Ameliorative Effects of Daphnopsis costaricensis Extract against Oxazolone-Induced Atopic Dermatitis-like Lesions in BALB/c Mice
Abstract
1. Introduction
2. Materials and Methods
2.1. Plant Material
2.2. General Experimental Procedures
2.3. Extraction and Isolation
2.4. Animals
2.5. Oxazolone-Induced Atopic Dermatitis BALB/c Mice
2.6. Histological Examination
2.7. Cell Culture
2.8. Measurement of IL-4 mRNA Expression
2.9. Measurement of β-Hexosaminidase Release
2.10. Statistical Analysis
3. Results
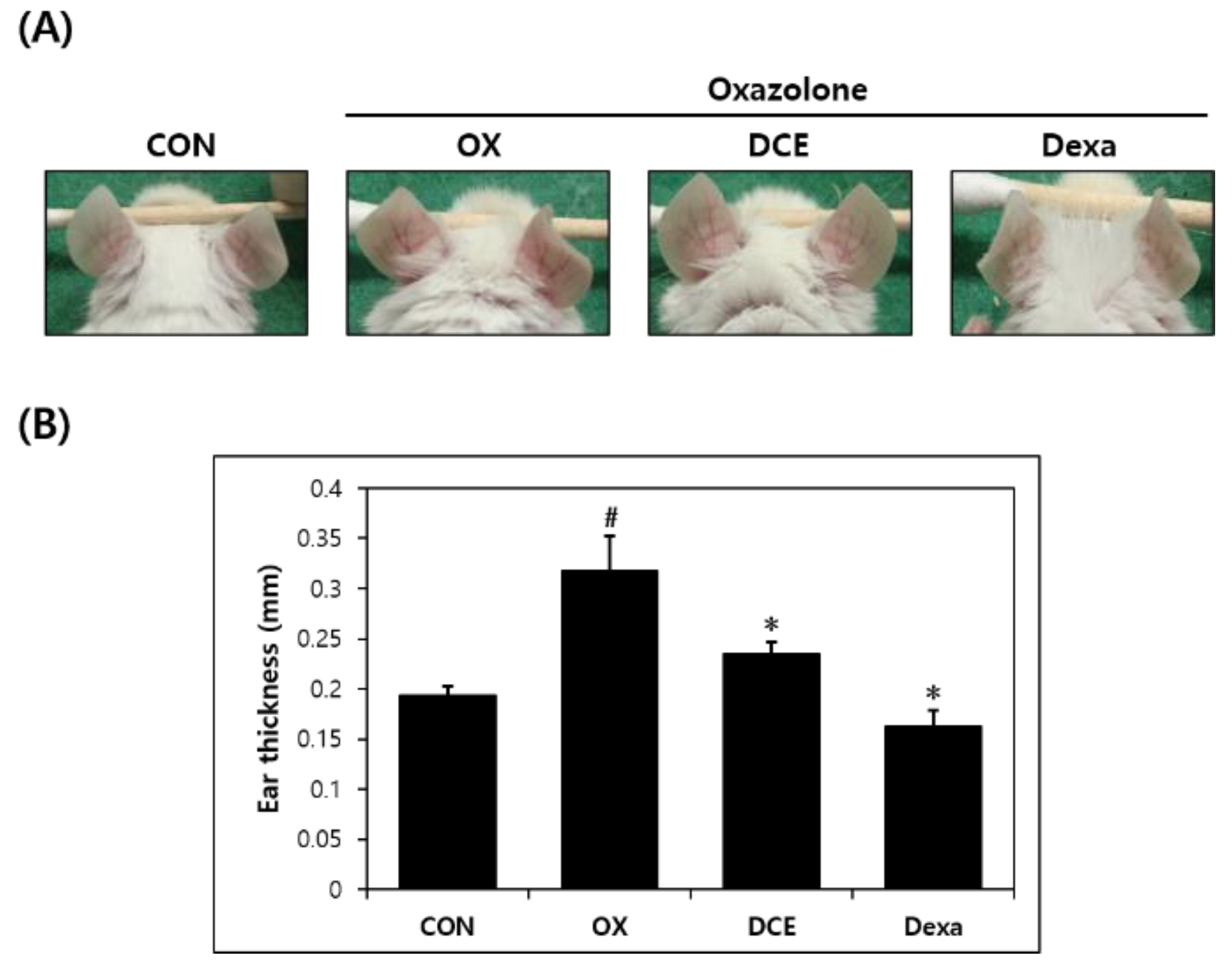
3.1. Effects of D. costaricensis EtOH Extract (DCE) on Oxazolone-Induced AD-Like Lesions
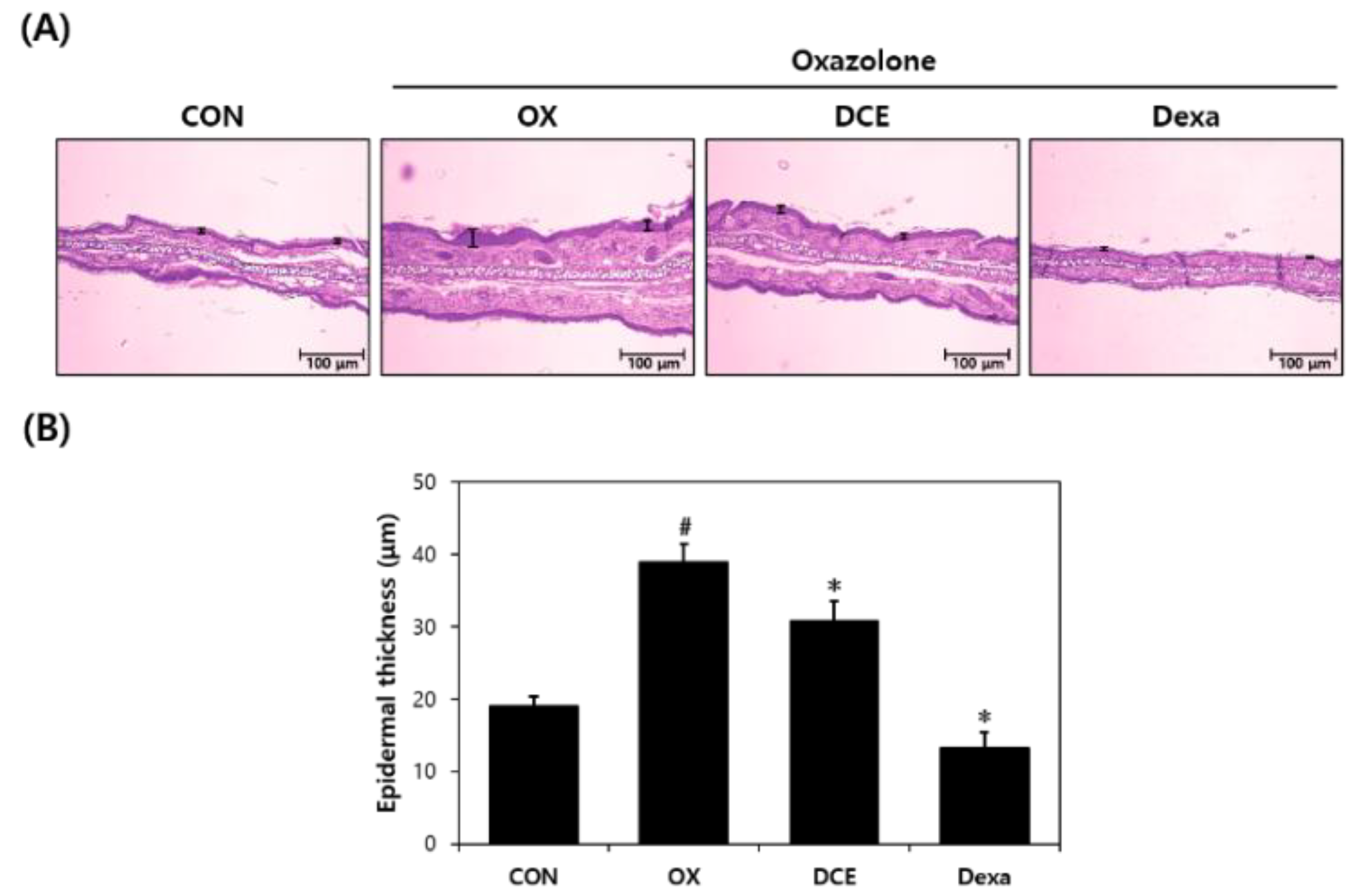
3.2. Histopathologic Effects of DCE on Oxazolone-Induced AD-Like Lesions
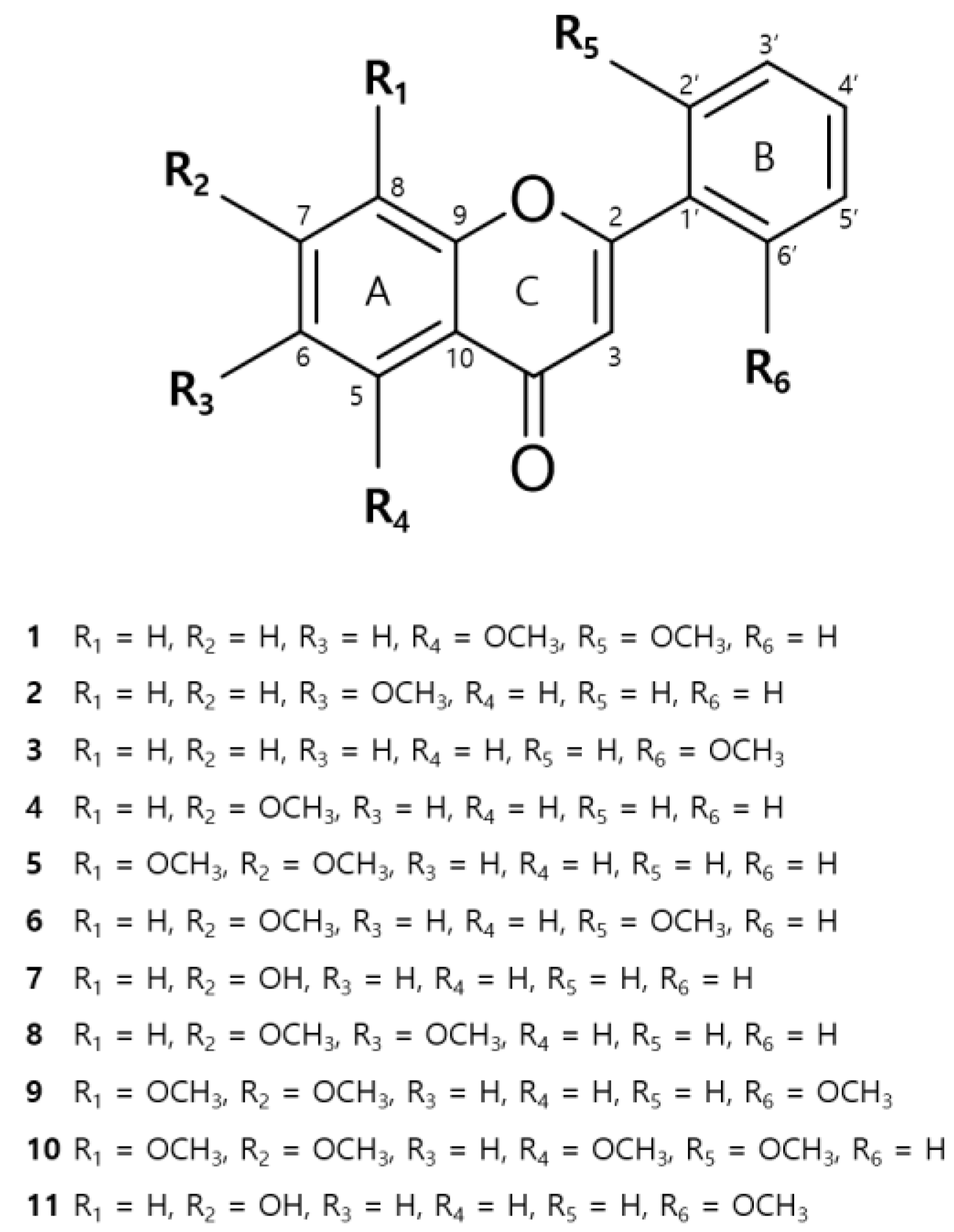
3.3. Isolation of Compounds from DCE
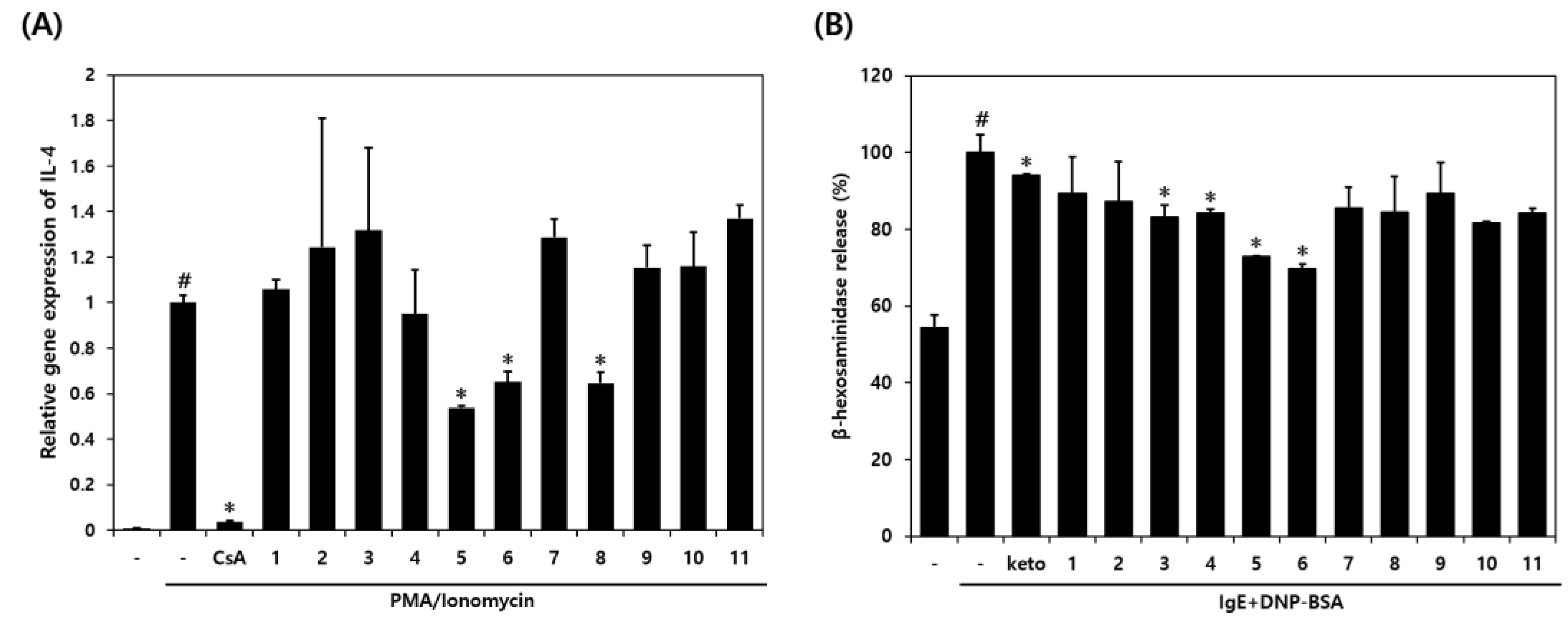
3.4. Compounds Isolated from DCE and Their Effects on RBL-2H3 Cells
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Leung, D.Y.M. Pathogenesis of atopic dermatitis. J. Allergy Clin. Immunol. 1999, 104, 99–108. [Google Scholar] [CrossRef]
- Koblenzer, C. Itching and the atopic skin. J. Allergy Clin. Immunol. 1999, 104, 109–113. [Google Scholar] [CrossRef]
- Deo, S.S.; Mistry, K.J.; Kakade, A.M.; Niphadkar, P.V. Role played by Th2 type cytokines in IgE mediated allergy and asthma. Lung India 2010, 27, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Leung, D.Y.M. Immunopathology of atopic dermatitis. Springer Semin. Immunopathol. 1992, 13, 427–440. [Google Scholar] [CrossRef] [PubMed]
