Prevalence and Sociodemographic Profiles of Grand Multipara in Abu Dhabi, United Arab Emirates
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Outcome Measures
2.3. Definitions
2.4. Data Collection
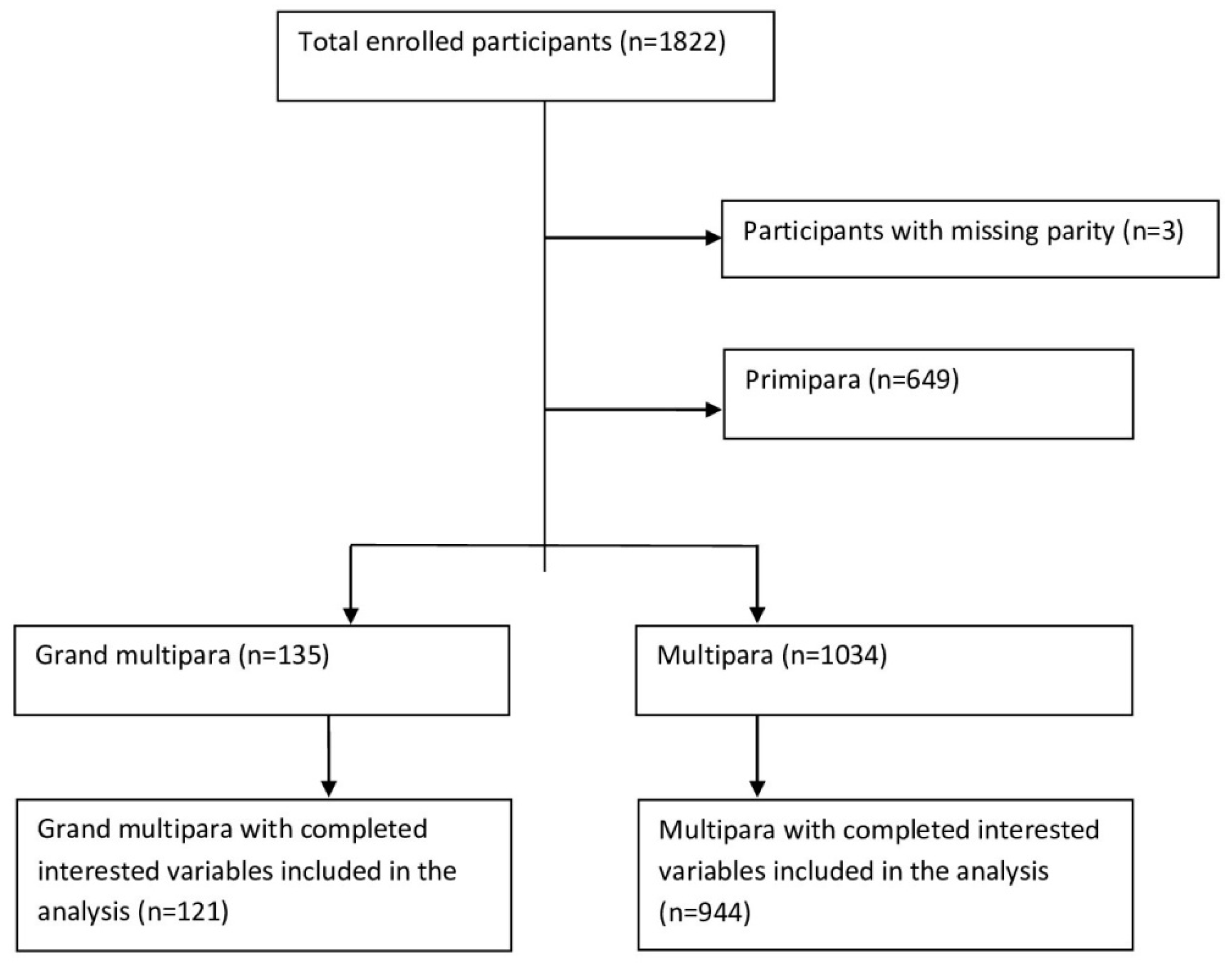
2.5. Study Population
2.6. Study Inclusion and Exclusion Criteria
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Thekrallah, F.; Alnadi, A.; Almajalii, A.; Muhaidat, N.; Badran, E.F. Obstetrics and perinatal outcome of grand multiparity in Jordan: A case-control study. Clin. Exp. Obstet. Gynecol. 2019, 2, 250–257. [Google Scholar] [CrossRef]
- Muniro, Z.; Tarimo, C.S.; Mahande, M.J.; Maro, E.; Mchome, B. Grand multiparity as a predictor of adverse pregnancy outcome among women who delivered at a tertiary hospital in Northern Tanzania. BMC Pregnancy Childbirth 2019, 19, 222. [Google Scholar] [CrossRef]
- Abdelmageed, E.; Bahaeldin, H.; Nadiah, A. Maternal and neonatal outcomes of grand multiparity in Khartoum, Sudan. Afr. Health Sci. 2022, 22, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Rizk, D.; Khalfan, M.; Ezimokhai, M. Obstetric outcome in grand multipara in the United Arab Emirates a case control study. Arch. Gynecol. Obstet. 2001, 264, 194–198. [Google Scholar] [CrossRef]
- Njoku, C.O.; Abeshi, S.E.; Emechebe, C.I. Grand Multiparity: Obstetric Outcome in Comparison with Multiparous Women in a Developing Country. Open J. Obstet. Gynecol. 2017, 7, 707–718. [Google Scholar] [CrossRef]
- Dasa, T.T. Effect of grand multiparity on the adverse birth outcome: A hospital-based prospective cohort study in Sidama Region, Ethiopia. Int. J. Women’s Health 2022, 14, 363–372. [Google Scholar] [CrossRef]
- Elhassan, E.M.; Hassan, A.A.; Mirghani, O.A.; Adam, I. Morbidity and mortality pattern of neonates admitted into nursery unit in Wad Medani Hospital, Sudan. Sudan J. Med. Sci. 2010, 5, 13–16. [Google Scholar] [CrossRef]
