A Year in the Life of U.S. Frontline Health Care Workers: Impact of COVID-19 on Weight Change, Physical Activity, Lifestyle Habits, and Psychological Factors
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Measures
2.4. Analytic Strategy
3. Results
3.1. Descriptive Analysis
3.2. Eating Pattern Changes Related to the COVID-19 Pandemic
3.3. Weight Changes Related to the COVID-19 Pandemic
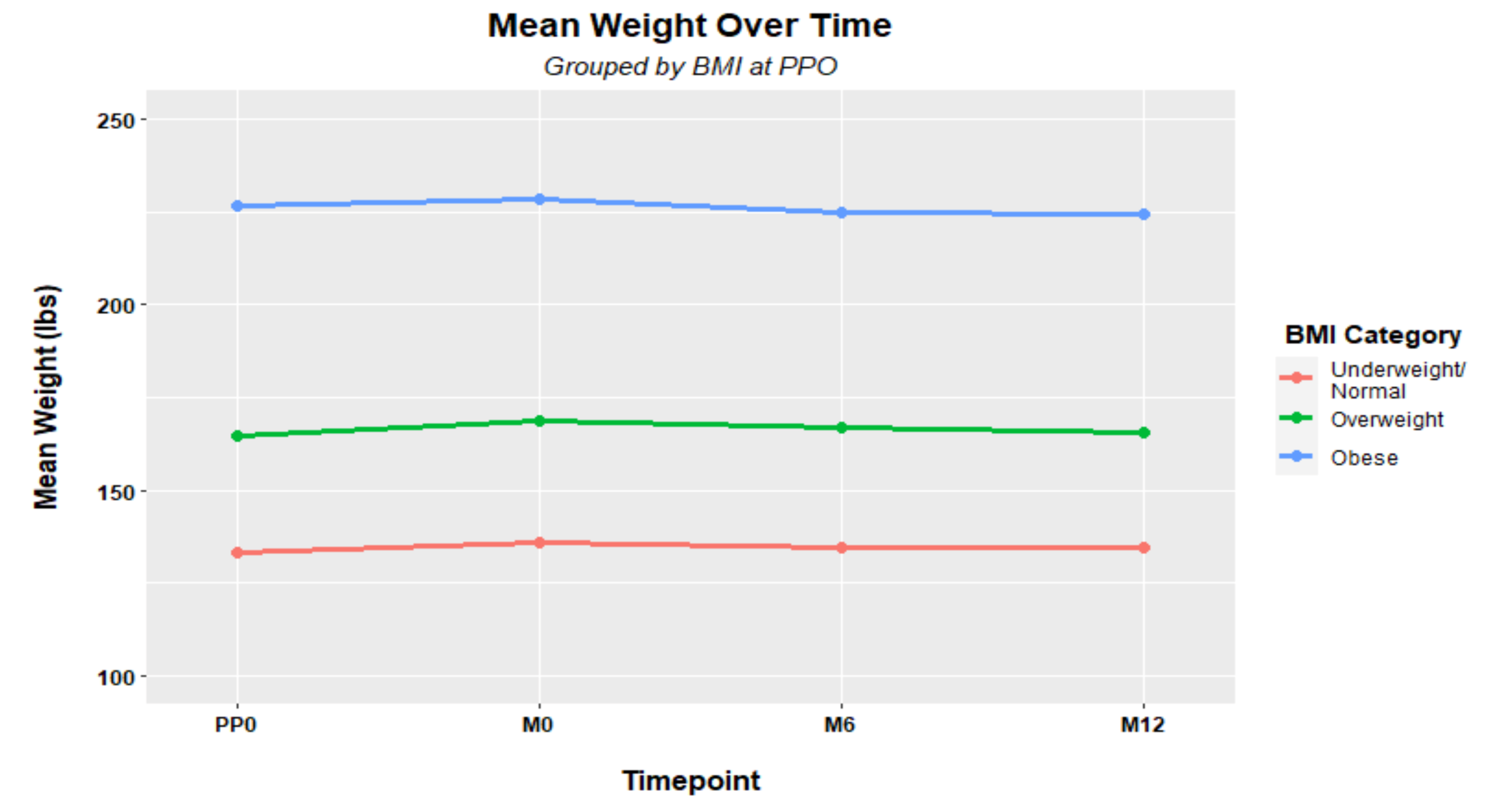
Weight Changes Associated with BMI Category
3.4. Physical Activity Changes Related to the COVID-19 Pandemic
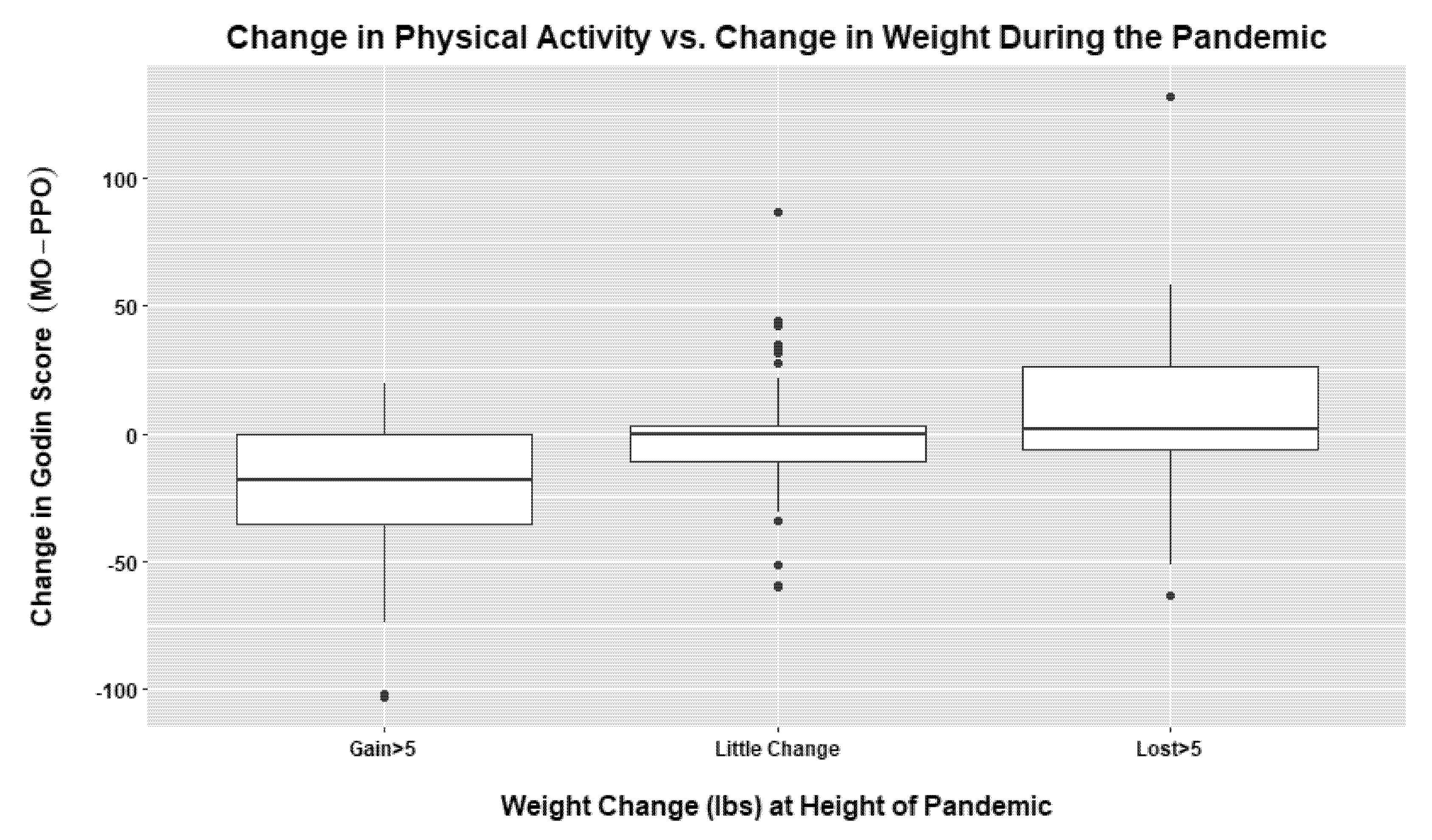
3.4.1. Physical Activity Changes Associated with Weight Changes
3.4.2. Physical Activity Changes Associated with Psychological Factors
3.5. Psychological Factors Related to the COVID-19 Pandemic
3.5.1. Depression
3.5.2. Anxiety
3.5.3. Insomnia
4. Discussion
4.1. COVID-19 Impacts on Eating Patterns
4.2. COVID-19 Impact on Weight Changes
4.3. COVID-19 Impact on Physical Activity
4.4. COVID-19 Impacts on Psychological Factors
4.5. Next Steps
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Variables | Total |
|---|---|
| Gender (n = 234) | |
| Male, n (%) | 30 (12.8) |
| Female, n (%) | 203 (86.8) |
| Gender non-conforming, n (%) | 1 (0.4) |
| Age, mean (SD), years | 38.69 (12) |
| Race (n = 234) | n (%) |
| Black/African American | 6 (2.6) |
| Latinx/Hispanic | 2 (0.9) |
| White/Non-Hispanic | 215 (91.9) |
| Asian/Pacific Islander | 4 (1.7) |
| Multi-racial/Mixed ethnicities | 5 (2.1) |
