Relationship between Mental Health and Emotional Eating during the COVID-19 Pandemic: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
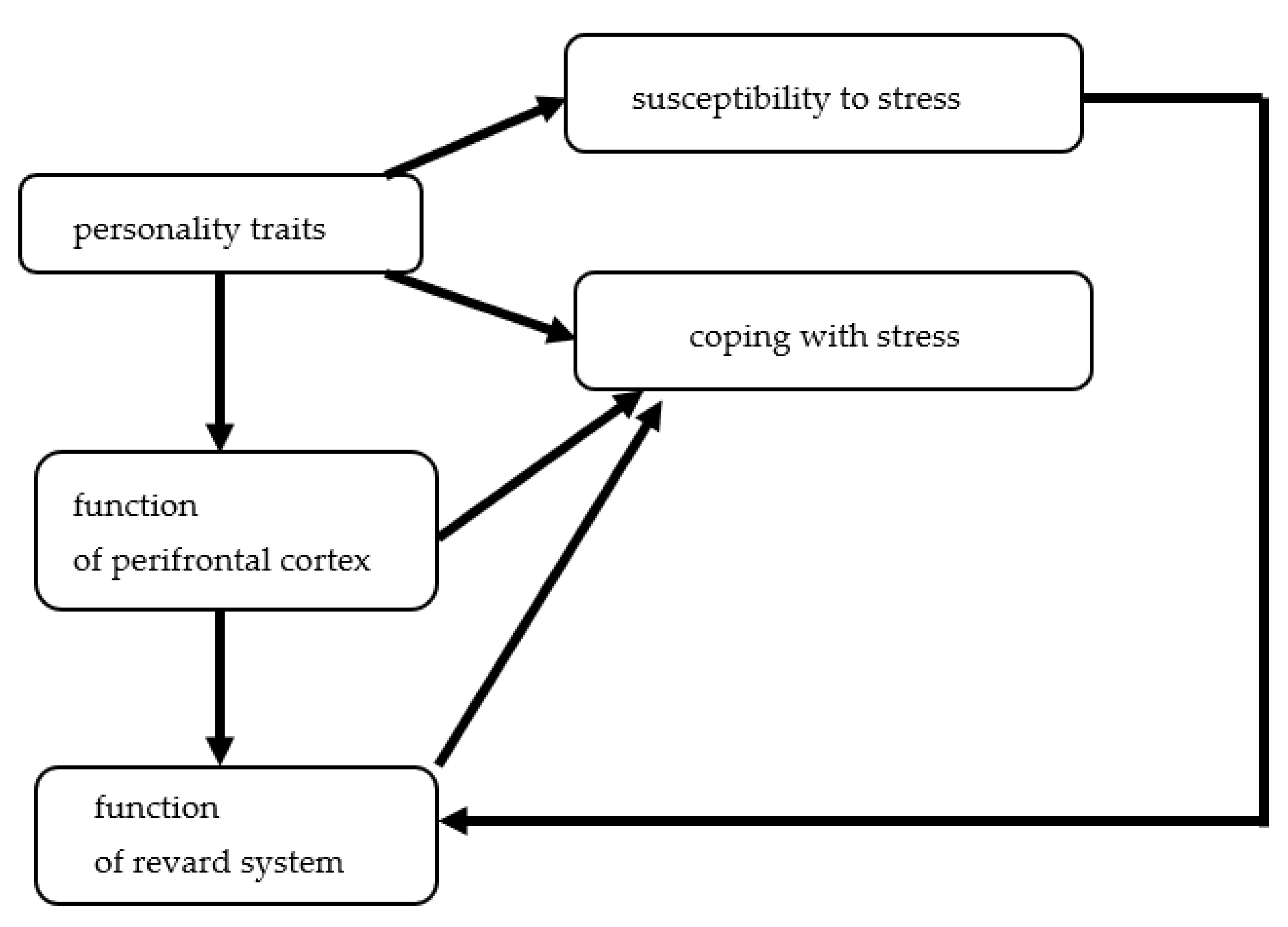
3. Emotional Eating, Definition, Risk Factors, Pathophysiologic Mechanism, and Consequences
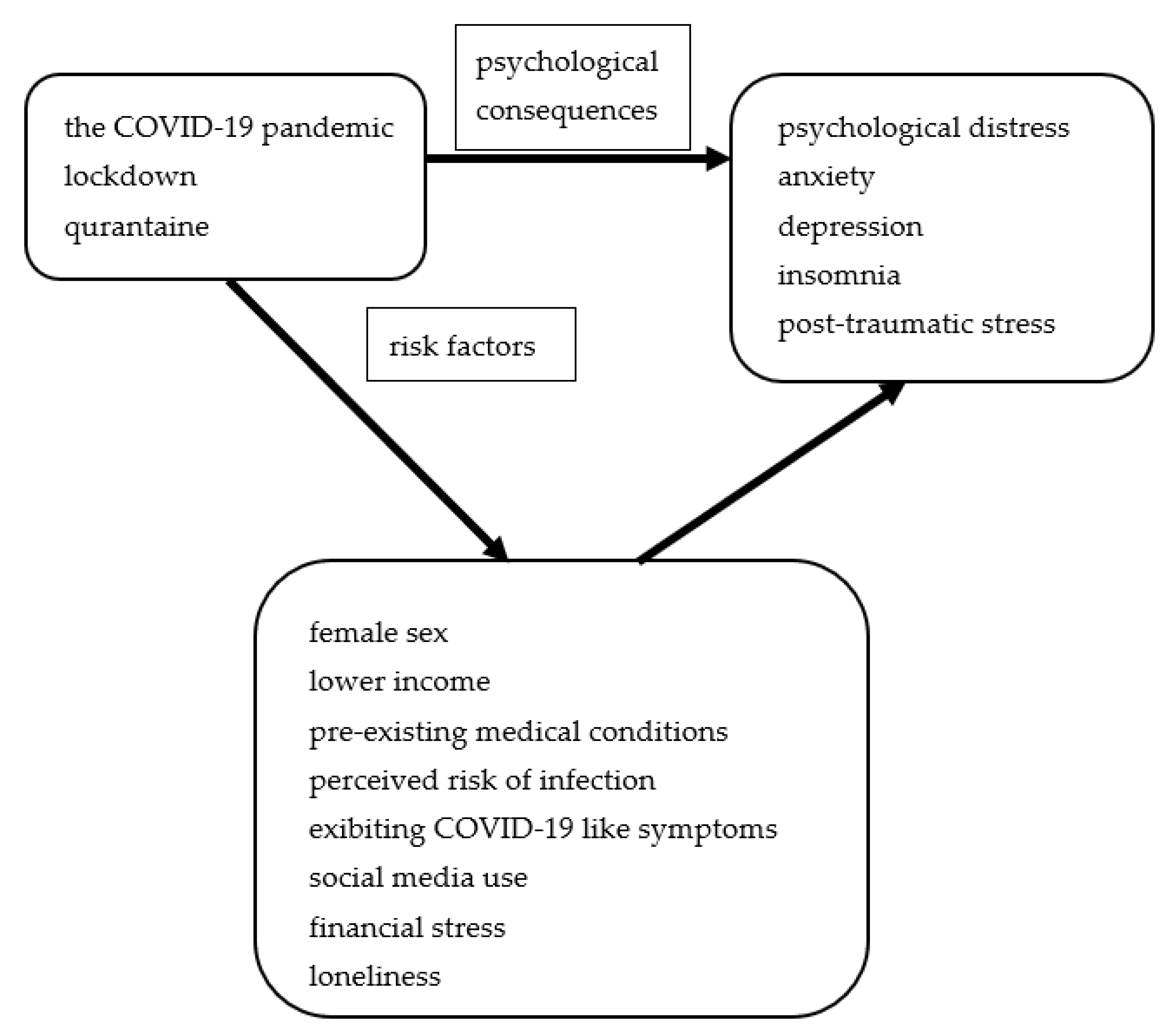
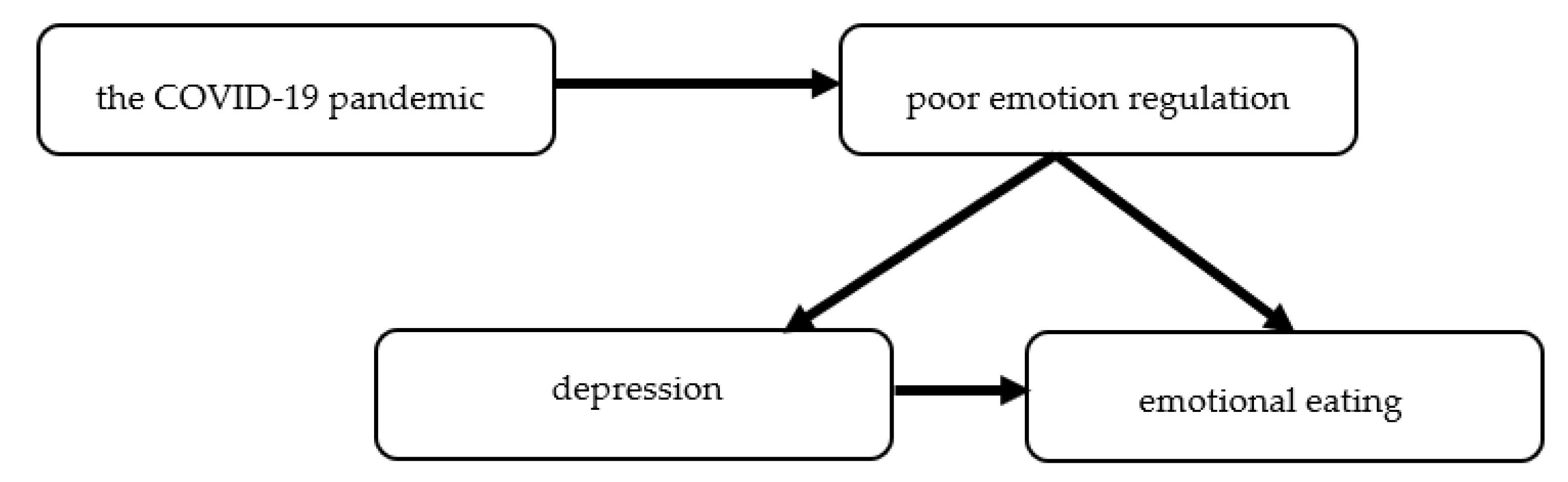
4. The Impact of the COVID-19 Pandemic on Mental Health
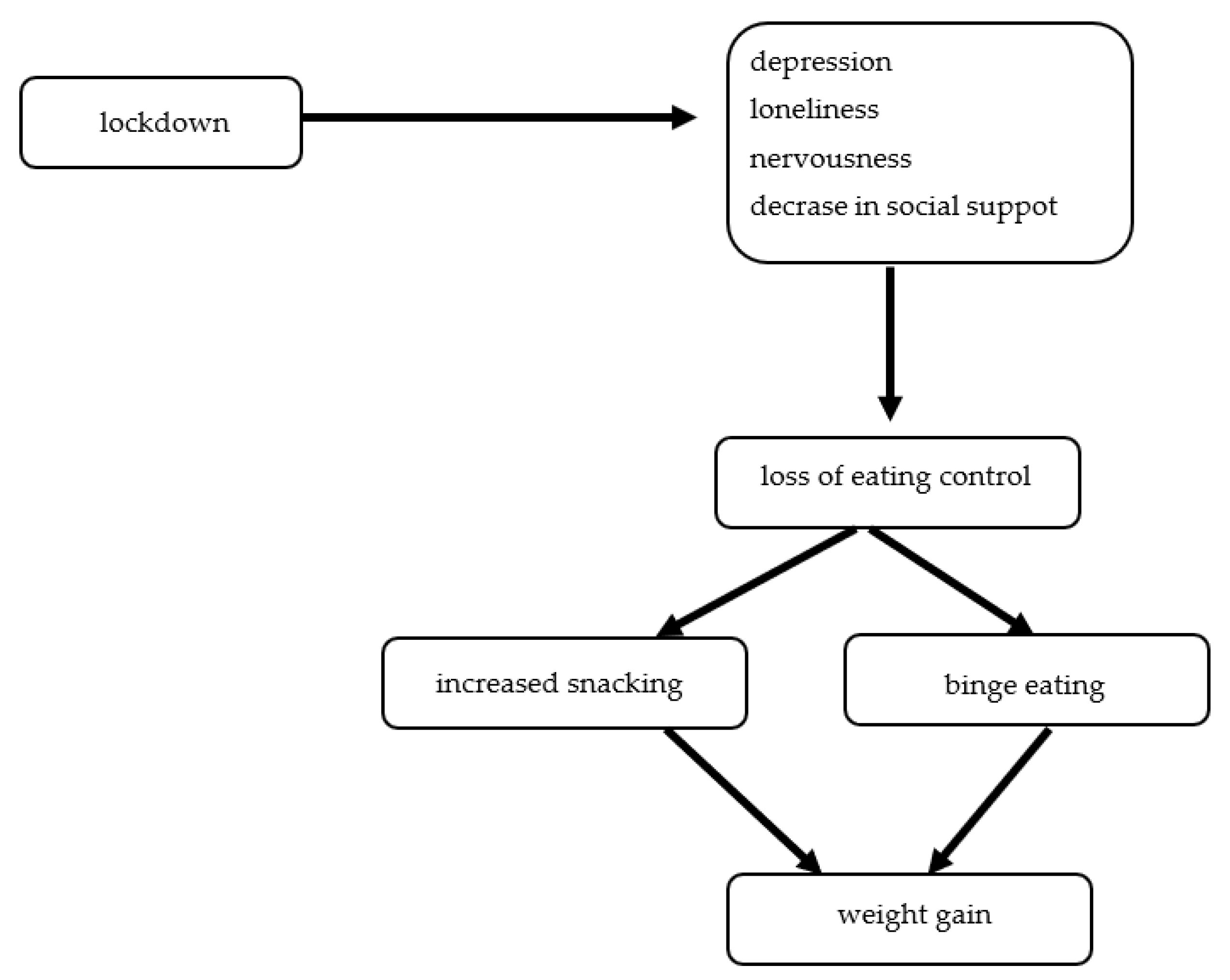
5. Emotional Eating during the COVID-19 Pandemic
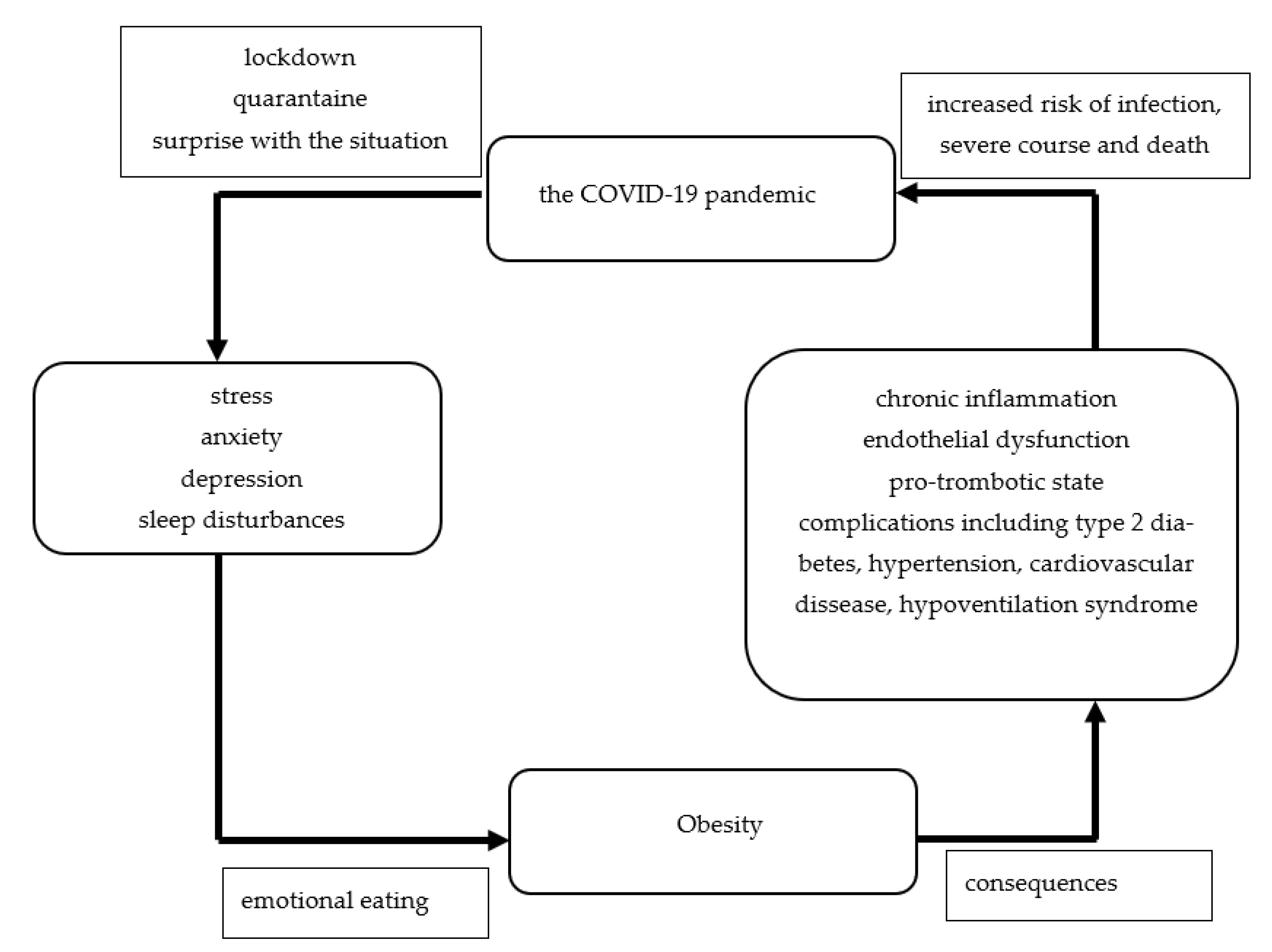
6. Emotional Eating during the COVID-19 Pandemic May Be the Risk Factor of Escalation of the Obesity Pandemic
7. The Limitation of the Review
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Oboza, P.; Ogarek, N.; Olszanecka-Glinianowicz, M.; Kocelak, P. COVID-19 and obesity: The confrontation of two pandemics. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 695–709. [Google Scholar] [PubMed]
- Daniels, N.F.; Burrin, C.; Chan, T.; Fusco, F. A systematic review of the Impact of the first year of COVID-19 on obesity risk factors: A pandemic fueling a pandemic? Curr. Dev. Nutr. 2022, 6, nzac011. [Google Scholar] [CrossRef]
- Bakaloudi, D.R.; Jeyakumar, D.T.; Jayawardena, R.; Chourdakis, M. The impact of COVID-19 lockdown on snacking habits, fast-food and alcohol consumption: A systematic review of the evidence. Clin. Nutr. 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- Cecchetto, C.; Aiello, M.; Gentili, C.; Ionta, S.; Osimo, S.A. Increased emotional eating during COVID-19 associated with lockdown, psychological and social distress. Appetite 2021, 160, 105122. [Google Scholar] [CrossRef]
- Barcın-Güzeldere, H.K.; Devrim-Lanpir, A. The association between body mass index, emotional eating and perceived stress during COVID-19 partial quarantine in healthy adults. Public Health Nutr. 2022, 25, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Bakaloudi, D.R.; Barazzoni, R.; Bischoff, S.C.; Breda, J.; Wickramasinghe, K.; Chourdakis, M. Impact of the first COVID-19 lockdown on body weight: A combined systematic review and a meta-analysis. Clin. Nutr. 2021, in press. [Google Scholar] [CrossRef]
- Konttinen, H.; van Strien, T.; Männistö, S.; Jousilahti, P.; Haukkala, A. Depression, emotional eating and long-term weight changes: A population-based prospective study. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 28. [Google Scholar] [CrossRef] [PubMed]
