Risk Factors Associated with the Consumption of Sugar-Sweetened Beverages among Czech Adults: The Kardiovize Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Data Collection
2.3. Variables Definition
2.4. Ethics Approval
2.5. Statistical Analysis
3. Results
3.1. Participants’ Characteristics
3.2. Prevalence of SSBs Consumption
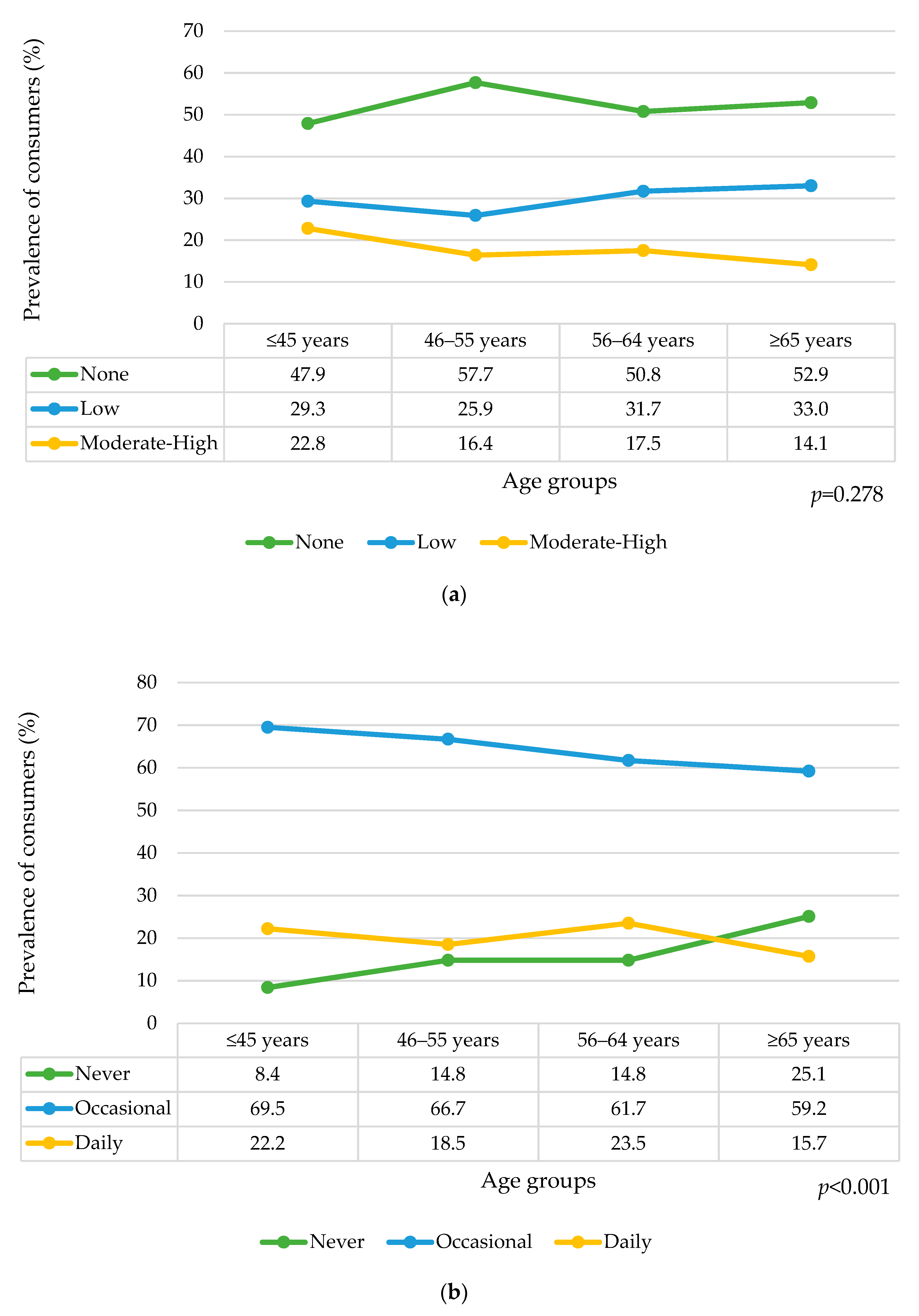
3.2.1. By Calorie Amount
3.2.2. By Frequency
3.3. SSBs Consumption and Cardiometabolic Biomarkers
3.3.1. By Calorie Amount
3.3.2. By Frequency
3.4. SSBs Consumption and Behavioral Risks Factors
3.4.1. By Calorie Amount
3.4.2. By Frequency
3.5. SSBs Consumption and Socioeconomic Determinants
3.5.1. By Calorie Amount
3.5.2. By Frequency
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pereira, M.A. Sugar-Sweetened and Artificially-Sweetened Beverages in Relation to Obesity Risk. Adv. Nutr. 2014, 5, 797–808. [Google Scholar] [CrossRef] [PubMed]
- Luger, M.; Lafontan, M.; Bes-Rastrollo, M.; Winzer, E.; Yumuk, V.; Farpour-Lambert, N. Sugar-Sweetened Beverages and Weight Gain in Children and Adults: A Systematic Review from 2013 to 2015 and a Comparison with Previous Studies. Obes Facts 2017, 10, 674–693. [Google Scholar] [CrossRef] [PubMed]
- Garduño-Alanís, A.; Malyutina, S.; Pajak, A.; Stepaniak, U.; Kubinova, R.; Denisova, D.; Pikhart, H.; Peasey, A.; Bobak, M.; Stefler, D. Association between Soft Drink, Fruit Juice Consumption and Obesity in Eastern Europe: Cross-sectional and Longitudinal Analysis of the HAPIEE Study. J. Hum. Nutr. Diet. 2020, 33, 66–77. [Google Scholar] [CrossRef] [PubMed]
- Guzman-Vilca, W.C.; Yovera-Juarez, E.A.; Tarazona-Meza, C.; García-Larsen, V.; Carrillo-Larco, R.M. Sugar-Sweetened Beverage Consumption in Adults: Evidence from a National Health Survey in Peru. Nutrients 2022, 14, 582. [Google Scholar] [CrossRef]
- Singh, G.M.; Micha, R.; Khatibzadeh, S.; Lim, S.; Ezzati, M.; Mozaffarian, D. Estimated Global, Regional, and National Disease Burdens Related to Sugar-Sweetened Beverage Consumption in 2010. Circulation 2015, 132, 639–666. [Google Scholar] [CrossRef]
- Sartor, F.; Donaldson, L.F.; Markland, D.A.; Loveday, H.; Jackson, M.J.; Kubis, H.-P. Taste Perception and Implicit Attitude toward Sweet Related to Body Mass Index and Soft Drink Supplementation. Appetite 2011, 57, 237–246. [Google Scholar] [CrossRef]
- Hernández-López, R.; Canto-Osorio, F.; Vidaña-Pérez, D.; Torres-Ibarra, L.; Rivera-Paredez, B.; Gallegos-Carrillo, K.; Velazquez, R.; Ramírez, P.; Barrientos-Gutiérrez, T.; Salmerón, J.; et al. Soft Drink and Non-Caloric Soft Drink Intake and Their Association with Blood Pressure: The Health Workers Cohort Study. Nutr. J. 2022, 21, 37. [Google Scholar] [CrossRef]