- Gardner, H.; Green, K.; Gardner, A.S.; Geddes, D. Observations on the health of infants at a time of rapid societal change: A longitudinal study from birth to fifteen months in Abu Dhabi. BMC Pediatr. 2018, 18, 32. [Google Scholar] [CrossRef]
- Al-shaikh, G.K.; Ibrahim, G.H.; Fayed, A.A.; Al-mandeel, H. Grand multiparity and the possible risk of adverse maternal and neonatal outcomes: A dilemma to be deciphered. BMC Pregnancy Childbirth 2017, 17, 310. [Google Scholar] [CrossRef]
- Paul, L.; Jennifer, L.; Jay, D. Generational and cultural changes in family life in the United Arab Emirates: A comparison of mothers and daughters. J. Comp. Fam. Stud. 2005, 36, 77–91. [Google Scholar]
- Nargund, G. Declining birth rate in Developed Countries: A radical policy re-think is required. Facts Views Vis. ObGyn. 2009, 1, 191–193. [Google Scholar] [PubMed]
- Mgaya, A.H.; Kidanto, H.L.; Mgaya, H.N. The association between child loss, children’s paternity and high parity in Dar Es Salaam, Tanzania: A cross sectional Survey at the National Referral Hospital. Obstet. Gynaecol. Cases-Rev. 2016, 3, 75. [Google Scholar] [CrossRef]
- Dasa, T.T.; Okunlola, M.A.; Dessie, Y. Multilevel analysis of grand multiparity: Trend and its determinants in the Sidama National Regional State sectional study of Ethiopia: A cross-sectional study design from demographic and health survey 2000–2016. BMJ Open 2022, 12, e061697. [Google Scholar] [CrossRef] [PubMed]
- Götmark, F. Human fertility in relation to education, economy, religion, contraception, and family planning programs. BMC Public Health 2020, 20, 265. [Google Scholar] [CrossRef] [PubMed]
- Samier, E. Emirati women’s higher educational leadership formation under globalisation: Culture, religion, politics, and the dialectics of modernisation. Gend. Educ. 2015, 27, 239–254. [Google Scholar] [CrossRef]
- World Bank. Population, Total—United Arab Emirates. 2021. Available online: https://data.worldbank.org/indicator/SP.POP.TOTL?locations=AE (accessed on 12 March 2021).