| Other | 2 (0.9) |
| Body Mass Index (pre-COVID) (n = 226) | n (%) |
| BMI, mean (SD) | 26.58 (6.22) |
| Underweight | 2 (0.9) |
| Normal | 104 (46.0) |
| Overweight | 70 (31.0) |
| Obesity | 50 (22.1) |
| Highest education level (n = 233) | n (%) |
| High school degree or equivalent (e.g., GED) | 2 (0.9) |
| Some college or trade school | 11 (4.7) |
| Associates or Technical Degree | 6 (2.6) |
| Bachelor’s degree | 114 (48.9) |
| Master’s degree | 75 (32.2) |
| Doctoral Degree (e.g., JD, MD, PhD) | 25 (10.7) |
| Job Role (n = 234) | |
| Aide | 4 (1.7) |
| Emergency Medical Technician (including EMTs, AEMTs, and EMRs) | 7 (3.0) |
| Housekeeping Services | 1 (0.4) |
| Occupational Therapist | 3 (1.3) |
| Medical Assistant | 1 (0.4) |
| Nurse (e.g., including RN, CRNP, CRNA, Nursing Assistant, LPN) | 151 (64.5) |
| Paramedic | 12 (5.1) |
| Pharmacist | 5 (2.1) |
| Physician Assistant | 1 (0.4) |
| Pharmacy technician | 2 (0.9) |
| Physical Therapist | 6 (2.6) |
| Physician | 8 (3.4) |
| Police Officer | 2 (0.9) |
| Reception/Unit Clerk/Administrative Assistant | 1 (0.4) |
| Registered Dietitian | 4 (1.7) |
| Social Work | 10 (4.3) |
| Other (please describe) | 16 (6.8) |
| Part-time or full-time status (n = 234) | n (%) |
| Part-time | 52 (22.2) |
| Full-time (>35 h per week) | 182 (77.8) |
| Eating Pattern Changes |
|
| Weight Change |
|
| Physical Activity (PA) |
|
| Psychological Factors at CHAMPS Parent and PA |
|
References