- Malik, V.S.; Hu, F.B. Sugar-Sweetened Beverages and Cardiometabolic Health: An Update of the Evidence. Nutrients 2019, 11, 1840. [Google Scholar] [CrossRef]
- Meng, Y.; Li, S.; Khan, J.; Dai, Z.; Li, C.; Hu, X.; Shen, Q.; Xue, Y. Sugar- and Artificially Sweetened Beverages Consumption Linked to Type 2 Diabetes, Cardiovascular Diseases, and All-Cause Mortality: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. Nutrients 2021, 13, 2636. [Google Scholar] [CrossRef]
- Popkin, B.M.; Hawkes, C. Sweetening of the Global Diet, Particularly Beverages: Patterns, Trends, and Policy Responses. Lancet Diabetes Endocrinol. 2016, 4, 174–186. [Google Scholar] [CrossRef]
- Statistics|Eurostat. Frequency of Drinking Sugar-Sweetened Soft Drinks by Sex, Age and Educational Attainment Level. Available online: https://ec.europa.eu/eurostat/databrowser/view/hlth_ehis_fv7e/default/bar?lang=en (accessed on 13 September 2022).
- European Commission; Statistical Office of the European Union. European Health Interview Survey (EHIS Wave 3): Methodological Manual: 2020 Edition (Re Edition); Publications Office: Luxemburgo, 2020. [Google Scholar]
- Cobiac, L.J.; Tam, K.; Veerman, L.; Blakely, T. Taxes and Subsidies for Improving Diet and Population Health in Australia: A Cost-Effectiveness Modelling Study. PLoS Med. 2017, 14, e1002232. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Taxes on Sugary Drinks: Why Do It? 2017. Available online: https://apps.who.int/iris/handle/10665/260253 (accessed on 20 July 2022).
- Movsisyan, N.K.; Vinciguerra, M.; Lopez-Jimenez, F.; Kunzová, Š.; Homolka, M.; Jaresova, J.; Cífková, R.; Sochor, O. Kardiovize Brno 2030, a Prospective Cardiovascular Health Study in Central Europe: Methods, Baseline Findings and Future Directions. Eur. J. Prev. Cardiolog. 2018, 25, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Czech Health Statistics Yearbook 2019. Available online: https://www.uzis.cz/en/publications/czech-health-statistics-yearbook-2019 (accessed on 9 August 2022).
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research Electronic Data Capture (REDCap)—A Metadata-Driven Methodology and Workflow Process for Providing Translational Research Informatics Support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- NutriPro Expert. Available online: https://nutripro.cz/ (accessed on 24 August 2022).
- Looman, M.; Boshuizen, H.C.; Feskens, E.J.; Geelen, A. Using Enhanced Regression Calibration to Combine Dietary Intake Estimates from 24 h Recall and FFQ Reduces Bias in Diet–Disease Associations. Public Health Nutr. 2019, 22, 2738–2746. [Google Scholar] [CrossRef] [PubMed]
- Guideline: Sugars Intake for Adults and Children; World Health Organization: Geneva, Switzerland, 2015; ISBN 978-92-4-154902-8. Available online: https://www.who.int/publications/i/item/9789241549028 (accessed on 25 August 2022).
