrolled, and emotional eating have a higher body mass index (BMI) compared to those who do not or who have low engagement with these behaviors [32,34,38]. Thus, the literature suggests temporal relationships between maladaptive eating behaviors, dietary risk, and BMI. More specifically, restrained, uncontrolled, and emotional eating can negatively influence dietary risk and weight status.
As stated above, perceived stress, described as the subjective perception of stress [39], is known to influence restrained, uncontrolled, and emotional eating behaviors [15,18,40]. Increases in perceived stress can induce restrained eating [40]. Stress can lead to a loss of control when eating, especially when eating hyperpalatable foods such as high-fat and sugary foods [18]. Additionally, higher perceived stress is associated with emotional eating [41], and the interaction between stress and emotional eating has a negative effect on BMI [15,42]. Taken together, this evidence suggests that higher levels of perceived stress could increase the frequency of engaging in maladaptive eating behaviors, including emotional, uncontrolled, and restrained eating. Given the temporal relationship between perceived stress and maladaptive eating behaviors, and the causal relationships between these behaviors and dietary risk and weight status [32,34,36], these maladaptive eating behaviors could mediate the relationships between perceived stress, dietary risk, and BMI.
Higher quality and adequate sleep are associated with lower stress [43,44], less frequent engagement in maladaptive eating behaviors identified by the TFEQ [45,46], lower dietary risk [47,48,49], and lower BMI [50,51]; therefore, sleep quality and duration could potentially moderate the relationships between these factors. Relationships between stress and sleep are bidirectional; that is, high levels of stress lead to shortened and poor sleep [52,53], and inadequate and poor sleep can exacerbate stress [54]. In terms of the relationships between stress and eating behaviors, previous work indicated that poor sleep quality is associated with increased frequency in emotional eating, and short sleep (<7 h per night) is associated with higher energy intake in emotional eaters [45]. Additionally, poor sleep quality and short sleep duration may induce stress and further exacerbate these maladaptive eating behaviors [45,46]. Moreover, the current body of literature has established associations between poor and inadequate sleep and higher BMI [50,51]. Given the evidence demonstrating the associations between sleep and stress, eating behaviors, dietary risks, and BMI, sleep could serve as a moderator of these relationships.
Previous studies examined the relationships between perceived stress, eating behaviors, dietary risk, BMI, and sleep in singular relationships; however, these factors interact with each other and should be examined in a more comprehensive manner. Therefore, the aim of the present study was to characterize the complex relationships between these factors using mediation and moderation analysis. Males and females appear to experience differences in terms of the degree and frequency of restrained, uncontrolled, and emotional eating [28,29,30,31]; thus, they were analyzed separately. Our hypotheses were: (1) maladaptive eating behaviors, including restrained eating, uncontrolled eating, and emotional eating, would mediate the relationships between perceived stress and dietary risk and perceived stress and BMI, and that the mediators could differ by gender; and (2) sleep quality and duration would moderate the relationship between perceived stress and dietary risk and perceived stress and BMI, and that the degree of moderation could differ by gender.
2. Materials and Methods
2.1. Study Design
Undergraduate and graduate students from universities in the United States (U.S.), the Netherlands, South Korea, Malaysia, Ireland, Ghana, and China were recruited. Only students who were at least 18 years old were included in the study. The study took place in late October 2020 to January 2021. Electronic surveys were used to collect information (see below), and were distributed via online platforms. All of the surveys were administered in English. During the data collection, Malaysia, South Korea, the Netherlands, and the U.S. had shelter-in-place orders, but China, Ghana, and Ireland did not. The study was approved by the Michigan State University Human Research Protection Program (East Lansing, MI, USA), STUDY00004285, 7 April 2020; Indiana University of Pennsylvania Institutional Review Board for the Protection of Human Subjects (Indiana, PA, USA), IRB Log 20-101, 26 October 2020; Bowling Green State University Office of Research Compliance (Bowling Green, OH, USA), 1,599,753 (US students), 29 April 2020; 1,599,753 (Chinese students), 22 May 2020; 1,599,753 (Korean students), 11 May 2020; Faculty of Governance and Global Affairs Ethics Committee (The Hague, South Holland, Netherlands), 2020-009-LUC-Cho, 25 May 2020; International Medical University Joint Committee on Research and Ethics (Kuala Lumpur, Malaysia), 481/2020, 14 May 2020; Institute Research Ethics Committee, Institute of Technology, Sligo (Sligo, Ireland), ref 2020015, 7 October 2020; and Kwame Nkrumah University of Science and Technology Committee on Human Research Publication and Ethics (School of Medical Sciences), CHRPE/AP/389/20, 30 October 2020. All participants consented to the study before filling out the online questionnaire.
2.2. Demographics and Biological Information
Age, gender, citizenship status (international vs. domestic), class status (undergraduate vs. graduate), and weight and height were all self-reported. Students who self-identified as neither male nor female were grouped as “other”, which included choices of transgender, genderqueer, additional gender category/other, or choose not to disclose. Race was collected only in the U.S. and Malaysia, and ethnicity was only collected in the U.S., as race and ethnicity diversification is more prevalent in these countries. Graduate status was defined as students who were pursuing masters, doctoral, or professional degrees; this information was collected because differences in stress [55], dietary risks [56], and BMI [57] between undergraduate and graduate students have been reported. International status was determined when students were attending universities outside of their home country. International status was collected as a covariate because it has been associated with the exposure (stress) and outcome variables (dietary risk and BMI) examined [58]. Self-reported weight and height were used to calculate body mass index (BMI).
2.3. Evaluation of Perceived Stress
The Perceived Stress Scale 10 (PSS-10) was used to assess perceived stress [39]. The questionnaire includes 10 questions, with four responses for each question ranging from 0 (never) to 4 (very often). One example question is, “In the last month, how often have you felt nervous and stressed?” The higher the total score, the more perceived stress there is. The highest possible PSS-10 score is 40 while the lowest is 0 [39].
2.4. Evaluation of Dietary Risk
The Starting the Conversation (STC) questionnaire was used to evaluate dietary risk [59]. This survey is a simplified food frequency questionnaire. The STC includes 8 questions that measure the consumption frequency of healthy foods (fruit, vegetables, and high-quality proteins) and unhealthy foods (chips, crackers, fast foods, desserts, solid fats, soda and sweet tea). One sample question is, “How many times a week did you eat regular snack chips or crackers (not low-fat)?” The possible answers include 1 time or less (0), 2 to 3 times (1), and 4 or more times (2). A global score ranging from 0 to 16 can be generated by the STC. A higher score means a higher frequency of engaging in unhealthy dietary behaviors [59].
2.5. Evaluation of Dietary Behaviors
The Three Factor Eating Questionnaire R18 (TFEQ-R18) was employed to examine the dietary behaviors of cognitive restraint, uncontrolled eating, and emotional eating [20]. The TFEQ-R18 includes 18 questions that measure maladaptive eating behaviors, and the instrument has been validated in many countries [60,61]. One example question is, “When I feel blue, I often overeat”. The possible answers include: “definitely true” (4), “mostly true” (3), “mostly false” (2), and “definitely false” (1). The TFEQ-R18 provides three subscale scores for the measured dietary behaviors. The formula, [(raw score-lowest possible raw score)/possible raw score range × 100], was used to transform subscale scores into scores on a scale of 0 to 100 [20]. Higher subscale scores indicate higher frequency of engaging in restrained eating caused by cognitive restraint, uncontrolled eating, or emotional eating.
2.6. Evaluation of Sleep Quality and Duration
The Pittsburgh Sleep Quality Index (PSQI) was used to determine subjective sleep quality [62,63]. The PSQI includes 10 questions assessing sleeping habits, duration, and degree of sleep problems, with scores ranging from 0 to 21. Higher PSQI scores indicate poorer sleep quality. Further to this, a PSQI score of ≥5 represents poor sleep quality while a PSQI score of <5 indicates good sleep quality [62].
Sleep duration was evaluated by asking participants the numbers of hours and minutes that they usually sleep for during weekdays and the weekend. A weighted method was used to calculate the average sleep duration of weekdays and weekends. The formula used was (((weekday sleep duration × 5) + (weekend sleep duration × 2))/7). Adequate sleep was defined by reporting an average sleep duration ≥7 h, while short sleep duration was defined as reporting average sleep duration <7 h [64].
2.7. Changes of Perceived Stress, Diet, and Sleep Due to the COVID-19 Pandemic
As the survey was conducted during the COVID-19 pandemic, changes in perceived stress, diet, and sleep due to the pandemic were assessed. Participants were asked whether and how their perceived stress, diet, and sleep quality and duration had changed during the COVID-19 pandemic compared to before the pandemic. For example, students were asked, “Have you made changes to your diet during the COVID-19 pandemic compared to before the pandemic?” The possible answers included eating healthier than before, eating less healthy than before, or no change.
2.8. Statistical Analysis
IBM SPSS Version 26 (IBM Corporation, Armonk, NY, USA) was used to analyze all data. Descriptive statistics are presented using percentages (%) or means ± standard deviations (SD). Outliers defined by greater or lower than mean ± 3SD were removed based on best practices for cleaning biological data such as BMI [65], and the variables examined were approximately normally distributed after outlier removal. Normal distribution was confirmed by skewness and kurtosis tests. To examine the relationships between the variables and covariates included in the mediation and moderation models, zero-order correlations were conducted. Significance was determined at p < 0.05. False discovery rate adjustment was performed to reduce the chance of type I error where appropriate, and the cut-off point was set at q = 0.05.