- Dagher, A. Functional brain imaging of appetite. Trends Endocrinol. Metab. 2012, 23, 250–260. [Google Scholar] [CrossRef]
- Rangel, A. Regulation of dietary choice by the decision-making circuitry. Nat. Neurosci. 2013, 16, 1717–1724. [Google Scholar] [CrossRef]
- Saljoughian, M. Emotional eating and binge eating disorder. U.S. Pharm. 2021, 46, 36–38. [Google Scholar]
- Haedt-Matt, A.A.; Keel, P.K.; Racine, S.E.; Burt, S.A.; Hu, J.Y.; Boker, S.; Neale, M.; Klump, K.L. Do emotional eating urges regulate affect? Concurrent and prospective associations and implications for risk models of binge eating. Int. J. Eat. Disord. 2014, 47, 874–877. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.; Curtis, C.; Levitan, R.D.; Carter, J.C.; Kaplan, A.S.; Kennedy, J.L. Evidence that “food addiction” is a valid phenotype of obesity. Appetite 2011, 57, 711–717. [Google Scholar] [CrossRef]
- Giuliani, N.R.; Mann, T.; Tomiyama, A.J.; Berkman, E.T. Neural systems underlying the reappraisal of personally craved foods. J. Cogn. Neurosci. 2014, 26, 1390–1402. [Google Scholar] [CrossRef] [PubMed]
- Hollmann, M.; Hellrung, L.; Pleger, B.; Schlögl, H.; Kabisch, S.; Stumvoll, M.; Villringer, A.; Horstmann, A. Neural correlates of the volitional regulation of the desire for food. Int. J. Obes. 2012, 36, 648–655. [Google Scholar] [CrossRef]
- Siep, N.; Roefs, A.; Roebroeck, A.; Havermans, R.; Bonte, M.; Jansen, A. Fighting food temptations: The modulating effects of short-term cognitive reappraisal, suppression and up-regulation on mesocorticolimbic activity related to appetitive motivation. Neuroimage 2012, 60, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Tryon, M.S.; Carter, C.S.; Decant, R.; Laugero, K.D. Chronic stress exposure may affect the brain’s response to high calorie food cues and predispose to obesogenic eating habits. Physiol. Behav. 2013, 120, 233–242. [Google Scholar] [CrossRef] [PubMed]
- Maier, S.U.; Makwana, A.B.; Hare, T.A. Acute stress impairs self-control in goal-directed choice by altering multiple functional connections within the brain’s decision circuits. Neuron 2015, 87, 621–631. [Google Scholar] [CrossRef] [PubMed]
- Hepworth, R.; Mogg, K.; Brignell, C.; Bradley, B.P. Negative mood increases selective attention to food cues and subjective appetite. Appetite 2010, 54, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Chao, A.; Grilo, C.M.; White, M.A.; Sinha, R. Food cravings mediate the relation- ship between chronic stress and body mass index. J. Health Psychol. 2015, 20, 721–729. [Google Scholar] [CrossRef]