- Branco, A.C.C.C.; Yoshikawa, F.S.Y.; Pietrobon, A.J.; Sato, M.N. Role of Histamine in Modulating the Immune Response and Inflammation. Mediat. Inflamm. 2018, 2018, 952407. [Google Scholar] [CrossRef] [PubMed]
- Furue, M. Regulation of Skin Barrier Function via Competition between AHR Axis versus IL-13/IL-4-JAK-STAT6/STAT3 Axis: Pathogenic and Therapeutic Implications in Atopic Dermatitis. J. Clin. Med. 2020, 9, 3741. [Google Scholar] [CrossRef]
- Giam, Y.C.; Hebert, A.A.; Dizon, M.V.; Van Bever, H.; Tiongco-Recto, M.; Kim, K.-H.; Soebono, H.; Munasir, Z.; Diana, I.A.; Luk, D.C.K. A review on the role of moisturizers for atopic dermatitis. Asia Pac. Allergy 2016, 6, 120–128. [Google Scholar] [CrossRef]
- Simpson, E.L. Atopic dermatitis: A review of topical treatment options. Curr. Med. Res. Opin. 2010, 26, 633–640. [Google Scholar] [CrossRef]
- Albader, S.S.; Alharbi, A.A.; Alenezi, R.F.; Alsaif, F.M. Dupilumab side effect in a patient with atopic dermatitis: A case report study. Biologics 2019, 13, 79–82. [Google Scholar] [CrossRef]
- Kim, H.S.; Cho, S.H. Treatment for atopic dermatitis. J. Korean Med. Assoc. 2014, 57, 226–233. [Google Scholar] [CrossRef]
- Berger, T.G.; Duvic, M.; Van Voorhees, A.S.; Frieden, I.J. The use of topical calcineurin inhibitors in dermatology: Safety concerns. Report of the American Academy of Dermatology Association Task Force. J. Am. Acad. Dermatol. 2006, 54, 818–823. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Pang, Y.; He, Y.; Zhang, X.; Peng, L.; Guo, J.; Zeng, J. A comprehensive review of natural products against atopic dermatitis: Flavonoids, alkaloids, terpenes, glycosides and other compounds. Biomed. Pharmacother. 2021, 140, 111741. [Google Scholar] [CrossRef] [PubMed]
