Ultra-Processed Food Consumption Associated with Incident Hypertension among Chinese Adults—Results from China Health and Nutrition Survey 1997–2015
Highlights
- This is the first association study that examines Ultra-Processed Food consumption using NOVA classification and incident hypertension in a large cohort of the Chinese adult population.
- The results of this study support the Chinese dietary guidelines published in 2022, in which new recommendations have been supplemented. The new guideline emphasizes the needs to avoid UPF, to acquire knowledge and skills regarding cooking, and to select packaged food by reading food labels in addition to food-based recommendations.
- The study may call for public awareness on the impact of food accessibility and exposure to UPF in terms of health risks, for example, the early onset of hypertension.
Abstract
1. Introduction
2. Research Design and Methods
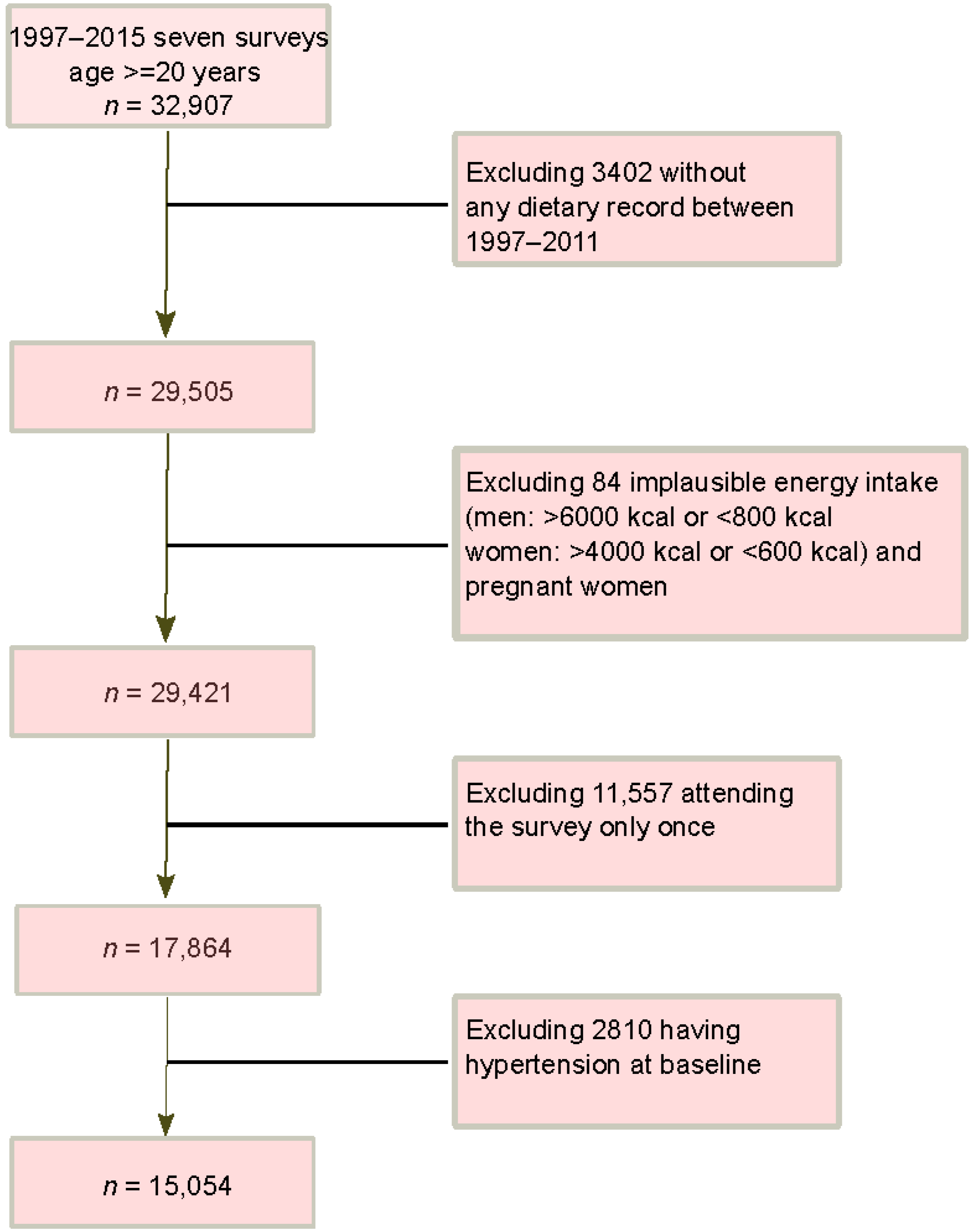
2.1. Study Design and Sample
2.2. Outcome Variable: Incident Hypertension
2.3. Exposure Variable: UPF Consumption
2.4. Covariates
2.5. Statistical Analysis
3. Results
3.1. Population Characteristics and UPF Consumption
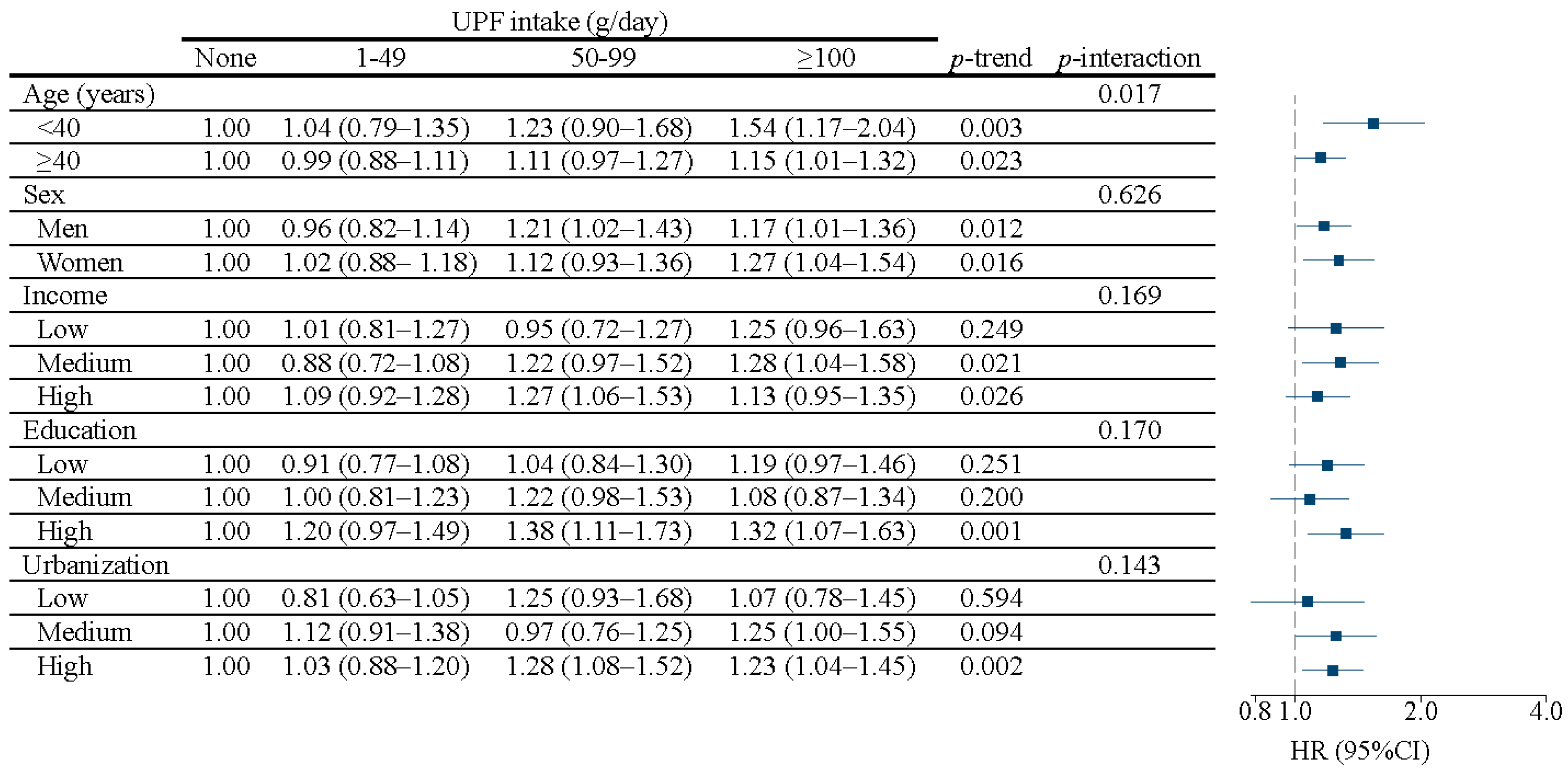
3.2. Incident Hypertension and the Association with UPF Consumption
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhou, B.; Perel, P.; Mensah, G.A.; Ezzati, M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat. Rev. Cardiol. 2021, 18, 785–802. [Google Scholar] [CrossRef] [PubMed]
- NCD Risk Factor Collaboration. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef]
- Yin, R.; Yin, L.; Li, L.; Silva-Nash, J.; Tan, J.; Pan, Z.; Zeng, J.; Yan, L.L. Hypertension in China: Burdens, guidelines and policy responses: A state-of-the-art review. J. Hum. Hypertens 2022, 36, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.; Yang, L.; Zhao, M.; Magnussen, C.G.; Xi, B. Trends in hypertension prevalence, awareness, treatment and control rates among Chinese adults, 1991–2015. J. Hypertens 2021, 39, 740–748. [Google Scholar] [CrossRef]
- Yang, B.Y.; Qian, Z.; Howard, S.W.; Vaughn, M.G.; Fan, S.J.; Liu, K.K.; Dong, G.H. Global association between ambient air pollution and blood pressure: A systematic review and meta-analysis. Environ. Pollut. 2018, 235, 576–588. [Google Scholar] [CrossRef]