- Oliver, G.; Wardle, J. Perceived effects of stress on food choice. Physiol. Behav. 1999, 66, 511–515. [Google Scholar] [CrossRef]
- Modrzejewska, A.; Czepczor-Bernat, K.; Brytek-Matera, A. The role of emotional eating and BMI in the context of chocolate consumption and avoiding situations related to body exposure in women of normal weight. Psychiatr. Pol. 2021, 55, 915–930. [Google Scholar] [CrossRef]
- Hill, D.C.; Moss, R.H.; Sykes-Muskett, B.; Conner, M.; O’Connor, D.B. Stress and eating behaviors in children and adolescents: Systematic review and meta-analysis. Appetite 2018, 123, 14–22. [Google Scholar] [CrossRef]
- Bilici, S.; Ayhan, B.; Karabudak, E.; Koksal, E. Factors affecting emotional eating and eating palatable food in adults. Nutr. Res. Pract. 2020, 14, 70–75. [Google Scholar] [CrossRef]
- Reichenberger, J.; Schnepper, R.; Arend, A.K.; Richard, A.; Voderholzer, U.; Naab, S.; Blechert, J. Emotional eating across different eating disorders and the role of body mass, restriction, and binge eating. Int. J. Eat. Disord. 2021, 54, 773–784. [Google Scholar] [CrossRef]
- Davis, C. From passive overeating to “food addiction”: A spectrum of compulsion and severity. ISRN Obes. 2013, 2013, 435027. [Google Scholar] [CrossRef] [PubMed]
- King, W.C.; Chen, J.Y.; Mitchell, J.E.; Kalarchian, M.A.; Steffen, K.J.; Engel, S.G.; Courcoulas, A.P.; Pories, W.J.; Yanovski, S.Z. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA 2012, 307, 2516–2525. [Google Scholar] [CrossRef] [PubMed]
- Conason, A.; Teixeira, J.; Hsu, C.-H.; Puma, L.; Knafo, D.; Geliebter, A. Substance use following bariatric weight loss surgery. JAMA Surg. 2013, 148, 145–150. [Google Scholar] [CrossRef]
- Steffen, K.J.; Engel, S.G.; Wonderlich, J.A.; Pollert, G.A.; Sondag, C. Alcohol and other addictive disorders following bariatric surgery: Prevalence, risk factors and possible etiologies. Eur. Eat. Disord. Rev. 2015, 23, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Luo, X.; Estill, J.; Wang, Q.; Lv, M.; Liu, Y.; Liu, E.; Chen, Y. The psychological impact of quarantine on coronavirus disease 2019 (COVID-19). Psychiatry Res. 2020, 291, 113193. [Google Scholar] [CrossRef] [PubMed]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Global Health 2020, 16, 57. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Jia, X.; Shi, H.; Niu, J.; Yin, X.; Xie, J.; Wang, X. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2021, 281, 91–98. [Google Scholar] [CrossRef]