- World Health Organization. WHO: Global Database on Body Mass Index; World Health Organization: Geneva, Switzerland, 2018; Available online: http://apps.who.int/bmi/index.jsp (accessed on 11 August 2018).
- Taha, Z.; Garemo, M.; Nanda, J. Patterns of breastfeeding and complementary feeding practices among infants and young children in Abu Dhabi, United Arab Emirates. Int. Breastfeed. J. 2018, 13, 48. [Google Scholar] [CrossRef]
- Lo, S.K.; Li, I.T.; Tsou, T.S.; See, L. Non-significant in univariate but significant in multivariate analysis: A discussion with examples. Search Life-Sci. Lit. 1995, 18, 95–101. Available online: http://www.ncbi.nlm.nih.gov/pubmed/7641117 (accessed on 13 March 2022).
- Li, W.; Wang, Y.; Shen, L.; Song, L.; Li, H.; Liu, B.; Yuan, J.; Wang, Y. Association between parity and obesity patterns in a middle-aged and older Chinese population: A cross-sectional analysis in the Tongji-Dongfeng cohort study. Nutr. Metab. 2016, 13, 72. [Google Scholar] [CrossRef]
- Iversen, D.S. Associations between parity and maternal BMI in a population-based cohort study. Acta Obstet. Gynecol. Scand. 2018, 62, 694–700. [Google Scholar] [CrossRef]
- Taha, Z.; Hassan, A.A.; Papandreou, D. Epidemiology of pre-pregnancy body mass index (BMI) among mothers in Abu Dhabi, the United Arab Emirates. Front. Glob. Women’s Health 2022, 3, 893808. [Google Scholar] [CrossRef]
- Relph, S.; Patel, T.; Delaney, L.; Sobhy, S.; Thangaratinam, S. Adverse pregnancy outcomes in women with diabetes-related microvascular disease and risks of disease progression in pregnancy: A systematic review and meta-analysis. PLoS Med. 2021, 18, e1003856. [Google Scholar] [CrossRef] [PubMed]
- Saquib, S.; Tambawala, Z.Y.; Waheed, S.; Hubaishi, N.M. Pregnancy outcome in women with type 1 and type 2 diabetes mellitus in Dubai Hospital: A retrospective observational study. Endocr. J. 2022, 12, 86–91. [Google Scholar]
- Elmugabil, A.; Rayis, D.A.; Hassan, A.A.; Ali, A.A.; Adam, I. Epidemiology of cesarean delivery in Kassala, eastern Sudan: A community-based study 2014–2015. Sudan J. Med. Sci. 2016, 11, 49–54. [Google Scholar]
- Mombo-Ngoma, G.; Mackanga, J.R.; Gonzalez, R.; Ouedraogo, S.; Kakolwa, M.A.; Manego, R.Z.; Basra, A.; Rupérez, M.; Cot, M.; Kabanywany, A.M.; et al. Young adolescent girls are at high risk for adverse pregnancy outcomes in sub-Saharan Africa: An observational multicountry study. BMJ Open 2016, 6, e011783. [Google Scholar] [CrossRef] [PubMed]
- Mekonnen, T.; Dune, T.; Perz, J. Maternal health service utilisation of adolescent women in sub-Saharan Africa: A systematic scoping review. BMC Pregnancy Childbirth 2019, 19, 366. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.A.A.; Mohammed, A.A.; Sulaiman, M.A. Education, poor antenatal care coverage and teenage pregnancy at Kassala Hospital, Eastern Sudan. J. Public Health Epidemiol. 2011, 3, 642–644. [Google Scholar]