- Polito, A.; Intorre, F.; Ciarapica, D.; Barnaba, L.; Tagliabue, A.; Ferraris, C.; Zaccaria, M. Physical Activity Assessment in an Italian Adult Population Using the International Physical Activity Questionnaire. Obes. Res. Open J. 2016, 3, 43–52. [Google Scholar] [CrossRef]
- Maugeri, A.; Barchitta, M.; Kunzova, S.; Bauerova, H.; Agodi, A.; Vinciguerra, M. The Association of Social and Behavioral Factors with Dietary Risks in Adults: Evidence from the Kardiovize Brno 2030 Study. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 896–906. [Google Scholar] [CrossRef]
- Ma, J.; Sloan, M.; Fox, C.S.; Hoffmann, U.; Smith, C.E.; Saltzman, E.; Rogers, G.T.; Jacques, P.F.; McKeown, N.M. Sugar-Sweetened Beverage Consumption Is Associated with Abdominal Fat Partitioning in Healthy Adults. J. Nutr. 2014, 144, 1283–1290. [Google Scholar] [CrossRef]
- Odegaard, A.O.; Choh, A.C.; Czerwinski, S.A.; Towne, B.; Demerath, E.W. Sugar-Sweetened and Diet Beverages in Relation to Visceral Adipose Tissue. Obesity 2012, 20, 689–691. [Google Scholar] [CrossRef]
- Malik, V.S.; Hu, F.B. Fructose and Cardiometabolic Health. J. Am. Coll. Cardiol. 2015, 66, 1615–1624. [Google Scholar] [CrossRef]
- Jung, S.H.; Ha, K.H.; Kim, D.J. Visceral Fat Mass Has Stronger Associations with Diabetes and Prediabetes than Other Anthropometric Obesity Indicators among Korean Adults. Yonsei Med. J. 2016, 57, 674. [Google Scholar] [CrossRef]
- Payne, A.N.; Chassard, C.; Lacroix, C. Gut Microbial Adaptation to Dietary Consumption of Fructose, Artificial Sweeteners and Sugar Alcohols: Implications for Host-Microbe Interactions Contributing to Obesity: Fructose Impacts on Gut Microbiota and Obesity. Obes. Rev. 2012, 13, 799–809. [Google Scholar] [CrossRef] [PubMed]
- Vallianou, N.; Stratigou, T.; Christodoulatos, G.S.; Dalamaga, M. Understanding the Role of the Gut Microbiome and Microbial Metabolites in Obesity and Obesity-Associated Metabolic Disorders: Current Evidence and Perspectives. Curr. Obes Rep. 2019, 8, 317–332. [Google Scholar] [CrossRef] [PubMed]
- Ramne, S.; Brunkwall, L.; Ericson, U.; Gray, N.; Kuhnle, G.G.C.; Nilsson, P.M.; Orho-Melander, M.; Sonestedt, E. Gut Microbiota Composition in Relation to Intake of Added Sugar, Sugar-Sweetened Beverages and Artificially Sweetened Beverages in the Malmö Offspring Study. Eur. J. Nutr. 2021, 60, 2087–2097. [Google Scholar] [CrossRef] [PubMed]
- von Philipsborn, P.; Stratil, J.M.; Burns, J.; Busert, L.K.; Pfadenhauer, L.M.; Polus, S.; Holzapfel, C.; Hauner, H.; Rehfuess, E. Environmental Interventions to Reduce the Consumption of Sugar-Sweetened Beverages and Their Effects on Health. Cochrane Database Syst. Rev. 2019, 6, CD012292. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. ‘Best Buys’ and Other Recommended Interventions for the Prevention and Control of Noncommunicable Diseases. 2017. Available online: https://apps.who.int/iris/bitstream/handle/10665/259232/WHO-NMH-NVI-17.9-eng.pdf (accessed on 12 October 2022).
- Thow, A.M.; Rippin, H.L.; Mulcahy, G.; Duffey, K.; Wickramasinghe, K. Sugar-Sweetened Beverage Taxes in Europe: Learning for the Future. Eur. J. Public Health 2022, 32, 273–280. [Google Scholar] [CrossRef]
- Bandy, L.K.; Scarborough, P.; Harrington, R.A.; Rayner, M.; Jebb, S.A. Reductions in Sugar Sales from Soft Drinks in the UK from 2015 to 2018. BMC Med. 2020, 18, 20. [Google Scholar] [CrossRef]
- Schwendicke, F.; Stolpe, M. Taxing Sugar-Sweetened Beverages: Impact on Overweight and Obesity in Germany. BMC Public Health 2017, 17, 88. [Google Scholar] [CrossRef]
- Eykelenboom, M.; van Stralen, M.M.; Olthof, M.R.; Renders, C.M.; Steenhuis, I.H.; PEN Consortium. Public Acceptability of a Sugar-Sweetened Beverage Tax and Its Associated Factors in the Netherlands. Public Health Nutr. 2021, 24, 2354–2364. [Google Scholar] [CrossRef]
- Sbírka zákonů. Vyhláška č. 282/2016 Sb.—VYHLÁŠKA o požadavcích na Potraviny, Pro Které je Přípustná Reklama a Které lze Nabízet k Prodeji a Prodávat ve Školách a Školských Zařízeních. Available online: https://www.msmt.cz/ministerstvo/novinar/pamlskova-zacne-platit-20-zari-2016 (accessed on 11 April 2022).