- Hu, B.; Liu, X.; Yin, S.; Fan, H.; Feng, F.; Yuan, J. Effects of psychological stress on hypertension in middle-aged Chinese: A cross-sectional study. PLoS ONE 2015, 10, e0129163. [Google Scholar] [CrossRef]
- Shen, Y.; Chang, C.; Zhang, J.; Jiang, Y.; Ni, B.; Wang, Y. Prevalence and risk factors associated with hypertension and prehypertension in a working population at high altitude in China: A cross-sectional study. Environ. Health Prev. Med. 2017, 22, 19. [Google Scholar] [CrossRef]
- Li, L.; Li, L.; Chai, J.X.; Xiao, L.; Ng, C.H.; Ungvari, G.S.; Xiang, Y.T. Prevalence of Poor Sleep Quality in Patients with Hypertension in China: A Meta-analysis of Comparative Studies and Epidemiological Surveys. Front. Psychiatry 2020, 11, 591. [Google Scholar] [CrossRef]
- Du, S.; Batis, C.; Wang, H.; Zhang, B.; Zhang, J.; Popkin, B.M. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. Am. J. Clin. Nutr. 2014, 99, 334–343. [Google Scholar] [CrossRef]
- Huang, L.; Trieu, K.; Yoshimura, S.; Neal, B.; Woodward, M.; Campbell, N.R.C.; Li, Q.; Lackland, D.T.; Leung, A.A.; Anderson, C.A.M.; et al. Effect of dose and duration of reduction in dietary sodium on blood pressure levels: Systematic review and meta-analysis of randomised trials. BMJ 2020, 368, m315. [Google Scholar] [CrossRef]
- Neal, B.; Wu, Y.; Feng, X.; Zhang, R.; Zhang, Y.; Shi, J.; Zhang, J.; Tian, M.; Huang, L.; Li, Z.; et al. Effect of Salt Substitution on Cardiovascular Events and Death. N. Engl. J. Med. 2021, 385, 1067–1077. [Google Scholar] [CrossRef] [PubMed]
- Grillo, A.; Salvi, L.; Coruzzi, P.; Salvi, P.; Parati, G. Sodium Intake and Hypertension. Nutrients 2019, 11, 1970. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guideline: Sodium Intake for Adults and Children; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Schwingshackl, L.; Schwedhelm, C.; Hoffmann, G.; Knuppel, S.; Iqbal, K.; Andriolo, V.; Bechthold, A.; Schlesinger, S.; Boeing, H. Food Groups and Risk of Hypertension: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. Adv. Nutr. 2017, 8, 793–803. [Google Scholar] [CrossRef] [PubMed]
- Xu, R.; Yang, K.; Ding, J.; Chen, G. Effect of green tea supplementation on blood pressure: A systematic review and meta-analysis of randomized controlled trials. Medicine 2020, 99, e19047. [Google Scholar] [CrossRef] [PubMed]