- Carroll, N.; Sadowski, A.; Laila, A.; Hruska, J.; Nixon, M.; Ma, D.W.L.; Haines, J. The Impact of COVID-19 on Health Behavior, Stress, Financial and Food Security among Middle to High Income Canadian Families with Young Children. Nutrients 2020, 12, 2352. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attina, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 8, 229. [Google Scholar] [CrossRef]
- Oni, T.; Micklesfield, L.K.; Wadende, P.; Obonyo, C.O.; Woodcock, J.; Mogo, E.R.I.; Odunitan-Wayas, F.A.; Assah, F.; Tatah, L.; Foley, L.; et al. Implications of COVID-19 control measures for diet and physical activity, and lessons for addressing other pandemics facing rapidly urbanising countries. Glob. Health Action 2020, 13, 1810415. [Google Scholar] [CrossRef] [PubMed]
- Puhl, R.; Lessard, L.; Larson, N.; Eisenberg, M.; Neumark-Stzainer, D. Weight Stigma as a Predictor of Distress and Maladaptive Eating Behaviors During COVID-19: Longitudinal Findings from the EAT Study. Ann. Behav. Med. 2020, 54, 738–746. [Google Scholar] [CrossRef]
- Khan, M.A.; Menon, P.; Govender, R.; Abu Samra, A.M.; Allaham, K.K.; Nauman, J.; Östlundh, L.; Mustafa, H.; Smith, J.E.M.; AlKaabi, J.M. Systematic review of the effects of pandemic confinements on body weight and their determinants. Br. J. Nutr. 2022, 127, 298–317. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. CDC Museum COVID-19 Timeline. Available online: https://www.cdc.gov/museum/timeline/covid19.html (accessed on 17 October 2022).