- de Sousa, G.M.; Tavares, V.D.O.; de Meiroz Grilo, M.L.P.; Coelho, M.L.G.; de Lima-Araújo, G.L.; Schuch, F.B.; Galvão-Coelho, N.L. Mental health in COVID-19 pandemic: A meta-review of prevalence meta-analyses. Front. Psychol. 2021, 12, 703838. [Google Scholar] [CrossRef]
- Nochaiwong, S.; Ruengorn, C.; Thavorn, K.; Hutton, B.; Awiphan, R.; Chabaphai Phosuya, C.; Ruanta, Y.; Wongpakaran, N.; Wongpakaran, T. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 10173. [Google Scholar] [CrossRef]
- Necho, M.; Tsehay, M.; Birkie, M.; Biset, G.; Tadesse, E. Prevalence of anxiety, depression, and psychological distress among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Int. J. Soc. Psychiatry 2021, 67, 892–906. [Google Scholar] [CrossRef]
- Dragioti, E.; Li, H.; Tsitsas, G.; Lee, K.H.; Choi, J.; Kim, J.; Choi, Y.J.; Tsamakis, K.; Estradé, A.; Agorastos, A.; et al. A large-scale meta-analytic atlas of mental health problems prevalence during the COVID-19 early pandemic. J. Med. Virol. 2022, 94, 1935–1949. [Google Scholar] [CrossRef]
- Dong, F.; Liu, H.L.; Dai, N.; Yang, M.; Liu, J.P. A living systematic review of the psychological problems in people suffering from COVID-19. J. Affect. Disord. 2021, 292, 172–188. [Google Scholar] [CrossRef]
- Alimoradi, Z.; Ohayon, M.M.; Griffiths, M.D.; Lin, C.Y.; Pakpour, A.H. Fear of COVID-19 and its association with mental health-related factors: Systematic review and meta-analysis. BJPsych Open 2022, 8, e73. [Google Scholar] [CrossRef]
- Leung, C.M.C.; Ho, M.K.; Bharwani, A.A.; Cogo-Moreira, H.; Wang, Y.; Chow, M.S.C.; Fan, Y.; Galea, S.; Leung, G.M.; Ni, M.Y. Mental disorders following COVID-19 and other epidemics: A systematic review and meta-analysis. Transl. Psychiatry 2022, 12, 205. [Google Scholar] [CrossRef]
- Panda, P.K.; Gupta, J.; Chowdhury, S.R.; Kumar, R.; Meena, A.K.; Madaan, P.; Sharawat, I.K.; Gulati, S. Psychological and behavioral impact of lockdown and quarantine measures for COVID-19 pandemic on children, adolescents and caregivers: A systematic review and meta-analysis. J. Trop. Pediatr. 2021, 67, fmaa122. [Google Scholar] [CrossRef]