- Appel, L.J.; Moore, T.J.; Obarzanek, E.; Vollmer, W.M.; Svetkey, L.P.; Sacks, F.M.; Bray, G.A.; Vogt, T.M.; Cutler, J.A.; Windhauser, M.M.; et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N. Engl. J. Med. 1997, 336, 1117–1124. [Google Scholar] [CrossRef]
- Ndanuko, R.N.; Tapsell, L.C.; Charlton, K.E.; Neale, E.P.; Batterham, M.J. Dietary Patterns and Blood Pressure in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Adv. Nutr. 2016, 7, 76–89. [Google Scholar] [CrossRef]
- Li, M.; Shi, Z. Dietary Pattern during 1991–2011 and Its Association with Cardio Metabolic Risks in Chinese Adults: The China Health and Nutrition Survey. Nutrients 2017, 9, 1218. [Google Scholar] [CrossRef]
- Xu, H.; Guo, B.; Qian, W.; Ciren, Z.; Guo, W.; Zeng, Q.; Mao, D.; Xiao, X.; Wu, J.; Wang, X.; et al. Dietary Pattern and Long-Term Effects of Particulate Matter on Blood Pressure: A Large Cross-Sectional Study in Chinese Adults. Hypertension 2021, 78, 184–194. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Cannon, G.; Moubarac, J.C.; Levy, R.B.; Louzada, M.L.C.; Jaime, P.C. The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018, 21, 5–17. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Cannon, G.; Levy, R.B.; Moubarac, J.C.; Louzada, M.L.; Rauber, F.; Khandpur, N.; Cediel, G.; Neri, D.; Martinez-Steele, E.; et al. Ultra-processed foods: What they are and how to identify them. Public Health Nutr. 2019, 22, 936–941. [Google Scholar] [CrossRef]
- Monteiro, C.A.; Lawrence, M.; Millett, C.; Nestle, M.; Popkin, B.M.; Scrinis, G.; Swinburn, B. The need to reshape global food processing: A call to the United Nations Food Systems Summit. BMJ Glob. Health 2021, 6, e006885. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, C.A.; Moubarac, J.C.; Cannon, G.; Ng, S.W.; Popkin, B. Ultra-processed products are becoming dominant in the global food system. Obes. Rev. 2013, 14 (Suppl. S2), 21–28. [Google Scholar] [CrossRef]
- Hovhannisyan, V.; Devadoss, S. Effects of urbanization on food demand in China. Empirl. Econ. 2020, 58, 699–721. [Google Scholar] [CrossRef]