- Statistia. Number of Cumulative Cases of COVID-19 in the United States from 20 January 2020 to 20 October 2022, by Day. Available online: https://www.statista.com/statistics/1103185/cumulative-coronavirus-covid19-cases-number-us-by-day/ (accessed on 17 October 2022).
- Becker’s Hospital Review. 16 Most Notable COVID-19 Developments of 2021: A Timeline. Available online: https://www.beckershospitalreview.com/public-health/16-most-notable-covid-19-developments-of-2021-a-timeline.html (accessed on 17 October 2022).
- Danet Danet, A. Psychological impact of COVID-19 pandemic in Western frontline healthcare professionals. A systematic review. Med. Clin. 2021, 156, 449–458. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, N. Mental health of healthcare workers in the COVID-19 era. Nat. Rev. Nephrol. 2020, 16, 425–426. [Google Scholar] [CrossRef]
- Barello, S.; Palamenghi, L.; Graffigna, G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. 2020, 290, 113129. [Google Scholar] [CrossRef] [PubMed]
- Firew, T.; Sano, E.D.; Lee, J.W.; Flores, S.; Lang, K.; Salman, K.; Greene, M.C.; Chang, B.P. Protecting the front line: A cross-sectional survey analysis of the occupational factors contributing to healthcare workers’ infection and psychological distress during the COVID-19 pandemic in the USA. BMJ Open 2020, 10, e042752. [Google Scholar] [CrossRef]
- Khasne, R.W.; Dhakulkar, B.S.; Mahajan, H.C.; Kulkarni, A.P. Burnout among Healthcare Workers during COVID-19 Pandemic in India: Results of a Questionnaire-based Survey. Indian J. Crit. Care Med. 2020, 24, 664–671. [Google Scholar] [CrossRef]
- Marvaldi, M.; Mallet, J.; Dubertret, C.; Moro, M.R.; Guessoum, S.B. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2021, 126, 252–264. [Google Scholar] [CrossRef]
- Moitra, M.; Rahman, M.; Collins, P.Y.; Gohar, F.; Weaver, M.; Kinuthia, J.; Rössler, W.; Petersen, S.; Unutzer, J.; Saxena, S.; et al. Mental Health Consequences for Healthcare Workers During the COVID-19 Pandemic: A Scoping Review to Draw Lessons for LMICs. Front. Psychiatry 2021, 12, 602614. [Google Scholar] [CrossRef]
- Norful, A.A.; Rosenfeld, A.; Schroeder, K.; Travers, J.L.; Aliyu, S. Primary drivers and psychological manifestations of stress in frontline healthcare workforce during the initial COVID-19 outbreak in the United States. Gen. Hosp. Psychiatry 2021, 69, 20–26. [Google Scholar] [CrossRef]
- Kazmierski, K.F.M.; Gillespie, M.L.; Kuo, S. Stress-Induced eating among racial/ethnic groups in the United States: A Systematic Review. J. Racial Ethn. Health Disparities 2020, 8, 912–926. [Google Scholar] [CrossRef]
- Khaled, K.; Tsofliou, F.; Hundley, V.; Helmreich, R.; Almilaji, O. Perceived stress and diet quality in women of reproductive age: A systematic review and meta-analysis. Nutr. J. 2020, 19, 92. [Google Scholar] [CrossRef]
- Neill, E.; Meyer, D.; Toh, W.L.; van Rheenen, T.E.; Phillipou, A.; Tan, E.J.; Rossell, S.L. Alcohol use in Australia during the early days of the COVID-19 pandemic: Initial results from the COLLATE project. Psychiatry Clin. Neurosci. 2020, 74, 542–549. [Google Scholar] [CrossRef]
- Buss, J. Associations between obesity and stress and shift work among nurses. Workplace Health Saf. 2012, 60, 453–458. [Google Scholar] [CrossRef]
- Antentas, J.M.; Vivas, E. Impact of the economic crisis on the right to a healthy diet. SESPAS report 2014. Gac. Sanit. 2014, 28, 58–61. [Google Scholar] [CrossRef]
- Epel, E.; Lapidus, R.; McEwen, B.; Brownell, K. Stress may add bite to appetite in women: A laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology 2001, 26, 37–49. [Google Scholar] [CrossRef]
- O’Connor, D.B.; Jones, F.; Conner, M.; McMillan, B.; Ferguson, E. Effects of daily hassles and eating style on eating behavior. Health Psychol. 2008, 27 (Suppl. S1), S20–S31. [Google Scholar] [CrossRef]
- González-Monroy, C.; Gómez-Gómez, I.; Olarte-Sánchez, C.M.; Motrico, E. Eating behaviour changes during the COVID-19 pandemic: A systematic review of longitudinal studies. Int. J. Environ. Res. Public Health 2021, 18, 11130. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. The Health Effects of Overweight and Obesity. 2021. Available online: https://www.cdc.gov/healthyweight/effects/index.html (accessed on 19 February 2021).