- Viner, R.; Russell, S.; Saulle, R.; Croker, H.; Stansfield, C.; Packer, J.; Nicholls, D.; Goddings, A.L.; Bonell, C.; Hudson, L.; et al. School closures during social lockdown and mental health, health behaviors, and well-being among children and adolescents during the first COVID-19 wave: A systematic review. JAMA Pediatr. 2022, 176, 400–409. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Mazidi, M.; Li, K.; Li, Y.; Chen, S.; Kirwan, R.; Zhou, H.; Yan, N.; Rahman, A.; Wang, W.; et al. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2021, 293, 78–89. [Google Scholar] [CrossRef] [PubMed]
- Rodgers, R.F.; Lombardo, C.; Cerolini, S.; Franko, D.L.; Omori, M.; Fuller-Tyszkiewicz, M.; Linardon, J.; Courtet, P.; Guillaume, S. The impact of the COVID-19 pandemic on eating disorder risk and symptoms. Int. J. Eat. Disord. 2020, 53, 1166–1170. [Google Scholar] [CrossRef]
- Bemanian, M.; Mæland, S.; Blomhoff, R.; Rabben, Å.K.; Arnesen, E.K.; Skogen, J.C.; Fadnes, L.T. Emotional eating in relation to worries and psychological distress amid the COVID-19 pandemic: A population-based survey on adults in Norway. Int. J. Environ. Res. Public Health 2020, 18, 130. [Google Scholar] [CrossRef] [PubMed]
- Madalı, B.; Alkan, Ş.B.; Örs, E.D.; Ayrancı, M.; Taşkın, H.; Kara, H.H. Emotional eating behaviors during the COVID-19 pandemic: A cross-sectional study. Clin. Nutr. ESPEN 2021, 46, 264–270. [Google Scholar] [CrossRef] [PubMed]
- Al-Musharaf, S. Prevalence and predictors of emotional eating among healthy young Saudi women during the COVID-19 pandemic. Nutrients 2020, 12, 2923. [Google Scholar] [CrossRef]
- McAtamney, K.; Mantzios, M.; Egan, H.; Wallis, D.J. Emotional eating during COVID-19 in the United Kingdom: Exploring the roles of alexithymia and emotion dysregulation. Appetite 2021, 161, 105120. [Google Scholar] [CrossRef]
- Coulthard, H.; Sharps, M.; Cunliffe, L.; van den Tol, A. Eating in the lockdown during the Covid 19 pandemic; self-reported changes in eating behaviour, and associations with BMI, eating style, coping and health anxiety. Appetite 2021, 161, 105082. [Google Scholar] [CrossRef]
- Modrzejewska, A.; Czepczor-Bernat, K.; Modrzejewska, J.; Matusik, P. Eating motives and other factors predicting emotional overeating during COVID-19 in a sample of Polish adults. Nutrients 2021, 13, 1658. [Google Scholar] [CrossRef]
- Cui, Y.; Liu, X.; Xiang, G.; Li, Q.; Xiao, M.; Chen, H. The association of restrained eating and overeating during COVID-19: A cross-lagged model. Nutrients 2021, 13, 4535. [Google Scholar] [CrossRef]
- Usubini, A.G.; Cattivelli, R.; Varallo, G.; Castelnuovo, G.; Molinari, E.; Giusti, E.M.; Pietrabissa, G.; Manari, T.; Filosa, M.; Franceschini, C.; et al. The relationship between psychological distress during the second wave lockdown of COVID-19 and emotional eating in Italian young adults: The mediating role of emotional dysregulation. J. Pers. Med. 2021, 11, 569. [Google Scholar] [CrossRef] [PubMed]