- Dohil, M.A. Natural ingredients in atopic dermatitis and other inflammatory skin disease. J. Drugs Dermatol. 2013, 12, 128–132. [Google Scholar]
- Dawid-Pać, R. Medicinal plants used in treatment of inflammatory skin diseases. Postep. Dermatol. Alergol. 2013, 30, 170–177. [Google Scholar] [CrossRef]
- Ambriz-Pérez, D.L.; Leyva-López, N.; Gutierrez-Grijalva, E.P.; Heredia, J.B. Phenolic compounds: Natural alternative in inflammation treatment. A Review. Cogent Food Agric. 2016, 2, 1131412. [Google Scholar] [CrossRef]
- Shi, X.; Niu, L.; Zhao, L.; Wang, B.; Jin, Y.; Li, X. The anti-allergic activity of flavonoids extracted from Citri Reticulatae Pericarpium. J. Food Process. Preserv. 2018, 42, 13588. [Google Scholar] [CrossRef]
- Li, Y.-J.; Guo, Y.; Yang, Q.; Weng, X.-G.; Yang, L.; Wang, Y.-J.; Chen, Y.; Zhang, D.; Li, Q.; Liu, X.-C.; et al. Flavonoids casticin and chrysosplenol D from Artemisia annua L. inhibit inflammation in vitro and in vivo. Toxicol. Appl. Pharmacol. 2015, 286, 151–158. [Google Scholar] [CrossRef]
- Ullah, A.; Munir, S.; Badshah, S.L.; Khan, N.; Ghani, L.; Poulson, B.G.; Emwas, A.-H.; Jaremko, M. Important Flavonoids and Their Role as a Therapeutic Agent. Molecules 2020, 25, 5243. [Google Scholar] [CrossRef]
- Daphnopsis Cotaricensis Barringer & Grayum|International Plant Names Index. Available online: https://www.ipni.org/n/275663-2 (accessed on 8 October 1984).