- Hoedl, M.; Bauer, S.; Eglseer, D. Influence of nursing staff working hours on the stress level during the COVID-19 pandemic: A cross-sectional online survey. HBScience 2020, 12, 92–98. [Google Scholar] [CrossRef]
- Melnyk, B.M.; Hsieh, A.P.; Tan, A.; Teall, A.M.; Weberg, D.; Jun, J.; Gawlik, K.; Hoying, J. Associations Among Nurses’ Mental/Physical Health, Lifestyle Behaviors, Shift Length, and Workplace Wellness Support During COVID-19. Nurs. Adm. Q. 2021, 46, 5–18. [Google Scholar] [CrossRef]
- Zachary, Z.; Forbes, B.; Lopez, B.; Pederson, G.; Welty, J.; Deyo, A.; Kerekes, M. Self-quarantine and weight gain related risk factors during the COVID-19 pandemic. Obes. Clin. Pract. 2020, 14, 210–216. [Google Scholar] [CrossRef]
- Lin, A.L.; Vittinghoff, E.; Olgin, J.E.; Pletcher, M.J.; Marcus, G.M. Body weight changes during pandemic-related shelter-in-place in a longitudinal cohort study. JAMA Netw. Open 2021, 4, e212536. [Google Scholar] [CrossRef]
- Agarwal, M.; Ravi, P.; Ramesh, C.; Neslin, J. Impact of the COVID-19 pandemic on the mental health of people. Int. J. Community Med. Public Health 2021, 8, 1305–1311. [Google Scholar] [CrossRef]
- Herrero San Martin, A.; Parra Serrano, J.; Diaz Cambriles, T.; Arias Arias, E.M.; Muñoz Méndez, J.; del Yerro Álvarez, M.J.; González Sánchez, M. Sleep characteristics in health workers exposed to the COVID-19 pandemic. Sleep Med. 2020, 75, 388–394. [Google Scholar] [CrossRef]
- Van Steenkiste, E.; Schoofs, J.; Gilis, S.; Messiaen, P. Mental health impact of COVID-19 in frontline healthcare workers in a Belgian Tertiary care hospital: A prospective longitudinal study. Acta Clin. Belg. 2021, 77, 533–540. [Google Scholar] [CrossRef]
- Jahrami, H.; BaHammam, A.S.; AlGahtani, H.; Ebrahim, A.; Faris, M.; AlEid, K.; Saif, Z.; Haji, E.; Dhahi, A.; Marzooq, H.; et al. The examination of sleep quality for frontline healthcare workers during the outbreak of COVID-19. Sleep Breath 2021, 25, 503–511. [Google Scholar] [CrossRef]
- Cabarkapa, S.; Nadjidai, S.E.; Murgier, J.; Ng, C.H. The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: A rapid systematic review. Brain Behav. Immun. Health 2020, 8, 100144. [Google Scholar] [CrossRef]
- Bhutani, S.; vanDellen, M.R.; Cooper, J.A. Longitudinal weight gain and related risk behaviors during the COVID-19 pandemic in adults in the US. Nutrients 2021, 13, 671. [Google Scholar] [CrossRef]
- Kaufmann, P.G.; Havens, D.S.; Mensinger, J.L.; Bradley, P.K.; Brom, H.M.; Copel, L.C.; Costello, A.; D’Annunzio, C.; Dean Durning, J.; Maldonado, L.; et al. The COVID-19 Study of Healthcare and Support Personnel (CHAMPS): Objectives and Design. JMIR Res. Protoc. 2021, 10, e30757. [Google Scholar] [CrossRef]
- Qualtrics [Computer Software]. (2021). Qualtrics. Available online: https://www.qualtrics.com/core-xm/ (accessed on 10 May 2022).
- Godin, G. The Godin-Shephard leisure-time physical activity questionnaire. Health Fit. J. Canada 2011, 4, 18–22. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Med. Care 2003, 41, 1284–1292. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022; Available online: https://www.R-project.org/ (accessed on 10 May 2022).