- Naska, A.; Lagiou, A.; Lagiou, P. Dietary Assessment Methods in Epidemiological Research: Current State of the Art and Future Prospects. F1000Research 2017, 6, 926. [Google Scholar] [CrossRef]
- Keyes, K.M.; Rutherford, C.; Popham, F.; Martins, S.S.; Gray, L. How Healthy Are Survey Respondents Compared with the General Population?: Using Survey-Linked Death Records to Compare Mortality Outcomes. Epidemiology 2018, 29, 299–307. [Google Scholar] [CrossRef]
- Sousa, A.; Sych, J.; Rohrmann, S.; Faeh, D. The Importance of Sweet Beverage Definitions When Targeting Health Policies—The Case of Switzerland. Nutrients 2020, 12, 1976. [Google Scholar] [CrossRef] [PubMed]
| Men | Women | Total | p-Value | ||
|---|---|---|---|---|---|
| Participants, n (%) | 346 (47.4) | 384 (52.6) | 730 (100) | ||
| Age (years) | 54.5 (10.9) | 55.9 (10.6) | 55.2 (10.8) | 0.079 | |
| Weight (kg) | 87.7 (13.9) | 72.1 (15.1) | 79.5 (16.5) | <0.001 | |
| Height (cm) | 180.4 (7.1) | 167.1 (6.5) | 173.4 (9.5) | <0.001 | |
| BMI (kg/m2) | 26.9 (4.0) | 25.8 (5.4) | 26.3 (4.8) | 0.001 | |
| Waist circumference (cm) | 98.2 (11.7) | 87.0 (13.5) | 92.3 (13.9) | <0.001 | |
| Visceral fat area (cm2) | 94.7 (41.8) | 108.4 (51.8) | 101.9 (47.8) | <0.001 | |
| Systolic Blood Pressure (mmHg) | 120.1 (13.6) | 118.0 (15.8) | 119.0 (14.8) | 0.047 | |
| Diastolic Blood Pressure (mmHg) | 78.6 (8.7) | 74.3 (8.9) | 76.4 (9.1) | <0.001 | |
| Total cholesterol (mmol/L) | 5.2 (0.9) | 5.4 (0.9) | 5.3 (0.9) | 0.004 | |
| HDL-cholesterol (mmol/L) | 1.3 (0.3) | 1.7 (0.4) | 1.5 (0.4) | <0.001 | |
| LDL-cholesterol (mmol/L) | 3.3 (0.9) | 3.3 (0.9) | 3.3 (0.9) | 0.630 | |
| Fasting Triglycerides (mmol/L) | 1.4 (0.7) | 1.1 (0.5) | 1.2 (0.7) | <0.001 | |
| Fasting blood glucose (mmol/L) | 5.5 (1.1) | 5.2 (0.8) | 5.3 (1.0) | <0.001 | |
| Hypertension | 41.6 (36.7–46.8) | 31.5 (27.3–36.2) | 36.3 (32.9–39.4) | 0.005 | |
| Physical activity level | Active | 46.2 (40.9–51.7) | 40.1 (35.1–44.9) | 43.0 (39.5–46.6) | |
| Minimally active | 36.7 (31.4–41.9) | 43.8 (38.9–48.8) | 40.4 (37.0–44.1) | 0.141 | |
| Inactive | 17.1 (13.1–21.1) | 16.1 (12.6–19.9) | 16.6 (14.1–19.3) | ||
| Smoking habit | Never smoker | 14.7 (11.3–18.6) | 15.1 (11.6–18.6) | 14.9 (12.3–17.5) | |
| Past smoker | 32.4 (27.4–37.3) | 26.3 (22.1–30.7) | 29.2 (25.8–32.6) | 0.185 | |
| Current smoker | 52.9 (47.8–58.0) | 58.6 (54.0–63.5) | 55.9 (52.3–59.5) | ||
| Alcohol intake | None | 59.5 (54.5–65.0) | 70.3 (65.5–74.9) | 65.2 (61.6–68.8) | |
| Middle | 16.2 (12.4–19.9) | 19.3 (15.4–23.2) | 17.8 (15.1–20.8) | <0.001 | |
| High | 24.3 (19.9–28.9) | 10.4 (7.6–13.6) | 17.0 (14.1–19.7) | ||
| Total energy intake (kcal/day) | <2000 | 42.8 (37.5–47.7) | 72.4 (68.1–76.7) | 58.4 (54.8–62.1) | |
| 2000–2500 | 28.0 (23.2–32.9) | 20.6 (16.6–24.8) | 24.1 (21.1–27.4) | <0.001 | |
| >2500 | 29.2 (24.5–34.3) | 7.0 (4.6–9.6) | 17.5 (14.8–20.3) | ||
| Education level | High | 51.4 (46.5–56.4) | 38.8 (34.0–43.6) | 44.8 (41.8–48.1) | |
| Medium | 28.0 (23.2–32.9) | 39.6 (34.5–44.5) | 34.1 (30.7–37.8) | 0.001 | |
| Low | 20.5 (16.1–25.0) | 21.6 (17.8–25.7) | 21.1 (18.4–24.1) | ||