- Blaskó, G.; Xun, L.; Cordell, G.A. Studies in the Thymelaeaceae, V. 2′-Hydroxyflavone from Daphnopsis Sellowiana: Isolation and Synthesis. J. Nat. Prod. 1988, 51, 60–65. [Google Scholar] [CrossRef]
- Borris, R.P.; Blaskó, G.; Cordell, G.A. Ethnopharmacologic and Phytochemical Studies of the Thymelaeaceae. J. Ethnopharmacol. 1988, 24, 41–91. [Google Scholar] [CrossRef]
- Jin, M.; Yoon, S.J.; Pyo, M.Y. Down-regulation of T helper 2-associated cytokine expression and selective transcription factors by fisetin. J. Appl. Biol. Chem. 2011, 54, 949–958. [Google Scholar] [CrossRef]
- Lee, E.-J.; Yu, M.-H.; Garcia, C.V.; Jhee, K.-H.; Yang, S.-A. Inhibitory effect of Zizania latifolia chloroform fraction on allergy-related mediator production in RBL-2H3 cells. Food Sci. Biotechnol. 2017, 26, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Moon, B.H.; Park, Y.H.; Lee, E.J.; Hong, S.W.; Lim, Y.H. Methyl Substitution Effects on 1H and 13C NMR Data of Methoxyflavones. Bull. Korean Chem. Soc. 2008, 29, 1793–1796. [Google Scholar] [CrossRef]
- McKendall, M.; Smith, T.; Anh, K.; Ellis, J.; McGee, T.; Foroozesh, M.; Zhu, N.; Stevens, C.L.K. Methoxyflavone Inhibitors of Cytochrome P450. J. Chem. Crystallogr. 2008, 38, 231–237. [Google Scholar] [CrossRef]
- Herath, W.; Mikell, J.R.; Khan, I.A. Microbial metabolism. Part 10: Metabolites of 7,8-dimethoxyflavone and 5-methoxyflavone. Nat. Prod. Res. 2009, 23, 1231–1239. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-I.; Son, H.-S.; Park, H. An efficient synthesis of flavones from 2-hydroxybenzoic acids. Bull. Korean Chem. Soc. 2004, 25, 1945–1947. [Google Scholar] [CrossRef]