- Chew, H.S.J.; Lopez, V. Global Impact of COVID-19 on Weight and Weight-Related Behaviors in the Adult Population: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 1876. [Google Scholar] [CrossRef]
- Dicken, S.J.; Mitchell, J.J.; Newberry Le Vay, J.; Beard, E.; Kale, D.; Herbec, A.; Shahab, L. Impact of COVID-19 Pandemic on Weight and BMI among UK Adults: A Longitudinal Analysis of Data from the HEBECO Study. Nutrients 2021, 13, 2911. [Google Scholar] [CrossRef]
- Lopez-Minguez, J.; Gómez-Abellán, P.; Garaulet, M. Timing of Breakfast, Lunch, and Dinner. Effects on Obesity and Metabolic Risk. Nutrients 2019, 11, 2624. [Google Scholar] [CrossRef]
- Manoogian, E.N.C.; Chaix, A.; Panda, S. When to Eat: The Importance of Eating Patterns in Health and Disease. J. Biol. Rhythms 2019, 34, 579–581. [Google Scholar] [CrossRef]
- American Psychological Association. STRESS IN AMERICA™ One Year Later, A New Wave of Pandemic Health Concerns. Available online: https://www.apa.org/news/press/releases/stress/2021/one-year-pandemic-stress (accessed on 15 December 2021).
- Almeida, A.L.C.; Melo, M.; Rodrigues, R.E.F.; Botelho, L.F.; Almeida, P.A.A.; Barberato, S.H. Impact of COVID-19 on the Life of Brazilian Cardiologists and Cardiovascular Surgeons. Arq. Bras. Cardiol. 2021, 117, 1048–1055. [Google Scholar] [CrossRef]
- Vitale, E.; Mea, R.; Di Dio, F.; Canonico, A.; Galatola, V. Anxiety, Insomnia and Body Mass Index Scores in Italian Nurses Engaged in the Care of COVID-19 Patients. Endocr. Metab. Immune Disord. Drug Targets 2021, 21, 1604–1612. [Google Scholar] [CrossRef]
- Zhang, J.; Lai, S.; Lyu, Q.; Zhang, P.; Yang, D.; Kong, J.; Qi, Y.; Yuan, W.; Zeng, S.; Song, P.; et al. Diet and Nutrition of Healthcare Workers in COVID-19 Epidemic-Hubei, China, 2019. China CDC Wkly. 2020, 3, 505–506. [Google Scholar] [CrossRef] [PubMed]
- Freedman, D.S.; Kompaniyets, L.; Daymont, C.; Zhao, L.; Blanck, H.M. Weight gain among US adults during the COVID-19 pandemic through May 2021. Obesity 2022, 30, 2064–2070. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Exercise or Physical Activity. 2021. Available online: https://www.cdc.gov/nchs/fastats/exercise.htm (accessed on 6 June 2021).
- Robinson, E.; Sutin, A.R.; Daly, M.; Jones, A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 2022, 296, 567–576. [Google Scholar] [CrossRef]
- COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Th’ng, F.; Rao, K.A.; Ge, L.; Mao, D.; Neo, H.N.; Molina, J.A.D.; Seow, E. A One-Year Longitudinal Study: Changes in Depression and Anxiety in Frontline Emergency Department Healthcare Workers in the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 11228. [Google Scholar] [CrossRef]
- Steinmetz, L.C.L.; Herrera, C.R.; Fong, S.B.; Godoy, J.C. A Longitudinal Study on the Changes in Mental Health of Healthcare Workers during the COVID-19 Pandemic. Psychiatry 2022, 85, 56–71. [Google Scholar] [CrossRef]
- Nashwan, A.J.; Villar, R.C.; Al-Qudimat, A.R.; Kader, N.; Alabdulla, M.; Abujaber, A.A.; Al-Jabry, M.M.; Harkous, M.; Philip, A.; Ali, R.; et al. Quality of Life, Sleep Quality, Depression, Anxiety, Stress, Eating Habits, and Social Bounds in Nurses during the Coronavirus Disease 2019 Pandemic in Qatar (The PROTECTOR Study): A Cross-Sectional, Comparative Study. J. Pers. Med. 2021, 11, 918. [Google Scholar] [CrossRef]