| Household income | High | 37.3 (32.1–42.2) | 18.0 (14.4–22.1) | 27.1 (24.0–30.3) | |
| Middle | 48.3 (42.8–53.5) | 49.2 (44.3–54.3) | 48.8 (45.2–52.6) | <0.001 | |
| Low | 14.5 (10.8–18.2) | 32.8 (28.1–37.6) | 24.1 (21.1–27.1) | ||
| SSBs Consumption | Men | Women | Total | p-Value |
|---|---|---|---|---|
| By calorie amount | ||||
| None | 47.1 (42.1–52.3) | 57.3 (52.6–62.8) | 52.5 (49.0–55.9) | <0.001 |
| Low | 29.5 (24.9–34.3) | 30.5 (25.4–35.0) | 30.0 (26.4–33.7) | |
| Moderate–High | 23.4 (19.0–28.0) | 12.2 (9.0–15.7) | 17.5 (14.8–20.3) | |
| By frequency | ||||
| Never | 11.8 (8.3–15.3) | 19.8 (15.7–23.9) | 16.0 (13.3–18.8) | |
| Occasional | 59.8 (55.0–64.9) | 68.0 (63.2–72.5) | 64.1 (60.7–67.3) | <0.001 |
| Daily | 28.3 (23.8–33.1) | 12.2 (8.9–15.6) | 19.9 (17.0–22.7) |
| By Calorie Amount | By Frequency | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Sex | None | Low | Moderate–High | p-Value | Never | Occasional | Daily | p-Value | |
| Waist circumference (cm) | M | 98.2 (11.2) | 96.9 (12.9) | 99.9 (11.1) | 0.222 | 96.6 (12.5) | 96.8 (11.2) | 101.9 (11.9) | 0.001 |
| W | 87.1 (14.1) | 85.5 (11.7) | 90.0 (14.4) | 0.152 | 85.3 (13.8) | 86.8 (12.6) | 90.7 (17.0) | 0.092 | |
| Visceral fat area (cm2) | M | 95.6 (43.6) | 90.3 (41.2) | 98.4 (38.5) | 0.397 | 92.9 (48.6) | 90.3 (40.4) | 104.7 (40.1) | 0.018 |
| W | 109.5 (53.3) | 103.5 (49.1) | 116.7 (50.8) | 0.317 | 105.4 (56.2) | 107.2 (48.6) | 121.1 (60.6) | 0.200 | |
| Systolic Blood Pressure (mmHg) | M | 120.3 (13.3) | 118.7 (14.3) | 121.6 (13.4) | 0.348 | 121.8 (14.8) | 119.4 (13.2) | 121.0 (14.0) | 0.468 |
| W | 118.8 (16.7) | 115.9 (13.9) | 118.9 (15.7) | 0.238 | 117.9 (17.0) | 117.8 (15.7) | 118.8 (14.9) | 0.933 | |
| Diastolic Blood Pressure (mmHg) | M | 78.6 (8.9) | 77.3 (7.9) | 80.2 (8.9) | 0.089 | 78.3 (10.2) | 78.2 (8.4) | 79.5 (8.6) | 0.465 |
| W | 74.5 (9.4) | 73.4 (7.9) | 75.8 (8.5) | 0.278 | 73.2 (8.4) | 74.5 (9.2) | 75.2 (8.2) | 0.389 | |
| Total cholesterol (mmol/L) | M | 5.2 (1.0) | 5.2 (1.0) | 5.3 (0.9) | 0.654 | 5.3 (1.1) | 5.2 (1.0) | 5.3 (0.9) | 0.721 |
| W | 5.4 (0.9) | 5.4 (1.1) | 5.4 (1.1) | 0.996 | 5.5 (0.9) | 5.4 (1.0) | 5.5 (1.0) | 0.778 | |
| HDL-cholesterol (mmol/L) | M | 1.3 (0.3) | 1.3 (0.3) | 1.3 (0.4) | 0.808 | 1.3 (0.4) | 1.3 (0.3) | 1.3 (0.3) | 0.908 |
| W | 1.7 (0.4) | 1.6 (0.3) | 1.6 (0.3) | 0.235 | 1.7 (0.4) | 1.7 (0.4) | 1.6 (0.4) | 0.444 | |
| LDL-cholesterol (mmol/L) | M | 3.3 (0.9) | 3.2 (0.9) | 3.3 (0.9) | 0.568 | 3.4 (0.9) | 3.3 (0.9) | 3.3 (0.9) | 0.662 |
| W | 3.2 (0.8) | 3.3 (1.0) | 3.3 (0.9) | 0.786 | 3.2 (0.9) | 3.2 (0.9) | 3.4 (1.0) | 0.728 | |
| Fasting Triglycerides (mmol/L) | M | 1.3 (0.6) | 1.3 (0.8) | 1.5 (0.9) | 0.224 | 1.3 (0.6) | 1.3 (0.7) | 1.5 (0.8) | 0.066 |
| W | 1.1 (0.6) | 1.1 (0.5) | 1.1 (0.4) | 0.676 | 1.1 (0.5) | 1.1 (0.6) | 1.1 (0.5) | 0.769 | |
| Fasting blood glucose (mmol/L) | M | 5.6 (1.3) | 5.4 (0.9) | 5.5 (0.9) | 0.446 | 5.6 (1.0) | 5.4 (1.1) | 5.6 (1.1) | 0.439 |
| W | 5.3 (0.9) | 5.1 (0.6) | 5.3 (0.9) | 0.275 | 5.2 (0.8) | 5.2 (0.8) | 5.3 (1.0) | 0.627 | |
| By Calorie Amount | By Frequency | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| None | Low | Moderate–High | p-Value | Never | Occasional | Daily | p-Value | ||