- Aksnes, D.W.; Standnes, A.; Andersen, Ø.M. Complete Assignment of the 1H and 13C NMR Spectra of Flavone and Its A-Ring Hydroxyl Derivatives. Magn. Reson. Chem. 1996, 34, 820–823. [Google Scholar] [CrossRef]
- Yoon, H.; Eom, S.L.; Hyun, J.Y.; Jo, G.H.; Hwang, D.S.; Lee, S.H.; Yong, Y.J.; Park, J.C.; L:ee, Y.H.; Lim, Y.H. 1H and 13C NMR Data on Hydroxy/Methoxy Flavonoids and the Effects of Substituents on Chemical Shifts. Bull. Korean Chem. Soc. 2011, 32, 2101–2104. [Google Scholar] [CrossRef][Green Version]
- Kim, Y.S.; Keyser, S.G.L.; Schneekloth, J.S. Synthesis of 2′,3′,4′-trihydroxyflavone (2-D08), an inhibitor of protein sumoylation. Bioorg. Med. Chem. Lett. 2014, 24, 1094–1097. [Google Scholar] [CrossRef]
- Bhardwaj, D.K.; Gupta, A.K.; Chand, R.; Jain, K. Syntheses of Andrographis paniculata flavones. Curr. Sci. 1981, 50, 750–753. [Google Scholar]
- Laget, M.; De Méo, M.; Wallet, J.C.; Gaydou, E.M.; Guiraud, H.; Duménil, G. Antimutagenic Activities of 24 Synthetic Flavones with the Salmonella Microsomal Assay. Arch. Pharm. Res. 1995, 18, 415–422. [Google Scholar] [CrossRef]
- Panche, A.N.; Diwan, A.D.; Chandra, S.R. Flavonoids: An overview. J. Nutr. Sci. 2016, 5, 47. [Google Scholar] [CrossRef] [PubMed]
- Karak, P. Biological activities of flavonoids: An overview. Int. J. Pharm. Sci. Res. 2019, 10, 1567–1574. [Google Scholar]