One-way analysis of variance (ANOVA) was conducted to determine gender differences in perceived stress, dietary risk, cognitive restraint, emotional eating, uncontrolled eating, sleep quality, and sleep duration. Bonferroni post hoc tests were performed, and significance was determined at p < 0.05. Students not identifying as either male or female were not included in the analysis due to the small sample size (n = 40).
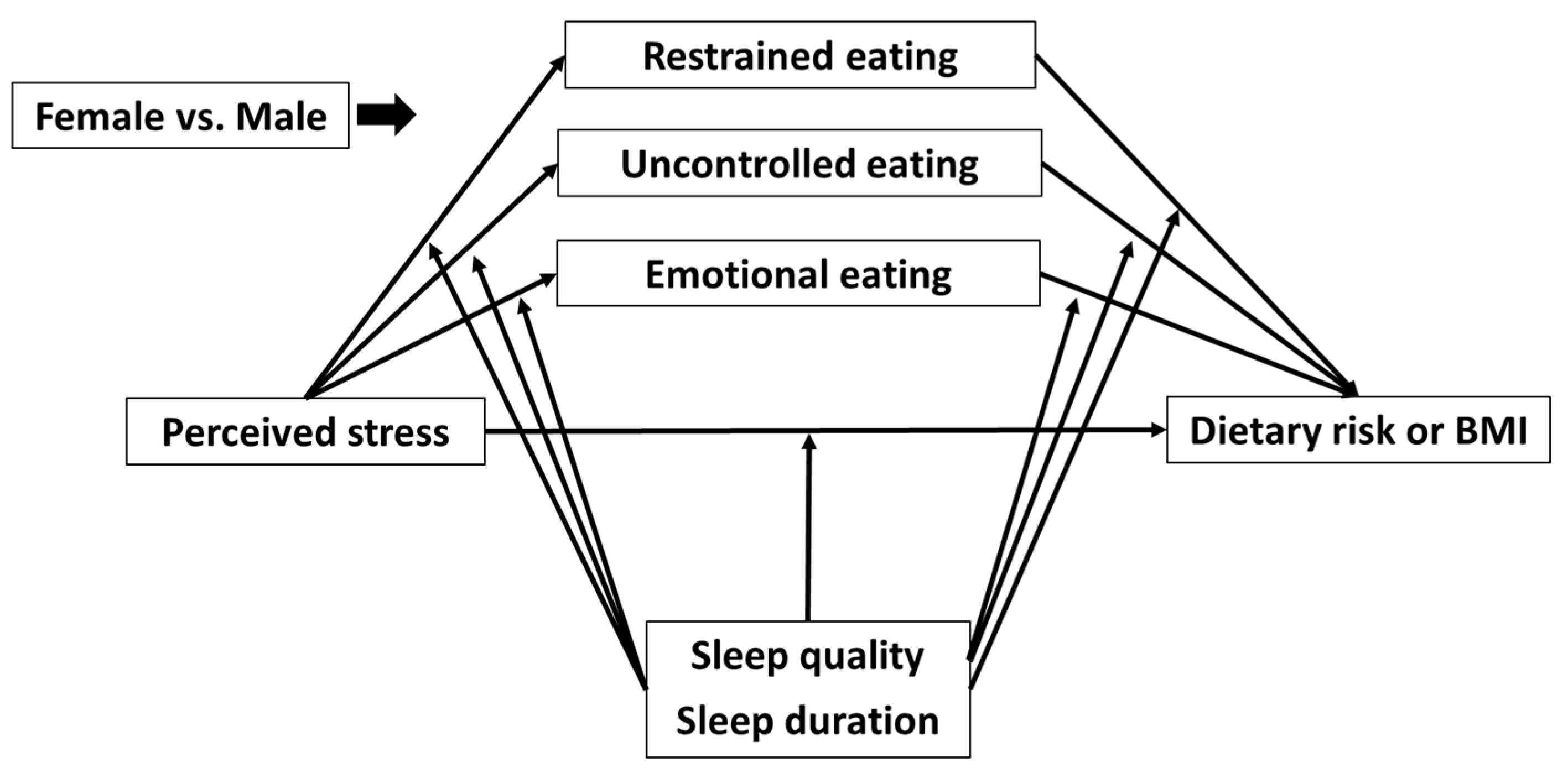
The SPSS PROCESS Macro was employed to conduct the moderated mediation analyses [66]. Model 59 was used. Previous studies suggest that testing mediation hypotheses using cross-sectional data is reasonable when temporal relationships between examined variables are shown [67,68,69]. Mediation analysis was used on the present cross-sectional dataset because temporal relationships between an independent variable (perceived stress), mediators (maladaptive eating behaviors), and dependent variables (dietary risk and BMI) are well established in the literature [15,18,23,26,40,70,71]. For example, increased stress leads to more frequent engagement in maladaptive eating behaviors [15,18,40], and these behaviors can further lead to the increased consumption of unhealthy foods and, thereafter, increased body weight [23,26,70,71]. Gender-specific models were developed because the mediation effects of cognitive constraint, uncontrolled eating, and emotional eating on the relationship between perceived stress and dietary risk have been shown to differ between males and females [28,29,30,31]. Students not identifying as either male or female were not included in the models because the sample size was too small (n = 40). A total of four models were built based on perceived stress as the independent variable and dietary risk as the dependent variable (Figure 1). The models were built to (1) examine the mediation effects of the three eating behaviors of interest on the relationship between perceived stress and dietary risk among female (Model 1) and male (Model 2) students, when under the moderation of sleep quality; and (2) examine the mediation effects of the three measured eating behaviors on the relationship between perceived stress and dietary risk among female (Model 3) and male (Model 4), when under the moderation of sleep duration. Four additional models were built based on perceived stress as the independent variable and BMI as the dependent variable. BMI was treated as a continuous variable. These models were similar to models 1 to 4, except BMI was the dependent variable (Model A—female students, sleep quality as the moderator; model B—male students, sleep quality as the moderator; Model C—female students, sleep duration as the moderator; Model D—male students, sleep duration as the moderator). Age, country, citizenship status, and class status were adjusted for all models, as these factors have been reported to be associated with either perceived stress, dietary risk, or BMI [57,72,73,74]. The number of bootstraps performed for bias corrected bootstrap confidence intervals was set at 10,000. p < 0.05 was used for determining significance for all analyses, and significant bootstrapping results were determined by the 95% confidence interval (CI) not crossing zero.

Figure 1.
Model 1: The mediation effect of restrained, uncontrolled, and emotional eating on the relationship between perceived stress and dietary risk under the moderation of sleep quality for female students; Model 2: The mediation effect of restrained, uncontrolled, and emotional eating on the relationship between perceived stress and dietary risk under the moderation of sleep quality for male students; Model 3: The mediation effect of restrained, uncontrolled, and emotional eating on the relationship between perceived stress and dietary risk under the moderation of sleep duration for female students; and Model 4: The mediation effect of restrained, uncontrolled, and emotional eating on the relationship between perceived stress and dietary risk under the moderation of sleep duration for male students. Models A to D: same as Models 1 to 4 but BMI was the dependent variable. Note that “others” were excluded from analysis.
For interpreting the results of the mediation analysis, the following conditions were used [66]. (1) Significant bootstrapping results for indirect effect indicated a significant mediation effect of a mediator on the relationship between an independent and a dependent variable. (2) The significance of the mediation effect, also known as the indirect effect, does not depend on the singular relationship between an independent variable and a dependent variable (the direct effect), an independent variable and a mediator, and a mediator and a dependent variable being significant.
The following principles and conditions were used to interpret the results of the moderation analysis [66,75]. First, a significant association must be present between two variables in order for a moderator to moderate the relationship. Second, for a significant moderation effect, the Johnson-Neyman method can be used to identify a transition point. Third, both direct and indirect moderation relationships can be present. Direct moderation examines whether a moderator moderates the relationship between an independent and a dependent variable while holding mediators constant. On the other hand, indirect moderation examines two types of conditional relationships. First, an indirect moderation examines whether a moderator moderates the relationship between an independent variable and a mediator. Second, an indirect moderation examines whether a moderator also moderates the relationship between a mediator and a dependent variable. Examining the indirect effect of moderators takes changes in mediators into account, whereas examining direct effects does not. Therefore, examination of the indirect effects of the moderators was also conducted.
3. Results
3.1. Demographics and Variable Associations
A total of 1392 students completed the online survey (Table 1). The majority of the participants were female (70%), undergraduate (79%), and domestic students (82%).

Table 1.
Demographics.
The mean age of the students was 22 ± 5 years and the mean BMI was classified as healthy (Table 2). The average sleep quality was classified as poor, while the average sleep duration was adequate. Most of the students experienced increased perceived stress during the pandemic compared to before. More than one third of students reported less healthy eating, and nearly one third of students reported reduced sleep quality during the pandemic compared to before. Over 40% of students reported longer sleep duration during the pandemic compared to before the pandemic.

Table 2.
Demographics, health parameters, and changes in health parameters during the COVID-19 pandemic.