- Mohr, R.; Austin, S.F.; Austin, S.F.; Sharma, B.B. The influence of educational attainment on teenage pregnancy in Low-Income Countries: A systematic literature review. J. Soc. Work. Glob. Community 2019, 4, 19–31. [Google Scholar] [CrossRef]
- Hackman, N.M.; Schaefer, E.W.; Beiler, J.S.; Rose, C.M.; Paul, I.M. Breastfeeding Outcome Comparison by Parity. Breastfeed Med. 2015, 10, 156–162. [Google Scholar] [CrossRef]
- Kieffer, E.; Novotny, R.; Welch, K.; Mor, J.; Thele, M. Health practitioners should consider parity when counseling mothers on decisions about infant feeding methods. J. Am. Diet. Assoc. 1997, 97, 1313–1316. [Google Scholar] [CrossRef]
- Abu Dhabi Government. Abu Dhabi Emirate: Facts and Figures. 2018. Available online: https://www.abudhabi.ae/portal/public/en/abu_dhabi_emirate/facts_figure_background?_adf.ctrl-state=ki3p4o0qf_4&_afrLoop=18541566215609417#! (accessed on 20 April 2019).
- Lahti, M.; Eriksson, J.G.; Heinonen, K.; Kajantie, E.; Lahti, J.; Wahlbeck, K.; Tuovinen, S.; Pesonen, An.; Mikkonen, M.; Osmond, C.; et al. Maternal grand multiparity and the risk of severe mental disorders in adult offspring. PLoS ONE 2014, 9, e114679. [Google Scholar] [CrossRef]
| Variable | Total (N = 1065) | Parity | |||
|---|---|---|---|---|---|
| Grand Multipara (n = 121) | Multipara (n = 944) | p-Value | |||
| Median (interquartile range) of | |||||
| Maternal age, years | 31 (28–35) | 37 (34–38) | 30 (27–34) | <0.001 | |
| Pre-pregnancy BMI | 23.8 (21.8–26.3) | 26.1 (23.2–28.4) | 23.5 (21.7–25.9) | <0.001 | |
| N (%) | N (%) | N (%) | p-value | ||
| Maternal education | ≥Secondary level | 1017 (95.5) | 113 (93.4) | 904 (95.8) | 0.236 |
| <Secondary level | 48 (4.5) | 8 (6.6) | 40 (4.2) | ||
| Paternal education | ≥Secondary level | 1060 (99.5) | 121 (100) | 939 (99.5) | 0.923 |
| <Secondary level | 5 (0.5) | 0 (0.0) | 5 (0.5) | ||
| Nationality | Arab | 737 (69.2) | 111 (91.7) | 626 (66.3) | <0.001 |
| Non-Arab | 328 (30.8) | 10 (8.3) | 318 (33.7) | ||
| Pre-pregnancy BMI | Normal BMI | 641 (60.2) | 43 (35.5) | 598 (63.3) | <0.001 |
| Underweight | 22 (2.1) | 2 (1.7) | 20 (2.1) | ||
| Overweight | 324 (30.4) | 60 (49.6) | 264 (28.0) | ||
| Obese | 78 (7.3) | 16 (13.2) | 62 (26.6) | ||
| Income rating | ≥Good | 993 (93.2) | 109 (90.9) | 884 (93.6) | 0.142 |
| <Good | 72 (6.8) | 12 (9.1) | 60 (6.4) | ||
| Received breastfeeding support during pregnancy | Yes | 945 (88.7) | 90 (74.4) | 855 (90.6) | <0.001 |
| No | 120 (11.3) | 31 (35.6) | 89 (9.4) | ||
| Mode of delivery | Vaginal delivery | 749 (70.3) | 90 (74.4) | 659 (69.8) | 0.582 |