- Zhai, F.Y.; Du, S.F.; Wang, Z.H.; Zhang, J.G.; Du, W.W.; Popkin, B.M. Dynamics of the Chinese diet and the role of urbanicity, 1991-2011. Obes Rev 2014, 15 (Suppl. S1), 16–26. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, Z.; Du, W.; Huang, F.; Jiang, H.; Bai, J.; Zhang, X.; Zhang, B.; Wang, H. Twenty-Five-Year Trends in Dietary Patterns among Chinese Adults from 1991 to 2015. Nutrients 2021, 13, 1327. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A.; Monsivais, P. Chapter 10-Taste, cost, convenience, and food choices. In Present Knowledge in Nutrition, 11th ed.; Marriott, B.P., Birt, D.F., Stallings, V.A., Yates, A.A., Eds.; Academic Press: Cambridge, MA, USA, 2020; pp. 185–200. [Google Scholar]
- Askari, M.; Heshmati, J.; Shahinfar, H.; Tripathi, N.; Daneshzad, E. Ultra-processed food and the risk of overweight and obesity: A systematic review and meta-analysis of observational studies. Int. J. Obes. 2020, 44, 2080–2091. [Google Scholar] [CrossRef] [PubMed]
- Lane, M.M.; Davis, J.A.; Beattie, S.; Gomez-Donoso, C.; Loughman, A.; O’Neil, A.; Jacka, F.; Berk, M.; Page, R.; Marx, W.; et al. Ultraprocessed food and chronic noncommunicable diseases: A systematic review and meta-analysis of 43 observational studies. Obes. Rev. 2021, 22, e13146. [Google Scholar] [CrossRef]
- Pagliai, G.; Dinu, M.; Madarena, M.P.; Bonaccio, M.; Iacoviello, L.; Sofi, F. Consumption of ultra-processed foods and health status: A systematic review and meta-analysis. Br. J. Nutr. 2021, 125, 308–318. [Google Scholar] [CrossRef]
- Mendonca, R.D.; Lopes, A.C.; Pimenta, A.M.; Gea, A.; Martinez-Gonzalez, M.A.; Bes-Rastrollo, M. Ultra-Processed Food Consumption and the Incidence of Hypertension in a Mediterranean Cohort: The Seguimiento Universidad de Navarra Project. Am. J. Hypertens 2017, 30, 358–366. [Google Scholar] [CrossRef]
- Scaranni, P.; Cardoso, L.O.; Chor, D.; Melo, E.C.P.; Matos, S.M.A.; Giatti, L.; Barreto, S.M.; da Fonseca, M.J.M. Ultra-processed foods, changes in blood pressure and incidence of hypertension: The Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Public Health Nutr. 2021, 24, 3352–3360. [Google Scholar] [CrossRef]