The zero-order correlations between variables tested and covariates revealed that perceived stress was positively associated with dietary risk, uncontrolled eating, emotional eating, sleep quality, and BMI, while negatively associated with sleep duration and age (Table 3). Sleep quality was measured using PSQI scores, where higher PSQI scores indicate poorer sleep quality. Additionally, dietary risk was positively associated with uncontrolled eating, emotional eating, sleep quality, and BMI, but negatively associated with cognitive restraint. Furthermore, uncontrolled eating was positively associated with emotional eating and sleep quality.

Table 3.
Zero order correlation of variables and covariates examined in the mediation/moderation models.
Sleep quality was negatively associated with sleep duration and positively associated with age and BMI. In addition, sleep duration was negatively associated with BMI. Age was negatively associated with BMI.
The one-way ANOVA analysis indicated that female students reported higher perceived stress and higher dietary risk (p < 0.001) compared to male students (Table 4). In terms of eating behaviors, female students reported higher restrained (p < 0.001) and emotional eating (p < 0.001) compared to male students. For sleep quality and duration, female students reported worse sleep quality (p = 0.003) but longer sleep duration compared to male students (p = 0.019).

Table 4.
Gender differences in outcomes of interest.
3.2. Mediation and Moderation Analyses
3.2.1. Model 1 Mediation of Eating Behaviors on the Relationship between Perceived Stress and Dietary Risk under the Moderation of Sleep Quality among Female Students
Model 1 mediation analysis revealed that perceived stress was positively associated with dietary risk among female students (Table 5). In addition, restrained eating negatively correlated with dietary risk, while uncontrolled and emotional eating positively correlated with dietary risk. Furthermore, uncontrolled (B = 0.0083, 95% CI = 0.0029, 0.0150) and emotional eating (B = 0.00138, 95% CI = 0.0068, 0.0223) significantly mediated the relationship between perceived stress and dietary risk among female students.

Table 5.
Model 1 mediation analysis of eating behaviors on the relationship between perceived stress and dietary risk for females.
In order to examine whether sleep quality moderated the relationship between perceived stress and dietary risk directly or indirectly through the three eating behaviors (Table 6), two moderation pathways were evaluated. Sleep quality did not directly moderate the relationship between perceived stress and dietary risk, which was evidenced by the insignificant interaction effect of sleep quality and perceived stress on dietary risk (p = 0.6368) in Path 1 analysis. However, Path 2 analysis indicated that sleep quality moderated the relationship between perceived stress and dietary risk indirectly through moderating the relationship between uncontrolled eating and dietary risk and the relationship between emotional eating and dietary risk. These results were evidenced by the significant interaction effect of sleep quality and uncontrolled eating on dietary risk (p = 0.0388) and the significant interaction effect of sleep quality and emotional eating on dietary risk (p = 0.0223). Furthermore, based on the Johnson-Neyman test, higher sleep quality (lower PSQI scores) weakens the relationship between uncontrolled eating and dietary risk, and when the PSQI score is lower than 4.5 the relationship between uncontrolled eating and dietary risk disappears. Notably, 14.5% of female students reported a PSQI sore below 4.5, while 85.5% of female students reported a PSQI score above 4.5. Additionally, better sleep quality also weakens the relationship between emotional eating and dietary risk, and when the PSQI score is lower than 2.8, the relationship disappears.

Table 6.
Model 1 moderation analysis for females (sleep quality as a moderator).
Taken together, the mediation and moderation analyses of Model 1 indicated that the relationship between perceived stress and dietary risk was associated with uncontrolled eating and emotional eating among female students. Sleep quality moderated the relationship between perceived stress and dietary risk indirectly through uncontrolled and emotional eating.
3.2.2. Model 2 Mediation of Eating Behaviors on the Relationship between Perceived Stress and Dietary Risk under the Moderation of Sleep Quality among Male Students
The Model 2 mediation analysis indicated that perceived stress positively correlated with uncontrolled eating (p = 0.0002) and emotional eating (p = 0.0021) among male students, while the other relationships presented in Table 7 were not significant, including a non-significant relationship between perceived stress and dietary risk. Additionally, restrained eating (B = −0.0076, 95% CI = −0.0189, 0.0018), uncontrolled eating (B = 0.0072, 95% CI = −0.0028, 0.0196), and emotional eating (B = 0.0057, 95% CI = −0.0046, 0.0178) did not mediate the relationship between perceived stress and dietary risk among male students.

Table 7.
Model 2 mediation Analysis of eating behaviors on the relationship between perceived stress and dietary risk for males.
To evaluate whether sleep quality moderated the relationship between perceived stress and dietary risk directly or indirectly through the measured eating behaviors among male students, two moderation pathways were assessed (Table 8). Path 1 analysis identified that sleep quality did not directly moderate the relationship between perceived stress and dietary risk, which was evidenced by the insignificant interaction effect of sleep quality and perceived stress on dietary risk (p = 0.1691). Additionally, Path 2 analysis indicated that sleep quality did not indirectly moderate the relationship between perceived stress and dietary risk, as the interaction effects of sleep quality and perceived stress on restrained eating (p = 0.4502), uncontrolled eating (p = 0.0740), and emotional eating (p = 0.2675) were insignificant, and the interaction effects of sleep quality and restrained eating (p = 0.5446), sleep quality and uncontrolled eating (p = 0.6480), and sleep quality and emotional eating (p = 0.2508) on dietary risk were insignificant.

Table 8.
Model 3 moderation analysis (sleep quality as a moderator).
In summary, these results confirmed that restrained, uncontrolled, and emotional eating did not mediate the relationship between perceived stress and dietary risk among male students, and that sleep quality did not moderate the relationship between perceived stress and dietary risk either directly or indirectly for male students.
3.2.3. Model 3 Mediation of Eating Behaviors on the Relationship between Perceived Stress and Dietary Risk under the Moderation of Sleep Duration among Female Students
Model 3 mediation analysis reported that uncontrolled (B = 0.0041, 95% CI = 0.0022, 0.0109) and emotional eating (B = 0.0202, 95% CI = 0.0112, 0.0311) significantly mediated the relationship between perceived stress and dietary risk among female students, which agrees with the Model 1 mediation analysis. Unlike the mediation analyses, the Model 3 moderation analysis indicated that sleep duration did not directly or indirectly moderate the relationship between perceived stress and dietary risk among female students.
3.2.4. Model 4 Mediation of Eating Behaviors on the Relationship between Perceived Stress and Dietary Risk under the Moderation of Sleep Duration among Male Students
The Model 4 mediation analysis indicated that restrained eating (B = −0.0053, 95% CI = −0.0171, 0.0064), uncontrolled eating (B = 0.0006, 95% CI = −0.0129, 0.0150), and emotional eating (B = 0.0157, 95% CI = −0.0002, 0.0370) did not mediate the relationship between perceived stress and dietary risk among male students. Furthermore, the Model 4 moderation analysis confirmed that sleep duration did not directly or indirectly moderate the relationship between perceived stress and dietary risk among male students.
3.2.5. Model A Mediation of Eating Behaviors on the Relationship between Perceived Stress and BMI under the Moderation of Sleep Quality among Female Students
Model A mediation analysis revealed that emotional eating (B = 0.0244, 95% CI = 0.0116, 0.0406) significantly mediated the relationship between perceived stress and BMI among female students (Table 9). However, perceived stress was not significantly associated with restrained eating, uncontrolled eating, emotional eating, and BMI in this model. Only emotional eating was positively associated with BMI among female students (p = 0.0432).

Table 9.
Model A mediation analysis of eating behaviors on the relationship between perceived stress and BMI for females.
To assess whether sleep quality moderated the relationship between perceived stress and BMI directly or indirectly through the three eating behaviors (Table 10), two moderation pathways were evaluated. Path 1 analysis indicated that sleep quality did not directly moderate the relationship between perceived stress and BMI, and this was shown by the insignificant interaction effect of sleep quality and perceived stress on BMI (p = 0.6710). However, Path 2 analysis revealed that sleep quality indirectly moderated the relationship between perceived stress and BMI through moderating the relationship between emotional eating and BMI. The result was evidenced by the significant interaction effect of sleep quality and emotional eating on BMI (p = 0.0154). Furthermore, based on the Johnson-Neyman test, better sleep quality weakens the relationship between emotional eating and BMI, and when the PSQI score is <4.7, the relationship between emotional eating and BMI disappears. Per the present data, 14.6% female students reported a PSQI score below 4.7, with the remainder of these students reporting a PSQI score above 4.7.

Table 10.
Model A moderation analysis (sleep quality as a moderator) for females.
In summary, these results demonstrated that the relationship between perceived stress and BMI was associated with emotional eating among female students. Sleep quality moderated the relationship between perceived stress and BMI indirectly through emotional eating.
3.2.6. Model B Mediation of Three Eating Behaviors on the Relationship between Perceived Stress and BMI under the Moderation of Sleep Quality among Male Students
Model B mediation analysis revealed that emotional eating (B = 0.0379, 95% CI = 0.0142, 0.0685) significantly mediated the relationship between perceived stress and BMI among male students. Additionally, perceived stress was positively associated with uncontrolled eating (p = 0.0001) and emotional eating (p = 0.0023) among male students.