| Planned cesarean delivery | 247 (23.2) | 24 (19.8) | 223 (23.6) | ||
| Emergency cesarean delivery | 69 (6.5) | 7 (5.8) | 62 (6.6) | ||
| Child gender | Male | 505 (47.4) | 62 (51.2) | 443 (46.9) | 0.699 |
| Female | 560 (52.6) | 59 (48.8) | 501 (53.1) | ||
| Gestational age at delivery | Term (≥37 weeks) | 989 (92.9) | 110 (90.9) | 879 (93.1) | 0.375 |
| Preterm (<37 weeks) | 76 (7.1) | 11 (9.1) | 65 (6.9) | ||
| Child birth weight at delivery | ≥2500 g | 981 (92.1) | 112 (92.6) | 869 (92.1) | 0.846 |
| Low birth weight (<2500 g) | 84 (7.9) | 9 (7.4) | 75 (7.9) | ||
| Macrosomia (≥4000 g) | Yes | 44 (4.1) | 5 (4.1) | 39 (4.1) | 1.000 |
| No | 1021 (95.9) | 116 (95.9) | 905 (95.9) | ||
| Variables | Odd Ratio 95% Confidence Interval (CI) | p-Value | Adjusted Odd Ratio 95% CI | p-Value | |
|---|---|---|---|---|---|
| Maternal age, years | 1.29 (1.22, 1.35) | <0.001 | 1.28 (1.21, 1.34) | <0.001 | |
| Maternal education | ≥Secondary level | 0.63 (0.29, 1.37) | 0.240 | 0.48 (0.17, 1.40) | 0.180 |
| <Secondary level (reference) | |||||
| Nationality | Arab | 5.64 (2.91, 10.92 | <0.001 | 5.66 (2.81, 11.40) | <0.001 |
| Non-Arab reference | |||||
| Pre-pregnancy BMI | Normal BMI (reference) | ||||
| Underweight | 1.39 (0.32, 6.15) | 0.664 | 0.89 (0.16, 5.12) | 0.898 | |
| Overweight | 3.16 (2.08, 4.80) | <0.001 | 2.01 (1.26, 3.21) | 0.004 | |
| Obese | 3.59 (1.91, 6.74) | <0.001 | 1.61 (0.78, 3.35) | 0.201 | |
| Income rating | ≥Good | 0.62 (0.32, 1.18) | 0.145 | 0.52 (0.24, 1.12) | 0.095 |
| <Good (reference) | |||||
| Received support during pregnancy | No | 3.31 (2.08, 5.26) | <0.001 | 2.05 (1.21, 3.50) | 0.008 |
| Yes (reference) | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taha, Z.; El Ktaibi, F.; Al Dhaheri, A.I.; Papandreou, D.; Ali Hassan, A. Prevalence and Sociodemographic Profiles of Grand Multipara in Abu Dhabi, United Arab Emirates. Nutrients 2022, 14, 4686. https://doi.org/10.3390/nu14214686
Taha Z, El Ktaibi F, Al Dhaheri AI, Papandreou D, Ali Hassan A. Prevalence and Sociodemographic Profiles of Grand Multipara in Abu Dhabi, United Arab Emirates. Nutrients. 2022; 14(21):4686. https://doi.org/10.3390/nu14214686
Chicago/Turabian StyleTaha, Zainab, Farid El Ktaibi, Aysha Ibrahim Al Dhaheri, Dimitrios Papandreou, and Ahmed Ali Hassan. 2022. "Prevalence and Sociodemographic Profiles of Grand Multipara in Abu Dhabi, United Arab Emirates" Nutrients 14, no. 21: 4686. https://doi.org/10.3390/nu14214686
APA StyleTaha, Z., El Ktaibi, F., Al Dhaheri, A. I., Papandreou, D., & Ali Hassan, A. (2022). Prevalence and Sociodemographic Profiles of Grand Multipara in Abu Dhabi, United Arab Emirates. Nutrients, 14(21), 4686. https://doi.org/10.3390/nu14214686