- Rezende-Alves, K.; Hermsdorff, H.H.M.; Miranda, A.; Lopes, A.C.S.; Bressan, J.; Pimenta, A.M. Food processing and risk of hypertension: Cohort of Universities of Minas Gerais, Brazil (CUME Project). Public Health Nutr. 2021, 24, 4071–4079. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Shi, Z. Ultra-Processed Food Consumption Associated with Overweight/Obesity among Chinese Adults-Results from China Health and Nutrition Survey 1997–2011. Nutrients 2021, 13, 2796. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Shi, Z. Association between Ultra-Processed Food Consumption and Diabetes in Chinese Adults-Results from the China Health and Nutrition Survey. Nutrients 2022, 14, 4241. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M.; Du, S.; Zhai, F.; Zhang, B. Cohort Profile: The China Health and Nutrition Survey-monitoring and understanding socio-economic and health change in China, 1989–2011. Int. J. Epidemiol. 2010, 39, 1435–1440. [Google Scholar] [CrossRef]
- Institute for Nutrition and Food Safety of the Chinese Center for Disease Control and Prevention. China Food Composition Table; Peking University Medical Press: Beijing, China, 2002. [Google Scholar]
- Institute for Nutrition and Food Safety of the Chinese Center for Disease Control and Prevention. China Food Composition Table 2004; Peking University Medical Press: Beijing, China, 2005. [Google Scholar]
- Korn, E.L.; Graubard, B.I.; Midthune, D. Time-to-event analysis of longitudinal follow-up of a survey: Choice of the time-scale. Am. J. Epidemiol. 1997, 145, 72–80. [Google Scholar] [CrossRef]
- Juul, F.; Vaidean, G.; Parekh, N. Ultra-processed Foods and Cardiovascular Diseases: Potential Mechanisms of Action. Adv. Nutr. 2021, 12, 1673–1680. [Google Scholar] [CrossRef]
- Simmons, A.L.; Schlezinger, J.J.; Corkey, B.E. What Are We Putting in Our Food That Is Making Us Fat? Food Additives, Contaminants, and Other Putative Contributors to Obesity. Curr. Obes. Rep. 2014, 3, 273–285. [Google Scholar] [CrossRef]
- Fardet, A.; Rock, E.; Bassama, J.; Bohuon, P.; Prabhasankar, P.; Monteiro, C.; Moubarac, J.C.; Achir, N. Current food classifications in epidemiological studies do not enable solid nutritional recommendations for preventing diet-related chronic diseases: The impact of food processing. Adv. Nutr. 2015, 6, 629–638. [Google Scholar] [CrossRef]
- Fardet, A.; Rock, E. Chronic diseases are first associated with the degradation and artificialization of food matrices rather than with food composition: Calorie quality matters more than calorie quantity. Eur. J. Nutr. 2022, 61, 2239–2253. [Google Scholar] [CrossRef]