- Singh, M.; Kaur, M.; Silakari, O. Flavones: An important scaffold for medicinal chemistry. Eur. J. Med. Chem. 2014, 84, 206–239. [Google Scholar] [CrossRef]
- Lee, D.; Park, J.; Choi, J.; Jang, H.; Seol, J. Anti-inflammatory effects of natural flavonoid diosmetin in IL-4 and LPS-induced macrophage activation and atopic dermatitis model. Int. Immunopharmacol. 2020, 89, 107046. [Google Scholar] [CrossRef]
- Maleki, S.J.; Crespo, J.F.; Cabanillas, B. Anti-inflammatory effects of flavonoids. Food Chem. 2019, 299, 125124. [Google Scholar] [CrossRef] [PubMed]
- Gębka, N.; Adamczyk, J.; Gębka-Kępińska, B.; Mizgała-Izworska, E. The role of flavonoids in prevention and treatment of selected skin diseases. J. Pre Clin. Clin. Res. 2022, 16, 99–107. [Google Scholar] [CrossRef]
- Moshiashvili, G.; Tabatadze, N.; Mshvildadze, V. The genus Daphne: A review of its traditional uses, phytochemistry and pharmacology. Fitoterapia 2020, 143, 104540. [Google Scholar] [CrossRef]
- Yeşilada, E.; Taninaka, H.; Takaishi, Y.; Honda, G.; Sezik, E.; Momota, H.; Ohmoto, Y.; Taki, T. In vitro inhibitory effects of ssp. on inflammatory cytokines and activity-guided isolation of active constituents. Cytokine 2001, 13, 359–364. [Google Scholar] [CrossRef]
- Jegal, J.; Park, N.-J.; Kim, T.-Y.; Choi, S.; Lee, S.W.; Hang, J.; Kim, S.-N.; Yang, M.H. Effect of Topically Applied Wikstroemia Dolichantha Diels on the Development of Atopic Dermatitis-Like Skin Symptoms in Mice. Nutrients 2019, 11, 914. [Google Scholar] [CrossRef]