Two moderation analyses were conducted in Model B. One pathway examined whether sleep quality moderated the relationship between perceived stress and BMI directly, and the other pathway tested whether sleep quality moderated the same relationship indirectly. The results indicated that sleep quality did not moderate the relationship between perceived stress and BMI directly or indirectly among male students. These results were supported by an insignificant interaction effect of sleep quality and perceived stress on BMI (p = 0.3526, direct effect) and the insignificant interaction effects of sleep quality and perceived stress on restrained eating (p = 0.6030), uncontrolled eating (p = 0.0550), and emotional eating (p = 0.2522). Additionally, the interaction effects of sleep quality and restrained eating (p = 0.8785), sleep quality and uncontrolled eating (p = 0.8333), and sleep quality and emotional eating on BMI were also insignificant (p = 0.9996).
Taken together, these results showed that the relationship between perceived stress and BMI was associated with emotional eating among male students. However, changes in sleep quality did not alter the relationship between perceived stress and BMI directly or indirectly among male students.
3.2.7. Model C Mediation of Eating Behaviors on the Relationship between Perceived Stress and BMI under the Moderation of Sleep Duration among Female Students
Model C mediation analysis observed that emotional eating significantly mediated the relationship between perceived stress and BMI for females (B = 0.0506, 95% CI = 0.0167, 0.0959). The moderation analysis of Model C indicated that sleep duration did not directly or indirectly moderate the relationship between perceived stress and BMI.
3.2.8. Model D Mediation of Eating Behaviors on the Relationship between Perceived Stress and BMI under the Moderation of Sleep Duration among Male Students
Model D mediation analysis indicated that emotional eating significantly mediated the relationship between perceived stress and BMI among male students (B = 0.0506, 95% CI = 0.0174, 0.0942). However, sleep duration did not directly or indirectly moderate the relationship between perceived stress and BMI.
4. Discussion
This study explored whether maladaptive eating behaviors, including restrained, uncontrolled, and emotional eating, mediated the relationships between perceived stress and dietary risk along with BMI, and further examined whether sleep quality and duration moderated these relationships. Results indicated that the relationship between perceived stress and BMI was mediated by emotional eating for both males and females; sleep quality, but not sleep duration, moderated this relationship indirectly through emotional eating, but only among females. Additionally, for female students, the relationship between perceived stress and dietary risk was mediated by uncontrolled eating and emotional eating, and sleep quality—but not duration—moderated this relationship indirectly, through uncontrolled and emotional eating. These findings suggest that reducing uncontrolled and emotional eating while improving sleep quality among female students, and reducing emotional eating among male students, could potentially reduce dietary risk and prevent weight gain among students experiencing high levels of stress.
4.1. The Mediation Effects of Retrained, Uncontrolled, and Emotional Eating on the Relationship between Perceived Stress and Dietary Risk
As hypothesized, study findings were influenced by gender. Uncontrolled eating and emotional eating mediated the relationship between perceived stress and dietary risk for females but not males. These observations are consistent with other reports where women tend to experience a higher frequency of uncontrolled and emotional eating compared to males [28,29,30,31]. Stress can trigger emotional eating [17], and stress-induced emotional eating is more common in women than men [17,35]. Furthermore, stress can lead to a greater tendency to overeat [1], especially among emotional eaters [76]. Both uncontrolled and emotional eating are characterized by eating a large quantity of foods that are highly palatable, such as sweets and high fat foods [18,27], which increase dietary risk. Thus, uncontrolled and emotional eating could serve as an intermediate connection between perceived stress and dietary risk, especially for female students.
Unlike what was hypothesized, restrained eating did not mediate the relationship between perceived stress and dietary risk, based on the insignificant bootstrapping result of the indirect effect of restrained eating on the relationship between perceived stress and dietary risk. Even though perceived stress is positively associated with dietary risk, and restrained eating is negatively associated with dietary risk, these singular relationships do not indicate a mediation effect [66]. A body of literature suggests that restrained eating is associated with overeating and higher dietary risk [77,78,79], and that restrained eaters are more likely to respond to stress by consuming highly palatable foods [80]. The discrepant results between this study and the work of others might be explained by the lack of relationship between perceived stress and restrained eating in our study sample. Students may tend to engage in other maladaptive eating behaviors such as emotional eating [81,82] during the COVID-19 pandemic. Little is known about the relationship between stress and restrained eating during the COVID-19 pandemic; however, one study reported that more severe COVID-19 lockdowns were associated with increased anxiety symptoms but lower restrained eating [83]. Thus, the stress related to the pandemic may help explain the lack of relationship between perceived stress and restrained eating in our study sample. In summary, restrained eating appears to have a limited association with dietary risk scores during the pandemic.
4.2. The Moderation Effects of Sleep Quality and Duration on the Relationship between Perceived Stress and Dietary Risk
As expected, sleep quality moderated the relationship between perceived stress and dietary risk indirectly by moderating the relationship between uncontrolled and emotional eating, but these relationships were only present in females. Furthermore, when the PSQI score was less than 4.5, the relationship between uncontrolled eating and dietary risk disappeared. To provide perspective, a PSQI score < 5 is considered to reflect good sleep quality. For emotional eating, when the PSQI score was less than 2.8, the relationship between emotional eating and dietary risk disappeared. Even though a PSQI score < 2.8 is clinically difficult to achieve, higher sleep quality weakening the effect of emotional eating on dietary risk is a practical finding. Therefore, improving sleep quality may weaken the relationship between perceived stress and dietary risk indirectly, by weakening the relationship between uncontrolled eating and dietary risk and by weakening the relationship between emotional eating and dietary risk for female students.
Unlike among female students, the same moderation effects of sleep quality on the relationship between perceived stress and dietary risk in males were not observed. The reason for this discrepancy is likely because uncontrolled and emotional eating did not mediate the relationship between perceived stress and dietary risk among these students. Furthermore, there were no associations among male students between either uncontrolled eating or emotional eating and dietary risk. Thus, improving sleep quality among male students may not reduce unhealthy dietary behaviors when under stress; however, better sleep quality is associated with better health outcomes later in life, such as lower cardiovascular disease [84,85,86] and infection risks [87,88] among both males and females. Therefore, even though a moderation effect of sleep quality on the relationship between perceived stress and dietary risk in males was not observed, good sleep quality is still important to the overall health of males.
4.3. The Mediation Effects of Retrained, Uncontrolled, and Emotional Eating on the Relationship between Perceived Stress and BMI
In the present study, results indicated that the relationship between perceived stress and BMI was associated with emotional eating for both males and females. These findings align with other studies where emotional eating mediated the relationship between negative emotion—including stress and depression—and weight gain in both males and females [34,70,71]. Furthermore, prospective studies conducted in Finland [34], France [89], South Korea [90], the Netherlands [71], and the U.S. [91] reported that higher levels of emotional eating were associated with greater weight gain. Additionally, stress tends to trigger undesirable food consumption among emotional eaters [17]. Therefore, targeting interventions that address emotional eating may help higher education students reduce risky dietary behaviors during stressful situations.
4.4. The Moderation Effects of Sleep Quality and Duration on the Relationship between Perceived Stress and BMI
Sleep quality moderated the relationship between perceived stress and BMI indirectly through emotional eating among female but not male students. This finding might be explained by female students suffering poorer sleep quality compared to male students. Several other studies reported similar findings where female young adults were more vulnerable to poor sleep quality [50,92,93]. Based on the literature and our findings, improved sleep quality may serve as an intervention target to disrupt the relationship between perceived stress and BMI indirectly, by weakening the relationship between emotional eating and BMI among female students.
Sleep duration did not moderate the relationship between perceived stress and dietary risk or BMI, which contradicts our hypothesis. These findings are inconsistent with studies that report that insufficient sleep leads to higher dietary risk and higher likelihood of weight gain [48,94,95,96], and that high stress can lead to shortened sleep [53,97]. The discrepancy between our findings and those reported by others might be explained by the fact that our study sample met recommended sleep duration guidelines, suggesting that many students achieved adequate sleep. Recent studies, along with our previous work, reported that students slept longer but with poorer sleep quality during the COVID-19 pandemic [98,99,100,101,102]. Additionally, over 40% of students in our study reported sleeping longer during the COVID-19 pandemic compared to before the pandemic. The current evidence points to focusing more on improving sleep quality rather than duration during a highly stressful event like the COVID-19 pandemic.
4.5. Public Health Messages
Our findings suggest that interventions focusing on helping students to address uncontrolled and emotional eating may be important strategies to reduce risky dietary behaviors and to prevent weight gain, especially during stressful times. However, screening for uncontrolled and emotional eating is not routinely conducted by universities [103,104]. Frequent engagement in uncontrolled and emotional eating increases the risk of developing eating disorders [105]. Eating disorders are more prevalent among university students compared to the general population [106,107]. Early detection of eating disorders and maladaptive eating behaviors is a key intervention for treating and preventing eating disorders [108]. Therefore, universities should consider implementing screenings for maladaptive eating behaviors for students and providing interventions as needed.
Improving sleep quality could serve as another target of intervention to help reduce dietary risk and prevent weight gain, especially among female students. However, there is currently a lack of programming for higher education institutions to address sleep issues [109,110]. Previous work reported that sleep disturbances are associated with academic success more strongly than drug use, drinking, and stress. However, screening for sleep issues and providing sleep hygiene interventions are not frequently conducted [111]. Besides screening, providing effective sleep programming also plays a key role in improving student sleep quality. Face-to-face [112,113] or virtual [114] delivery of cognitive behavior therapy for insomnia (CBTi) has been shown to be an effective strategy for improving sleep, and could help reduce dietary risk and prevent weight gain, especially during stressful situations.