- Matos, R.A.; Adams, M.; Sabate, J. Review: The Consumption of Ultra-Processed Foods and Non-communicable Diseases in Latin America. Front. Nutr. 2021, 8, 622714. [Google Scholar] [CrossRef]
- Tian, X.; Zhong, L.; von Cramon-Taubadel, S.; Tu, H.; Wang, H. Restaurants in the Neighborhood, Eating Away from Home and BMI in China. PLoS ONE 2016, 11, e0167721. [Google Scholar] [CrossRef] [PubMed]
- Andrade, G.C.; Gombi-Vaca, M.F.; Louzada, M.; Azeredo, C.M.; Levy, R.B. The consumption of ultra-processed foods according to eating out occasions. Public Health Nutr. 2020, 23, 1041–1048. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Diao, Q.; Shao, N.; Liang, Y.; Lin, L.; Lei, Y.; Zheng, L. The Frequency of Unhealthy Food Advertising on Mainland Chinese Television (TV) and Children and Adolescents’ Risk of Exposure to Them. PLoS ONE 2015, 10, e0128746. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Wang, Y.; Wang, H.; Liu, Z.; Yu, X.; Yan, J.; Yu, Y.; Kou, C.; Xu, X.; Lu, J.; et al. Prevalence of mental disorders in China: A cross-sectional epidemiological study. Lancet Psychiatry 2019, 6, 211–224. [Google Scholar] [CrossRef]
- Li, M.; Dibley, M.J.; Sibbritt, D.W.; Yan, H. Dietary habits and overweight/obesity in adolescents in Xi’an City, China. Asia Pac. J. Clin. Nutr. 2010, 19, 76–82. [Google Scholar] [PubMed]
- Gupta, S.; Harper, A.; Ruan, Y.; Barr, R.; Frazier, A.L.; Ferlay, J.; Steliarova-Foucher, E.; Fidler-Benaoudia, M.M. International Trends in the Incidence of Cancer Among Adolescents and Young Adults. J. Natl. Cancer Inst. 2020, 112, 1105–1117. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.X.; Wang, X.L.; Leong, P.M.; Zhang, H.M.; Yang, X.G.; Kong, L.Z.; Zhai, F.Y.; Cheng, Y.Y.; Guo, J.S.; Su, Y.X. New Chinese dietary guidelines: Healthy eating patterns and food-based dietary recommendations. Asia Pac. J. Clin. Nutr. 2018, 27, 908–913. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Li, M.; Shi, Z. Higher egg consumption associated with increased risk of diabetes in Chinese adults-China Health and Nutrition Survey. Br. J. Nutr. 2021, 126, 110–117. [Google Scholar] [CrossRef]
| UPF Intake Level | None | 1–49 | 50–99 | ≥100 | p-Value |