- Zhou, Y.; Ding, H.; Zhang, Y.; Zhang, B.; Guo, Y.; Cheung, T.; Hall, B.J.; Shi, T.; Xiang, Y.; Tang, Y. Prevalence of poor psychiatric status and sleep quality among frontline healthcare workers during and after the COVID-19 outbreak: A longitudinal study. Transl. Psychiatry 2021, 11, 223. [Google Scholar] [CrossRef]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated with Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef] [PubMed]
| PP0 to M0 | M0 to M6 | M6 to M12 | |
|---|---|---|---|
| Snacking/Grazing | n = 211 | n = 148 | n = 125 |
| Less/Decrease | 15 (7.1) | 28 (18.9) | 21 (22.4) |
| No Change | 49 (23.2) | 59 (39.8) | 54 (47.2) |
| More/Increase | 147 (69.7) | 61 (41.2) | 50 (48.8) |
| Change from previous? | - | p-val < 0.001 | p-val = 0.953 |
| Fast food or take-out consumption | n = 211 | n = 148 | n = 125 |
| Less/Decrease | 27 (12.8) | 27 (18.2) | 17 (13.6) |
| No Change | 62 (29.4) | 83 (56.1) | 73 (58.4) |
| More/Increase | 122 (57.8) | 38 (25.7) | 35 (28.0) |
| Change from previous? | - | p-val < 0.001 | p-val = 0.733 |
| Alcoholic beverage intake | n = 211 | n = 148 | n = 125 |
| Less/Decrease | 25 (11.8) | 26 (17.6) | 19 (15.2) |
| No Change | 83 (39.3) | 91 (61.5) | 81 (64.8) |
| More/Increase | 103 (48.8) | 31 (20.9) | 25 (20.0) |
| Change from previous? | - | p-val < 0.001 | p-val = 0.991 |
| Caffeinated beverage intake | n = 211 | n = 148 | n = 125 |
| Less/Decrease | 6 (2.8) | 11 (7.4) | 11 (8.8) |
| No Change | 104 (49.2) | 81 (54.7) | 66 (52.8) |
| More/Increase | 101 (47.9) | 56 (37.8) | 48 (38.4) |
| Change from previous? | - | p-val = 0.014 | p-val = 0.666 |
| Appetite | n = 211 | n = 148 | n = 125 |
| Less/Decrease | 32 (15.2) | 25 (16.9) | 20 (16.0) |
| No Change | 94 (44.5) | 85 (57.4) | 84 (67.2) |
| More/Increase | 85 (40.3) | 38 (25.7) | 21 (16.8) |
| Change from previous? | - | p-val = 0.063 | p-val = 0.532 |
| Food portion sizes | n = 211 | n = 148 | n = 125 |
| Less/Decrease | 16 (7.6) | 32 (21.6) | 24 (19.2) |
| No Change | 117 (55.5) | 89 (60.1) | 82 (65.6) |
| More/Increase | 78 (37.0) | 27 (18.2) | 19 (15.2) |
| Change from previous? | - | p-val < 0.001 | p-val = 0.224 |
| Sweetened beverage intake | n = 211 | n = 148 | n = 125 |
| Less/Decrease | 13 (6.2) | 16 (10.8) | 9 (7.2) |
| No Change | 161 (76.3) | 116 (78.4) | 106 (84.8) |
| More/Increase | 37 (17.5) | 16 (10.8) | 10 (8.0) |
| Change from previous? | - | p-val = 0.257 | p-val = 0.435 |
| Daily vegetable intake | n = 211 | n = 148 | n = 125 |
| Less/Decrease | 33 (15.6) | 13 (8.7) | 17 (13.6) |
| No Change | 161 (71.6) | 90 (60.8) | 80 (64.0) |
| More/Increase | 37 (12.8) | 45 (30.4) | 28 (22.4) |
| Change from previous? | - | p-val = 0.001 | p-val = 0.324 |
| Daily fruit intake | n = 211 | n = 148 | n = 125 |
| Less/Decrease | 36 (17.1) | 7 (4.7) | 13 (10.4) |
| No Change | 148 (70.1) | 95 (64.2) | 84 (67.2) |
| More/Increase | 27 (12.8) | 46 (31.1) | 28 (22.4) |
| Change from previous? | - | p-val < 0.001 | p-val = 0.196 |
| Do you think your general health changed during the height of the COVID-19 pandemic in your area? (n = 232) | n (%) |
| Yes, I think my health declined | 119 (51.3) |
| No change | 90 (38.8) |
| Yes, I think my health improved | 23 (9.9) |