4.6. Strengths and Limitations
The study has several strengths. In terms of study strengths, surveys were collected from a large population of students from seven countries, which broadens the generalizability of the results. Additionally, a more comprehensive examination of the relationships between perceived stress, eating behaviors, sleep, dietary risk, and BMI was performed using moderated mediation analyses. Furthermore, all instruments used in the study were validated, often in multiple countries [39,60,61,115]. Finally, the study was conducted during the COVID-19 pandemic, a time of heightened stress, which offers a unique perspective.
Several limitations are present in the study. First, the study is a cross-sectional study, in which the results only suggest relational, rather than causal, relationships between the variables examined. Therefore, a prospective longitudinal study is needed to confirm the relationship sequence suggested by the current study. Second, while the COVID-19 pandemic provided a unique time point to measure student stress, it also altered some student responses. A post-pandemic study is recommended to confirm the relationships observed. Third, the study did not control for the “shelter in place” status of each country included because the definition of “shelter in place” varied from country and country. Fourth, the study only included English speaking students, which excluded students who do not have English proficiency.
5. Conclusions
The current study demonstrated that uncontrolled and emotional eating mediated the relationship between perceived stress and dietary risk, and higher sleep quality weakened this relationship among female university students but not males. Additionally, emotional eating mediated the relationship between perceived stress and BMI for both males and females, but higher sleep quality weakened this relationship only among females. These findings suggest that interventions addressing uncontrolled and emotional eating, as well as sleep hygiene training, may be important strategies to reduce dietary risk and prevent weight gain among university students, especially when under considerable stress.
Author Contributions
Conceptualization, C.D., W.S. and R.M.T.; Data curation, C.D., M.A., M.C.H.Z., M.J.C., J.I.F., P.Y.H., L.K., H.L., M.-J.L., W.S., W.C.S.S., J.T., F.A.-A., E.d.K., W.W. and R.M.T.; Formal analysis, C.D.; Funding acquisition, R.M.T.; Investigation, C.D., M.A., M.C.H.Z., M.J.C., J.I.F., P.Y.H., L.K., H.L., M.-J.L., W.S., W.C.S.S., J.T. and R.M.T.; Methodology, C.D. and R.M.T.; Project administration, R.M.T.; Resources, R.M.T.; Supervision, R.M.T.; Validation, C.D.; Visualization, C.D.; Writing–original draft, C.D., R.M.T., E.d.K. and W.W.; Writing–review & editing, C.D., M.A., M.C.H.Z., M.J.C., J.I.F., P.Y.H., L.K., H.L., M.-J.L., W.S., W.C.S.S., J.T., F.A.-A., E.d.K., W.W. and R.M.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research and the APC were funded by the USDA National Institute of Food and Agriculture, Hatch #1012976, and Michigan AgBioResearch and the Indiana University of Pennsylvania Faculty Incidental Research Support award.
Institutional Review Board Statement
The study was approved by the Michigan State University Human Research Protection Program (East Lansing, MI, USA), STUDY00004285, 7 April 2020; Indiana University of Pennsylvania Institutional Review Board for the Protection of Human Subjects (Indiana, PA, USA), IRB Log 20-101, 26 October 2020; Bowling Green State University Office of Research Compliance (Bowling Green, OH, USA); 1,599,753 (US students), 29 April 2020; 1,599,753 (Chinese students), 22 May 2020; 1,599,753 (Korean students), 11 May 2020; Faculty of Governance and Global Affairs Ethics Committee (The Hague, South Holland, Netherlands), 2020-009-LUC-Cho, 25 May 2020; International Medical University Joint Committee on Research and Ethics (Kuala Lumpur, Malaysia), 481/2020, 14 May 2020; Institute Research Ethics Committee, Institute of Technology, Sligo (Sligo, Ireland), ref 2020015, 7 October 2020; Kwame Nkrumah University of Science and Technology Committee on Human Research Publication and Ethics (School of Medical Sciences), CHRPE/AP/389/20, 30 October 2020.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to ongoing analyses.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Peltzer, K.; Pengpid, S.; Samuels, T.A.; Özcan, N.K.; Mantilla, C.; Rahamefy, O.H.; Wong, M.L.; Gasparishvili, A. Prevalence of Overweight/Obesity and Its Associated Factors among University Students from 22 Countries. Int. J. Environ. Res. Public. Health 2014, 11, 7425–7441. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pengpid, S.; Peltzer, K. Prevalence of Overweight/Obesity and Central Obesity and Its Associated Factors among a Sample of University Students in India. Obes. Res. Clin. Pract. 2014, 8, e558–e570. [Google Scholar] [CrossRef]
- Asif, S.; Mudassar, A.; Shahzad, T.Z.; Raouf, M.; Pervaiz, T. Frequency of Depression, Anxiety and Stress among University Students. Pak. J. Med. Sci. 2020, 36, 971–976. [Google Scholar] [CrossRef]
- Du, C.; Zan, M.C.H.; Cho, M.J.; Fenton, J.I.; Hsiao, P.Y.; Hsiao, R.; Keaver, L.; Lai, C.-C.; Lee, H.; Ludy, M.-J.; et al. Health Behaviors of Higher Education Students from 7 Countries: Poorer Sleep Quality during the COVID-19 Pandemic Predicts Higher Dietary Risk. Clocks Sleep 2021, 3, 12–30. [Google Scholar] [CrossRef] [PubMed]
- Jiang, N.; Yan-Li, S.; Pamanee, K.; Sriyanto, J. Depression, Anxiety, and Stress during the COVID-19 Pandemic: Comparison among Higher Education Students in Four Countries in the Asia-Pacific Region. J. Popul. Soc. Stud. JPSS 2021, 29, 370–383. [Google Scholar] [CrossRef]
- Allman-Farinelli, M.; Partridge, S.R.; Roy, R. Weight-Related Dietary Behaviors in Young Adults. Curr. Obes. Rep. 2016, 5, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Jang, H.J.; Kim, B.S.; Won, C.W.; Kim, S.Y.; Seo, M.W. The Relationship between Psychological Factors and Weight Gain. Korean J. Fam. Med. 2020, 41, 381–386. [Google Scholar] [CrossRef]
- León-Muñoz, L.M.; García-Esquinas, E.; Soler-Vila, H.; Guallar-Castillón, P.; Banegas, J.R.; Rodríguez-Artalejo, F. Unhealthy Eating Behaviors and Weight Gain: A Prospective Study in Young and Middle-Age Adults. Obesity 2016, 24, 1178–1184. [Google Scholar] [CrossRef] [Green Version]
- Oliver, G.; Wardle, J. Perceived Effects of Stress on Food Choice. Physiol. Behav. 1999, 66, 511–515. [Google Scholar] [CrossRef]
- Vidal, E.J.; Alvarez, D.; Martinez-Velarde, D.; Vidal-Damas, L.; Yuncar-Rojas, K.A.; Julca-Malca, A.; Bernabe-Ortiz, A. Perceived Stress and High Fat Intake: A Study in a Sample of Undergraduate Students. PLoS ONE 2018, 13, e0192827. [Google Scholar] [CrossRef]
- Zellner, D.A.; Loaiza, S.; Gonzalez, Z.; Pita, J.; Morales, J.; Pecora, D.; Wolf, A. Food Selection Changes under Stress. Physiol. Behav. 2006, 87, 789–793. [Google Scholar] [CrossRef] [PubMed]
- Sung, M.-J.; Chang, K.-J. Correlations among life stress, dietary behaviors and food choice of college students. J. East Asian Soc. Diet. Life 2006, 16, 655–662. [Google Scholar]
- Radavelli-Bagatini, S.; Blekkenhorst, L.C.; Sim, M.; Prince, R.L.; Bondonno, N.P.; Bondonno, C.P.; Woodman, R.; Anokye, R.; Dimmock, J.; Jackson, B.; et al. Fruit and Vegetable Intake Is Inversely Associated with Perceived Stress across the Adult Lifespan. Clin. Nutr. 2021, 40, 2860–2867. [Google Scholar] [CrossRef]
- Errisuriz, V.L.; Pasch, K.E.; Perry, C.L. Perceived Stress and Dietary Choices: The Moderating Role of Stress Management. Eat. Behav. 2016, 22, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Diggins, A.; Woods-Giscombe, C.; Waters, S. The Association of Perceived Stress, Contextualized Stress, and Emotional Eating with Body Mass Index in College-Aged Black Women. Eat. Behav. 2015, 19, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Katterman, S.N.; Kleinman, B.M.; Hood, M.M.; Nackers, L.M.; Corsica, J.A. Mindfulness Meditation as an Intervention for Binge Eating, Emotional Eating, and Weight Loss: A Systematic Review. Eat. Behav. 2014, 15, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Tan, C.C.; Chow, C.M. Stress and Emotional Eating: The Mediating Role of Eating Dysregulation. Personal. Individ. Differ. 2014, 66, 1–4. [Google Scholar] [CrossRef]