|---|---|---|---|---|---|
| n | 11,010 | 1699 | 1069 | 1276 | |
| Survey year | <0.001 | ||||
| 1997 | 51.8% | 41.1% | 25.4% | 19.4% | |
| 2000 | 16.1% | 11.1% | 10.2% | 7.0% | |
| 2004 | 10.3% | 8.1% | 6.8% | 4.5% | |
| 2006 | 5.0% | 5.5% | 5.1% | 6.0% | |
| 2009 | 7.7% | 9.1% | 12.4% | 14.5% | |
| 2011 | 9.0% | 25.3% | 40.0% | 48.7% | |
| Age (years), mean (SD) | 39.9 (14.4) | 40.8 (14.7) | 40.7 (14.4) | 41.6 (14.3) | <0.001 |
| Sex | <0.001 | ||||
| Men | 46.2% | 44.2% | 49.8% | 60.4% | |
| Women | 53.8% | 55.8% | 50.2% | 39.6% | |
| Income | <0.001 | ||||
| Low | 31.4% | 21.5% | 19.4% | 17.9% | |
| Medium | 34.5% | 32.3% | 33.1% | 29.4% | |
| High | 34.1% | 46.2% | 47.5% | 52.7% | |
| Education | <0.001 | ||||
| Low | 41.1% | 27.3% | 20.8% | 19.8% | |
| Medium | 35.5% | 34.2% | 29.7% | 27.9% | |
| High | 23.4% | 38.5% | 49.5% | 52.2% | |
| Urbanization | <0.001 | ||||
| Low | 36.1% | 19.3% | 15.1% | 12.2% | |
| Medium | 30.7% | 23.8% | 23.2% | 21.9% | |
| High | 33.2% | 56.9% | 61.7% | 65.9% | |
| Energy intake (kcal/d), mean (SD) | 2206.6 (653.5) | 2037.3 (635.2) | 2104.3 (670.7) | 2260.7 (722.8) | <0.001 |
| Fat intake (g/d), mean (SD) | 65.4 (35.9) | 68.7 (34.0) | 75.8 (37.1) | 81.3 (38.7) | <0.001 |
| Protein intake (g/d), mean (SD) | 66.8 (22.7) | 67.3 (22.8) | 71.2 (23.9) | 75.3 (25.6) | <0.001 |
| Carbohydrate intake (g/d), mean (SD) | 337.2 (125.0) | 285.0 (120.8) | 275.5 (117.0) | 277.7 (107.4) | <0.001 |
| Sodium intake (mg/d), mean (SD) | 5465.8 (6880.9) | 5157.6 (4455.0) | 4885.6 (4721.0) | 5450.1 (5236.1) | 0.014 |
| Potassium intake (mg/d), mean (SD) | 1611.6 (895.8) | 1596.7 (664.2) | 1703.7 (757.2) | 1872.7 (1174.8) | <0.001 |
| Vegetable intake (g/day), mean (SD) | 283.7 (173.4) | 262.9 (160.2) | 253.9 (156.9) | 255.3 (158.2) | <0.001 |
| Fruit intake (g/day), mean (SD) | 20.9 (78.0) | 49.7 (103.4) | 64.9 (112.8) | 89.0 (129.2) | <0.001 |
| Tea intake (cup/day) | <0.001 | ||||
| None | 64.4% | 57.1% | 54.4% | 51.3% | |
| <2 | 12.3% | 16.0% | 16.0% | 17.2% | |
| 2–3.9 | 12.0% | 13.0% | 14.6% | 12.1% | |
| 4 | 11.2% | 13.8% | 15.1% | 19.4% | |
| Smoking | <0.001 | ||||
| Non-smoker | 69.8% | 70.7% | 65.0% | 60.1% | |
| Ex-smokers | 1.3% | 1.4% | 3.2% | 3.8% | |
| Current smokers | 29.0% | 27.8% | 31.8% | 36.1% | |