| Total | 47.1 (42.1–52.3) | 29.5 (24.9–34.3) | 23.4 (19.0–28.0) | 11.8 (8.3–15.3) | 59.8 (55.0–64.9) | 28.3 (23.8–33.1) | |||
| Physical activity | Active | 47.5 (40.2–54.9) | 28.1 (21.5–35.1) | 24.4 (18.2–31.3) | 13.8 (9.0–19.6) | 55.0 (47.4–62.2) | 31.3 (24.2–38.3) | ||
| Minimally | 46.5 (37.7–55.5) | 33.9 (25.6–43.1) | 19.7 (12.5–26.4) | 0.532 | 9.4 (4.5–15.0) | 66.9 (58.5–74.8) | 23.6 (16.8–31.1) | 0.352 | |
| Inactive | 47.5 (34.7–60.6) | 23.7 (13.1–35.3) | 28.8 (17.6–40.7) | 11.9 (3.6–20.0) | 57.6 (45.0–70.2) | 30.5 (19.4–43.1) | |||
| Smoking | Never | 43.1 (28.6–57.1) | 35.3 (23.3–49.0) | 21.6 (10.5–34.2) | 11.8 (3.6–21.3) | 51.0 (36.2–64.9) | 37.3 (24.5–52.1) | ||
| Past | 50.9 (40.9–60.0) | 27.7 (19.8–35.9) | 21.4 (14.0–30.5) | 0.775 | 15.2 (8.7–21.6) | 59.8 (50.0–69.4) | 25.0 (17.7–33.3) | 0.353 | |
| Current | 45.9 (38.8–53.6) | 29.0 (22.5–35.6) | 25.1 (19.0–31.1) | 9.8 (5.5–14.6) | 62.3 (54.6–69.0) | 27.9 (21.5–34.5) | |||
| Alcohol intake | 0 | 45.6 (38.6–52.4) | 28.6 (22.0–35.0) | 25.7 (19.6–32.0) | 13.1 (8.6–18.1) | 58.7 (52.0–65.9) | 28.2 (21.9–34.4) | ||
| >0–20 | 48.2 (34.4–61.5) | 23.2 (11.8–35.6) | 28.6 (16.7–40.3) | 0.181 | 12.5 (4.3–22.0) | 62.5 (49.0–75.5) | 25.0 (13.7–36.4) | 0.788 | |
| >20 | 50.0 (39.2–61.3) | 35.7 (25.3–46.0) | 14.3 (7.2–21.6) | 8.3 (2.8–14.9) | 60.7 (50.0–70.9) | 31.0 (21.4–41.5) | |||
| Total energy intake | <2000 | 52.0 (43.8–60.0) | 27.7 (20.0–34.8) | 20.3 (13.9–26.8) | 15.5 (10.2–21.9) | 64.2 (56.2–71.9) | 20.3 (14.0–26.7) | ||
| 2000–2500 | 46.4 (36.1–56.1) | 27.8 (19.3–37.5) | 25.8 (16.9–34.9) | 0.460 | 11.3 (5.4–18.3) | 59.8 (50.0–70.0) | 28.9 (19.8–38.0) | 0.012 | |
| >2500 | 40.6 (30.6–50.0) | 33.7 (23.9–42.9) | 25.7 (17.4–34.1) | 6.9 (2.1–12.4) | 53.5 (43.6–63.9) | 39.6 (29.9–49.1) | |||
| Household income | High | 46.5 (38.1–55.2) | 29.5 (21.1–37.1) | 24.0 (16.5–31.5) | 11.6 (6.5–17.4) | 67.4 (59.7–75.0) | 20.9 (13.9–28.3) | ||
| Middle | 50.9 (43.2–59.0) | 29.9 (22.8–37.2) | 19.2 (13.6–25.2) | 0.160 | 10.2 (5.7–15.5) | 59.3 (51.9–66.7) | 30.5 (23.7–37.1) | 0.026 | |
| Low | 36.0 (22.6–50.0) | 28.0 (15.4–41.1) | 36.0 (23.9–50.0) | 18.0 (7.4–28.6) | 42.0 (27.5–56.5) | 40.0 (26.5–54.4) | |||
| Education level | High | 51.1 (43.1–59.0) | 24.2 (17.8–30.9) | 24.7 (18.2–31.2) | 12.4 (7.9–17.7) | 64.0 (56.4–71.3) | 23.6 (17.6–29.7) | ||
| Medium | 41.2 (30.9–51.5) | 35.1 (25.6–45.5) | 23.7 (15.6–31.8) | 0.244 | 8.2 (3.3–14.1) | 58.8 (49.5–69.1) | 33.0 (23.3–42.9) | 0.175 | |
| Low | 45.1 (33.9–57.1) | 35.2 (24.3–47.3) | 19.7 (10.1–29.0) | 15.5 (7.7–24.4) | 50.7 (39.2–62.3) | 33.8 (22.5–44.9) | |||
| By Calorie Amount | By Frequency | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| None | Low | Moderate–High | p-Value | Never | Occasional | Daily | p-Value | ||
| Total | 57.3 (52.6–62.8) | 30.5 (25.4–35.0) | 12.2 (9.0–15.7) | 19.8 (15.7–23.9) | 68.0 (63.2–72.5) | 12.2 (8.9–15.6) | |||
| Physical activity | Active | 59.7 (51.3–67.3) | 28.6 (21.9–35.5) | 11.7 (6.7–17.2) | 24.7 (18.0–32.1) | 62.3 (54.5–70.0) | 13.0 (7.8–18.5) | ||
| Minimally | 56.5 (49.1–64.1) | 29.2 (22.6–36.5) | 14.3 (9.0–19.8) | 0.476 | 17.3 (12.0–23.3) | 73.8 (66.9–80.4) | 8.9 (4.9–13.9) | 0.061 | |