- Yau, Y.H.C.; Potenza, M.N. Stress and Eating Behaviors. Minerva Endocrinol. 2013, 38, 255–267. [Google Scholar]
- Anglé, S.; Engblom, J.; Eriksson, T.; Kautiainen, S.; Saha, M.-T.; Lindfors, P.; Lehtinen, M.; Rimpelä, A. Three Factor Eating Questionnaire-R18 as a Measure of Cognitive Restraint, Uncontrolled Eating and Emotional Eating in a Sample of Young Finnish Females. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 41. [Google Scholar] [CrossRef] [Green Version]
- de Lauzon, B.; Romon, M.; Deschamps, V.; Lafay, L.; Borys, J.-M.; Karlsson, J.; Ducimetière, P.; Charles, M.A.; Fleurbaix Laventie Ville Sante Study Group. The Three-Factor Eating Questionnaire-R18 Is Able to Distinguish among Different Eating Patterns in a General Population. J. Nutr. 2004, 134, 2372–2380. [Google Scholar] [CrossRef]
- Herman, C.P.; Polivy, J.; Lank, C.N.; Heatherton, T.F. Anxiety, Hunger, and Eating Behavior. J. Abnorm. Psychol. 1987, 96, 264–269. [Google Scholar] [CrossRef]
- Polivy, J.; Herman, C.P.; Mills, J.S. What Is Restrained Eating and How Do We Identify It? Appetite 2020, 155, 104820. [Google Scholar] [CrossRef] [PubMed]
- Polivy, J.; Herman, C.P. Dieting and Binging: A Causal Analysis. Am. Psychol. 1985, 40, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Lowe, M.R.; Kleifield, E.I. Cognitive Restraint, Weight Suppression, and the Regulation of Eating. Appetite 1988, 10, 159–168. [Google Scholar] [CrossRef]
- Jansen, A.; Nederkoorn, C.; van Baak, L.; Keirse, C.; Guerrieri, R.; Havermans, R. High-Restrained Eaters Only Overeat When They Are Also Impulsive. Behav. Res. Ther. 2009, 47, 105–110. [Google Scholar] [CrossRef]
- Stunkard, A.J.; Messick, S. Eating Inventory: Manual; Psychological Corporation, Harcourt Brace Jovanovich: San Diego, CA, USA, 1988. [Google Scholar]
- van Strien, T.; Ouwens, M.A. Effects of Distress, Alexithymia and Impulsivity on Eating. Eat. Behav. 2007, 8, 251–257. [Google Scholar] [CrossRef]
- Davis, E.; Greenberger, E.; Charles, S.; Chen, C.; Zhao, L.; Dong, Q. Emotion Experience and Regulation in China and the United States: How Do Culture and Gender Shape Emotion Responding? Int. J. Psychol. J. Int. Psychol. 2012, 47, 230–239. [Google Scholar] [CrossRef]
- De Lauzon-Guillain, B.; Romon, M.; Musher-Eizenman, D.; Heude, B.; Basdevant, A.; Charles, M.A. Cognitive Restraint, Uncontrolled Eating and Emotional Eating: Correlations between Parent and Adolescent. Matern. Child. Nutr. 2008, 5, 171–178. [Google Scholar] [CrossRef] [Green Version]
- Kemp, E.; Bui, M.; Grier, S. Eating Their Feelings: Examining Emotional Eating in at-Risk Groups in the United States. J. Consum. Policy 2011, 34, 211–229. [Google Scholar] [CrossRef]
- Thompson, S. Gender and Racial Differences in Emotional Eating, Food Addiction Symptoms, and Body Weight Satisfaction among Undergraduates. J. Diabetes Obes. 2015, 2, 1–6. [Google Scholar] [CrossRef] [Green Version]
- de Lauzon-Guillain, B.; Basdevant, A.; Romon, M.; Karlsson, J.; Borys, J.-M.; Charles, M.A.; The FLVS Study Group. Is Restrained Eating a Risk Factor for Weight Gain in a General Population? Am. J. Clin. Nutr. 2006, 83, 132–138. [Google Scholar] [CrossRef] [PubMed]
- Keller, C.; Hartmann, C.; Siegrist, M. The Association between Dispositional Self-Control and Longitudinal Changes in Eating Behaviors, Diet Quality, and BMI. Psychol. Health 2016, 31, 1311–1327. [Google Scholar] [CrossRef] [PubMed]
- Konttinen, H.; van Strien, T.; Männistö, S.; Jousilahti, P.; Haukkala, A. Depression, Emotional Eating and Long-Term Weight Changes: A Population-Based Prospective Study. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 28. [Google Scholar] [CrossRef] [Green Version]
- Beydoun, M.A. The Interplay of Gender, Mood, and Stress Hormones in the Association between Emotional Eating and Dietary Behavior. J. Nutr. 2014, 144, 1139–1141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Michels, N.; Sioen, I.; Braet, C.; Eiben, G.; Hebestreit, A.; Huybrechts, I.; Vanaelst, B.; Vyncke, K.; De Henauw, S. Stress, Emotional Eating Behaviour and Dietary Patterns in Children. Appetite 2012, 59, 762–769. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nguyen-Michel, S.T.; Unger, J.B.; Spruijt-Metz, D. Dietary Correlates of Emotional Eating in Adolescence. Appetite 2007, 49, 494–499. [Google Scholar] [CrossRef] [Green Version]
- Neumark-Sztainer, D.; Wall, M.; Haines, J.; Story, M.; Eisenberg, M.E. Why Does Dieting Predict Weight Gain in Adolescents? Findings from Project EAT-II: A 5-Year Longitudinal Study. J. Am. Diet. Assoc. 2007, 107, 448–455. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Herhaus, B.; Petrowski, K. The Effect of Restrained Eating on Acute Stress-Induced Food Intake in People with Obesity. Appetite 2021, 159, 105045. [Google Scholar] [CrossRef]
- Shen, W.; Long, L.M.; Shih, C.-H.; Ludy, M.-J. A Humanities-Based Explanation for the Effects of Emotional Eating and Perceived Stress on Food Choice Motives during the COVID-19 Pandemic. Nutrients 2020, 12, 2712. [Google Scholar] [CrossRef]
- Guerrini Usubini, A.; Cattivelli, R.; Varallo, G.; Castelnuovo, G.; Molinari, E.; Giusti, E.M.; Pietrabissa, G.; Manari, T.; Filosa, M.; Franceschini, C.; et al. The Relationship between Psychological Distress during the Second Wave Lockdown of COVID-19 and Emotional Eating in Italian Young Adults: The Mediating Role of Emotional Dysregulation. J. Pers. Med. 2021, 11, 569. [Google Scholar] [CrossRef] [PubMed]
- Kashani, M.; Eliasson, A.; Vernalis, M. Perceived Stress Correlates with Disturbed Sleep: A Link Connecting Stress and Cardiovascular Disease. Stress 2012, 15, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Caldwell, K.; Harrison, M.; Adams, M.; Quin, R.H.; Greeson, J. Developing Mindfulness in College Students through Movement-Based Courses: Effects on Self-Regulatory Self-Efficacy, Mood, Stress, and Sleep Quality. J. Am. Coll. Health 2010, 58, 433–442. [Google Scholar] [CrossRef]
- Dweck, J.S.; Jenkins, S.M.; Nolan, L.J. The Role of Emotional Eating and Stress in the Influence of Short Sleep on Food Consumption. Appetite 2014, 72, 106–113. [Google Scholar] [CrossRef]
- Konttinen, H. Emotional Eating and Obesity in Adults: The Role of Depression, Sleep and Genes. Proc. Nutr. Soc. 2020, 79, 283–289. [Google Scholar] [CrossRef]
- Brondel, L.; Romer, M.A.; Nougues, P.M.; Touyarou, P.; Davenne, D. Acute Partial Sleep Deprivation Increases Food Intake in Healthy Men. Am. J. Clin. Nutr. 2010, 91, 1550–1559. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Markwald, R.R.; Melanson, E.L.; Smith, M.R.; Higgins, J.; Perreault, L.; Eckel, R.H.; Wright, K.P. Impact of Insufficient Sleep on Total Daily Energy Expenditure, Food Intake, and Weight Gain. Proc. Natl. Acad. Sci. USA 2013, 110, 5695–5700. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spaeth, A.M.; Dinges, D.F.; Goel, N. Effects of Experimental Sleep Restriction on Weight Gain, Caloric Intake, and Meal Timing in Healthy Adults. Sleep 2013, 36, 981–990. [Google Scholar] [CrossRef]
- Fatima, Y.; Doi, S.A.R.; Mamun, A.A. Sleep Quality and Obesity in Young Subjects: A Meta-Analysis. Obes. Rev. 2016, 17, 1154–1166. [Google Scholar] [CrossRef]
- Grandner, M.A.; Schopfer, E.A.; Sands-Lincoln, M.; Jackson, N.; Malhotra, A. Relationship between Sleep Duration and Body Mass Index Depends on Age. Obes. Silver Spring Md 2015, 23, 2491–2498. [Google Scholar] [CrossRef] [Green Version]
- Charles, L.E.; Slaven, J.E.; Mnatsakanova, A.; Ma, C.; Violanti, J.M.; Fekedulegn, D.; Andrew, M.E.; Vila, B.J.; Burchfiel, C.M. Association of Perceived Stress with Sleep Duration and Sleep Quality in Police Officers. Int. J. Emerg. Ment. Health 2011, 13, 229–241. [Google Scholar] [PubMed]
- Hicks, R.A.; Garcia, E.R. Level of Stress and Sleep Duration. Percept. Mot. Skills 1987, 64, 44–46. [Google Scholar] [CrossRef] [PubMed]
- Stress and Insomnia. Available online: https://www.sleepfoundation.org/insomnia/stress-and-insomnia (accessed on 29 June 2021).