| Alcohol drinking | 31.7% | 35.8% | 44.1% | 51.5% | <0.001 |
| Sleep duration (hours/day) | <0.001 | ||||
| ≤6 | 7.5% | 10.3% | 9.9% | 11.2% | |
| 6–9 | 80.4% | 81.0% | 79.6% | 80.8% | |
| >9 | 12.1% | 8.8% | 10.5% | 8.0% | |
| Physical activity (MET hours/week), mean (SD) | 142.3 (115.2) | 127.3 (106.2) | 127.8 (104.9) | 128.4 (99.7) | <0.001 |
| BMI (kg/m2), mean (SD) | 22.3 (3.1) | 22.7 (3.2) | 22.9 (3.4) | 23.2 (3.4) | <0.001 |
| Diabetes | 5.5% | 7.6% | 4.7% | 8.6% | 0.43 |
| UPF Intake Level | None | 1–49 | 50–99 | ≥100 | p for Trend |
|---|---|---|---|---|---|
| Number of incident cases | 3137 | 459 | 327 | 406 | |
| Rate (per 1000 person years) | 29.5 | 29.5 | 33.4 | 36.3 | |
| Person years | 106,364 | 15,542 | 9777 | 11,186 | |
| Unadjusted model | 1.00 | 0.95 (0.86–1.05) | 1.08 (0.96–1.21) | 1.12 (1.01–1.25) | 0.031 |
| Model 1 | 1.00 | 1.03 (0.93–1.13) | 1.14 (1.02–1.28) | 1.25 (1.13–1.39) | 0.000 |
| Model 2 | 1.00 | 1.00 (0.90–1.12) | 1.17 (1.04–1.33) | 1.20 (1.06–1.35) | 0.001 |
| Model 3 | 1.00 | 1.00 (0.90–1.12) | 1.17 (1.04–1.33) | 1.20 (1.06–1.35) | 0.001 |
| Model 4 | 1.00 | 1.00 (0.90–1.12) | 1.17 (1.03–1.32) | 1.19 (1.06–1.34) | 0.001 |
| Model 5 | 1.00 | 1.00 (0.90–1.12) | 1.17 (1.03–1.33) | 1.19 (1.06–1.35) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, M.; Shi, Z. Ultra-Processed Food Consumption Associated with Incident Hypertension among Chinese Adults—Results from China Health and Nutrition Survey 1997–2015. Nutrients 2022, 14, 4783. https://doi.org/10.3390/nu14224783
Li M, Shi Z. Ultra-Processed Food Consumption Associated with Incident Hypertension among Chinese Adults—Results from China Health and Nutrition Survey 1997–2015. Nutrients. 2022; 14(22):4783. https://doi.org/10.3390/nu14224783
Chicago/Turabian StyleLi, Ming, and Zumin Shi. 2022. "Ultra-Processed Food Consumption Associated with Incident Hypertension among Chinese Adults—Results from China Health and Nutrition Survey 1997–2015" Nutrients 14, no. 22: 4783. https://doi.org/10.3390/nu14224783
APA StyleLi, M., & Shi, Z. (2022). Ultra-Processed Food Consumption Associated with Incident Hypertension among Chinese Adults—Results from China Health and Nutrition Survey 1997–2015. Nutrients, 14(22), 4783. https://doi.org/10.3390/nu14224783