| Self-reported weight change during height of pandemic (n = 226) | n (%) |
| >10 pounds lost | 16 (7.1) |
| 6–10 pounds lost | 16 (7.1) |
| 1–5 pounds lost | 21 (9.3) |
| No weight change | 40 (17.7) |
| 1–5 pounds gained | 44 (19.5) |
| 6–10 pounds gained | 39 (17.3) |
| >10 pounds gained | 50 (22.1) |
| BMI | PP0 (n = 226) | M0 (n = 226) | M6 (n = 148) | M12 (n = 122) |
|---|---|---|---|---|
| Underweight/Normal | 133.2 (16.2) | 136.0 (17.9) | 134.6 (17.9) | 134.8(19.3) |
| Overweight | 164.5 (15.3) | 168.8 (17.6) | 167.1 (19.4) | 165.4 (23.3) |
| Obesity | 226.8 (43.5) | 228.3 (45.7) | 224.8 (51.4) | 224.4 (52.8) |
| All | 163.6 (43.8) | 166.6 (44.6) | 164.5 (44.5) | 165.1 (46.4) |
| Exercise Level | Prior (n = 218) | Height (n = 218) | M6 (n = 148) | M12 (n = 124) |
|---|---|---|---|---|
| Mild | 3.55 (2.60) | 3.13 (2.62) | 5.17 (3.29) | 4.84 (3.09) |
| Moderate | 2.33 (2.08) | 2.14 (2.47) | 3.84 (2.61) | 3.13 (2.28) |
| Strenuous | 2.12 (2.09) | 1.54 (2.12) | 2.99 (2.17) | 2.69 (2.29) |
| Total | 8.00 (5.09) | 6.80 (5.67) | 12.00 (6.37) | 10.67 (5.78) |
| Godin Score | 41.40 (28.22) | 33.90 (30.92) | 61.64 (33.62) | 54.40 (32.13) |
| Psychological Variable | Category | M0 | M12 |
|---|---|---|---|
| Depression (PHQ-2) (M0: n = 234, M12: n = 124) | None (0) | 69 (29.5) | 51 (41.1) |
| Mild (1) | 42 (17.9) | 20 (16.1) | |
| Moderate (2) | 64 (27.4) | 34 (27.4) | |
| Severe (3–6) | 59 (25.2) | 19 (15.3) | |
| Anxiety (GAD-7) (M0: n = 234, M12: n = 124) | None (0–4) | 69 (29.5) | 58 (46.8) |
| Mild (5–9) | 101 (43.2) | 38 (30.6) | |
| Moderate (10–14) | 42 (17.9) | 16 (12.9) | |
| Severe (15–21) | 22 (9.4) | 12 (9.6) | |
| Insomnia (ISI) (M0: n = 229, M12: n = 124) | Normal (0–7) | 63 (27.5) | 26 (21.0) |
| Subthreshold (8–14) | 99 (43.2) | 57 (46.0) | |
| Moderate (15–21) | 58 (25.3) | 30 (24.2) | |
| Severe (22–28) | 9 (3.9) | 11 (8.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliver, T.L.; Shenkman, R.; Diewald, L.K.; Bernhardt, P.W.; Chen, M.-H.; Moore, C.H.; Kaufmann, P.G. A Year in the Life of U.S. Frontline Health Care Workers: Impact of COVID-19 on Weight Change, Physical Activity, Lifestyle Habits, and Psychological Factors. Nutrients 2022, 14, 4865. https://doi.org/10.3390/nu14224865
Oliver TL, Shenkman R, Diewald LK, Bernhardt PW, Chen M-H, Moore CH, Kaufmann PG. A Year in the Life of U.S. Frontline Health Care Workers: Impact of COVID-19 on Weight Change, Physical Activity, Lifestyle Habits, and Psychological Factors. Nutrients. 2022; 14(22):4865. https://doi.org/10.3390/nu14224865
Chicago/Turabian StyleOliver, Tracy L., Rebecca Shenkman, Lisa K. Diewald, Paul W. Bernhardt, Mu-Hsun Chen, Caroline H. Moore, and Peter G. Kaufmann. 2022. "A Year in the Life of U.S. Frontline Health Care Workers: Impact of COVID-19 on Weight Change, Physical Activity, Lifestyle Habits, and Psychological Factors" Nutrients 14, no. 22: 4865. https://doi.org/10.3390/nu14224865
APA StyleOliver, T. L., Shenkman, R., Diewald, L. K., Bernhardt, P. W., Chen, M.-H., Moore, C. H., & Kaufmann, P. G. (2022). A Year in the Life of U.S. Frontline Health Care Workers: Impact of COVID-19 on Weight Change, Physical Activity, Lifestyle Habits, and Psychological Factors. Nutrients, 14(22), 4865. https://doi.org/10.3390/nu14224865