| Inactive | 53.2 (40.0–65.3) | 38.7 (26.3–50.9) | 8.1 (1.7–15.4) | 14.5 (5.8–24.2) | 66.1 (54.4–77.4) | 19.4 (9.4–29.5) | |||
| Smoking | Never | 55.2 (41.0–68.6) | 31.0 (19.6–44.4) | 13.8 (5.3–23.1) | 22.4 (11.9–34.0) | 63.8 (50.0–75.9) | 13.8 (5.4–23.9) | ||
| Past | 58.4 (48.1–68.0) | 32.7 (23.2–42.2) | 8.9 (3.7–14.3) | 0.813 | 19.8 (12.0–27.7) | 64.4 (55.7–74.2) | 15.8 (8.9–23.6) | 0.597 | |
| Current | 57.3 (50.4–63.8) | 29.3 (23.6–35.5) | 13.3 (8.8–17.8) | 19.1 (13.7–23.9) | 70.7 (64.9–76.8) | 10.2 (6.3–14.1) | |||
| Alcohol intake | 0 | 57.8 (51.7–63.7) | 29.3 (23.7–34.9) | 13.0 (9.2–17.0) | 18.9 (14.2–23.5) | 68.1 (62.7–73.3) | 13.0 (8.9–17.2) | ||
| >0–20 | 55.4 (43.7–66.7) | 35.1 (24.3–46.5) | 9.5 (3.2–16.2) | 0.861 | 17.6 (9.3–26.2) | 77.0 (67.5–86.1) | 5.4 (1.2–11.5) | 0.039 | |
| >20 | 57.5 (42.4–73.2) | 30.0 (16.7–43.9) | 12.5 (2.9–23.5) | 30.0 (16.1–44.1) | 50.0 (35.3–66.0) | 20.0 (7.7–32.4) | |||
| Total energy intake | <2000 | 61.9 (56.3–67.7) | 25.9 (20.8–31.2) | 12.2 (8.6–16.2) | 22.3 (17.3–27.0) | 67.6 (62.3–73.3) | 10.1 (6.5–13.8) | ||
| 2000–2500 | 46.8 (35.9–57.5) | 40.5 (30.0–52.1) | 12.7 (6.2–20.8) | 0.025 | 12.7 (5.7–20.5) | 72.2 (61.9–82.2) | 15.2 (7.7–23.3) | 0.049 | |
| >2500 | 40.7 (22.2–60.0) | 48.1 (28.0–66.7) | 11.1 (0.0–24.2) | 14.8 (3.4–28.1) | 59.3 (40.6–78.6) | 25.9 (10.0–44.8) | |||
| Household income | High | 59.4 (47.1–71.8) | 31.9 (20.3–42.6) | 8.7 (2.8–16.0) | 14.5 (7.2–24.2) | 76.8 (65.8–86.1) | 8.7 (2.9–16.0) | ||
| Middle | 60.3 (53.3–67.6) | 29.1 (22.6–35.8) | 10.6 (6.4–15.4) | 0.348 | 19.6 (13.8–25.0) | 67.7 (61.3–74.4) | 12.7 (8.2–17.4) | 0.446 | |
| Low | 51.6 (41.8–60.6) | 31.7 (24.0–40.5) | 16.7 (10.3–23.8) | 23.0 (15.9–30.5) | 63.5 (54.7–72.0) | 13.5 (7.7–19.8) | |||
| Education level | High | 65.1 (58.2–72.3) | 28.9 (21.4–36.1) | 6.0 (2.4–9.8) | 20.1 (13.9–26.5) | 73.8 (66.9–80.8) | 6.0 (2.6–9.9) | ||
| Medium | 50.0 (42.4–57.8) | 33.6 (26.6–40.5) | 16.4 (11.2–22.8) | 0.022 | 19.1 (13.3–25.4) | 64.5 (56.6–72.0) | 16.4 (10.8–22.6) | 0.062 | |
| Low | 56.6 (45.7–67.4) | 27.7 (18.2–37.5) | 15.7 (8.3–23.9) | 20.5 (12.1–29.1) | 63.9 (53.6–73.5) | 15.7 (7.8–23.9) | |||
| By Calorie Amount | By Frequency | ||||
|---|---|---|---|---|---|
| Low | Moderate–High | Occasional | Daily | ||
| Physical activity | Active | 1 | 1 | 1 | 1 |
| Minimally active | 1.14 (0.79–1.64) | 1.00 (0.64–1.57) | 1.77 (1.12–2.78) | 1.06 (0.60–1.86) | |
| Inactive | 1.17 (0.72–1.90) | 1.10 (0.61–1.96) | 1.60 (0.86–2.98) | 1.72 (0.84–3.53) | |
| Smoking | Never | 1 | 1 | 1 | 1 |
| Past | 0.81 (0.48–1.37) | 0.76 (0.39–1.48) | 1.08 (0.57–2.05) | 0.78 (0.37–1.67) | |
| Current | 0.84 (0.52–1.36) | 1.00 (0.55–1.82) | 1.25 (0.69–2.27) | 0.80 (0.40–1.62) | |
| Alcohol intake | None | 1 | 1 | 1 | 1 |
| Middle | 0.91 (0.51–1.60) | 1.67 (0.80–3.48) | 1.55 (0.75–3.19) | 0.74 (0.31–1.79) | |
| High | 0.88 (0.56–1.38) | 1.71 (0.93–3.12) | 1.24 (0.69–2.22) | 0.95 (0.49–1.85) | |
| Total energy intake | <2000 | 1 | 1 | 1 | 1 |
| 2000–2500 | 1.61 (1.07–2.43) | 1.41 (0.86–2.31) | 1.46 (0.85–2.49) | 2.22 (1.17–4.21) | |