- Liboredo, J.C.; Anastácio, L.R.; Ferreira, L.G.; Oliveira, L.A.; Della Lucia, C.M. Quarantine during COVID-19 outbreak: Eating behavior, perceived stress, and their independently associated factors in a Brazilian sample. Front. Nutr. 2021, 8, 704619. [Google Scholar] [CrossRef] [PubMed]
- Ilktac, Y.H.; Savci, C.; Cil Akinci, A. Nutritional behavior during the COVID-19 pandemic: The association of fear and sleep quality with emotional eating. Eat. Weight Disord. 2022, 1–11. [Google Scholar] [CrossRef]
- Carpio-Arias, T.V.; Solís Manzano, A.M.; Sandoval, V.; Vinueza-Veloz, A.F.; Betancourt, A.R.; Betancourt Ortíz, S.L.; Vinueza-Veloz, M.F. Relationship between perceived stress and emotional eating. A cross sectional study. Clin. Nutr. ESPEN 2022, 49, 314–318. [Google Scholar] [CrossRef] [PubMed]
- Dominte, M.E.; Swami, V.; Enea, V. Fear of COVID-19 mediates the relationship between negative emotional reactivity and emotional eating. Scand. J. Psychol. 2022, 63, 462–467. [Google Scholar] [CrossRef]
- Pak, H.; Süsen, Y.; Nazlıgül, M.D.; Griffiths, M. The mediating effects of fear of COVID-19 and depression on the association between intolerance of uncertainty and emotional eating during the COVID-19 pandemic in Turkey. Int. J. Ment. Health Addict. 2022, 20, 1882–1896. [Google Scholar] [CrossRef]
- Costa, M.L.; Costa, M.G.O.; de Souza, M.F.C.; da Silva, D.G.; Dos Santos Vieira, A.D.; Mendes-Netto, R.S. Cognitive restraint, emotional eating and uncontrolled eating: Exploring factors associated with the cycle of behaviors during the COVID-19 pandemic. Food Qual. Prefer. 2022, 100, 104579. [Google Scholar] [CrossRef]
- Gao, Y.; Ao, H.; Hu, X.; Wang, X.; Huang, D.; Huang, W.; Han, Y.; Zhou, C.; He, L.; Lei, X.; et al. Social media exposure during COVID-19 lockdowns could lead to emotional overeating via anxiety: The moderating role of neuroticism. Appl. Psychol. Health Well Being 2022, 14, 64–80. [Google Scholar] [CrossRef]
- Shen, W.; Long, L.M.; Shih, C.H.; Ludy, M.J. A humanities-based explanation for the effects of emotional eating and perceived stress on food choice motives during the COVID-19 pandemic. Nutrients 2020, 12, 2712. [Google Scholar] [CrossRef]