- Dial, L.A.; DeNardo, F.A.; Fevrier, B.; Morgan, A.L.; Du, C.; Tucker, R.M.; Hsiao, P.Y.; Ludy, M.-J. Comparing Mental Health and Well-Being of US Undergraduate and Graduate Students during the Early Stages of the COVID-19 Pandemic. J. Am. Coll. Health 2021, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Olatona, F.A.; Onabanjo, O.O.; Ugbaja, R.N.; Nnoaham, K.E.; Adelekan, D.A. Dietary Habits and Metabolic Risk Factors for Non-Communicable Diseases in a University Undergraduate Population. J. Health Popul. Nutr. 2018, 37, 21. [Google Scholar] [CrossRef]
- Brunt, A.B.; PhD, Y.R.; MS, L.Z. Differences in Dietary Patterns among College Students According to Body Mass Index. J. Am. Coll. Health 2008, 56, 629–634. [Google Scholar] [CrossRef]
- Du, C.; Luo, N.; Wu, L.; Gadd, S.; Zhang, X.; Tucker, R.M. Health Behavior Changes Associated with Weight Gain among First-Year International Students Studying at an American University. J. Am. Coll. Health J ACH 2021, 1–10. [Google Scholar] [CrossRef]
- Paxton, A.E.; Strycker, L.A.; Toobert, D.J.; Ammerman, A.S.; Glasgow, R.E. Starting the Conversation: Performance of a Brief Dietary Assessment and Intervention Tool for Health Professionals. Am. J. Prev. Med. 2011, 40, 67–71. [Google Scholar] [CrossRef]
- Jáuregui-Lobera, I.; García-Cruz, P.; Carbonero-Carreño, R.; Magallares, A.; Ruiz-Prieto, I. Psychometric Properties of Spanish Version of the Three-Factor Eating Questionnaire-R18 (Tfeq-Sp) and Its Relationship with Some Eating- and Body Image-Related Variables. Nutrients 2014, 6, 5619–5635. [Google Scholar] [CrossRef] [Green Version]
- Mostafavi, S.-A.; Akhondzadeh, S.; Mohammadi, M.R.; Eshraghian, M.R.; Hosseini, S.; Chamari, M.; Keshavarz, S.A. The Reliability and Validity of the Persian Version of Three-Factor Eating Questionnaire-R18 (TFEQ-R18) in Overweight and Obese Females. Iran. J. Psychiatry 2017, 12, 100–108. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Buysse, D.J.; Hall, M.L.; Strollo, P.J.; Kamarck, T.W.; Owens, J.; Lee, L.; Reis, S.E.; Matthews, K.A. Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and Clinical/Polysomnographic Measures in a Community Sample. J. Clin. Sleep Med. JCSM Off. Publ. Am. Acad. Sleep Med. 2008, 4, 563–571. [Google Scholar] [CrossRef] [Green Version]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Katz, E.S.; Kheirandish-Gozal, L.; et al. National Sleep Foundation’s Sleep Time Duration Recommendations: Methodology and Results Summary. Sleep Health 2015, 1, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Aguinis, H.; Gottfredson, R.K.; Joo, H. Best-Practice Recommendations for Defining, Identifying, and Handling Outliers. Organ. Res. Methods 2013, 16, 270–301. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 2nd ed.; Guilford Publications: New York, NY, USA, 2017; ISBN 978-1-4625-3465-4. [Google Scholar]
- Fairchild, A.J.; McDaniel, H.L. Best (but Oft-Forgotten) Practices: Mediation Analysis. Am. J. Clin. Nutr. 2017, 105, 1259–1271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MacKinnon, D.P. Introduction to Statistical Mediation Analysis; Routledge: New York, NY, 2008; ISBN 978-0-203-80955-6. [Google Scholar]
- Shrout, P.; Keyes, K.; Ornstein, K. Causality and Psychopathology: Finding the Determinants of Disorders and Their Cures, 1st ed.; Oxford University Press: New York, NY, USA, 2011; ISBN 978-0-19-975464-9. [Google Scholar]
- van Strien, T.; Konttinen, H.M.; Ouwens, M.A.; van de Laar, F.A.; Winkens, L.H.H. Mediation of Emotional and External Eating between Dieting and Food Intake or BMI Gain in Women. Appetite 2020, 145, 104493. [Google Scholar] [CrossRef] [PubMed]
- van Strien, T.; Konttinen, H.; Homberg, J.R.; Engels, R.C.M.E.; Winkens, L.H.H. Emotional Eating as a Mediator between Depression and Weight Gain. Appetite 2016, 100, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Masood, M.; Aggarwal, A.; Reidpath, D.D. Effect of National Culture on BMI: A Multilevel Analysis of 53 Countries. BMC Public Health 2019, 19, 1212. [Google Scholar] [CrossRef] [Green Version]
- Racette, S.B.; Deusinger, S.S.; Strube, M.J.; Highstein, G.R.; Deusinger, R.H. Weight Changes, Exercise, and Dietary Patterns during Freshman and Sophomore Years of College. J. Am. Coll. Health J ACH 2005, 53, 245–251. [Google Scholar] [CrossRef] [Green Version]
- Stawski, R.S.; Sliwinski, M.J.; Almeida, D.M.; Smyth, J.M. Reported Exposure and Emotional Reactivity to Daily Stressors: The Roles of Adult-Age and Global Perceived Stress. Psychol. Aging 2008, 23, 52–61. [Google Scholar] [CrossRef] [Green Version]
- Hayes, A.F. PROCESS: A Versatile Computational Tool for Observed Variable Mediation, Moderation, and Conditional Process Modeling 1. 2012. Available online: https://www.semanticscholar.org/paper/PROCESS-%3A-A-Versatile-Computational-Tool-for-%2C-%2C-1-Hayes/aa753b543c78d6c4f344fb431c6683edaa062c07 (accessed on 1 April 2021).
- Bongers, P.; de Graaff, A.; Jansen, A. ‘Emotional’ Does Not Even Start to Cover It: Generalization of Overeating in Emotional Eaters. Appetite 2016, 96, 611–616. [Google Scholar] [CrossRef] [Green Version]
- Contento, I.R.; Zybert, P.; Williams, S.S. Relationship of Cognitive Restraint of Eating and Disinhibition to the Quality of Food Choices of Latina Women and Their Young Children. Prev. Med. 2005, 40, 326–336. [Google Scholar] [CrossRef] [PubMed]
- Morin, I.; Bégin, C.; Maltais-Giguère, J.; Bédard, A.; Tchernof, A.; Lemieux, S. Impact of Experimentally Induced Cognitive Dietary Restraint on Eating Behavior Traits, Appetite Sensations, and Markers of Stress during Energy Restriction in Overweight/Obese Women. J. Obes. 2018, 2018, 4259389. [Google Scholar] [CrossRef]
- Stinson, E.J.; Graham, A.L.; Thearle, M.S.; Gluck, M.E.; Krakoff, J.; Piaggi, P. Cognitive Dietary Restraint, Disinhibition, and Hunger Are Associated with 24-h Energy Expenditure. Int. J. Obes. 2005 2019, 43, 1456–1465. [Google Scholar] [CrossRef] [PubMed]
- Habhab, S.; Sheldon, J.P.; Loeb, R.C. The Relationship between Stress, Dietary Restraint, and Food Preferences in Women. Appetite 2009, 52, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Karakose, T.; Yirci, R.; Basyigit, H.; Kucukcakir, A. Investigation of Associations between the Effects of COVID-19 Fear on School Administrators and Nutrition and Problematic Eating Behaviors. Prog. Nutr. 2021, 23, e2021187. [Google Scholar] [CrossRef]
- McAtamney, K.; Mantzios, M.; Egan, H.; Wallis, D.J. Emotional Eating during COVID-19 in the United Kingdom: Exploring the Roles of Alexithymia and Emotion Dysregulation. Appetite 2021, 161, 105120. [Google Scholar] [CrossRef]
- Papandreou, C.; Arija, V.; Aretouli, E.; Tsilidis, K.K.; Bulló, M. Comparing Eating Behaviours, and Symptoms of Depression and Anxiety between Spain and Greece during the COVID-19 Outbreak: Cross-Sectional Analysis of Two Different Confinement Strategies. Eur. Eat. Disord. Rev. 2020, 28, 836–846. [Google Scholar] [CrossRef]
- Clark, A.J.; Salo, P.; Lange, T.; Jennum, P.; Virtanen, M.; Pentti, J.; Kivimäki, M.; Rod, N.H.; Vahtera, J. Onset of Impaired Sleep and Cardiovascular Disease Risk Factors: A Longitudinal Study. Sleep 2016, 39, 1709–1718. [Google Scholar] [CrossRef]
- Lao, X.Q.; Liu, X.; Deng, H.-B.; Chan, T.-C.; H, K.F.; Wang, F.; Vermeulen, R.; Tam, T.; Wong, M.C.S.; Tse, L.A.; et al. Sleep Quality, Sleep Duration, and the Risk of Coronary Heart Disease: A Prospective Cohort Study with 60,586 Adults. J. Clin. Sleep Med. 2018, 14, 109–117. [Google Scholar] [CrossRef] [Green Version]