| >2500 | 2.08 (1.28–3.38) | 1.55 (0.87–2.74) | 1.45 (0.71–2.97) | 3.80 (1.75–8.26) | |
| Household income | High | 1 | 1 | 1 | 1 |
| Middle | 0.91 (0.60–1.38) | 0.39 (0.56–1.54) | 0.99 (0.57–1.73) | 1.75 (0.89–3.41) | |
| Low | 1.15 (0.68–1.95) | 2.30 (1.24–4.26) | 0.79 (0.41–1.50) | 1.96 (0.89–4.33) | |
| Education level | High | 1 | 1 | 1 | 1 |
| Middle | 1.66 (1.13–2.44) | 1.75 (1.09–2.79) | 1.14 (0.71–1.89) | 2.25 (1.24–4.08) | |
| Low | 1.35 (0.86–2.11) | 1.38 (0.80–2.39) | 0.88 (0.51–1.50) | 1.78 (0.93–3.41) | |
| By Calorie Amount | By Frequency | ||||
|---|---|---|---|---|---|
| Low | Moderate–High | Occasional | Daily | ||
| Physical activity | Active | 1 | 1 | 1 | 1 |
| Minimally active | 1.24 (0.85–1.82) | 1.04 (0.66–1.66) | 1.78 (1.12–2.82) | 1.20 (0.67–2.15) | |
| Inactive | 1.26 (0.77–2.05) | 1.10 (0.60–2.00) | 1.69 (0.9–3.19) | 2.02 (0.96–4.23) | |
| Smoking | Never | 1 | 1 | 1 | 1 |
| Past | 0.83 (0.49–1.42) | 0.74 (0.37–1.46) | 1.15 (0.60–2.21) | 0.86 (0.39–1.87) | |
| Current | 0.90 (0.55–1.49) | 1.01 (0.54–1.89) | 1.30 (0.71–2.40) | 0.92 (0.44–1.93) | |
| Alcohol intake | None | 1 | 1 | 1 | 1 |
| Middle | 1.02 (0.57–1.84) | 1.91 (0.89–4.10) | 1.57 (0.74–3.32) | 0.94 (0.37–2.37) | |
| High | 1.02 (0.63–1.65) | 2.00 (1.06–3.76) | 1.28 (0.70–2.36) | 1.18 (0.58–2.39) | |
| Total energy intake | <2000 | 1 | 1 | 1 | 1 |
| 2000–2500 | 1.71 (1.12–2.60) | 1.55 (0.93–2.59) | 1.15 (0.88–2.64) | 2.44 (1.26–4.70) | |
| >2500 | 2.32 (1.39–3.85) | 1.88 (1.03–3.44) | 1.65 (0.78–3.45) | 4.76 (2.11–10.76) | |
| Household income | High | 1 | 1 | 1 | 1 |
| Middle | 0.80 (0.51–1.24) | 0.83 (0.48–1.42) | 1.00 (0.57–1.78) | 1.52 (0.74–3.09) | |
| Low | 0.94 (0.53–1.66) | 2.05 (1.05–4.00) | 0.77 (0.39–1.53) | 1.54 (0.65–3.64) | |
| Education level | High | 1 | 1 | 1 | 1 |
| Middle | 1.87 (1.24–2.84) | 1.72 (1.03–2.86) | 1.35 (0.80–2.26) | 2.42 (1.27–4.62) | |
| Low | 1.52 (0.94–2.48) | 1.31 (0.71–2.41) | 1.05 (0.59–1.87) | 1.87 (0.91–3.85) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kunzova, M.; Neto, G.A.M.; Infante-Garcia, M.M.; Nieto-Martinez, R.; González-Rivas, J.P. Risk Factors Associated with the Consumption of Sugar-Sweetened Beverages among Czech Adults: The Kardiovize Study. Nutrients 2022, 14, 5297. https://doi.org/10.3390/nu14245297
Kunzova M, Neto GAM, Infante-Garcia MM, Nieto-Martinez R, González-Rivas JP. Risk Factors Associated with the Consumption of Sugar-Sweetened Beverages among Czech Adults: The Kardiovize Study. Nutrients. 2022; 14(24):5297. https://doi.org/10.3390/nu14245297
Chicago/Turabian StyleKunzova, Monika, Geraldo A. Maranhao Neto, María M. Infante-Garcia, Ramfis Nieto-Martinez, and Juan P. González-Rivas. 2022. "Risk Factors Associated with the Consumption of Sugar-Sweetened Beverages among Czech Adults: The Kardiovize Study" Nutrients 14, no. 24: 5297. https://doi.org/10.3390/nu14245297
APA StyleKunzova, M., Neto, G. A. M., Infante-Garcia, M. M., Nieto-Martinez, R., & González-Rivas, J. P. (2022). Risk Factors Associated with the Consumption of Sugar-Sweetened Beverages among Czech Adults: The Kardiovize Study. Nutrients, 14(24), 5297. https://doi.org/10.3390/nu14245297