- Guttman-Yassky, E.; Nograles, K.E.; Krueger, J.G. Contrasting pathogenesis of atopic dermatitis and psoriasis—Part I: Clinical and pathologic concepts. J. Allergy Clin. Immunol. 2011, 127, 1110–1118. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.-W.; Kim, M.-R.; Lee, E.-Y.; Kim, J.H.; Kim, Y.-S.; Jeon, S.G.; Yang, J.-M.; Lee, B.-J.; Pyun, B.-Y.; Gho, Y.S.; et al. Extracellular vesicles derived from Staphylococcus aureus induce atopic dermatitis-like skin inflammation. Allergy 2011, 66, 351–359. [Google Scholar] [CrossRef] [PubMed]
- Jin, H.; He, R.; Oyoshi, M.; Geha, R.S. Animal models of atopic dermatitis. J. Investig. Dermatol. 2009, 129, 31–40. [Google Scholar] [CrossRef]
- Fujii, M. Current Understanding of Pathophysiological Mechanisms of Atopic Dermatitis: Interactions among Skin Barrier Dysfunction, Immune Abnormalities and Pruritus. Biol. Pharm. Bull. 2020, 43, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Takahashi, R. Flavonoids and asthma. Nutrients 2013, 5, 2128–2143. [Google Scholar] [CrossRef]
- Kinet, J.-P.; Blank, U.; Brini, A.; Jouvin, M.-H.; Küster, H.; Mejan, O.; Ra, C. The high-affinity receptor for immunoglobulin E: A target for therapy of allergic diseases. Int. Arch. Allergy Appl. Imm. 1991, 94, 51–55. [Google Scholar] [CrossRef]
- Oliver, J.M.; Seagrave, J.; Stump, R.F.; Pfeiffer, J.R.; Deanin, G.G. Signal transduction and cellular response in RBL-2H3 mast cells. Chem. Immunol. Allergy 1988, 42, 185–245. [Google Scholar]
- Wang, X.; Cao, Y.; Chen, S.; Lin, J.; Bian, J.; Huang, D. Anti-inflammation Activity of Flavones and Their Structure–Activity Relationship. J. Agric. Food Chem. 2021, 69, 7285–7302. [Google Scholar] [CrossRef]