- Sadler, J.R.; Thapaliya, G.; Jansen, E.; Aghababian, A.H.; Smith, K.R.; Carnell, S. COVID-19 stress and food intake: Protective and risk factors for stress-related palatable food intake in U.S. Adults. Nutrients 2021, 13, 901. [Google Scholar] [CrossRef]
- Almandoz, J.P.; Xie, L.; Schellinger, J.N.; Mathew, M.S.; Gazda, C.; Ofori, A.; Kukreja, S.; Messiah, S.E. Impact of COVID-19 stay-at-home orders on weight-related behaviours among patients with obesity. Clin. Obes. 2020, 10, e12386. [Google Scholar] [CrossRef] [PubMed]
- Białek-Dratwa, A.; Szczepańska, E.; Grajek, M.; Całyniuk, B.; Staśkiewicz, W. Health behaviors and associated feelings of remote workers during the COVID-19 pandemic-Silesia (Poland). Front. Public Health 2022, 10, 774509. [Google Scholar] [CrossRef] [PubMed]
- Puhl, R.M.; Lessard, L.M.; Larson, N.; Eisenberg, M.E.; Neumark-Stzainer, D. Weight stigma as a predictor of distress and maladaptive eating behaviors during COVID-19: Longitudinal findings from the EAT study. Ann. Behav. Med. 2020, 54, 738–746. [Google Scholar] [CrossRef] [PubMed]
- Athanasiadis, D.I.; Hernandez, E.; Hilgendorf, W.; Roper, A.; Embry, M.; Selzer, D.; Stefanidis, D. How are bariatric patients coping during the coronavirus disease 2019 (COVID-19) pandemic? Analysis of factors known to cause weight regain among postoperative bariatric patients. Surg. Obes. Relat. Dis. 2021, 17, 756–764. [Google Scholar] [CrossRef]
- Umano, G.R.; Rondinelli, G.; Rivetti, G.; Klain, A.; Aiello, F.; Del Giudice, M.M.; Decimo, F.; Papparella, A.; Del Giudice, E.M. Effect of COVID-19 lockdown on children’s eating behaviours: A longitudinal study. Children 2022, 9, 1078. [Google Scholar] [CrossRef]
- Wang, S.D.; Devjani, S.; Chillakanti, M.; Dunton, G.F.; Mason, T.B. The COMET study: Examining the effects of COVID-19-related perceived stress on Los Angeles Mothers’ dysregulated eating behaviors, child feeding practices, and body mass index. Appetite 2021, 163, 105209. [Google Scholar] [CrossRef]
- Zeigler, Z. COVID-19 Self-quarantine and weight gain risk factors in adults. Curr. Obes. Rep. 2021, 10, 423–433. [Google Scholar] [CrossRef]
- Khubchandani, J.; Price, J.H.; Sharma, S.; Wiblishauser, M.J.; Webb, F.J. COVID-19 pandemic and weight gain in American adults: A nationwide population-based study. Diabetes Metab. Syndr. 2022, 16, 102392. [Google Scholar] [CrossRef]
- Elmacıoğlu, F.; Emiroğlu, E.; Ülker, M.T.; Kırcali, B.Ö.; Oruç, S. Evaluation of nutritional behaviour related to COVID-19. Public Health Nutr. 2021, 24, 512–518. [Google Scholar] [CrossRef]