- Newman, A.B.; Nieto, F.J.; Guidry, U.; Lind, B.K.; Redline, S.; Shahar, E.; Pickering, T.G.; Quan for the Sleep Heart Health Study Research Group. Relation of Sleep-Disordered Breathing to Cardiovascular Disease Risk Factors: The Sleep Heart Health Study. Am. J. Epidemiol. 2001, 154, 50–59. [Google Scholar] [CrossRef] [Green Version]
- Ibarra-Coronado, E.G.; Pantaleón-Martínez, A.M.; Velazquéz-Moctezuma, J.; Prospéro-García, O.; Méndez-Díaz, M.; Pérez-Tapia, M.; Pavón, L.; Morales-Montor, J. The Bidirectional Relationship between Sleep and Immunity against Infections. J. Immunol. Res. 2015, 2015, e678164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Motivala, S.J.; Irwin, M.R. Sleep and Immunity: Cytokine Pathways Linking Sleep and Health Outcomes. Curr. Dir. Psychol. Sci. 2007, 16, 21–25. [Google Scholar] [CrossRef]
- Bénard, M.; Bellisle, F.; Etilé, F.; Reach, G.; Kesse-Guyot, E.; Hercberg, S.; Péneau, S. Impulsivity and Consideration of Future Consequences as Moderators of the Association between Emotional Eating and Body Weight Status. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 84. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.-M.; Lee, K.; Sung, J.; Yang, Y.; Yang, Y.J. Changes in Eating Behaviors and Body Weight in Koreans: The Healthy Twin Study. Nutr. Burbank Los Angel. Cty. Calif 2013, 29, 66–70. [Google Scholar] [CrossRef]
- Koenders, P.G.; van Strien, T. Emotional Eating, Rather than Lifestyle Behavior, Drives Weight Gain in a Prospective Study in 1562 Employees. J. Occup. Environ. Med. 2011, 53, 1287–1293. [Google Scholar] [CrossRef]
- Hung, H.-C.; Yang, Y.-C.; Ou, H.-Y.; Wu, J.-S.; Lu, F.-H.; Chang, C.-J. The Association between Self-Reported Sleep Quality and Metabolic Syndrome. PLoS ONE 2013, 8, e54304. [Google Scholar] [CrossRef]
- Ohayon, M.M.; Reynolds, C.F.; Dauvilliers, Y. Excessive Sleep Duration and Quality of Life. Ann. Neurol. 2013, 73, 785–794. [Google Scholar] [CrossRef]
- Bel, S.; Michels, N.; Vriendt, T.D.; Patterson, E.; Cuenca-García, M.; Diethelm, K.; Gutin, B.; Grammatikaki, E.; Manios, Y.; Leclercq, C.; et al. Association between Self-Reported Sleep Duration and Dietary Quality in European Adolescents. Br. J. Nutr. 2013, 110, 949–959. [Google Scholar] [CrossRef]
- Chaput, J.-P.; Tremblay, A. Adequate Sleep to Improve the Treatment of Obesity. CMAJ 2012, 184, 1975–1976. [Google Scholar] [CrossRef] [Green Version]
- Dashti, H.S.; Scheer, F.A.; Jacques, P.F.; Lamon-Fava, S.; Ordovás, J.M. Short Sleep Duration and Dietary Intake: Epidemiologic Evidence, Mechanisms, and Health Implications. Adv. Nutr. 2015, 6, 648–659. [Google Scholar] [CrossRef]
- Vgontzas, A.N.; Lin, H.-M.; Papaliaga, M.; Calhoun, S.; Vela-Bueno, A.; Chrousos, G.P.; Bixler, E.O. Short Sleep Duration and Obesity: The Role of Emotional Stress and Sleep Disturbances. Int. J. Obes. 2008, 32, 801–809. [Google Scholar] [CrossRef] [Green Version]
- Benham, G. Stress and Sleep in College Students Prior to and during the COVID-19 Pandemic. Stress Health 2020, 37, 504–515. [Google Scholar] [CrossRef] [PubMed]
- Du, C.; Zan, M.C.H.; Cho, M.J.; Fenton, J.I.; Hsiao, P.Y.; Hsiao, R.; Keaver, L.; Lai, C.-C.; Lee, H.; Ludy, M.-J.; et al. Increased Resilience Weakens the Relationship between Perceived Stress and Anxiety on Sleep Quality: A Moderated Mediation Analysis of Higher Education Students from 7 Countries. Clocks Sleep 2020, 2, 334–353. [Google Scholar] [CrossRef] [PubMed]
- Du, C.; Zan, M.C.H.; Cho, M.J.; Fenton, J.I.; Hsiao, P.Y.; Hsiao, R.; Keaver, L.; Lai, C.-C.; Lee, H.; Ludy, M.-J.; et al. The Effects of Sleep Quality and Resilience on Perceived Stress, Dietary Behaviors, and Alcohol Misuse: A Mediation-Moderation Analysis of Higher Education Students from Asia, Europe, and North America during the COVID-19 Pandemic. Nutrients 2021, 13, 442. [Google Scholar] [CrossRef] [PubMed]
- Hyun, S.; Hahm, H.C.; Wong, G.T.F.; Zhang, E.; Liu, C.H. Psychological Correlates of Poor Sleep Quality among U.S. Young Adults during the COVID-19 Pandemic. Sleep Med. 2021, 78, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Marelli, S.; Castelnuovo, A.; Somma, A.; Castronovo, V.; Mombelli, S.; Bottoni, D.; Leitner, C.; Fossati, A.; Ferini-Strambi, L. Impact of COVID-19 Lockdown on Sleep Quality in University Students and Administration Staff. J. Neurol. 2021, 268, 8–15. [Google Scholar] [CrossRef]
- Fitzsimmons-Craft, E.E.; Karam, A.M.; Monterubio, G.E.; Taylor, C.B.; Wilfley, D.E. Screening for Eating Disorders on College Campuses: A Review of the Recent Literature. Curr. Psychiatry Rep. 2019, 21, 101. [Google Scholar] [CrossRef]
- Grammer, A.C.; Fitzsimmons-Craft, E.E.; Laing, O.; Pietro, B.D.; Wilfley, D.E. Eating Disorders on College Campuses in the United States: Current Insight on Screening, Prevention, and Treatment. Curr. Psychopharmacol. 2020, 9, 91–102. [Google Scholar] [CrossRef]
- Marchi, M.; Cohen, P. Early Childhood Eating Behaviors and Adolescent Eating Disorders. J. Am. Acad. Child Adolesc. Psychiatry 1990, 29, 112–117. [Google Scholar] [CrossRef]
- Stice, E.; Marti, C.N.; Rohde, P. Prevalence, Incidence, Impairment, and Course of the Proposed DSM-5 Eating Disorder Diagnoses in an 8-Year Prospective Community Study of Young Women. J. Abnorm. Psychol. 2013, 122, 445–457. [Google Scholar] [CrossRef] [Green Version]
- Volpe, U.; Tortorella, A.; Manchia, M.; Monteleone, A.M.; Albert, U.; Monteleone, P. Eating Disorders: What Age at Onset? Psychiatry Res. 2016, 238, 225–227. [Google Scholar] [CrossRef] [PubMed]
- Flynn, M.; Austin, A.; Lang, K.; Allen, K.; Bassi, R.; Brady, G.; Brown, A.; Connan, F.; Franklin-Smith, M.; Glennon, D.; et al. Assessing the Impact of First Episode Rapid Early Intervention for Eating Disorders on Duration of Untreated Eating Disorder: A Multi-Centre Quasi-Experimental Study. Eur. Eat. Disord. Rev. J. Eat. Disord. Assoc. 2021, 29, 458–471. [Google Scholar] [CrossRef]
- Center for Colegiate Mental Health (CCMH) 2017 Annual Report. Available online: https://sites.psu.edu/ccmh/files/2018/01/2017_CCMH_Report-1r3iri4.pdf (accessed on 1 April 2021).
- Prichard, J.R.; Hartmann, M.E. Follow-up to Hartmann & Prichard: Should Universities Invest in Promoting Healthy Sleep? A Question of Academic and Economic Significance. Sleep Health 2019, 5, 320–325. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, M.E.; Prichard, J.R. Calculating the Contribution of Sleep Problems to Undergraduates’ Academic Success. Sleep Health 2018, 4, 463–471. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, A.; Schlarb, A.A. Let’s Talk about Sleep: A Systematic Review of Psychological Interventions to Improve Sleep in College Students. J. Sleep Res. 2018, 27, 4–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hershner, S.; O’Brien, L.M. The Impact of a Randomized Sleep Education Intervention for College Students. J. Clin. Sleep Med. JCSM Off. Publ. Am. Acad. Sleep Med. 2018, 14, 337–347. [Google Scholar] [CrossRef] [Green Version]
- Bowen, L. Assessing the Effectiveness of Online Cognitive Behavioral Therapy in Adults with Chronic Insomnia: A Systematic Review and Meta-Analysis. Lynchburg J. Med. Sci. 2019, 1, 3. [Google Scholar]
- Sohn, S.I.; Kim, D.H.; Lee, M.Y.; Cho, Y.W. The Reliability and Validity of the Korean Version of the Pittsburgh Sleep Quality Index. Sleep Breath. Schlaf Atm. 2012, 16, 803–812. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).