- Matsuda, H.; Morikawa, T.; Ando, S.; Toguchida, I.; Yosikawa, M. Structural requirements of flavonoids for nitric oxide production inhibitory activity and mechanism of action. Bioorg. Med. Chem. 2003, 11, 1995–2000. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bae, Y.; Kim, T.; Park, N.; Choi, S.; Yi, D.; Soto, S.; Zamora, N.; Kim, S.; Yang, M. Ameliorative Effects of Daphnopsis costaricensis Extract against Oxazolone-Induced Atopic Dermatitis-like Lesions in BALB/c Mice. Nutrients 2022, 14, 4521. https://doi.org/10.3390/nu14214521
Bae Y, Kim T, Park N, Choi S, Yi D, Soto S, Zamora N, Kim S, Yang M. Ameliorative Effects of Daphnopsis costaricensis Extract against Oxazolone-Induced Atopic Dermatitis-like Lesions in BALB/c Mice. Nutrients. 2022; 14(21):4521. https://doi.org/10.3390/nu14214521
Chicago/Turabian StyleBae, Yunji, Taeyoung Kim, Nojune Park, Sangho Choi, Dongkeun Yi, Silvia Soto, Nelson Zamora, Sunam Kim, and Minhye Yang. 2022. "Ameliorative Effects of Daphnopsis costaricensis Extract against Oxazolone-Induced Atopic Dermatitis-like Lesions in BALB/c Mice" Nutrients 14, no. 21: 4521. https://doi.org/10.3390/nu14214521
APA StyleBae, Y., Kim, T., Park, N., Choi, S., Yi, D., Soto, S., Zamora, N., Kim, S., & Yang, M. (2022). Ameliorative Effects of Daphnopsis costaricensis Extract against Oxazolone-Induced Atopic Dermatitis-like Lesions in BALB/c Mice. Nutrients, 14(21), 4521. https://doi.org/10.3390/nu14214521