- López-Moreno, M.; López, M.T.I.; Miguel, M.; Garcés-Rimón, M. Physical and psychological effects related to food habits and lifestyle changes derived from COVID-19 home confinement in the Spanish population. Nutrients 2020, 12, 3445. [Google Scholar] [CrossRef]
- Zhang, J.; Zhang, Y.; Huo, S.; Ma, Y.; Ke, Y.; Wang, P.; Zhao, A. Emotional eating in pregnant women during the COVID-19 pandemic and its association with dietary intake and gestational weight gain. Nutrients 2020, 12, 2250. [Google Scholar] [CrossRef] [PubMed]
- Glazer, S.A.; Vallis, M. Weight gain, weight management and medical care for individuals living with overweight and obesity during the COVID-19 pandemic (EPOCH study). Obes. Sci. Pract. 2022. [Google Scholar] [CrossRef]
- Andreu, A.; Flores, L.; Molero, J.; Mestre, C.; Obach, A.; Torres, F.; Moizé, V.; Vidal, J.; Navinés, R.; Peri, J.M.; et al. Patients undergoing bariatric surgery: A special risk group for lifestyle, emotional and behavioral adaptations during the COVID-19 lockdown. Lessons from the first wave. Obes. Surg. 2022, 32, 441–449. [Google Scholar] [CrossRef] [PubMed]
- Olszanecka-Glinianowicz, M.; Dudek, D.; Filipiak, K.J.; Krzystanek, M.; Markuszewski, L.; Ruchała, M.; Tomiak, E. Treatment of overweight and obesity during and after a pandemic. Let’s not wait for the development of complications—New guidelines for doctors. Nutr. Obes. Metab. Surg. 2020, 24, 93–105. [Google Scholar]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Burnatowska, E.; Surma, S.; Olszanecka-Glinianowicz, M. Relationship between Mental Health and Emotional Eating during the COVID-19 Pandemic: A Systematic Review. Nutrients 2022, 14, 3989. https://doi.org/10.3390/nu14193989
Burnatowska E, Surma S, Olszanecka-Glinianowicz M. Relationship between Mental Health and Emotional Eating during the COVID-19 Pandemic: A Systematic Review. Nutrients. 2022; 14(19):3989. https://doi.org/10.3390/nu14193989
Chicago/Turabian StyleBurnatowska, Ewelina, Stanisław Surma, and Magdalena Olszanecka-Glinianowicz. 2022. "Relationship between Mental Health and Emotional Eating during the COVID-19 Pandemic: A Systematic Review" Nutrients 14, no. 19: 3989. https://doi.org/10.3390/nu14193989
APA StyleBurnatowska, E., Surma, S., & Olszanecka-Glinianowicz, M. (2022). Relationship between Mental Health and Emotional Eating during the COVID-19 Pandemic: A Systematic Review. Nutrients, 14(19), 3989. https://doi.org/10.3390/nu14193989






